Automated Breast Ultrasound vs. Mammography: A Comparative Analysis for Enhanced Cancer Detection and Screening
This article provides a comprehensive comparison between traditional mammography and automated breast ultrasound (ABUS) for breast cancer screening, with a focus on implications for clinical research and diagnostic development.
Automated Breast Ultrasound vs. Mammography: A Comparative Analysis for Enhanced Cancer Detection and Screening
Abstract
This article provides a comprehensive comparison between traditional mammography and automated breast ultrasound (ABUS) for breast cancer screening, with a focus on implications for clinical research and diagnostic development. It explores the foundational principles and technological evolution of both modalities, detailing their methodological applications, particularly in challenging populations like women with dense breast tissue. The analysis addresses key operational challenges and optimization strategies, including the integration of artificial intelligence and standardized protocols. Finally, it presents a rigorous validation of diagnostic performance through recent meta-analyses and large-scale trials, comparing sensitivity, specificity, and accuracy to guide future research and technological innovation in cancer diagnostics.
The Evolution of Breast Imaging: Unpacking the Core Technologies of Mammography and Automated Ultrasound
For decades, digital mammography (DM) and its advanced iteration, digital breast tomosynthesis (DBT), have served as the cornerstone of population-based breast cancer screening programs worldwide. The establishment of mammography as the gold standard is predicated on extensive evidence from large, randomized trials demonstrating its efficacy in reducing breast cancer mortality. This review examines the fundamental principles underlying mammography, consolidates its well-documented strengths, and provides a critical analysis of its inherent limitations, particularly in the context of evolving imaging technologies and specific patient populations. Furthermore, within the broader thesis of comparing traditional mammography with automated breast ultrasound (ABUS) research, this analysis will objectively evaluate their respective performances based on current empirical evidence. Understanding this comparative landscape is essential for researchers and clinicians aiming to optimize screening protocols and develop next-generation diagnostic tools.
Principles of Mammography
Mammography operates on the principle of using low-dose X-rays to generate high-resolution images of the internal structure of the breast. The technique relies on differential attenuation of X-rays by various breast tissues. Adipose tissue, being less dense, attenuates fewer X-rays, appearing radiolucent or dark on the resultant image. In contrast, fibroglandular tissue and potential calcifications attenuate more radiation, presenting as radiopaque or white areas. This contrast allows radiologists to identify architectural distortions, masses, and microcalcifications that are often the earliest signs of malignancy.
Full-field digital mammography (FFDM) represented a significant advancement over screen-film mammography by replacing the X-ray film with solid-state detectors. These detectors convert X-rays into electrical signals, which are then translated into digital images. This transition offers superior contrast resolution, particularly in the dense periphery of the breast, and facilitates image storage, retrieval, and transmission via Picture Archiving and Communication Systems (PACS). A further refinement, digital breast tomosynthesis (DBT), acquires multiple low-dose images from different angles across a limited arc. These projections are then reconstructed into a series of thin-slice, high-resolution images. This "3D mammography" technique mitigates the issue of tissue superposition, which is a primary limitation of 2D FFDM, by allowing radiologists to scroll through the breast tissue one layer at a time.
Established Strengths of Mammography
The preeminent strength of mammography is its proven role in reducing breast cancer mortality. Large-scale, organized service screening programs have consistently demonstrated a significant reduction in breast carcinoma mortality, a benefit that has been robustly confirmed through decades of data [1].
Mammography excels in the detection of specific malignant features, most notably microcalcifications. These tiny calcium deposits, which can be an early sign of ductal carcinoma in situ (DCIS), are often exquisitely visualized on mammography, sometimes remaining occult on other imaging modalities like ultrasound. The standardization of the BI-RADS (Breast Imaging-Reporting and Data System) lexicon, built around mammographic findings, has provided a unified framework for reporting, auditing, and guiding patient management, thereby enhancing the consistency and quality of breast care globally.
Table 1: Key Strengths of Mammography as a Screening Tool
| Strength | Description | Supporting Evidence |
|---|---|---|
| Mortality Reduction | Proven to reduce breast cancer mortality in large randomized controlled trials. | Organized service screening substantially reduces breast carcinoma mortality [1]. |
| Microcalcification Detection | High sensitivity for detecting suspicious microcalcifications, an early sign of cancer. | Critical for diagnosing DCIS; a capability where mammography often outperforms other modalities. |
| Standardized Framework | Use of the BI-RADS system ensures consistent reporting and management recommendations. | Provides a universal language for radiologists, surgeons, and oncologists. |
| Extensive Evidence Base | Decades of longitudinal data and technological refinements (e.g., DBT). | DBT improves performance over DM alone due to enhanced tissue differentiation [2]. |
Inherent Limitations and the Challenge of Dense Breasts
Despite its established role, the diagnostic performance of mammography is not uniform across all patient populations. Its most significant limitation is the degradation of sensitivity in women with dense breast tissue. Radiographically dense breasts have a higher proportion of fibroglandular tissue, which, like many cancers, appears white on a mammogram. This effect, known as the "masking" effect, can obscure underlying malignancies, reducing the sensitivity of mammography from over 85% in fatty breasts to as low as 50% in extremely dense breasts [3]. As breast density is also an independent risk factor for developing breast cancer—with women in the highest density categories having a 4 to 6 times higher risk compared to those with fatty breasts—this limitation affects a population at elevated risk [4].
Other inherent limitations include the use of ionizing radiation, albeit at low doses, and patient discomfort due to the necessary breast compression during the examination. Furthermore, the quest for high sensitivity can sometimes come at the cost of lower specificity, leading to false-positive results. These false positives necessitate additional imaging, ultrasound, or biopsy, contributing to increased healthcare costs, resource utilization, and patient anxiety.
Comparative Performance Data: Mammography vs. Emerging Modalities
Recent high-quality studies have directly compared the diagnostic efficacy of mammography against newer supplemental and standalone modalities, providing quantitative data for objective comparison. A large 2025 randomized controlled trial published in The Lancet compared abbreviated MRI (AB-MRI), ABUS, and contrast-enhanced mammography (CEM) in women with dense breasts and a negative mammogram. The findings were revealing: the cancer detection rate for ABUS was 4.2 per 1,000 examinations, significantly lower than the 17.4 for AB-MRI and 19.2 for CEM. For invasive cancers, the rate was 4.2 for ABUS versus 15.0 for AB-MRI and 15.7 for CEM [5]. The study concluded that "contrast-enhanced techniques such as abbreviated MRI and contrast-enhanced mammography have a superior performance compared with whole breast ultrasound" [5].
Another 2025 retrospective study offered a comprehensive comparison of four modalities within the same patient cohort. It confirmed the superior diagnostic performance of Breast MRI, which showed the highest sensitivity (95.1%), specificity (78.7%), and overall accuracy (87.2%). In contrast, DM demonstrated a sensitivity of 87.7% and a notably low specificity of 49.3%. Crucially, this study highlighted that while the combination of DM, DBT, and US achieved a high sensitivity of 96.3%, its specificity plummeted to 32%, illustrating a critical sensitivity-specificity trade-off in multimodal screening [2].
Table 2: Comparative Diagnostic Performance of Breast Imaging Modalities
| Modality | Sensitivity (%) | Specificity (%) | Overall Accuracy (%) | Key Strength / Weakness |
|---|---|---|---|---|
| Digital Mammography (DM) | 87.7 [2] | 49.3 [2] | - | Lower sensitivity in dense breasts; low specificity. |
| DM + DBT + US | 96.3 [2] | 32.0 [2] | - | High sensitivity but very low specificity (overdiagnosis risk). |
| ABUS alone | 80.43 [1] | 27.78 [1] | 71.82 [1] | Low specificity; valuable as a complement to DM. |
| Contrast-Enhanced Mammography (CEM) | 93.48 [1] | 11.11 [1] | 80.00 [1] | High cancer detection rate [5]. |
| Breast MRI | 95.1 [2] | 78.7 [2] | 87.2 [2] | Highest overall accuracy; constrained by cost & logistics. |
The Role of Automated Breast Ultrasound (ABUS) in the Screening Paradigm
ABUS was developed to address key limitations of handheld ultrasound (HHUS), namely operator-dependence and non-reproducibility, while leveraging the benefits of sonography in dense tissue [4] [3]. As a supplementary screening tool for women with dense breasts, ABUS increases the cancer detection rate beyond what is achievable with mammography alone. The SomoInsight study, a large multicenter trial, found that adding ABUS to FFDM increased the detection rate by 1.9 per 1000 women, boosting sensitivity by 26.7% [4].
The strengths of ABUS include its standardized acquisition by technologists, multiplanar reconstruction capabilities (particularly the diagnostic "surgical" coronal plane), and the absence of ionizing radiation. However, its disadvantages are notable and include a high false-positive rate, leading to a higher recall rate and lower specificity compared to mammography and MRI [1] [4]. It is also unable to assess the axilla or provide functional data on vascularization and elasticity. From a health economics perspective, a 2025 cost-effectiveness analysis concluded that adding ABUS to mammographic imaging is a cost-effective screening strategy for women with increased breast density or elevated risk [6].
Experimental Protocols and Research Workflows
To contextualize the data presented in this review, understanding the methodologies of key cited studies is crucial for researchers.
- The Lancet RCT Protocol (2025) [5]: This randomized controlled trial recruited women aged 50-70 with dense breasts and a negative mammogram. Participants were independently allocated to receive AB-MRI, ABUS, or CEM. The primary outcome was the cancer detection rate, confirmed by histopathology. The analysis was performed on a per-examination basis, and detection rates were compared for statistical significance.
- Single-Centre Comparative Analysis Protocol (2025) [1]: This study involved patients with focal breast lesions who underwent ABUS, FFDM, and CEM. A total of 169 lesions were identified, with 110 verified by histopathology. The diagnostic performance of each modality was assessed by calculating sensitivity, specificity, PPV, NPV, and accuracy against the histological gold standard. Statistical correlation between lesion margins and histopathology was also evaluated.
- Multimodal Deep Learning Workflow (2025) [7]: Reflecting a frontier in screening research, this study developed a deep learning-based model using both mammography and ultrasound images. The workflow involved: 1) Data Pre-processing: Localizing and cropping tumor regions in US images using YOLOv8 and grayscale normalization; 2) Data Augmentation: Applying random flipping and elastic deformation to increase dataset size and diversity; 3) Model Construction: Using a late-fusion strategy to train separate deep learning models on DM and US images, with the extracted features fused and connected to a classifier for the final diagnosis.
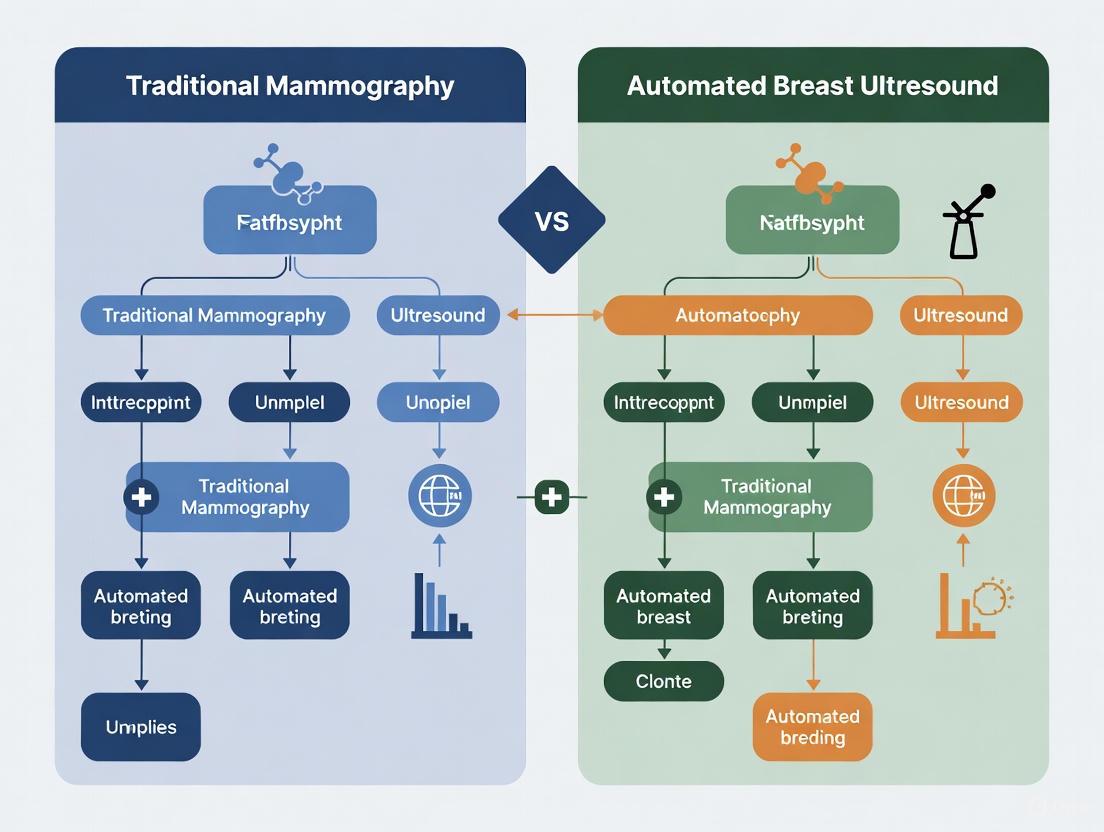
The diagram below illustrates a generalized diagnostic workflow for evaluating breast lesions, integrating multiple imaging modalities and outcome pathways.
Diagram 1: Integrated Diagnostic Workflow for Breast Lesion Evaluation. This flowchart outlines a potential clinical pathway integrating mammography, ABUS, and MRI for comprehensive diagnosis, highlighting decision points based on breast density and risk factors.
The Scientist's Toolkit: Key Research Reagents and Solutions
For researchers conducting experimental studies in breast imaging comparison, the following tools and methodologies are essential.
Table 3: Essential Research Tools for Breast Imaging Comparison Studies
| Research Tool / Solution | Function in Experimental Context |
|---|---|
| Full-Field Digital Mammography (FFDM) System | Provides the 2D digital baseline images for comparison; the standard against which new modalities are often evaluated. |
| Digital Breast Tomosynthesis (DBT) System | Generates 3D tomosynthesis slices for analysis, used to study the reduction of tissue superposition artifacts. |
| Automated Breast Ultrasound (ABUS) Scanner | Acquires standardized, reproducible 3D volumetric ultrasound data for quantitative analysis and comparison with mammography. |
| Contrast-Enhanced Mammography (CEM) or MRI | Serves as a higher-sensitivity comparator in studies, providing a reference for evaluating the performance of ABUS and standard MG. |
| Histopathology Database | The definitive gold standard for confirming malignancy; essential for calculating sensitivity, specificity, and accuracy of imaging tests. |
| Radiomics Software Platforms | Enables high-throughput extraction of quantitative features (shape, texture) from MG, ABUS, and MRI images for AI model development. |
| Deep Learning Frameworks (e.g., CNN models) | Used to develop and train multimodal classification models that fuse data from MG and US/ABUS to improve diagnostic performance [7]. |
Mammography remains the foundational pillar of breast cancer screening, with an unparalleled evidence base supporting its role in reducing mortality. Its strengths in detecting microcalcifications and its standardized implementation are undeniable. However, its inherent limitation in women with dense breasts—a population at elevated risk—is a significant challenge that the field must address. Contemporary research clearly demonstrates that while supplemental screening with ABUS effectively increases cancer detection rates and is a cost-effective strategy, its performance in terms of cancer detection yield and specificity is surpassed by contrast-enhanced techniques like MRI and CEM. The future of breast imaging research lies not in supplanting mammography, but in optimizing its integration with other modalities. The development of AI-based multimodal models that synergistically combine data from mammography, ABUS, and other imaging sources represents a promising frontier for enhancing diagnostic accuracy, personalizing screening approaches, and ultimately improving patient outcomes.
Breast cancer remains a pervasive global health challenge, with early detection being a cornerstone of reducing mortality. Mammography (MG) has long been the primary screening method, credited with a significant reduction in breast cancer deaths [8]. However, its effectiveness is substantially compromised in women with dense breast tissue—a condition present in approximately 40% of the screening population [9] [10]. This "density dilemma" creates a dual problem: dense breast tissue can mask underlying tumors on a mammogram due to a summation phenomenon where both tumors and glandular tissue appear white, and it is also an independent risk factor for developing breast cancer [8] [10]. The sensitivity of mammography can plummet from over 88% in fatty breasts to as low as 62% in extremely dense breasts, leaving many cancers undetected [10]. It is within this clinical gap that Automated Breast Ultrasound (ABUS) has emerged as a critical adjunctive imaging modality. ABUS offers a standardized, reproducible ultrasound-based approach designed to enhance cancer detection in dense breasts without the operator-dependency that characterizes traditional Handheld Ultrasound (HHUS). This guide provides a objective comparison of the diagnostic performance of ABUS against MG and other alternatives, supported by experimental data and detailed methodologies for the research community.
Performance Comparison: ABUS vs. Established Modalities
Extensive clinical studies have systematically evaluated the diagnostic performance of ABUS against mammography and handheld ultrasound. The data, summarized in the table below, reveals a nuanced landscape of complementary strengths.
Table 1: Diagnostic Performance of ABUS vs. Mammography and Handheld Ultrasound
| Modality | Sensitivity (%) | Specificity (%) | Area Under the Curve (AUC) | Key Study Findings |
|---|---|---|---|---|
| ABUS | 92.8 [11] | 93.0 [11] | 0.96 [12] | In women 40-69, ABUS had significantly higher sensitivity (93.5%) than MG (87.9%) [11]. |
| Mammography (MG) | 87.9 [11] | 91.6 [11] | - | MG sensitivity drops significantly in dense breasts; specificity is comparable to ABUS [11]. |
| Handheld Ultrasound (HHUS) | 96.3 [11] | 89.6 [11] | - | HHUS has higher sensitivity but lower specificity compared to ABUS [11]. |
| Contrast-Enhanced Ultrasound (CEUS) | 88 [12] | 76 [12] | 0.89 [12] | ABUS shows higher specificity and Diagnostic Odds Ratio (89 vs. 24) than CEUS [12]. |
Comparative Analysis with Other Modalities
ABUS vs. Contrast-Enhanced Mammography (CEM): A 2025 single-center study provided a direct comparison. It found that while CEM detected 88 lesions and ABUS detected 106 out of a total of 169, ABUS showed the highest compliance with histopathology for determining lesion size (p=0.258). The sensitivity and accuracy of the combination of FFDM and ABUS were 100% and 84.55%, respectively, outperforming the FFDM+CEM combination [13].
ABUS in a Multimodal Context: The superior post-test probability of ABUS (75%) compared to CEUS (48%) underscores its utility in confirming a diagnosis [12]. Furthermore, the integration of ABUS with mammography in dense breasts has been shown to find 35.7% more cancers than mammography alone, establishing its vital role as an adjunctive screening tool [10].
Insights from Key Experimental Studies
Multicenter Cross-Sectional Study in China
A large-scale study provides robust, head-to-head data on ABUS, HHUS, and MG.
Experimental Protocol: This multicenter study recruited 1,922 symptomatic women aged 30-69 across five tertiary hospitals in China [11]. Women aged 30-39 underwent ABUS and HHUS, while women aged 40-69 underwent ABUS, HHUS, and MG [11]. All images were interpreted using the BI-RADS lexicon, and all BI-RADS 4 and 5 lesions were confirmed pathologically, establishing a definitive gold standard [11]. The primary outcomes were the sensitivity and specificity of each modality, compared using appropriate statistical tests [11].
Key Outcomes: The study demonstrated that ABUS had a significantly higher specificity than HHUS (93.0% vs. 89.6%, p<0.01) while HHUS had a marginally higher sensitivity (96.3% vs. 92.8%, p=0.01) [11]. Crucially, in the older cohort, ABUS showed significantly higher sensitivity than mammography (93.5% vs. 87.9%) with comparable specificity, affirming its value in breast cancer diagnosis [11].
The TDSC-ABUS2023 Challenge
This recent challenge highlights the evolving role of artificial intelligence in enhancing ABUS.
Experimental Protocol: The TDSC-ABUS2023 challenge was organized to advance algorithmic research for tumor detection, segmentation, and classification in 3D ABUS images [14]. The initiative created a benchmark dataset to address the significant variability in tumor size and shape, unclear boundaries, and low signal-to-noise ratio that complicate ABUS image analysis [14]. Participants developed and submitted algorithms to perform these tasks on a well-labeled ABUS dataset, with performance evaluated against ground-truth annotations [14].
Key Outcomes: The challenge successfully established a public benchmark for ABUS image analysis and summarized top-performing algorithms [14]. It serves as an open-access platform to inspire and measure future developments in computer-aided diagnosis systems for ABUS, which can further reduce interpretation time and improve diagnostic consistency [14].
The Research Toolkit for ABUS Studies
Table 2: Essential Research Reagents and Materials for ABUS Studies
| Item | Function/Description | Example/Note |
|---|---|---|
| ABUS Imaging System | Acquires full breast volume scans automatically. | Systems like GE Healthcare's Invenia ABUS use a 6–14 MHz transducer for image acquisition [8]. |
| Ultrasound Coupling Gel | Ensures acoustic contact between transducer and skin. | Must be hypoallergenic and applied evenly to eliminate air gaps [8]. |
| Sponge Wedge | Positions the patient to evenly distribute breast tissue. | Placed under the patient's arm while supine for standardized scanning [8]. |
| BI-RADS Atlas | Standardized lexicon for reporting and classifying findings. | Essential for consistent image interpretation and study comparison [11]. |
| Histopathology Setup | Provides the gold standard for diagnostic confirmation. | Includes core needle biopsy (CNB), tissue processing, and H&E staining [13]. |
| Workstation with 3D MPR | Enables review and multi-planar reconstruction of volume data. | Allows radiologists to scroll through coronal, sagittal, and axial planes [15]. |
Workflow and Conceptual Framework
The integration of ABUS into clinical practice and research follows a structured workflow, while its primary value is conceptualized in addressing the limitations of mammography.
Diagram 1: ABUS research workflow.
Diagram 2: ABUS addresses the density dilemma.
The evidence demonstrates that ABUS has firmly established itself as a pivotal technology in the landscape of breast imaging, primarily by effectively addressing the significant diagnostic challenge posed by dense breast tissue. While mammography remains the foundational screening tool, ABUS provides a vital adjunct that significantly increases cancer detection rates with higher sensitivity and comparable or superior specificity to other modalities. Its standardized, reproducible nature mitigates the operator-dependency of HHUS, making it suitable for broader screening applications. For researchers and clinicians, the data indicates that the future of breast cancer detection lies not in a single monolithic technology, but in an integrated, intelligent approach. ABUS is a key component of this approach, contributing to a personalized, multi-modal strategy that promises to improve early detection and, ultimately, patient outcomes for the large population of women with dense breasts.
