Cancer Stem Cells: Decoding Their Central Role in Tumor Heterogeneity and Therapeutic Resistance
Cancer stem cells (CSCs) are a pivotal subpopulation driving tumor initiation, progression, and relapse due to their self-renewal capacity, differentiation potential, and profound resistance to conventional therapies.
Cancer Stem Cells: Decoding Their Central Role in Tumor Heterogeneity and Therapeutic Resistance
Abstract
Cancer stem cells (CSCs) are a pivotal subpopulation driving tumor initiation, progression, and relapse due to their self-renewal capacity, differentiation potential, and profound resistance to conventional therapies. This article synthesizes current research for an audience of researchers and drug development professionals, exploring the fundamental biology of CSCs, including their defining characteristics, key signaling pathways (Wnt/β-catenin, Notch, Hedgehog), and contributions to intratumoral heterogeneity. We detail advanced methodologies for CSC identification and isolation, examine the core mechanisms underlying their drug-resistant phenotype—such as quiescence, enhanced DNA repair, epithelial-mesenchymal transition (EMT), and ABC transporter upregulation—and evaluate emerging therapeutic strategies. These innovations, including nanomaterial-based targeting, metabolic inhibitors, immunotherapy, and dual-pathway inhibition, are critically assessed for their potential to eradicate CSCs, overcome resistance, and improve clinical outcomes.
Deconstructing Cancer Stem Cells: The Architects of Tumor Heterogeneity and Relapse
Cancer Stem Cells (CSCs) represent a functionally distinct subpopulation within tumors that drive tumor initiation, progression, therapeutic resistance, and recurrence [1] [2]. These cells exhibit core biological capabilities that define their pathogenic role in cancer biology: self-renewal, the ability to generate identical copies of themselves; differentiation, the capacity to produce heterogeneous lineages of cancer cells that constitute the tumor bulk; and tumorigenic potential, the capability to initiate and sustain tumor growth [2] [3]. These three hallmarks operate within a dynamic framework of cellular plasticity, enabled by the tumor microenvironment (TME) and underpinned by distinct molecular signaling pathways [2] [4]. Understanding these defining properties is fundamental to addressing the challenges of tumor heterogeneity and drug resistance in oncology research and therapeutic development [1] [5].
The CSC model fundamentally challenges previous conceptualizations of tumors as homogeneous masses, instead proposing a hierarchical organization wherein CSCs sit at the apex [3]. This review comprehensively examines the molecular mechanisms, experimental evidence, and research methodologies central to investigating the three defining hallmarks of CSCs, with particular emphasis on their role in fostering tumor heterogeneity and conferring resistance to conventional therapies.
Molecular Mechanisms Governing CSC Hallmarks
Core Signaling Pathways Regulating Self-Renewal and Plasticity
The hallmark capabilities of CSCs are maintained through the intricate operation of several evolutionarily conserved signaling pathways. These pathways, which are crucial for normal stem cell function and embryonic development, are frequently dysregulated in CSCs [6] [5].
Wnt/β-catenin Signaling: The Wnt pathway plays a pivotal role in maintaining CSC self-renewal [6] [5]. Upon Wnt ligand binding to the Frizzled receptor, the destruction complex (AXIN/GSK-3/APC) is inactivated, leading to β-catenin stabilization and its subsequent nuclear translocation [5]. In the nucleus, β-catenin associates with TCF/LEF transcription factors to activate target genes including MYC and CCND1, thereby promoting self-renewal and cell cycle progression [5]. Notably, β-catenin directly binds to the TERT promoter to enhance telomerase expression, maintaining telomere length—a critical feature for limitless replicative potential [5]. Non-canonical Wnt/Ca2+ signaling has also been implicated in promoting self-renewal and proliferation in colon CSCs [6].
Hedgehog (HH) Signaling: This pathway is integral to embryogenesis and tissue repair [5]. Hedgehog ligands (Sonic, Indian, and Desert) bind to Patched receptors, relieving inhibition of Smoothened and leading to activation of GLI transcription factors [5]. Activated GLI translocates to the nucleus and induces expression of genes governing cell survival, proliferation, and stemness maintenance [5]. Hedgehog signaling activation is also a known driver of epithelial-to-mesenchymal transition (EMT), a process closely linked to the acquisition of CSC properties [5].
Notch Signaling: Operating through direct cell-cell communication, Notch signaling is critical for cell fate decisions [5]. Ligand-receptor binding between adjacent cells triggers proteolytic cleavage of the Notch receptor, releasing the Notch intracellular domain (NICD) which translocates to the nucleus and forms a complex with CSL/RBP-Jκ to activate transcription of genes like HES and HEY [5]. With four receptors (Notch1-4) and five ligands (DLL1, DLL3, DLL4, Jagged-1, Jagged-2), this pathway demonstrates complex context-dependent regulation across cancer types [5].
JAK/STAT3, PI3-K/Akt, and Hippo/YAP1 Pathways: Additional pathways contribute significantly to the CSC phenotype. JAK/STAT3 and PI3-K/Akt signaling promote cell survival and growth [6] [7]. The Hippo pathway, particularly its effector YAP1, regulates CSC properties, chemo-resistance, and radio-resistance through targets including SOX9, EGFR, and CDK6 [4]. YAP1 also serves as a signaling hub integrating microenvironmental cues [4].
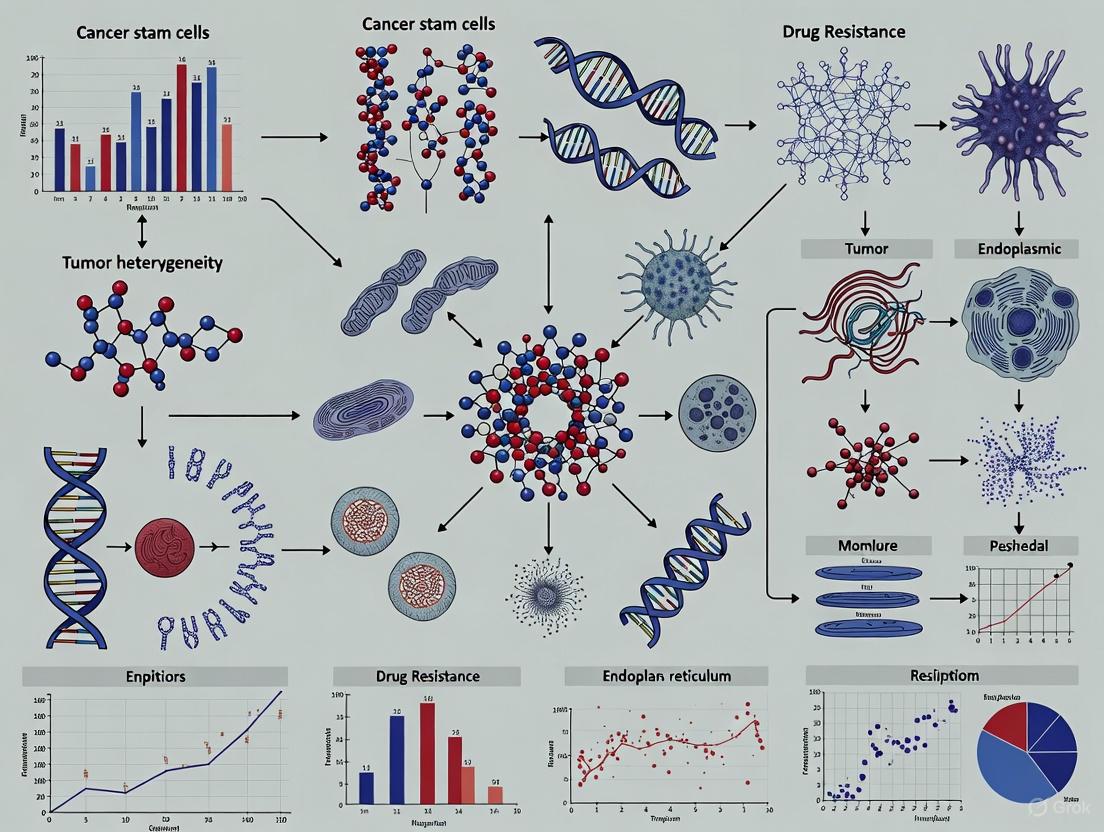
The following diagram illustrates the key signaling pathways and their interconnections in maintaining CSC hallmarks:
Metabolic Programming Supporting CSC Function
CSCs exhibit remarkable metabolic plasticity that supports their hallmark functions [1] [7]. Unlike normal stem cells that primarily rely on glycolysis to minimize reactive oxygen species (ROS) production, CSCs actively utilize both glycolysis and mitochondrial oxidative phosphorylation (OXPHOS) to meet energy demands for tumor growth while maintaining stemness [7]. This metabolic flexibility allows CSCs to adapt to varying microenvironmental conditions, including hypoxia and nutrient deprivation [1]. Additional metabolic adaptations include upregulated lipid desaturation pathways to maintain stem cell-like properties, altered iron metabolism and ferroptosis sensitivity, and enhanced ceramide signaling to facilitate immune evasion [7]. These metabolic dependencies represent emerging vulnerabilities for therapeutic targeting.
Experimental Methodologies for Investigating CSC Hallmarks
Functional Assays for Quantifying Hallmark Capabilities
Rigorous experimental methodologies are essential for investigating the functional properties of CSCs. The table below summarizes key assays and their applications in CSC research:
Table 1: Core Functional Assays for Investigating CSC Hallmarks
| Hallmark | Assay Type | Key Readouts | Experimental Significance | References |
|---|---|---|---|---|
| Self-Renewal | Sphere Formation Assay | Number and size of tumorspheres under non-adherent conditions | Measures clonal expansion and self-renewal capacity in vitro | [5] |
| In Vivo Limiting Dilution Assay | Tumor incidence and frequency of tumor-initiating cells | Quantifies self-renewal potential in immunocompromised mice | [5] [2] | |
| Tumorigenic Potential | Serial Transplantation Assay | Tumor formation capacity in secondary and tertiary recipients | Assesses long-term self-renewal and tumor-propagating ability | [2] [3] |
| In Vivo Tumor Initiation | Minimum cell number required for tumor formation | Measures potency for tumor initiation and growth | [2] [3] | |
| Differentiation | Lineage Tracing & Clonal Analysis | Heterogeneity of differentiated progeny from single CSCs | Demonstrates multi-lineage differentiation capacity | [3] |
| In Vitro Differentiation Assays | Expression of differentiation markers in adherent conditions | Evaluates potential to generate heterogeneous cancer cells | [3] |
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for CSC Investigation
| Reagent Category | Specific Examples | Research Application | Functional Role | |
|---|---|---|---|---|
| Cell Surface Marker Antibodies | Anti-CD44, Anti-CD133, Anti-CD34 | Identification and isolation of CSCs via FACS or MACS | Enables purification of CSC subpopulations for functional studies | [1] [4] [8] |
| Intracellular Marker Detection | ALDEFLUOR Assay, Anti-ALDH1 | Detection of aldehyde dehydrogenase activity | Identifies CSCs with enhanced detoxification capabilities | [5] [4] |
| Signaling Pathway Inhibitors | DKK1 (Wnt inhibitor), GANT61 (HH inhibitor), DAPT (Notch inhibitor) | Functional perturbation of stemness pathways | Determines pathway necessity for hallmark maintenance | [5] |
| Lineage Tracing Systems | Cre-lox, Fluorescent reporters (GFP, RFP) | Fate mapping of CSCs and their progeny | Tracks differentiation outcomes and cellular heterogeneity | [2] [3] |
| Cytokines & Growth Factors | TGF-β, EGF, bFGF, HGF | Modulation of CSC plasticity and EMT | Induces or maintains stem-like states in culture | [5] [3] |
The following workflow diagram illustrates a typical integrated experimental approach for characterizing CSC hallmarks:
CSC Hallmarks in Tumor Heterogeneity and Therapy Resistance
Generating and Sustaining Tumor Heterogeneity
The dual capabilities of self-renewal and differentiation enable CSCs to generate and maintain the complex cellular heterogeneity characteristic of malignant tumors [3]. Through asymmetric division, a single CSC can produce both an identical daughter stem cell and a progenitor cell committed to differentiation, thereby establishing a cellular hierarchy within the tumor [2] [3]. This hierarchy results in intratumoral heterogeneity—variations observed within a single tumor—including diverse cell surface markers, genetic and epigenetic changes, growth rates, and metastatic potential among different subpopulations [3]. Recent spatial transcriptomics studies have further revealed that this heterogeneity is spatially organized, with distinct regions of tumors exhibiting different hallmark activities and molecular profiles [9].
The plasticity of CSCs significantly amplifies this heterogeneity. Non-stem cancer cells can regain stemness characteristics through dedifferentiation processes, often induced by microenvironmental cues such as hypoxia, inflammation, or therapeutic pressure [1] [3]. Key transcription factors including OCT3/4, SOX2, NANOG, and KLF4 are frequently overexpressed in CSCs and contribute to this plasticity by maintaining pluripotency networks [8]. This dynamic interconversion between stem and non-stem states creates a continuous source of cellular diversity that complicates therapeutic targeting and promotes tumor adaptation.
Mechanisms of Therapy Resistance
CSCs employ multiple mechanisms to resist conventional cancer therapies, largely rooted in their defining hallmarks:
Quiescence and Dormancy: Many CSCs reside in a quiescent, non-dividing state (G0 phase), making them insensitive to therapies that target rapidly proliferating cells [5]. This dormancy provides time for DNA repair and survival under therapeutic stress [5] [4]. Strategies to "wake up" CSCs, such as Fbxw7 ablation or PPAR-γ agonism, have shown promise in sensitizing them to subsequent treatment [5].
Enhanced DNA Repair Capacity: CSCs exhibit heightened DNA damage response mechanisms, including constitutive activation of checkpoint pathways, enabling efficient repair of therapy-induced DNA lesions [5]. This is particularly relevant for radiotherapy and DNA-damaging chemotherapeutics.
Drug Efflux Transporters: High expression of ATP-binding cassette (ABC) transporters such as ABCB5 and ABCG2 allows CSCs to actively expel chemotherapeutic agents, conferring multidrug resistance [5] [7] [4].
Epithelial-Mesenchymal Transition (EMT): The EMT program, closely associated with CSC states, promotes therapy resistance through multiple mechanisms including induction of quiescence, upregulation of survival pathways, and enhanced interaction with protective microenvironments [5].
Metabolic Adaptations: The metabolic plasticity of CSCs enables them to switch between energy production pathways to survive under diverse conditions, including hypoxic regions of tumors that are poorly penetrated by therapeutics [1] [7].
The defining hallmarks of CSCs—self-renewal, differentiation, and tumorigenic potential—establish these cells as central drivers of tumor heterogeneity, progression, and therapeutic resistance. Understanding the molecular underpinnings of these capabilities provides critical insights for developing more effective cancer treatments. Current research is increasingly focused on targeting the unique vulnerabilities of CSCs, including their signaling dependencies, metabolic adaptations, and interactions with the tumor microenvironment [1] [2].
Emerging therapeutic approaches include dual metabolic inhibition to overcome metabolic plasticity, synthetic biology-based interventions, immune-based strategies such as CSC-targeted CAR-T cells, and nanotechnology-enabled drug delivery systems designed to specifically target CSCs [1] [10]. The integration of single-cell multi-omics, spatial transcriptomics, and AI-driven analysis holds promise for unraveling the complexity of CSC biology and identifying novel therapeutic targets [1] [9]. As these advanced technologies and targeted strategies mature, they offer the potential to overcome CSC-mediated therapy resistance and significantly improve outcomes for cancer patients.
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [1]. These cells demonstrate capacities for self-renewal, differentiation, and tumor initiation, contributing significantly to intratumoral heterogeneity and treatment failure [11] [1]. The identification and characterization of CSCs rely heavily on specific cellular biomarkers, which serve not only as identification tools but also as potential therapeutic targets. Among the most extensively studied CSC markers are the surface proteins CD44, CD133, ALDH1, and EpCAM, each playing distinct roles in CSC biology across various cancer types [11] [1].
The clinical significance of CSC biomarkers extends beyond basic identification, offering potential prognostic value and insights into therapy resistance mechanisms. However, a major challenge in the field is the lack of universal CSC markers, as their expression and functional significance vary considerably across different tumor types and even within subtypes of the same cancer [1]. This variability reflects the profound influence of tissue origin and microenvironmental context on CSC phenotypes, necessitating a nuanced understanding of each marker's specific roles and interactions.
Marker Profiles and Biological Functions
Individual Marker Characteristics
CD44: A cell surface glycoprotein receptor for hyaluronic acid, CD44 is strongly involved in cancer cell adhesion, migration, and metastasis [12]. It has been used to identify putative CSCs in various tumor types including breast, prostate, pancreatic, and head and neck carcinomas [12]. CD44 positive populations often demonstrate more robust colony formation, higher proliferation, less spontaneous apoptosis, and higher resistance to drug-induced cell death [13].
CD133 (Prominin-1): A transmembrane glycoprotein that localizes to cellular protrusions, CD133 was one of the first CSC markers identified in various solid tumors [14]. Its expression alone may not always define the CSC population, as in some colorectal cancers where CD133 expression is detectable in a large majority of tumor cells irrespective of their tumorigenicity [14]. However, in lung adenocarcinoma, CD133 expression specifically correlates with poorer overall survival and shorter disease-free interval [15].
ALDH1 (Aldehyde Dehydrogenase 1): This cytosolic enzyme plays a key role in oxidizing intracellular aldehydes and converting retinol to retinoic acid in early stem cell differentiation [12]. ALDH1 activity serves as a functional marker for stem-like properties, with ALDH1-bright cells demonstrating enhanced drug resistance and tumorigenic potential in ovarian cancer models [16]. In oral cancer, ALDH1 expression increases with dysplasia progression, suggesting its utility as a specific marker for malignant transformation [12].
EpCAM (Epithelial Cell Adhesion Molecule): A transmembrane glycoprotein that mediates homotypic calcium-independent cell adhesion in epithelia [14]. Interestingly, in colorectal cancer, loss rather than overexpression of membranous EpCAM is linked to tumor progression, supporting the notion that membranous evaluation may represent cell adhesion functions rather than intracellular signaling [14].
Table 1: Core CSC Biomarkers and Their Functional Roles
| Biomarker | Type | Primary Localization | Key Functions | Associated Cancers |
|---|---|---|---|---|
| CD44 | Surface glycoprotein | Cell membrane | Cell adhesion, migration, metastasis, drug resistance | Breast, ovarian, colorectal, HNSCC |
| CD133 | Transmembrane glycoprotein | Cellular protrusions | Maintenance of stem cell properties, potential interaction with membrane lipids | Lung, colorectal, glioblastoma |
| ALDH1 | Metabolic enzyme | Cytoplasm | Detoxification, retinoic acid production, chemoresistance | Ovarian, lung, oral, HNSCC |
| EpCAM | Cell adhesion molecule | Cell membrane | Homotypic cell adhesion, intracellular signaling | Colorectal, pancreatic, breast |
Combinatorial Marker Profiles
Research increasingly indicates that combinatorial marker profiles rather than single markers better define CSC populations across different cancer types. The specific combinations vary significantly between tissues and cancer types:
In colorectal cancer, the CD44+CD133- subpopulation in SW620 cells correlates with most CSC features, including enhanced migration and invasion capabilities [13]. This profile aligns with CSC phenotypes in other tumors such as CD44+CD24- for breast and pancreatic tumors and CD34+CD38- for acute myeloid leukemia [13].
In ovarian cancer, ALDH1-bright cells are associated with CD44 expression, with ALDH1br cells showing greater enrichment in CD44 (by 1.74-fold to 5.18-fold) than in CD133 (by 1.39-fold to 1.17-fold) compared with ALDH1low cells [16]. This co-expression pattern underscores the potential synergy between different CSC markers in defining the most tumorigenic cell populations.
Table 2: Clinically Significant CSC Marker Combinations in Different Cancers
| Cancer Type | Marker Combination | Clinical/Prognostic Association |
|---|---|---|
| Colorectal Cancer | CD44+CD133- | Enhanced migration, invasion, and colony formation [13] |
| Lung Adenocarcinoma | ALDH1A1+/CD133+ | Poor overall survival and shorter disease-free interval [15] |
| Ovarian Cancer | ALDH1br/CD44+ | Drug resistance, poor clinical outcome [16] |
| Oral Squamous Cell Carcinoma | ALDH1+/CD44+ | Association with dysplasia and lymph node metastasis [12] |
| Acute Myeloid Leukemia | CD34+CD38- | Leukemia-initiating potential [1] |
Methodologies for CSC Marker Analysis
Immunohistochemical Analysis
Immunohistochemistry (IHC) represents a cornerstone technique for evaluating CSC marker expression in formalin-fixed, paraffin-embedded tissue sections, allowing for correlation with clinicopathological parameters. The methodology involves several critical steps:
- Tissue Preparation: Sections of 3-4μm thickness are mounted on slides, deparaffinized in xylene, and rehydrated through a graded alcohol series [12] [15].
- Antigen Retrieval: Heat-induced epitope retrieval is performed using citrate buffer (pH 6.0) at 121°C for 30 minutes under pressure [12].
- Antibody Incubation: Primary antibodies are applied with specific concentrations: anti-CD44 (clone DF1485, ready-to-use) [12], anti-CD133 (clone C24B9; 1:100) [14], anti-ALDH1 (polyclonal; 1:500) [14], and anti-EpCAM (clone VU-1D9; 1:200) [14].
- Detection and Visualization: Following secondary antibody application, 3,3'-diaminobenzidine-tetrahydrochloride (DAB) is used as a chromogen, followed by counterstaining with Mayer's hematoxylin [12].
Scoring methodologies vary by marker localization pattern. For CD133, CD166, CD44s, and EpCAM, membranous staining is evaluated, while for ALDH1, cytoplasmic immunoreactivity is assessed [14]. Scoring typically involves semi-quantitative assessment of the percentage of positive tumor cells, often using cutoff values determined by receiver-operating characteristic (ROC) curve analysis for prognostic studies [14].
Flow Cytometry and Cell Sorting
Fluorescence-Activated Cell Sorting (FACS) enables isolation of live CSC subpopulations for functional characterization, using the following standard protocol:
- Cell Preparation: Single-cell suspensions are obtained from cell lines or dissociated tumor tissues [13].
- Antibody Staining: Cells are incubated with fluorochrome-conjugated antibodies against CSC markers (e.g., PE-conjugated anti-CD133, FITC-conjugated anti-CD44) for 1 hour at 4°C in the dark [13].
- Viability Staining: Propidium iodide (1μg/ml) is added to exclude dead cells during sorting [13].
- Cell Sorting: Subpopulations are isolated based on marker expression profiles (e.g., CD133+CD44+, CD133+CD44-, CD133-CD44+, and CD133-CD44-) using a flow cytometer [13].
- Functional Assays: Sorted populations are subsequently subjected to colony formation, drug resistance, migration, and invasion assays [13].
The Aldefluor assay provides a functional approach to identify cells with high ALDH enzymatic activity [16]. This assay utilizes a fluorescent substrate that is converted and retained in cells with high ALDH activity, allowing isolation of ALDH1-bright populations that demonstrate stem-like properties.
Figure 1: Experimental Workflow for CSC Marker Analysis and Functional Validation
Research Reagent Solutions
Table 3: Essential Research Reagents for CSC Marker Studies
| Reagent/Category | Specific Examples | Application Purpose | Technical Notes |
|---|---|---|---|
| Primary Antibodies | Anti-CD44 (clone DF1485) [12], Anti-CD133 (clone C24B9) [14], Anti-ALDH1 (polyclonal) [14], Anti-EpCAM (clone VU-1D9) [14] | IHC, Western blot, flow cytometry | Validate for specific applications; concentrations vary (e.g., 1:50-1:500 for IHC) |
| Fluorochrome-Conjugated Antibodies | PE-conjugated anti-CD133, FITC-conjugated anti-CD44, eFluor 660-conjugated anti-ESA [13] | Flow cytometry, FACS | Include isotypic controls and unstained cells as negative controls |
| Cell Separation Tools | Fluorescence-Activated Cell Sorter (FACS) [13], Aldefluor Assay Kit [16] | Isolation of live CSC subpopulations | Purity of sorted cells should be ≥97%; include viability staining (PI or DAPI) |
| Cell Culture Assays | CyQuant cell proliferation assay [13], Caspase-Glo assay [13], BD BioCoat Tumor Invasion System [13] | Functional characterization of CSCs | Serum-free medium for invasion assays; matrigel-coated membranes |
| Cell Lines | SW620, Colo205, LS180 (colorectal) [13] [14]; ES-2, TOV-21G, CP70 (ovarian) [16] | In vitro CSC studies | Authenticate cell lines regularly; check marker expression profiles |
Clinical Implications and Therapeutic Applications
Prognostic Significance
CSC marker expression demonstrates significant correlations with clinical outcomes across various malignancies, although these relationships can be complex and context-dependent:
In ovarian cancer, patients with higher ALDH1 expression (>50% positive cells) demonstrate significantly poorer overall survival compared with those with lower ALDH1 expression, with multivariate analysis yielding an odds ratio of death of 2.43 [16]. This association between ALDH1 and poor outcome underscores its potential utility as a prognostic biomarker.
In lung adenocarcinoma, CD133 expression specifically correlates with poorer overall survival and shorter disease-free interval, with multivariate analysis revealing that double negativity for ALDH1A1 and CD133 is independently associated with increased survival and longer disease-free interval [15].
Unexpectedly, in colorectal cancer, loss rather than overexpression of membranous CD44s and CD166 is associated with higher pT and pN stages, infiltrating growth pattern, and worse survival [14]. This paradoxical finding highlights the importance of considering the specific cellular localization and function of these markers, as membranous evaluation may primarily reflect cell adhesion functions rather than intracellular signaling roles.
Role in Drug Resistance
CSCs contribute significantly to therapy resistance through multiple interconnected mechanisms, making their marker profiles potentially valuable for predicting treatment response:
Chemoresistance: ALDH1-bright ovarian cancer cells demonstrate significant resistance to conventional chemotherapeutic agents, with ALDH1br cells maintaining viability after drug exposure that eliminates the majority of tumor cells [16]. Similarly, CD44 positive cells in colorectal cancer show higher resistance to drug-induced cell death and become enriched after drug treatment [13].
Radiation Resistance: CSCs generally exhibit enhanced DNA repair capacity and resistance to radiation-induced apoptosis, contributing to tumor recurrence after radiotherapy [1].
Multidrug Resistance Phenotypes: CSCs frequently overexpress ATP-binding cassette (ABC) transporters that efflux chemotherapeutic drugs, along with enhanced detoxification systems including ALDH1 activity [1] [17].
Figure 2: CSC-Associated Therapy Resistance Mechanisms Leading to Recurrence
Emerging Research and Future Directions
The landscape of CSC research continues to evolve with emerging technologies enabling more precise characterization of these critical cell populations. Single-cell sequencing and spatial transcriptomics are significantly advancing our understanding of CSC heterogeneity and plasticity, revealing how stem-like features can be acquired de novo by non-CSCs in response to environmental stimuli [1]. These findings challenge the notion of a fixed CSC hierarchy and highlight CSC phenotypes as dynamic functional states influenced by microenvironmental cues.
The development of 3D organoid models and CRISPR-based functional screens is paving the way for more physiologically relevant studies of CSC biology and drug resistance mechanisms [1]. These platforms enable more accurate modeling of tumor heterogeneity and microenvironmental interactions, potentially leading to more effective therapeutic strategies.
Emerging therapeutic approaches focus on targeting CSC vulnerabilities through dual metabolic inhibition, synthetic biology-based interventions, and immune-based strategies [1]. The integration of CSC biomarkers with artificial intelligence-driven multiomics analysis holds promise for developing personalized treatment approaches that effectively target both the bulk tumor and therapy-resistant CSC populations [1].
As research progresses, the combinatorial analysis of multiple CSC markers within specific tumor contexts will be essential for developing more effective prognostic tools and therapeutic strategies. The future of CSC-targeted therapy likely lies in integrated approaches that simultaneously address multiple resistance mechanisms while accounting for the dynamic plasticity of CSC populations within diverse tumor microenvironments.
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with capabilities for self-renewal, differentiation, and tumor initiation, driving intra-tumoral heterogeneity, therapeutic resistance, and cancer recurrence. The functional properties of CSCs are governed by an intricate network of conserved signaling pathways. This technical review examines the core regulatory circuits of Wnt/β-catenin, Hedgehog (Hh), Notch, and Hippo/YAP signaling, detailing their mechanisms, crosstalk, and roles in maintaining CSC functionality. The document provides structured quantitative data, experimental methodologies, and visualization tools to support research and therapeutic development efforts aimed at overcoming CSC-mediated drug resistance. Framed within the broader context of CSC biology, this resource equips scientists with foundational knowledge and practical references for targeting these pathways in precision oncology.
Cancer stem cells (CSCs) are a functionally distinct subpopulation within tumors that possess stem cell-like properties, including self-renewal, differentiation capacity, and tumor-initiating potential [18] [2]. First identified in acute myeloid leukemia and subsequently isolated in various solid tumors, CSCs contribute significantly to tumor heterogeneity, metastatic dissemination, and resistance to conventional therapies [18] [19]. Their ability to persist after treatment and drive recurrence underscores their clinical importance in oncology research and drug development.
The molecular identity and maintenance of CSCs are regulated by key developmental signaling pathways that are often dysregulated in cancer. The Wnt/β-catenin, Hedgehog, Notch, and Hippo/YAP pathways represent core regulatory systems that control CSC self-renewal, metabolic adaptation, and interactions with the tumor microenvironment [18] [20] [21]. These pathways exhibit extensive crosstalk, forming an integrated network that maintains CSC plasticity and survival under therapeutic stress [22] [19]. This review systematically examines each pathway's architecture, regulatory mechanisms, and experimental approaches for their investigation, with particular emphasis on their collective role in sustaining CSC functionality and promoting treatment resistance.
Pathway Mechanisms and Dysregulation in Cancer
Wnt/β-Catenin Signaling Pathway
The Wnt/β-catenin pathway is a highly conserved system regulating cell fate determination, tissue homeostasis, and stem cell maintenance. In the canonical pathway, binding of Wnt ligands to Frizzled receptors and LRP co-receptors inhibits the destruction complex (APC, Axin, GSK-3β, CK1α), preventing β-catenin phosphorylation and degradation [18] [20]. Stabilized β-catenin accumulates and translocates to the nucleus, where it partners with TCF/LEF transcription factors to activate target genes including c-MYC, CYCLIN D1, and CD44 that promote self-renewal and proliferation [18] [21].
In CSCs, Wnt/β-catenin signaling is frequently hyperactivated, enhancing CSC self-renewal and therapeutic resistance [18] [23]. The pathway exhibits crosstalk with Hippo/YAP signaling, where YAP/TAZ can interact with β-catenin to reinforce transcriptional programs supporting stemness [22] [21]. Dysregulation occurs through multiple mechanisms, including mutations in pathway components (APC, β-catenin), autocrine Wnt signaling, and Wnt production from tumor-associated stromal cells [18].
Table 1: Core Components of Wnt/β-catenin Signaling Pathway
| Component Type | Key Elements | Functional Role in Pathway | Cancer Associations |
|---|---|---|---|
| Ligands/Receptors | Wnt ligands, Frizzled, LRP5/6 | Signal initiation and receptor complex formation | Overexpression in colorectal, breast cancer |
| Destruction Complex | APC, Axin, GSK-3β, CK1α | β-catenin phosphorylation and degradation | APC mutations in colorectal cancer |
| Effectors | β-catenin, TCF/LEF | Transcriptional activation of target genes | β-catenin mutations in hepatocellular carcinoma |
| Target Genes | c-MYC, CYCLIN D1, CD44, AXIN2 | Regulation of cell cycle, stemness, metastasis | Elevated in various CSCs |
| Regulatory Proteins | DKK, SFRP | Natural pathway inhibitors | Epigenetic silencing in cancers |
Hedgehog Signaling Pathway
The Hedgehog (Hh) pathway is crucial for embryonic patterning, tissue repair, and stem cell maintenance. In the canonical pathway, Hh ligand binding to Patched (PTCH1) relieves its inhibition of Smoothened (SMO), leading to activation of GLI transcription factors (GLI1, GLI2, GLI3) that regulate target genes including BCL-2, CYCLIN D, and MYC [20]. In CSCs, Hh signaling promotes self-renewal, survival, and metabolic adaptations that support therapy resistance [18] [20].
Hh pathway dysregulation in cancer occurs through ligand-dependent mechanisms (paracrine signaling from tumor microenvironment) or ligand-independent mechanisms (mutations in PTCH1, SMO, SUFU) [20]. The pathway demonstrates significant crosstalk with Hippo/YAP signaling; for instance, in pancreatic ductal adenocarcinoma, microRNA-301a mediates interplay between Hh and Hippo pathways to promote progression [22].
Notch Signaling Pathway
Notch signaling mediates cell-cell communication and fate determination through proteolytic cleavage events. Canonical activation involves Delta/Serrate/LAG-2 (DSL) ligand binding, followed by γ-secretase-mediated cleavage of Notch receptors, releasing the Notch intracellular domain (NICD) that translocates to the nucleus and partners with CSL transcription factors to activate target genes including HES, HEY, and MYC [18] [20].
In CSCs, Notch signaling maintains the undifferentiated state and promotes survival through regulation of apoptosis inhibitors and EMT transcription factors [18] [23]. The pathway exhibits contextual oncogenic or tumor-suppressive functions depending on tissue type and cellular context. Notch crosstalk with Hippo/YAP occurs through multiple mechanisms, including YAP/TAZ enhancement of NOTCH receptor expression and collaborative regulation of shared target genes [22].
Hippo/YAP Signaling Pathway
The Hippo/YAP pathway is an evolutionarily conserved kinase cascade that controls organ size, cell proliferation, and stem cell function. In the canonical pathway, upstream signals activate MST1/2 kinases, which phosphorylate LATS1/2, leading to phosphorylation and cytoplasmic retention or degradation of YAP/TAZ effectors [22] [24]. When the pathway is inactive, unphosphorylated YAP/TAZ translocate to the nucleus and partner with TEAD transcription factors to activate target genes including CTGF, CYR61, and BIRC5 that promote cell growth and survival [22] [24].