Breast density, defined as the proportion of fibroglandular tissue relative to fatty tissue visible on a mammogram, presents a significant dual challenge in breast cancer care. First, dense breast tissue is an independent risk factor for developing breast cancer. Second, it can mask tumors during standard mammographic screening, leading to decreased sensitivity and potential false-negative results [16]. This combination of increased risk and reduced detection capability creates a critical problem in oncology and diagnostic imaging. The recognition of breast density as a major factor influencing screening outcomes has catalyzed research into complementary imaging technologies, such as Automated Breast Ultrasound (ABUS), to improve early cancer detection in this population. Understanding the prevalence, risk implications, and technical challenges associated with breast density is fundamental to advancing breast cancer detection strategies and developing more personalized screening protocols for at-risk women.
Breast Density Prevalence and Risk Correlation
Classification and Prevalence
Breast density is clinically classified using the Breast Imaging Reporting and Data Systems (BI-RADS) into four categories: (A) almost entirely fatty, (B) scattered areas of fibroglandular density, (C) heterogeneously dense, and (D) extremely dense. Breasts categorized as C and D are considered "dense breasts" [16]. The prevalence of dense breasts varies significantly across populations and demographic factors. Approximately 43% of women aged 40-74 have heterogeneously or extremely dense breasts (types C and D) [16]. Prevalence demonstrates a strong inverse relationship with age, decreasing from 56.6% in women aged 40-44 years to 28.4% in women aged 85 and older [16].
Significant racial and ethnic variations in breast density prevalence have been documented. A large study of 2,667,207 mammography examinations found that dense breasts are most prevalent among Asian women (66.0%), followed by non-Hispanic White (45.5%), Hispanic/Latina (45.3%), and non-Hispanic Black (37.0%) women [17]. These differences persist even after adjusting for age, menopausal status, and body mass index (BMI), with Asian women maintaining a 19% higher prevalence and Black women an 8% higher prevalence of dense breasts compared to the overall population [17].
Table 1: Breast Density Prevalence Across Demographic Groups
| Demographic Factor | Category | Prevalence of Dense Breasts | Notes |
|---|---|---|---|
| Overall (Age 40-74) | - | 43% | Heterogeneously or extremely dense (BI-RADS C & D) [16] |
| By Age | 40-44 years | 56.6% | Decreases with advancing age [16] |
| 85+ years | 28.4% | [16] | |
| By Race/Ethnicity | Asian | 66.0% | Highest prevalence [17] |
| Non-Hispanic White | 45.5% | Slightly below average [17] | |
| Hispanic/Latina | 45.3% | Similar to White population [17] | |
| Non-Hispanic Black | 37.0% | Lowest prevalence [17] |
Mammographic Density and Cancer Risk
Mammographic density is a well-established independent risk factor for breast cancer, associated with a 1- to 6-fold increase in incidence [16]. A 2022 meta-analysis of nine observational studies determined that individuals with extremely dense breast tissue (BI-RADS D) had a 2.11-fold (95% CI 1.84-2.42) higher risk of developing breast cancer compared to those with scattered dense breast tissue (BI-RADS B) [16]. This risk association persists for extended periods, with studies demonstrating that the magnitude of association between percent density and breast cancer remains similar when the time since the mammogram is <2, 2 to <5, and 5 to <10 years [18].
The increased cancer risk associated with breast density has become sufficiently significant that it has been incorporated into epidemiologically based cancer risk calculation models, such as the Tyrer-Cuzick model (version 8), since 2022 [16]. This inclusion has enhanced the accuracy of risk stratification for both high-risk (>8% 10-year risk) and low-risk (<2% 10-year risk) women [16]. The biological mechanisms underlying this increased risk are thought to involve both mammographic masking (where dense tissue obscures tumors) and specific histopathological features associated with dense tissue, including increased stromal volume, epithelial content, and reduced lobular involution [16].
Impact on Conventional Mammography Performance
The Masking Effect and Sensitivity Reduction
The presence of dense breast tissue significantly impairs the performance of conventional mammography through a "masking effect," where the radiologically dense (white) fibroglandular tissue obscures tumors, which also appear white on mammograms [16] [8]. This phenomenon substantially reduces mammographic sensitivity, creating a critical diagnostic challenge. The sensitivity of full-field digital mammography (FFDM) decreases dramatically with increasing breast density—from approximately 98% for entirely fatty breasts (BI-RADS A) to just 48% for extremely dense breasts (BI-RADS D) [8]. This reduction in sensitivity leads to higher rates of interval cancers (cancers diagnosed between routine screenings) and delayed diagnoses in women with dense breasts [16] [19].
The masking effect occurs because mammography produces summation images where structures in the same plane overlap. In dense breasts, glandular and stromal tissues are poorly distinguishable, causing overlapping of structures that can obscure tumors [8]. Additionally, denser breasts are often more difficult to compress adequately during mammography, further exacerbating the tissue overlap issue and reducing image quality [8]. This technical limitation of conventional mammography has driven the development and evaluation of supplemental screening modalities for women with dense breasts.
Table 2: Impact of Breast Density on Mammography Performance
| BI-RADS Density Category | Breast Composition | Mammography Sensitivity | Key Challenges |
|---|---|---|---|
| A (Almost entirely fatty) | ≤25% fibroglandular tissue | ~98% [8] | Minimal masking effect |
| B (Scattered fibroglandular densities) | 25%-50% fibroglandular tissue | High | Limited masking effect |
| C (Heterogeneously dense) | 50%-75% fibroglandular tissue | Significantly reduced | Moderate masking effect, increased cancer risk [16] |
| D (Extremely dense) | ≥75% fibroglandular tissue | ~48% [8] | Severe masking effect, 2.11x higher cancer risk vs. category B [16] |
Automated Breast Ultrasound (ABUS) as a Complementary Modality
Technology and Workflow
Automated Breast Ultrasound (ABUS) is an advanced ultrasound technology developed to address the limitations of both mammography and handheld ultrasound (HHUS) in evaluating dense breasts. Approved by the U.S. Food and Drug Administration in 2012 as a supplemental screening tool for women with dense breasts, ABUS uses an automated transducer to systematically acquire volumetric images of the entire breast [20] [4]. Unlike HHUS, which is operator-dependent and provides limited field-of-view images, ABUS standardizes the image acquisition process, separating acquisition from interpretation and providing comprehensive, reproducible datasets [20] [4].
The ABUS examination typically involves imaging each breast in three standard views (anterior-posterior, medial, and lateral) using a high-frequency linear transducer (typically 6-14 MHz) [4] [8]. For women with larger breasts (cup size D or larger), additional views may be necessary to ensure complete coverage [4]. During acquisition, the transducer moves automatically across the breast in overlapping linear rows, generating volumetric data that is reconstructed into three orthogonal planes: axial, sagittal, and coronal [20]. The coronal plane, unique to ABUS, provides a "surgical view" of the breast that often reveals the "retraction phenomenon" characteristic of malignant lesions—appearing as hyperechoic straight lines radiating from the mass surface [4].
Comparative Performance Data
Multiple studies have demonstrated that ABUS significantly improves cancer detection rates when used as an adjunct to mammography in women with dense breasts. The SomoInsight study, one of the largest screening trials evaluating ABUS, included 15,318 asymptomatic women with dense breasts and found that adding ABUS to FFDM increased the cancer detection rate by 1.9 per 1000 women screened, representing a 26.7% increase in sensitivity [4]. Other studies have reported even greater improvements, with cancer detection rates increasing by 2.4 to 7.7 per 1000 women screened when ABUS was combined with FFDM compared to FFDM alone [4].
A 2025 comparative analysis of ABUS and contrast-enhanced mammography (CEM) found that while CEM demonstrated higher sensitivity (93.48% vs. 80.43%) and accuracy (80% vs. 71.82%) than ABUS, the combination of FFDM and ABUS achieved 100% sensitivity with an AUC of 0.947 [1]. The same study reported that ABUS showed the highest correlation with histopathology in determining lesion size (p=0.258) and detected 36 additional lesions not visible on other imaging examinations [1].
Recent data from the BRAID study, a large prospective trial published in 2025, provides direct comparison of multiple supplemental screening modalities. This study of over 9,000 women with dense breasts and negative mammograms found that ABUS detected 4.2 cancer cases per 1000 examinations, compared to 17.4 for abbreviated MRI (AB-MRI) and 19.2 for CEM [19]. While AB-MRI and CEM demonstrated superior detection rates, ABUS had a lower recall rate (4%) compared to both AB-MRI (9.7%) and CEM (9.7%) [19].
Table 3: Comparative Performance of Imaging Modalities in Dense Breasts
| Imaging Modality | Sensitivity (%) | Specificity (%) | Cancer Detection Rate (per 1000 exams) | Recall Rate (%) |
|---|---|---|---|---|
| FFDM alone | 40-76 [4] | 85.4-99.7 [4] | Baseline | 150.2/1000 [4] |
| FFDM + ABUS | 81-100 [1] [4] | 72-98.7 [1] [4] | +1.9 to +7.7 over FFDM alone [4] | 284.9/1000 [4] |
| Abbreviated MRI | - | - | 17.4 [19] | 9.7 [19] |
| Contrast-Enhanced Mammography | 93.48 [1] | 11.11 [1] | 19.2 [19] | 9.7 [19] |
Research Reagent Solutions for Breast Density and ABUS Studies
Table 4: Essential Research Reagents and Materials for Breast Density and ABUS Studies
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| ABUS Imaging Systems | Volumetric breast image acquisition | Invenia ABUS (GE Healthcare); ACUSON S2000 ABVS (Siemens) [20] |
| High-Frequency Transducers | Tissue penetration and resolution | 6-14 MHz linear transducers optimized for automated scanning [8] |
| BI-RADS Reference Standards | Standardized density classification and reporting | BI-RADS 5th edition density categories (A-D) [16] |
| Image Analysis Software | Quantitative density measurement and feature extraction | Computerized texture analysis, convolutional neural networks (CNN) for automated classification [20] [16] |
| Radiomics Analysis Platforms | High-dimensional feature extraction from images | Texture, shape, and wavelet feature analysis; machine learning model development [20] |
| Histopathological Validation Tools | Correlation of imaging findings with tissue pathology | Immunohistochemistry markers, tissue staining for fibrosis and lobular involution [16] |
Experimental Protocols for ABUS Performance Evaluation
Comparative Diagnostic Performance Study
A 2025 single-center study provides a robust methodological framework for comparing ABUS with other complementary breast imaging modalities [1]. The study enrolled 81 patients with focal breast lesions who underwent ABUS, FFDM, and contrast-enhanced mammography (CEM), with 169 focal lesions identified and 110 lesions histopathologically verified (92 malignant, 5 B3 lesions, 13 benign) [1].
Key Methodology:
- Patient Selection: Consecutive patients with focal breast lesions identified through screening or diagnostic workup
- Imaging Protocol: All participants underwent ABUS, FFDM, and CEM examinations
- Reference Standard: Histopathological verification through biopsy or surgical resection
- Image Analysis: Qualitative assessment of lesion characteristics (margin, size) and quantitative analysis of detection rates
- Statistical Analysis: Calculation of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy for each modality, with comparison of area under the curve (AUC) for combined approaches [1]
This study demonstrated that while CEM showed superior individual performance metrics, the combination of FFDM and ABUS achieved the highest sensitivity (100%) with excellent accuracy (AUC=0.947) [1].
Artificial Intelligence and Radiomics Analysis
Emerging research methodologies incorporate artificial intelligence (AI) and radiomics to enhance ABUS performance. The standard workflow for AI-based ABUS radiomics analysis involves multiple systematic stages [20]:
Protocol Steps:
- Image Acquisition and Pre-processing: Standardized ABUS volume acquisition with noise reduction and resolution enhancement
- Tumor Segmentation: Manual, semi-automatic, or automatic delineation of regions of interest (ROIs)
- Feature Extraction: High-throughput extraction of quantitative features including shape, texture, and wavelet features
- Feature Selection: Dimensionality reduction using filter, wrapper, or embedded methods to identify most predictive features
- Model Building and Validation: Development of machine learning or deep learning classifiers with cross-validation and external validation [20]
This methodology enables the extraction of subvisual imaging biomarkers that can improve diagnostic accuracy and risk stratification beyond conventional image interpretation.
The challenge of breast density significantly impacts both cancer risk and detection capability, necessitating advanced imaging approaches beyond conventional mammography. ABUS has emerged as a valuable standardized supplemental modality that improves cancer detection rates in women with dense breasts, particularly when combined with mammography. Current evidence supports its role in providing reproducible, comprehensive evaluation of breast tissue, with the unique coronal plane offering additional diagnostic information. However, recent comparative studies indicate that while ABUS provides definite improvements over mammography alone, alternative supplemental modalities like abbreviated MRI and contrast-enhanced mammography may offer higher detection rates, though with different trade-offs in accessibility, cost, and recall rates. Future research directions should focus on optimizing patient selection criteria for different supplemental screening modalities, further developing AI and radiomics approaches to enhance ABUS performance, and establishing cost-effective integrated screening protocols for women with dense breasts.
Breast cancer remains a paramount public health challenge, being the most frequent malignant tumor diagnosed in women worldwide [21]. The evolution of breast imaging technologies has been fundamentally driven by a critical limitation of the foundational screening tool: the reduced sensitivity of conventional 2D mammography in radiographically dense breasts, where overlapping tissue can mask cancers [22]. This technological trajectory has progressed from two-dimensional projections to advanced three-dimensional modalities that minimize tissue superposition, namely Digital Breast Tomosynthesis (DBT) and volumetric ultrasound, including Automated Breast Ultrasound (ABUS). DBT, often termed 3D mammography, utilizes a moving X-ray tube to acquire multiple low-dose images across an arc, which are reconstructed into thin slices of the breast [23]. ABUS, on the other hand, employs automated transducers to generate a three-dimensional volume dataset of the entire breast using ultrasound, providing a completely different contrast mechanism based on acoustical properties [24]. This guide provides an objective, data-driven comparison of the diagnostic performance, technical protocols, and clinical applications of 2D mammography, DBT, and ABUS, with a specific focus on their role in evaluating breast masses within the context of dense breast tissue.
Technical Principles and Imaging Protocols
2D Digital Mammography (FFDM)
Full-Field Digital Mammography (FFDM) produces a single, two-dimensional image of the compressed breast from two standard views: craniocaudal (CC) and mediolateral oblique (MLO) [23]. Each pixel in the image represents the summation of X-ray attenuation through the entire thickness of the breast. This tissue superposition is the primary cause of both false positives, where normal overlapping tissue simulates a lesion, and false negatives, where cancers are obscured by dense parenchyma [25] [22]. The radiation dose per view for FFDM typically ranges between 150-250 millirads [22].
Digital Breast Tomosynthesis (DBT)
DBT addresses the limitation of tissue superposition by acquiring a series of low-dose projection images as the X-ray tube moves through a limited arc (typically 11-60 degrees) over a few seconds [22] [23]. The number of projections varies by manufacturer, typically from 9 to 25 exposures [22]. These projection images are then reconstructed using algorithms (e.g., filtered back projection, iterative reconstruction) into a stack of thin, high-resolution slices, usually 1 mm thick, for radiologist review [22] [23]. This allows the radiologist to scroll through the breast tissue in thin sections, effectively "unmasking" lesions hidden by overlapping tissue.
- Radiation Dose: The radiation dose for a DBT exam is a key consideration. When DBT is combined with a standard 2D mammogram (combo-mode), the total dose is higher than FFDM alone. However, the development of synthesized 2D images (C-View), generated from the DBT dataset, allows for a radiation dose that is only about 19% higher on average than FFDM alone, a significant reduction from the combo-mode [23]. Some 1-view DBT protocols can achieve a dose comparable to or even slightly lower than 2D mammography [23].
Automated Breast Ultrasound (ABUS)
ABUS is a three-dimensional volumetric imaging technique designed to overcome the operator-dependence and time-intensive nature of handheld ultrasound (HHUS) for screening [24]. A standard ABUS protocol involves scanning each breast separately in three planes: anterior-posterior (AP), lateral (LAT), and medial (MED), resulting in a minimum of six volume sets [24]. For larger breasts, additional views may be required to ensure complete coverage. The system uses a long, automated transducer that applies uniform compression, and the volume data is automatically processed with multiplanar reconstruction (axial, coronal, and sagittal planes) [24]. The entire examination, including patient preparation, takes approximately 15-20 minutes [24]. ABUS is particularly valuable as a supplemental screening tool following a negative mammogram in women with dense breasts (BI-RADS density C and D) [24].
Table 1: Summary of Key Technical Parameters for Breast Imaging Modalities
| Parameter | 2D FFDM | Digital Breast Tomosynthesis (DBT) | Automated Breast Ultrasound (ABUS) |
|---|---|---|---|
| Fundamental Principle | 2D X-ray projection | Quasi-3D reconstruction from limited-angle X-ray projections | 3D volumetric imaging using ultrasound |
| Standard Views | CC, MLO (2 per breast) | CC, MLO (2 per breast) | AP, LAT, MED (≥3 per breast) |
| Image Output | 2 flat images per view | ~60-120 thin slices (1 mm) per view | Hundreds of images per volume set |
| Primary Strength | Calcification assessment | Mass detection, characterizing margins, reducing tissue overlap | Detecting mammographically-occult cancers in dense tissue |
| Radiation | Yes (reference dose) | Similar to slightly higher than FFDM; ~19% higher with synthetic 2D | No |
| Exam Duration | ~10 minutes [26] | Similar to FFDM | 15-20 minutes [24] |
Comparative Diagnostic Performance
The transition from 2D to 3D imaging is substantiated by a wealth of data demonstrating improvements in key performance metrics, including cancer detection rates, recall rates, and diagnostic accuracy.
Cancer Detection and Recall Rates
A large meta-analysis comparing DBT plus synthetic 2D mammography to 2D mammography alone demonstrated a statistically significant increase in the cancer detection rate (CDR) from 4.68 to 7.40 per 1000 women screened [23]. The same analysis showed that the recall rate (the proportion of women called back for additional imaging) dropped dramatically from 78.8 to 42.3 per 1000 screened with the combined DBT and synthetic 2D approach [23]. This combination of higher CDR and lower recall rate represents a major advancement in screening efficiency.
For ABUS used as a supplemental screening tool in women with dense breasts, the incremental cancer detection rate compared to mammography alone ranges from 1.9 to 7.7 cases per 1000 women [24]. The cancers detected by supplemental ABUS are often small, invasive, and node-negative, indicating a benefit for early detection [24]. A direct, prospective comparison study of DBT and ABUS in characterizing breast masses found their sensitivity to be equivalent (100% for both), while DBT showed a marginally higher specificity (81.25% for DBT vs. 75% for ABUS) [27].
Characterization of Breast Masses
The ability to characterize a detected mass—distinguishing benign from malignant features—is critical for avoiding unnecessary biopsies. DBT excels in this domain by providing superior visualization of mass margins and architecture. It allows radiologists to better assess spiculations and the true extent of a lesion, which are crucial indicators of malignancy [21]. Similarly, ABUS provides detailed information on mass shape, margins, and echogenicity. A study comparing the two modalities found high agreement in assessing the shape and location of masses, though DBT was more sensitive in detecting associated calcifications [27]. The study also noted that DBT was superior to ABUS in demonstrating the extension of a lesion beyond the mass margin [27].
Table 2: Comparison of Diagnostic Performance Metrics in Screening
| Metric | 2D FFDM | DBT (+ Synthetic 2D) | ABUS (Supplemental) |
|---|---|---|---|
| Cancer Detection Rate (per 1000) | 4.68 [23] | 7.40 [23] | Incremental 1.9 - 7.7 [24] |
| Recall Rate (per 1000) | 78.8 [23] | 42.3 [23] | Increases vs. mammography alone [24] |
| Sensitivity (Mass Characterization) | Benchmark | 100% [27] | 100% [27] |
| Specificity (Mass Characterization) | Benchmark | 81.25% [27] | 75% [27] |
| Strength in Dense Breasts | Low sensitivity, high masking | Improved over 2D | High for mammographically-occult cancers |
Experimental Protocols and Methodologies
For researchers designing studies to evaluate these technologies, understanding the standardized protocols and methodologies used in pivotal clinical trials is essential.
Digital Breast Tomosynthesis Characterization Study
A prospective study comparing DBT and ABUS for mass characterization provides a robust experimental model [27].
- Patient Cohort: 32 women with 37 breast masses (16 benign, 21 malignant) detected via clinical or mammographic exam.
- Image Acquisition: All patients underwent both DBT and ABUS examinations. DBT was performed using a GE prototype system, acquiring CC and MLO views with breast compression similar to mammography. ABUS was performed using a GE Invenia ABUS system, with a layer of lotion applied and a curved transducer panel used to flatten the tissue against the body [27].
- Image Analysis: Images from both modalities were analyzed in consensus by two experienced radiologists blinded to pathological data. Each mass was evaluated for shape, margin, asymmetry, calcifications, number, location, extension, skin thickening, and final BI-RADS classification [27].
- Reference Standard: Pathological results (for 32 masses) and imaging follow-up for typically benign findings (5 masses) served as the gold standard [27].
- Statistical Analysis: Data were analyzed using SPSS. Standard diagnostic indices (sensitivity, specificity, PPV, NPV) were calculated, and categorical data were compared using the Chi-square test [27].
Automated Breast Ultrasound (ABUS) with CAD
A multiple-reader, multiple-case study evaluated the impact of Computer-Aided Detection (CAD) on ABUS performance [28].
- Sample Selection: 120 unilateral ABUS examinations were randomly selected from a multi-institutional archive, comprising 30 malignant (20 of which were mammography-occult), 30 benign, and 60 normal cases. All cases had histopathological verification or ≥2 years of negative follow-up [28].
- Reading Protocol: Eight radiologists read each case twice: once with CAD (CAD-ABUS) and once without (ABUS), with a washout period of over 8 weeks between sessions. For each case, readers provided a BI-RADS score and a level of suspiciousness (0-100) [28].
- Outcome Measures: The primary outcomes were reading time (RT), sensitivity, specificity, Positive Predictive Value (PPV), and the area under the curve (AUC). These metrics were compared between the CAD-ABUS and ABUS reading sessions [28].
- Key Finding: The use of CAD for ABUS significantly reduced the average reading time per case (133.4 seconds with CAD vs. 158.3 seconds without) without compromising sensitivity or specificity, demonstrating its potential to improve workflow efficiency [28].
Visualization of Workflows and Applications
The distinct imaging principles of DBT and ABUS lead to different clinical workflows and strengths, which can be visualized in the following diagram.
Diagram 1: Imaging Workflows and Primary Outcomes
The Scientist's Toolkit: Research Reagents and Materials
For researchers conducting clinical studies or developing algorithms in breast imaging, familiarity with the following key tools and technologies is essential.
Table 3: Essential Research Tools and Technologies
| Item | Function in Research | Example/Note |
|---|---|---|
| DBT System with Synthetic 2D | Enables comparison of DBT performance against 2D without increased radiation dose from combo-mode. | Key for studies on radiation dose optimization [23]. |
| ABUS System with Dedicated Workstation | Provides standardized 3D ultrasound volumes for radiologist interpretation or CAD development. | Volume data cannot be viewed on standard PACS [24]. |
| Computer-Aided Detection (CAD) Software | Object of study for improving reading efficiency and reducing perceptual errors. | Shown to reduce ABUS reading time without loss of accuracy [28]. |
| BI-RADS Atlas (5th Ed. or later) | Standardizes lexicon for describing findings, density, and final assessment categories across studies. | Critical for ensuring consistent data collection and reporting [21]. |
| Statistical Analysis Software (e.g., SPSS) | For analysis of diagnostic performance metrics (sensitivity, specificity, AUC) and comparative statistics. | Used in pivotal studies to calculate performance indices [27]. |
| Annotated Image Databases | Serves as a ground-truthed dataset for training and validating machine learning algorithms. | Should include pathology-proven cases with different modalities [28]. |
The technological trajectory from 2D mammography to 3D tomosynthesis and volumetric ultrasound scanning represents a paradigm shift in breast imaging, driven by the need to overcome the fundamental physical limitation of tissue superposition. DBT has firmly established itself as a superior screening tool, increasing cancer detection while reducing false positives, and is increasingly becoming the standard of care. ABUS has carved out a vital role as a reproducible and effective supplemental screening modality, particularly for women with dense breasts where mammography's sensitivity is compromised. The choice of modality is not a matter of one being universally superior, but rather of understanding their complementary strengths. Future directions point toward the integration of artificial intelligence, further refinement of synthetic 2D imaging to reduce radiation, and the continued use of multi-modal approaches to achieve the ultimate goal of detecting every breast cancer at its earliest, most treatable stage.
Operationalizing Screening: Clinical Workflows and Application Scenarios for ABUS and Mammography
Breast cancer remains a pervasive global health challenge, driving the continuous evolution of imaging technologies for early detection and diagnosis. Mammography has served as the cornerstone of breast cancer screening for decades, while Automated Breast Ultrasound (ABUS) has more recently emerged as a standardized, operator-independent ultrasound technique. Understanding the distinct procedural methodologies of these two imaging modalities is critical for researchers and clinicians aiming to optimize diagnostic pathways. This guide provides a systematic, step-by-step comparison of ABUS and mammography image acquisition processes, supported by experimental data and technical protocols, to elucidate their respective roles in breast imaging research and clinical practice.
The core technologies underpinning mammography and ABUS are fundamentally different, which directly influences their application and diagnostic capabilities.
Mammography: This technique utilizes low-dose ionizing radiation to create two-dimensional or three-dimensional summation images of the compressed breast. The differential absorption of X-rays by various breast tissues (adipose, glandular, pathological) creates the image contrast. Recent advancements include Digital Breast Tomosynthesis (DBT), which acquires images from multiple angles to create thin-slice reconstructions, reducing tissue superposition artifacts [29]. As a screening tool, its primary strength lies in detecting microcalcifications and architectural distortions, though its sensitivity decreases significantly in dense breast tissue [30].
Automated Breast Ultrasound (ABUS): Approved by the FDA in 2012 as a supplemental screening tool, ABUS employs high-frequency sound waves (typically 6–14 MHz) to generate volumetric data of the entire breast [4] [20]. A transducer moves automatically across the breast, emitting ultrasound waves and receiving echoes to construct multiplanar images (axial, sagittal, and coronal). A key technological advantage is the reconstruction of the coronal plane, which provides a unique "surgical view" of the breast parenchyma and can reveal the "retraction phenomenon" often associated with malignant lesions [4]. ABUS was developed to standardize breast ultrasound, eliminating the operator-dependency of handheld ultrasound (HHUS) and enabling comprehensive documentation for comparison across serial exams [8].
Table 1: Core Technological Principles of Mammography and ABUS
| Feature | Mammography | ABUS |
|---|---|---|
| Physical Principle | Ionizing Radiation | High-Frequency Sound Waves |
| Primary Output | 2D or 3D Summation Images | Volumetric, Multiplanar Reconstructions |
| Key Technological Advancements | Full-Field Digital Mammography (FFDM), Digital Breast Tomosynthesis (DBT) | Whole-Breast Volumetric Scanning, Coronal Plane Reconstruction |
| Standard of Practice | Primary screening tool; well-established guidelines | Supplemental screening for dense breasts; evolving guidelines |
Step-by-Step Image Acquisition Protocols
A detailed comparison of the acquisition protocols reveals profound differences in patient positioning, preparation, and the technical execution of the scan, each with distinct implications for patient experience and image quality.
Patient Preparation and Positioning
Mammography Procedure:
- Preparation: Patients are advised to avoid using deodorants, talcum powders, or lotions on their breasts or underarms on the day of the exam, as these can create artifacts mimicking pathology [29].
- Positioning: The examination is performed with the patient standing. Each breast is positioned in turn on a special platform.
- Compression: A clear plastic paddle progressively compresses the breast. This is a critical step to:
- Even out breast thickness to visualize all tissue.
- Spread out tissue to reduce superimposition, preventing small lesions from being hidden.
- Immobilize the breast to prevent motion blur.
- Allow for a lower radiation dose by imaging a thinner tissue volume [29].
- Standard Views: A minimum of two views per breast are acquired: the cranio-caudal (CC), from top to bottom, and the mediolateral-oblique (MLO), from the center to the side at an angle [29]. The entire process typically takes about 30 minutes.
ABUS Procedure:
- Preparation: Unlike mammography, no restrictions on lotions or powders are needed. A hypoallergenic acoustic coupling gel is applied to the breast to ensure proper contact and transmission of sound waves [8].
- Positioning: The patient lies in a supine position. To evenly distribute breast tissue, a sponge wedge may be placed under the patient's arm, with the nipple pointing toward the ceiling [8]. This position is more comfortable and eliminates the need for compression.
- Scanning: The technologist selects the appropriate scan settings based on breast size (cup A-D+). A large, automated transducer then scans the breast in overlapping linear rows.
- Standard Views: Typically, three scans per breast are acquired in the anterior-posterior (AP), medial, and lateral views. For larger breasts (cup D and above), additional superior and inferior views may be necessary to ensure complete coverage [4] [11]. The patient must remain still and breathe quietly during the acquisition, which takes just a few minutes per view.
The workflow diagrams below illustrate the distinct steps involved in each procedure.
Diagram 1: Mammography Image Acquisition Workflow
Diagram 2: ABUS Image Acquisition Workflow
Comparative Diagnostic Performance in Clinical Research
Extensive clinical studies have quantified the performance of ABUS and mammography, both as standalone modalities and in combination. The data consistently highlights the complementary nature of these techniques, particularly in specific patient subgroups.
Sensitivity and Specificity Analysis
A large 2021 multicenter, cross-sectional study in China involving 1,922 women provided robust, head-to-head comparative data. The study evaluated the diagnostic performance of ABUS, handheld ultrasound (HHUS), and mammography in symptomatic women [11].
Table 2: Diagnostic Performance of ABUS, HHUS, and Mammography (Whole Study Population, n=1,922) [11]
| Modality | Sensitivity | Specificity |
|---|---|---|
| ABUS | 92.8% (375/404) | 93.0% (1411/1518) |
| HHUS | 96.3% (389/404) | 89.6% (1360/1518) |
| Mammography (MG)* | 87.9% (282/321) | 91.6% (846/924) |
Note: Mammography data was from Group B (women aged 40-69).
The study concluded that ABUS had a significantly higher specificity than HHUS (p<0.01), while HHUS had a higher sensitivity (p=0.01). When compared to mammography in women over 40, ABUS demonstrated significantly higher sensitivity (93.5% vs. 87.9%, p=0.02) with comparable specificity [11].
Impact of Breast Density
Breast density is a critical factor influencing diagnostic performance. Mammographic sensitivity decreases as breast density increases due to the masking effect of radiodense glandular tissue. A 2004 study found mammographic sensitivity could be as low as 45% in extremely dense breasts [30]. This is a key area where ABUS provides supplemental value.
A 2023 single-center retrospective study of 117 patients with core needle biopsy further underscored the complementary role of ABUS. The study found that while FFDM revealed 122 lesions, ABUS detected 246 focal lesions. The combined application of both methods increased sensitivity to 100% and improved overall diagnostic accuracy. Furthermore, ABUS showed higher compliance with histological tumor size measurements compared to FFDM [31].
Table 3: Performance in Dense Breasts and Combined Modality Use
| Scenario | Key Finding | Source |
|---|---|---|
| Mammography in Dense Breasts | Sensitivity can drop to ~45-55% in extremely dense breasts. | [30] |
| ABUS as Supplemental Screening | Increases cancer detection rate by 1.9–7.7 per 1000 women screened when combined with FFDM. | [4] |
| Combined FFDM + ABUS | Achieves 100% sensitivity, significantly improving over either modality alone. | [31] |
Research Reagent Solutions and Essential Materials
For researchers designing experimental protocols or validating imaging biomarkers, a detailed understanding of the required materials and their functions is essential. The following toolkit outlines the key components for both imaging modalities.
Table 4: Research Reagent Solutions and Essential Materials for Imaging Protocols
| Item | Function in Protocol | Application / Modality |
|---|---|---|
| Full-Field Digital Mammography Unit | Core imaging device; acquires 2D digital images using ionizing radiation. | Mammography (FFDM) |
| Digital Breast Tomosynthesis Unit | Advanced mammography device; acquires 3D tomographic images via moving X-ray tube. | Mammography (DBT) |
| Automated Breast Ultrasound System | Core imaging device; performs automated volumetric scanning with dedicated transducer. | ABUS |
| Acoustic Coupling Gel | Ensures optimal transmission of ultrasound waves by eliminating air between transducer and skin. | ABUS |
| BI-RADS Atlas | Standardized lexicon for reporting and classifying breast imaging findings; critical for study consistency. | Mammography, ABUS |
| Computer-Aided Detection (CAD) Software | Assists radiologists by highlighting potentially abnormal areas (density, mass, calcification). | Mammography, ABUS |
| Sponge Wedge | Placed under patient's arm in supine position to evenly distribute breast tissue during ABUS scan. | ABUS |
| Phantom Test Objects | Quality control tools with simulated lesions to ensure consistent image quality and machine performance. | Mammography, ABUS |
Advantages, Limitations, and Research Implications
A balanced evaluation of both modalities must consider their inherent advantages and limitations, which directly inform their appropriate application in research and clinical practice.
Mammography:
- Advantages: Remains the gold standard for population-based screening with proven mortality reduction benefits. It is highly effective for detecting microcalcifications, a hallmark of ductal carcinoma in situ (DCIS) [29]. Advanced techniques like DBT improve detection rates and reduce recall rates [29].
- Limitations: Involves ionizing radiation and breast compression, which can cause discomfort and deter participation. Its primary limitation is reduced sensitivity in dense breast tissue, which is a significant confounder in research studies involving pre-menopausal women [30].
ABUS:
- Advantages: Eliminates ionizing radiation and compression. It provides standardized, reproducible volumetric data, reducing operator-dependency. The coronal plane offers unique diagnostic information, and the modality demonstrates superior sensitivity in dense breasts [11] [4].
- Limitations: The acquisition can be challenged by very large breasts, requiring additional scan time and views. It cannot assess the axilla, vascularization, or lesion elasticity without Doppler or elastography functions available in HHUS. Image quality can be degraded by motion artifacts or poor positioning, and the interpretation time can be longer due to the large volumetric dataset [4].
The image acquisition processes for mammography and ABUS are fundamentally distinct, rooted in their different physical principles and leading to unique diagnostic profiles. Mammography, with its standardized compression and 2D/3D X-ray imaging, is an indispensable, proven screening tool, albeit with recognized limitations in dense breast tissue. ABUS offers a radiation-free, comfortable alternative that provides standardized, volumetric imaging of the breast with particular value for evaluating dense parenchyma.
Robust multicenter studies demonstrate that these modalities are not mutually exclusive but are powerfully complementary. ABUS has been shown to provide significantly higher sensitivity than mammography with comparable specificity, while also offering higher specificity than handheld ultrasound. For researchers and drug development professionals, this comparative analysis underscores the importance of modality selection based on specific research questions, patient populations (especially regarding breast density), and the critical need for standardized acquisition protocols to ensure reproducible and valid results in clinical trials and imaging studies. The integration of both technologies, alongside emerging artificial intelligence applications for ABUS analysis [20], represents the forward path in the personalized, early detection of breast cancer.
Breast cancer remains a significant global health challenge, being the most commonly diagnosed cancer with an estimated 2.3 million new cases worldwide [32]. In this context, early and accurate detection is paramount for improving treatment outcomes and patient survival. The diagnostic landscape relies on multiple imaging modalities, including digital mammography (MG), handheld ultrasound (HHUS), and the increasingly adopted automated breast ultrasound (ABUS). Each modality offers distinct advantages and limitations, particularly in different breast tissue densities and patient populations.
The Breast Imaging Reporting and Data System (BI-RADS), developed by the American College of Radiology, serves as a critical framework for standardizing mammogram reports and providing clear, meaningful communication across healthcare facilities [33]. This system classifies findings into categories ranging from 0 (incomplete) to 6 (known biopsy-proven malignancy), with categories 4 and 5 indicating suspicious findings requiring pathological correlation [33]. As breast imaging evolves with new technologies, BI-RADS provides the essential lexicon and categorization system that enables consistent interpretation and management recommendations across different imaging modalities, making direct comparison of their performance both possible and clinically meaningful.
Performance Comparison Across Imaging Modalities
Cancer Detection Capabilities
Table 1: Cancer Detection Performance in Dense Breasts
| Imaging Modality | Cancer Detection Rate per 1000 Examinations | Recall Rate | Average Size of Detected Invasive Cancers | Study/Reference |
|---|---|---|---|---|
| Abbreviated MRI | 17.4 (CI: 12.2-23.9) | 9.7% | 10 mm | BRAID RCT (2025) [34] |
| Contrast-Enhanced Mammography | 19.2 (CI: 13.7-26.1) | 9.7% | 11 mm | BRAID RCT (2025) [34] |
| Automated Breast Ultrasound | 4.2 (CI: 1.9-8.0) | 4.0% | 22 mm | BRAID RCT (2025) [34] |
| Full-Field Digital Mammography | 8.4 (CI: 7.2-9.9) | 5.4% | Not specified | BRAID RCT (2025) [34] |
The interim results from the large-scale BRAID randomized controlled trial (2025) provide compelling evidence regarding the comparative performance of supplemental imaging techniques in women with dense breasts and negative mammograms. As shown in Table 1, both abbreviated MRI and contrast-enhanced mammography demonstrated significantly higher cancer detection rates compared to ABUS, detecting approximately three times as many invasive cancers [34]. Crucially, the cancers detected by MRI and CEM were substantially smaller (10-11mm versus 22mm), suggesting potential for earlier detection when screening women with dense breasts [34].
BI-RADS Classification Concordance and Size Assessment
Table 2: BI-RADS Concordance and Pathological Size Correlation
| Comparison Metric | ABUS vs. HHUS | ABUS vs. MG | Reference |
|---|---|---|---|
| BI-RADS Category Agreement | 86.63% (kappa = 0.77) | 32.22% (kappa = 0.10) | PMC Study (2021) [32] |
| Correlation with Pathological Size (Spearman) | 0.74 | 0.58 | PMC Study (2021) [32] |
| Size Assessment Accuracy (±5mm threshold) | 48.84% | 43.87% | PMC Study (2021) [32] |
| BI-RADS Category Agreement in Primary Care | 98.2% (kappa = 0.726) | ~96% (kappa = 0.21-0.25) | Frontiers (2025) [35] |
A 2021 study examining 344 confirmed malignant lesions provided detailed insights into the agreement between different modalities on BI-RADS categorization and lesion size assessment. The findings demonstrated excellent agreement between ABUS and HHUS in BI-RADS categorization (86.63%, kappa=0.77), indicating that these ultrasound-based modalities interpret lesion characteristics similarly [32]. In contrast, agreement between ABUS and mammography was notably poor (32.22%, kappa=0.10), highlighting the fundamental differences in how these technologies visualize and characterize breast tissue [32].
Both ABUS and HHUS showed superior correlation with pathological tumor size compared to mammography, with correlation coefficients of 0.75 and 0.74 respectively, versus 0.58 for MG [32]. This accurate size assessment is clinically significant for surgical planning and prognosis estimation.
Diagnostic Accuracy in Specific Clinical Scenarios
Table 3: Diagnostic Performance in BI-RADS 0 Recalls and Small Cancers
| Clinical Scenario | Modality | Sensitivity | Specificity | Key Findings | Reference |
|---|---|---|---|---|---|
| BI-RADS 0 Recalls | 3D ABUS | 72.1% | 84.4% | Missed 27.9% of malignancies detected by DBT/HHUS | Insights into Imaging (2024) [36] |
| BI-RADS 0 Recalls | DBT + HHUS | 100% | 71.4% | All malignancies detected | Insights into Imaging (2024) [36] |
| Small Cancers (≤1cm) | ABUS vs. HHUS | Maintained suspicion | - | 37.3% downcategorized vs. HHUS | Diagnostics (2025) [37] |
For small breast cancers (≤1cm), a 2025 study found that while ABUS maintained suspicion for malignancy in categories 4A or higher, it assigned lower BI-RADS categories compared to HHUS in 37.3% of cases [37]. This downcategorization, despite maintaining suspicious features, suggests that ABUS may depict less aggressive features for some small malignant lesions, potentially affecting clinical management decisions [37].
Methodological Approaches in Comparative Studies
Experimental Protocols for Modality Comparison
The following dot code illustrates a standardized experimental design for multi-modality imaging comparison studies:
Imaging Acquisition Protocols: Recent comparative studies have implemented rigorous standardization in image acquisition. For ABUS examinations, the Invenia ABUS system (GE Healthcare) is commonly employed with a 6-15 MHz transducer acquiring images in anteroposterior, lateral, and medial views [32] [37]. Patients are positioned supine with a sponge under the shoulder to evenly distribute breast tissue [32]. HHUS examinations typically utilize high-frequency linear transducers (10-15 MHz) with systematic overlapping scanning in radial and anti-radial planes [32]. Mammography follows standard mediolateral oblique and craniocaudal views using digital mammography or tomosynthesis systems [32].
Image Interpretation Methodology: Studies employed blinded reading protocols where radiologists specialized in breast imaging interpreted each modality separately without knowledge of other imaging results [32] [37]. BI-RADS categorization follows the standardized lexicon including shape, orientation, margin, echo pattern, posterior features, and calcifications [33]. Multiplanar reconstruction and review of ABUS images in transverse, sagittal, and coronal planes is essential for comprehensive evaluation [37].
Validation and Statistical Analysis: Pathological results from surgical specimens or biopsies serve as the reference standard, with lesion size defined as the maximum diameter [32]. Statistical analyses typically include kappa statistics for inter-modality agreement, correlation coefficients (Spearman) for size comparisons, and receiver operating characteristic (ROC) analysis for diagnostic performance [32] [35].
Emerging Methodological Innovations
Artificial Intelligence Integration: Deep learning approaches are increasingly applied to mammography interpretation, with one 2025 study demonstrating that a DL model could reduce unnecessary biopsies for BI-RADS 4A lesions by 55.1% while maintaining diagnostic accuracy [38]. Similarly, AI-based radiomics analysis of ABUS images shows promise in extracting high-dimensional quantitative features for improved tumor characterization [20].
Radiomics Workflow: The radiomics pipeline for ABUS involves image acquisition, preprocessing and tumor segmentation, feature extraction, feature selection, and model construction using either traditional machine learning or deep learning approaches [20]. This quantitative analysis complements traditional BI-RADS categorization by providing additional data on tumor heterogeneity and characteristics.
Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Multi-Modality Imaging Studies
| Item | Function/Application | Example Specifications |
|---|---|---|
| ABUS System | Automated 3D whole-breast ultrasound acquisition | Invenia ABUS (GE Healthcare) with 6-15 MHz transducer [32] |
| HHUS System | Handheld ultrasound for comparison | High-frequency linear array transducer (10-15 MHz) [32] |
| Digital Mammography System | Standard 2D mammography or tomosynthesis | Hologic Selenia Dimensions, GE Senographe DS [32] |
| BI-RADS Reference Guide | Standardized classification and lexicon | ACR BI-RADS Atlas, 5th Edition [33] |
| Pathology Consortium | Histopathological validation | Surgical specimen analysis, biomarker assessment (ER, PR, HER2) [32] |
| Dedicated Workstation | Multiplanar image review and analysis | ABUS review workstation with coronal reconstruction [37] |
| Statistical Analysis Software | Data analysis and agreement statistics | SPSS, R Studio with appropriate packages [32] |
The evidence from recent studies demonstrates that BI-RADS provides an essential standardized framework that enables meaningful comparison across breast imaging modalities. Each modality offers distinct advantages: mammography remains fundamental for microcalcification detection; ABUS provides standardized, reproducible whole-breast coverage with excellent correlation to HHUS; and advanced techniques like MRI and contrast-enhanced mammography show superior sensitivity in dense breasts.
The integration of artificial intelligence and radiomics holds promise for enhancing BI-RADS categorization, particularly for indeterminate lesions where biopsy reduction is desirable. Future directions should focus on optimizing modality selection based on individual patient factors, further refining BI-RADS categorization through quantitative imaging biomarkers, and developing integrated diagnostic pathways that leverage the complementary strengths of each imaging technology within a standardized BI-RADS framework.
For researchers and clinicians focused on breast cancer, dense breast tissue presents a significant diagnostic challenge. Full-field digital mammography (FFDM), the traditional cornerstone of breast screening, experiences a marked reduction in sensitivity in dense breasts, falling from over 85% in fatty breasts to as low as 61% in extremely dense tissue [39] [40]. This masking effect occurs because both fibroglandular tissue and malignancies appear radiographically white on a mammogram. Furthermore, dense breast tissue is an independent risk factor for breast cancer, with women possessing extremely dense breasts having a four to six times higher risk compared to those with fatty breasts [39] [40]. This dual problem of reduced detection sensitivity and increased intrinsic risk has driven the investigation of supplemental imaging modalities. Among these, Automated Breast Ultrasound (ABUS) has emerged as a promising technology, offering a standardized, operator-independent ultrasound approach. This guide provides a comparative analysis of ABUS's diagnostic performance against FFDM and other advanced modalities like contrast-enhanced mammography (CEM), with a specific focus on its application in high-risk and dense-breast populations.
Comparative Diagnostic Performance Data
The efficacy of any imaging modality is quantified by its sensitivity, specificity, and cancer detection rate. The data below, synthesized from recent studies, allows for a direct comparison of ABUS against established and emerging technologies.