In CSCs, Hippo/YAP signaling enhances self-renewal, metabolic reprogramming, and therapy resistance. YAP/TAZ activity supports CSC maintenance through regulation of glutamine metabolism and interaction with key stemness transcription factors [22]. The pathway exhibits extensive crosstalk, integrating with Wnt, TGF-β, NF-κB, and Hedgehog signaling to form a complex regulatory network that influences CSC plasticity and tumorigenicity [22] [21].
Table 2: Pathway Crosstalk in Cancer Stem Cell Regulation
| Signaling Pathway | Crosstalk Mechanisms | Functional Consequences in CSCs | Therapeutic Implications |
|---|---|---|---|
| Hippo-YAP & Wnt | YAP/TAZ interact with β-catenin/DVL; shared target gene regulation | Enhanced self-renewal, EMT promotion, metabolic reprogramming | Combined YAP/β-catenin inhibition strategies |
| Hippo-YAP & TGF-β | SMAD-TEAD complexes; YAP-TGF-β synergy in EMT | Stemness maintenance, immune evasion, metastasis | Dual SMAD/YAP targeting in metastatic disease |
| Hippo-YAP & Hedgehog | microRNA-mediated crosstalk (e.g., miR-301a); GLI-YAP interactions | Pancreatic cancer progression, therapy resistance | Combinatorial SMO/YAP inhibitors |
| Hippo-YAP & Notch | YAP enhancement of NOTCH receptor expression; TEAD-NOTCH collaboration | Regulation of stem cell fate decisions, differentiation control | Context-dependent combination therapies |
| Hippo-YAP & NF-κB | YAP as NF-κB co-activator; inflammatory gene regulation | Osteoclastogenesis, immune modulation, bone metastasis | YAP/NF-κB targeting in inflammatory cancers |
Experimental Approaches for Pathway Analysis
Core Methodologies for Signaling Pathway Investigation
Investigation of CSC signaling pathways requires integrated experimental approaches spanning molecular, cellular, and functional assays. Gene expression profiling using RNA-seq and single-cell RNA-seq enables comprehensive analysis of pathway activity states and heterogeneity within CSC populations [1] [2]. Protein localization and quantification through immunohistochemistry, western blotting, and flow cytometry provide critical data on pathway activation status, particularly for YAP/TAZ nuclear translocation and β-catenin accumulation [24].
Functional pathway analysis employs reporter assays (TOPFlash for Wnt, GLI-luciferase for Hh, TEAD-luciferase for Hippo) to quantify transcriptional activity [24]. CRISPR-based functional screens enable systematic identification of essential pathway components and regulators in specific CSC contexts [1] [18]. Additionally, 3D organoid cultures and patient-derived xenograft models provide physiologically relevant systems for evaluating pathway functions in CSC maintenance and therapeutic response [1] [2].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Pathway Analysis
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Pathway Reporters | TOPFlash (Wnt), GLI-luciferase (Hh), TEAD-luciferase (Hippo), CBF1-luciferase (Notch) | Quantitative pathway activity measurement | Normalize to control reporters; context-dependent specificity |
| Small Molecule Inhibitors | IWR/IWP (Wnt), GANT61 (Hh), DAPT (Notch), Verteporfin (YAP) | Pathway inhibition and functional validation | Assess specificity and off-target effects |
| Activation Compounds | CHIR99021 (Wnt), SAG (Hh), Recombinant DLL/JAG (Notch) | Experimental pathway stimulation | Concentration optimization critical |
| Antibodies | Anti-β-catenin, anti-YAP/TAZ, anti-GLI1, anti-NICD | Protein localization and quantification | Phospho-specific antibodies for activation status |
| CRISPR Tools | sgRNA libraries, Cas9 variants, base editors | Functional genetic screening | Use multiple sgRNAs per gene to confirm findings |
Therapeutic Targeting and Clinical Implications
The strategic targeting of CSC signaling pathways represents a promising approach to overcome therapy resistance and prevent tumor recurrence. Current therapeutic development focuses on several key strategies: small molecule inhibitors targeting critical pathway nodes (SMO in Hh, γ-secretase in Notch, TEAD-YAP interaction in Hippo) [22] [24] [20]; monoclonal antibodies against pathway ligands and receptors; natural compounds with multi-pathway activity; and combination approaches that target complementary pathways or combine pathway inhibition with conventional therapies [24] [23].
Clinical challenges in targeting CSC pathways include pathway crosstalk and compensatory activation, tissue-specific toxicities due to pathway roles in normal stem cell maintenance, and the dynamic plasticity of CSCs that enables adaptation to targeted therapies [1] [18]. Emerging solutions incorporate pharmacological modulation of multiple pathways, biomarker-driven patient stratification, and nanotechnology-based delivery systems to enhance specificity and reduce toxicity [2] [20]. The integration of AI-driven multiomics analysis and advanced disease modeling continues to refine therapeutic targeting strategies for improved clinical outcomes [1] [18].
The Wnt/β-catenin, Hedgehog, Notch, and Hippo/YAP signaling pathways constitute fundamental regulatory networks that maintain CSC populations and drive tumor heterogeneity, therapy resistance, and metastatic progression. Understanding the intricate mechanisms, contextual functions, and extensive crosstalk among these pathways provides critical insights for developing targeted therapeutic interventions. Future research directions should emphasize multi-pathway targeting approaches, advanced modeling of CSC-TME interactions, and translational strategies that leverage emerging technologies in single-cell analysis, computational modeling, and precision drug delivery. By dismantling the signaling foundations that sustain CSCs, the oncology research community can advance toward more effective and durable cancer treatments.
The cancer stem cell (CSC) paradigm has fundamentally transformed our understanding of tumorigenesis, progression, and therapeutic resistance. Historically, CSCs were viewed as a static hierarchical compartment situated at the apex of a rigid cellular organization within tumors. However, emerging evidence has dramatically reshaped this concept, revealing that CSCs exist in a state of dynamic equilibrium with their non-stem cancer cell (NSCC) counterparts [25] [26]. This continuous, bidirectional interconversion between CSC and NSCC states—termed cancer stem cell plasticity—represents a critical adaptive mechanism that fuels tumor heterogeneity, enables metastatic dissemination, and undermines conventional therapies [2] [4].
The plasticity paradigm posits that stemness is not a fixed cellular attribute but rather a transient, context-dependent state that can be acquired or relinquished based on cell-intrinsic signals and microenvironmental cues [25]. This fluidity complicates therapeutic targeting of CSCs and provides tumors with a resilient reservoir for regeneration following treatment. This review examines the molecular drivers, regulatory mechanisms, and functional implications of CSC-NSCC interconversion, framing this plasticity within the broader context of tumor heterogeneity and drug resistance research.
Molecular Mechanisms Governing Plasticity
Key Signaling Pathways and Transcriptional Networks
The dynamic interconversion between CSCs and NSCCs is orchestrated by complex signaling networks and transcriptional programs that respond to both intrinsic and extrinsic cues.
Table 1: Core Signaling Pathways Regulating CSC Plasticity
| Pathway | Key Components | Role in Plasticity | Therapeutic Implications |
|---|---|---|---|
| Wnt/β-catenin | Frizzled receptors, β-catenin, GSK-3, APC | Enhances self-renewal; maintains stemness; stabilizes telomeres via TERT [5] | Wnt inhibitors in development; challenges with on-target toxicity |
| Hedgehog | Smoothened, GLI transcription factors | Induces EMT; promotes therapy resistance; regulates cell survival [5] | Smoothened inhibitors (e.g., vismodegib) show efficacy in basal cell carcinoma |
| Notch | Notch 1-4 receptors, DLL/Jagged ligands | Maintains stemness through cell-cell communication; influences cell fate decisions [5] | Notch signaling inhibitors being evaluated in clinical trials |
| TGF-β | TGF-β ligands, SMAD proteins | Primary inducer of EMT; accelerates CSC-NSCC equilibrium [27] | TGF-β inhibitors can disturb plasticity equilibrium |
| Hippo/YAP1 | YAP1, TAZ, MST1/2, LATS1/2 | Regulates stem cell maintenance; confers therapy resistance; nuclear YAP1 associated with poor prognosis [4] | YAP1 inhibition restores drug sensitivity in resistant models |
The epithelial-mesenchymal transition (EMT) program serves as a master regulator of CSC plasticity, enabling epithelial cells to acquire mesenchymal traits including enhanced motility, invasiveness, and stem-like properties [28]. EMT is not a binary process but rather a spectrum of intermediate states, with hybrid epithelial/mesenchymal (E/M) phenotypes often exhibiting the highest stemness potential [29]. This plasticity is maintained by double-negative feedback loops, such as the Snail/miR-34 and Zeb/miR-200 circuits, which create toggle switches enabling reversible phenotypic transitions [28].
Epigenetic Regulation and Metabolic Adaptations
Epigenetic mechanisms serve as crucial mediators of CSC plasticity, allowing rapid phenotypic switching without permanent genetic alterations. DNA methylation, histone modifications, and chromatin remodeling enable dynamic reprogramming of gene expression patterns in response to therapeutic stress or microenvironmental changes [25] [2]. Additionally, CSCs exhibit metabolic plasticity, shifting between oxidative phosphorylation, glycolysis, and fatty acid oxidation to meet energy demands and mitigate oxidative stress under various conditions [2]. This metabolic flexibility supports survival during therapeutic challenges and facilitates transitions between stem and non-stem states.
Figure 1: Molecular Network Regulating CSC Plasticity. Multiple signaling pathways converge on EMT transcription factors and epigenetic regulators to enable bidirectional interconversion between cellular states.
Experimental Evidence and Methodological Approaches
Key Studies Demonstrating Dynamic Interconversion
Seminal research has provided compelling evidence for the spontaneous interconversion between CSCs and NSCCs across multiple cancer types:
Colon and Breast Cancer Models: SW620 colon cancer and MCF-7 breast cancer cells maintain constant CSC proportions over multiple generations despite sorting for CSC and NSCC populations, indicating continuous repopulation through bidirectional conversion [27]. This equilibrium is maintained irrespective of prior radiation exposure, demonstrating the resilience of plasticity mechanisms.
Glioblastoma Plasticity: CSC markers (CD133, A2B5, SSEA, CD15) do not represent clonal entities but rather plastic states that can be adapted by most cells in response to microenvironmental conditions [26]. This dynamic state enables rapid adaptation to therapeutic pressures.
Melanoma Phenotypic Switching: JARID1B-positive melanoma CSCs and JARID1B-negative cells undergo reversible phenotypic changes, with negative cells capable of re-expressing the marker and regenerating tumor heterogeneity [26].
Colorectal Cancer Lineage Tracing: Targeted ablation of Lgr5+ CSCs does not lead to tumor regression because Lgr5− cells can regenerate the Lgr5+ population, demonstrating the reversible nature of the stem cell state [26] [30].
Table 2: Quantitative Evidence for CSC-NSCC Interconversion
| Cancer Type | Experimental System | CSC Markers | Key Finding | Reference |
|---|---|---|---|---|
| Colon Cancer | SW620 cell line | CD133 | Spontaneous reconstitution of both CSC and NSCC populations from purified fractions within days | [27] |
| Breast Cancer | MCF-7 cell line | CD44+/CD24− | Dynamic equilibrium maintained between cellular states across multiple generations | [27] |
| Glioblastoma | Patient-derived samples | CD133, A2B5, SSEA | Marker expression represents plastic states adaptable by most cells | [26] |
| Colorectal Cancer | Lineage tracing in vivo | LGR5 | LGR5− cells regenerate LGR5+ CSCs following ablation | [30] |
| Breast Cancer | Basal-like subtype | ZEB1 | Non-stem cells spontaneously convert to stem-like state regulated by ZEB1 | [26] |
Methodological Framework for Studying Plasticity
Cell Sorting and Functional Validation
Fluorescence-Activated Cell Sorting (FACS) enables isolation of CSC and NSCC populations based on specific surface markers:
- Protocol: Cells are stained with fluorescently conjugated antibodies against CSC markers (e.g., CD133-APC, CD44-PE, CD24-Alex488) at concentrations of 10^7 cells per 100μl buffer. After incubation, cells are sorted using instruments such as BD FACS Aria II, with analysis on BD LSR II flow cytometers [27].
- Validation: Sorted populations must be functionally validated through sphere formation assays, in vivo limiting dilution transplantation, and Aldefluor assays to confirm stemness properties [5].
Lineage Tracing and Clonal Analysis
Genetic lineage tracing provides the most compelling evidence for plasticity by tracking the fate of individual cells and their progeny:
- Approach: Introduction of heritable genetic markers (e.g., Cre-recombinase systems, fluorescent reporters) under control of CSC-specific promoters (e.g., LGR5) enables visualization of lineage relationships over time [30].
- Application: In colorectal cancer models, this approach demonstrated that LGR5− cells can give rise to LGR5+ CSCs, confirming bidirectional interconversion [30].
Single-Cell Analysis and Mathematical Modeling
Single-cell RNA sequencing reveals transcriptional states along the epithelial-mesenchymal spectrum and identifies intermediate hybrid states [2] [29]. Mathematical modeling approaches, including ordinary differential equation (ODE)-based models and Boolean networks, help conceptualize the dynamics of CSC-NSCC interconversion and predict cellular behaviors under different conditions [29].
Figure 2: Experimental Workflow for CSC Plasticity. Process from tumor dissociation to functional validation demonstrates bidirectional conversion.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for CSC Plasticity Studies
| Reagent/Category | Specific Examples | Application/Function | Experimental Notes |
|---|---|---|---|
| CSC Surface Markers | Anti-CD133, Anti-CD44, Anti-CD24, Anti-ALDH1 | Identification and isolation of CSC populations | CD133 controversial in glioblastoma; ALDH1 activity via Aldefluor assay [4] |
| Signaling Inhibitors | SB431542 (TGF-β inhibitor), DAPT (Notch inhibitor), Cyclopamine (Hedgehog inhibitor) | Perturb signaling pathways to test plasticity regulation | SB431542 significantly decreases CSC proportion in equilibrium models [27] |
| Cytokines/Growth Factors | Recombinant TGF-β1 | Induce EMT and promote stemness | 0.4 ng/ml TGF-β1 accelerates CSC-NSCC equilibrium [27] |
| Cell Tracking Dyes | Hoechst 33342, CFSE, Photo-convertible proteins | Lineage tracing and proliferation monitoring | Hoechst 33342 for DNA staining in microfluidic devices [27] |
| 3D Culture Matrices | Matrigel, Collagen, Organoid media | Maintain tumor architecture and niche interactions | Patient-derived organoids preserve cellular heterogeneity [30] |
| Drug Selection Agents | Cisplatin, 5-FU, Targeted inhibitors | Apply selective pressure to study plasticity in resistance | Low-dose platinum induces ABCG2 upregulation and CD133+ expansion [4] |
Therapeutic Implications and Future Perspectives
The dynamic interconversion between CSCs and NSCCs represents a fundamental challenge in cancer therapeutics, as conventional treatments that eliminate rapidly dividing cells may enrich for CSCs through selective pressure and plasticity mechanisms [5] [4]. Several strategic approaches emerge from understanding this plasticity:
Targeting Plasticity Mechanisms
Rather than attempting to eliminate CSCs permanently—a challenging goal due to continuous repopulation from NSCCs—therapeutic efforts are shifting toward targeting the plasticity process itself. Potential strategies include:
- Locking cells in differentiated states: Forcing CSCs to adopt NSCC phenotypes without regenerative capacity [26].
- Preventing adaptive plasticity: Inhibiting molecular switches that enable transition to treatment-resistant states [28].
- Dual-targeting approaches: Simultaneously targeting both CSCs and NSCCs to prevent repopulation from either compartment [4].
Clinical Translation Challenges
The development of CSC plasticity-targeting therapies faces several obstacles:
- Toxicity concerns: Key plasticity pathways (Wnt, Notch, Hedgehog) play crucial roles in normal tissue homeostasis [5].
- Biomarker limitations: Current CSC markers insufficiently capture the dynamic nature of stemness states [25] [2].
- Microenvironmental influence: Niche-specific factors significantly modulate plasticity, creating context-dependent therapeutic responses [2] [30].
Future Research Directions
Advancing our ability to therapeutically target CSC plasticity requires:
- Improved model systems: Patient-derived organoids that better recapitulate tumor heterogeneity and microenvironmental interactions [30].
- Single-cell multi-omics: Integrated analysis of transcriptional, epigenetic, and protein expression to define plasticity trajectories [2].
- Mathematical modeling: Computational approaches to predict plasticity dynamics and treatment responses [29].
- Real-time monitoring: Advanced imaging and biosensor technologies to track plasticity events in living systems.
The plasticity paradigm underscores the remarkable adaptability of cancer cells and highlights the necessity for therapeutic strategies that account for dynamic cellular states rather than static cellular hierarchies. As our understanding of the molecular circuitry governing CSC-NSCC interconversion deepens, so too will our ability to develop interventions that target this fundamental driver of tumor resilience and therapeutic resistance.
Cancer stem cells (CSCs) represent a dynamic subpopulation within tumors that drive intratumoral heterogeneity, therapeutic resistance, and disease recurrence. This technical review examines the genetic and epigenetic mechanisms through which CSCs generate and maintain heterogeneity, creating significant challenges for cancer therapy. CSCs exhibit remarkable plasticity, transitioning between functional states in response to therapeutic pressure and microenvironmental cues. Their capacity for self-renewal, differentiation, and adaptive resistance is governed by complex interactions between mutational processes, epigenetic reprogramming, and signaling pathway dysregulation. Understanding these mechanisms provides critical insights for developing CSC-targeted therapies to overcome treatment resistance. Emerging technologies in single-cell analysis, functional genomics, and computational biology are advancing our ability to dissect CSC heterogeneity and identify novel therapeutic vulnerabilities for precision medicine applications.
The cancer stem cell (CSC) paradigm has revolutionized our understanding of tumor biology, revealing that tumors are not uniform masses of identical cells but rather organized hierarchies with functional heterogeneity [1] [31]. CSCs sit at the apex of this hierarchy, possessing self-renewal capacity and the ability to differentiate into the diverse cell populations that constitute the tumor bulk [31]. This model explains critical clinical challenges including therapeutic resistance, metastasis, and relapse, as conventional therapies often eliminate rapidly dividing differentiated cancer cells while sparing the more quiescent CSCs [1] [32].
Intratumoral heterogeneity manifests both spatially (within different regions of the same tumor) and temporally (as tumors evolve over time and in response to treatment) [33] [34]. CSCs contribute to this heterogeneity through genetic instability, epigenetic plasticity, and dynamic interactions with the tumor microenvironment [1] [35]. The traditional view of CSCs as a fixed cellular entity has been replaced by a more nuanced understanding of stemness as a dynamic functional state that cancer cells can enter or exit based on intrinsic programs and extrinsic cues [25]. This plasticity enables tumors to adapt to therapeutic pressures and environmental challenges, making CSCs a moving target for treatment interventions.
This review examines the genetic and epigenetic mechanisms through which CSCs drive intratumoral heterogeneity, with implications for drug resistance and cancer progression. By synthesizing current research advances, we aim to provide a comprehensive framework for understanding CSC biology and its therapeutic implications.
Genetic Mechanisms of CSC-Driven Heterogeneity
CSCs contribute to genetic heterogeneity through multiple mechanisms that generate genomic diversity and enable evolutionary selection within tumor ecosystems. These mechanisms operate both in untreated tumors and under therapeutic pressure, leading to clonal expansion of resistant populations.
Genomic Instability and Mutational Diversity
CSCs exhibit elevated genomic instability, which serves as a fundamental source of genetic heterogeneity. Most tumors display some form of genomic instability, encompassing both solid malignancies and hematopoietic tumors [33]. This instability manifests through increased mutation rates and chromosomal segregation errors, which occur approximately once every 100 cell divisions [33] [34].
Therapy-induced mutations and severe genomic instability can accumulate, leading to a hypermutator phenotype that further increases intratumoral heterogeneity [34]. For example, temozolomide can induce a hypermutated phenotype by enriching transitional mutations in mismatch repair (MMR) genes [33]. This genomic plasticity enables CSCs to continuously generate diverse subclones with varying functional capabilities and drug sensitivities.
Extrachromosomal DNA and Clonal Evolution
Extrachromosomal DNA (eccDNA) represents another significant mechanism through which CSCs amplify genetic heterogeneity. These circular DNA elements exist outside chromosomes and can contain amplified oncogenes and drug resistance genes [33]. During tumor evolution, the asymmetric distribution of eccDNA to daughter cells results in tumor cell evolution and accumulated variation, producing different molecular and genetic characteristics from the primary cell [33] [34].
This process enables a form of "forced evolution" where CSCs rapidly generate diverse subclones in response to selective pressures. The genomic instability and distribution of eccDNA to offspring cells result in tumor cell evolution and accumulated variation, producing different molecular, genetic characteristics, and biological phenotypes from primary cells [33].
Table 1: Genetic Mechanisms Driving CSC-Mediated Heterogeneity
| Mechanism | Functional Consequence | Therapeutic Impact |
|---|---|---|
| Genomic instability | Elevated mutation rates and chromosomal abnormalities | Increased adaptive potential and resistance evolution |
| Extrachromosomal DNA (eccDNA) | Amplification of oncogenes and resistance genes | Rapid generation of resistant subclones |
| Clonal evolution | Selection of fitter subpopulations under therapy | Treatment failure and disease progression |
| DNA repair dysregulation | Enhanced repair capacity in CSCs | Resistance to DNA-damaging therapies |
Spatial and Temporal Heterogeneity
Genetic heterogeneity manifests as both spatial and temporal diversity within tumors. Spatial heterogeneity refers to genetic differences between different regions of the same tumor or between primary tumors and metastases [33] [34]. For instance, in non-small cell lung cancer (NSCLC), different regions of the same tumor may contain varying proportions of EGFR mutant and wild-type cells, with significant implications for response to tyrosine kinase inhibitors [33].
Temporal heterogeneity reflects the dynamic changes in tumor genetics over time and in response to therapeutic interventions [33] [34]. Successive biopsies to study tumor evolution suggest that chemotherapy can alter the tumor mutational spectrum and induce molecular changes over time [33]. Targeted therapies exert particularly strong selective pressure on cancer cells carrying oncogenes, leading to the emergence of resistance mutations [33].
Epigenetic Regulation of CSC Plasticity and Heterogeneity
Epigenetic mechanisms enable CSCs to dynamically alter their functional state without changes to their DNA sequence, creating non-genetic heterogeneity that contributes significantly to therapeutic resistance and adaptive potential.
Chromatin Remodeling and Cell State Transitions
The epigenetic landscape of CSCs governs their capacity for state transitions and phenotypic plasticity. Each cell state reflects a distinct configuration of gene regulatory networks (GRNs) that emerge from the complex interplay among chromatin structure, transcription factors, and gene expression [35]. The differential response of cancer cell states to treatment may be explained by variations in their chromatin architecture itself and the resulting activation of specific GRNs [35].
Histone modifications play a particularly significant role in tumor evolution processes [35]. For example, breast cancer cells can reach a drug-tolerant state by reducing H3K27me3 histone marks, while inhibition of H3K27me3 demethylation in combination with chemotherapy prevents the transition to this drug-tolerant state [35]. These epigenetic alterations create a reservoir of cell states that can be selected under therapeutic pressure.
Polycomb Complexes and Stemness Maintenance
Polycomb group complexes (PRC1 and PRC2) serve as critical regulators that bridge epigenetic control and stemness maintenance. Their synergistic activity leads to the formation of transcriptionally repressive Polycomb domains characterized by compacted chromatin enriched in H2AK119ub1 (catalyzed by PRC1) and H3K27me3 (catalyzed by PRC2) [35].
BMI1 (a component of PRC1) is associated with self-renewal capacity of various adult stem cells and plays a preponderant role in maintaining stemness in malignant cells [35]. Beyond its function in stemness regulation, BMI1 contributes to the DNA damage response by depositing H2AK119ub mark at DNA lesions, facilitating repair through homologous recombination [35]. This dual function connects stemness maintenance with DNA repair capacity, contributing to therapy resistance in CSCs.
Similarly, EZH2 (the catalytic component of PRC2) is frequently overexpressed in CSCs and regulates DNA repair through modulation of SLFN11 expression and inhibition of transcriptional activity at DNA damage sites [35]. The MELK-FOXM1-EZH2 signaling axis has been identified as essential for glioblastoma stem cell radioresistance [35].
Table 2: Epigenetic Regulators in CSC Maintenance and Heterogeneity
| Epigenetic Regulator | Function in CSCs | Role in Heterogeneity |
|---|---|---|
| BMI1 (PRC1) | Self-renewal maintenance, DNA damage response | Promotes stem state stability and therapeutic resistance |
| EZH2 (PRC2) | Histone methylation, gene silencing | Maintains undifferentiated state, suppresses differentiation |
| BRD4 (BET protein) | Enhancer activity, transcriptional elongation | Regulates state transitions and phenotypic plasticity |
| DNA methylation enzymes | Promoter methylation, gene silencing | Stabilizes cellular states and restricts differentiation |
DNA Methylation and Cellular Identity
DNA methylation patterns contribute significantly to CSC identity and heterogeneity. Temporal shifts in DNA methylation patterns and DNA methylation in the transcription of genes represent key epigenetic mechanisms that influence cellular identity and functional states [33]. These methylation changes can create stable epigenetic states that persist across cell divisions, contributing to the maintenance of distinct cellular subpopulations within tumors.
Epigenetic modifications participate in tumor heterogeneity through their influence on drug-tolerant persister (DTP) cells and their role in increased tolerance to higher drug pressure [36]. Additionally, altering the epigenetic landscapes by DNA methylation aids in the maintenance and survival of CSCs which exhibit resistance features at the individual level [36].
Interplay Between DNA Damage Repair and Epigenetic Regulation
The relationship between DNA damage response and epigenetic regulation represents a critical interface that influences CSC behavior and contributes to intratumoral heterogeneity.
Cell Identity Influences DNA Damage Mapping
The epigenetic state of CSCs directly influences their pattern of DNA damage susceptibility. Genome-wide mapping of double-strand breaks (DSBs) demonstrates a relationship between genomic instability and nucleosome density [35]. DSBs are enriched in regions bearing epigenetic marks of transcriptionally active genes (H3K4me2/3), enhancer loci (H3K27ac, H3K9ac, and H3K4me1), and regions rich in structural proteins such as CTCF [35].
This mapping of genomic breaks or "breakome" is influenced by cell identity [35]. For example, glioblastoma CSCs exhibit high expression activity of genes located at common fragile sites compared to the glioblastoma cells composing the tumor bulk, leading to transcription-replication conflicts and increased DSB formation [35]. Thus, the specific transcriptional and epigenetic state of CSCs creates unique patterns of genomic vulnerability.
Epigenetic Regulation of DNA Repair Pathway Choice
Cell identity guides not only the distribution of DNA damage but also the choice of repair pathways. Beyond the traditional factors of damage type and cell cycle phase, the epigenetic state directly influences DNA damage response and repair capacity [35]. Dual-role regulators that maintain cell identity can activate specific DNA damage response pathways, creating a direct link between stemness and DNA repair.
As previously mentioned, BMI1 promotes DNA repair via homologous recombination through deposition of H2AK119ub at DNA lesions [35]. Similarly, BRD4 interacts with BRG1 and CtIP to facilitate homology-directed repair of DSBs [35]. These mechanisms enhance the DNA repair capacity of CSCs, contributing to their resistance to DNA-damaging therapies.
Diagram 1: Interplay between DNA damage repair and epigenetic regulation in CSCs. Epigenetic regulators including PRC1/BMI1, PRC2/EZH2, and BRD4 influence repair pathway choice through chromatin modifications, contributing to CSC therapeutic resistance.
CSC Signaling Pathways and Heterogeneity Maintenance
CSCs utilize evolutionarily conserved signaling pathways to maintain their stemness and generate cellular heterogeneity. These pathways respond to both intrinsic cues and signals from the tumor microenvironment.
Core Stemness Signaling Pathways
Three primary signaling pathways—Wnt, Notch, and Hedgehog—play central roles in regulating CSC self-renewal and differentiation. These pathways, often dysregulated in cancer, represent a critical link to the tumorigenic potential of CSCs [31]. Targeting these self-renewal pathways offers promising therapeutic strategies to inhibit tumor proliferation and prevent recurrence.
In breast CSCs, specific signaling pathways including Notch, Wnt, PI3K/AKT/mTOR, TGF-β, and Hippo-YAP/TAZ regulate stemness maintenance and therapeutic resistance [32]. These pathways control processes such as drug escape and enhanced DNA repair that characterize CSC behavior [32]. The activity of these pathways varies across CSC subpopulations, contributing to functional heterogeneity.
Metabolic Plasticity and Heterogeneity
CSCs exhibit metabolic plasticity that enables their survival under diverse environmental conditions. Metabolic plasticity allows CSCs to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids, enabling them to survive under diverse environmental conditions [1]. This metabolic flexibility contributes to functional heterogeneity and enables CSCs to adapt to nutrient deprivation, hypoxia, and therapeutic challenges.
Interactions with stromal cells, immune components, and vascular endothelial cells facilitate metabolic symbiosis, further promoting CSC survival and drug resistance [1]. The tumor microenvironment creates distinct metabolic niches that support different CSC states, adding another layer to intratumoral heterogeneity.
Diagram 2: Signaling pathways regulating CSC states and functional heterogeneity. Multiple signaling pathways integrate microenvironmental cues to generate diverse CSC states with distinct functional properties.
Methodologies for Investigating CSC Heterogeneity
Advanced experimental approaches are essential for dissecting the genetic and epigenetic complexity of CSCs and their contribution to intratumoral heterogeneity.
Single-Cell Analysis Technologies
Single-cell technologies have revolutionized our ability to characterize CSC heterogeneity. Recent advances in single-cell sequencing, spatial transcriptomics, and multiomics integration have significantly improved our understanding of CSC heterogeneity and metabolic adaptability [1]. These approaches enable researchers to resolve the cellular diversity within tumors and identify rare CSC subpopulations that might be missed in bulk analyses.
Single-cell RNA sequencing and mutation characterization enable investigation of evolutionary dynamics in tumor cell populations, with important implications for individualized therapy [36]. These technologies can identify the cellular, molecular, and genetic processes that govern cancer cell plasticity [37].
Functional Screening Approaches
CRISPR-based functional screens provide powerful tools for identifying genetic and epigenetic dependencies in CSCs. The development of 3D organoid models, CRISPR-based functional screens, and AI-driven multiomics analysis is paving the way for precision-targeted CSC therapies [1]. These approaches enable systematic interrogation of gene function across diverse CSC states and genetic backgrounds.
Functional screens can identify vulnerabilities specific to CSCs versus more differentiated cancer cells, revealing potential therapeutic targets. Combining these screens with single-cell readouts further enhances resolution of cell-state-specific dependencies.
Table 3: Experimental Approaches for CSC Heterogeneity Research
| Methodology | Application | Key Insights |
|---|---|---|
| Single-cell RNA sequencing | Transcriptomic profiling of individual cells | Identification of rare CSC states and transition trajectories |
| CRISPR functional screens | Systematic gene function assessment | Discovery of CSC-specific genetic dependencies |
| Spatial transcriptomics | Gene expression in tissue context | Mapping CSC spatial distribution and niche interactions |
| Lineage tracing | Cell fate mapping | Understanding CSC differentiation hierarchies and plasticity |
| Organoid models | 3D culture of patient-derived cells | Preservation of tumor heterogeneity and drug response |
Research Reagent Solutions
Table 4: Essential Research Reagents for CSC Heterogeneity Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| CSC surface markers | CD44, CD133, CD24, EpCAM | Isolation and purification of CSC subpopulations |
| Signaling pathway inhibitors | LGK974 (Wnt), DAPT (Notch), Vismodegib (Hedgehog) | Functional interrogation of stemness pathways |
| Epigenetic probes | GSK126 (EZH2 inhibitor), JQ1 (BET inhibitor) | Modulation of epigenetic states and plasticity |
| CSC functional assay kits | Mammosphere formation, ALDEFLUOR | Assessment of self-renewal and stemness properties |
| Lineage tracing systems | Cre-lox, barcoding technologies | Fate mapping and plasticity assessment |
Therapeutic Implications and Future Perspectives
Understanding the genetic and epigenetic basis of CSC heterogeneity opens new avenues for therapeutic intervention to overcome treatment resistance.
Targeting CSC-Specific Vulnerabilities
Emerging therapeutic strategies aim to specifically target CSCs by exploiting their unique genetic and epigenetic dependencies. Emerging strategies such as dual metabolic inhibition, synthetic biology-based interventions, and immune-based approaches hold promise for overcoming CSC-mediated therapy resistance [1]. Moving forward, an integrative approach combining metabolic reprogramming, immunomodulation, and targeted inhibition of CSC vulnerabilities is essential for developing effective CSC-directed therapies [1].
Promising approaches include targeting the self-renewal pathways (Wnt, Notch, Hedgehog), epigenetic modifiers (EZH2, BET proteins), and immune evasion mechanisms employed by CSCs [1] [31]. Combination therapies that simultaneously target multiple vulnerabilities may be required to effectively eliminate CSCs and prevent resistance development.
Challenges in CSC-Targeted Therapy
Several significant challenges complicate the development of CSC-targeted therapies. Major hurdles remain, including the lack of universally reliable CSC biomarkers and the challenge of targeting CSCs without affecting normal stem cells [1]. The dynamic plasticity of CSCs enables them to adapt to therapeutic pressure by transitioning between states, creating a moving target for interventions [25] [37].
Tumor heterogeneity itself presents a barrier to effective treatment, as a single therapeutic agent may only be effective for subsets of cells with certain features, but not for others [33] [34]. This necessitates a shift from current treatment approaches to ones that are tailored against the killing patterns of cancer cells in different clones [33].
Future Research Directions
Future research should focus on deciphering the regulatory networks that control CSC state transitions and heterogeneity. Advanced technologies including artificial intelligence-driven analysis of multiomics data, improved organoid and tumor microenvironment models, and sophisticated lineage tracing approaches will be essential for mapping the complex dynamics of CSC populations [1] [31].