Table 1: Comparative Diagnostic Performance in Dense Breasts (BI-RADS C & D)
| Imaging Modality | Sensitivity (%) | Specificity (%) | Cancer Detection Rate (per 1000 screens) | Overall Accuracy (%) |
|---|---|---|---|---|
| FFDM (Mammography) | 61.8 - 85.4 [39] [40] | 91.9 [39] | Baseline | 66.1 - 83.3 [39] [40] |
| Handheld Ultrasound (HHUS) | 85.3 [39] | 88.4 [39] | +4.9 (as adjunct to FFDM) [41] | 87.1 [39] |
| ABUS | 78.1 - 93.8 [40] [42] | 40.0 - 88.2 [40] [42] | +1.9 - 2.4 (as adjunct to FFDM) [37] | 67.9 - 90.0 [40] [42] |
| Contrast-Enhanced Mammography (CEM) | 92.7 - 93.5 [43] [40] | 8.3 - 11.1 [43] [40] | 19.2 [44] | 73.6 - 80.0 [43] [40] |
| Abbreviated Breast MRI (AB-MRI) | Not Reported | Not Reported | 17.4 [44] | Not Reported |
| FFDM + ABUS Combination | 100 [43] [40] | Not Reported | Not Reported | 75.0 - 84.6 [43] [40] |
Table 2: Head-to-Head Comparison of Supplemental Imaging from the BRAID Trial
| Modality | Invasive Cancer Detection Rate (per 1000) | Typical Invasive Cancer Size Detected | Key Advantages & Limitations |
|---|---|---|---|
| ABUS | 4.2 [44] | Larger (approx. twice the size of CEM/MRI-detected cancers) [44] | + No radiation or contrast- Lower detection rate for small invasive cancers |
| CEM | 15.7 [44] | Smaller (half the size of ABUS-detected cancers) [44] | + High detection rate- Iodinated contrast reactions (17 minor, 6 moderate, 1 severe per 1000) [44] |
| AB-MRI | 15.0 [44] | Smaller (half the size of ABUS-detected cancers) [44] | + High detection rate- Requires gadolinium contrast, higher cost |
Key Research Findings and Experimental Evidence
ABUS vs. Traditional Mammography and HHUS
A prospective, comparative observational study highlights ultrasound's superior sensitivity over mammography in dense breasts (85.3% vs. 61.8%), concluding that ultrasound significantly improves detection in this population [39]. The area under the ROC curve (AUC) was 0.89 for ultrasound compared to 0.78 for mammography [39]. ABUS, specifically, addresses key limitations of its predecessor, HHUS, by standardizing the image acquisition process. It separates acquisition from interpretation, improving reproducibility and reducing operator-dependence [41]. Studies show ABUS has comparable diagnostic performance to HHUS, with one retrospective analysis of small (≤1 cm) cancers finding that while ABUS sometimes assigned lower BI-RADS categories, it still maintained malignancy suspicion for all lesions [37].
ABUS in Multi-Modality Comparative Trials
Large, randomized controlled trials provide the highest level of evidence. The interim results from the BRAID trial in the UK revealed that while ABUS detected additional cancers beyond FFDM, its cancer detection rate was significantly lower than that of CEM and abbreviated MRI (AB-MRI) [44]. Crucially, the invasive cancers detected by AB-MRI and CEM were half the size of those found with ABUS, suggesting these modalities may enable earlier diagnosis [44]. Another single-center study comparing ABUS and CEM as adjuncts to FFDM found that the combination of FFDM+ABUS achieved a sensitivity of 100%, outperforming FFDM+CEM (93.5%) in their cohort, though CEM alone had higher sensitivity and accuracy than ABUS alone [43] [40].
Detailed Experimental Protocols for ABUS Research
For researchers designing studies, understanding the technical protocols from key cited experiments is essential. The following workflow summarizes a typical comparative study design.
Figure 1: Workflow of a comparative imaging study.
Patient Cohort and Imaging Protocol
- Patient Selection: Studies typically enroll women aged 40-70 with heterogeneously dense (BI-RADS C) or extremely dense (BI-RADS D) breasts, confirmed on a prior mammogram. Key exclusion criteria often include a prior history of breast cancer, breast surgery, or current pregnancy/lactation [39] [42].
- ABUS Image Acquisition: Using an FDA-cleared system like the Invenia ABUS (GE Healthcare), images are acquired by trained radiographers or technologists, not the interpreting radiologist. The patient is positioned supine, and each breast is scanned in three standard views: anteroposterior, lateral, and medial. For larger breasts, additional views may be needed. The system uses a wide high-frequency transducer (e.g., 6-15 MHz) to capture volumetric data, which is then transmitted to a dedicated workstation for review [37] [42].
- Comparative Modalities: In a typical comparative study, all patients undergo FFDM and ABUS. FFDM includes standard craniocaudal (CC) and mediolateral oblique (MLO) views. The comparator modality (e.g., HHUS, CEM, or DBT) is performed either on the same day or within a short interval (e.g., one week) to ensure diagnostic consistency [39] [43].
Image Interpretation and Statistical Analysis
- Blinded Interpretation: The ABUS, FFDM, and other modality images are interpreted independently by experienced breast radiologists who are blinded to the other imaging results and final pathology to prevent bias. For ABUS, reviewers analyze multiplanar reconstructions (axial, sagittal, and coronal) on the dedicated workstation [37].
- Reference Standard: Lesions classified as BI-RADS 4 (suspicious) or 5 (highly suggestive of malignancy) undergo histopathological verification via core needle biopsy or surgical excision. Benign-appearing lesions (BI-RADS 2 or 3) are confirmed through typical benign imaging features or imaging follow-up at 6-month to 2-year intervals [39] [42].
- Statistical Evaluation: Diagnostic performance is assessed by calculating sensitivity, specificity, positive and negative predictive values (PPV, NPV), and overall accuracy against the histological gold standard. Differences in performance are tested using the McNemar's test or Chi-square test. Receiver operating characteristic (ROC) curves are plotted, and the area under the curve (AUC) is calculated to compare the overall diagnostic capability of each modality [39] [43].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials and Equipment for ABUS Research
| Item | Function in Research | Example Specification / Model |
|---|---|---|
| ABUS Imaging System | Acquires standardized, whole-breast volumetric ultrasound data. Essential for the intervention arm of studies. | Invenia ABUS system with Reverse Curve transducer (GE Healthcare) [37]. |
| Full-Field Digital Mammography System | Serves as the standard of care control. Provides baseline images and breast density assessment. | GE Mammography system with tomosynthesis capability for DBT comparison [42]. |
| Contrast Agent | Enables comparative studies with Contrast-Enhanced Mammography (CEM). | Iodinated contrast medium (e.g., administered at 1.5 ml/kg) [43]. |
| Dedicated Workstation | Allows for multi-planar reconstruction and analysis of ABUS volume data. Critical for accurate interpretation. | Invenia ABUS review workstation (GE Healthcare) [37]. |
| Biopsy System | Provides histopathological verification of imaging findings, which is the reference standard. | Ultrasound-guided core needle biopsy (CNB) or vacuum-assisted biopsy (VAAB) systems [43]. |
| BI-RADS Atlas | Standardizes the lexicon for describing and categorizing breast imaging findings across all modalities. | ACR BI-RADS 5th Edition or newer [37]. |
The body of evidence confirms that ABUS is a valuable supplemental tool to FFDM for breast cancer detection in women with dense breasts, significantly improving sensitivity over mammography alone and offering a standardized, non-ionizing alternative to HHUS. However, interim results from high-quality randomized trials like BRAID indicate that for the purest metric of screening performance—the detection of small, invasive cancers—AB-MRI and CEM currently demonstrate superior efficacy [44] [45].
Future research directions are increasingly focused on personalization and efficiency. The integration of Artificial Intelligence (AI) for ABUS image analysis holds promise for reducing false-positive rates and improving interpretation efficiency [41]. Furthermore, initiatives like the ScreenTrustMRI trial in Sweden are exploring the use of AI to identify a sub-population of women with dense breasts who are at the very highest risk of interval cancers, thereby maximizing the cost-effectiveness of supplemental MRI [45]. This trend towards risk-stratified, personalized screening protocols, rather than a one-size-fits-all approach, will likely define the next era of breast cancer imaging research and clinical practice.
While mammography remains the cornerstone of breast cancer screening, its sensitivity significantly decreases in women with dense breast tissue, presenting a challenge for accurate preoperative staging. Automated Breast Ultrasound (ABUS) has emerged as a standardized, reproducible imaging modality that extends beyond supplemental screening to play a crucial role in preoperative tumor assessment and surgical planning. This comprehensive analysis compares the performance of ABUS against traditional mammography and hand-held ultrasound (HHUS) in the preoperative setting, demonstrating that ABUS provides superior lesion visualization, more accurate tumor size measurement, and improved detection of additional malignant foci in dense breasts. By synthesizing evidence from clinical studies, we elucidate how the unique capabilities of ABUS, particularly its coronal plane reconstruction and standardized acquisition, directly influence surgical decision-making and potentially reduce positive margin rates through enhanced preoperative visualization of tumor extent.
Preoperative evaluation of breast cancer is paramount for determining appropriate surgical strategy, particularly when considering breast-conserving surgery versus mastectomy. The accuracy of tumor size measurement and delineation of disease extent directly impacts surgical margin status, local recurrence rates, and overall survival outcomes. Traditional full-field digital mammography (FFDM) faces significant limitations in women with dense breast tissue, where its sensitivity can drop to as low as 48% [8]. This reduced sensitivity stems from the masking effect of dense parenchyma, where both tumor and glandular tissue appear radiographically white, creating a camouflage effect that obscures malignancies [46].
The clinical imperative for improved preoperative imaging is clear: incomplete tumor excision with positive margins necessitates re-operation in 20-40% of breast-conserving surgeries, subjecting patients to additional surgical trauma, psychological distress, and delayed adjuvant therapies. Magnetic resonance imaging (MRI), while highly sensitive, presents challenges of cost, accessibility, contrast agent requirements, and time-intensive interpretation [8] [4]. Hand-held ultrasound (HHUS) offers an alternative but suffers from operator dependency, limited reproducibility, and inter-observer variability [8] [4]. Within this diagnostic landscape, ABUS has emerged as a standardized, reproducible technique that addresses many limitations of conventional modalities while providing unique diagnostic information critical to surgical planning.
Technical Foundations of ABUS: Standardized Acquisition and Reconstruction
System Components and Image Acquisition
ABUS systems utilize an automated linear transducer (typically 6-14 MHz) that moves over the breast in a standardized pattern, capturing volumetric data through multiple overlapping scans [8] [4]. During examination, patients are positioned supine with a sponge wedge placed under the arm to evenly distribute breast tissue with the nipple pointing toward the ceiling. Hypoallergenic fluid ensures proper contact between the probe and breast surface, while patients must remain still with quiet breathing during the scanning process [8]. A typical bilateral examination consists of three standardized views per breast (anterior-posterior, medial, and lateral), with additional views (superior and inferior) required for larger (cup size D) breasts to ensure complete tissue coverage [4].
The fundamental innovation of ABUS lies in its separation of image acquisition from interpretation. Technologists perform the scanning procedure using standardized protocols, while radiologists interpret the reconstructed volumes independently. This workflow not only reduces operator dependency but also enables objective comparison across serial examinations and facilitates second opinions without repeating the scan [4] [46]. The system automatically reconstructs the acquired data into thin-slice volumetric images that can be reviewed in axial, sagittal, and coronal planes, with the latter providing unique diagnostic information not routinely available with HHUS.
The Diagnostic Power of the Coronal Plane
The coronal reconstruction, often termed the "surgical plane" because it presents the breast as viewed from the surgical perspective, represents a significant advantage of ABUS technology [4]. In this plane, benign lesions typically display a continuous hyperechoic rim, while malignant lesions often present with a discontinuous hyperechoic rim and a distinctive "retraction phenomenon" [4]. This retraction phenomenon appears as hyperechoic straight lines radiating from the tumor surface, representing tumor infiltration and desmoplastic reaction of surrounding tissue against the malignancy [4]. This "black hole" appearance with surrounding architectural distortion provides crucial visual cues for malignancy detection and characterization.
Research by van Zelst et al. demonstrated a positive correlation between a proposed "spiculation and retraction phenomenon index" evaluated in the coronal plane and the likelihood of cancer [4]. Furthermore, the retraction phenomenon has been statistically correlated with smaller tumor size, lower histological grade, and positive estrogen and progesterone receptor status, suggesting its potential prognostic value [4]. The coronal plane also facilitates reconstruction of the ductal system throughout the breast, aiding identification of ductal dilatation associated with intraductal papillary lesions or ductal carcinoma in situ (DCIS) through detection of intraluminal echoes in dilated lactiferous ducts [4].
Comparative Performance Analysis: ABUS Versus Conventional Modalities
Detection Capabilities in Dense Breast Tissue
Table 1: Cancer Detection Rates of ABUS in Combination with FFDM Compared to FFDM Alone
| Study | Year | Patients (n) | Sensitivity FFDM (%) | Sensitivity FFDM+ABUS (%) | Specificity FFDM (%) | Specificity FFDM+ABUS (%) | Additional Cancers Detected/1000 |
|---|---|---|---|---|---|---|---|
| Brem et al. (SomoInsight) [4] | 2014 | 15,318 | 73.2 | 100 | 85.4 | 72 | 1.9 |
| Kelly et al. [4] | 2010 | 4,419 | 40 | 81 | 95.15 | 98.7 | 3.9 |
| Giuliano et al. [4] | 2012 | 3,418 | 76 | 96.7 | 99.70 | 98.2 | 7.7 |
| Wilczek et al. [4] | 2016 | 1,668 | 63.6 | 100 | 99 | 98.4 | 2.4 |
The SomoInsight study, the most extensive investigation of ABUS in screening, demonstrated that combining ABUS with FFDM increased cancer detection by 1.9 per 1000 women screened, representing a 26.7% improvement in sensitivity compared to mammography alone [4]. Similar studies have reported even greater incremental cancer detection rates ranging from 2.4 to 7.7 additional cancers per 1000 women screened [4]. This enhanced detection capability is particularly valuable in the preoperative setting, where identifying additional malignant foci may alter surgical management from breast conservation to mastectomy.
Comparison with Hand-Held Ultrasound
Table 2: Performance Comparison of ABUS Versus HHUS in Preoperative Assessment
| Parameter | ABUS | HHUS | Clinical Significance |
|---|---|---|---|
| Interobserver agreement [47] | Near-perfect (κ=0.994) | Variable | Standardized interpretation improves consistency |
| Architectural distortion detection [47] | Superior | Standard | Better visualization of spiculations and retraction phenomena |
| Examination time | Acquisition: 5-7 min per breast [46] | 10-20 min per breast | Technologist-performed acquisition frees radiologist time |
| Operator dependency | Low | High | Standardized acquisition protocol |
| Whole-breast documentation | Complete volumetric dataset | Selected representative images | Enables retrospective review and second opinions |
| Coronal plane visualization | Available | Limited | Unique "surgical plane" overview of tumor architecture |
A 2018 prospective study of 1,886 women with dense breasts demonstrated exceptional agreement between ABUS and HHUS (99.8%; κ=0.994), confirming comparable performance in lesion detection and characterization [47]. Notably, the study identified several cases where ABUS detected carcinomas that were graded as BI-RADS 2 (benign) on mammography, including three cases correctly classified as BI-RADS 4 (suspicious) on ABUS and two as BI-RADS 5 (highly suggestive of malignancy) [47]. The research also suggested ABUS superiority in detecting architectural distortions, a critical feature for preoperative planning often challenging to visualize with conventional ultrasound [47].
Tumor Sizing Accuracy and Multifocal Disease Detection
Accurate preoperative tumor measurement critically influences surgical planning. A key study investigating MRI with computer-aided detection (CAD) found that a 30% enhancement threshold provided optimal correlation with pathological tumor size (concordance rate of 72.5% for invasive cancers), outperforming higher thresholds (50% and 100%) that risked significant underestimation [48]. While this study focused on MRI, the principle of threshold optimization applies similarly to ABUS image interpretation, where appropriate windowing and level settings are essential for accurate tumor delineation.
Regarding multifocal disease identification, Girometti et al. compared the combination of ABUS with digital breast tomosynthesis (DBT) against MRI for preoperative staging [4]. While MRI demonstrated higher sensitivity (91.7% vs. 76.5%) for supplemental disease detection, the combination of ABUS and DBT provided valuable preoperative information with greater accessibility and lower cost [4]. This suggests ABUS may serve as a viable alternative to MRI for preoperative staging when MRI is contraindicated, unavailable, or poorly tolerated.
ABUS in Preoperative Workflow: Experimental Protocols and Clinical Implementation
Standardized Preoperative ABUS Protocol
For preoperative staging, the following protocol is recommended based on analyzed studies:
Patient Selection: Women with BI-RADS density categories C (heterogeneously dense) or D (extremely dense) breasts with known biopsy-proven malignancy being considered for breast-conserving surgery [47].
Image Acquisition: Bilateral ABUS examination performed using standardized positioning with anterior-posterior, medial, and lateral views for each breast. Additional superior and inferior views for cup size D or larger breasts [4].
Image Interpretation: Multiplanar review of volumetric data with particular attention to:
- Coronal plane for retraction phenomenon and architectural distortion [4]
- Tumor size measurement in three dimensions with electronic calipers
- Identification of additional suspicious lesions within the ipsilateral and contralateral breasts
- Relationship to anatomical landmarks (nipple, chest wall, skin)
Image-Guided Biopsy: Suspicious additional lesions identified on ABUS require HHUS correlation for biopsy guidance, as current ABUS systems do not permit direct biopsy capability [8] [4].
Surgical Planning Documentation: Comprehensive report including:
- Lesion size in three dimensions
- Distance from nipple, skin, and chest wall
- Presence of multifocal or multicentric disease
- Relationship to anatomical compartments
Workflow Integration and Economic Considerations
Implementation of ABUS into preoperative workflows offers significant operational advantages. A case study from Acıbadem Altunizade Hospital demonstrated that integrating ABUS reduced radiologist time by enabling technologists to perform scans, resulting in an 18% reduction in operational costs (approximately $300 USD monthly based on 665 patients) [46]. The separation of image acquisition from interpretation allows radiologists to review cases during less busy periods, improving workflow efficiency [46]. Furthermore, the standardized volumetric dataset enables review at specialized workstations without patient presence, potentially reducing time pressures and interpretation errors.
Limitations and Technical Challenges in Preoperative Application
Despite its advantages, ABUS presents several limitations in the preoperative setting that warrant consideration:
Inability to Assess Axilla: ABUS cannot adequately visualize axillary lymph nodes, requiring supplemental HHUS for complete nodal staging [4] [49].
Limited Functional Assessment: Current ABUS systems lack Doppler capability for vascular assessment and elastography for tissue stiffness evaluation, both sometimes useful in lesion characterization [4].
Biopsy Guidance Limitation: While ABUS can detect additional lesions, it does not permit direct biopsy guidance, necessitating second-look HHUS for tissue sampling [8] [4].
Artifact Vulnerability: Image quality can be compromised by poor positioning, lack of contact, patient motion, or lesion-related artifacts [4] [49]. Specific artifacts include shadowing from the nipple, reverberation in the superficial tissues, and motion artifacts from breathing or patient movement.
Learning Curve: Radiologists require specific training to master ABUS interpretation, particularly recognizing normal anatomical structures and artifacts in the coronal plane [4].
Dense Breast Limitation: While superior to mammography in dense tissue, ABUS performance remains somewhat limited in extremely dense breasts (ACR category D) due to posterior shadowing and decreased beam penetration [8].
The Research Toolkit: Essential Reagent Solutions for ABUS Investigation
Table 3: Essential Research Materials and Methodologies for ABUS Studies
| Research Component | Function | Example Implementation |
|---|---|---|
| ABUS System with Coronal Reconstruction | Volumetric image acquisition and multi-planar display | GE HealthCare Invenia ABUS 2.0; Siemens ACUSON S2000 ABVS |
| BI-RADS Standardization Lexicon | Standardized terminology for lesion description and classification | ACR BI-RADS Atlas (5th edition) for ultrasound |
| Phantom Test Objects | System performance verification and quality control | CIRS Model 054; Gammex 169 Multi-Purpose Breast Phantom |
| Dedicated Workstation with 3D Capability | Image interpretation with multiplanar reconstruction and analysis | CADstream; Mediphan ABUS ViewStation |
| Statistical Analysis Tools | Diagnostic performance calculation and comparison | ROC analysis; Cohen's kappa for inter-reader agreement |
| Pathological Correlation Standard | Reference standard for diagnostic test accuracy | Histopathological analysis of surgical specimens |
| HHUS with Biopsy Capability | Second-look examination and tissue sampling | High-frequency linear array transducers with biopsy guidance |
Future Directions and Research Opportunities
The evolving landscape of ABUS technology presents several promising research avenues for enhancing its preoperative role. Artificial intelligence (AI) integration represents the most significant advancement, with deep learning algorithms showing potential for automated lesion detection, characterization, and even response assessment following neoadjuvant chemotherapy [50]. Wang et al. demonstrated that coronal plane features could predict complete pathological response after two cycles of neoadjuvant chemotherapy with 85.7-88.1% sensitivity and 81.5-85.1% specificity [4].
Quantitative biomarker development from ABUS data represents another promising direction. Chang et al. demonstrated excellent reliability in ABUS measurements for lesion location (ICC=0.926) and size (ICC=0.980), though depth measurement reliability was lower (ICC=0.342) due to scanning pressure variations [4]. Future systems with pressure standardization may improve depth measurement consistency.
Additional research priorities include:
- Standardized protocols for monitoring tumor response to neoadjuvant chemotherapy
- Development of automated 3D tumor volumetry for precise surgical planning
- Integration with mammographic data for fused multimodal visualization
- Optimization of workflows for radiologist efficiency and diagnostic accuracy
- Long-term outcome studies correlating ABUS findings with surgical margin status and local recurrence rates
ABUS represents a significant advancement in preoperative breast imaging, particularly for women with dense breast tissue where mammographic sensitivity is limited. The technology provides standardized, reproducible volumetric imaging with unique coronal plane visualization that enhances detection of architectural distortions and improves tumor extent assessment. While MRI remains more sensitive for additional disease detection, ABUS offers a valuable alternative with greater accessibility, lower cost, and workflow advantages. The integration of ABUS into preoperative planning provides surgeons with enhanced roadmaps for conservative breast surgery, potentially reducing positive margin rates and re-operation frequency. As ABUS technology evolves with AI integration and quantitative analytics, its role in personalized surgical planning will likely expand, further strengthening its position as an essential tool beyond screening in comprehensive breast cancer management.
Navigating Clinical Hurdles: Artifacts, Workflow Integration, and Diagnostic Pitfalls
Identifying and Mitigating Common ABUS Artifacts from Acquisition to Interpretation
Automated Breast Ultrasound (ABUS) has emerged as a valuable complementary modality in breast imaging, particularly for women with dense breast tissue where mammography sensitivity is reduced [3] [51]. While it addresses issues of operator-dependence and standardization inherent in handheld ultrasound (HHUS) [51], the ABUS acquisition and interpretation pathway introduces unique artifacts. This guide objectively compares ABUS performance with alternative modalities and details protocols for identifying and mitigating its characteristic artifacts, providing researchers with a framework for rigorous evaluation.
The ABUS Artifact Profile: Types and Impact
Artifacts in ABUS can originate from acquisition, patient physiology, or reconstruction software. Misidentification can lead to false positives, increased recall rates, or missed cancers.