Integration of these approaches with clinical studies will enable validation of preclinical findings and facilitate translation to patient care. Additionally, developing strategies to manipulate CSC plasticity and differentiation states represents a promising avenue for neutralizing the threat posed by CSCs without necessarily eliminating them entirely.
CSCs drive intratumoral heterogeneity through complex genetic and epigenetic mechanisms that enable tumor adaptation, therapeutic resistance, and disease progression. Genetic instability generates diversity upon which selection can act, while epigenetic plasticity allows dynamic reprogramming of cellular states in response to environmental cues. The interplay between these mechanisms creates a complex ecosystem within tumors, with CSCs at its foundation.
Advancing our understanding of these processes requires sophisticated experimental approaches that can resolve heterogeneity at single-cell resolution and capture dynamic state transitions. Therapeutic progress will depend on developing strategies that account for and target this heterogeneity, potentially through combination approaches that address multiple vulnerabilities simultaneously. As research in this field advances, targeting CSC-driven heterogeneity holds promise for overcoming therapeutic resistance and improving cancer outcomes.
Advanced Techniques for Isolating, Validating, and Modeling CSCs
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [1]. Their ability to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies. A fundamental challenge in CSC research is their heterogeneity and the lack of universal biomarkers; for instance, glioblastoma (GBM) CSCs frequently express neural lineage markers like CD133, whereas gastrointestinal cancers may harbor CSCs characterized by LGR5 or CD166 expression [1]. Marker-based isolation via Fluorescence-Activated Cell Sorting (FACS) provides a powerful method to isolate these rare CSCs from a heterogeneous tumor mass, enabling deeper study of their role in tumor heterogeneity and drug resistance [38] [39]. This guide details the core principles and protocols for using FACS to isolate CSCs, a critical step in understanding and ultimately overcoming therapeutic failure.
Core Principles of Flow Cytometry and FACS
Flow cytometry is an analytical technique that measures the physical and chemical properties of cells as they flow in a fluid stream past a laser beam [39]. FACS is a specialized form of flow cytometry that adds a cell sorting capability, allowing for the physical isolation of specific cell populations based on their measured characteristics [39].
Key System Components
The FACS system integrates several components to achieve this:
- Fluidics System: Utilizes sheath fluid and laminar flow to focus cells into a single-file stream, ensuring they pass through the laser interrogation point one at a time [39].
- Optical System: Includes lasers for illumination and lenses and filters to collect the resulting light signals. As cells pass through the laser, they scatter light. Fluorophores attached to antibodies on the cell emit light at specific wavelengths upon laser excitation [39].
- Electronics System: Photodetectors convert the scattered and fluorescent light signals into electronic signals. These are digitized and processed by computer software for analysis and decision-making [39].
- Sorting Mechanism: In FACS, the stream is broken into droplets. Based on the analyzed signals, an electrical charging ring applies a charge to droplets containing target cells. These charged droplets are then deflected by an electrostatic field into collection tubes [39].
Critical Parameters and Measurements
- Forward Scatter (FSC): Correlates with cell size; larger cells scatter more light in the forward direction [39].
- Side Scatter (SSC): Correlates with cellular granularity and internal complexity [39].
- Fluorescence Intensity: Measured by detectors for specific wavelengths, indicating the abundance of the target marker on the cell surface or inside the cell [39].
Table 1: Comparison of Flow Cytometry and FACS
| Aspect | Flow Cytometry | FACS |
|---|---|---|
| Definition | Analytical technique for measuring cell properties | Specialized flow cytometry that sorts cells |
| Sorting Capability | Limited or absent | Ability to sort cells based on fluorescence |
| Primary Output | Multiparameter data for population analysis | Physically isolated cell populations |
| Instrument Complexity | Relatively simple | More complex due to sorting mechanisms |
FACS Workflow for CSC Isolation: A Detailed Protocol
The following protocol, adapted for CSC isolation, outlines the process from sample preparation to sorted cell collection.
Sample Preparation and Staining
- Create a Single-Cell Suspension: Dissociate solid tumor tissue or prepare a suspension from blood or bone marrow using appropriate enzymatic (e.g., collagenase) and/or mechanical dissociation methods. Filter the suspension through a cell strainer (e.g., 40-70µm) to remove clumps and obtain a single-cell suspension.
- Cell Counting and Viability Assessment: Count cells using a hemocytometer or automated cell counter. Assess viability with a dye like Trypan Blue. High viability (>90%) is crucial for efficient sorting.
- Antibody Staining:
- FC Receptor Blocking: Incubate cells with an Fc receptor blocking agent (e.g., human or mouse IgG) for 10-15 minutes on ice to prevent non-specific antibody binding [39].
- Surface Marker Staining: Resuspend cells in a staining buffer (e.g., PBS with 1-2% FBS or BSA). Add fluorescently-conjugated antibodies against CSC-specific surface markers (e.g., anti-CD133-APC for glioblastoma stem cells) [38]. Include viability dyes (e.g., DAPI or 7-AAD) to exclude dead cells [39].
- Incubation: Incubate the cell-antibody mixture for 20-30 minutes in the dark on ice.
- Washing: Centrifuge the cells and resuspend in fresh staining buffer to remove unbound antibody. Repeat this wash step twice.
- Final Resuspension: Resuspend the stained cell pellet in an appropriate FACS sorting buffer (e.g., PBS with 1-2% FBS and potentially 1-2 mM EDTA to prevent clumping) [39]. Pass the cell suspension through a filter again immediately before sorting to remove any aggregates that may have formed.
Instrument Setup and Sorting
- Startup and Calibration: Power on the FACS sorter and perform startup and quality control procedures as per the manufacturer's instructions. Use calibration beads to align the instrument and ensure optimal performance.
- Compensation: Due to the overlap in emission spectra of different fluorophores, compensation is critical in multicolor experiments. Use compensation beads or stained control cells to set up the compensation matrix in the software, correcting for this spectral overlap [39].
- Gating Strategy:
- Gating on Intact Cells: Use FSC-A vs. SSC-A to gate on the population of interest and exclude debris.
- Singlets Gating: Use FSC-A vs. FSC-H to gate on single cells and exclude doublets or aggregates.
- Viability Gating: Exclude dead cells by gating out the population positive for the viability dye (e.g., DAPI+).
- CSC Population Isolation: Create a gate based on the fluorescence of the CSC marker (e.g., CD133-APC) to identify the target population. A negative control (unstained or isotype control) is essential for accurately setting this gate [38] [39].
- Sorting Setup: Define the sort logic (e.g., sort CD133+ cells into one tube and CD133- into another). Choose the sort precision (e.g., purity mode vs. yield mode) and collection device (tubes, plates). Collection tubes should contain a suitable recovery medium (e.g., complete growth medium with high serum or other supplements to support cell viability post-sort).
- Sorting Execution: Begin the sort. Monitor key parameters like sort efficiency and abort rate, making adjustments to the sample concentration or instrument settings if necessary.
Post-Sort Analysis and Culture
- Validation: Analyze an aliquot of the sorted populations to confirm purity. The sorted CD133+ population should be highly enriched, and the CD133- population should be largely depleted of positive cells.
- Culturing or Downstream Applications: Culture the sorted CSCs in conditions that maintain their stemness (e.g., serum-free medium with growth factors like EGF and FGF on a low-attachment surface). Alternatively, use the cells immediately for downstream applications such as functional assays (e.g., sphere formation, in vivo transplantation), molecular analysis (e.g., RNA sequencing), or drug sensitivity testing [38].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for FACS-based CSC Isolation
| Reagent/Material | Function/Purpose | Examples & Notes |
|---|---|---|
| Fluorophore-Conjugated Antibodies | Specific detection of CSC surface markers. | Anti-CD133-APC [38]; Antibodies for CD44, CD24, EpCAM, LGR5. Critical for defining the target population. |
| Viability Dyes | Distinguish live from dead cells to improve sort purity and data quality. | DAPI, Propidium Iodide (PI), 7-AAD, Zombie dyes [39]. These dyes typically are excluded by live cells. |
| Staining & Sorting Buffers | Maintain cell viability, prevent clumping, and block non-specific binding. | PBS with 1-2% FBS or BSA (staining); with EDTA (sorting) [39]. |
| Fc Receptor Blocking Agent | Reduces background signal by preventing non-specific antibody binding. | Species-specific IgG; essential for immune cells like macrophages [39]. |
| Compensation Beads | Account for spectral overlap between fluorophores in multicolor panels. | Ultraviolet- or antibody-capture beads; used to create a compensation matrix [39]. |
| Permeabilization Reagents | Allow antibody access to intracellular targets for broader phenotyping. | Saponin, Triton X-100; used after cell fixation [39]. |
Advanced Analytical Techniques
Marker Enrichment Modeling (MEM)
For deep characterization of isolated populations, Marker Enrichment Modeling (MEM) can be used to generate quantitative identity labels. MEM quantifies each feature's relative enrichment in a population compared to a reference, creating a human-readable and machine-readable label that is particularly useful for comparing novel cell populations discovered through automated clustering [40]. The MEM score is calculated as:
MEM = |MAG~pop~ - MAG~ref~| + (IQR~ref~/IQR~pop~ - 1); if MAG~pop~ < MAG~ref~, MEM = -MEM [40]
Where MAG is the median fluorescence intensity and IQR is the interquartile range. This score reflects protein enrichment more effectively than a simple z-score [40].
Diagram 1: MEM Analysis Workflow
Applications in CSC Research and Therapeutic Development
The ability to isolate pure CSC populations via FACS has profound implications for both basic research and clinical translation.
- Research Applications: Isolated CSCs are used to study the mechanisms underlying therapy resistance, metastatic dissemination, and tumor heterogeneity. They enable the investigation of CSC-specific metabolic pathways [1], genetic and epigenetic profiles [1], and interactions with the tumor microenvironment [1].
- Diagnostic and Prognostic Potential: The presence and abundance of CSCs, as quantified by flow cytometry, can serve as a biomarker for disease aggressiveness and prognosis in cancers like AML (with CD34⁺CD38⁻ cells) [1] and glioblastoma (with CD133⁺ cells) [38].
- Cell-Based Therapies and Drug Discovery: FACS is critical for purifying cell populations, including stem cells, for use in autologous or allogeneic cell-based therapies [39]. Furthermore, isolated CSCs are used in high-throughput drug screens to identify compounds that specifically target the therapy-resistant core of tumors, with the goal of overcoming drug resistance and preventing relapse [41].
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [1]. Their ability to evade conventional treatments and contribute to intratumoral heterogeneity makes them critical targets for innovative therapeutic strategies [42] [1]. The identification and targeting of CSCs remain challenging due to their phenotypic heterogeneity and cellular plasticity, which limit the utility of surface marker-based isolation methods alone [43]. This has necessitated the development of functional assays that probe the biological capabilities defining CSCs, primarily their self-renewal potential (sphere formation), stem cell metabolism (ALDH activity), and treatment resilience (chemoresistance) [1] [44]. This whitepaper provides an in-depth technical examination of these three core functional assays, framing them within the broader context of understanding and targeting the role of CSCs in tumor heterogeneity and drug resistance.
Sphere Formation Assay
Principle and Applications
The sphere formation assay is a marker-free methodology for the functional identification and enrichment of CSCs in vitro [42] [43]. This model is based on the ability of CSCs to grow under ultralow-attachment conditions in serum-free medium supplemented with growth factors [42]. In contrast to adherent 2D culture, the 3D culture of tumorsphere assay exploits inherent biological features of CSCs such as anoikis resistance and self-renewal [42]. When cancer cells are cultured in suspension, bulk non-stem cells undergo anoikis—a form of programmed cell death triggered by detachment from the extracellular matrix—while only stem-like cells survive and proliferate to form clonal spheres [43]. The formation of tumorspheres from cancer cells thus serves to identify cells with these stem-like characteristics and is frequently used as a metric for testing the viability of tumor cells to anticancer agents [42].
Standard Protocol for Tumorsphere Formation
The following protocol summarizes the detailed methodology for the generation and propagation of spheres from pediatric brain tumor medulloblastoma (MB) cells, as described by SpringerLink [42]. The process is broadly applicable to other cancer types with appropriate modifications to culture media.
Key Materials:
- Ultra-low attachment plates: Prevents cell attachment and forces suspension culture.
- Serum-free medium: Typically DMEM/F12 base.
- Growth factor supplements: Including EGF, bFGF, and B27 supplement.
- Single-cell suspension: Prepared via enzymatic dissociation and filtration.
Procedure:
- Preparation of Single Cell Suspension: Dissociate tumor tissue or monolayer cells using enzyme-free dissociation buffer or low-concentration trypsin. Mechanically disrupt aggregates and pass through a 40μm cell strainer to obtain a single-cell suspension. Determine viability and concentration.
- Plating: Resuspend cells in serum-free medium supplemented with growth factors. Plate cells at clonal density (500–10,000 cells/well, depending on cell type) in ultra-low attachment multiwell plates. A density of 5,000 cells/well in a 6-well plate is common [45].
- Culture: Incubate cells at 37°C with 5% CO₂ for 7–14 days. The duration depends on the cell type's doubling time and sphere-forming capacity; for example, pancreatic cancer cells may require 14 days [45].
- Media Maintenance: Carefully add fresh growth factor-supplemented medium every 2–3 days without disrupting the forming spheres.
- Quantification and Analysis: After the incubation period, count spheres under an inverted microscope. Typically, only spheres with a diameter >50μm are counted, and sphere-forming efficiency (SFE) is calculated as (number of spheres formed / number of single cells seeded) × 100% [43].
Advanced Microfluidic Platform for High-Throughput Analysis
Conventional sphere formation assays face limitations including potential cell aggregation, labor-intensive processes, and low throughput. A high-throughput microfluidic platform addresses these challenges [43].
Platform Design:
- Composition: 1,024 microchambers for massive parallel single-cell culture.
- Cell Capture: Uses a hydrodynamic capturing scheme with two fluidic paths (central and serpentine) per chamber. The central path has a lower flow resistance but a smaller opening (10μm x 15μm) that sterically captures the first cell, redirecting subsequent cells to serpentine paths downstream.
- Non-adherent Coating: Features a spin-coated polyHEMA hydrogel to create a uniform, non-adherent surface (roughness <0.2μm RMS) that prevents focal adhesion formation, ensuring true suspension culture.
Performance and Workflow:
- Capture Efficiency: >70% of microchambers capture a single cell, enabling definitive clonal analysis.
- Throughput: Allows monitoring of 700–800 single cells in a single experiment.
- Downstream Analysis: Single-cell derived spheres can be retrieved and dissociated for subsequent analysis, such as single-cell PCR to probe heterogeneity within clonal CSC spheres.
The diagram below illustrates the workflow and cell capture mechanism of this microfluidic platform.
Quantitative Data from Representative Studies
Table 1: Sphere Formation Efficiency in Different Cell Models
| Cell Type / Model | Seeding Density | Culture Duration | Sphere Formation Efficiency | Key Experimental Conditions | Source |
|---|---|---|---|---|---|
| SUM159 (Breast Cancer) | Single cells in 1,024-chamber chip | 10 days | 55% (spheres >50μm diameter) | Serum-free media, continuous perfusion | [43] |
| CFPAC-1 (Pancreatic Cancer) | 5,000 cells/well (6-well plate) | 14 days | Reported as countable spheres | Ultra-low attachment plate | [45] |
| BxPC-3 (Pancreatic Cancer) | 5,000 cells/well (6-well plate) | 14 days | Reported as countable spheres | Ultra-low attachment plate | [45] |
| Medulloblastoma (MB) Cells | Varies by cell line potency | 7-14 days | Used to test STAT3 inhibition | Growth factor-supplemented media | [42] |
Aldefluor Assay and ALDH Activity Detection
Principle and Significance
The Aldefluor assay detects cells with high aldehyde dehydrogenase (ALDH) activity, a functional hallmark of both normal and cancer stem and progenitor cells across various lineages, including hematopoietic, mammary, endothelial, mesenchymal, and neural cells [46]. ALDH is a detoxifying enzyme responsible for oxidizing intracellular aldehydes, and its high activity contributes to the resistance and self-renewal properties of CSCs [47] [46]. The Aldefluor system provides a non-immunological, flow cytometry-based method to identify, evaluate, and isolate viable ALDH-bright (ALDHbr) cells, which have been shown to possess stem-like properties in over 80 different tissues [46].
Standard ALDEFLUOR Protocol
Key Reagents:
- BODIPY-aminoacetaldehyde (BAAA): The fluorescent, non-toxic substrate for ALDH.
- ALDEFLUOR Assay Buffer: Specific buffer for the reaction.
- DEAB (Diethylaminobenzaldehyde): A specific ALDH inhibitor used as a negative control.
Procedure:
- Sample Preparation: Create a single-cell suspension from tumor tissue or cultured cells. Maintain cell viability throughout the process.
- Staining:
- Test Sample: Incubate cells with BAAA substrate at 1.5 µM for 30-45 minutes at 37°C.
- Control Sample: Pre-incubate an aliquot of cells with DEAB inhibitor for 15 minutes, then add BAAA substrate.
- Reaction Arrest and Analysis: After incubation, centrifuge cells to remove excess substrate and resuspend in cold ALDEFLUOR Assay Buffer. Keep samples on ice until analysis.
- Flow Cytometry: Analyze cells using a standard flow cytometer equipped with a 488nm excitation laser. The converted product, BODIPY-aminoacetate (BAA), is detected in the green fluorescence channel (FITC/GFP, ~520 nm). The DEAB-treated control establishes the baseline fluorescence, and cells significantly brighter than this control are designated as ALDHbr.
Emerging ALDH Probe Technology
While the ALDEFLUOR kit is widely used, it requires specific buffers and inhibitors. Recent research has developed novel fluorescent probes like AldeCou-1 to enhance specificity and simplify protocols [47].
Key Features of AldeCou-1:
- Design: Built on a coumarin-linker-benzaldehyde scaffold.
- Optical Property: Exhibits a significant Stokes shift of 125 nm (λex/λem = 380/505 nm), which enhances the signal-to-noise ratio and minimizes inner-filter effects.
- Mechanism: Fluorescence turn-on is driven by an ALDH-mediated photoinduced electron transfer (PET) mechanism.
- Protocol Advantage: Eliminates the need for ATP-binding cassette (ABC) transporter inhibitors and specialized buffers, enabling simplified assay conditions and direct green fluorescence imaging in live cells (e.g., A549 and MDA-MB-231) [47].
The diagram below illustrates the workflow of the standard Aldefluor assay and the mechanism of the novel AldeCou-1 probe.
Research Reagent Solutions
Table 2: Key Reagents for ALDH Activity Detection
| Reagent / Kit Name | Primary Function | Species Applicability | Key Features / Applications |
|---|---|---|---|
| ALDEFLUOR Kit [46] | Detection of viable ALDHbr stem/progenitor cells | Human, Mouse, Rat | Non-immunological; compatible with flow cytometry & cell sorting; used in >1000 publications. |
| BODIPY-aminoacetaldehyde (BAAA) [46] | Fluorescent ALDH substrate | Human, Mouse, Rat | Converted to fluorescent BAA retained in cells with ALDH activity. |
| DEAB (Diethylaminobenzaldehyde) [46] | Specific ALDH inhibitor for control | Human, Mouse, Rat | Used to set background fluorescence in flow cytometry. |
| AldeCou-1 [47] | Novel fluorescent ALDH probe | Cell lines tested | Large Stokes shift (125nm); simplified protocol; no ABC inhibitors needed. |
Chemoresistance Profiling
Linking Chemoresistance to CSC Properties
A direct functional link exists between chemoresistance and the acquisition of CSC-like properties. Research on Panc-1 pancreatic cancer cells demonstrated that apoptosis-resistant cells surviving 5-fluorouracil (5-FU) treatment exhibited enhanced CSC characteristics [44]. Compared to control cells, these chemoresistant cells showed:
- A higher frequency of sphere-initiating cells.
- Overexpression of stem cell marker genes (OCT4 and NANOG).
- Enhanced invasion ability in response to EMT stimulation [44].
This evidence underscores that conventional chemotherapy can selectively enrich for CSCs, highlighting the need for therapies that specifically target this resistant population.
Chromosomal Instability Signatures as Predictive Biomarkers
Beyond functional assays, genomic biomarkers offer a powerful approach to predicting chemotherapy resistance. Chromosomal instability (CIN) signatures derived from a single genomic test can identify inherent resistance to major chemotherapy classes: platinum-based agents, taxanes, and anthracyclines [48].
Biomarker Formulations:
- Platinum Resistance: Classifies tumors as resistant if they either show no detectable CIN or have a ratio of homologous recombination deficiency signatures where CX2 > CX3 [48].
- Taxane Resistance: Classifies tumors as resistant if they have no CIN or have a low activity (z-score < 0) of signature CX5 [48].
- Anthracycline Resistance: Classifies tumors as resistant based on the presence of focal amplification signatures (CX8, CX9, or CX13) linked to extrachromosomal DNA and potential tolerance to micronuclei-induced cell death [48].
Clinical Validation: These CIN signature biomarkers have demonstrated predictive capacity in real-world cohort studies, showing that patients classified as resistant had a significantly elevated risk of treatment failure. For instance, hazard ratios for taxane resistance were as high as 7.44 in ovarian cancer and 5.46 in metastatic prostate cancer [48].
Protocol forIn VitroChemoresistance Profiling
The following protocol outlines a method to establish and characterize chemoresistant cells, based on studies in pancreatic cancer [44].
Procedure:
- Drug Selection:
- Incplicate cancer cells (e.g., Panc-1) with a relevant chemotherapeutic agent (e.g., 5-FU) at a predetermined sublethal or IC50 concentration for 24 hours.
- Recovery and Expansion:
- Remove the drug-containing medium and wash the cells.
- Culture the surviving cells in complete growth medium without the drug for an extended period (e.g., 28 days) to allow for recovery and expansion of the resistant population.
- Functional Characterization of Resistant Cells:
- Sphere Formation Assay: Plate the surviving cells at clonal density in ultra-low attachment plates and quantify sphere-forming efficiency. An increased frequency indicates enrichment of CSCs [44].
- Gene Expression Analysis: Isolate mRNA from resistant and control cells. Perform real-time PCR for stem cell markers (e.g., OCT4, NANOG) and epithelial-to-mesenchymal transition (EMT) markers (e.g., SNAIL, Vimentin, E-cadherin). Chemoresistant cells typically overexpress stemness and mesenchymal markers [44].
- Invasion Assay: Use a Matrigel invasion chamber to assess the invasive potential of the cells. Chemoresistant cells often exhibit enhanced invasive capacity [44].
The diagram below illustrates the multi-faceted approach to profiling chemoresistance, connecting functional assays with genomic biomarkers.
Quantitative Resistance Data
Table 3: Biomarkers and Functional Assay Outcomes in Chemoresistance
| Assay Type / Biomarker | Cancer Model / Type | Treatment / Agent | Key Outcome / Hazard Ratio (HR) | Source |
|---|---|---|---|---|
| Functional Enrichment [44] | Panc-1 Pancreatic Cancer | 5-Fluorouracil (5-FU) | Increased sphere-forming frequency; OCT4/NANOG overexpression; enhanced invasion. | |
| CIN Signature (Taxane) [48] | Ovarian Cancer | Taxane | HR=7.44 for treatment failure in predicted resistant patients. | |
| CIN Signature (Taxane) [48] | Metastatic Prostate Cancer | Taxane | HR=5.46 for treatment failure in predicted resistant patients. | |
| CIN Signature (Anthracycline) [48] | Metastatic Breast Cancer | Anthracycline | HR=3.69 for treatment failure in predicted resistant patients. |
Functional assays including sphere formation, Aldefluor, and chemoresistance profiling are indispensable tools for identifying and characterizing cancer stem cells. These assays move beyond static marker expression to reveal the dynamic functional capacities of CSCs—self-renewal, metabolic adaptation, and therapy resistance—that drive tumor heterogeneity and clinical relapse [42] [1] [44]. The integration of these functional readouts with emerging genomic biomarkers, such as chromosomal instability signatures, and advanced technological platforms, like high-throughput microfluidics and novel molecular probes, provides a more comprehensive framework for understanding CSC biology [47] [48] [43]. This multi-faceted approach is critical for developing targeted strategies to eradicate CSCs, overcome drug resistance, and ultimately improve patient outcomes in oncology.
The hierarchical organization of tumors, with cancer stem cells (CSCs) at its apex, is a fundamental paradigm in oncology research. CSCs constitute a minor subpopulation within tumors characterized by self-renewal capacity, multi-lineage differentiation, and enhanced tumor-initiating potential [1] [2]. These properties enable CSCs to drive tumor genesis, heterogeneity, metastasis, and therapy resistance [5] [19]. Consequently, accurately quantifying the functional properties of CSCs—specifically their tumorigenicity and self-renewal potential—is critical for understanding cancer biology and developing targeted therapies.
Within this research context, two methodologies stand as gold standards for functional CSC characterization: the in vivo tumorigenicity assay and the limiting dilution assay (LDA). The tumorigenicity assay directly measures the in vivo potential of cells to initiate and form tumors in immunocompromised host animals [49] [50]. When combined with limiting dilution principles, this assay transforms into a powerful quantitative tool for estimating the frequency of tumor-initiating cells within a population [50] [51]. These techniques provide the definitive functional validation required to complement surface marker expression and in vitro sphere formation assays, offering indispensable insights for research aimed at overcoming drug resistance and eradicating CSCs [52].
The In Vivo Tumorigenicity Assay
Core Principles and Significance
The in vivo tumorigenicity assay tests the fundamental functional capacity of CSCs: their ability to form a tumor in vivo. The core principle involves transplanting putative CSC populations into immunocompromised mice and observing tumor formation [49]. This assay is considered a definitive validation because it recapitulates the complex in vivo microenvironment and confirms that the implanted cells possess the necessary machinery to initiate and sustain tumor growth [2] [53].
The selection of the immunocompromised mouse model is a critical variable that significantly impacts the assay's sensitivity and outcomes. The degree of immunodeficiency determines the ability of human cancer cells to engraft and proliferate.
Table 1: Commonly Used Immunocompromised Mouse Models in Tumorigenicity Assays
| Mouse Model | Immune Deficiencies | Key Features & Impact on Assay |
|---|---|---|
| Nude Mice | Lack a thymus, no T-cells [50]. | Permits some human tumor engraftment; lower sensitivity for rare CSCs [50]. |
| SCID Mice | Severe Combined Immunodeficiency; lack functional T and B cells [50]. | Improved engraftment over nude mice; retain NK cell and innate immunity activity [50]. |
| NOD/SCID Mice | Non-obese diabetic SCID background; lack T, B cells, and have reduced NK cell function and defective innate immunity [50]. | Higher engraftment rates; previously considered the model of choice for CSC assays [50]. |
| NSG Mice | NOD/SCID IL-2Rγnull; lack T, B, and NK cells, and have defective macrophage function [49] [50]. | Most immunocompromised model; highest sensitivity for detecting rare CSCs; considered the current gold standard for tumor initiation studies [49] [50]. |
The choice of mouse strain can profoundly influence the experimental results. For instance, a study on melanoma showed that in NSG mice, both CD271⁺ and CD271⁻ tumor cells could initiate tumors, whereas in less immunocompromised models like nude or NOD/SCID mice, only the CD271⁺ population was tumorigenic [50]. This highlights that the use of highly deficient models like NSG mice can reveal a greater complexity and frequency of tumor-initiating cells.
Key Quantitative Thresholds and Experimental Timing
Determining the minimum cell number required for tumor formation and the appropriate observation period is essential for a well-designed tumorigenicity assay.
Table 2: Key Quantitative Parameters for Tumorigenicity Assays
| Parameter | Typical Range | Context and Significance |
|---|---|---|
| Cell Number Threshold | ~100 to 10,000 undifferentiated stem cells per million [49]. | Far above single-cell resolution; consistent with colony/cluster-based growth of CSCs [49]. |
| Minimum for Teratoma | As few as 100 ESCs in Matrigel can form teratomas, but 10 ESCs showed 0% risk in one study [49]. | Demonstrates a non-linear, threshold-dependent relationship for tumor initiation [49]. |
| Assay Sensitivity Goal | Should achieve at least 0.001% sensitivity (100 cells per million) [49]. | Necessary to detect rare CSC populations within a heterogeneous tumor bulk [49]. |
| Monitoring Period | 10 to 36 weeks in research settings; FDA recommends 4 to 7 months for assay development [49]. | A lengthy process that conflicts with the 1-3 month typical turnaround for stem cell product manufacturing, driving need for faster methods [49]. |
The Limiting Dilution Assay (LDA)
Conceptual Foundation and Quantitative Power
The limiting dilution assay (LDA) is a dose-response experimental method that quantitatively estimates the frequency of biologically active units within a larger population [50]. When applied to CSC research, it transforms the qualitative tumorigenicity assay into a rigorous, quantitative tool. The core premise is to transplant serially diluted concentrations of cells into immunocompromised mice (for in vivo LDA) or to culture them in non-adherent conditions (for in vitro tumorsphere LDA) [50] [51]. By analyzing the relationship between the injected cell number and the proportion of animals that develop tumors (or wells that form spheres), researchers can statistically calculate the frequency of cells with tumor-initiating or self-renewal capacity [50].
This method is particularly powerful because it moves beyond simply identifying a tumorigenic subpopulation to precisely estimating its prevalence. This allows for direct comparisons between different tumor samples, genetic manipulations, or pre- and post-treatment conditions. For example, LDA has been used to demonstrate that knocking down NQO1 in non-small cell lung cancer cells reduces their tumor-initiating frequency, while rescuing NQO1 expression restores it [51].
Extreme Limiting Dilution Assay (ELDA) and Statistical Analysis
The Extreme Limiting Dilution Assay (ELDA) is a specific implementation and statistical software tool that has become a gold standard for estimating active CSC frequencies [52]. In this protocol, cells are plated at a range of densities (e.g., 40, 120, 360, and 720 cells per well) across many replicate wells (e.g., 24 wells per dilution) in low-attachment plates [51]. After a cultivation period (e.g., 21 days), the number of wells containing tumorspheres is counted for each dilution.
The data—the number of positive wells per cell dose—is then analyzed using specialized software (available at http://bioinf.wehi.edu.au/software/elda/) [51]. This statistical analysis fits a Poisson distribution to the data, calculating the frequency of sphere-initiating cells along with a confidence interval, providing a robust and comparable metric for CSC activity.
Figure 1: Workflow Diagram for an In Vitro Extreme Limiting Dilution Assay (ELDA)
Integrated Experimental Protocols
Protocol A: In Vivo Limiting Dilution Tumorigenicity Assay
This protocol details the steps to quantitatively assess the tumor-initiating cell frequency in vivo using hepatocellular carcinoma (HCC) cells as a model [50].
Necessary Materials and Equipment:
- Laminar flow biosafety cabinet (BSC)
- Sterile pipettes and conical tubes
- Hemocytometer or cell counter
- 37°C humidified CO₂ incubator
- Centrifuge with swinging-bucket rotor
- Phosphate Buffer Saline (PBS), trypsin-EDTA
- NOD/SCID IL-2Rγ⁻/⁻ (NSG) mice
- Matrigel (optional, to enhance engraftment)
Detailed Procedure:
- Cell Preparation: Harvest human liver cancer cell lines (e.g., Hep3B, HCCLM3) using 0.25% trypsin-EDTA. Resuspend cells in culture medium and pass through a sterile 35 μm-pore filter to acquire a single cell suspension [50].
- Serial Dilution: Count cells and prepare a series of serially diluted cell concentrations. A typical range for HCC could be from 10,000 cells down to 10 cells per injection volume.
- Cell Injection: For each dilution, inject the cell suspension subcutaneously or intramuscularly into groups of NSG mice (commonly 5-8 mice per group). The injection site is often supplemented with Matrigel, which has been shown to increase the frequency of tumorigenic cells detected by several orders of magnitude [50].
- Tumor Monitoring: Monitor mice for tumor growth regularly for a period of several weeks to months (e.g., 10-36 weeks) [49] [50]. Palpate the injection site for visible masses.
- Endpoint Analysis: Sacrifice mice at the defined endpoint or when tumors reach a predetermined size (e.g., 1.5 cm in diameter). Excise and weigh tumors. A portion of the tumor can be dissociated to create a single-cell suspension for serial transplantation into secondary recipient mice, which is a definitive test for self-renewal capacity [50].
- Data Calculation: Record the number of tumor-positive mice per group for each cell dose. Input this data into LDA software (like ELDA) to calculate the tumor-initiating cell frequency and its confidence interval.
Protocol B: In Vitro Limiting Dilution Spheroid Formation Assay
This protocol assesses self-renewal potential in a 3D culture system, which often serves as a surrogate for in vivo tumorigenicity [50] [51].
Necessary Materials and Equipment:
- Low-attachment 96-well and 24-well plates (or plates coated with poly-HEMA)
- Fibrin gel or methylcellulose-based serum-free medium
- Growth factors (EGF, bFGF)
- DMEM/F12 medium
- Inverted microscope
Detailed Procedure:
- Plate Coating (if required): Coat culture plates twice with 0.2% poly-HEMA in 95% ethanol and allow to dry overnight to create a non-adhesive surface [51].
- Cell Preparation and Plating: Harvest and count cells as in Protocol A. Plate cells in serially diluted densities (e.g., from 1000 cells/well down to 1 cell/well in a 96-well plate) in serum-free medium supplemented with growth factors and containing 1% methylcellulose or in a soft fibrin gel. Fibrin gel has been shown to be an ideal matrix for maintaining self-renewal and tumorigenic potential, enabling as few as 10 CSCs to generate tumors in vivo [50]. Use a sufficient number of replicates per dilution (e.g., 24-96 wells).
- Culture and Feed: Culture cells for 1-3 weeks in a 37°C incubator. Add a small volume of fresh medium weekly if needed.
- Scoring and Analysis: After 1-3 weeks, score each well under a microscope for the presence of tumorspheres (tight, spherical, non-adherent clusters). A well is typically scored positive if it contains a sphere of a defined minimum size (e.g., >50 μm diameter). Input the counts of positive wells for each dilution into the ELDA software to calculate the frequency of sphere-initiating cells.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Tumorigenicity and LDA
| Reagent/Category | Function in Assay | Specific Examples & Notes |
|---|---|---|
| Immunodeficient Mice | Provide the in vivo environment for human cell engraftment and tumor formation. | NSG (NOD/SCID IL-2Rγnull) mice are the gold standard due to maximal immunodeficiency [49] [50]. |
| Extracellular Matrix (ECM) | Mimics the tumor microenvironment; enhances engraftment and supports 3D growth. | Matrigel is used for in vivo injections [50]. Fibrin gel is excellent for in vitro 3D tumorsphere culture, inducing CSC dormancy and preserving therapy resistance [50]. |
| Low-Attachment Surfaces | Enriches for CSCs by forcing anchorage-independent growth in serum-free conditions. | Commercially available low-attachment plates or lab-coated plates using poly-HEMA [51]. |
| CSC Culture Media | Selectively supports the growth and maintenance of undifferentiated CSCs. | Serum-free media (e.g., DMEM/F12) supplemented with growth factors like EGF and bFGF [50]. |
| Flow Cytometry Antibodies | Enables isolation and purification of putative CSC subpopulations for functional testing. | Antibodies against CD133, CD44, CD24, EpCAM, ALDH1 (via ALDEFLUOR assay), and CD90 [53] [52]. |
| Statistical Software | Calculates the frequency of tumor-initiating or sphere-initiating cells from LDA data. | ELDA (Extreme Limiting Dilution Analysis) software is a widely used, web-accessible tool [51] [52]. |
Connecting the Assays to the Broader Research Context
The gold standard assays detailed herein are not performed in isolation. They are integral to a broader research workflow aimed at deciphering the role of CSCs in tumor heterogeneity and drug resistance.
Figure 2: Integration of Gold Standard Assays in the CSC Research Workflow
These assays are crucial for validating the functional effects of manipulating key signaling pathways that govern CSC self-renewal, such as Wnt/β-catenin, Hedgehog, and Notch [5] [19]. Furthermore, they are the ultimate test for assessing the efficacy of novel CSC-targeting strategies, including small molecule inhibitors, natural compounds, antibodies, and CAR-T cells [52] [19]. A successful therapeutic agent should show a significant reduction in tumor-initiating cell frequency as measured by LDA, providing a direct link between molecular intervention and functional CSC eradication, a critical step toward overcoming therapy resistance and improving patient outcomes.
Single-Cell Omics and CRISPR Screens for Deep Phenotyping
The convergence of single-cell omics and CRISPR screening technologies represents a paradigm shift in cancer stem cell (CSC) research. This technical guide examines how these integrated approaches are revolutionizing our understanding of CSC-driven tumor heterogeneity and therapeutic resistance. We detail experimental frameworks that combine high-resolution cellular phenotyping with functional genomics to dissect CSC plasticity, identify vulnerability signatures, and uncover novel therapeutic targets. By providing comprehensive methodologies, analytical workflows, and reagent solutions, this review serves as an essential resource for researchers pursuing targeted interventions against the CSC subpopulations that drive tumor recurrence and treatment failure.
Cancer stem cells (CSCs) constitute a dynamic subpopulation within tumors that possess self-renewal capacity, enhanced survival mechanisms, and resistance to conventional therapies, thereby driving tumor initiation, progression, metastasis, and relapse [1]. Their ability to evade treatment makes them critical targets for improving cancer therapies, yet their elusive nature and phenotypic plasticity have complicated eradication efforts [18]. The traditional view of CSCs as rare, static entities defined by surface markers has been fundamentally challenged by single-cell RNA sequencing (scRNA-seq) studies, suggesting that "stemness might be a rather dynamic, context-dependent state" [54].
Single-cell omics technologies have transformed our capacity to profile rare CSC subsets at unprecedented resolution, capturing their functional heterogeneity and transcriptional dynamics within complex tumor ecosystems [54] [55]. When integrated with CRISPR-based functional genomics, these platforms enable systematic mapping of gene regulatory networks underlying CSC maintenance, plasticity, and drug resistance [56]. This powerful combination allows researchers to move beyond correlative observations toward causal mechanistic insights, positioning the field to overcome long-standing challenges in CSC targeting [57] [58].
Computational Framework for CSC Stemness Assessment
Single-cell transcriptomics enables the identification and characterization of CSCs without relying solely on traditional surface markers. Several computational tools have been developed to infer stemness properties and differentiation potential from high-dimensional gene expression data [54].
Table 1: Computational Tools for Assessing Stemness from Single-Cell Data
| Tool | Algorithm Type | Underlying Principle | Application Context |
|---|---|---|---|
| CytoTRACE | Unsupervised | Uses gene counts per cell as indicator of differentiation state | Predicts developmental hierarchy; higher counts correlate with stemness [54] |
| StemID | Unsupervised | Shannon entropy of transcriptome | Quantifies differentiation potential through transcriptional heterogeneity [54] |
| SCENT | Unsupervised | Signaling entropy | Models network entropy from gene expression to measure plasticity [54] |
| mRNAsi | Supervised | Machine learning trained on stem cell references | Computes stemness index based on pluripotency signatures [54] |
| StemSC | Supervised | Relative expression ordering of gene pairs | Classifies stem-like cells using reference expression patterns [54] |
| scEpath | Unsupervised | Inference of transition probabilities | Maps phenotypic plasticity and state transitions along trajectories [54] |
These computational approaches have revealed that CSCs represent reversible states along developmental and treatment-induced trajectories rather than fixed phenotypic entities. This dynamic nature creates therapeutic opportunities to target transient high-entropy states during cell state transitions—periods of instability that may represent windows of vulnerability [54].
Single-Cell Omics Technologies: Experimental Workflows and Applications
Core Methodological Framework
Standardized single-cell processing workflows have been developed to dissect both tissue and liquid biopsies using droplet/microfluidic platforms or robotic picking [54]. The foundational scRNA-seq workflow encompasses several critical stages:
Sample Preparation and Dissociation: Optimization based on cellular dimensions, viability, and cultivation conditions is crucial for generating high-quality single-cell transcriptome data. Single-cell suspensions are typically procured through enzymatic and mechanical dissociation techniques [55].
Single-Cell Capture: Platforms include plate-based fluorescence-activated cell sorting (FACS) and droplet-based systems. The Chromium system by 10× Genomics, a predominant droplet-based platform, facilitates rapid, simultaneous profiling of thousands of cells within discrete droplets but constrains cell diameter to <30 µm. For larger cells, plate-based FACS employing nozzles of up to 130 µm provides a viable alternative [55].
Transcript Barcoding, Reverse Transcription, and Amplification: All transcripts from individual cells are barcoded, reverse transcribed into barcoded cDNA, followed by second-strand synthesis and PCR-based cDNA amplification. Droplet-based systems employ pooled PCR coupled with cell barcoding techniques to markedly enhance throughput [55].
Library Preparation and Sequencing: Libraries constructed with 3' end enrichment are cost-effective with reduced sequencing noise, while full-length transcript libraries offer superior transcriptome insights, including alternative splicing and isoforms [55].
For clinical applications, single-nuclei RNA sequencing (snRNA-seq) presents a viable alternative that doesn't require immediate sample processing, allowing snap-freezing and proper storage of valuable clinical specimens [55].
Advanced Methodological Innovations
Recent technological advances are addressing key limitations in single-cell analysis. The scCLEAN method utilizes CRISPR/Cas9 to globally recompose scRNA-seq libraries by targeting and removing highly abundant transcripts (comprising <1% of the transcriptome), thereby redistributing approximately half of sequencing reads toward less abundant transcripts [59]. This approach significantly enhances detection sensitivity for biologically relevant low-abundance transcripts that would otherwise fall below the noise threshold [59].
Other emerging platforms include:
- Single-cell combinatorial indexed sequencing (SCI-seq): Constructs numerous single-cell libraries while simultaneously detecting somatic cell copy number variations [55].
- scCOOL-seq: Analyzes single-cell chromatin state/nuclear niche localization, copy number variations, ploidy, and DNA methylation simultaneously [55].
- Topographic single-cell sequencing (TSCS): Provides precise spatial position data for individual cells, enabling in-depth investigation of tumor cell invasion and metastasis [55].
CRISPR Screening Modalities for CSC Vulnerability Mapping
CRISPR-based functional genomics provides a powerful toolkit for systematically identifying genetic dependencies and resistance mechanisms in CSCs. Multiple screening approaches have been developed, each with distinct applications and advantages.
CRISPR Screening Archetypes
Table 2: CRISPR Screening Modalities for CSC Research
| Screening Type | Mechanism | Key Applications in CSC Research | Technical Considerations |
|---|---|---|---|
| CRISPR Knockout (CRISPRko) | Cas9-induced double-strand breaks cause frameshift mutations | Genome-wide loss-of-function screening for CSC essential genes [57] | Favors identification of loss-of-function mutations that confer resistance |
| CRISPR Interference (CRISPRi) | dCas9-KRAB fusion blocks transcription | Temporary gene repression; studies of essential genes without cell death [57] | Avoids double-strand breaks; reversible phenotype |
| CRISPR Activation (CRISPRa) | dCas9-activator fusion enhances transcription | Gain-of-function screening; identifies genes conferring resistance when overexpressed [57] | Reveals mechanisms missed by knockout screens |
| Base Editing | Cas9 nickase-deaminase fusion installs point mutations | Saturation mutagenesis of specific domains; models resistance variants [58] | Creates precise single nucleotide changes without double-strand breaks |
| Prime Editing | Cas9-reverse transcriptase fusion edits without DSBs | Installation of desired edits without donor templates [56] | High precision with minimal indels |
Integrated Screening Workflow
The general workflow for CRISPR screens begins with generation of cells stably expressing the desired CRISPR construct, typically via lentiviral delivery. Cells are expanded to adequate population size for genome-wide representation, then segregated into drug-treated and non-treated control groups. Following selection, genomic DNA is extracted, sgRNAs are PCR-amplified, and sequencing is performed. Bioinformatics analysis utilizes tools such as MAGeCK, STARS, or PinAPL-Py to identify significantly enriched or depleted sgRNAs [57].
Base editing screens have proven particularly valuable for prospectively identifying genetic mechanisms of resistance to oncology drugs. These approaches can define the genetic landscape of cancer drug resistance mechanisms by installing specific variants in cancer genes and assessing their functional impact under therapeutic selection [58]. Such screens have identified four functional classes of variants modulating drug sensitivity: (1) drug addiction variants that confer proliferation advantage only in drug presence but are deleterious without drug; (2) canonical drug resistance variants conferring advantage only with drug; (3) driver variants conferring advantage regardless of drug presence; and (4) drug-sensitizing variants that are deleterious only with drug [58].
Integrated Experimental Design: Converging Single-Cell Omics with CRISPR Screens
The strategic integration of single-cell omics with CRISPR screening creates a powerful framework for mapping gene function to cellular phenotypes at unprecedented resolution. Two primary approaches enable this convergence:
Perturb-seq Framework
Perturb-seq combines CRISPR-based perturbations with single-cell RNA sequencing readouts, enabling high-resolution mapping of gene regulatory networks and cellular responses [56]. The experimental protocol involves:
- Library Design and Cloning: Select sgRNAs targeting genes of interest and clone into lentiviral backbone with appropriate promoters.
- Lentivirus Production: Generate lentiviral particles in HEK293T cells using standard packaging plasmids.
- Cell Infection and Selection: Infect target cells at low MOI (0.3-0.5) to ensure single integration events, followed by antibiotic selection.
- Single-Cell Partitioning and Library Prep: Harvest cells and load onto single-cell partitioning system (10× Genomics Chromium). Prepare libraries per manufacturer protocol with modified amplification to preserve sgRNA representation.
- Sequencing and Analysis: Sequence libraries on Illumina platform (minimum 20,000 reads/cell for transcriptome, 100x coverage for sgRNAs). Process data with Cell Ranger and custom pipelines to link sgRNAs to transcriptional phenotypes.
This approach has been instrumental in revealing how CSC-specific vulnerabilities operate through distinct mechanisms, including eliciting drug-addicted cell states [58].
Functional Validation Workflow
For candidate genes identified through integrated analysis, the following validation protocol is recommended:
Arrayed CRISPR-Cas9 Mediated Gene Knockout in CSCs:
- Isolate CSCs using established markers (CD44, CD133, ALDH) or functional assays.
- Design and synthesize sgRNAs targeting top candidate genes alongside non-targeting controls.
- Transfect CSCs with ribonucleoprotein (RNP) complexes of Cas9 and sgRNAs using electroporation.
- Validate editing efficiency (48-72h post-editing) via T7E1 assay or next-generation sequencing.
- Assess functional phenotypes:
- Self-renewal: Limiting dilution sphere formation assays in ultra-low attachment plates
- Chemoresistance: IC50 determination via CellTiter-Glo viability assays
- Differentiation: Flow cytometry for differentiation markers
- In vivo tumorigenesis: Limiting dilution transplantation in immunocompromised mice
Research Reagent Solutions
Table 3: Essential Research Reagents for Integrated Single-Cell and CRISPR Approaches
| Reagent Category | Specific Products/Systems | Key Applications | Technical Notes |
|---|---|---|---|
| Single-Cell Platforms | 10× Genomics Chromium, Fluidigm C1, Dolomite Bio Nadia | Partitioning cells for RNA-seq | 10× supports high-throughput; C1 offers full-length transcripts [55] |
| CRISPR Enzymes | Wild-type SpCas9, Base editors (CBE, ABE), Prime editors | Gene knockout, precise editing, transcriptional modulation | Base editors enable point mutations without double-strand breaks [56] [58] |
| sgRNA Libraries | Brunello, GeCKO v2, Custom target-specific libraries | Genome-wide and focused screens | Optimized sgRNA designs reduce off-target effects [57] |
| Delivery Systems | Lentiviral particles, Lipid nanoparticles (LNPs), Electroporation | Introducing CRISPR components | LNPs show promise for in vivo delivery [60] |
| Bioinformatics Tools | Cell Ranger, Seurat, Scanpy, MAGeCK, STARS | Data processing and analysis | Specialized support needed for computational analysis [55] [57] |
The integration of single-cell multi-omics platforms with CRISPR-based functional genomics represents a transformative approach for dissecting CSC biology. These technologies have enabled a paradigm shift from viewing CSCs as static entities defined by surface markers to understanding them as dynamic cellular states shaped by transcriptional, epigenetic, and microenvironmental influences [54]. This refined perspective is critical for developing innovative therapeutic strategies that disrupt CSC plasticity, niche adaptation, and immune evasion.
Looking forward, several emerging areas promise to further advance CSC research. The development of more sophisticated Cas variants with reduced off-target effects and expanded targeting ranges will enhance the precision of genetic screens [56]. Improvements in single-cell multi-omics now enable simultaneous profiling of transcriptome, epigenome, and surface proteins from the same cell, providing more comprehensive views of CSC states [54] [55]. Additionally, spatial transcriptomics technologies are mapping CSC localization and niche interactions within tissue architecture, while advanced computational methods, particularly artificial intelligence-driven predictive modeling, are extracting deeper insights from complex multi-omics datasets [54].
As these technologies mature and converge, they pave the way for cross-cancer CSC plasticity atlases that integrate single-cell profiling with spatial and functional omics to guide future therapeutic strategies. By providing unprecedented resolution into the molecular mechanisms driving CSC maintenance and therapeutic resistance, these integrated approaches offer renewed hope for developing precision medicine strategies that effectively target the root causes of tumor recurrence and treatment failure.
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [1]. Their ability to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies [1]. The CSC model has revolutionized our understanding of tumor biology by challenging the traditional view that all cancer cells contribute equally to tumor development, progression, and recurrence [18]. This paradigm shift is particularly relevant for addressing therapeutic resistance, as CSCs possess enhanced survival mechanisms, including robust DNA repair systems, drug efflux transporters, and the capacity for quiescence, allowing them to survive conventional therapies that target rapidly dividing cells [1] [18].
Patient-derived organoids (PDOs) and three-dimensional (3D) culture systems have emerged as transformative technologies that bridge the critical gap between conventional two-dimensional (2D) cell cultures and in vivo models [61] [62]. These innovative platforms faithfully recapitulate the histoarchitecture, genetic stability, and phenotypic complexity of primary tumors while preserving the CSC populations responsible for tumor maintenance and therapeutic resistance [63]. By maintaining cancer stem cell hierarchies and clonal subpopulations, PDOs enable researchers to investigate CSC-driven intratumoral heterogeneity, drug resistance mechanisms, and tumor-stroma interactions with unprecedented fidelity [1] [63]. The integration of these advanced models into cancer research represents a pivotal advancement in precision oncology, offering powerful tools for drug screening, biomarker discovery, and the development of CSC-targeted therapies aimed at overcoming treatment resistance and preventing tumor recurrence [18] [64].
The Biological Foundation: Cancer Stem Cells and Tumor Heterogeneity
Defining Characteristics of Cancer Stem Cells
Cancer stem cells exhibit three fundamental properties that distinguish them from the bulk tumor population and underpin their critical role in tumor progression and treatment resistance. Self-renewal allows CSCs to maintain their population over time through symmetric division (producing two identical CSCs) or asymmetric division (producing one CSC and one differentiated daughter cell) [18]. This capacity for perpetual self-replication ensures long-term tumor maintenance and regenerative potential after therapeutic intervention. Differentiation potential enables CSCs to give rise to the heterogeneous lineages of cancer cells that constitute the tumor mass, thereby driving cellular diversity and functional complexity within neoplasms [18]. Therapy resistance, perhaps the most clinically relevant characteristic, allows CSCs to survive conventional treatments through multiple mechanisms, including enhanced DNA repair capability, upregulated drug efflux transporters (particularly ABC transporters like ABCG2), metabolic plasticity, and dormancy (quiescence) that protects them from therapies targeting proliferating cells [1] [18] [65].
Table 1: Key Characteristics of Cancer Stem Cells Versus Regular Cancer Cells
| Characteristic | Cancer Stem Cells (CSCs) | Regular Cancer Cells |
|---|---|---|
| Self-renewal | Can self-renew, maintaining their population over time through symmetric and asymmetric division | Limited or no self-renewal capability |
| Differentiation | Can differentiate into multiple cell types within the tumor, contributing to cellular diversity | Limited differentiation potential, typically forming homogeneous populations |
| Transdifferentiation | Can undergo transdifferentiation into different cell types (e.g., endothelial cells) to support tumor growth | Rarely exhibit transdifferentiation capability |
| Therapy Resistance | Highly resistant to chemotherapy and radiation through multiple mechanisms | More susceptible to conventional therapies |
| Tumor Initiation | Capable of initiating and sustaining tumor growth with high tumorigenic potential | Limited tumor-initiating capacity |
| Metabolic Profile | Exhibit metabolic plasticity, switching between glycolysis, oxidative phosphorylation, and alternative fuel sources | Typically maintain consistent metabolic programming |
CSC Signaling Pathways and Therapeutic Targets
The fundamental properties of CSCs are regulated by an intricate network of evolutionarily conserved signaling pathways that represent promising targets for therapeutic intervention. The Wnt/β-catenin pathway plays a crucial role in maintaining CSC self-renewal, particularly in gastrointestinal cancers [18]. When Wnt ligands bind to Frizzled receptors and LRP co-receptors, β-catenin accumulates and translocates to the nucleus, activating transcription of genes involved in stemness maintenance. The Notch signaling pathway regulates cell fate decisions and contributes to therapy resistance in various cancers, including breast cancer [65]. Upon ligand binding, Notch receptors undergo proteolytic cleavage, releasing the Notch intracellular domain (NICD) that translocates to the nucleus to activate target genes. The Hedgehog (Hh) pathway is critical for tissue patterning and stem cell maintenance, with aberrant activation observed in basal cell carcinoma and other malignancies [18]. Additionally, PI3K/AKT/mTOR signaling integrates environmental cues to regulate CSC metabolism, survival, and proliferation, while TGF-β/SMAD signaling facilitates epithelial-mesenchymal transition (EMT), enhancing CSC plasticity and metastatic potential [65].
CSC-Microenvironment Interactions
CSCs reside within specialized niches in the tumor microenvironment (TME) that provide critical signals for their maintenance and protection [1]. These dynamic interactions involve multiple cellular components, including cancer-associated fibroblasts (CAFs) that secrete growth factors and remodel the extracellular matrix (ECM), immune cells such as tumor-associated macrophages (TAMs) that can adopt immunosuppressive phenotypes, and endothelial cells that form vascular niches supporting CSC maintenance [65]. Non-cellular components, particularly the extracellular matrix, provide not only structural support but also biochemical and biophysical cues that influence CSC behavior through integrin-mediated signaling and mechanotransduction pathways [62]. The hypoxic conditions often found in CSC niches stabilize hypoxia-inducible factors (HIFs), which further promote stemness and therapeutic resistance [66]. This complex network of microenvironmental interactions represents a formidable barrier to effective cancer therapy and underscores the importance of developing models that accurately recapitulate these dynamics.
3D Culture Technologies: Methodologies and Applications
Comparative Analysis of 3D Culture Platforms
The limitations of conventional 2D cultures in modeling the tumor microenvironment and CSC niches have driven the development of sophisticated 3D culture systems that better recapitulate in vivo conditions [62]. These platforms vary in complexity, physiological relevance, and technical requirements, each offering distinct advantages for specific research applications.
Table 2: Comparison of 3D Culture Technologies for Cancer Research
| Technology | Key Features | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Scaffold-Based Hydrogels (Matrigel, BME, synthetic hydrogels) | Porous 3D structure simulating ECM; supports cell growth and signaling [61] | CSC expansion, drug screening, differentiation studies | Excellent biochemical support; tunable properties; commercial availability | Batch-to-batch variability (natural hydrogels); potential immunogenicity |
| Suspension Drop Culture | Gravity-driven cell aggregation in hanging droplets [61] | Spheroid formation, preliminary drug testing | Simple setup; no specialized equipment required; low cost | Limited scale-up capacity; challenging media exchange; small spheroid size |
| Rotating Cell Culture Systems (RCCS) | Simulated microgravity environment; minimal shear stress [61] | Large spheroid generation, tissue engineering | Uniform nutrient distribution; enhanced cell viability; scalable | Specialized equipment required; higher cost; technical complexity |
| 3D Bioprinting | Layer-by-layer deposition of bioinks containing cells and biomaterials [61] [64] | Personalized tumor models, TME engineering, vascularized models | High precision; spatial control; customizable architecture; patient-specific | High cost; technical expertise required; limited resolution for small features |
| Microfluidic Organoid-on-Chip | Microscale channels and chambers simulating fluid flow and mechanical forces [67] [64] | Metastasis studies, immune-oncology, high-throughput screening | Controlled microenvironments; gradient generation; integration with sensors | Design complexity; specialized equipment; potential bubble formation |
Establishing Patient-Derived Organoids: Detailed Workflow
The generation of PDOs involves a multi-step process that maintains the cellular heterogeneity and CSC populations of the original tumor [68]. The success of PDO establishment depends critically on careful execution at each stage, from sample acquisition to functional characterization.
Sample Acquisition and Processing: Patient-derived organoids can be generated from various sources, including surgical specimens, biopsies, or biological fluids such as ascites and blood [68]. The sample processing begins with meticulous mechanical and/or enzymatic dissociation to create a suspension of single cells or small aggregates while preserving cellular viability. The specific enzymatic cocktail (e.g., collagenase, dispase) and digestion time must be optimized for each tumor type to balance yield and viability. For samples with significant stromal contamination, differential centrifugation or filtration steps may be incorporated to enrich for epithelial components [68].
Matrix Embedding and Culture Initiation: The dissociated cells are subsequently embedded in an extracellular matrix dome, typically using commercial preparations like Matrigel or BME, which provide a basal membrane-rich environment conducive to 3D growth [68]. Recent advances have introduced defined synthetic hydrogels based on polymers such as polyethylene glycol (PEG) or poly(lactic-co-glycolic acid) (PLGA) to improve reproducibility and reduce batch variability [68]. The embedded cells are then overlaid with a specialized, tissue-specific medium containing a precise combination of growth factors and pathway modulators. Essential components typically include Wnt pathway agonists (R-spondin, Wnt3a), epidermal growth factor (EGF), Noggin (a BMP antagonist), and other niche-specific factors that support stem cell maintenance and proliferation [68].
Medium Formulation and Optimization: The culture medium composition must be carefully optimized for each cancer type and accounts for the specific mutational profile of the tumor. For instance, colorectal cancers with activating mutations in the Wnt pathway may not require exogenous Wnt agonists, while tumors with EGFR pathway mutations might be cultured without EGF supplementation [68]. Advanced culture systems, such as the air-liquid interface (ALI) method, can maintain microenvironment components, including fibroblasts and immune cells, for extended periods [68]. This approach involves finely slicing tissue and coating it with collagen before deposition on a filter with growth factor-poor media, preserving native stromal interactions for up to one month [68].
Expansion and Quality Control: Once established, PDOs can be dissociated and reseeded for amplification, typically every 1-3 weeks depending on the growth rate. Quality control assessments include histological analysis to verify recapitulation of original tumor architecture, genetic profiling to confirm maintenance of driver mutations, and functional assays to demonstrate preservation of CSC activity through sphere-forming assays or in vivo tumorigenicity studies [68] [63]. Successful PDO cultures can be cryopreserved for long-term biobanking, enabling the creation of extensive collections that capture inter- and intra-tumor heterogeneity [68].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents for PDO and 3D Culture Establishment
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Extracellular Matrices | Matrigel, BME, synthetic PEG-based hydrogels, collagen I, fibrin [68] | Provide 3D structural support; present biochemical and biophysical cues | Natural matrices show batch variability; synthetic matrices offer tunable properties |
| Growth Factors & Cytokines | EGF, R-spondin, Wnt3a, Noggin, FGF10, N2/B27 supplements [68] | Support stem cell maintenance and proliferation; direct differentiation | Concentration optimization required for different cancer types |
| Signaling Pathway Modulators | A83-01 (TGF-β inhibitor), Y-27632 (ROCK inhibitor), CHIR99021 (GSK-3 inhibitor) [68] | Enhance cell survival; maintain stemness; inhibit differentiation | Particularly important during initial establishment and passaging |
| Dissociation Reagents | Collagenase, dispase, accutase, trypsin-EDTA [68] | Tissue disaggregation; organoid passaging | Enzyme concentration and duration must be optimized to preserve viability |
| Cell Culture Media | Advanced DMEM/F12, William's E Medium [68] | Base medium providing essential nutrients and salts | Supplementation varies by cancer type and research objectives |
| Characterization Reagents | CellTiter-Glo, CCK-8, Calcein-AM/EthD-1 (live/dead staining) [68] | Assess viability, proliferation, and drug response | 3D-optimized protocols required for accurate quantification |
Applications in Cancer Research and Drug Development
Modeling Therapy Resistance and Tumor Recurrence
PDOs have emerged as powerful tools for investigating CSC-mediated therapy resistance and tumor recurrence mechanisms. These models faithfully recapitulate the drug tolerance observed in clinical settings, particularly the contributions of CSCs to treatment failure [61] [65]. In breast cancer, BCSCs demonstrate robust resistance through multiple mechanisms, including overexpression of ATP-binding cassette (ABC) transporters like ABCG2 that actively efflux chemotherapeutic agents, enhanced DNA repair capacity, activation of pro-survival signaling pathways (PI3K/AKT, Notch, Hedgehog), and interactions with protective niche components within the TME [65]. PDOs enable researchers to dissect these resistance mechanisms in a physiologically relevant context and identify strategies to overcome them. For instance, studies using PDOs have revealed that matrix stiffness through CD44-mediated mechanosignaling can induce chemoresistance in pancreatic ductal adenocarcinoma organoids, and that disrupting this signaling can resensitize tumors to treatment [64].
High-Throughput Drug Screening and Personalized Medicine
The implementation of PDOs in drug discovery has transformed preclinical screening paradigms by providing more predictive models for therapeutic efficacy [61] [64]. Traditional 2D screening platforms often fail to identify compounds effective against CSC populations, contributing to the high attrition rate of oncology drugs in clinical trials [62]. Advanced 3D platforms, including microfluidic-based devices that miniaturize PDO cultures into 384-well formats, now enable high-throughput compound screening while maintaining the cellular heterogeneity and TME interactions critical for accurate response prediction [64]. These systems allow for simultaneous assessment of drug effects on both differentiated cancer cells and therapy-resistant CSCs, facilitating the identification of agents that effectively target the root drivers of tumor maintenance and recurrence. In functional precision oncology approaches, PDO drug sensitivity testing has been successfully integrated with genomic analysis to guide personalized treatment decisions for cancer patients, with ongoing clinical studies validating this strategy for multiple cancer types including metastatic colorectal cancer and recurrent glioblastoma [64].
Investigating Tumor Heterogeneity and Clonal Evolution
The capacity of PDOs to preserve the genetic and phenotypic diversity of original tumors makes them invaluable tools for studying tumor heterogeneity and clonal dynamics [63]. Through serial passaging and single-cell analysis, researchers can track the evolution of CSC subpopulations under selective pressures such as therapeutic interventions or microenvironmental changes [1]. This approach has revealed the remarkable plasticity of non-CSCs, which can regain stem-like properties through dedifferentiation processes in response to environmental cues [66]. In prostate and lung cancer models, PDOs have been instrumental in characterizing neuroendocrine differentiation, a resistance mechanism whereby adenocarcinoma cells transform into aggressive neuroendocrine variants in response to targeted therapies like androgen deprivation or EGFR inhibition [66]. The faithful maintenance of CSC hierarchies in PDO cultures enables researchers to reconstruct phylogenetic relationships between subclones and identify the molecular drivers of lineage plasticity and phenotype switching.
Current Challenges and Future Directions
Technical Limitations and Standardization Needs
Despite their significant advantages, PDO and 3D culture technologies face several challenges that must be addressed to maximize their translational impact. Protocol variability across laboratories and cancer types remains a substantial hurdle, complicating data comparison and reproducibility [63]. The development of standardized, Good Manufacturing Practice (GMP)-compliant manufacturing protocols will be essential for clinical integration. Incomplete microenvironment recapitulation, particularly the absence of vascularization, neural input, and systemic immune components, limits the physiological relevance of current PDO models [68] [63]. While co-culture systems incorporating fibroblasts, immune cells, and endothelial elements have shown promise, creating fully functional tissue contexts remains challenging. Scalability and throughput limitations, though improving with microfluidic and bioprinting technologies, still restrict the widespread implementation of PDOs in large-scale drug discovery campaigns [64]. Additionally, the selection bias during PDO establishment may favor the expansion of certain subclones while underrepresenting others, potentially altering the original tumor's cellular composition and heterogeneity [68].
Emerging Technologies and Innovative Solutions
The convergence of bioengineering, multi-omics, and computational biology is driving the development of next-generation PDO platforms with enhanced physiological relevance and analytical capabilities. Organoid-on-chip systems integrate microfluidic technology with PDO cultures to introduce dynamic fluid flow, mechanical forces, and multi-tissue interactions that better mimic in vivo conditions [67] [64]. These platforms enable sophisticated studies of metastasis, immune cell trafficking, and pharmacokinetic/pharmacodynamic relationships. Vascularized organoid models incorporating endothelial cells and perfusion systems address the critical limitation of nutrient diffusion, supporting the growth of larger, more complex structures and enabling studies of angiogenesis and intravasation [64]. Advanced biomaterials with tunable mechanical and biochemical properties allow researchers to decouple the individual contributions of matrix stiffness, ligand density, and degradability to CSC behavior and drug resistance [64]. CRISPR-based functional genomics in PDOs provides powerful tools for conducting genetic screens to identify novel vulnerabilities and resistance mechanisms in a physiologically relevant context [1] [63]. Finally, AI-driven multi-omics integration combines high-content imaging, transcriptomic, proteomic, and drug response data to identify predictive biomarkers and optimize personalized treatment strategies [63].
Clinical Translation and Regulatory Considerations
The progressive validation of PDOs as predictive biomarkers for treatment response is accelerating their integration into clinical oncology workflows [64]. Prospective clinical studies are currently evaluating the utility of PDO-based functional testing for guiding therapy selection in various malignancies, with preliminary results demonstrating promising correlation between ex vivo drug sensitivity and patient clinical responses [64]. However, several translational challenges remain, including the timeline constraints for PDO establishment and drug testing, which must align with clinical decision-making schedules, particularly in rapidly progressive diseases. Success rate variability in PDO generation across different cancer types and sample qualities necessitates optimized protocols for reliable culture establishment [68]. The development of regulatory frameworks for validating PDO-based diagnostic applications will require extensive clinical correlation studies and standardization of analytical performance characteristics. Additionally, ethical considerations surrounding patient tissue usage, data privacy, and the potential use of PDOs for germline gene editing warrant ongoing discussion and guideline development as these technologies advance toward routine clinical implementation [63].
Patient-derived organoids and advanced 3D culture systems represent a paradigm shift in preclinical cancer modeling, offering unprecedented opportunities to study cancer stem cell biology, tumor heterogeneity, and therapeutic resistance in physiologically relevant contexts. By faithfully maintaining CSC hierarchies and their functional properties, these innovative platforms bridge the critical gap between traditional 2D cultures and in vivo models, enabling more accurate prediction of drug responses and facilitating the development of novel therapeutic strategies targeting the root causes of tumor recurrence and metastasis. While challenges related to standardization, scalability, and complete microenvironment recapitulation remain, the rapid integration of bioengineering, computational, and omics technologies continues to enhance the capabilities and translational relevance of these models. As validation studies progressively demonstrate their clinical predictive value, PDOs are poised to become indispensable tools in precision oncology, driving the development of more effective, CSC-targeted therapies and ultimately improving outcomes for cancer patients.
Conquering CSC-Mediated Drug Resistance: Mechanisms and Counter-Strategies
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with the capacity for self-renewal, differentiation, and enhanced therapy resistance. These cells are now recognized as a fundamental source of intratumoral heterogeneity and the primary cause of treatment failure, tumor recurrence, and metastasis in many cancer types [4] [1]. Their resilience stems from intrinsic resistance mechanisms that enable survival under therapeutic pressure. Among these mechanisms, quiescence, enhanced DNA repair, and apoptosis evasion constitute a core triad that protects CSCs from conventional chemo- and radiotherapies, which typically target rapidly dividing cells [5] [69]. This whitepaper provides an in-depth technical analysis of these three core mechanisms, framing them within the broader context of CSC-driven tumor heterogeneity and drug resistance. It is intended to equip researchers and drug development professionals with current mechanistic insights, experimental methodologies, and emerging targeting strategies.