Table 1: Common ABUS Artifacts and Mitigation Strategies
| Artifact Type | Cause/Origin | Impact on Interpretation | Mitigation Strategies |
|---|---|---|---|
| Nipple Shadow | Inadequate contact or shadowing from the nipple complex. | Obscures underlying tissue, potentially hiding lesions. | Proper nipple lotion application [51]; use of nipple marker for spatial reference [51]. |
| Skin/Contact Artifacts | Air gaps between transducer and skin, or hair/debris. | Appears as bright echoes near the skin surface, mimicking lesions. | Ensure even application of hypoallergenic lotion and clean skin surface [51]. |
| Rib Artifacts | Acoustic shadowing from ribs. | Can mimic or obscure posterior lesions. | Recognize characteristic periodic patterns; correlate with patient anatomy. |
| Posterior Enhancement | Reduced sound wave attenuation behind cystic structures. | Suggests benign, fluid-filled nature; can be used for characterization. | Confirm through multiplanar reformations; a key feature for cyst identification. |
| Coronal Plane "Retraction" | Software reconstruction of architectural distortion from desmoplastic reaction. | Highly specific sign of malignancy [52]. | Critical diagnostic feature, not a technical artifact; requires expert recognition. |
| Motion Artifacts | Patient movement during automated scan. | Blurring or duplication of structures, reducing image clarity. | Instruct patient to remain still and breathe smoothly during acquisition [51]. |
ABUS Artifact Decision Pathway: A workflow for categorizing and addressing common ABUS findings.
ABUS in the Comparative Imaging Landscape
Understanding ABUS performance relative to other modalities is crucial for appropriate application in research and clinical practice.
Table 2: Modality Performance Comparison in Key Studies
| Imaging Modality | Sensitivity (%) | Specificity (%) | Cancer Detection Rate (per 1,000) | Key Study Findings |
|---|---|---|---|---|
| FFDM alone | 50 [1] | 11.11 - 95.15 [1] [51] | 4.6 [51] | Standard for screening; sensitivity drops significantly in dense breasts. |
| ABUS alone | 80.43 [1] | 27.78 - 89.9 [1] [51] | N/A | Superior sensitivity to FFDM; lower specificity leading to recalls. |
| HHUS alone | 100 [3] | 85.0 - 95.0 [3] | N/A | Operator-dependent; excellent sensitivity but non-reproducible. |
| FFDM + ABUS | 100 [1] | N/A | 12.3 [51] | Combined approach yields highest sensitivity and cancer detection. |
| Contrast-Enhanced Mammography (CEM) | 93.48 [1] | 11.11 [1] | 19.2 [5] | High cancer detection; involves contrast agent and ionizing radiation. |
| Abbreviated MRI (AB-MRI) | N/A | N/A | 17.4 [5] | Very high detection rate; high cost and limited availability. |
The data reveals ABUS as a high-sensitivity tool for detection, particularly valuable as an adjunct to FFDM. However, its relatively low specificity is a key limitation, often driven by the misinterpretation of artifacts and benign features, which can increase unnecessary recalls and biopsies [1]. While HHUS can achieve similar sensitivity, its operator dependence makes it less suitable for standardized screening programs [3]. Advanced modalities like CEM and AB-MRI demonstrate superior overall performance in dense breasts [5], but with trade-offs in cost, complexity, and (for CEM) the use of ionizing radiation.
Experimental Protocols for Artifact Analysis
For researchers validating ABUS systems or developing new algorithms, a standardized protocol for artifact assessment is essential.
Protocol 1: Evaluating ABUS as an Adjunct to Mammography
This protocol is based on a comparative analysis of diagnostic performance [1].
- Objective: To compare the diagnostic performance of ABUS and CEM as complementary methods to full-field digital mammography (FFDM).
- Patient Cohort: 81 patients with 169 focal breast lesions were included. 110 lesions were histopathologically verified (92 malignant, 5 B3 lesions, 13 benign) [1].
- Methodology:
- All patients underwent FFDM, ABUS, and CEM examinations.
- Lesion detection rates, size correlation with histopathology, and diagnostic performance metrics (sensitivity, specificity, PPV, NPV, accuracy) were calculated for each modality.
- The combination of FFDM+ABUS was directly compared to FFDM+CEM.
- Key Metrics:
- Lesion Detection: The number of additional lesions detected by each modality beyond FFDM was recorded. ABUS detected 36 new lesions, while CEM detected 19 [1].
- Size Concordance: Compliance in determining lesion size compared to histopathology was highest for ABUS (p=0.258), indicating excellent correlation [1].
- Diagnostic Performance: The sensitivity and accuracy of FFDM+ABUS were 100% and 84.55%, respectively, which was superior to the FFDM+CEM combination (93.48% and 79.09%) in this study [1].
Protocol 2: Re-evaluation of High-Risk Non-Mass Lesions (NMLs)
This protocol focuses on a challenging diagnostic scenario [52].
- Objective: To reevaluate high-risk non-mass-like lesions (NMLs) found on mammography using target US and ABUS to improve diagnosis and reduce unnecessary biopsies.
- Patient Cohort: 161 patients with 166 NMLs diagnosed as BI-RADS 4 or 5 by MG [52].
- Methodology:
- All NMLs underwent MG, targeted HHUS, and ABUS before biopsy or surgery.
- Sonographic features such as blood supply, hyperechogenicity, ductal changes, peripheral changes, and coronal plane features were analyzed.
- Pathological results served as the gold standard.
- Key Findings:
- Coronal Plane Superiority: The coronal features of ABUS were more sensitive than targeted HHUS in showing structural abnormalities, a critical factor for malignancy [52].
- Calcification Limitation: Target US was less effective than MG in detecting micro-calcifications [52].
- Performance Improvement: ABUS significantly improved the sensitivity, specificity, and accuracy for diagnosing high-risk NMLs compared to MG alone [52].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Analytical Tools
| Item | Function/Application in ABUS Research |
|---|---|
| GE Invenia ABUS | A commercially available supine ABUS system used in clinical studies for 3D whole-breast acquisition [52]. |
| Dedicated Workstation with Multiplanar Reformation | Essential for post-processing, allowing review in axial, sagittal, and coronal planes to differentiate artifacts from true lesions [51]. |
| Nipple Marker | A critical fiducial marker placed during scanning to provide accurate spatial localization and orient the reader [51]. |
| Hypoallergenic Lotion | Ensures consistent acoustic coupling between the transducer and skin, minimizing contact artifacts [51]. |
| Computed Aided Detection (CAD) Software | Software used alongside ABUS to improve radiologists' detection rates of breast masses, with studies showing a 5.2–10.6% sensitivity increase [3]. |
ABUS Research Workflow: Key stages from data acquisition to analysis.
ABUS represents a significant technological advancement for standardized breast ultrasound, offering high sensitivity, especially in dense breasts. Its primary research and clinical challenge lies not in detection power, but in managing artifacts and low-specificity findings. Mastery of its artifact profile, coupled with an understanding of its performance relative to alternatives like CEM and AB-MRI, is essential for its effective use. Future research integrating artificial intelligence with multiplanar ABUS data holds strong potential to further improve specificity and automate artifact detection, solidifying its role in comprehensive breast cancer screening and diagnosis.
Strategies for Improving Specificity and Reducing False-Positive Recall Rates
False-positive recalls represent a significant challenge in breast cancer screening, causing unnecessary patient anxiety, additional invasive procedures, and increased healthcare costs. Conventional mammography screening, while successful in reducing mortality, entails substantial collateral harms including high false-positive recall rates. Contemporary cohort data shows that approximately 50-60% of women undergoing ten years of annual mammography will experience at least one false-positive recall, with about 11% undergoing unnecessary needle biopsies over this period [53]. This review systematically compares the performance of traditional mammography with automated breast ultrasound, focusing on strategies to improve specificity while maintaining high cancer detection rates. We examine technological advancements including artificial intelligence integration and multimodal approaches that show promise in optimizing the benefit-to-harm ratio of breast screening programs.
Comparative Performance Metrics Across Imaging Modalities
Diagnostic Performance of Mammography, ABUS, and CEM
Table 1: Comparison of diagnostic performance across imaging modalities in dense breasts (BI-RADS categories C & D)
| Modality | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | Study/Reference |
|---|---|---|---|---|---|---|
| FFDM (Mammography) | 29-61.8 | 91.9 | 75.0 | 85.8 | 66.1-83.3 | [54] [39] |
| ABUS (Automated Breast Ultrasound) | 72-86.1 | 88.4 | 74.4-78.1 | 93.8 | 67.9-87.1 | [54] [4] [39] |
| Contrast-Enhanced Mammography (CEM) | 56-92.7 | 8.3-91 | 77.6 | 25 | 73.6 | [54] |
| FFDM + ABUS Combined | 100 | 75-81.4* | - | - | 75-81.4 | [54] [39] |
| ABUS + DBT Combined | 76.5 | - | 78.0 | - | - | [4] |
*Specificity and accuracy values for combined approaches represent range across studies. PPV = Positive Predictive Value; NPV = Negative Predictive Value.
Meta-Analysis Data on Diagnostic Accuracy
Table 2: Pooled diagnostic accuracy data from meta-analysis of 31 studies including 8,107 lesions [55]
| Modality | Sensitivity (Pooled) | Specificity (Pooled) | Diagnostic Odds Ratio | Area Under Curve (AUC) |
|---|---|---|---|---|
| HHUS (Hand-Held Ultrasound) | 0.86 (0.84, 0.87) | 0.80 (0.78, 0.81) | 22.88 (16.84, 31.08) | 0.898 |
| ABUS (Automated Breast Ultrasound) | 0.90 (0.89, 0.91) | 0.87 (0.86, 0.88) | 74.63 (45.37, 122.76) | 0.956 |
| Molybdenum-Target Mammography | 0.81 (0.78, 0.84) | 0.90 (0.88, 0.91) | 31.41 (17.01, 57.98) | 0.887 |
Artificial Intelligence as a Specificity-Enhancing Tool
AI Implementation in Clinical Workflows
Artificial intelligence systems are being deployed in mammography screening with two primary approaches to improve specificity: normal triaging and safety net functions. The normal triaging function identifies examinations with a very low probability of malignancy, potentially reducing radiologists' workload and minimizing over-reading. The safety net function alerts radiologists to potentially suspicious findings that might otherwise be dismissed, particularly serving as a safeguard against missed diagnoses [56].
In the prospective PRAIM implementation study involving 461,818 women, AI-supported double reading demonstrated a statistically significant improvement in cancer detection rate (6.7 vs. 5.7 per 1,000) while maintaining non-inferior recall rates (37.4 vs. 38.3 per 1,000) compared to standard double reading [56]. This real-world evidence indicates that AI integration can simultaneously improve sensitivity and specificity in population-based screening.
AI-Driven Risk Stratification for Personalized Screening
AI-based mammographic risk models are advancing risk-stratified screening approaches that could optimize specificity at a programmatic level. These models demonstrate superior discriminatory accuracy compared to classical risk models (e.g., Gail, Tyrer-Cuzick) and can identify women who would benefit from modified screening intervals or supplemental imaging [53]. Emerging multimodal AI systems integrate imaging data with genetic, clinical, and density risk factors to enable dynamic, personalized screening strategies that potentially reduce false positives in low-risk populations while intensifying surveillance for high-risk individuals [53].
Methodological Approaches in Key Studies
Experimental Protocols for ABUS Evaluation
The diagnostic performance of Automated Breast Volume Scanning (ABVS) was evaluated in a prospective study involving 93 patients with 103 breast lesions classified as BI-RADS category 4 or higher. All participants underwent both ABVS and ultrasound elastography (UE), with pathological biopsy results serving as the reference standard [57]. The ABVS examination was performed using an intelligent automated breast volume ultrasound system with a high-frequency linear volumetric probe. Patients were positioned supine with arms raised for full breast exposure, with scanning in medial, lateral, and central positions (additional planes for larger breasts). Two radiologists with over eight years of experience analyzed images independently, evaluating features including convergence sign, angulation, spiculation, and microcalcifications [57].
The combination of ABVS and UE demonstrated superior diagnostic performance compared to either modality alone, with sensitivity of 91%, specificity of 75%, and overall accuracy of 84%. This integrated approach enhances lesion localization, reduces operator dependency, and improves diagnostic reliability for breast cancer detection [57].
AI Implementation Study Design
The PRAIM study employed an observational, multicenter, real-world implementation design comparing AI-supported double reading to standard double reading without AI support. From July 2021 to February 2023, 463,094 women were screened across 12 sites in Germany by 119 radiologists. Examinations were assigned to the AI group when at least one radiologist used the AI-supported viewer, with radiologists free to choose on a per-examination basis [56].
The AI system featured two key functions: (1) Normal triaging, which tagged 56.7% of examinations as highly unsuspicious, and (2) Safety net, which triggered alerts for 1.5% of examinations deemed highly suspicious. The study controlled for confounders through overlap weighting based on propensity scores, with the primary endpoints being cancer detection rate and recall rate [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for breast imaging studies
| Item | Function/Application | Example Specifications |
|---|---|---|
| Automated Breast Volume Scanner (ABVS) | Acquisition of whole-breast volumetric ultrasound images | High-frequency linear volumetric probe (7-14 MHz); standard medial, lateral, and central scanning positions [57] |
| Ultrasound Elastography System | Assessment of tissue stiffness for lesion characterization | Samsung RS80A system with 7-14 MHz probe; modified BI-RADS-based 5-point elastography scoring system [57] |
| AI-Based CAD Software | Mammogram triage, lesion detection, risk assessment | Vara MG (CE-certified); normal triage and safety net functionality; abnormality scores (0-99%) [56] [58] |
| Contrast-Enhanced Mammography System | Functional imaging of lesion vascularity | GE Healthcare Senographe Essential; iodine contrast medium (1.5 mL/kg); low-energy and high-energy image acquisition [54] |
| BI-RADS Reference Standards | Standardized classification and reporting | BI-RADS density categories (A-D); assessment categories (0-6) with subcategories for precise risk stratification [54] [57] |
Integrated Strategies for Optimal Specificity
The evidence supports a multimodal, risk-adapted approach to optimizing specificity in breast cancer screening. Combined modality strategies demonstrate superior performance, with FFDM + ABUS achieving 100% sensitivity while maintaining reasonable specificity (75-81.4%) in dense breasts [54] [39]. Artificial intelligence systems show particular promise, with the PRAIM study demonstrating a 17.6% higher cancer detection rate without increasing recall rates [56].
Future directions should focus on implementing risk-stratified screening protocols that utilize AI-based risk prediction to personalize screening intervals and modalities. Women at higher risk may benefit from supplemental ABUS or CEM, while those at lower risk could maintain standard mammographic screening with potentially extended intervals. This approach requires prospective validation through ongoing trials such as WISDOM and MyPeBS, which are comparing personalized, risk-based screening to conventional age-based screening [53].
The integration of AI decision support with automated ultrasound technologies represents the most promising frontier for simultaneously maximizing sensitivity and specificity while addressing the limitations of conventional mammography in dense breast tissue.
Breast cancer remains one of the most significant health challenges for women worldwide, making efficient and accurate diagnostic workflows critical for early detection and treatment planning [55]. Within this context, the choice of imaging modality directly impacts clinical efficiency, diagnostic consistency, and resource allocation. This guide provides an objective, data-driven comparison of two fundamental imaging technologies—traditional digital mammography and Automated Breast Ultrasound (ABUS)—focusing specifically on workflow efficiency metrics, namely examination times and operator dependency. As healthcare systems globally face increasing screening demands and radiologist shortages [59], understanding these practical operational differences is essential for researchers designing imaging studies and evaluating diagnostic pathways.
Full-Field Digital Mammography (FFDM) and Digital Breast Tomosynthesis (DBT)
Full-Field Digital Mammography (FFDM) is a well-established digital technology that has largely replaced screen-film mammography. It uses digital detectors to convert X-ray photons into an electric charge, which is then processed by a computer to display an image on a high-resolution monitor [60]. While FFDM offers better contrast resolution than its film-based predecessors, it retains a core workflow constraint: the need for firm breast compression in two standard views (craniocaudal and mediolateral oblique) for each breast [60]. This process is a significant factor in the patient's experience and the technologist's active involvement time.
Digital Breast Tomosynthesis (DBT), or 3D mammography, represents a major advancement. It involves capturing a series of low-dose, two-dimensional projections from different X-ray tube angles, which are then reconstructed into thin slices (typically 0.5–1 mm thick) [60]. This minimizes the masking effect of overlapping tissue, particularly in dense breasts. However, this comes with workflow trade-offs: the breast compression time is longer than in conventional mammography, and the interpretation time for radiologists is significantly longer due to the larger volume of images to review [60]. The radiation dose for DBT is also approximately 2.2 times that of standard digital mammography [60].
Automated Breast Ultrasound (ABUS)
Automated Breast Ultrasound (ABUS) is a volumetric sonographic technique designed to standardize breast ultrasound imaging. Approved by the U.S. Food and Drug Administration in 2012, it separates image acquisition from interpretation [55] [60]. A trained technician or radiographer positions an automated transducer on the breast in several standard views (typically anteroposterior, lateral, and medial). The system then automatically acquires 3D volumetric data of the entire breast, which is stored and sent to a dedicated workstation for radiologist review [20] [13].
The key workflow advantages of ABUS stem from its reduced operator dependence during acquisition. Unlike Hand-Held Ultrasound (HHUS), which requires a skilled sonographer to both manipulate the probe and interpret images in real-time, ABUS standardizes the process. This results in higher reproducibility and more consistent imaging results [55] [60]. The system provides high-resolution, multiplanar reconstructions, including a unique coronal plane, which offers valuable anatomical information not available with conventional ultrasound [20].
Comparative Workflow and Performance Data
The following table summarizes the key quantitative and qualitative differences in workflow and diagnostic performance between FFDM, ABUS, and, where data is available, HHUS.
Table 1: Comparative Workflow and Diagnostic Performance of Breast Imaging Modalities
| Parameter | Full-Field Digital Mammography (FFDM) | Automated Breast Ultrasound (ABUS) | Hand-Held Ultrasound (HHUS) |
|---|---|---|---|
| Examination & Interpretation Workflow | Technologist-operated acquisition; Radiologist interprets 2D images. | Technician-operated acquisition; Radiologist interprets 3D volume datasets at a workstation [20]. | Sonographer performs both acquisition and real-time interpretation; highly operator-dependent [60]. |
| Operator Dependency | Moderate (standardized compression and positioning required) [60]. | Low during acquisition; minimizes operator variability [55] [60]. | Very High; quality and completeness of exam depend on sonographer's skill and experience [60]. |
| Typical Examination Time (Data Acquisition) | Relatively fast image acquisition per view. | Image acquisition is minimally operator-dependent and consistent [55]. | Operator-dependent and time-consuming; duration varies by operator [55]. |
| Radiologist Interpretation Time | Standard time for 4 images (2 per breast). | Less radiologist time required compared to HHUS [60]. | Considerable radiologist time is required for real-time scanning. |
| Reproducibility | High, due to standardized projections and compression. | High; provides standardized, reproducible scans [55] [60]. | Low, due to high operator dependence [55]. |
| Sensitivity (Pooled) | 0.81 (0.78, 0.84) [55] | 0.90 (0.89, 0.91) [55] | 0.86 (0.84, 0.87) [55] |
| Specificity (Pooled) | 0.90 (0.88, 0.91) [55] | 0.87 (0.86, 0.88) [55] | 0.80 (0.78, 0.81) [55] |
| Area Under Curve (AUC) | 0.887 [55] | 0.956 [55] | 0.898 [55] |
| Key Workflow Advantage | Rapid, standardized image acquisition; gold standard for screening. | Standardized acquisition, less operator dependence, and efficient radiologist review [55] [60]. | Real-time feedback and ability to assess areas of concern dynamically. |
| Key Workflow Limitation | Long compression time for DBT; long interpretation time for DBT slices [60]. | Inability to assess axilla; artifacts from poor positioning can occur [13]. | High operator dependency leads to variability and longer, more costly exams [55]. |
Experimental Protocols for Performance Evaluation
To ensure the validity and reproducibility of comparative studies between mammography and ABUS, researchers must adhere to rigorous methodological protocols. The following synthesizes a standard framework based on published diagnostic accuracy studies.
Patient Selection and Study Design
- Study Population: Recruit a consecutive series of women presenting for diagnostic breast evaluation following an abnormal screening mammogram or with symptomatic breast lesions. The study should aim to include a representative sample of breast density types [13].
- Inclusion Criteria: Women aged 18 years or older with focal breast lesions detectable by at least one imaging modality, who provide informed consent for all examination types and subsequent pathological verification if indicated [13].
- Exclusion Criteria: Standard exclusions include pregnancy, lactation, prior breast surgery or biopsy within the last 12 months, and contraindications to any of the study procedures (e.g., allergy to iodinated contrast if CEM is also being evaluated) [13].
- Study Design: A single-center, prospective or retrospective, within-subject comparative design is typical, where each participant undergoes both index tests (FFDM and ABUS) and a reference standard test.
Imaging Acquisition Protocols
FFDM/DBT Protocol:
- Equipment: Use FDA-approved digital mammography systems with tomosynthesis capability.
- Procedure: Perform standard craniocaudal (CC) and mediolateral oblique (MLO) views for each breast with adequate compression. For DBT, the equipment will automatically acquire the series of low-dose projections over a specified arc [60].
- Technologist Requirements: Procedures must be performed by certified radiographers following MQSA standards.
ABUS Protocol:
- Equipment: Use an FDA-approved ABUS system (e.g., GE Invenia ABUS, Siemens ACUSON S2000 ABVS) [20].
- Procedure: With the patient in a supine position, a trained radiology technician applies the automated transducer to scan each breast in at least three standard views: anteroposterior, lateral, and medial. Additional views may be taken to ensure complete coverage [13].
- Data Handling: The acquired volumetric datasets are stored digitally on a dedicated workstation for subsequent review by radiologists [20].
Image Analysis and Reference Standard
- Blinded Reading: The FFDM/DBT and ABUS studies should be interpreted independently by different radiologists, or by the same radiologist with a sufficient washout period (e.g., 4 weeks), who are blinded to the other modality's results and the final pathological outcome [13].
- Standardized Reporting: All lesions must be described and classified according to the Breast Imaging Reporting and Data System (BI-RADS) [13]. Key features to document for each lesion include size, margin characteristics (circumscribed vs. indistinct), and other morphological descriptors specific to each modality.
- Reference Standard: Histopathological analysis of tissue samples obtained via core needle biopsy (CNB) or vacuum-assisted biopsy (VAAB) serves as the reference standard for verified lesions. For studies evaluating screening efficacy, a minimum one-year clinical follow-up is an acceptable alternative for benign cases [13].
Statistical Analysis
- Outcome Measures: Calculate sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and overall accuracy for each modality, along with their 95% confidence intervals.
- Comparison Tests: Use McNemar's test for paired proportions to compare sensitivity and specificity between FFDM and ABUS. The Mann-Whitney U test can be used to compare the agreement of lesion size measurements with histopathology [13].
- Workflow Metrics: Record and compare the average total examination time (from patient setup to scan completion) and the average radiologist interpretation time for each modality. Data can be analyzed using paired t-tests.
Workflow and Operational Pathways
The fundamental difference in operational workflow between technologist-driven mammography and technician-driven ABUS has significant implications for staffing, training, and throughput. The diagram below illustrates these distinct pathways.
Essential Research Reagents and Materials
For researchers aiming to replicate or build upon comparative studies of breast imaging modalities, familiarity with the key technological systems and analysis tools is fundamental. The following table details the essential "research reagents" in this field.
Table 2: Key Research Reagents and Materials for Breast Imaging Comparison Studies
| Item Name | Function/Description | Example Products/Vendors |
|---|---|---|
| Full-Field Digital Mammography (FFDM) System | Acquires high-resolution 2D digital images of the compressed breast; the baseline technology for comparison. | Systems from Hologic Inc., GE Healthcare, Siemens Healthineers AG [61]. |
| Digital Breast Tomosynthesis (DBT) System | Acquires a series of low-dose projections to create 3D slice images; used to assess advantages over 2D FFDM. | Systems from Fujifilm Holdings Corp, Hologic Inc, GE Healthcare [61]. |
| Automated Breast Ultrasound (ABUS) System | Acquires standardized, volumetric 3D ultrasound data of the entire breast with minimal operator dependence. | GE Invenia ABUS, Siemens ACUSON S2000 ABVS [20] [62]. |
| Hand-Held Ultrasound (HHUS) System | Serves as a control for traditional ultrasound; requires a skilled operator for both acquisition and interpretation. | High-resolution systems from Hitachi Ltd., Canon Medical Systems, Philips [63] [62]. |
| BI-RADS Atlas | The standardized lexicon for describing breast imaging findings; critical for ensuring consistent reporting and data collection across readers. | Published by the American College of Radiology (ACR). |
| Dedicated Workstation with 3D Post-Processing | Allows radiologists to review, manipulate, and interpret multi-planar ABUS reconstructions (axial, sagittal, coronal). | Vendor-specific workstations (e.g., GE Invenia ABUS Workstation, Siemens syngo BREAST CARE). |
| Statistical Analysis Software | For performing advanced statistical comparisons of diagnostic accuracy and workflow metrics (e.g., McNemar's test, ROC analysis). | R, SPSS, SAS; Meta-DiSc for meta-analyses [55]. |
The objective comparison of workflow metrics between traditional mammography and automated breast ultrasound reveals a clear trade-off. While digital mammography (FFDM/DBT) remains the reference standard for population-based screening with a rapid acquisition time, it faces challenges related to operator-dependent compression and, in the case of DBT, increased radiologist interpretation times [60].
ABUS addresses the critical limitation of high operator dependency associated with conventional HHUS, providing a standardized, reproducible imaging process that is less reliant on the technician's skill during acquisition [55] [60]. This makes ABUS a powerful tool for supplemental screening, particularly in women with dense breast tissue, where it has demonstrated superior sensitivity and overall diagnostic accuracy (AUC: 0.956) compared to both HHUS and mammography [55]. For researchers and clinicians, the choice between these modalities must balance diagnostic performance with practical workflow considerations, including technologist and radiologist time, staffing expertise, and the need for consistent, reproducible results in both clinical and research settings.
Breast cancer remains a paramount global health challenge, representing the most frequent malignant tumor in women worldwide [21]. While mammography has served as the cornerstone of breast cancer screening programs, demonstrating significant value in early detection and mortality reduction, its limitations are well-documented, particularly regarding variable sensitivity in dense breast tissue [25] [21]. The evolution from screen-film mammography to full-field digital mammography (FFDM) marked one significant advancement, yet the quest for improved accuracy has propelled the development of two transformative technologies: Digital Breast Tomosynthesis (DBT) and Automated Breast Ultrasound (ABUS).
DBT, often called 3D mammography, addresses the fundamental issue of tissue superposition by creating a three-dimensional volumetric image through multiple low-dose X-ray exposures [25]. ABUS, conversely, employs automated ultrasound technology to generate standardized, reproducible 3D images of the entire breast, offering a radiation-free alternative that is particularly beneficial for dense breast evaluation [50] [49]. This comprehensive analysis objectively compares the performance of these imaging modalities, synthesizing experimental data to elucidate the synergistic potential of combining ABUS with tomosynthesis and traditional mammography within a rapidly advancing diagnostic landscape.
Technical Foundations and Operational Principles
Digital Breast Tomosynthesis (DBT): 3D Mammographic Imaging
Digital Breast Tomosynthesis represents a significant technological evolution from conventional 2D mammography. The system operates by moving an X-ray tube along a circular arc, capturing a series of low-dose exposures from different angles over a few seconds [25]. These projection images are subsequently reconstructed into thin-section images, typically 1 mm thick, which radiologists can scroll through individually. For a breast compressed to 60 mm, this process yields approximately 60 individual images for review, effectively eliminating the tissue superposition that plagues conventional 2D mammography [25]. In clinical practice, DBT is often performed in "combo-mode" (2D+3D), where both standard 2D digital mammography and tomosynthesis are acquired during the same examination, though this approach increases radiation exposure compared to 2D mammography alone [25].
Automated Breast Ultrasound (ABUS): Standardized Sonographic Evaluation
Automated Breast Ultrasound Systems address the critical limitations of traditional handheld ultrasound (HHUS), namely operator dependency and non-standardized documentation [49] [3]. ABUS utilizes a computer-guided automated arm with an attached transducer that acquires images in a standardized protocol, capturing the entire breast volume in rows both longitudinally and transversally [3]. The system typically generates images in anteroposterior, lateral, and medial standard views for each breast, with capability for additional views when necessary [3]. Dedicated software then reconstructs these acquisitions into 3D volume sets that radiologists can review at a workstation, allowing examination of the breast tissue in multiple planes and angles [50]. This automation not only standardizes the examination but also significantly reduces the operator time required compared to HHUS, saving approximately 20-30 minutes per examination according to some studies [3].
Table 1: Core Technical Specifications of DBT and ABUS
| Parameter | Digital Breast Tomosynthesis (DBT) | Automated Breast Ultrasound (ABUS) |
|---|---|---|
| Imaging Principle | X-ray tomography with multiple low-dose exposures | High-frequency sound waves (typically 7-13 MHz) |
| Image Output | Series of 1-mm thick reconstructed slices | 3D volumetric dataset of entire breast |
| Standard Views | Mediolateral-oblique (MLO) and craniocaudal (CC) | Anteroposterior (AP), lateral, and medial |
| Acquisition Time | 10-25 seconds per projection [21] | Varies by breast size; automated sequence |
| Key Innovation | Reduces tissue superposition artifact | Eliminates operator dependency |
| Radiation Exposure | Higher than 2D mammography in combo-mode | None |
Comparative Performance Metrics: Experimental Data Analysis
Cancer Detection Rates: Sensitivity Across Breast Densities
The fundamental metric for any breast imaging modality is its ability to detect malignancies accurately. Large-scale observational studies demonstrate that DBT achieves significantly higher cancer detection rates compared to 2D mammography alone. In a massive analysis of 7,602,869 screening mammograms across 4,580,698 women, DBT was associated with a cancer detection rate of 4.9 per 1000 screens compared to 3.8 for 2D mammography (P < 0.001) [64]. This represents a statistically significant 29% increase in cancer detection. The improvement is particularly notable in specific patient subgroups, with younger women (aged 40-44 years) experiencing greater benefit [64].
ABUS demonstrates particularly strong performance in populations where mammography has recognized limitations. In women with dense breast tissue (ACR categories C and D), where mammographic sensitivity can decrease to 50% or lower, ABUS provides substantial diagnostic gains [3]. One prospective study of 25 women found that ABUS detected three additional lesions categorized as BI-RADS 2 and 3 compared to mammography alone, with reported sensitivity of 100% and specificity of 62.5% in this cohort [3]. The integration of computer-aided detection (CAD) software with ABUS further improves detection rates, with studies showing sensitivity improvements of 5.2-10.6% across readers [3].
Recall Rates and Specificity: Reducing False Positives
Recall rates, representing the proportion of women requiring additional imaging following screening, directly impact healthcare costs, resource utilization, and patient anxiety. DBT consistently demonstrates favorable recall characteristics compared to 2D mammography. In the large observational study previously referenced, DBT was associated with modestly lower recall rates overall (113.6 vs. 115.4 per 1000 screens, P < 0.001), with more substantial reductions observed in younger women aged 40-44 years (153 vs. 164 per 1000 screens, P < 0.001) [64]. This reduction in false positives stems from DBT's ability to clarify ambiguous findings caused by tissue superposition in conventional 2D mammography [25].
A screening cohort study of 1,499 Mexican patients demonstrated the recalibration potential of DBT when used for secondary assessment. After tomosynthesis review, 30 patients over age 50 initially assigned higher BI-RADS categories were appropriately downgraded to BI-RADS 2, preventing unnecessary follow-up [21]. When specifically evaluating the re-staging of suspicious lesions (BI-RADS 3, 4, or 5), the study reported a specificity of 98% for DBT, significantly reducing false positive assignments [21].
Table 2: Comparative Performance Metrics from Clinical Studies
| Performance Metric | Digital Mammography | Digital Breast Tomosynthesis | Automated Breast Ultrasound |
|---|---|---|---|
| Cancer Detection Rate | 3.8/1000 screens [64] | 4.9/1000 screens [64] | Increases detection in dense breasts [3] |
| Overall Recall Rate | 115.4/1000 screens [64] | 113.6/1000 screens [64] | Data limited |
| Specificity | 57% (suspicious lesions) [21] | 70% (suspicious lesions) [21] | 62.5% (reported in one study) [3] |
| Sensitivity in Dense Breasts | Decreases significantly [3] | Improved over 2D mammography [25] | 100% (reported in small study) [3] |
| Biopsy Rate | 15.2/1000 screens [64] | 19.6/1000 screens [64] | Data limited |
| Positive Predictive Value (PPV3) | Data limited | Data limited | Data limited |
Limitations and Trade-offs: Balancing Benefits with Drawbacks
Each modality presents distinct limitations that must be considered in clinical implementation. DBT exposes patients to higher radiation doses compared to 2D mammography alone, particularly when operated in "combo-mode" [25]. While the development of synthesized 2D images from DBT data may reduce this exposure by nearly 50%, this approach remains under investigation [25]. Additionally, the interpretation time for DBT studies is generally longer than for 2D mammography due to the increased number of images requiring review [25].
ABUS, while radiation-free, has several notable limitations. The system cannot assess the axilla, evaluate tissue vascularization via Doppler, or perform elasticity assessment [49]. Image quality can be compromised by various artifacts, including those related to patient positioning, lack of transducer contact, patient motion, or lesion characteristics [49]. Furthermore, the coronal plane images generated by ABUS may present a learning curve for radiologists accustomed primarily to mammographic interpretation [49].
Synergistic Integration: Experimental Evidence for Combined Approaches
Complementary Strengths in Clinical Practice
The integration of ABUS with mammographic technologies creates a powerful diagnostic paradigm that leverages the complementary strengths of each modality. DBT excels in characterizing microcalcifications and architectural distortions, while ABUS provides superior soft-tissue contrast resolution particularly valuable in dense parenchyma [49] [3]. This complementary relationship was evidenced in a 2025 cost-effectiveness analysis which concluded that combined screening with both mammographic and ABUS imaging results in an incremental cost-effectiveness ratio of $7,071 when compared to traditional mammographic imaging alone (p < 0.05) [6]. The study further determined that for women with increased breast density or elevated breast cancer risk, this combined approach represents a cost-effective screening strategy [6].
Workflow Integration and Diagnostic Pathways
The combination of these technologies can be integrated into screening workflows through various pathways, depending on patient risk factors, breast density, and available resources. For women with dense breasts (ACR categories C and D), sequential screening with mammography (2D or DBT) followed by ABUS maximizes detection sensitivity. For high-risk patients where MRI is contraindicated or unavailable, the mammography-ABUS combination provides a valuable alternative screening strategy.
Diagram 1: Integrated Screening Pathway for DBT and ABUS. This workflow demonstrates how DBT and ABUS can be sequentially implemented in a screening population, with ABUS serving as a valuable adjunct in cases of dense breast tissue or discordant findings.
Research Reagents and Methodological Toolkit
Table 3: Essential Research Materials and Methodological Components
| Component | Function in Research | Exemplars/Notes |
|---|---|---|
| DBT Imaging Systems | Acquisition of 3D tomosynthesis datasets | Systems from GE HealthCare, Hologic, Inc., Siemens Healthineers [65] |
| ABUS Imaging Systems | Automated 3D ultrasound volume acquisition | Systems from GE HealthCare, Siemens Healthineers, Delphinus Medical Technologies [65] |
| BI-RADS Atlas | Standardized lesion classification and reporting | BI-RADS 5th edition for consistent terminology [21] |
| Phantom Test Objects | Quality control and system performance validation | Required for standardized comparison across platforms |
| CAD Software | Computer-aided detection/diagnosis | Improves sensitivity for both DBT and ABUS interpretation [3] |
| Dedicated Workstations | Multiplanar image review and analysis | Essential for interpretation of 3D datasets from both modalities |
| Validation Reference Standard | Histopathological correlation | Essential for determining true positive and false positive rates |
The comprehensive analysis of current evidence demonstrates that both Digital Breast Tomosynthesis and Automated Breast Ultrasound offer significant advantages over conventional digital mammography alone, albeit with distinct and complementary strengths. DBT provides generalized improvement in cancer detection rates and recall reduction across broad screening populations, while ABUS delivers particularly powerful enhancement in diagnostic sensitivity for women with dense breast tissue. The synergistic combination of these technologies represents a promising pathway toward personalized breast cancer screening based on individual patient characteristics, particularly breast density and risk profile. Future research directions should prioritize long-term outcome studies, refined patient selection criteria, and continued technological innovation integrating artificial intelligence to further optimize detection accuracy while minimizing unnecessary interventions.
Evidence-Based Performance Metrics: A Rigorous Diagnostic Accuracy Assessment
The early and accurate detection of breast cancer is a cornerstone of improving patient outcomes. This guide provides a systematic, data-driven comparison of the diagnostic performance of various breast imaging modalities, with a specific focus on the evolving role of automated breast ultrasound. The following data, synthesized from recent meta-analyses and multicenter studies, offers researchers and clinicians a quantitative basis for technology selection and evaluation.
Table 1: Pooled Diagnostic Performance of Breast Imaging Modalities
| Imaging Modality | Pooled Sensitivity (95% CI) | Pooled Specificity (95% CI) | Area Under Curve (AUC) | Diagnostic Odds Ratio (DOR) | Primary Source (Year) |
|---|---|---|---|---|---|
| Automated Breast Volume Scanning (ABVS) | 0.90 (0.89–0.91) | 0.87 (0.86–0.88) | 0.956 | 74.63 | [66] (2025) |
| Hand-Held Ultrasound (HHUS) | 0.86 (0.84–0.87) | 0.80 (0.78–0.81) | 0.898 | 22.88 | [66] (2025) |
| Mammography (MG) | 0.81 (0.78–0.84) | 0.90 (0.88–0.91) | 0.887 | 31.41 | [66] (2025) |
| Mammography (in Dense Breasts) | 0.74 | 0.93 | - | - | [67] (2020) |
| Contrast-Enhanced MRI (CE-MRI) | 0.97 (0.86–0.99) | 0.69 (0.46–0.85) | - | - | [68] (2022) |
| Contrast-Enhanced Mammography (CEM) | 0.91 (0.77–0.97) | 0.74 (0.52–0.89) | - | - | [68] (2022) |
| ML-based MRI Models | 0.86 (0.82–0.90) | 0.82 (0.78–0.86) | 0.90 | 39.11 | [69] (2025) |
| AI-Assisted Ultrasound Elastography | 0.90 (0.85–0.94) | 0.88 (0.81–0.93) | 0.95 | 67 | [70] (2025) |
The data in Table 1 reveals a clear hierarchy of sensitivity. Contrast-Enhanced MRI (CE-MRI) demonstrates the highest pooled sensitivity (97%), making it a powerful tool for ruling out disease [68]. Following closely are Automated Breast Volume Scanning (ABVS) and emerging AI-assisted techniques, which show significantly higher sensitivity (90% and above) than traditional mammography [66] [70]. Mammography, while offering high specificity, shows a marked decrease in sensitivity, particularly in women with dense breast tissue, where it falls to 74% [67]. The combination of MG and US significantly improves detection sensitivity to 96%, albeit with a slight trade-off in specificity [67].
Detailed Methodological Protocols of Key Studies
A critical understanding of the data requires an examination of the experimental designs from which it was derived. The following section details the methodologies of pivotal studies cited in this guide.
Protocol: Large-Scale Diagnostic Meta-Analysis (2025)
This seminal meta-analysis provided a direct comparison of ABVS, HHUS, and MG, forming a core dataset for this guide [66].
- Objective: To systematically evaluate and compare the diagnostic accuracy of ABVS, HHUS, and molybdenum-target mammography for breast lesions.
- Data Sources & Search Strategy: Researchers conducted a comprehensive computer-based search of eight major databases, including PubMed, Embase, Web of Science, Cochrane Library, Wanfang Data, CNKI, VIP, and SinoMed.
- Study Selection & Eligibility: The search included studies from database inception to August 2022. Inclusion was limited to studies reporting on the accuracy of the three modalities for diagnosing benign and malignant breast lesions. The final analysis incorporated 31 studies, encompassing 8,107 lesions.
- Data Synthesis & Quality Assessment: Meta-Disc software was used for Chi-square tests, and the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool was employed to evaluate risk of bias and methodological quality. Pooled estimates for sensitivity, specificity, and other metrics were calculated using bivariate models.
Protocol: Multicenter Cross-Sectional Study in China (2021)
This large prospective study offers robust, head-to-head performance data in a symptomatic population [71].
- Objective: To evaluate the diagnostic performance of ABUS by directly comparing it to HHUS and mammography.
- Study Design & Population: A multicenter cross-sectional study was conducted across five tertiary hospitals in China between February 2016 and March 2017. It recruited 1,922 symptomatic women aged 30-69.
- Imaging Protocol:
- Women aged 30-39 (Group A, n=677) underwent both ABUS and HHUS.
- Women aged 40-69 (Group B, n=1245) underwent ABUS, HHUS, and mammography.
- Image Interpretation & Reference Standard: All images were interpreted using the BI-RADS classification. Pathological confirmation (via biopsy or surgery) was obtained for all BI-RADS 4 and 5 lesions, providing a robust reference standard. Sensitivities and specificities were directly compared using statistical tests.
Protocol: Evaluation of Small (≤2 cm) Breast Cancer Detection (2021)
This study highlights the impact of tumor size and breast density on diagnostic performance [72].
- Objective: To compare the sensitivity of MG, US, MRI, and their combinations for detecting small (≤2 cm) breast cancer.
- Study Design & Patients: An observational retrospective review of 475 patients with pathologically confirmed breast cancer (tumor size ≤2 cm) was performed.
- Imaging Analysis: Preoperative MG, US, and MRI reports were reviewed and categorized as either benign (BI-RADS 1-3) or malignant (BI-RADS 4-5). Mammographic density was classified according to ACR guidelines.
- Statistical Analysis: The sensitivities of the different techniques and their combinations were compared using the McNemar test. Analysis was also stratified by breast density (low vs. high) and tumor size (≤1.0 cm vs. 1.1-2.0 cm).
Figure 1: A generalized workflow for the diagnostic evaluation of breast lesions, integrating multiple imaging modalities based on initial findings and patient factors.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing clinical studies or developing novel AI algorithms in breast imaging, the following table outlines essential "research reagents" and their functions in this field.
Table 2: Key Research Reagents and Materials for Breast Imaging Studies
| Item / Solution | Function / Rationale in Research |
|---|---|
| BI-RADS Lexicon (ACR) | Standardized terminology for reporting and data system; critical for ensuring consistency in image interpretation and study variable definition across multiple readers and sites. |
| QUADAS-2 Tool | A critical methodological "reagent" for quality assessment. Used to evaluate risk of bias and applicability in diagnostic accuracy studies included in meta-analyses. |
| Gadolinium-Based Contrast Agents | Essential for performing Contrast-Enhanced MRI and Contrast-Enhanced Mammography. The kinetics of contrast uptake are a primary source of data for malignancy assessment. |
| High-Frequency Linear Ultrasound Probes (e.g., 6-12 MHz) | The fundamental hardware for acquiring high-resolution hand-held and automated breast ultrasound images. The transducer frequency directly impacts spatial resolution. |
| Pathology Specimens (Histopathology) | The definitive reference standard against which all imaging tests are validated. Requires protocols for core needle biopsy or surgical excision of imaged lesions. |
| Machine Learning Classifiers (SVM, CNN, etc.) | Algorithmic tools for developing AI-assisted diagnostic models. Support Vector Machines (SVM), for instance, have shown high performance in MRI-based classification [69]. |
| Shear Wave Elastography (SWE) Software | Provides quantitative tissue stiffness measurements. Serves as a key input feature for AI models designed to classify benign and malignant lesions on ultrasound [70]. |
Emerging Frontiers: AI and Machine Learning Integration
The field of breast imaging is being transformed by artificial intelligence, which acts as a force multiplier for radiologists. Meta-analyses show that machine learning-based MRI models achieve a pooled sensitivity of 0.86 and specificity of 0.82 (AUC: 0.90) in classifying breast lesions, with Support Vector Machine (SVM) classifiers outperforming others like Naive Bayes [69]. Similarly, AI-assisted Ultrasound Elastography demonstrates exceptional performance, with a pooled sensitivity of 0.90, specificity of 0.88, and an AUC of 0.95, indicating high potential to standardize and improve ultrasound interpretation [70]. In mammography, AI algorithms not only match or surpass the diagnostic accuracy of human radiologists but also significantly enhance workflow efficiency, reducing reading times by 17% to 91% and proving particularly valuable in analyzing dense breast tissue [73].
Figure 2: A generalized workflow for developing and evaluating an AI-based model for breast image classification, from raw data input to performance assessment.
Breast cancer screening is a critical component of public health strategies aimed at reducing cancer mortality through early detection. The comparative effectiveness of various imaging modalities has been the subject of extensive research, particularly for women with dense breast tissue where traditional mammography demonstrates limitations. This guide provides a systematic comparison of cancer detection rates between established and emerging screening technologies, focusing on direct trial evidence and large-scale studies to inform researchers, scientists, and drug development professionals.
The fundamental challenge in breast cancer screening lies in optimizing the balance between sensitivity (correctly identifying cancer cases) and specificity (correctly excluding non-cases), while considering practical implementation factors such as cost, accessibility, and patient acceptance. This comparison examines traditional digital mammography (DM), digital breast tomosynthesis (DBT), automated breast ultrasound (ABUS), and emerging artificial intelligence (AI)-augmented approaches, with particular attention to their performance in different patient populations and breast density categories.