Core Mechanisms of Intrinsic Resistance
Quiescence: The Dormant Survival Strategy
Quiescence, a reversible state of cell cycle arrest (G0 phase), is a key survival strategy employed by CSCs [5]. This dormant state allows them to persist during treatment with cytotoxic agents designed to kill actively proliferating cells.
Molecular Regulation and Associated Markers: The quiescent state is maintained by complex molecular regulation. The Fbxw7 protein plays a crucial role in maintaining leukemic CSC quiescence; its genetic ablation has been shown to push cells into the cell cycle, sensitizing them to imatinib treatment [5]. Furthermore, the HIF2α-CITED2 axis, particularly in leukemic CSCs, is a critical modulator of quiescence and stemness, and can be inhibited by peroxisome proliferator-activated receptor-γ (PPARγ) agonists [5]. In solid tumors, CSCs marked by CD24 expression have been observed to be more quiescent and possess greater tumorigenic potential, with their presence upregulated in residual tumors following cisplatin treatment [4]. CD49f (ITGA6) has also been associated with radiation therapy resistance, further underscoring the link between specific surface markers and the quiescent, therapy-resistant phenotype [4].
Table 1: Key Molecular Regulators of CSC Quiescence
| Regulator/Marker | Function in Quiescence | Experimental Evidence |
|---|---|---|
| Fbxw7 | Maintains quiescence in leukemic CSCs | Fbxw7 depletion + imatinib combinational therapy attenuated leukemia development [5]. |
| HIF2α/CITED2 | Key modulators of quiescence and stemness | PPARγ agonists decrease their expression, inhibiting quiescence [5]. |
| CD24 | Marker for quiescent, tumorigenic cells | CD24+ cells are more quiescent and enriched in cisplatin-resistant tumors [4]. |
| CD49f (ITGA6) | Associated with therapy-resistant populations | CD49f+ population mediates radiation and taxane resistance [4]. |
Enhanced DNA Repair: Fortifying Genomic Integrity
CSCs possess enhanced DNA damage response (DDR) and repair capabilities, enabling them to efficiently rectify DNA lesions induced by radio- and chemotherapy [1] [5]. This proficiency is a major contributor to intrinsic resistance.
Constitutive Activation and Key Pathways: In glioblastoma CSCs, the DNA damage response is constitutively activated due to higher levels of replicative stress, priming them for rapid repair of therapy-induced damage [5]. Key pathways involved include those mediated by ALDH1, which has been correlated with platinum resistance in ovarian and esophageal cancers by regulating cell cycle checkpoints and the DNA repair pathway [4]. The Hippo/YAP1 signaling pathway also strongly mediates chemo- and radiation resistance in gastroesophageal cancers through the upregulation of DNA repair and survival genes [4].
Therapeutic Targeting: Inhibiting the DNA damage checkpoint pathway is a promising strategy to target CSCs. For instance, the combination of YAP1 and RAF or MEK inhibition has been shown to be synthetically lethal, enhancing treatment response [4].
Diagram 1: Enhanced DNA damage response and repair mechanisms in CSCs. Key pathways like ALDH1 and YAP1 provide resistance, creating vulnerabilities for targeted inhibitors.
Apoptosis Evasion: Subverting Cell Death
Evading programmed cell death is a hallmark of cancer, and CSCs have evolved multiple strategies to resist apoptosis, a primary mechanism of action for many chemotherapeutic drugs [4] [69].
Key Mechanisms of Evasion: CSCs can turn off apoptotic pathways, providing a direct survival advantage [4]. The Hippo/YAP1 pathway is a central hub, not only in DNA repair but also in promoting cell survival and resisting apoptosis. YAP1 mediates chemo- and radiation resistance by upregulating pro-survival genes such as EGFR and CDK6 in esophageal cancer [4]. Furthermore, the detoxifying enzyme ALDH1 is highly expressed in CSCs and contributes to therapy resistance by alleviating the toxic effects of reactive oxygen species (ROS) and providing time for DNA repair, indirectly promoting survival [4].
Table 2: Apoptosis Evasion Mechanisms in CSCs
| Mechanism | Molecular Players | Functional Outcome |
|---|---|---|
| Pro-survival Signaling | YAP1 (upregulating EGFR, CDK6) | Promotes cell survival and proliferation despite genotoxic stress [4]. |
| Detoxification | ALDH1 (detoxification of aldehydes, ROS management) | Reduces intracellular concentration of toxic chemotherapeutic intermediates [4]. |
| Apoptotic Pathway Downregulation | Downregulation of pro-apoptotic proteins | Directly inhibits the execution phase of apoptosis [4]. |
Experimental Protocols for Studying Intrinsic Resistance
Analyzing Quiescence and Cell Cycle Status
Protocol: Combining Label-Retaining Cell (LRC) Assays with Flow Cytometry
- Pulse-Chase Labeling: Cells are pulsed with a fluorescent dye like CFSE (Carboxyfluorescein succinimidyl ester) or BrdU (Bromodeoxyuridine) for a defined period (e.g., 48-72 hours). This "pulse" incorporates the label into proliferating cells.
- Chase Period: The dye-containing medium is removed and replaced with fresh medium. The cells are then cultured for an extended "chase" period (e.g., 7-14 days). Actively dividing cells dilute the label with each division.
- Cell Sorting and Analysis: After the chase, cells are analyzed via flow cytometry. The Label-Retaining Cells (LRCs), which maintain high fluorescence intensity, represent the quiescent (or slow-cycling) population. These LRCs can be sorted for downstream functional assays.
- Cell Cycle Profiling: Sorted LRCs and non-LRCs can be stained with a DNA-binding dye like Propidium Iodide (PI) or DAPI and analyzed by flow cytometry to confirm their accumulation in the G0/G1 phase of the cell cycle.
- Functional Validation: The tumor-initiating potential and therapy resistance of sorted LRCs versus non-LRCs are validated using in vivo limiting dilution assays and in vitro drug treatment assays, respectively [5].
Assessing DNA Damage Response and Repair Capacity
Protocol: Immunofluorescence Analysis of DNA Repair Foci
- Treatment and Fixation: Cells (both CSC and non-CSC populations) are treated with a DNA-damaging agent (e.g., ionizing radiation, cisplatin). Untreated cells serve as a control. At specific time points post-treatment (e.g., 1, 6, 24 hours), cells are fixed with paraformaldehyde.
- Immunostaining: Fixed cells are permeabilized and immunostained with antibodies against DNA damage and repair markers.
- Primary Antibodies: Anti-γ-H2AX (marks DNA double-strand breaks), anti-53BP1 or anti-RAD51 (key proteins in DNA repair pathways).
- Microscopy and Quantification: Cells are visualized using confocal microscopy. The number of γ-H2AX foci per nucleus is quantified before and after damage induction. A faster rate of foci resolution in CSCs compared to non-CSCs indicates enhanced DNA repair capacity [5]. The co-localization of γ-H2AX with 53BP1 or RAD51 can provide insights into the specific repair pathway employed.
Evaluating Apoptosis Evasion
Protocol: Annexin V/PI Staining Combined with CSC Markers
- Therapy Challenge: CSC-enriched populations (e.g., tumorspheres) and bulk cancer cells are exposed to a relevant chemotherapeutic drug (e.g., cisplatin, paclitaxel) at their respective IC50 concentrations for a defined period.
- Staining for Apoptosis and CSCs: After treatment, cells are harvested and stained with:
- Fluorochrome-conjugated antibodies against CSC surface markers (e.g., anti-CD44, anti-CD133) to identify the CSC subpopulation.
- Annexin V-FITC and Propidium Iodide (PI), following the manufacturer's protocol. This allows discrimination between live (Annexin V-/PI-), early apoptotic (Annexin V+/PI-), late apoptotic (Annexin V+/PI+), and necrotic (Annexin V-/PI+) cells.
- Flow Cytometry Analysis: Using multicolor flow cytometry, the percentage of apoptotic cells (Annexin V+) within the CSC marker-positive and CSC marker-negative gates is determined. A significantly lower percentage of apoptosis in the CSC-marked population confirms their enhanced ability to evade cell death [4] [69].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying CSC Intrinsic Resistance
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| CSC Markers (Antibodies) | Anti-CD133, Anti-CD44, Anti-CD24, Anti-ALDH1 | Identification and isolation of CSC subpopulations via Flow Cytometry or Immunostaining [4]. |
| Cell Cycle & Quiescence Tracking | CFSE, BrdU, Ki-67 Antibody, Propidium Iodide | Label-retaining assays to track cell division and identify quiescent (G0) populations [5]. |
| DNA Damage & Repair Assays | Anti-γ-H2AX, Anti-53BP1, Anti-RAD51 | Quantification of DNA double-strand breaks and repair kinetics via immunofluorescence [5]. |
| Apoptosis Detection | Annexin V Conjugates, Propidium Iodide, Caspase-3/7 Activity Assays | Discrimination and quantification of apoptotic cell stages [4] [69]. |
| Key Pathway Inhibitors | ALDH1 Inhibitors (e.g., DEAB), YAP1 Inhibitors (e.g., Verteporfin), DDR Inhibitors (e.g., ATMi) | Functional validation of mechanisms and potential therapeutic agents [4] [5]. |
| Functional Assay Kits | Aldefluor Assay Kit, Tumorsphere Culture Media, ATP-based Viability Assays (e.g., CellTiter-Glo) | Assessment of stemness properties, self-renewal capacity, and cell viability post-treatment [4] [5]. |
Diagram 2: The consequence of intrinsic resistance. Therapy selectively kills bulk tumor cells but enriches for CSCs, which survive via quiescence, enhanced DNA repair, and apoptosis evasion, ultimately leading to relapse.
The intrinsic resistance mechanisms of quiescence, enhanced DNA repair, and apoptosis evasion form a robust defensive triad that secures the survival of CSCs through various cancer therapies. This survival underpins tumor recurrence and contributes significantly to the dynamic heterogeneity of tumors. Future research must focus on developing agents that target these specific vulnerabilities—such as forcing CSCs out of quiescence, inhibiting key DNA repair components, or reactivating apoptotic pathways—and effectively integrating these agents into combination therapies. Successfully targeting these core pillars of CSC resistance is paramount to achieving durable therapeutic responses and improving patient outcomes in oncology.
Multidrug resistance (MDR) remains a paramount obstacle in successful cancer chemotherapy, largely orchestrated by the overexpression of ATP-binding cassette (ABC) transporters in cancer cells, particularly within the cancer stem cell (CSC) subpopulation. This technical guide delineates the role of ABC transporters—with a focus on ABCG2—in fostering the resilient CSC phenotype, details the mechanisms underlying their efflux capabilities, and synthesizes current and emerging tactical approaches to inhibit their function. Framed within the context of tumor heterogeneity and CSC-driven resistance, this whitepaper provides a comprehensive resource for researchers and drug development professionals, integrating quantitative data summaries, experimental protocols, and strategic visualizations to advance the development of effective, targeted therapies.
Tumors are not homogeneous masses but complex ecosystems composed of genetically and functionally distinct subclones [70]. The cancer stem cell (CSC) model posits that a hierarchical organization exists within this heterogeneity, with a small population of slow-cycling CSCs at the apex. These CSCs are endowed with enhanced tumorigenic potential, self-renewal capabilities, and intrinsic resistance to conventional and targeted therapies [70] [71]. Consequently, CSCs are implicated in disease progression and relapse, as they are often able to survive chemotherapy and repopulate the tumor.
A key molecular mechanism conferring this resistant phenotype is the increased expression and activity of ABC transporters [70] [71]. These transmembrane proteins utilize ATP hydrolysis to actively efflux a wide spectrum of structurally unrelated chemotherapeutic agents from the cell, leading to multidrug resistance. Overexpression of specific ABC transporters, notably ABCG2 (BCRP), ABCB1 (P-gp), and ABCC1 (MRP1), has been consistently reported in CSCs isolated from various cancers [70] [72] [73]. Therefore, understanding and targeting these efflux pumps is a critical frontier in overcoming therapeutic failure and preventing recurrence in cancer treatment.
Mechanistic Foundations of ABC Transporter-Mediated Efflux
ABC transporters constitute one of the largest families of transmembrane proteins, with 48 members in humans classified into seven subfamilies (ABCA–ABCG) [70] [72]. They share a conserved core architecture consisting of four domains:
- Two Transmembrane Domains (TMDs): These domains, each typically comprising six alpha-helices, form the passageway through the lipid bilayer and contain the substrate-binding pockets.
- Two Nucleotide-Binding Domains (NBDs): These cytosolic domains bind and hydrolyze ATP, providing the energy required for the conformational changes that drive substrate translocation [72] [74].
The transport cycle involves the binding of substrates to the TMDs, followed by ATP binding and hydrolysis at the NBDs. This energy input triggers a conformational shift from an inward-facing, high-affinity substrate-binding state to an outward-facing, low-affinity state that releases the substrate outside the cell or into extracellular compartments [72].
ABCG2: A Key Efflux Transporter in CSCs
ABCG2 is a half-transporter that must homodimerize to form a functional unit. It is highly expressed in normal tissues with barrier or secretory functions, such as the placenta, blood-brain barrier, and intestinal epithelium, where it plays a protective role by excluding xenobiotics [74] [73]. In oncology, its significance is profound due to its broad substrate profile, which includes:
- Chemotherapeutic agents: Mitoxantrone, topotecan, irinotecan/SN-38, methotrexate, and tyrosine kinase inhibitors (e.g., gefitinib, erlotinib, imatinib) [74] [73].
- Photosensitizers used in photodynamic therapy, such as pheophorbide a and porfimer sodium [73].
- Endogenous compounds: Uric acid, protoporphyrin IX, and steroid conjugates [74].
In CSCs, high ABCG2 activity contributes to the "side population" (SP) phenotype, a key functional marker for stem-like cells. This phenotype is identified via flow cytometry using fluorescent dyes like Hoechst 33342, which is effluxed by ABCG2 [70] [73]. Cells within the SP demonstrate enhanced tumorigenicity and are resistant to multiple drugs, underscoring the link between ABCG2 and the CSC phenotype.
Table 1: Key ABC Transporters Implicated in Cancer Stem Cell Multidrug Resistance
| Transporter (Common Name) | Gene | Primary Substrates in Oncology | Association with CSCs |
|---|---|---|---|
| ABCG2 (BCRP/MXR) | ABCG2 | Mitoxantrone, Topotecan, Irinotecan/SN-38, Tyrosine Kinase Inhibitors, Methotrexate [74] [73] | High expression; defines the "Side Population" via Hoechst 33342 efflux [70] [73] |
| ABCB1 (P-gp) | ABCB1 | Anthracyclines, Taxanes, Vinca alkaloids, Etoposide [72] | High expression; confers resistance to a broad range of cytotoxics [71] |
| ABCC1 (MRP1) | ABCC1 | Anthracyclines, Vinca alkaloids, Etoposide, Glutathione conjugates [72] | Contributes to the multidrug-resistant phenotype [72] |
Quantifying the Challenge: Data on ABC Transporters in Resistance
The impact of ABC transporter expression on clinical outcomes and drug efficacy has been extensively documented. The following table summarizes key quantitative findings from preclinical and clinical studies.
Table 2: Quantitative Impact of ABCG2 Overexpression on Drug Efficacy and Resistance
| Context / Assay | Measured Outcome | Key Finding | Source/Model |
|---|---|---|---|
| In Vitro Cytotoxicity | IC50 shift for Topotecan | Overexpression of ABCG2 can lead to a significant increase (often 10-100 fold) in the IC50 of chemotherapeutic substrates [73] | Various drug-selected cell lines |
| In Vivo Brain Penetration | Brain Distribution (VT) of ^11C-Erlotinib | In nonhuman primates, ABCB1/ABCG2 inhibition with Elacridar increased brain distribution of ^11C-Erlotinib by 3.5-fold [75] | PET study in Papio anubis baboons |
| Clinical Correlation | Response to Porfimer Sodium PDT | Lung cancer patients with high ABCG2 protein levels responded worse to porfimer sodium PDT than those with low levels [73] | Human lung cancer study |
| Side Population (SP) Analysis | Percentage of SP in Tumors | CSCs often represent a small population ( 2-8% ) within the bulk tumor, identifiable by ABC transporter-mediated dye efflux [70] | Various primary tumors and cell lines |
Tactical Approaches to Inhibit ABCG2-Mediated Efflux
Overcoming ABCG2-mediated resistance has been pursued through several strategic avenues, evolving from non-specific chemical inhibitors to more sophisticated, targeted approaches.
Classical Chemical Inhibitors and Their Limitations
The development of small-molecule inhibitors progressed through generations:
- First Generation: Verapamil, Cyclosporine A. These drugs, repurposed for ABCB1 inhibition, had low potency and significant off-target toxicities [72] [71].
- Second Generation: Valspodar (PSC 833). While more potent, they altered the pharmacokinetics of co-administered chemotherapeutics, leading to unpredictable drug-drug interactions and requiring dose reductions [72] [71].
- Third Generation: Elacridar (GF120918), Tariquidar. Designed for high specificity and potency against ABCB1 and ABCG2, these inhibitors showed promise in preclinical models. A PET study in non-human primates demonstrated that elacridar infusion resulted in a 3.5-fold increase in the brain distribution of ^11C-erlotinib [75]. However, clinical trials have largely failed due to low efficacy, unexpected toxicities, and unsuitable pharmacokinetic profiles [76] [72].
The failure of these broad-spectrum inhibitors in the clinic, combined with the understanding that they may sensitize normal stem cells to chemotherapy, has prompted a shift in strategy [71].
Emerging and Novel Inhibition Modalities
Allosteric Inhibition via Nanobodies
A groundbreaking approach involves the use of nanobodies (single-domain antibodies). Recent cryo-EM structural studies have revealed that inhibitory nanobodies (e.g., Nb8, Nb17, Nb96) can allosterically inhibit ABCG2 by binding to its Nucleotide-Binding Domains (NBDs) [77]. For instance, Nb8 binding prevents the full closure of the NBDs, thereby halting the transport cycle without blocking the substrate-binding pocket itself. This represents a novel mechanism of action that could lead to a new generation of highly specific inhibitors [77].
Transcriptional and Epigenetic Regulation
Instead of inhibiting the transporter's function directly, this tactic aims to downregulate its expression. This can be achieved by targeting transcription factors or epigenetic modifiers that control ABCG2 gene expression. For example, BET inhibitors like JQ1 can suppress the expression of ABC transporters and other resistance genes in CSCs [71].
Developing Non-Substrate Chemotherapeutics
A paradigm shift in drug development involves engineering or identifying anticancer agents that are poor substrates for ABC transporters. This strategy aims to circumvent resistance entirely. Examples include ixabepilone (an epothilone analog not effluxed by ABCB1) and modified taxanes like cabazitaxel [71]. This approach is increasingly favored as it avoids the pharmacokinetic complications and toxicities associated with transporter inhibitors.
Table 3: Strategic Approaches to Overcome ABCG2-Mediated Resistance
| Strategy | Mechanism of Action | Example Agents | Advantages | Challenges/Limitations |
|---|---|---|---|---|
| Direct Pump Inhibition | Competitively or allosterically blocks drug efflux | Elacridar, Tariquidar [72] [75] | Potentially broad applicability | Toxicity, drug-drug interactions, low clinical efficacy [76] [72] |
| Allosteric Modulation | Binds outside substrate pocket, preventing conformational changes | Nanobodies (Nb8, Nb17, Nb96) [77] | High specificity; novel mechanism | Preclinical stage; delivery and immunogenicity concerns |
| Transcriptional/Epigenetic Downregulation | Reduces ABCG2 gene expression | BET inhibitors (JQ1) [71] | Targets root cause; can impact multiple resistance pathways | Potential for off-target effects on global gene expression |
| Non-Substrate Drug Development | Bypasses efflux pump | Ixabepilone, Cabazitaxel [71] | Circumvents resistance mechanism entirely | Requires de novo drug development; may not address pre-existing ABCG2+ CSCs |
The Scientist's Toolkit: Essential Reagents and Protocols
Key Research Reagent Solutions
Table 4: Essential Reagents for Studying ABCG2 Function and Inhibition
| Reagent / Assay | Function / Purpose | Key Example |
|---|---|---|
| Substrate Probes | To measure ABCG2 transport activity in cells or membrane vesicles | Hoechst 33342 (for SP assay), Mitoxantrone, ^3H-Estrone-3-sulfate [70] [73] |
| Chemical Inhibitors | To pharmacologically block ABCG2 function in vitro and in vivo | Elacridar (GF120918), Ko143 [75] [73] |
| Fluorescent Dyes | To identify and sort the ABCG2-positive Side Population (SP) | Hoechst 33342 (dual-wavelength analysis) [70] [73] |
| Genetically Modified Models | To study ABCG2 function in a physiological context | Abcg2/- knockout mice [72] |
| Radiolabeled or Tagged Substrates | For quantitative transport and inhibition studies | ^11C-Erlotinib (for PET imaging) [75] |
| Inhibitory Nanobodies | For structural studies and allosteric inhibition | Nb8, Nb17, Nb96 (for Cryo-EM and functional analysis) [77] |
Detailed Experimental Protocols
Protocol: Side Population (SP) Analysis by Flow Cytometry
The SP assay is a cornerstone technique for identifying stem-like cells based on functional efflux activity [70] [73].
Methodology:
- Cell Preparation: Create a single-cell suspension from the tumor tissue or cell culture. Ensure viability is >90%.
- Dye Loading: Resuspend cells at a concentration of 1x10^6 cells/mL in pre-warmed culture medium. Add Hoechst 33342 dye at a final concentration of 5 µg/mL. Include a control sample stained with Hoechst 33342 in the presence of a specific ABCG2 inhibitor (e.g., 50 µM Verapamil or 10 µM Elacridar) to confirm that the SP is due to transporter activity.
- Incubation: Incubate the cells for 90 minutes at 37°C in a water bath with periodic, gentle mixing.
- Counterstaining and Maintenance: After incubation, centrifuge the cells at 4°C and resuspend in ice-cold PBS. To discriminate dead cells, add a viability dye (e.g., Propidium Iodide at 2 µg/mL) immediately before analysis.
- Flow Cytometry Analysis: Analyze the cells using a flow cytometer equipped with a UV laser. Hoechst 33342 is excited and its fluorescence is collected with two filters: blue red (675 nm LP). The SP will appear as a distinct, dimly stained population of cells that is eliminated in the inhibitor-treated control.
Protocol: Assessing Transporter Inhibition via PET Imaging
This protocol, adapted from Tournier et al. [75], evaluates the efficacy of ABCB1/ABCG2 inhibitors at the blood-brain barrier.
Methodology:
- Radiotracer Administration: Administer the radiolabeled ABCG2 substrate (e.g., ^11C-erlotinib) intravenously to the animal model (e.g., non-human primate).
- PET Scanning: Perform a dynamic PET scan of the brain under baseline conditions to establish the normal distribution volume (V~T~) of the tracer.
- Inhibitor Coadministration: On a separate day, administer the inhibitor. In the referenced study, Elacridar was infused intravenously at 12 mg/kg/h, starting 1 hour before the radiotracer injection and continuing throughout the scan.
- Image and Data Analysis: Reconstruct PET images and calculate the distribution volume of the tracer in the brain region of interest. A significant increase in V~T~ during inhibitor infusion compared to baseline indicates successful transporter inhibition.
Visualizing Pathways and Mechanisms
The Role of ABCG2 in the Cancer Stem Cell Hierarchy
Allosteric Inhibition of ABCG2 by Nanobodies
The role of ABC transporters, especially ABCG2, in protecting CSCs and driving multidrug resistance is a well-established pillar of oncology research. While past strategies focused on broad-spectrum chemical inhibitors have faced significant clinical hurdles, the field is evolving toward more sophisticated tactics. The emergence of allosteric inhibitors like nanobodies, the strategic downregulation of transporter expression, and the paradigm-shifting development of non-substrate therapeutics represent the vanguard of this effort.
Future success will depend on a deep understanding of tumor heterogeneity and the CSC niche. Targeting ABCG2 effectively will likely require combination therapies that simultaneously attack the transporter and other hallmark capabilities of CSCs, such as their quiescence, enhanced DNA repair, and survival signaling pathways. Integrating these approaches holds the promise of dismantling the efflux barrier, sensitizing the most resilient tumor-initiating cells, and ultimately, achieving more durable remissions for cancer patients.
Metabolic plasticity, the dynamic ability of cells to rewire their metabolic pathways in response to environmental cues, has emerged as a critical hallmark of cancer. This adaptability is particularly pronounced in cancer stem cells (CSCs), a subpopulation driving tumor initiation, progression, and therapeutic resistance [78] [1]. CSCs demonstrate remarkable flexibility in shifting their energy production between glycolysis, oxidative phosphorylation (OXPHOS), and fatty acid oxidation (FAO) to meet biosynthetic demands and survive under stress [78] [79]. This metabolic reprogramming directly contributes to tumor heterogeneity and constitutes a fundamental mechanism of drug resistance across cancer types [78] [17].
The metabolic phenotype of CSCs is not fixed but exists in a dynamic equilibrium, influenced by both cell-intrinsic factors (oncogenic signaling, epigenetic status) and cell-extrinsic factors (hypoxia, nutrient availability) [78] [26]. Understanding the molecular mechanisms governing these metabolic adaptations provides crucial insights for developing novel therapeutic strategies to target the resilient CSC population and overcome treatment failure [1] [80].
Metabolic Pathways in Cancer Stem Cells
Glycolytic Adaptations
The Warburg effect or aerobic glycolysis, wherein cells preferentially utilize glycolysis over OXPHOS even in oxygen-sufficient conditions, remains a foundational concept in cancer metabolism [81] [79]. CSCs often leverage this pathway to generate ATP rapidly and produce essential biosynthetic intermediates. Glycolysis provides precursors for nucleotide synthesis, amino acids, and lipids necessary for rapid proliferation [78] [81]. Key regulatory nodes in CSC glycolysis include:
- HIF-1α Stabilization: Under hypoxic conditions commonly found in the tumor microenvironment, HIF-1α upregulates glucose transporters (GLUT1) and glycolytic enzymes (HK2, PDK1, LDHA) to enhance glycolytic flux [78] [81].
- Oncogenic Signaling: MYC activation directly promotes expression of glycolytic genes and lactate production, while mutant KRAS enhances glucose metabolism through the MEK/ERK pathway [78].
- p53 Inactivation: Loss of p53 function removes suppression of glycolytic transporters and enzymes, further shifting metabolism toward glycolysis [78].
Oxidative Phosphorylation Dependence
Contrary to the traditional Warburg perspective, emerging evidence identifies OXPHOS as a preferred metabolic strategy for certain CSCs, particularly under metabolic stress, nutrient deprivation, or during quiescence [78] [82]. Mitochondrial respiration offers greater ATP yield per glucose molecule and supports CSC stemness maintenance through:
- Enhanced Mitochondrial Biogenesis: Regulated by PGC-1α, promoting efficient electron transport chain function [82].
- Redox Homeostasis: OXPHOS helps maintain appropriate levels of reactive oxygen species (ROS), preventing oxidative damage while supporting signaling pathways [79].
- TCA Cycle Anaplerosis: Glutaminolysis replenishes TCA cycle intermediates, enabling continuous OXPHOS function [81].
Fatty Acid Oxidation Utilization
Fatty acid oxidation (FAO) represents an alternative energy source particularly important for CSCs under nutrient-limited conditions [81] [82]. FAO generates substantial ATP through mitochondrial β-oxidation while also producing acetyl-CoA for the TCA cycle and ketone bodies. Key aspects of FAO in CSCs include:
- Lipid Droplet Storage: CSCs often accumulate lipid droplets that serve as endogenous FAO substrates during metabolic stress [80].
- Energy Flexibility during Dormancy: Quiescent CSCs utilize FAO to meet energy needs while minimizing ROS production, supporting long-term survival [79].
- Stemness Regulation: FAO inhibition reduces CSC self-renewal capacity, indicating its functional importance beyond energy production [80].
Table 1: Metabolic Phenotypes of Cancer Stem Cells Across Cancer Types
| Metabolic Phenotype | Cancer Type | Regulatory Factors | Functional Consequences |
|---|---|---|---|
| Glycolysis-Dependent | Colorectal Cancer (HT-29, Caco2, SW480) | HIF-1α, MYC, KRAS | Rapid proliferation, acidification of TME, biosynthetic precursor generation |
| OXPHOS-Dependent | Leukemia, Breast Cancer, Glioblastoma | PGC-1α, ERRα, SIRT1 | Quiescence maintenance, stemness preservation, therapeutic resistance |
| FAO-Preferential | Pancreatic Cancer, Prostate Cancer | PPARδ, CPT1/2, ACADVL | Survival under nutrient deprivation, redox balance, slow-cycling persistence |
| Hybrid/Mixed | Ovarian Cancer, Melanoma | AMPK, mTOR, HIF-1α | Metabolic plasticity, adaptation to fluctuating TME conditions |
Metabolic Plasticity and Therapeutic Resistance
The ability of CSCs to dynamically switch between metabolic programs constitutes a primary mechanism of therapy resistance and disease relapse [78] [17]. Conventional treatments often target rapidly proliferating, glycolysis-dependent bulk tumor cells, inadvertently selecting for resistant CSC populations that leverage alternative metabolic pathways [78] [83].
Metabolic Switching in Treatment Resistance
The glycolysis-OXPHOS switch represents a key adaptive response enabling CSCs to evade targeted therapies [78]. For example:
- Chemotherapy: Treatment with conventional agents can induce a metabolic shift from glycolysis to OXPHOS in residual CSCs, contributing to enrichment of aggressive subpopulations [78].
- Radiation Therapy: Radiation-resistant CSCs frequently demonstrate enhanced mitochondrial function and OXPHOS dependency [83].
- Targeted Therapy: Inhibition of oncogenic signaling pathways (e.g., EGFR, BRAF) can trigger metabolic rewiring toward alternative energy sources, including FAO and glutaminolysis [17] [81].
This metabolic plasticity presents a therapeutic challenge, as CSCs can dynamically reprogram their metabolism in response to targeted interventions, effectively bypassing single-pathway inhibition [78] [17].
Molecular Regulators of Metabolic Plasticity
Multiple interconnected signaling pathways coordinate metabolic plasticity in CSCs:
- Epigenetic Modifications: DNA methylation, histone modifications, and non-coding RNAs regulate metabolic gene expression, enabling rapid adaptation [17] [66].
- HIF-1α/c-MYC Interplay: Under hypoxic conditions, the typical antagonism between HIF-1α and c-MYC transforms into collaboration, co-activating glycolytic genes while maintaining mitochondrial function [78].
- AMPK/mTOR Axis: AMPK activation under energy stress inhibits anabolic processes (via mTOR suppression) while promoting catabolic pathways like FAO [81].
- TGF-β/SMAD Signaling: Promotes epithelial-mesenchymal transition (EMT), enhancing metabolic flexibility and stemness properties [83] [80].
Diagram: Regulatory Network of CSC Metabolic Plasticity. The diagram illustrates how cancer stem cells (CSCs) dynamically shift between glycolysis, OXPHOS, and fatty acid oxidation (FAO) in response to environmental cues and regulatory factors.
Experimental Approaches for Studying CSC Metabolism
Methodologies for Metabolic Analysis
Comprehensive assessment of CSC metabolism requires integrated approaches spanning biochemical, molecular, and functional analyses:
- Seahorse Extracellular Flux Analysis: Real-time measurement of oxygen consumption rate (OCR, indicating OXPHOS) and extracellular acidification rate (ECAR, indicating glycolysis) in live cells [79]. Protocol: Seed CSCs in XF microplates (20,000 cells/well), equilibrate in substrate-limited media, and sequentially inject modulators (oligomycin for ATP-linked respiration, FCCP for maximal respiration, rotenone/antimycin A for non-mitochondrial oxygen consumption).
- Metabolomic Profiling: LC-MS/MS-based quantification of intracellular metabolites to map pathway utilization [81]. Protocol: Extract metabolites from 1-2 million CSCs using 80% methanol at -80°C, analyze central carbon metabolites (glucose-6-phosphate, lactate, TCA intermediates, amino acids) via reverse-phase chromatography coupled to triple quadrupole mass spectrometer.
- Isotopic Tracer Analysis: Track nutrient fate through metabolic networks using 13C/15N-labeled substrates (e.g., U-13C-glucose, U-13C-glutamine) [81] [82]. Protocol: Incubate CSCs with labeled substrates for specified durations (minutes to hours), quench metabolism with cold methanol, and analyze metabolite labeling patterns via GC-MS to determine pathway fluxes.
- Mitochondrial Functional Assays: JC-1 or TMRM staining to measure mitochondrial membrane potential, complemented by ROS detection using CM-H2DCFDA or MitoSOX Red [79].
Table 2: Key Metabolic Parameters and Their Measurement in CSCs
| Metabolic Parameter | Experimental Method | Key Reagents | Data Interpretation |
|---|---|---|---|
| Glycolytic Flux | Extracellular acidification rate (Seahorse) | Glucose, oligomycin, 2-DG | Glycolytic capacity, glycolytic reserve |
| OXPHOS Activity | Oxygen consumption rate (Seahorse) | Oligomycin, FCCP, rotenone/antimycin | Basal respiration, ATP-linked respiration, maximal respiration |
| Fatty Acid Oxidation | Palmitate oxidation assay | 3H-palmitate, BSA, carnitine | FAO rate normalized to protein content |
| Glutaminolysis | 13C-glutamine tracing | U-13C-glutamine, LC-MS | TCA cycle anaplerosis, glutamate production |
| Mitochondrial Content | mtDNA quantification | DNA isolation kits, qPCR primers | mtDNA/nDNA ratio |
| ATP Production | Luminescent ATP assay | Cell lysis buffer, luciferase reagent | Glycolytic vs. mitochondrial ATP contribution |
CSC Identification and Isolation Techniques
Reliable CSC isolation is prerequisite for metabolic studies:
- Surface Marker-Based Sorting: Flow cytometry using CSC-specific surface markers (CD44+/CD24-/low for breast cancer, CD133+ for glioblastoma/colon, EpCAM for various carcinomas) [1] [80]. Include viability dyes (DAPI) and appropriate isotype controls.