Methodological Approaches in Screening Trials
Study Designs and Evaluation Metrics
Cancer screening trials employ specific methodological frameworks to assess diagnostic performance. The most common designs include prospective screening studies, retrospective reader studies, and network meta-analyses that combine direct and indirect comparisons. Key performance metrics include:
- Cancer Detection Rate (CDR): Number of cancers detected per 1,000 screening examinations
- Recall Rate: Percentage of examinations requiring additional follow-up
- Sensitivity: Proportion of true cancer cases correctly identified
- Specificity: Proportion of cancer-free cases correctly identified
- Interval Cancer Rate (ICR): Cancers diagnosed between scheduled screening sessions
- Positive Predictive Value (PPV): Probability that a positive screening result truly indicates cancer
Recent advancements in trial methodology include the use of large-scale real-world evidence studies that assess performance in clinical practice settings rather than highly controlled environments. The ASSURE study, for instance, examined AI-powered workflow in over 579,000 women across 109 community-based imaging sites, providing insights into real-world effectiveness [74].
Statistical Analysis Frameworks
Comprehensive meta-analyses employ sophisticated statistical approaches including bivariate random-effects models to pool sensitivity and specificity estimates across studies. Network meta-analyses enable comparative effectiveness research between multiple modalities simultaneously, even when direct head-to-head trials are limited. Quality assessment tools such as QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies) are routinely employed to evaluate risk of bias in included studies [75].
Table 1: Key Methodological Standards in Cancer Detection Trials
| Methodological Element | Standard Approach | Purpose |
|---|---|---|
| Study Design | Prospective screening cohort | Minimize verification bias |
| Reference Standard | Histopathological confirmation | Establish definitive diagnosis |
| Outcome Metrics | CDR, sensitivity, specificity, PPV | Comprehensive performance assessment |
| Analysis Method | Bivariate random-effects models | Account for between-study heterogeneity |
| Quality Assessment | QUADAS-2 tool | Evaluate risk of bias and applicability |
Comparative Performance of Screening Modalities
Traditional Mammography and Digital Breast Tomosynthesis
Digital mammography (DM) remains the foundational breast cancer screening modality, with established mortality reduction benefits. However, its performance varies significantly based on breast density. A comprehensive meta-analysis comparing DM with digital breast tomosynthesis (DBT) demonstrated a pooled sensitivity of 80% (95% CI: 76-84%) for DM alone, with specificity of 96% (95% CI: 95-97%) [75].
DBT, which acquires multiple low-dose images to create a three-dimensional reconstruction of the breast, addresses the limitation of tissue superposition in conventional DM. The same meta-analysis, incorporating 11 studies and over 762,000 participants, found that DBT (alone or combined with DM) achieved significantly higher sensitivity of 86% (95% CI: 81-90%) while maintaining equivalent specificity of 96% (95% CI: 95-98%) [75]. This translates to a detection of approximately 70% more breast cancers compared to DM alone in randomized controlled trials [75].
The impact of DBT on interval cancer rates (ICR) is particularly noteworthy. The Malmö trial reported substantial reduction in ICR using DBT for screening, suggesting improved detection of aggressive, fast-growing tumors that would otherwise present clinically between scheduled screenings [75].
Automated Breast Ultrasound (ABUS) in Dense Breasts
For women with dense breast tissue, where mammographic sensitivity declines substantially, automated breast ultrasound has emerged as an important supplemental screening tool. ABUS addresses key limitations of handheld ultrasound by providing standardized acquisition, reduced operator dependence, and multiplanar reconstruction capabilities [4].
A large prospective observational study integrating second-generation 3D ABUS with full-field digital mammography (FFDM) in women with dense breasts demonstrated a significant increase in cancer detection. Mammography alone detected 4 cancers, while the combination with ABUS detected 8 cancers, doubling the detection rate with a diagnostic yield difference of 3.4 per 1000 women screened [76].
The performance of ABUS in clinical settings shows consistency with research environments. A retrospective study of 3,616 ABUS examinations in a screening population with 95.5% dense breasts reported a cancer detection yield of 2.77 per 1000 screening tests, with recall and biopsy rates lower than those reported in prospective trials [77]. This suggests improved real-world performance as radiologists gain experience with the technology.
Direct Comparison Through Meta-Analysis
A network meta-analysis of 19 different imaging methods provides comprehensive comparative effectiveness data. The analysis revealed that contrast-enhanced MRI (CE-MRI), magnetic resonance mammography (MRM), combined mammography and scintimammography (MG + SMM), and combined ultrasound elastography with ultrasonography (UE + US) demonstrated higher sensitivity compared to mammography alone [78].
For automated breast ultrasound specifically, a systematic review and meta-analysis of 16 studies comprising 4,115 participants reported a combined sensitivity of 0.88 (95% CI: 0.73-0.95) and specificity of 0.93 (95% CI: 0.82-0.97) for breast cancer detection. The area under the summary receiver operator characteristic curve (AUC) was 0.96 (95% CI: 0.94-0.96), indicating high overall diagnostic accuracy [79].
Table 2: Comparative Performance of Screening Modalities in Large-Scale Studies
| Modality | Sensitivity (95% CI) | Specificity (95% CI) | Cancer Detection Rate | Recall Rate |
|---|---|---|---|---|
| Digital Mammography (DM) | 80% (76-84%) | 96% (95-97%) | Reference | Variable by density |
| Digital Breast Tomosynthesis (DBT) | 86% (81-90%) | 96% (95-98%) | +70% vs. DM [75] | Similar to DM |
| ABUS + FFDM (dense breasts) | 100% (combined) [76] | 72% (combined) [4] | +3.4/1000 vs. DM alone [76] | 26.6/1000 (combined) [76] |
| ABUS alone | 88% (73-95%) [79] | 93% (82-97%) [79] | 2.77/1000 [77] | 5.2% [77] |
| AI-Powered DBT | Not reported | Not reported | +21.6% vs. DBT alone [74] | Within ACR guidelines [74] |
Emerging Technologies and Methodologies
Artificial Intelligence in Cancer Detection
Artificial intelligence has emerged as a transformative technology in cancer screening, with recent large-scale studies demonstrating significant improvements in detection performance. The ASSURE study, the largest real-world analysis of AI-driven breast cancer screening in U.S. history, evaluated an AI-powered workflow that combines computer-aided detection/diagnosis software with an AI-supported safeguard review process [74].
This novel approach demonstrated a 21.6% increase in cancer detection rate compared to state-of-the-art 3D mammography alone, while maintaining recall rates within American College of Radiology guidelines and increasing positive predictive value by 15% [74]. Importantly, these benefits were consistent across diverse patient populations, including a 22.7% boost in cancer detection for women with dense breasts and improved detection among Black women, who experience 40% higher breast cancer mortality [74].
The AI workflow demonstrates particular value in addressing disparities in screening access and performance. By providing consistent, specialist-level interpretation across community settings, AI technologies potentially reduce geographic and institutional variations in screening quality [74].
Protocol Standardization and Workflow Integration
A critical advancement in screening methodology involves the standardization of acquisition protocols and reading workflows, particularly for emerging modalities like ABUS. A typical ABUS examination includes three to five standardized views per breast (anterior-posterior, medial, and lateral), with additional views for larger breasts [4]. The coronal plane reconstruction, often described as the "surgical plane," provides unique diagnostic information through the "retraction phenomenon" - hyperechoic straight lines radiating from malignant masses [4].
The integration of ABUS into screening workflows demonstrates acceptable impacts on operational efficiency. While image acquisition takes approximately 15 minutes, the separation of acquisition from interpretation allows radiologists to read cases more efficiently [4]. Double-reading protocols and computer-aided detection (CAD) software further improve detection rates, with studies showing sensitivity improvements of 5.2-10.6% with CAD for ABUS interpretation [4].
Diagram 1: Advanced Screening Workflow with AI Integration. This diagram illustrates a contemporary breast cancer screening pathway that incorporates density assessment, supplemental imaging, and AI-powered safeguard review.
Research Reagent Solutions and Essential Materials
Table 3: Key Research Materials and Technologies for Screening Studies
| Research Tool | Function/Application | Representative Examples |
|---|---|---|
| 3D ABUS Systems | Automated acquisition of whole breast volumes | Siemens Acuson s2000 ABUS [77] |
| DBT Systems | 3D tomosynthesis acquisition | Siemens Mammomat Revelation/Inspiration [77] |
| Volumetric Density Software | Quantitative breast density assessment | Volpara Density [77] |
| AI CADe/x Systems | Computer-aided detection/diagnosis | DeepHealth Breast Suite [74] |
| BI-RADS Atlas | Standardized reporting and classification | ACR BI-RADS [77] |
| Phantom Test Objects | Quality assurance and calibration | Various commercial phantoms |
Direct trial comparisons reveal significant differences in cancer detection capabilities across screening modalities. While digital mammography remains the cornerstone of population-based screening, its limitations in dense breast tissue have driven the development and implementation of supplemental technologies. Digital breast tomosynthesis demonstrates superior sensitivity to DM while maintaining specificity, resulting in significantly improved cancer detection rates. Automated breast ultrasound provides substantial additional detection capability in women with dense breasts, though with variable impacts on recall rates.
The emerging integration of artificial intelligence into screening workflows represents a promising advancement, with large-scale real-world evidence demonstrating improved detection rates across diverse patient populations without exceeding recall rate benchmarks. These technologies appear particularly valuable for addressing disparities in screening access and performance.
Future research directions should include long-term outcomes for interval cancer reduction with advanced modalities, optimized screening strategies based on individualized risk and breast density, and continued refinement of AI algorithms for diverse populations and imaging technologies.
Analyzing Diagnostic Performance in Dense vs. Non-Dense Breast Tissue Cohorts
Breast density is a critical factor influencing the accuracy of cancer detection in medical imaging. Dense breast tissue, characterized by a high proportion of fibroglandular tissue relative to fatty tissue, appears radiologically white on mammograms—the same density as many tumors, creating a masking effect that can obscure malignancies [80]. Approximately 50% of women have dense breast tissue, which not only reduces screening sensitivity but also independently increases cancer risk [80]. This comprehensive analysis compares the diagnostic performance of digital mammography (DM) and automated breast ultrasound (ABUS) across different breast density categories, providing researchers with critical insights into optimal imaging strategies for diverse patient populations.
The fundamental challenge in dense breast imaging stems from anatomical noise. In heterogeneously dense (ACR C) and extremely dense (ACR D) breasts, the overlapping fibroglandular tissue can conceal small lesions while simultaneously creating patterns that mimic pathological findings, leading to both false-negative and false-positive results [81]. While digital breast tomosynthesis (DBT) addresses some limitations of 2D mammography by creating pseudo-3D images that reduce tissue overlap, ultrasound-based modalities leverage different physical principles to differentiate tissues based on their acoustic properties, potentially offering complementary diagnostic information [81] [80].
Comparative Diagnostic Performance Data
Performance Metrics Across Imaging Modalities
Table 1: Diagnostic Performance of Imaging Modalities in Dense Breasts
| Imaging Modality | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC |
|---|---|---|---|---|---|
| Digital Mammography (DM) | 87.7 | 49.3 | 65.1 | 78.7 | 0.820 |
| Digital Breast Tomosynthesis (DBT) | 98.2 | 15.4 | 61.3 | - | 0.568 |
| Handheld Ultrasound (HHUS) | 80.0 | 55.0 | 71.0 | - | 0.671 |
| Automated Breast Ultrasound (ABUS) | 92.8 | 93.0 | - | - | - |
| Breast MRI | 95.1 | 78.7 | 82.8 | 93.7 | 0.958 |
Data compiled from multiple studies [81] [80] [82]. PPV: Positive Predictive Value; NPV: Negative Predictive Value; AUC: Area Under Curve.
Table 2: Performance Comparison in Dense vs. Non-Dense Breasts for DBT and Ultrasound
| Breast Density | Modality | Sensitivity (%) | Specificity (%) | PPV (%) | AUC |
|---|---|---|---|---|---|
| Dense Breasts | DBT | 98.2 | 15.4 | 61.3 | 0.568 |
| Ultrasound | 80.0 | 55.0 | 71.0 | 0.671 | |
| Non-Dense Breasts | DBT | 99.2 | 22.0 | 69.2 | 0.606 |
| Ultrasound | 84.0 | 33.0 | 68.8 | 0.583 |
Data adapted from a study of 482 women recalled for assessment [81].
The quantitative data reveals several critical patterns. DBT demonstrates consistently high sensitivity across both dense (98.2%) and non-dense (99.2%) breasts, significantly outperforming ultrasound in this metric [81]. However, this high sensitivity comes at the cost of substantially reduced specificity, particularly in dense breasts (15.4%), suggesting a tendency toward false positives that may lead to unnecessary recalls and biopsies [81].
Ultrasound exhibits an inverse performance profile, with moderate sensitivity (80% in dense breasts) but superior specificity (55% in dense breasts) compared to DBT [81]. This fundamental trade-off between sensitivity and specificity represents a critical consideration when selecting imaging protocols for specific clinical scenarios.
ABUS demonstrates a more balanced performance profile with 92.8% sensitivity and 93.0% specificity in the general population, addressing some limitations of both DBT and handheld ultrasound [11]. Its automated nature reduces operator dependency while maintaining the inherent advantages of ultrasound in dense tissue characterization.
Breast MRI emerges as the superior modality across all metrics, with 95.1% sensitivity, 78.7% specificity, and an AUC of 0.958, confirming its status as the gold standard for dense breast imaging [80] [2]. However, practical constraints including cost, availability, and examination time limit its widespread implementation as a primary screening tool.
Combined Modality Approaches
Table 3: Diagnostic Performance of Multimodal Imaging Strategies
| Modality Combination | Sensitivity (%) | Specificity (%) |
|---|---|---|
| DM + DBT + US | 96.3 | 32.0 |
| DM + DBT + US + MRI | 97.5 | 29.3 |
Data from a retrospective study of 156 women with dense breasts [80] [82].
Multimodal approaches demonstrate a characteristic pattern of dramatically improved sensitivity at the expense of significantly reduced specificity. The combination of DM, DBT, and US achieves high sensitivity (96.3%), nearing MRI performance, but with markedly low specificity (32.0%) [80]. The addition of MRI to this combination only marginally improves sensitivity (97.5%) while further reducing specificity (29.3%), suggesting diminished returns and potential overdiagnosis risks [80] [82].
Experimental Protocols and Methodologies
Study Designs and Patient Populations
The cited research employs rigorous methodological approaches to compare diagnostic performance. A key study analyzed 482 women recalled for assessment after screening mammography, with participants undergoing both DBT and ultrasound examinations followed by biopsy confirmation [81]. This retrospective design with histopathological verification provides robust evidence for comparative performance analysis.
Another comprehensive investigation adopted a cross-sectional retrospective design, enrolling 156 women with dense breasts (BI-RADS categories C and D) who underwent all four imaging modalities (DM, DBT, US, and MRI) within a six-week period [80] [82]. The utilization of multiple imaging assessments in the same patient cohort enables direct within-subject comparison, minimizing confounding factors.
The reference standards employed across studies include histopathological confirmation for suspicious lesions (BI-RADS 4 and 5) and stability assessment over 12-24 months for probably benign findings (BI-RADS 3), ensuring diagnostic accuracy validation against clinically relevant endpoints [80] [82].
Image Acquisition Protocols
Standardized image acquisition protocols are critical for ensuring comparability across studies. DM and DBT examinations were typically performed using dedicated mammography systems such as the Selenia Dimensions unit (Hologic), with standard craniocaudal (CC) and mediolateral oblique (MLO) projections [81] [82]. DBT acquisitions involved X-ray tube rotation across an angular range of approximately 15° in both projections, with subsequent reconstruction of 1-mm thick slices [82].
ABUS protocols employed automated scanning systems (e.g., Invenia ABUS from GE or ACUSON S2000 ABVS from Siemens) to acquire volumetric data in three standard views: axial, sagittal, and coronal [20]. This comprehensive coverage ensures complete breast evaluation while eliminating operator dependency, a significant advantage over handheld techniques.
Breast MRI examinations utilized high-field systems (3.0 T) with dedicated breast coils and standardized protocols including T2-weighted sequences, diffusion-weighted imaging (DWI/ADC), and dynamic contrast-enhanced (DCE) T1-weighted sequences with multiple post-contrast acquisitions [82]. The inclusion of both morphological and kinetic curve analysis provides complementary diagnostic information.
Figure 1: Experimental Workflow for Comparative Imaging Studies
Technological Advancements and Research Directions
Artificial Intelligence in Breast Ultrasound
The integration of artificial intelligence (AI) with ABUS represents a transformative advancement in breast imaging. AI-based radiomics involves extracting high-dimensional quantitative features from ABUS images to construct predictive models for detection, diagnosis, and prognosis [20]. Deep learning approaches, particularly convolutional neural networks (CNNs), have demonstrated remarkable capabilities in analyzing complex ABUS datasets.
Recent research has developed innovative frameworks such as the Double Attention Recurrent Residual U-Net (DATTR2U-Net) for mass detection in ABUS images, achieving a recall of 0.7963 with a false positive rate of 5.67 per volume [83]. These architectures leverage multi-task learning approaches to simultaneously train inpainting and denoising pretext tasks, enhancing detection accuracy while reducing false positives [83].
The radiomics workflow encompasses several standardized steps: image acquisition, pre-processing and tumor segmentation, feature extraction, feature selection, and model building [20]. Traditional machine learning methods employ handcrafted feature extraction followed by classifier training, while deep learning approaches enable end-to-end feature learning directly from image data [20].
Clinical Implementation Considerations
Figure 2: Diagnostic Pathway for Dense Breast Tissue
The implementation of optimized imaging protocols must consider practical constraints and resource availability. While breast MRI demonstrates superior performance, its widespread adoption faces significant barriers including high costs, limited accessibility, and prolonged acquisition times [80]. In resource-constrained settings, the combination of DM, DBT, and US presents a pragmatic alternative with high sensitivity, albeit with specificity limitations [80].
Emerging evidence suggests that risk-adapted screening approaches incorporating individual risk factors, breast density, and local resources represent the most effective strategy for optimizing early detection while minimizing false positives and patient burden [80]. The European Society of Breast Imaging (EUSOBI) now recommends supplemental screening with breast MRI every 2-4 years for women aged 50-70 with extremely dense breasts, reflecting the evolving standard of care [80] [82].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Breast Imaging Studies
| Item | Function/Application | Example Specifications |
|---|---|---|
| Digital Mammography System | Acquisition of 2D mammographic images | Hologic Selenia Dimensions, Rhodium/Silver filters |
| Tomosynthesis System | 3D image acquisition with reduced tissue overlap | 15° tube rotation, 1mm slice reconstruction |
| Automated Breast Ultrasound | Volumetric ultrasound imaging with operator independence | GE Invenia ABUS or Siemens ACUSON S2000 ABVS |
| Handheld Ultrasound | Targeted examination with real-time imaging | High-frequency linear array transducer (e.g., L14-4.5 MHz) |
| Breast MRI System | High-resolution multiparametric imaging | 3.0 T with dedicated breast coil, dynamic contrast enhancement |
| Contrast Agents | Enhancement of vascularized lesions in MRI | Gadolinium-based (e.g., Gadovist, 0.1 mmol/kg) |
| BI-RADS/RANZCR Atlas | Standardized lesion classification and reporting | ACR BI-RADS 5th edition or RANZCR classification system |
| Histopathology Materials | Tissue processing and analysis for reference standard | Formalin fixation, paraffin embedding, H&E staining |
| Radiomics Software | High-throughput feature extraction and analysis | PyRadiomics, custom deep learning frameworks |
Essential materials and reagents compiled from multiple methodological descriptions [81] [80] [82].
The research tools and technologies outlined in Table 4 represent the foundational infrastructure for conducting rigorous comparative studies in breast imaging. The integration of AI-assisted detection systems is becoming increasingly prevalent, with recent FDA approvals of multiple machine learning algorithms for clinical applications [20] [84]. These technologies not only enhance diagnostic accuracy but also facilitate the extraction of quantitative imaging biomarkers that may reflect underlying tumor biology and prognosis.
Advanced image analysis platforms enable the computation of texture features, morphological descriptors, and deep learning-derived features that capture tumor heterogeneity [20]. The standardization of acquisition parameters and analysis methodologies remains crucial for ensuring reproducibility and comparability across research sites and clinical implementations.
The comprehensive analysis of diagnostic performance across breast density categories reveals a complex landscape of complementary strengths and limitations among imaging modalities. While DBT demonstrates superior sensitivity in both dense and non-dense breasts, its limited specificity presents clinical challenges. ABUS addresses several limitations of both mammography and handheld ultrasound, offering a balanced performance profile with reduced operator dependency.
The integration of artificial intelligence with ABUS radiomics represents a promising frontier, enabling enhanced detection accuracy while providing insights into tumor characterization and biological behavior. Future research directions should focus on optimizing multimodal imaging protocols, validating AI algorithms in diverse populations, and developing standardized reporting frameworks for quantitative imaging biomarkers.
For researchers and clinical investigators, these findings underscore the importance of context-specific modality selection based on diagnostic priorities, resource constraints, and patient characteristics. The continued advancement of imaging technologies, coupled with sophisticated computational analysis, holds significant potential for transforming breast cancer detection and personalized risk assessment across all breast density categories.
Breast cancer screening stands as a critical component of women's healthcare, with mammography serving as the cornerstone for early detection programs worldwide. However, the interpretation of screening mammograms presents significant challenges, including reader fatigue, inter-observer variability, and the masking effect of dense breast tissue. For decades, Computer-Aided Detection (CAD) systems were deployed to address these challenges, yet their impact remained limited. The emergence of Artificial Intelligence (AI), particularly deep learning-based approaches, represents a paradigm shift in assistive technologies for breast imaging. Concurrently, Automated Breast Ultrasound (ABUS) has developed as an important supplemental screening tool, especially for women with dense breasts. This article provides a comprehensive comparison of traditional CAD versus modern AI systems, framed within the context of advancements in mammography and ABUS research, examining how these technologies enhance diagnostic confidence and accuracy in clinical practice.
Technological Foundations: From Traditional CAD to Modern AI
Fundamental Differences in Approach and Capabilities
Traditional CAD and modern AI-based systems differ fundamentally in their underlying technology, learning capabilities, and clinical application. Understanding these distinctions is crucial for appreciating their divergent impacts on diagnostic performance.
Table 1: Fundamental Comparison Between Traditional CAD and Modern AI Systems
| Feature | Traditional CAD | Modern AI Systems |
|---|---|---|
| Core Technology | Traditional machine learning | Deep learning with convolutional neural networks |
| Learning Capability | Limited training on small datasets; cannot improve independently | Trained on very large datasets; capable of continuous improvement |
| Functionality | Detects structures without distinguishing malignancy | Detects and characterizes findings, displaying only suspicious ones |
| Output | Highlights all types of lesions regardless of clinical significance | Assigns a global level of suspicion to help decision-making |
| Integration | On-premise software requiring cumbersome equipment | Cloud-based technologies with lightweight deployment |
| Typical Use Case | Pattern detection without contextual understanding | Risk-stratified findings with clinical context [85] |
Visualizing the Workflow Differences
The fundamental technological differences between traditional CAD and modern AI systems create distinct workflows that directly impact radiologist performance and efficiency. The following diagrams illustrate these contrasting processes.
Performance Comparison: Quantitative Evidence from Clinical Studies
Diagnostic Accuracy in Mammography Interpretation
Recent prospective studies provide compelling evidence regarding the performance advantages of AI systems compared to traditional CAD. The AI-STREAM study, a prospective multicenter cohort study conducted within South Korea's national breast cancer screening program, offers particularly insightful data.
Table 2: Performance Metrics of Radiologists With and Without AI Assistance (AI-STREAM Study)
| Reading Condition | Cancer Detection Rate (CDR) ‰ | Recall Rate (RR) % | Number of Cancers Detected | Statistical Significance (p-value) |
|---|---|---|---|---|
| Breast Radiologists without AI | 5.01 | 4.48 | 123 | Reference |
| Breast Radiologists with AI-CAD | 5.70 | 4.53 | 140 | p < 0.001 |
| General Radiologists without AI | 3.87 | 6.31 | 95 | Reference |
| General Radiologists with AI-CAD | 4.89 | 6.89 | 120 | p < 0.001 |
| Standalone AI | 5.21 | 6.25 | 128 | No significant difference vs. breast radiologists with AI (p = 0.462) [86] [87] |
The AI-STREAM study demonstrated that AI assistance significantly improved cancer detection rates without compromising specificity—a crucial advancement over traditional CAD, which typically increased recall rates. Breast radiologists using AI-CAD detected 13.8% more cancers (140 vs. 123) without a statistically significant increase in recall rates (p = 0.564). The benefit was even more pronounced for general radiologists, who showed a 26.4% increase in cancer detection with AI support, though with a modest increase in recall rates [86].
Impact on Reading Time and Workflow Efficiency
Beyond diagnostic accuracy, the effect of assistive technologies on radiologist workflow represents a critical practical consideration.
Table 3: Workflow Impact Comparison Between Traditional CAD and AI Systems
| Efficiency Metric | Traditional CAD | Modern AI Systems |
|---|---|---|
| Reading Time Impact | Increased by approximately 25% | Enables faster reading of benign cases |
| Case Triage | Not available | Capable of prioritizing suspicious cases |
| Data Integration | Limited to single workstation | Cloud-based with multi-site compatibility |
| Result Interpretation | Multiple irrelevant markings requiring review | Global suspicion score with only meaningful findings highlighted |
| Deployment Flexibility | Requires on-site installation and maintenance | Lightweight deployment with remote support [85] |
ABUS as a Supplemental Screening Tool: Technical and Diagnostic Considerations
ABUS in the Context of Dense Breast Screening
Automated Breast Ultrasound has emerged as a valuable supplemental screening tool, particularly for women with heterogeneously dense (ACR C) and extremely dense (ACR D) breasts. The sensitivity of mammography drops from 86% in fatty breasts to less than 61% in dense breasts, while simultaneously, women with dense breasts face a 4.7-fold increased risk of developing breast cancer compared to those with fatty breasts [88]. ABUS addresses this clinical challenge through standardized, reproducible image acquisition that is operator-independent, unlike conventional handheld ultrasound.
The SomoInsight study, which included 15,318 asymptomatic women with dense breasts, demonstrated that adding ABUS to full-field digital mammography (FFDM) increased the cancer detection rate by 1.9 per 1000 women, representing a 26.7% increase in sensitivity. Similar studies have reported even greater improvements, with cancer detection rates increasing by 2.4 to 7.7 per 1000 women screened when ABUS was combined with FFDM compared to FFDM alone [4].
Technical Advantages and Limitations of ABUS
ABUS offers several technical advantages over handheld ultrasound, including standardized volumetric acquisition, multiplanar reconstruction capabilities, and the valuable coronal plane—often referred to as the "surgical plane" due to its operative perspective. The coronal plane enables visualization of the "retraction phenomenon," a stellate pattern with hyperechoic straight lines radiating from malignant lesions, which is strongly associated with smaller tumor size, lower histological grade, and positive estrogen and progesterone receptor status [4] [88].
However, ABUS has limitations, including the inability to assess axillary lymph nodes comprehensively, lack of vascularity and elasticity assessment, and various artifacts related to patient positioning, motion, or lesion characteristics. Proper technician training is crucial to minimize artifacts such as drop-out artifacts from inadequate transducer positioning, air contact artifacts, nipple shadows, and wandering shadows adjacent to Cooper's ligaments [4] [88].
Research Reagent Solutions: Essential Tools for Breast Imaging Studies
Table 4: Key Research Reagents and Platforms in Breast Imaging Studies
| Reagent/Platform | Function | Application in Featured Studies |
|---|---|---|
| Invenia ABUS System (GE Healthcare) | Automated 3D ultrasound image acquisition | Standardized volumetric breast imaging with multiplanar reconstruction [89] |
| AI-CAD Deep Learning Algorithms | Lesion detection and characterization | Improves cancer detection rates in screening mammography [86] [87] |
| BI-RADS Lexicon | Standardized terminology and reporting | Provides consistent classification across studies and modalities [90] |
| Convolutional Neural Networks (CNN) | Image analysis through deep learning | Enables feature extraction and pattern recognition in mammography [91] |
| Digital Breast Tomosynthesis (DBT) | 3D mammographic imaging | Reduces tissue superposition effects; often combined with ABUS [4] |
Experimental Protocols and Methodologies
AI-STREAM Prospective Cohort Study Design
The AI-STREAM study provides a robust methodological framework for evaluating AI in breast cancer screening. This prospective, multicenter cohort study was conducted within South Korea's national breast cancer screening program and included 24,543 women aged ≥40 years who underwent regular mammography screening between February 2021 and December 2022. Key methodological components included:
- Participant Selection: Women were excluded for parenchymal changes due to previous procedures, mammoplasty, insertion of foreign substances, withdrawn consent, or data errors.
- Reference Standard: Pathologically diagnosed breast cancer was analyzed one year after the last participant's enrollment to ensure complete follow-up.
- Reading Protocol: Radiologists interpreted screening mammograms with and without AI-based CAD assistance in a single-reading strategy.
- Outcome Measures: Primary outcomes were screen-detected breast cancer within one year, with focus on cancer detection rates and recall rates [86] [87].
ABUS Imaging Protocol
Standardized ABUS examination follows a specific protocol to ensure comprehensive breast coverage and minimize artifacts:
- Patient Positioning: Supine position with arm elevated and pillow under the shoulder to optimize comfort and breast flattening.
- Transducer Application: Three standard views per breast (anteroposterior, lateral, and medial) using a curved transducer with appropriate compression.
- Image Acquisition: Volumetric acquisitions in the axial plane with transducer movement from inferior to superior breast sections.
- Image Processing: Automatic transfer to workstation for multi-planar reconstruction with coronal and sagittal views.
- Quality Assurance: Technician evaluation of depth coverage to ensure inclusion of deep and peripheral breast tissues [88] [89].
Integrated Diagnostic Approaches: Combining Modalities for Enhanced Performance
AI with Mammography and ABUS: Future Directions
The combination of AI-enhanced mammography and ABUS represents a promising integrated approach for comprehensive breast cancer screening, particularly in high-risk populations and women with dense breasts. Recent research indicates that adding ABUS to mammographic imaging is a cost-effective screening strategy for women with increased breast density or elevated breast cancer risk, with an incremental cost-effectiveness ratio of $7,071 when compared to traditional mammographic imaging alone [6].
The emerging field of radiomics and radiogenomics further expands the potential of these technologies by extracting quantitative data from medical images and correlating imaging features with molecular characteristics. This approach allows for non-invasive analysis on the molecular level, potentially identifying subtypes, predicting treatment response, and assessing prognosis without invasive procedures [91].
Visualizing the Integrated Screening Pathway
The combination of AI-enhanced mammography and ABUS creates a comprehensive screening pathway that optimizes sensitivity and specificity for different patient populations. The following diagram illustrates this integrated approach.
The evolution from traditional CAD to modern AI systems represents a fundamental transformation in breast imaging assistance, with profound implications for diagnostic confidence and accuracy. AI-based systems demonstrate superior performance across multiple metrics, including cancer detection rates, recall rates, and workflow efficiency. When integrated with supplemental modalities like ABUS, particularly for women with dense breasts, these technologies enable a comprehensive, personalized approach to breast cancer screening. Future developments in radiomics and radiogenomics promise to further enhance the diagnostic and prognostic capabilities of these imaging technologies, ultimately advancing the goal of early detection and improved outcomes in breast cancer care.
Conclusion
The comparative analysis confirms that ABUS and mammography are complementary, not replacement, technologies in the breast cancer screening arsenal. While mammography remains the foundational population-wide screening tool, ABUS demonstrates superior diagnostic accuracy, particularly in women with dense breasts, as evidenced by recent meta-analyses showing higher pooled sensitivity and specificity. The integration of AI and standardized coronal plane imaging further enhances ABUS's diagnostic value. Future directions for biomedical research should focus on refining AI algorithms for automated interpretation, developing cost-effective protocols for widespread ABUS implementation, and conducting long-term studies to assess the impact of combined modality screening on mortality reduction. The evolution towards personalized, risk-stratified screening regimens that leverage the strengths of both technologies represents the most promising pathway for improving early detection and patient outcomes.
References
- 1. analysis of diagnostic Comparative of performance ... automatic breast [https://pubmed.ncbi.nlm.nih.gov/40196314/]
- 2. Comparative Diagnostic Efficacy of Four Breast Imaging Modalities in Dense Breasts: A Single-Center Retrospective Study - PubMed [https://pubmed.ncbi.nlm.nih.gov/40722820/]
- 3. Automated breast ultrasound system (ABUS): can it replace mammography as a screening tool? | Egyptian Journal of Radiology and Nuclear Medicine | Full Text [https://ejrnm.springeropen.com/articles/10.1186/s43055-019-0051-6]
- 4. Pros and Cons for Automated Breast Ultrasound (ABUS): A Narrative Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8400952/]
- 5. MRI, Mammography Outperform Whole Breast for Dense... Ultrasound [https://www.drugs.com/news/mri-mammography-outperform-whole-breast-ultrasound-dense-breasts-125172.html]
- 6. Adding automated breast ultrasound to mammography in women with increased breast density or at an elevated risk of breast cancer is a cost-effective screening strategy - PubMed [https://pubmed.ncbi.nlm.nih.gov/39752002/]
- 7. A deep learning-based multimodal medical imaging model for breast cancer screening | Scientific Reports [https://www.nature.com/articles/s41598-025-99535-2]
- 8. The Role of ABUS in The Diagnosis of Breast Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9231518/]
- 9. GE ABUS Club - General News - 6 New Webinars [https://www.abusclub.net/us/generalnews?id=3]
- 10. Mammography Systems Market to Reach US$ 5,719.51 Million by 2033 | Astute Analytica [https://www.globenewswire.com/news-release/2025/11/19/3191214/0/en/Mammography-Systems-Market-to-Reach-US-5-719-51-Million-by-2033-Astute-Analytica.html]
- 11. The diagnostic performance of automated versus handheld breast... [https://link.springer.com/article/10.1007/s00330-020-07197-7]
- 12. A systematic review and meta-analysis comparing the diagnostic... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10803446/]
- 13. analysis of diagnostic Comparative of automatic breast... performance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11973704/]
- 14. [2501.15588] Tumor Detection, Segmentation and Classification... [https://arxiv.org/abs/2501.15588]
- 15. : Breast or hand-held? Exploring patients... ultrasound automated [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-019-0136-z]
- 16. Dense breasts and women's health: which screenings are essential? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12356387/]
- 17. Impact of BMI on Prevalence of Dense Breasts by Race and Ethnicity - PubMed [https://pubmed.ncbi.nlm.nih.gov/37284771/]
- 18. Mammographic breast density and subsequent risk of breast cancer in postmenopausal women according to the time since the mammogram - PubMed [https://pubmed.ncbi.nlm.nih.gov/23603205/]
- 19. New Imaging Triples Dense Breast Cancer Detection [https://www.medscape.com/viewarticle/new-imaging-triples-dense-breast-cancer-detection-2025a1000d7j]
- 20. Frontiers | Artificial intelligence-based automated ... breast ultrasound [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1578991/full]
- 21. Effectiveness of Tomosynthesis Versus Digital Mammography in the Diagnosis of Suspicious Lesions for Breast Cancer in an Asymptomatic Population - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7952495/]
- 22. Digital Mammography Imaging: Breast Tomosynthesis and Advanced Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3118307/]
- 23. 2D vs. 3D Tomosynthesis - Radiology | UCLA Health [https://www.uclahealth.org/departments/radiology/education/breast-imaging-teaching-resources/screening-mammogram/2d-vs-3d-tomosynthesis]
- 24. Automated Breast Ultrasound: Technical Aspects, Impact on Breast Screening, and Future Perspectives | Current Breast Cancer Reports [https://link.springer.com/article/10.1007/s12609-021-00423-1]
- 25. Pros and cons for breast cancer screening with tomosynthesis – a review of the literature - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7664734/]
- 26. , Mammograms and MRIs: What's the... | Cedars-Sinai Ultrasounds [https://www.cedars-sinai.org/blog/mammograms-ultrasounds-mris-whats-the-difference.html]
- 27. Characterization of breast masses: a comparative study between... [https://link.springer.com/article/10.1186/s43055-020-00161-x]
- 28. Dedicated computer-aided detection software for automated 3D breast ultrasound; an efficient tool for the radiologist in supplemental screening of women with dense breasts - PubMed [https://pubmed.ncbi.nlm.nih.gov/29417251/]
- 29. ( Mammography ): Early detection of Mammogram disease. breast [https://www.radiologyinfo.org/en/info/mammo]
- 30. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/15486214/]
- 31. Enhanced Detection of Suspicious Breast Lesions: A Comparative ... [https://pubmed.ncbi.nlm.nih.gov/37689969/]
- 32. Dependability of Automated (ABUS) in Assessing... Breast Ultrasound [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647168/]
- 33. Mammography BI RADS Grading - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK539816/]
- 34. Comparison of supplemental breast cancer imaging techniques-interim results from the BRAID randomised controlled trial | Association of Breast Surgery [https://associationofbreastsurgery.org.uk/professionals/information-hub/publications/2025/comparison-of-supplemental-breast-cancer-imaging-techniques-interim-results-from-the-braid-randomised-controlled-trial]
- 35. Frontiers | BI-RADS application for breast cancer screening in primary healthcare settings: assessing protocol adherence and diagnostic validity [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1599759/full]
- 36. Diagnostic accuracy of supplemental three-dimensional breast ultrasound in the work-up of BI-RADS 0 screening recalls | Insights into Imaging | Full Text [https://insightsimaging.springeropen.com/articles/10.1186/s13244-024-01714-8]
- 37. Comparative Analysis of Automated and Handheld Breast Ultrasound Findings for Small (≤1 cm) Breast Cancers Based on BI-RADS Category [https://www.mdpi.com/2075-4418/15/2/212]
- 38. Frontiers | Reducing unnecessary biopsies of BI - RADS 4 lesions based... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1543553/full]
- 39. Comparison of Diagnostic Accuracy of Ultrasound and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535270/]
- 40. Comparative Analysis of Diagnostic Performance ... [https://www.mdpi.com/2227-9059/11/12/3226]
- 41. The evidence and concerns about screening ultrasound for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032836/]
- 42. Digital breast tomosynthesis and automated breast ultrasound [https://ejrnm.springeropen.com/articles/10.1186/s43055-025-01584-0]
- 43. Comparative analysis of diagnostic performance ... [https://www.polradiol.com/Comparative-analysis-of-diagnostic-performance-of-automatic-breast-ultrasound-and,199755,0,2.html]
- 44. Comparison of supplemental breast cancer imaging ... [https://pubmed.ncbi.nlm.nih.gov/40412427/]
- 45. The future of breast imaging: a date with density [https://healthcare-in-europe.com/en/news/future-breast-imaging-density.html]
- 46. The power of ABUS : The innovative... | GE HealthCare (United States) [https://www.gehealthcare.com/insights/article/the-power-of-abus-the-innovative-ultrasound-system-providing-endless-benefits]
- 47. The performance of 3D ABUS HHUS in the visualisation and... versus [https://link.springer.com/article/10.1007/s00330-017-5011-9]
- 48. size measurement in breast cancer patients... Preoperative tumor [https://cancerimagingjournal.biomedcentral.com/articles/10.1186/s40644-020-00307-0]
- 49. Pros and Cons for Automated ( Breast )... Ultrasound ABUS [https://pubmed.ncbi.nlm.nih.gov/34442347/]
- 50. What is Automated Systems Breast ? Uses, How It... Ultrasound Abus [https://www.linkedin.com/pulse/what-automated-breast-ultrasound-systems-abus-uses-9r24e]
- 51. : state of the art and future... - ecancer Automatic breast ultrasound [https://ecancer.org/en/journal/article/1062-automatic-breast-ultrasound-state-of-the-art-and-future-perspectives]
- 52. Re-evaluation of high-risk breast mammography lesions by target... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8549220/]
- 53. Artificial Intelligence-Driven Personalization in Breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428423/]
- 54. Comparative Analysis of Diagnostic Performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10741119/]
- 55. Diagnostic accuracy of automated breast volume scanning ... [https://gs.amegroups.org/article/view/136384/html]
- 56. Nationwide real-world implementation of AI for cancer ... [https://www.nature.com/articles/s41591-024-03408-6]
- 57. Innovative integration of automated breast volume scan ... [https://www.nature.com/articles/s41598-025-01061-8]
- 58. The Clinical Application of Artificial Intelligence in ... [https://ejbc.kr/DOIx.php?id=10.4048/jbc.2025.0123]
- 59. The Future of Breast Imaging: Navigating Change... | Signify Research [https://www.signifyresearch.net/insights/the-future-of-breast-imaging-navigating-change-capturing-growth/]
- 60. Atlas of breast cancer early detection [https://screening.iarc.fr/atlasbreastdetail.php?Index=19&e=]
- 61. Market Size, Demand & Trends to 2035 Mammography [https://www.futuremarketinsights.com/reports/mammography-market]
- 62. U.S. Automated Breast Ultrasound Systems Market Size, 2034 [https://www.gminsights.com/industry-analysis/us-automated-breast-ultrasound-systems-market]
- 63. Automated Whole-Breast Ultrasound Market to Hit USD 10.7 Bn by 2033 [https://media.market.us/automated-whole-breast-ultrasound-market-news-2025/]
- 64. Comparative Effectiveness of Digital Breast Tomosynthesis for Breast Cancer Screening Among Women 40-64 Years Old - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8757313/]
- 65. Systems ( Automated ) Market Report... Breast Ultrasound ABUS [https://finance.yahoo.com/news/automated-breast-ultrasound-systems-abus-120900891.html]
- 66. Diagnostic accuracy of automated volume scanning, hand-held... breast [https://pubmed.ncbi.nlm.nih.gov/40256474/]
- 67. Supplemental breast cancer-screening ultrasonography in women with... [https://www.nature.com/articles/s41416-020-0928-1?error=cookies_not_supported]
- 68. Contrast-enhanced Mammography versus Contrast-enhanced Breast MRI: A Systematic Review and Meta-Analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/36154284/]
- 69. Diagnostic accuracy of machine learning-based magnetic resonance imaging models in breast cancer classification: a systematic review and meta-analysis | World Journal of Surgical Oncology | Full Text [https://wjso.biomedcentral.com/articles/10.1186/s12957-025-03874-3]
- 70. Performance of artificial intelligence-assisted ultrasound elastography... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-025-01982-w]
- 71. The diagnostic performance of automated versus handheld breast ultrasound and mammography in symptomatic outpatient women: a multicenter, cross-sectional study in China - PubMed [https://pubmed.ncbi.nlm.nih.gov/32852589/]
- 72. Comparison of the sensitivity of mammography, ultrasound, magnetic resonance imaging and combinations of these imaging modalities for the detection of small (≤2 cm) breast cancer - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8257894/]
- 73. Systematic Review and Meta-Analysis of AI-Assisted Mammography and the Systemic Immune-Inflammation Index in Breast Cancer: Diagnostic and Prognostic Perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300038/]
- 74. Study Shows Effectiveness of Novel AI-Powered Breast Cancer Detection Workflow | Imaging Technology News [https://www.itnonline.com/content/study-shows-effectiveness-novel-ai-powered-breast-cancer-detection-workflow]
- 75. Impact of digital breast tomosynthesis on screening... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0315466]
- 76. Second-Generation 3D Automated Ultrasonography... Breast [https://pubmed.ncbi.nlm.nih.gov/34575652/]
- 77. Diagnostic performance of 3D automated ... breast ultrasound [https://link.springer.com/article/10.1007/s00330-023-10568-5]
- 78. Diagnostic Value of Nineteen Different Imaging Methods for Patients... [https://pubmed.ncbi.nlm.nih.gov/29723846/]
- 79. Frontiers | A systematic review and meta - analysis the... comparing [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1305545/full]
- 80. Comparative Diagnostic Efficacy of Four Breast Imaging Modalities in Dense Breasts: A Single-Center Retrospective Study [https://www.mdpi.com/2227-9059/13/7/1750]
- 81. Efficacy across Diagnostic and Dense - Non during... Dense Breasts [https://pmc.ncbi.nlm.nih.gov/articles/PMC9222054/]
- 82. study of Comparative Accuracy of Ultrasonography Diagnostic .... vs [https://www.preprints.org/manuscript/202501.0740/v1]
- 83. A multi-task self-supervised approach for mass detection in automated ... [https://pubmed.ncbi.nlm.nih.gov/39983360/]
- 84. Emerging Research and News in Breast Imaging — October 2025 | Diagnostic Imaging [https://www.diagnosticimaging.com/view/emerging-research-news-in-breast-imaging-october-2025]
- 85. vs. AI in CAD : The differences... - MammoScreen breast imaging [https://www.mammoscreen.com/is-ai-cad]
- 86. Artificial intelligence for breast cancer screening in mammography (AI-STREAM): preliminary analysis of a prospective multicenter cohort study | Nature Communications [https://www.nature.com/articles/s41467-025-57469-3]
- 87. Artificial intelligence for breast cancer screening in mammography ... [https://pubmed.ncbi.nlm.nih.gov/40050619/]
- 88. Automated Breast Ultrasound (ABUS): A Pictorial Essay of Common Artifacts and Benign and Malignant Pathology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9714281/]
- 89. Automated breast ultrasound (ABUS) as a screening tool: initial experience | Egyptian Journal of Radiology and Nuclear Medicine | Full Text [https://ejrnm.springeropen.com/articles/10.1186/s43055-019-0032-9]
- 90. Artificial Intelligence Applications in Breast Imaging: Current Status and Future Directions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10296832/]
- 91. Overview of Artificial Intelligence in Breast Cancer Medical Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9864608/]