- ALDH Activity Assay: Aldefluor assay detecting high aldehyde dehydrogenase activity using BODIPY-aminoacetate substrate [80]. Protocol: Incubate cells with Aldefluor substrate with/without DEAB inhibitor, analyze via flow cytometry within 3 hours.
- Functional Sphere Formation: Serum-free non-adherent culture assessing self-renewal capability [80]. Protocol: Plate single cells at clonal density (1,000-10,000 cells/mL) in ultra-low attachment plates with defined growth factors, count primary spheres after 7-14 days, dissociate and replate for secondary sphere formation efficiency.
Research Reagent Solutions
Table 3: Essential Research Reagents for CSC Metabolism Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Metabolic Inhibitors | 2-DG (glycolysis), oligomycin (ATP synthase), etomoxir (CPT1), GLS-1 (glutaminase) | Pathway inhibition studies | Off-target effects, compensatory mechanisms |
| Isotopic Tracers | U-13C-glucose, U-13C-glutamine, 13C-palmitate | Metabolic flux analysis | Isotope purity, appropriate labeling duration |
| CSC Markers | Anti-CD44, anti-CD133, anti-EpCAM antibodies | CSC isolation and validation | Marker heterogeneity across cancer types |
| Mitochondrial Dyes | JC-1, TMRM, MitoTracker Red, MitoSOX | Mitochondrial function and ROS | Concentration optimization, photostability |
| Cell Culture Media | DMEM/F-12, neurobasal medium, B27 supplement | CSC sphere culture | Serum-free formulation, growth factor composition |
| Metabolic Assay Kits | Seahorse XF Glycolysis/OXPHOS kits, ATP luminescence kits | Functional metabolic profiling | Cell number optimization, normalization methods |
Therapeutic Targeting Strategies
The metabolic vulnerabilities of CSCs present promising therapeutic opportunities, though their plasticity demands sophisticated approaches:
Combination Therapies
Dual metabolic inhibition strategies prevent compensatory pathway activation:
- Glycolysis + OXPHOS Targeting: Combining 2-deoxyglucose (glycolysis inhibitor) with metformin (complex I inhibitor) demonstrates synergistic efficacy against heterogeneous tumors [78] [81].
- Metabolic + Conventional Therapy: OXPHOS inhibitors (like IACS-010759) sensitize CSCs to chemotherapy, reducing relapse potential [78] [17].
- Microenvironment Disruption: Anti-angiogenic agents normalize tumor vasculature, mitigating hypoxia-induced metabolic adaptations [83].
Emerging Approaches
- Synthetic Lethality Strategies: Exploiting context-specific vulnerabilities, such as targeting heme oxygenase-1 (HO-1) in fumarate hydratase (FH)-deficient tumors [81].
- Nanoparticle Delivery: Precisely target metabolic inhibitors to CSCs using CSC marker-functionalized nanoparticles [83].
- Immunometabolic Modulation: Reprogramming immune cell metabolism to overcome CSC-mediated immunosuppression [1] [80].
Diagram: Therapeutic Strategies Targeting CSC Metabolic Plasticity. The diagram illustrates interconnected approaches to overcome therapy resistance by targeting different aspects of CSC biology.
Metabolic plasticity in CSCs, particularly their adaptations in glycolysis, OXPHOS, and FAO, represents a critical determinant of tumor heterogeneity and therapeutic resistance. The dynamic interplay between these metabolic pathways enables CSCs to survive conventional treatments and drive disease recurrence. Future research directions should focus on:
- Advanced Modeling Systems: Patient-derived organoids and 3D culture technologies that better preserve native metabolic heterogeneity [1] [80].
- Single-Cell Multi-omics: Integrated transcriptomic, metabolomic, and proteomic analyses at single-cell resolution to decipher metabolic heterogeneity [1].
- Dynamic Metabolic Imaging: Real-time in vivo tracking of metabolic adaptations using hyperpolarized MRI and other novel imaging modalities [81].
- AI-Driven Predictive Modeling: Machine learning approaches to predict metabolic vulnerabilities based on tumor genetic and microenvironmental features [1] [17].
Targeting CSC metabolic plasticity requires sophisticated combination strategies that simultaneously address multiple pathways while accounting for dynamic adaptation capabilities. Success in this endeavor promises to overcome the fundamental challenges of therapeutic resistance and metastasis, ultimately improving long-term cancer outcomes.
The epithelial-mesenchymal transition (EMT) represents a critical paradigm of cellular plasticity in carcinoma progression, serving as a cornerstone for understanding metastatic dissemination, therapeutic resistance, and tumor heterogeneity. This whitepaper examines the fundamental mechanistic links between EMT programs and the acquisition of cancer stem cell (CSC) properties, exploring how this plasticity drives treatment failure and disease recurrence. Within the broader context of CSC biology, we synthesize current research demonstrating that EMT activation induces stem-like characteristics through specific transcriptional networks, signaling pathways, and metabolic adaptations. We further detail experimental methodologies for investigating EMT-CSC connections and present emerging therapeutic strategies targeting this dynamic interplay. For researchers and drug development professionals, this analysis provides a comprehensive technical framework for understanding and targeting EMT-driven stemness in cancer progression.
EMT constitutes a fundamental cellular reprogramming event wherein epithelial cells shed their differentiated characteristics—including cell-cell adhesion and polarity—and acquire mesenchymal features with enhanced migratory and invasive capabilities [84] [85]. This plasticity is orchestrated by core transcription factors (EMT-TFs) such as SNAIL, TWIST, and ZEB families, which collectively repress epithelial genes (e.g., E-cadherin) while activating mesenchymal genes (e.g., vimentin, N-cadherin) [85]. Concurrently, CSCs represent a tumor subpopulation with self-renewal capacity, differentiation potential, and enhanced resistance mechanisms that drive tumor initiation, propagation, and relapse [1] [53].
The conceptual linkage between these phenomena was solidified by seminal studies demonstrating that EMT activation in immortalized human mammary epithelial cells could induce stem cell properties, including enhanced tumorigenicity and mammosphere formation [86]. This established the paradigm that cellular reprogramming during EMT confers not only migratory capacity but also stem-like attributes. However, contemporary research reveals a more nuanced relationship, wherein hybrid epithelial/mesenchymal (E/M) states often correlate most strongly with stemness, rather than fully mesenchymal phenotypes [87] [88]. This hybrid state, characterized by epithelial-mesenchymal plasticity, appears optimally adapted for metastatic dissemination and therapeutic evasion [88].
Within tumor heterogeneity frameworks, CSCs occupy a hierarchical apex, and their association with EMT programs provides a mechanistic explanation for the observed clinical behaviors of aggression, dormancy, and recurrence [1] [53]. Understanding this EMT-CSC axis is therefore paramount for developing effective strategies against metastatic disease and therapy resistance.
Molecular Mechanisms Linking EMT to Stemness
Core Transcription Factors and Signaling Networks
The molecular interconnection between EMT and stemness is mediated through shared transcriptional regulators and signaling pathways that coordinately regulate both programs. Key embryonic signaling pathways—TGF-β, Wnt, and Notch—simultaneously activate EMT-TFs and stemness-associated factors [89] [85].
Table 1: Key Transcription Factors Regulating EMT and Stemness
| Transcription Factor | Function in EMT | Role in Stemness | Cancer Types Where Expressed |
|---|---|---|---|
| SNAIL | Represses E-cadherin; induces mesenchymal markers | Directly regulates Nanog expression; promotes tumor-initiating capacity | Breast, colorectal, various carcinomas |
| TWIST | Promotes mesenchymal transition | Enhances self-renewal; associated with CSC phenotypes | Breast, prostate, various carcinomas |
| ZEB1 | Represses epithelial genes; activates mesenchymal program | Induces stemness properties; regulates miR-203 | Lung, prostate, pancreatic |
| OCT4 | Modulated during plasticity | Core pluripotency factor; maintains self-renewal | Leukemia, brain, lung, bladder, ovarian |
| SOX2 | Expressed in hybrid E/M states | Pluripotency regulation; stem cell maintenance | Brain, breast, lung, liver, prostate |
| Nanog | Associated with EMT activation | Stem cell self-renewal and pluripotency maintenance | Breast, prostate, colon, liver, ovarian |
TGF-β signaling exemplifies this integration, activating SMAD complexes that transcriptionally upregulate SNAIL and ZEB, while simultaneously inducing stemness factors like Nanog [89]. In breast cancer models, TGF-β-induced EMT correlates directly with acquisition of tumor-initiating stem cells (TISCs), with SNAIL directly regulating Nanog expression [88]. Similarly, Wnt/β-catenin signaling stabilizes nuclear β-catenin, which activates EMT-TFs while cooperating with stemness regulators such as OCT4 and SOX2 [89]. The convergence of these pathways creates a robust molecular framework that synchronizes plastic cellular states with stem-like properties.
The Hybrid E/M State and Stemness Plasticity
Contemporary single-cell RNA sequencing studies have revolutionized our understanding of EMT progression, revealing that cells frequently reside in stable hybrid E/M states rather than binary endpoints [87]. This epithelial-mesenchymal plasticity represents a dynamic equilibrium along the epithelial-mesenchymal spectrum, with specific hybrid states exhibiting maximal stemness potential [88].
In lung adenocarcinoma, trajectory analysis of 16,310 malignant epithelial cells identified five distinct EMT states, with hybrid E/M phenotypes demonstrating the highest metastatic potential and poorest patient prognosis [87]. Similarly, in prostate cancer, single-cell atlases have identified a stem cell-like EMT subtype (CD44+) enriched in castration-resistant disease [85]. This hybrid state appears optimally adapted for dissemination while retaining proliferative capacity—a combination essential for successful metastasis.
The regulatory network stabilizing hybrid states involves balancing acts between EMT-TFs. For instance, PRRX1 expression promotes EMT and dissemination, but its downregulation enhances stemness and metastatic colonization, illustrating the context-dependent functions of EMT-TFs [88]. This plasticity enables dynamic adaptation to microenvironmental cues and therapeutic pressures, making it a critical determinant of cancer progression.
EMT-Driven Stemness in Therapeutic Resistance
CSCs intrinsically exhibit enhanced resilience to conventional therapies through multiple mechanisms, including dormancy, DNA repair capacity, drug efflux pumps, and apoptotic resistance [1] [53]. When EMT programs activate CSC properties, they concomitantly confer these resistance mechanisms, creating a formidable therapeutic barrier.
The resistance mechanisms employed by EMT-derived CSCs operate through both intrinsic and extrinsic pathways:
Metabolic Plasticity: Mesenchymal-like CSCs demonstrate metabolic flexibility, shifting between glycolysis, oxidative phosphorylation, and alternative fuel sources like fatty acids and glutamine to survive therapeutic stress [1]. In prostate cancer, EMT-transitioned cells exhibit a twofold increase in glycolytic flux and heightened glutamine dependence, supporting energy production and redox balance under treatment pressure [85].
Microenvironment Interaction: EMT-activated CSCs engage in metabolic symbiosis with stromal cells, further enhancing resistance capacity [1]. They also secrete factors that create an immunosuppressive niche, protecting them from immune surveillance [85].
Epigenetic Adaptation: EMT induces epigenetic reprogramming that stabilizes hybrid plastic states and enhances stress adaptation. In metastatic castration-resistant prostate cancer, hypermethylation of the CDH1 (E-cadherin) promoter maintains mesenchymal characteristics while bivalent domains allow rapid response to therapeutic challenges [85].
Drug Efflux Systems: CSCs frequently express ABC transporters that actively export chemotherapeutic agents, a feature enhanced in EMT-derived stem cells [53].
This multi-faceted resistance paradigm explains why conventional therapies that effectively bulk tumor populations often fail to eradicate CSCs, ultimately leading to disease recurrence. Targeting the EMT-stemness axis therefore represents a strategic approach to overcome therapeutic resistance.
Experimental Models and Methodologies
Investigating the EMT-stemness connection requires integrated experimental approaches that capture cellular plasticity and functional stemness properties. The following methodologies represent key techniques in this research domain.
Table 2: Experimental Methods for Studying EMT and Stemness
| Method Category | Specific Techniques | Key Readouts | Considerations |
|---|---|---|---|
| In Vitro Functional Assays | Scratch/wound healing assay; Transwell migration/invasion; 3D spheroid/organoid culture | Migration velocity; Invasion capacity; Collective vs. single-cell dissemination | Limited microenvironmental complexity; Controlled experimental variables |
| Stemness Assessment | Mammosphere/Prostasphere formation; Extreme limiting dilution assay (ELDA) | Self-renewal capacity; Tumor-initiating cell frequency | Serum-free conditions essential; Confirmation with in vivo models |
| In Vivo Models | Cell-derived xenografts (CDX); Patient-derived xenografts (PDX); Genetically engineered models (GEM) | Metastatic colonization; Therapy response; Tumor initiation capacity | Preserves microenvironment; Resource-intensive; Ethical considerations |
| Single-Cell Analysis | scRNA-seq; Lineage tracing; Spatial transcriptomics | EMT continuum states; Stemness signatures; Cellular heterogeneity | High-resolution data; Computational complexity; Preserves cellular diversity |
Key Experimental Protocols
Migration and Invasion Assays: Standard protocols include scratch assays where confluent cell monolayers are wounded, and migration into the void is quantified over 24-48 hours. For invasion assessment, Transwell chambers coated with Matrigel (∼1-2 mg/mL) simulate basement membrane penetration, with cells migrating toward serum gradients over 24 hours [84]. These assays should be coupled with molecular analysis of EMT markers (E-cadherin, vimentin) via immunofluorescence or Western blot.
Stemness Characterization: The gold standard mammosphere/prostasphere assay involves plating single-cell suspensions in ultra-low attachment plates with serum-free media supplemented with B27, EGF (20 ng/mL), and FGF (10 ng/mL). Primary spheres >50μm are counted after 7-14 days, with self-renewal assessed through serial passaging [53]. Functional tumor initiation capacity must be validated in immunocompromised mice via limiting dilution transplantation.
Single-Cell RNA Sequencing Workflow: Fresh tumor tissue is dissociated to single-cell suspensions, followed by viability assessment (>80% required). Cells are loaded onto platforms (10X Genomics) for barcoded library preparation, followed by sequencing depth of >50,000 reads/cell. Bioinformatic analysis includes normalization, dimensionality reduction (UMAP/t-SNE), and trajectory inference (Monocle3, Slingshot) to reconstruct EMT continuums and identify stemness signatures [87].
Research Reagent Solutions
Table 3: Essential Research Reagents for EMT and Stemness Investigations
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| EMT Inducers | Recombinant TGF-β (2-10 ng/mL); TNF-α (10-50 ng/mL); Hypoxia chambers (1% O₂) | Induce EMT programming in epithelial cells; Concentration and duration critical for phenotype | May induce different EMT spectra; TGF-β浓度尤为重要 |
| CSC Markers | Antibodies to CD44, CD133, ALDH1A1; Fluorescent substrates (ALDEFLUOR) | Identification and isolation of CSC populations via FACS/MACS | Marker combinations improve specificity; Context-dependent expression |
| Signaling Inhibitors | SB431542 (TGF-βR inhibitor); XAV939 (Wnt inhibitor); DAPT (Notch inhibitor) | Pathway inhibition to dissect mechanistic contributions | Off-target effects possible; Combination approaches informative |
| Extracellular Matrices | Matrigel (basement membrane extract); Collagen I (3D culture) | 3D microenvironment modeling; Invasion assays | Lot-to-lot variability; Optimal concentration determination required |
| Lineage Tracing Tools | FUCCI cell cycle reporters; EMT reporter constructs (E-cadherin-GFP) | Real-time tracking of cell state transitions | Construct validation essential; May perturb native biology |
Therapeutic Targeting Strategies
Overcoming EMT-driven stemness and resistance requires innovative therapeutic approaches that target specific vulnerabilities in this adaptive system. Emerging strategies include:
Dual Metabolic Inhibition: Simultaneously targeting glycolysis and oxidative phosphorylation in mesenchymal-like CSCs to exploit their metabolic dependencies [1]. This approach addresses the metabolic plasticity that allows CSCs to adapt to therapeutic stress.
Epigenetic Modulators: DNMT and HDAC inhibitors that reverse EMT-stabilizing epigenetic modifications and restore drug sensitivity [85]. These agents target the epigenetic memory that maintains stemness properties.
Nanoparticle-Mediated Therapies: Advanced nanocarriers designed for CSC-targeted delivery of therapeutic agents, including those that overcome physiological barriers to drug delivery [41]. These systems improve specificity while reducing off-target effects.
Immunotherapy Approaches: CAR-T cells engineered against CSC surface markers (EpCAM, CD133) and immune checkpoint inhibitors that reverse EMT-associated immunosuppression [1] [53].
Hybrid State Stabilization: Therapeutic interventions that lock cells in hybrid E/M states, potentially reducing their metastatic potency and stemness properties [87] [88].
The integration of these approaches with conventional therapies represents the most promising avenue for durable treatment responses. Clinical trials are increasingly incorporating CSC and EMT biomarkers to stratify patients and monitor therapeutic efficacy.
The intricate interconnection between EMT plasticity and cancer stemness represents a fundamental determinant of tumor progression, therapeutic resistance, and metastatic competence. Rather than a binary relationship, this association involves dynamic transitions along epithelial-mesenchymal spectra, with specific hybrid states exhibiting enhanced stemness properties. Understanding this plasticity provides critical insights into cancer biology and reveals novel therapeutic vulnerabilities.
Future research directions should prioritize:
- Spatiotemporal Resolution: Advanced imaging and spatial transcriptomics to map EMT-stemness dynamics within intact tumor architectures and metastatic niches.
- Mechanistic Decoupling: Identifying context-specific regulators that can disrupt the EMT-stemness connection without impairing physiological plasticity.
- Metabolic Dependencies: Comprehensive mapping of metabolic vulnerabilities in EMT-derived CSCs across tumor types.
- Clinical Translation: Development of robust biomarkers for EMT-CSC states and therapeutic response monitoring.
As single-cell technologies and functional genomics continue to advance, our understanding of EMT-driven stemness will undoubtedly evolve, offering new opportunities for intervention. For researchers and drug development professionals, targeting this plasticity represents a promising frontier in overcoming cancer's adaptive resilience.
The tumor microenvironment (TME) represents a complex ecosystem that plays a decisive role in cancer progression, therapy resistance, and immune evasion. Hypoxia, characterized by low oxygen partial pressure (<10 mmHg in many solid tumors), emerges as a hallmark feature of aggressive and treatment-resistant malignancies [90]. This oxygen deprivation initiates a cascade of adaptive biological responses that promote tumor survival, angiogenesis, metastasis, and immune evasion through the activation of hypoxia-inducible factors (HIFs) [91]. Within this hypoxic niche, cancer stem cells (CSCs)—a highly plastic and therapy-resistant cell subpopulation—thrive, driving tumor initiation, progression, metastasis, and relapse [1]. The intricate interplay between hypoxia, CSCs, and immune suppression creates a formidable barrier to effective cancer treatment, making the targeting of this axis a critical frontier in oncology research and drug development.
The fundamental premise that reversing tumor hypoxia can potentiate anti-tumor immunity is strongly supported by seminal studies demonstrating that physiologically relevant hypoxic conditions directly impair T lymphocyte development and effector functions [91]. Hypoxia-driven immune suppression occurs through multiple mechanisms: it suppresses T cell infiltration by disrupting chemokine gradients, drives the recruitment of immunosuppressive cells, and induces metabolic reprogramming that limits T cell proliferation and cytotoxic potential [91]. Concurrently, hypoxia promotes and maintains CSC phenotypes, further contributing to therapeutic resistance [90]. This review explores the dynamic interrelationships between hypoxia, CSCs, and immune evasion, while providing technical guidance for researchers developing targeted interventions against this pathogenic triad.
Quantitative Landscape of Hypoxia and CSC-Mediated Resistance
Table 1: Quantitative Features of Tumor Hypoxia Across Cancer Types
| Cancer Type | Oxygen Partial Pressure (pO₂) | Prevalence of Hypoxia | Key Hypoxia-Associated Markers | Impact on Survival |
|---|---|---|---|---|
| Pancreatic Cancer | <10 mmHg [90] | >90% of solid tumors [90] | HIF-1α, HIF-2α, CA-IX | Decreased disease-free survival [90] |
| Head and Neck Tumors | <10 mmHg [90] | >90% of solid tumors [90] | HIF-1α, VEGF, GLUT-1 | Linked to poor prognosis [90] [92] |
| Breast Cancer | <10 mmHg [90] | >90% of solid tumors [90] | HIF-1α, LOX, PD-L1 | Correlates with metastasis [90] |
| Cervical Cancer | <10 mmHg [90] | >90% of solid tumors [90] | HIF-1α, VEGF, carbonic anhydrase | Decreased disease-free survival [90] |
Table 2: Cancer Stem Cell Markers and Functional Characteristics Across Tumors
| Cancer Type | Key CSC Markers | Self-Renewal Pathways | Therapy Resistance Mechanisms | Contribution to Metastasis |
|---|---|---|---|---|
| Acute Myeloid Leukemia (AML) | CD34⁺CD38⁻ [1] | Wnt/β-catenin, Notch | Enhanced DNA repair, drug efflux | Bone marrow dissemination [1] |
| Glioblastoma (GBM) | CD133, Nestin, SOX2 [1] | SHH, STAT3 | ALDH activity, MGMT expression | Invasive growth patterns [1] |
| Gastrointestinal Cancers | LGR5, CD166 [1] | Wnt, BMP/TGF-β | Upregulation of ABC transporters | Liver metastasis [41] |
| Breast Cancer | CD44⁺CD24⁻, ALDH1⁺ [1] | Hippo, NF-κB | Quiescence, autophagy | Bone and lung tropism [1] |
The spatial distribution of immune cells within the TME represents a critical determinant of therapeutic response. Recent advances in spatial analysis technologies like Spatiopath have enabled quantitative assessment of cell-cell and cell-region interactions, revealing that immune "desert" and immune "excluded" phenotypes correlate with poor response to immunotherapy [93] [92]. In head and neck squamous cell carcinoma (HNSCC), spatial transcriptomic studies have characterized regions with substantial loss of effector T cells and dendritic cells, forming "cold tumors" devoid of immune monitoring [92]. These patterns highlight the hierarchical organization of the TME and its profound impact on treatment outcomes.
Core Signaling Pathways and Molecular Mechanisms
Hypoxia-Inducible Factor Signaling Axis
The cellular response to hypoxia is predominantly mediated by hypoxia-inducible factors (HIFs), transcription factors that regulate adaptive gene expression programs under low oxygen conditions. HIF-1α and HIF-2α are the most studied isoforms that play pivotal roles in tumor adaptation to hypoxia [91] [90]. Under normoxic conditions, HIF-α subunits undergo prolyl hydroxylation by prolyl hydroxylase domain (PHD) enzymes, leading to von Hippel-Lindau (pVHL)-mediated ubiquitination and proteasomal degradation. Under hypoxic conditions, this degradation is inhibited, allowing HIF-α subunits to dimerize with HIF-1β and translocate to the nucleus, where they activate transcription of target genes involved in angiogenesis (VEGF), metabolic reprogramming (GLUT1), invasion (MMPs), and immune modulation (PD-L1) [90].
CSC-Immune Evasion Circuits
Cancer stem cells employ multiple sophisticated mechanisms to evade immune surveillance. The "Trinity" regulatory network of immune evasion encompasses three interlinked pathways: (1) metabolic reprogramming-mediated immune checkpoint modulation, (2) stromal cell-driven immune dysfunction, and (3) epigenetic remodeling fostering immune tolerance [92]. CSCs upregulate immune checkpoint molecules such as PD-L1 through HIF-1α-dependent and independent mechanisms. In HNSCC, spatial proteomic analyses reveal PD-L1 enrichment at invasive fronts, particularly on CSCs, where PD-1/PD-L1 interactions impair immune synapse formation [92]. Additionally, CSCs secrete immunosuppressive cytokines including IL-10, TGF-β, and prostaglandin E2, which recruit and activate regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs), creating an immunosuppressive niche that protects CSCs from immune attack [1] [92].
Experimental Protocols for TME Analysis and Targeting
Protocol 1: Spatial Analysis of Immune Cell Distributions Using Spatiopath
Principle: Spatiopath is a mathematical framework for spatial pattern analysis within the TME that distinguishes statistically significant immune cell associations from random distributions using a null-hypothesis paradigm [93].
Procedure:
- Tissue Preparation and Staining: Prepare formalin-fixed, paraffin-embedded tumor sections (5μm thickness). Perform multiplex immunofluorescence staining using markers for immune cells (CD8 for cytotoxic T cells, CD4 for helper T cells, CD68 for macrophages, CD33 for MDSCs) and tumor epithelium (pan-cytokeratin).
- Image Acquisition and Processing: Acquire whole-slide images using a high-throughput slide scanner with multispectral imaging capabilities. Process images using cell segmentation algorithms to identify and classify different cell types based on marker expression.
- Spatial Mapping: Export spatial coordinates (x,y positions) and cell type classifications for all detected cells. Segment tumor epithelium regions and export their boundaries as closed 2-D contours.
- Spatial Analysis Using Spatiopath Framework:
- For cell-cell interactions: Apply Ripley's K-function to analyze spatial associations between different immune cell populations.
- For cell-tumor epithelium interactions: Use the generalized accumulation function to quantify immune cell distributions relative to tumor epithelium boundaries.
- Compute the vector R = [..., R{m+1,m}, ...]^T where R{m+1,m} = R(r{m+1}) - R(rm) provides information about the average accumulation of immune cells within distances between rm and r{m+1} from reference cells or tumor boundaries.
- Statistical Validation: Compare observed spatial patterns against null distributions generated from random cell localization to identify statistically significant associations (p<0.05 with multiple testing correction).
Applications: This protocol enables identification of "immune desert" and "immune excluded" phenotypes, correlation of spatial patterns with clinical outcomes, and assessment of treatment-induced changes in TME organization [93] [92].
Protocol 2: Targeting Hypoxic CSCs with Oxygen-Supplied Nanomaterials (OSNs)
Principle: Oxygen-supplied nanomaterials (OSNs) are engineered to deliver or generate oxygen at the tumor site, alleviating hypoxia and potentially reversing its immunosuppressive and CSC-promoting effects [91].
Procedure:
- OSN Fabrication:
- Perfluorocarbon-based Nanoemulsions: Prepare by high-pressure homogenization of perfluorocarbons (e.g., perfluoro-15-crown-5-ether) with phospholipid surfactants (e.g., lecithin) in aqueous phase. Load oxygen by bubbling with 95% O₂/5% CO₂ before administration.
- Catalytic Nanoparticles: Synthesize manganese dioxide (MnO₂) nanoparticles that react with endogenous hydrogen peroxide (H₂O₂) to produce oxygen: MnO₂ + H₂O₂ + 2H⁺ → Mn²⁺ + 2H₂O + O₂.
- In Vitro Validation:
- Establish 3D spheroid cultures from patient-derived xenografts or cancer cell lines under hypoxic conditions (1% O₂).
- Treat spheroids with OSNs and measure oxygen levels using fluorescent oxygen probes (e.g., Image-IT Hypoxia Reagent).
- Assess CSC viability using flow cytometry with CSC-specific markers (CD44+/CD24- for breast cancer, CD133+ for glioblastoma).
- Evaluate T cell-mediated killing in co-culture systems with tumor-infiltrating lymphocytes.
- In Vivo Therapeutic Efficacy:
- Use immunocompetent mouse models (e.g., syngeneic grafts, genetically engineered models).
- Administer OSNs intravenously at optimized dosage (typically 10-20 mg/kg) and schedule (2-3 times weekly).
- Monitor tumor hypoxia non-invasively using pimonidazole immunohistochemistry or hypoxia-sensitive PET tracers.
- Analyze immune cell infiltration by flow cytometry and immunohistochemistry at endpoint.
- Evaluate effects on CSC population using limiting dilution assays and sphere formation assays.
Applications: OSNs can be combined with immune checkpoint inhibitors (anti-PD-1/PD-L1), adoptive T cell therapies (CAR-T), or conventional therapies to overcome hypoxia-mediated therapy resistance [91].
Visualization of Key Biological Workflows
Research Reagent Solutions for TME Targeting
Table 3: Essential Research Tools for Hypoxia and CSC Research
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Hypoxia Detection | Pimonidazole HCl, Image-iT Hypoxia Reagent | Quantification of hypoxic regions in vitro and in vivo | Pimonidazole requires immunohistochemistry for detection; fluorescent reagents allow live imaging |
| CSC Isolation & Analysis | Anti-CD44, Anti-CD133, ALDEFLUOR Assay | Identification and isolation of CSC populations | Combination of surface markers and functional assays recommended due to CSC plasticity |
| Oxygen-Supplying Nanomaterials | Perfluorocarbon nanoemulsions, MnO₂ nanoparticles | Experimental reversal of tumor hypoxia | Oxygen loading capacity and tumor targeting efficiency are critical parameters |
| Spatial Analysis Platforms | Spatiopath algorithm, CODEX, Visium Spatial Transcriptomics | Mapping cellular distributions and interactions in TME | Requires specialized computational expertise for data interpretation |
| Immune Monitoring | Multiplex IHC/IF, CyTOF, TCR sequencing | Comprehensive profiling of immune cell populations | Spatial context is essential for understanding immune function |
| 3D Culture Models | Patient-derived organoids, Tumor spheroids | Physiologically relevant drug screening platforms | Can be adapted to hypoxic culture conditions for CSC enrichment |
The targeting of hypoxic niches and CSC microenvironments represents a promising frontier in overcoming therapy resistance and immune evasion in cancer. The integration of advanced spatial analysis tools with innovative therapeutic approaches such as oxygen-supplied nanomaterials provides powerful strategies to dissect and disrupt the pathogenic interplay between hypoxia, CSCs, and immune suppression. Future research directions should focus on developing more sophisticated in vitro models that recapitulate the spatial and metabolic heterogeneity of the TME, identifying conserved vulnerabilities across different cancer types, and designing clinical trials that combine hypoxia-targeting agents with CSC-directed therapies and immunotherapies. As our understanding of the dynamic functional landscape of stemness in cancer continues to evolve [25], so too will our ability to develop precision therapies that effectively target the heart of tumor resistance and recurrence.
Evaluating Emerging CSC-Targeted Therapies and Clinical Translation
The efficacy of conventional cancer therapeutics is fundamentally limited by multiple physiological barriers that prevent drugs from reaching their intended targets at sufficient concentrations. These barriers are particularly problematic in the context of cancer stem cells (CSCs), a subpopulation of tumor cells with self-renewal capacity, enhanced survival mechanisms, and resistance to conventional therapies that drive tumor initiation, progression, metastasis, and relapse [1]. CSCs exhibit exceptional therapeutic resistance through multiple mechanisms, including enhanced DNA repair, drug efflux pumps, metabolic plasticity, and interactions with protective microenvironments [1] [94] [17]. The blood-brain barrier (BBB) represents an additional formidable obstacle for treating central nervous system malignancies, as it excludes more than 98% of small-molecule drugs and all macromolecular therapeutics from entering the brain [95].
Nanotechnology has emerged as a powerful platform to overcome these biological obstacles through engineered systems that enhance drug delivery to specific cellular targets. By designing nanocarriers with precise physicochemical properties and surface functionalities, researchers can now develop strategies to bypass both physiological barriers and CSC-mediated resistance mechanisms [96] [94]. This technical guide examines the current state of nanotechnology-based approaches for targeted drug delivery, with particular emphasis on overcoming CSC-associated treatment resistance in oncology.
Physiological Barriers to Drug Delivery
The Blood-Brain Barrier and Blood-Tumor Barriers
The BBB is a multicellular, dynamic semi-permeable membrane that isolates the central nervous system from circulating blood [95]. Its core anatomical structure consists of:
- Endothelial cells connected by tight junctions that significantly limit paracellular transport
- Pericytes embedded in the basement membrane that modulate vascular function and barrier integrity
- Astrocytes whose end feet link with the basement membrane and help regulate vascular function
- Tight junctions that form nearly continuous impermeable barriers controlling molecular traffic [95]
In glioblastoma and other brain malignancies, the blood-tumor barrier may display some disruption but still retains significant barrier function, particularly in infiltrative regions and micrometastases [95]. The BBB's efflux transporters, especially P-glycoprotein, actively remove many therapeutic compounds, further reducing drug penetration [97].
Tumor Microenvironment Barriers
Solid tumors present multiple physiological barriers that impede drug delivery:
- Abnormal vasculature with heterogeneous blood flow and distribution
- Elevated interstitial fluid pressure that reduces convective transport
- Dense extracellular matrix that hinders diffusion
- Hypoxic and acidic regions that alter drug activity and promote CSC maintenance [96] [17]
The enhanced permeability and retention (EPR) effect, whereby macromolecules and nanoparticles tend to accumulate in neoplastic tissues due to leaky vasculature and impaired lymphatic drainage, provides a foundational principle for passive tumor targeting [96]. However, the EPR effect exhibits significant heterogeneity across tumor types and individual patients, limiting its reliability as a universal delivery mechanism [96].
Cancer Stem Cell-Specific Barriers
CSCs employ multiple mechanisms to resist therapies, creating additional biological barriers:
- ABC transporter overexpression that actively effluxes chemotherapeutic drugs
- Enhanced DNA repair capacity that mitigates genotoxic damage
- Metabolic plasticity enabling adaptation to nutrient stress
- Quiescence that protects against cell cycle-active therapeutics
- Epigenetic reprogramming that maintains stemness under stress
- Interaction with protective niches in the tumor microenvironment [1] [94] [17]
Table 1: Key Physiological Barriers and Nanotechnology Solutions
| Barrier Type | Specific Challenges | Nanotechnology Solutions |
|---|---|---|
| Blood-Brain Barrier | Tight junctions, efflux transporters, limited transcytosis | Receptor-mediated transcytosis, cell-mediated transport, stimuli-responsive opening |
| Tumor Microenvironment | Heterogeneous vasculature, high interstitial pressure, dense ECM | EPR-mediated accumulation, ECM-degrading enzymes, size-controlled nanoparticles (20-200 nm) |
| CSC Resistance Mechanisms | Drug efflux pumps, quiescence, DNA repair, metabolic plasticity | CSC-targeting ligands, combination therapies, stimuli-responsive release, bypassing efflux pumps |
Nanotechnology Platforms for Overcoming Biological Barriers
Nanocarrier Design Principles
Effective nanocarriers for overcoming biological barriers share several key design principles:
- Size control (typically 20-200 nm) to optimize circulation time and tissue penetration [94]
- Surface functionalization with hydrophilic polymers (e.g., PEG) to reduce opsonization and extend circulation half-life [96]
- Targeting ligands (antibodies, peptides, aptamers) for specific cellular interactions
- Stimuli-responsive elements that trigger drug release in response to pathological cues [96] [98]
Major Nanocarrier Classes
Table 2: Nanocarrier Platforms for Targeted Drug Delivery
| Nanocarrier Type | Composition | Key Advantages | Clinical Examples |
|---|---|---|---|
| Liposomes | Phospholipid bilayers | High drug loading, biocompatible, tunable surface properties | Doxil, Onivyde, Vyxeos |
| Polymeric Nanoparticles | PLGA, chitosan, dendrimers | Controlled release, functionalizable surface, degradation tuning | Investigational stages |
| Inorganic Nanoparticles | Gold, silica, iron oxide | Unique optical/magnetic properties, uniform size distribution | Preclinical development |
| Biomimetic Nanocarriers | Exosomes, cell membranes | Natural targeting, immune evasion, biocompatibility | Early clinical evaluation |
Targeting Cancer Stem Cells with Nanotechnology
CSC-Specific Targeting Strategies
Nanocarriers can be engineered to specifically target CSCs through multiple approaches:
- Surface marker targeting using ligands against CSC markers such as CD44, CD133, EpCAM, and LGR5 [1] [99]
- Signaling pathway inhibition targeting Wnt/β-catenin, Notch, Hedgehog, and Hippo pathways that maintain stemness [94]
- Microenvironment modulation disrupting CSC-niche interactions that promote maintenance and drug resistance [1] [25]
- Metabolic targeting exploiting unique CSC metabolic dependencies such as oxidative phosphorylation or fatty acid oxidation [1]
Combination Strategies for CSC Elimination
Effective CSC targeting often requires combination approaches:
- Dual metabolic inhibition simultaneously targeting glycolysis and oxidative phosphorylation to address CSC metabolic plasticity [1]
- Co-delivery of conventional chemotherapy with CSC-targeting agents to eliminate both bulk tumor cells and CSCs [94]
- Immunotherapy combinations using engineered immune cells or immune-modulating agents to enhance CSC elimination [1] [99]
Diagram 1: Nanotechnology Strategies for Overcoming Physiological Barriers in Cancer Therapy. This workflow illustrates how engineered nanoparticles address multiple barriers to eliminate CSCs and reduce tumor recurrence.
Experimental Protocols and Methodologies
Protocol: Development of CSC-Targeted Nanocarriers
Objective: Synthesize and characterize lipid nanoparticles functionalized with CD44-targeting hyaluronic acid for CSC-specific drug delivery.
Materials:
- Lipid components: DSPC, cholesterol, PEG-DSPE, cationic lipid (DOTAP)
- Targeting ligand: Hyaluronic acid (MW 10-20 kDa)
- Therapeutic payload: Salinomycin or other CSC-targeting agent
- Characterization equipment: Dynamic light scattering, HPLC, fluorescence spectroscopy
Methodology:
Nanoparticle formulation using ethanol injection or thin-film hydration method
- Dissolve lipid mixture (55% DSPC, 35% cholesterol, 5% PEG-DSPE, 5% DOTAP) in ethanol
- Hydrate with ammonium sulfate buffer (pH 6.5) at 65°C with vortexing
- Extrude through polycarbonate membranes (100 nm pore size)
Remote loading of therapeutic agent
- Incubate nanoparticles with drug solution (1:10 weight ratio) at 60°C for 30 minutes
- Purify via dialysis or size exclusion chromatography
Surface functionalization
- Activate hyaluronic acid with EDC/NHS chemistry
- Conjugate to amine-containing PEG lipids at 1:5 molar ratio
- Incubate with pre-formed nanoparticles for 12 hours at 4°C
- Purify by ultracentrifugation
Characterization
- Size distribution: DLS measurement (target: 80-120 nm)
- Surface charge: Zeta potential measurement
- Drug loading: HPLC quantification after nanoparticle dissolution
- Targeting ligand density: Colorimetric assay or fluorescence labeling
Protocol: Evaluation of CSC Targeting Efficiency
In vitro assessment:
CSC enrichment from established cancer cell lines (MCF-7, U87MG) using:
- Serum-free sphere-forming conditions
- Fluorescence-activated cell sorting for CD44+/CD24- or CD133+ populations
Cellular uptake studies
- Incubate fluorescently labeled nanoparticles with CSCs vs. non-CSCs
- Quantify uptake via flow cytometry and confocal microscopy
- Perform competitive inhibition with free hyaluronic acid
CSC viability and self-renewal assays
- Treat sphere cultures with nanoformulations (0.1-100 μM range)
- Assess viability using ATP-based assays at 72 hours
- Evaluate secondary sphere formation capacity after treatment
Mechanistic studies
- Analyze ABC transporter activity using efflux dyes
- Evaluate apoptosis and cell cycle distribution
- Assess effects on stemness signaling pathways (Wnt, Notch) via Western blot
In vivo evaluation:
- Orthotopic tumor models with CSC-enriched xenografts
- Biodistribution studies using near-infrared fluorescent imaging
- Therapeutic efficacy monitoring tumor growth and metastasis
- CSC quantification in residual tumors via immunohistochemistry and flow cytometry
Diagram 2: Experimental Workflow for CSC-Targeted Nanocarrier Development. This comprehensive methodology encompasses nanoparticle formulation, characterization, and biological evaluation to establish therapeutic efficacy.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Nanotechnology-Based CSC Targeting
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Nanoparticle Core Materials | PLGA, PEG-PLGA, DSPC, cholesterol, gold nanoparticles, mesoporous silica | Scaffold for drug encapsulation and delivery | Biocompatibility, degradation profile, drug loading capacity |
| Targeting Ligands | Hyaluronic acid (CD44), anti-CD133 antibodies, EGFR-targeting peptides, transferrin (TfR) | Specific recognition of CSC surface markers | Binding affinity, stability, conjugation efficiency, immunogenicity |
| Therapeutic Payloads | Salinomycin, doxorubicin, paclitaxel, gemcitabine, siRNA against stemness factors | Direct elimination of CSCs or disruption of stemness pathways | Solubility, compatibility with nanocarrier, release kinetics |
| Characterization Tools | Dynamic light scattering, HPLC systems, TEM, fluorescence imaging systems | Physicochemical characterization and biological evaluation | Sensitivity, resolution, quantification capabilities |
| Biological Assay Reagents | Aldefluor assay kits, sphere culture media, apoptosis detection kits, Western blot antibodies | Functional assessment of CSC targeting and elimination | Specificity, reproducibility, quantitative output |
Emerging Frontiers and Future Perspectives
The field of nanotechnology for overcoming physiological barriers in cancer therapy continues to evolve rapidly. Several emerging approaches show particular promise:
- Multifunctional nanocarriers that combine targeting, diagnostic, and therapeutic capabilities
- Biomimetic systems utilizing exosomes or cell membrane coatings for enhanced biocompatibility and targeting [94]
- Stimuli-responsive designs that release payloads in response to pathological cues (pH, enzymes, redox status)
- CRISPR-based approaches using nanotechnology to deliver gene-editing tools specifically to CSCs [94] [99]
- Advanced targeting strategies exploiting newly identified CSC-specific surface markers and signaling pathways
Artificial intelligence-driven design and multi-omics integration are accelerating the development of next-generation nanotherapeutics [1]. Additionally, the growing understanding of CSC plasticity and heterogeneity is informing more sophisticated targeting approaches that address the dynamic nature of stemness in cancer [25].
The continued translation of these technologies will require close attention to manufacturing scalability, regulatory considerations, and comprehensive safety assessment. As these challenges are addressed, nanotechnology-based approaches for overcoming physiological barriers offer tremendous potential for improving outcomes in cancer therapy, particularly for malignancies driven by treatment-resistant CSCs.
Chimeric antigen receptor (CAR)-T cell therapy and immune checkpoint blockade (ICI) represent two pillars of the cancer immunotherapy revolution. CAR-T cells are engineered synthetic receptors that redirect T lymphocytes to recognize and eliminate cells expressing a specific target antigen, independent of major histocompatibility complex (MHC) presentation [100] [101]. Immune checkpoint inhibitors, particularly those targeting the PD-1/PD-L1 axis, function by releasing inhibitory brakes on T cells, thereby reactivating an exhausted immune response against tumors [102] [103]. While both modalities have demonstrated remarkable efficacy in specific malignancies, their success is often tempered by the development of therapeutic resistance, a phenomenon increasingly linked to cancer stem cells (CSCs) [104] [1] [105]. This technical review examines the integration of CAR-T cells and checkpoint inhibitors, framed within the context of CSC-mediated tumor heterogeneity and drug resistance.
Core Technological Principles
CAR-T Cell Architecture and Generational Evolution
CARs are modular synthetic receptors consisting of four fundamental components: an extracellular antigen-binding domain, a hinge region, a transmembrane domain, and intracellular signaling domains [101]. The antigen-binding domain is typically derived from single-chain variable fragments (scFvs) of monoclonal antibodies, conferring specificity for tumor-associated antigens [100]. The hinge or spacer region provides flexibility to overcome steric hindrance, with its length critically influencing epitope accessibility and CAR functionality [101]. The transmembrane domain, often derived from CD3ζ, CD8α, or CD28, anchors the CAR to the T cell membrane and can influence receptor stability and signaling [101]. Intracellular signaling domains combine T-cell activation motifs (typically CD3ζ) with co-stimulatory domains that enhance persistence and efficacy [100].
CAR-T cells are classified into generations based on their intracellular signaling architecture:
Table 1: Generational Evolution of CAR-T Cell Designs
| Generation | Signaling Domains | Key Features | Functional Implications |
|---|---|---|---|
| First | CD3ζ only | Limited persistence and clinical efficacy | Dependent on exogenous cytokines; insufficient T cell activation [100] [101] |
| Second | CD3ζ + one co-stimulatory domain (CD28 or 4-1BB) | Enhanced persistence and cytotoxicity | CD28 domains promote effector memory differentiation; 4-1BB domains enhance mitochondrial biogenesis and central memory formation [100] [101] |
| Third | CD3ζ + multiple co-stimulatory domains (e.g., CD28+4-1BB) | Potential for enhanced activation | Mixed preclinical results; not consistently superior to second generation [101] |
| Fourth (TRUCKs) | Second-generation base + cytokine secretion | Engineered to release cytokines (e.g., IL-12) | Modulates tumor microenvironment; recruits and activates endogenous immune cells [100] |
| Fifth | Second-generation base + cytokine receptor signaling | Incorporates additional membrane receptors (e.g., IL-2Rβ) | Enables antigen-dependent JAK/STAT activation; promotes memory formation and broader immune stimulation [100] |
Immune Checkpoint Biology and Mechanism of Action
Immune checkpoints are naturally occurring inhibitory pathways that maintain self-tolerance and prevent immune overactivation. Malignant cells co-opt these pathways, particularly the PD-1/PD-L1 axis, to suppress antitumor immunity [102]. Programmed cell death protein 1 (PD-1; CD279) expressed on T cells interacts with its ligand PD-L1 (CD274; B7-H1) on tumor and host cells, triggering a signaling cascade that inhibits T-cell receptor signaling and abrogates T-cell function [102] [103]. Other clinically relevant checkpoints include cytotoxic T-lymphocyte-associated protein 4 (CTLA-4; CD154), T-cell immunoglobulin and mucin-domain containing-3 (TIM3), and lymphocyte-activation gene 3 (LAG3; CD223) [102].
Checkpoint inhibitors are monoclonal antibodies that disrupt these inhibitory interactions. Ipilimumab (anti-CTLA-4) was the first FDA-approved checkpoint inhibitor in 2011, followed by pembrolizumab and nivolumab (both anti-PD-1) [102]. These agents have demonstrated durable responses across multiple malignancies, though response rates generally remain below 40% as monotherapies [102].
Figure 1: Synergistic Mechanisms of CAR-T Cells and Checkpoint Blockade. CAR-T cells directly recognize tumor antigens independent of MHC, while checkpoint inhibitors block the PD-1/PD-L1 inhibitory axis to enhance T-cell function.
The Cancer Stem Cell Challenge in Immunotherapy
CSC-Mediated Resistance Mechanisms
Cancer stem cells constitute a highly plastic, therapy-resistant subpopulation within tumors that drives initiation, progression, metastasis, and relapse [1] [105]. Their ability to evade immunotherapeutic interventions stems from multiple interconnected mechanisms:
Table 2: CSC-Specific Mechanisms of Immunotherapy Resistance
| Resistance Mechanism | Molecular Players | Functional Consequences |
|---|---|---|
| Altered Antigen Presentation | Downregulated MHC class I [104] [105] | Reduced visibility to CD8+ cytotoxic T cells |
| Immune Checkpoint Upregulation | PD-L1, B7-H4, B7-H3, CD155, CD47, CD24 [105] | Direct inhibition of effector immune cells; phagocytosis resistance |
| Immunosuppressive Secretome | Cytokines, chemokines, exosomes [104] [105] | Recruitment of Tregs, MDSCs; polarization of macrophages to M2 phenotype |
| Metabolic Plasticity | Glycolysis/OXPHOS switching; glutamine/fatty acid utilization [1] | Survival under metabolic stress; creation of immunosuppressive niche |
| Quiescence & DNA Repair | Slow cell cycling; enhanced DNA damage response [104] [1] | Resistance to therapies targeting rapidly dividing cells |
| Niche Interaction | Adhesion molecules; cytokine crosstalk [106] [105] | Physical protection in specialized microenvironments |
CSC-Immune Cell Interactions in the Tumor Microenvironment
The CSC niche represents a specialized microenvironment that sustains stemness and fosters immune suppression through intricate cellular crosstalk [105]. CSCs actively recruit regulatory immune cells including tumor-associated macrophages (TAMs), myeloid-derived suppressor cells (MDSCs), and regulatory T cells (Tregs) through secretion of factors like IL-10, TGF-β, and prostaglandin E2 [104] [106]. This bidirectional communication creates a protective ecosystem that shields CSCs from immune surveillance while simultaneously inhibiting the function of cytotoxic immune effectors [106] [105]. The resulting immunosuppressive milieu represents a fundamental barrier to both CAR-T cell therapy and checkpoint blockade, particularly in "cold" tumors with limited pre-existing immune infiltration [102] [105].
Integrated Therapeutic Approaches: Combining CAR-T Cells and Checkpoint Blockade
Preclinical Rationale for Combination Therapy
The synergistic potential of CAR-T cells and checkpoint inhibitors stems from their complementary mechanisms of action. CAR-T cells provide a specific, engineered immune infiltrate capable of recognizing and eliminating tumor cells, while checkpoint inhibitors counteract the immunosuppressive environment that undermines optimal CAR-T cell function [102]. Preclinical studies demonstrate that PD-1/PD-L1 interaction induces exhaustion in CAR-T cells, limiting their persistence and antitumor efficacy [102]. Combination approaches have shown enhanced tumor control in solid tumor models, supporting clinical translation of this strategy [102].
Clinical Evidence and Timing Considerations
Clinical trials investigating CAR-T cell and checkpoint inhibitor combinations have yielded nuanced insights, particularly regarding treatment sequencing. A phase 1 clinical trial in large B-cell lymphoma (LBCL) patients combining CD19-targeted CAR-T cells with the PD-L1 antibody durvalumab revealed that timing significantly impacts efficacy [103]. Contrary to initial hypotheses, patients receiving durvalumab before CAR-T cell infusion showed lower response rates than those starting durvalumab after CAR-T cells [103]. This counterintuitive outcome was attributed to overlapping peaks of soluble PD-L1 (sPD-L1) and CAR-T cell expansion when durvalumab was administered first, potentially inhibiting CAR-T cell function during their critical expansion phase [103]. These findings underscore that simply combining these modalities is insufficient—their precise temporal coordination is critical for optimal outcomes.
Advanced Engineering Strategies to Overcome CSC-Mediated Resistance
Next-Generation CAR Designs Against Heterogeneous Tumors
Innovative CAR architectures are being developed specifically to address tumor heterogeneity and antigen escape, hallmarks of CSC-driven resistance:
Adapter CAR (AdCAR) System: This platform utilizes T cells transduced with a CAR that recognizes an exogenous adapter molecule (AM) rather than a direct tumor antigen [107]. These bifunctional adapters bridge target cells with AdCAR-T cells, enabling: (1) Multiplex targeting of multiple antigens with a single CAR-T product; (2) Precise controllability through AM dosing; and (3) Treatment intervals to prevent exhaustion [107]. In AML models, sequential administration of adapters against different antigens (CD33, CLL-1, CD123) significantly improved control of heterogeneous populations [107].
Logic-Gated CARs: These sophisticated systems incorporate Boolean operations to enhance specificity. "OR" gates (e.g., tandem CARs) trigger activation upon recognition of any of multiple antigens, preventing escape through single antigen loss [107]. "AND" gates require simultaneous recognition of two antigens, potentially enhancing safety by restricting activity to cells expressing both targets [107].
Table 3: Advanced CAR-T Platforms to Counter CSC Heterogeneity
| Platform | Mechanism | Advantages | Current Status |
|---|---|---|---|
| Adapter CARs | Bifunctional adapters bridge CAR to tumor antigens | Target switching without re-engineering; dose-dependent control; reduced exhaustion | Preclinical validation in AML, NHL, breast cancer [107] |
| Tandem CARs (OR-gating) | Single CAR with multiple binding domains | Reduced antigen escape; activity against heterogeneous tumors | Clinical evaluation in B-cell malignancies [107] |
| TRUCKs (4th Gen) | Cytokine secretion (e.g., IL-12) upon activation | TME modification; host immunity activation; counter immunosuppression | Phase I/II trials for solid tumors [100] [108] |
| PD-1-Edited CAR-Ts | CRISPR-mediated PD-1 disruption | Intrinsic checkpoint resistance; enhanced persistence in immunosuppressive TME | Early clinical trials [100] |
CSC-Targeted Immunotherapeutic Approaches
Emerging strategies specifically aim to dismantle CSC defense mechanisms:
Dual checkpoint inhibition targeting both PD-L1 and CD47 has demonstrated synergistic efficacy in preclinical models, simultaneously blocking T-cell inhibition and macrophage "don't eat me" signals [105].
Epitope editing through CRISPR-based approaches enables selective targeting of tumor-specific antigen variants while sparing normal tissues [107].
Metabolic reprogramming of CAR-T cells enhances their fitness within the nutrient-poor, immunosuppressive CSC niche [1].
Experimental Protocols and Methodologies
Standardized CAR-T Cell Generation Protocol
Stage 1: T-Cell Isolation and Activation
- Source: Leukapheresis product from patients or donors
- Isolation: Density gradient centrifugation followed by CD3+ selection using magnetic-activated cell sorting (MACS)
- Activation: Culture with anti-CD3/CD28 antibodies immobilized on beads or artificial antigen-presenting cells (aAPCs)
- Culture Conditions: X-VIVO 15 or TexMACS medium with 5-10% human serum AB, IL-7 (5ng/mL), and IL-15 (5ng/mL) [100] [101]
Stage 2: Genetic Modification
- Transduction: Lentiviral or retroviral vectors containing CAR construct at MOI 3-10 in retronectin-coated plates
- Alternative Approaches: Transposon/transposase systems (Sleeping Beauty) or CRISPR-based gene editing for specific integration (e.g., TRAC or PDCD1 loci) [100] [101]
Stage 3: Expansion and Formulation
- Expansion: 7-10 days in gas-permeable culture bags with continuous cytokine support
- Quality Control: Flow cytometry for CAR expression; mycoplasma testing; sterility testing; endotoxin testing
- Cryopreservation: Formulation in cryoprotectant solution (e.g., CryoStor CS10) at target cell dose [101]
In Vitro Potency and Specificity Assessment
Cytotoxicity Assays
- Standardized Co-culture: Effector:Target ratios from 1:1 to 20:1 over 24-72 hours
- Readouts: Real-time cell analysis (RTCA); luciferase-based bioluminescence; flow cytometric detection of apoptosis (Annexin V/7-AAD)
- Specificity Validation: Inclusion of antigen-negative and antigen-positive control cell lines [101]
Cytokine Profiling
- Multiplex ELISA: Simultaneous quantification of IFN-γ, TNF-α, IL-2, IL-6, IL-10 from co-culture supernatants
- Time Course: Measurements at 6, 24, and 48 hours to capture activation kinetics [101]
Exhaustion and Memory Phenotyping
- Flow Cytometry Panel: PD-1, TIM-3, LAG-3, CD62L, CD45RO, CD45RA, CCR7
- Functional Assay: Repeated antigen stimulation to assess sustained cytotoxicity and proliferative capacity [102] [101]
Research Reagent Solutions for Combination Therapy Studies
Table 4: Essential Research Tools for CAR-T/Checkpoint Inhibitor Investigations
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| CAR Detection Reagents | Anti-Fab antibodies, Protein L, target antigen tetramers | Quantification of CAR expression and transduction efficiency |
| Checkpoint Inhibitors | Anti-PD-1 (nivolumab, pembrolizumab), anti-PD-L1 (durvalumab, atezolizumab) | In vitro and in vivo blockade of checkpoint pathways |
| CSC Isolation Tools | Anti-CD44, anti-CD133, ALDEFLUOR assay, side population staining | Identification and purification of CSC populations |
| Cytokine Analysis | Luminex multiplex arrays, ELISA kits for IFN-γ, IL-2, IL-6 | Profiling of immune activation and cytokine release syndrome biomarkers |
| Exhaustion Markers | Anti-PD-1, anti-TIM-3, anti-LAG-3 antibodies | Flow cytometric assessment of T-cell dysfunction |
| 3D Culture Systems | Tumor spheroids, organoid co-cultures, microfluidic devices | Modeling tumor microenvironment and CSC niche interactions |
The convergence of CAR-T cell therapy and immune checkpoint blockade represents a promising frontier in overcoming CSC-mediated treatment resistance. The strategic integration of these modalities, informed by growing understanding of CSC biology and immune evasion tactics, offers a path toward more durable responses. Future success will hinge on sophisticated engineering approaches that address tumor heterogeneity while countering the immunosuppressive networks protecting CSCs. As these technologies mature, their rational combination based on mechanistic insights rather than empirical pairing will be essential for translating preclinical promise into clinical reality for cancer patients.
Therapeutic resistance and tumor recurrence in cancer are largely driven by a subpopulation of cancer stem cells (CSCs), which exhibit remarkable plasticity and adaptive capabilities. The PI3K/AKT/mTOR (PAM) and Wnt signaling pathways are frequently co-activated in CSCs, enabling their maintenance, self-renewal, and survival. Emerging evidence reveals that these pathways engage in extensive cross-talk, where inhibition of one often leads to compensatory upregulation of the other, thereby fostering resistance. This whitepaper synthesizes current research demonstrating that dual-pathway inhibition of PAM and Wnt signaling represents a synergistic and innovative strategy to overcome CSC-mediated therapy resistance. We provide a detailed analysis of the molecular mechanisms, summarize key experimental data in structured tables, outline essential methodologies, and visualize the core signaling networks, offering a technical guide for researchers and drug development professionals aiming to develop more durable cancer therapies.
Cancer stem cells (CSCs) are a subpopulation of tumor cells with the capacity for self-renewal, differentiation, and tumor initiation, first identified in leukemia and subsequently in solid tumors [1] [109]. These cells are now recognized as a primary source of intratumoral heterogeneity and a key driver of therapeutic resistance, metastasis, and relapse [1] [4]. CSCs possess intrinsic resistance mechanisms, including quiescence, enhanced DNA repair, upregulation of drug efflux pumps, and metabolic plasticity, allowing them to survive conventional treatments that target rapidly dividing cells [5] [4]. The persistence of even a minimal number of CSCs post-therapy can lead to disease recurrence, often with a more aggressive phenotype [5].
A deeper understanding of the signaling pathways that govern CSC fate is crucial for developing strategies to eradicate them. The PI3K/AKT/mTOR (PAM) and Wnt pathways are two such evolutionarily conserved signaling cascades. The PAM pathway is a central regulator of cell survival, growth, proliferation, and metabolism, and it is one of the most frequently dysregulated pathways in human cancer [110]. Concurrently, the Wnt pathway is critical for embryonic development, tissue homeostasis, and stem cell maintenance [111]. In many cancers, including triple-negative breast cancer (TNBC), colorectal cancer, and others, both pathways are aberrantly activated and contribute to the maintenance of CSC pools [111] [109]. This co-activation, coupled with their well-documented cross-talk, presents a compelling therapeutic opportunity for dual-pathway inhibition to preempt compensatory resistance mechanisms and more effectively target the CSC population.
Scientific Rationale for Dual Targeting
Pathway Cross-Talk and Compensatory Activation
The core rationale for dual targeting lies in the robust reciprocal feedback and compensatory activation between the PAM and Wnt pathways. A seminal study in triple-negative breast cancer (TNBC) demonstrated this phenomenon clearly. Using an in silico Molecular Activity Predictor (IPA) tool, researchers predicted that inhibition of the PI3K pathway would result in the activation of the Wnt pathway [111]. This prediction was experimentally validated when treatment of TNBC cell lines with the pan-PI3K inhibitor buparlisib led to a significant increase in the expression of multiple Wnt pathway genes, including porcupine (PORCN), Frizzled receptors (FZD), and β-catenin (CTNNB1) [111]. Porcupine, a membrane-bound acyltransferase essential for Wnt ligand secretion, was upregulated up to 8-fold at the protein level following PI3K inhibition. This compensatory activation creates a mechanistic escape route for cancer cells, allowing them to maintain survival and stem-like signals through the Wnt pathway when the PAM pathway is blocked.
Convergence on CSC Maintenance and Survival
Both pathways converge on critical processes that sustain CSCs. The PAM pathway promotes CSC survival by inhibiting apoptosis and driving the translation of proteins required for cell cycle progression [112] [110]. Meanwhile, the Wnt pathway, through the stabilization and nuclear translocation of β-catenin, activates a transcriptional program that enforces self-renewal and inhibits differentiation [111]. Key stemness transcription factors like c-MYC are common downstream targets of both pathways, creating a synergistic signaling network that reinforces the CSC state [109]. Dual inhibition disrupts this cooperative maintenance of stemness, leading to a more profound loss of CSC viability and tumor-initiating capacity than targeting either pathway alone.
Key Experimental Evidence and Data
Research across multiple cancer models has provided compelling evidence supporting the synergistic efficacy of dual PAM and Wnt pathway inhibition.
Table 1: Summary of Key In Vitro Findings on Dual PI3K and Wnt Inhibition
| Cancer Model | PI3K Inhibitor | Wnt Inhibitor | Key Findings | Synergy (Combination Index) | Citation |
|---|---|---|---|---|---|
| TNBC (MDA-MB-231) | Buparlisib | WNT974 (Porcupine inhibitor) | ~50% reduction in cell viability at 100 nM each; compensatory Wnt activation post-PI3Ki | 0.33 (Synergistic) | [111] |
| TNBC (Hs578T) | Buparlisib | WNT974 | ~50% reduction in cell viability at 100 nM each | 0.36 (Synergistic) | [111] |
| TNBC (HCC70) | Buparlisib | WNT974 | Additive effect; more resistant, IC50 of 1 μM | Additive | [111] |
| NSCLC (A549) | Fisetin (dietary flavonoid) | (Inherent mTOR/Wnt inhibition) | Dual inhibition of PI3K/Akt and mTOR signaling; reduced colony formation | Not Calculated | [112] |
Table 2: In Vivo Efficacy of Dual Pathway Inhibition
| Cancer Model | Inhibitors | Dosing Regimen | Key Outcomes | Citation |
|---|---|---|---|---|
| TNBC Xenografts | Buparlisib + WNT974 | In vivo dosing established; combination well-tolerated | Significant synergy in reducing tumor growth compared to monotherapies | [111] |
The data from these studies underscore several critical points. First, the synergy is highly potent in specific contexts, with combination indices well below 1, indicating strong synergistic interaction [111]. Second, the response can be cell-context dependent, varying from synergistic to additive, highlighting the need for biomarker-driven patient selection [111]. Finally, naturally occurring compounds like fisetin have been shown to inherently possess dual inhibitory activity against the PAM pathway, suppressing phosphorylation of AKT, mTOR, and its downstream effectors like p70S6K1, and inhibiting colony formation in NSCLC models [112].
Experimental Protocols and Methodologies
For researchers seeking to replicate or build upon these findings, the following detailed methodologies from key studies serve as a guide.
In Vitro Synergy Assay (Chou-Talalay Method)
This protocol is essential for quantitatively determining the synergy between two inhibitors.
- Cell Seeding and Treatment: Seed TNBC cells (e.g., MDA-MB-231, Hs578T) in 96-well plates at a density of 3-5 x 10³ cells/well and allow to adhere overnight. Prepare a matrix of serial dilutions for buparlisib and WNT974, ensuring a constant ratio of their individual IC50 values across the combinations. Treat cells with single agents and all possible combinations for 72-96 hours [111].
- Viability Assessment: After treatment, assess cell viability using a standardized assay such as MTT or CellTiter-Glo. The MTT assay involves adding 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazoliumbromide to each well, incubating for 2-4 hours, solubilizing the formed formazan crystals in DMSO, and measuring the absorbance at 540 nm [112] [111].
- Data Analysis: Calculate the fraction of cells affected (Fa) for each drug combination. Input the dose and response data into software such as CompuSyn to calculate the Combination Index (CI) according to the Chou-Talalay method. A CI < 1, =1, and >1 indicates synergy, additivity, and antagonism, respectively [111].
Molecular Validation of Compensatory Pathway Activation
This protocol confirms the underlying mechanism of synergy by measuring pathway changes after single-agent treatment.
- Treatment for RNA/Protein Analysis: Culture cancer cells in 6-well plates or culture dishes until they are 60-70% confluent. Treat with a PI3K inhibitor (e.g., 1x IC50 of buparlisib), a Wnt inhibitor, or a vehicle control (DMSO) for 24-48 hours [112] [111].
- RNA Extraction and qPCR: Extract total RNA using a commercial kit (e.g., Qiagen RNeasy). Synthesize cDNA and perform quantitative PCR (qPCR) using SYBR Green or TaqMan chemistry. Primers should target Wnt pathway genes such as PORCN, FZD receptors, and CTNNB1, with GAPDH or ACTB as a housekeeping control. Fold changes in gene expression are calculated using the 2^–ΔΔCt method [111].
- Protein Extraction and Western Blotting: Lyse cells in RIPA buffer supplemented with protease and phosphatase inhibitors. Determine protein concentration using a BCA assay. Separate proteins by SDS-PAGE (e.g., on Novex precast Tris-glycine gels), transfer to a PVDF membrane, and block with 5% non-fat milk. Probe the membrane overnight at 4°C with primary antibodies against targets like p-AKT (Ser473), total AKT, Porcupine, and β-catenin. After incubation with an HRP-conjugated secondary antibody, visualize bands using enhanced chemiluminescence (ECL) [112] [111]. An increase in Porcupine protein levels after PI3K inhibitor treatment confirms compensatory activation.
Signaling Pathways and Workflow Visualization
The following diagrams, generated with Graphviz DOT language, illustrate the core signaling pathways and the experimental logic underpinning dual-pathway inhibition.
Pathway Cross-Talk and Inhibitor Mechanism
Title: Core signaling pathways and cross-talk between PAM and Wnt.
Compensatory Activation and Dual Inhibition Logic
Title: Logic flow of compensatory resistance and dual inhibition strategy.
The Scientist's Toolkit: Key Research Reagents
Successful investigation into this dual-targeting approach requires a well-characterized toolkit of reagents, inhibitors, and assays.
Table 3: Essential Reagents and Resources for Dual-Pathway Research
| Reagent / Resource | Function / Target | Example Products / Catalog Numbers | Key Application in Research |
|---|---|---|---|
| Pan-PI3K Inhibitor | Reversibly inhibits all four class I PI3K isoforms (α, β, γ, δ) | Buparlisib (BKM120) | In vitro and in vivo inhibition of the PI3K/AKT/mTOR axis; induces compensatory Wnt activation [111]. |
| Porcupine Inhibitor | Inhibits Porcupine (PORCN), preventing Wnt ligand palmitoylation and secretion | WNT974 (LGK974) | In vitro and in vivo inhibition of the canonical Wnt pathway; used in combination with PI3Ki [111]. |
| mTOR Inhibitor | Specifically inhibits mTOR kinase, a key node in the PAM pathway | Rapamycin (Sirolimus) | Used to validate mTOR-specific effects and its role in CSC survival [112]. |
| siRNA/mTOR | Genetic knockdown of mTOR expression | mTOR-siRNA (e.g., Dharmacon) | Confirms pharmacological inhibition results and demonstrates specificity of mTOR targeting [112]. |
| Antibody: p-AKT | Detects phosphorylated (active) AKT at Ser473 | Cell Signaling Technology #4060 | Western blot validation of PAM pathway inhibition [112] [111]. |
| Antibody: Porcupine | Detects PORCN protein levels | Cell Signaling Technology | Western blot validation of compensatory Wnt pathway upregulation post-PI3K inhibition [111]. |
| Antibody: β-Catenin | Detects total and/or active β-catenin | Cell Signaling Technology | Assesses Wnt pathway activity and nuclear localization. |
| Cell Viability Assay | Measures metabolic activity as a proxy for cell viability/cytotoxicity | MTT Assay, CellTiter-Glo | Quantifies dose-response and synergy in inhibitor treatments [112] [111]. |
| qPCR Assay Probes | Quantifies mRNA expression of Wnt pathway genes | TaqMan probes for PORCN, FZD, CTNNB1 | Validates transcriptional upregulation of Wnt components [111]. |
| CSC Marker Antibodies | Identifies and isolates CSC subpopulations | Anti-CD133, Anti-CD44, Anti-ALDH1 | Used in FACS or immunofluorescence to correlate pathway inhibition with reduction in CSC frequency [4] [109]. |
Dual-pathway inhibition of PI3K/AKT/mTOR and Wnt signaling represents a rationally designed, synergistic strategy to target the resilient CSC population that underpins tumor heterogeneity, drug resistance, and relapse. The preclinical evidence, particularly in aggressive cancers like TNBC, is compelling, demonstrating that this approach can preempt compensatory resistance mechanisms and more effectively eradicate tumors [111]. The translation of this strategy into the clinic, however, presents several key challenges and opportunities for future research. These include identifying robust biomarkers to predict which patients and tumor types are most likely to benefit, carefully managing the potential toxicities associated with inhibiting these fundamental signaling pathways, and designing innovative clinical trials with appropriate endpoints that can capture effects on the CSC population. As our understanding of CSC biology and pathway cross-talk deepens, and as more targeted inhibitors enter the clinical arena, dual-pathway inhibition stands as a promising pillar in the next generation of cancer therapeutics aimed at achieving durable, long-term remissions.
Cancer stem cells (CSCs) represent a pivotal frontier in oncology, serving as key drivers of tumor heterogeneity, therapeutic resistance, and disease recurrence. These cells possess enhanced DNA repair capabilities, maintain low reactive oxygen species (ROS) levels, exhibit metabolic flexibility, and evade conventional therapies through both intrinsic and extrinsic mechanisms [113] [94] [114]. The development of novel therapeutic modalities specifically designed to target these resilient cell populations is therefore critical for advancing cancer treatment outcomes. Within this context, three innovative approaches—ferroptosis inducers, photothermal therapy, and epigenetic modulators—have emerged as promising strategies to overcome CSC-mediated resistance. These modalities target distinct vulnerabilities of CSCs: ferroptosis inducers exploit altered iron metabolism and redox homeostasis, photothermal therapy utilizes physical energy deposition to bypass conventional resistance mechanisms, and epigenetic modulators reverse the transcriptional programs that maintain stemness and plasticity. This technical guide provides a comprehensive overview of these approaches, detailing their molecular mechanisms, experimental methodologies, and potential for clinical translation within the framework of CSC biology.
Ferroptosis Inducers: Exploiting Metabolic Vulnerabilities
Molecular Mechanisms and Key Pathways
Ferroptosis is an iron-dependent form of regulated cell death characterized by the lethal accumulation of lipid peroxides, distinct from apoptosis, necrosis, and autophagy in its morphological and biochemical features [113] [115]. The core execution machinery involves three interconnected processes: iron dysmetabolism, lipid peroxidation accumulation, and inactivation of the glutathione-dependent antioxidant defense system [116] [117].
CSCs demonstrate particular vulnerability to ferroptosis due to their altered iron metabolism. Research indicates that CSCs exhibit elevated iron concentrations relative to their non-stem counterparts, which is essential for sustaining their characteristics but also increases their susceptibility to ferroptosis inducers [113]. This iron overload creates a favorable environment for the Fenton reaction, where Fe²⁺ ions react with hydrogen peroxide to generate highly reactive hydroxyl radicals and lipid peroxides [115].
The central defense system against ferroptosis is the cystine/glutathione/GPX4 axis. System Xc⁻, a cystine/glutamate antiporter composed of SLC7A11 and SLC3A2 subunits, imports cystine for glutathione (GSH) synthesis [113]. GSH serves as an essential cofactor for glutathione peroxidase 4 (GPX4), which reduces phospholipid hydroperoxides to nontoxic lipid alcohols, thereby protecting cells from ferroptotic death [115] [116]. CSCs frequently rely on this pathway for their survival, making it a promising therapeutic target.
Additional regulatory pathways include the FSP1/CoQH₂ system, which functions independently of GPX4. Ferroptosis suppressor protein 1 (FSP1) reduces ubiquinone (CoQ) to ubiquinol (CoQH₂) using NAD(P)H, and CoQH₂ acts as a lipophilic radical-trapping antioxidant that inhibits lipid peroxidation [113] [117]. The GCH1/BH4 pathway represents another parallel protective system, where GTP cyclohydrolase-1 (GCH1) and its metabolite tetrahydrobiopterin (BH4) inhibit ferroptosis through lipid remodeling and CoQ10 regeneration [117].
Figure 1: Core Regulatory Pathways of Ferroptosis. The diagram illustrates key ferroptosis triggers (red) and defense mechanisms (green) that regulate lipid peroxidation and cell death.
Experimental Protocols for Ferroptosis Induction
In Vitro Assessment of Ferroptosis in CSCs
Cell Culture and CSC Enrichment:
- Maintain cancer cells in appropriate media. For CSC enrichment, culture cells as spheroids in serum-free DMEM/F12 medium supplemented with 20 ng/mL EGF, 10 ng/mL bFGF, and B27 supplement in low-attachment plates [113] [94].
- Validate CSC enrichment through flow cytometry analysis of surface markers (CD44+/CD24⁻ for breast CSCs, CD133⁺ for glioblastoma CSCs, EpCAM⁺ for digestive CSCs) and ALDH1 activity assay [94].
Ferroptosis Induction and Inhibition:
- Treat CSCs with ferroptosis inducers: Erastin (10-20 μM) to inhibit system Xc⁻, RSL3 (1-5 μM) to directly inhibit GPX4, or FIN56 (5-10 μM) to promote GPX4 degradation [113] [115].
- For negative controls, pre-treat cells with ferroptosis inhibitors: ferrostatin-1 (1-2 μM), liproxstatin-1 (1-2 μM), or the iron chelator deferoxamine (100 μM) for 2 hours before inducer treatment [115].
Assessment and Quantification:
- Measure cell viability using CCK-8 or MTT assays after 24-48 hours of treatment.
- Quantify lipid peroxidation using C11-BODIPY⁵⁸¹/⁵⁹¹ fluorescence probe (5 μM incubation for 30 minutes) followed by flow cytometry analysis, or measure malondialdehyde (MDA) levels via thiobarbituric acid reactive substances (TBARS) assay [115] [116].
- Detect intracellular iron levels using FerroOrange (1 μM) or Phen Green SK (5 μM) fluorescent probes [115].
- Analyze GSH/GSSG ratio using commercial colorimetric or fluorometric kits.
- Confirm ferroptosis specificity by comparing with apoptosis inhibitor (Z-VAD-FMK, 20 μM) and necroptosis inhibitor (Necrostatin-1, 10 μM) [115].
Nanoparticle-Mediated Ferroptosis Induction
Iron Oxide Nanoparticle Synthesis:
- Prepare iron-based nanoparticles (Fe₃O₄) through co-precipitation method: mix FeCl₂ and FeCl₃ solutions in 1:2 molar ratio under nitrogen atmosphere, add NH₄OH solution dropwise with vigorous stirring at 60°C [115] [114].
- Characterize nanoparticles for size (dynamic light scattering), morphology (transmission electron microscopy), and surface charge (zeta potential).
- Functionalize nanoparticles with CSC-targeting ligands (e.g., CD44 antibodies, CD133 aptamers) via EDC/NHS chemistry [94] [114].
In Vitro Evaluation:
- Treat CSCs with nanoparticles (50-200 μg/mL) for 24 hours.
- Assess cellular uptake via Prussian blue staining or immunofluorescence.
- Evaluate lysosomal degradation of nanoparticles and subsequent Fe²⁺ release using Lysotracker and FerroOrange staining [115].
- Measure synergistic effects with conventional chemotherapy (e.g., cisplatin, doxorubicin) [115] [118].
Research Reagent Solutions for Ferroptosis Studies
Table 1: Essential Reagents for Ferroptosis Research
| Reagent/Category | Specific Examples | Function/Mechanism | Working Concentration |
|---|---|---|---|
| Ferroptosis Inducers | Erastin, RSL3, FIN56 | Inhibit system Xc⁻ or GPX4 to trigger lipid peroxidation | 1-20 μM |
| Inhibitors | Ferrostatin-1, Liproxstatin-1 | Radical-trapping antioxidants that block lipid peroxidation | 1-2 μM |
| Iron Chelators | Deferoxamine (DFO), Ciclopirox | Bind intracellular iron to prevent Fenton reaction | 50-100 μM |
| Lipid Peroxidation Probes | C11-BODIPY⁵⁸¹/⁵⁹¹, Liperfluo | Detect and quantify lipid peroxidation in live cells | 1-5 μM |
| Iron Sensors | FerroOrange, Phen Green SK | Monitor labile iron pool (Fe²⁺) dynamics | 1-5 μM |
| GSH Assay Kits | DTNB-based colorimetric assays | Quantify glutathione levels and redox state | N/A |
| CSC Markers | Anti-CD44, Anti-CD133, ALDH1 assay | Identify and isolate cancer stem cell populations | Antibody-dependent |
Photothermal Therapy: Precision Thermal Ablation of CSCs
Principles and Nanomaterial Design
Photothermal therapy (PTT) employs photothermal agents (PTAs) that convert near-infrared (NIR) laser energy into localized heat, inducing thermal ablation of cancer cells [119]. This approach is particularly valuable against CSCs, as it bypasses conventional resistance mechanisms through a physical mode of action that carries limited risk of resistance development [119] [114].
The efficacy of PTT depends critically on the properties of both the PTAs and the laser parameters. Ideal PTAs exhibit high photothermal conversion efficiency (PCE), excellent thermal stability, tunable surface plasmon resonance, and biocompatibility [119]. Gold-based nanomaterials have been extensively studied due to their tunable localized surface plasmon resonance (LSPR). For instance, gold nanorods (AuNRs) with aspect ratios of 3-4 exhibit strong absorption in the NIR-I window (700-950 nm), while miniaturized AuNRs (5-11 nm) can be engineered to absorb in the NIR-II window (1000-1350 nm) for deeper tissue penetration [119]. Gold nanostars with branched structures demonstrate enhanced electromagnetic fields and plasma coupling effects, further improving light absorption in the NIR region [119].
Organic PTAs offer advantages in biodegradability and reduced long-term toxicity. Single-component organic phototherapeutic agents (SCOPAs), including indocyanine green and aza-BODIPY derivatives, can be designed with tumor-specific activation mechanisms for enhanced precision [119]. These organic systems represent a promising direction for clinical translation due to their favorable safety profiles.
Laser parameters significantly influence treatment precision and efficacy. The NIR wavelength range (700-950 nm for NIR-I, 1000-1350 nm for NIR-II) provides optimal tissue penetration with minimal photonic absorption by tissue components [119]. Lower power densities (0.12-0.22 W/cm²) coupled with optimized pulse durations enable deeper tissue penetration while minimizing collateral damage to healthy tissue [119].
Experimental Protocol for CSC-Targeted PTT
Photothermal Agent Synthesis and Characterization:
- Synthesize gold nanorods using seed-mediated growth method: prepare gold seed solution with NaBH₄, then grow rods in growth solution containing CTAB, HAuCl₄, AgNO₃, and ascorbic acid [119].
- Functionalize AuNRs with CSC-targeting ligands (e.g., anti-CD133 antibodies, anti-CD44 peptides) via thiol chemistry or EDC/NHS coupling [119] [114].
- Characterize optical properties using UV-Vis-NIR spectroscopy to confirm LSPR peak in NIR region.
- Measure photothermal conversion efficiency using method described by R. R. Anderson et al. [119].
In Vitro PTT Treatment:
- Incubate CSC-enriched spheroids with targeted PTAs (10-50 μg/mL) for 4-6 hours.
- Wash cells to remove unbound PTAs and irradiate with NIR laser (808 nm, 0.5-1.0 W/cm², 5-10 minutes).
- Include controls: no treatment, laser only, PTAs only, and non-targeted PTAs plus laser.
- Monitor temperature changes during irradiation using infrared thermal camera [119].
Assessment of Therapeutic Efficacy:
- Evaluate cell viability 24 hours post-PTT using Calcein-AM (live, green) and propidium iodide (dead, red) staining.
- Quantify apoptosis and necrosis by Annexin V/PI flow cytometry.
- Assess CSC elimination efficiency through post-treatment sphere-forming assay [119] [114].
- Examine effects on stemness markers (OCT4, NANOG, SOX2) via immunofluorescence and Western blotting.
Combination Therapy Evaluation:
- Investigate synergistic effects with chemotherapy (e.g., paclitaxel, doxorubicin) by administering drugs 2 hours before or after PTT [119] [114].
- Evaluate immunogenic cell death markers (CRT exposure, ATP release, HMGB1) following PTT treatment [119].
Research Reagent Solutions for Photothermal Therapy
Table 2: Essential Reagents for Photothermal Therapy Research
| Reagent/Category | Specific Examples | Function/Mechanism | Key Parameters |
|---|---|---|---|
| Inorganic PTAs | Gold nanorods, Gold nanostars, Gold-silica nanoshells | Convert NIR light to localized heat via LSPR | Aspect ratio (3-4), LSPR peak (808 nm) |
| Organic PTAs | Indocyanine green, Aza-BODIPY derivatives, SCOPAs | Biodegradable NIR absorbers with metabolic clearance | High PCE, tumor-specific activation |
| Targeting Ligands | Anti-CD44, Anti-CD133, Peptides (RGD, GE11) | Enhance CSC-specific binding and internalization | Conjugation density, binding affinity |
| NIR Lasers | Diode lasers (808 nm) | Provide precise photonic energy for PTT | Wavelength (NIR-I/NIR-II), power density (0.1-1 W/cm²) |
| Thermal Cameras | Infrared imaging systems | Monitor real-time temperature changes during PTT | Thermal sensitivity < 50 mK |
| Viability Assays | Calcein-AM/PI, MTT, Annexin V/PI | Assess cell death and viability post-PTT | Multiparametric analysis |
| CSC Functional Assays | Sphere-forming assay, ALDEFLUOR | Evaluate effects on CSC self-renewal capacity | Quantitative colony counting |
Figure 2: Photothermal Therapy Mechanism. The diagram illustrates how different photothermal agents convert NIR light to heat, inducing temperature-dependent biological effects that lead to cancer cell elimination.
Epigenetic Modulators: Reprogramming CSC Identity
Epigenetic Regulation of Stemness and Plasticity
CSCs utilize dynamic epigenetic modifications to maintain their stem-like properties, drive tumor heterogeneity, and evade therapeutic pressure [120] [35]. These reversible changes—including DNA methylation, histone modifications, RNA modifications, and non-coding RNA regulation—create a plastic chromatin state that allows CSCs to transition between different functional states in response to microenvironmental cues and therapeutic insults [120].
The polycomb repressive complexes (PRC1 and PRC2) play particularly important roles in maintaining CSC identity. PRC2, through its catalytic component EZH2, deposits the repressive H3K27me3 mark at key differentiation promoters, locking cells in a stem-like state [35]. BMI1, a core component of PRC1, contributes to both stemness maintenance and DNA damage response through H2AK119ub deposition at DNA lesions, promoting repair via homologous recombination [35]. This dual function explains the enhanced resistance of CSCs to genotoxic therapies.
DNA methylation patterns also significantly influence CSC behavior. Hypermethylation of tumor suppressor gene promoters can silence differentiation programs, while hypomethylation of oncogenic and developmental genes can reinforce stemness pathways [120]. Additionally, RNA modifications—particularly N6-methyladenosine (m6A)—have emerged as critical regulators of CSC metabolism, self-renewal, and drug resistance through effects on RNA stability, translation efficiency, and splicing [120].
The interplay between DNA damage repair and epigenetic landscape represents another key mechanism in CSC maintenance. DNA double-strand breaks induced by chemotherapy can reshape chromatin organization through mis-restoration during repair, ultimately altering cell identity and promoting adaptive transitions to resistant states [35]. This dynamic relationship between genomic integrity and epigenetic regulation provides CSCs with a robust mechanism for surviving therapeutic assault.
Experimental Protocol for Epigenetic Targeting
Epigenetic Drug Screening in CSCs:
- Culture CSCs as spheroids in low-attachment plates with stem cell-permissive media [120] [35].
- Treat CSCs with epigenetic inhibitors: EZH2 inhibitors (GSK126, 1-5 μM; Tazemetostat, 5-10 μM), BET bromodomain inhibitors (JQ1, 0.5-2 μM; I-BET151, 1-5 μM), or DNA methyltransferase inhibitors (Azacitidine, 0.5-5 μM; Decitabine, 0.1-1 μM) for 72-96 hours [120].
- Assess effects on sphere-forming capacity through limiting dilution assays.
- Evaluate differentiation markers via flow cytometry and immunofluorescence.
Combination Therapy Studies:
- Pre-treat CSCs with epigenetic modulators for 24-48 hours before adding conventional chemotherapeutics (e.g., cisplatin, temozolomide, doxorubicin) [120].
- Assess synergistic effects using Chou-Talalay combination index analysis.
- Investigate sequential versus concurrent administration schedules.
Molecular Profiling:
- Perform RNA-seq to examine transcriptome changes following epigenetic modulation.
- Conduct ChIP-seq for H3K27ac, H3K4me3, and H3K27me3 to map epigenetic landscape alterations.
- Analyze DNA methylation patterns using whole-genome bisulfite sequencing [120] [35].
- Integrate multi-omics data to identify key regulatory nodes in CSC maintenance.
Functional Validation:
- Knock down target genes using CRISPR/Cas9 or siRNA to validate their role in CSC maintenance.
- Perform in vivo limiting dilution transplantation assays to quantify effects on tumor-initiating capacity [35].
Research Reagent Solutions for Epigenetic Studies
Table 3: Essential Reagents for Epigenetic Research
| Reagent/Category | Specific Examples | Function/Mechanism | Working Concentration |
|---|---|---|---|
| EZH2 Inhibitors | GSK126, Tazemetostat, UNC1999 | Inhibit H3K27me3 deposition to promote differentiation | 1-10 μM |
| BET Inhibitors | JQ1, I-BET151, OTX015 | Displace BET proteins from acetylated chromatin | 0.5-5 μM |
| DNMT Inhibitors | Azacitidine, Decitabine | Reduce DNA methylation to reactivate silenced genes | 0.1-5 μM |
| HDAC Inhibitors | Vorinostat, Panobinostat | Increase histone acetylation and gene expression | 1-10 μM |
| Chromatin Profiling | H3K27me3, H3K4me3, H3K27ac antibodies | Map activating and repressive chromatin states | Antibody-dependent |
| DNA Methylation Assays | Bisulfite conversion kits, Methylation arrays | Analyze genome-wide DNA methylation patterns | N/A |
| Multi-omics Integration | scRNA-seq, ATAC-seq, CUT&Tag | Resolve cellular heterogeneity and regulatory networks | N/A |
Figure 3: Epigenetic Regulation of Cancer Stem Cells. The diagram illustrates how different epigenetic mechanisms maintain CSC properties and how targeted interventions can disrupt these regulatory networks.
Comparative Analysis and Integration Strategies
Quantitative Comparison of Therapeutic Modalities
Table 4: Comparative Analysis of Novel Therapeutic Modalities Against CSCs
| Parameter | Ferroptosis Inducers | Photothermal Therapy | Epigenetic Modulators |
|---|---|---|---|
| Primary Molecular Target | System Xc⁻/GPX4, Iron metabolism | Physical hyperthermia, Protein denaturation | Chromatin modifiers, DNA/histone methylation |
| Key Vulnerabilities Exploited | Altered iron metabolism, Lipid peroxidation defense | Differential heat sensitivity, Physical ablation | Epigenetic plasticity, Transcriptional dependencies |
| Resistance Risk | Low to moderate (compensatory pathways may emerge) | Very low (physical mechanism) | Moderate to high (epigenetic rewiring) |
| Therapeutic Index | Moderate (normal cells affected at higher doses) | High (with targeted PTAs) | Variable (context-dependent) |
| Time to Effect | Hours to days | Minutes to hours | Days to weeks |
| Combination Potential | High with chemo, radio, and immunotherapy | High with chemo, immune, and targeted therapy | High with most conventional therapies |
| Clinical Translation Stage | Early clinical trials ongoing | Advanced preclinical and early clinical | Several FDA-approved agents |
| Key Challenges | Tumor-specific delivery, On-target toxicity | Tissue penetration, Heat dissipation | Cellular plasticity, Adaptive resistance |
Integrated Workflow for Combination Therapy Development
The complementary mechanisms of these three modalities present significant opportunities for combination strategies that simultaneously target multiple vulnerabilities of CSCs. Below is an integrated experimental workflow for developing such combination therapies:
Phase 1: Target Validation and Single-Agent Screening
- Establish CSC-enriched models from relevant cancer types (e.g., TNBC, glioblastoma, pancreatic cancer)
- Screen ferroptosis inducers, PTT agents, and epigenetic modulators as single agents
- Identify synergistic pairs based on mechanistic complementarity [113] [120] [114]
Phase 2: Sequential Therapy Optimization
- Test different administration sequences (epigenetic priming followed by ferroptosis induction, PTT followed by epigenetic modulation)
- Identify optimal timing windows using functional CSC assays (sphere formation, tumor initiation)
- Validate epigenetic plasticity changes using multi-omics approaches [120] [35]
Phase 3: Nanoplatform Development
- Design multifunctional nanoparticles incorporating iron oxide (ferroptosis), gold components (PTT), and epigenetic drug payloads
- Functionalize with CSC-targeting ligands (CD44, CD133) and tumor-penetrating peptides
- Optimize release kinetics for sequential drug delivery [115] [94] [114]
Phase 4: In Vivo Validation
- Evaluate antitumor efficacy and CSC elimination in patient-derived xenograft models
- Assess effects on tumor initiation and metastasis in limiting dilution assays
- Monitor therapy-induced plasticity and adaptive resistance mechanisms [35] [114]
This integrated approach leverages the unique strengths of each modality: epigenetic modulators to "prime" CSCs by altering their transcriptional state and making them vulnerable to subsequent challenges, ferroptosis inducers to exploit the metabolic dependencies of CSCs, and PTT to physically eliminate CSCs that survive pharmaceutical interventions. The sequential application of these complementary mechanisms presents a promising strategy for addressing the profound clinical challenge of CSC-mediated treatment resistance.
The persistent challenge of therapeutic resistance in oncology necessitates innovative approaches that specifically target the root causes of treatment failure. Cancer stem cells, with their unique biological properties and dynamic plasticity, represent a critical therapeutic target for achieving durable responses and preventing recurrence. The three modalities discussed in this technical guide—ferroptosis inducers, photothermal therapy, and epigenetic modulators—each offer distinct mechanisms for attacking CSCs through their specific vulnerabilities.
Ferroptosis inducers exploit the altered iron metabolism and redox homeostasis of CSCs, photothermal therapy utilizes physical energy to bypass conventional resistance mechanisms, and epigenetic modulators reprogram the transcriptional networks that maintain stemness. Importantly, these approaches are not mutually exclusive; rather, they can be strategically combined to create multimodal regimens that simultaneously target multiple aspects of CSC biology. The integration of nanomaterial-based delivery systems further enhances the specificity and efficacy of these interventions while minimizing off-target effects.
As research in this field advances, the rational design of combination therapies based on comprehensive understanding of CSC biology, tumor microenvironment interactions, and therapy-induced plasticity will be essential for overcoming the formidable challenge of therapeutic resistance. The experimental frameworks and methodologies outlined in this guide provide a foundation for developing these next-generation therapeutic strategies that ultimately aim to improve outcomes for cancer patients.
Comparative Analysis of Therapeutic Efficacy, Toxicity, and Biomarker-Driven Strategies
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with self-renewal capacity, differentiation potential, and enhanced resistance to conventional therapies, driving tumor initiation, progression, metastasis, and recurrence [1] [80]. These cells exhibit unique biological properties, including metabolic plasticity, interaction with the tumor microenvironment (TME), and efficient DNA repair mechanisms that enable them to survive conventional cancer treatments and initiate new tumor growth [1] [19]. The presence of CSCs within tumors creates significant therapeutic challenges due to their contribution to intratumoral heterogeneity, therapy resistance, and disease relapse, making them critical targets for innovative cancer treatment strategies [1] [31].
Understanding CSC biology and developing effective therapeutic approaches requires a multifaceted strategy that integrates biomarker identification, signaling pathway inhibition, and advanced therapeutic modalities. This review provides a comprehensive analysis of current and emerging CSC-targeted therapies, focusing on their efficacy, toxicity profiles, and the biomarker-driven approaches that enable precision targeting of these resilient cell populations. By examining both conventional and novel therapeutic platforms, we aim to elucidate the most promising directions for overcoming CSC-mediated treatment resistance in clinical oncology.
Therapeutic Approaches: Efficacy and Toxicity Profiles
Conventional cancer therapies, including chemotherapy and radiation, primarily target rapidly dividing cells but often fail to eradicate quiescent CSCs, leading to tumor recurrence and metastasis [121] [19]. The development of CSC-specific therapies focuses on targeting unique CSC properties, including surface markers, signaling pathways, and metabolic dependencies, while minimizing toxicity to normal stem cells and healthy tissues [1] [94]. The table below provides a comparative analysis of major therapeutic classes targeting CSCs, their mechanisms of action, efficacy metrics, and associated toxicity concerns.
Table 1: Comparative Analysis of CSC-Targeted Therapeutic Approaches
| Therapeutic Class | Mechanism of Action | Efficacy Strengths | Toxicity/Limitations |
|---|---|---|---|
| Signaling Pathway Inhibitors (e.g., Wnt, Notch, Hedgehog inhibitors) | Targets self-renewal pathways critical for CSC maintenance [19] [31]. | Reduces CSC self-renewal and tumorigenicity; potential for combination therapies [31]. | On-target toxicity to normal stem cells; compensatory pathway activation [1] [19]. |
| CAR-T Cell Therapies | Engineered T-cells target CSC-specific surface antigens (e.g., EpCAM, CD133) [1] [8]. | Potent, specific elimination of CSCs; long-term immunological memory [1] [122]. | Cytokine release syndrome; on-target/off-tumor toxicity against normal cells expressing target [8]. |
| Nanoparticle-Based Delivery | Enables targeted delivery of cytotoxic drugs or RNAi to CSCs via specific ligands [94]. | Bypasses ABC transporter-mediated efflux; reduces off-target effects [94]. | Potential for immune reactions; complex manufacturing and scalability challenges [94]. |
| Dual Metabolic Inhibitors | Simultaneously targets multiple metabolic pathways (e.g., glycolysis & OXPHOS) [1]. | Overcomes CSC metabolic plasticity; effective against quiescent CSCs [1]. | High potential for toxicity to normal tissues with high metabolic demands [1]. |
| Immunomodulatory Agents | Reverses CSC-mediated immunosuppression; enhances immune recognition [80]. | Synergizes with immunotherapy; targets CSC niche [122] [80]. | Risk of autoimmune reactions; variable patient response [8]. |
The comparative analysis reveals that while each therapeutic class demonstrates unique strengths in targeting CSCs, they also present distinct challenges. Signaling pathway inhibitors effectively disrupt essential self-renewal mechanisms but risk damaging normal stem cell populations that depend on the same pathways [1] [19]. Immunotherapeutic approaches like CAR-T cells offer high specificity but face limitations due to the shared expression of CSC markers on normal cells [8] [122]. Nanoparticle-based systems and combination therapies represent promising strategies to enhance therapeutic specificity and overcome multiple resistance mechanisms simultaneously [94].
Biomarker-Driven Strategies and Personalized Medicine
Biomarker discovery and validation are fundamental to developing precise CSC-targeted therapies. CSC identification relies on a combination of surface markers, functional assays, and molecular profiling to isolate and characterize these rare cell populations within tumors [8] [80]. The integration of multi-OMICS technologies, including single-cell sequencing and spatial transcriptomics, has significantly advanced our understanding of CSC heterogeneity and provided novel biomarkers for therapeutic targeting [1] [123].
Table 2: Key CSC Biomarkers and Their Clinical Applications
| Biomarker Category | Key Examples | Detection Methods | Clinical/Research Utility |
|---|---|---|---|
| Surface Markers | CD44, CD133, CD24, EpCAM, CD90 [8] [122] | Flow cytometry, immunohistochemistry [80] | CSC isolation and enrichment; therapeutic targeting [8] [124]. |
| Functional Markers | ALDH1 activity, ABC transporter expression [121] [122] | Aldefluor assay, dye efflux assays [80] | Identification of therapy-resistant CSC populations [121] [19]. |
| Transcriptional Factors | OCT4, SOX2, NANOG, KLF4 [94] [8] | Immunofluorescence, RNA sequencing [1] | Assessment of stemness potential; prognosis [94] [31]. |
| Signaling Pathway Activation | β-catenin, Notch intracellular domain [19] [31] | Pathway reporter assays, phospho-protein detection [31] | Patient stratification for pathway-targeted therapies [1] [31]. |
| Metabolic Markers | Mitochondrial mass, ROS levels [1] | Metabolic flux analysis, fluorescent probes [1] | Identification of metabolic vulnerabilities for targeting [1]. |
Emerging hypothesis-free biomarker discovery approaches that leverage AI-driven analysis of multi-OMICS data are revolutionizing CSC research by identifying novel biomarkers without preconceived notions of their relevance [123]. These data-driven methods complement traditional hypothesis-driven research by uncovering unexpected biomarkers and relationships in the complex landscape of cancer biology, potentially accelerating the development of personalized therapeutic strategies [123].
Experimental Models and Methodologies
CSC Isolation and Characterization Protocols
Reliable isolation and characterization of CSCs are prerequisite for evaluating therapeutic efficacy and resistance mechanisms. The following experimental workflows represent standardized methodologies in CSC research:
Surface Marker-Based Isolation using Flow Cytometry
- Principle: Exploits unique cell surface antigen expression to physically separate CSC populations [80].
- Protocol: Single-cell suspensions from fresh tumor tissues are incubated with fluorochrome-conjugated antibodies against CSC markers (e.g., CD44, CD133, EpCAM). Labeled cells are sorted using fluorescence-activated cell sorting (FACS). The tumor-initiating capacity of sorted populations is validated through in vivo limiting dilution assays in immunocompromised mice [122] [80].
- Applications: Isolation of pure CSC populations for functional studies, transcriptomic profiling, and drug screening [124] [80].
Aldefluor Assay for ALDH Activity Detection
- Principle: Measures intracellular aldehyde dehydrogenase (ALDH) enzyme activity, a functional marker of CSCs in various cancers [121] [122].
- Protocol: Cells are incubated with BODIPY-aminoacetaldehyde substrate, which is converted to a fluorescent product by intracellular ALDH. The ALDH-high population is isolated via FACS. Specificity is confirmed using ALDH inhibitor diethylaminobenzaldehyde (DEAB) as a control [80].
- Applications: Identification of CSCs with enhanced detoxification capacity and resistance to chemotherapeutic agents [121] [122].
Sphere Formation Assay
- Principle: Evaluates self-renewal capacity under non-adherent, serum-free conditions that favor stem cell proliferation [80].
- Protocol: Single cells are plated in ultra-low attachment plates with serum-free medium supplemented with growth factors (EGF, bFGF). Primary spheres are counted after 7-14 days. For serial passaging, spheres are dissociated and re-plated to assess self-renewal capacity [80].
- Applications: Quantification of self-renewal potential, screening for compounds that target CSCs, and studying CSC biology in vitro [124] [80].
In Vivo Tumorigenicity and Therapy Response Assessment
The gold standard for validating CSC properties remains in vivo tumorigenicity assays [80]. Key methodologies include:
Limiting Dilution Transplantation Assay
- Purpose: Quantitatively measure the frequency of tumor-initiating cells [80].
- Protocol: Serial dilutions of candidate CSC populations are transplanted into immunocompromised mice (e.g., NOD/SCID, NSG). Tumor incidence is monitored over several months. Tumor-initiating cell frequency is calculated using statistical methods like ELDA software [80].
- Endpoint Analysis: Tumors are examined for histology, marker expression, and heterogeneity to confirm recapitulation of original tumor [122] [80].
Patient-Derived Xenograft (PDX) Models for Therapeutic Testing
- Purpose: Maintain tumor heterogeneity and CSC hierarchy for preclinical drug testing [1].
- Protocol: Fresh tumor fragments are implanted into immunodeficient mice. Upon engraftment, tumors are passaged serially. For drug testing, tumor-bearing mice are treated with investigational agents, and response is monitored through tumor volume measurements and endpoint analysis of CSC frequency via flow cytometry or IHC [1].
- Advantages: Preserves original tumor heterogeneity and drug response patterns more accurately than cell line models [1].
Visualization of Core Concepts
Key Signaling Pathways in Cancer Stem Cells
The following diagram illustrates the major signaling pathways that regulate self-renewal, survival, and therapeutic resistance in CSCs. These pathways represent prime targets for therapeutic intervention.
Experimental Workflow for CSC Therapeutic Development
This workflow outlines the integrated process from CSC identification and biomarker discovery to therapeutic development and validation, highlighting key decision points in the pipeline.
Research Reagent Solutions
The following table outlines essential reagents, tools, and platforms used in CSC research and therapeutic development. These resources enable the isolation, characterization, and targeting of CSCs in experimental and preclinical settings.
Table 3: Essential Research Reagents and Platforms for CSC Studies
| Reagent/Platform | Specific Examples | Research Application |
|---|---|---|
| CSC Surface Marker Antibodies | Anti-CD44, Anti-CD133, Anti-CD24, Anti-EpCAM [8] [122] | Flow cytometry, immunohistochemistry, immunomagnetic separation of CSCs [80]. |
| Pathway-Specific Inhibitors | Wnt inhibitors (e.g., LGK974), Notch inhibitors (e.g., DAPT), Hedgehog inhibitors (e.g., GDC-0449) [19] [31] | Functional validation of signaling pathways; combination therapy studies [31]. |
| Patient-Derived Organoid Models | 3D organoid cultures from various cancer types [1] [80] | Disease modeling, drug screening, personalized therapy testing while preserving tumor heterogeneity [1]. |
| Single-Cell OMICS Platforms | Single-cell RNA sequencing, ATAC-seq [1] [123] | Dissecting CSC heterogeneity, identifying novel biomarkers, understanding therapy resistance mechanisms [1]. |
| Nanoparticle Delivery Systems | Liposomes, polymeric nanoparticles, inorganic NCs [94] | Targeted drug delivery to CSCs, overcoming ABC transporter-mediated resistance [94]. |
The strategic targeting of cancer stem cells represents a paradigm shift in oncology, moving beyond bulk tumor reduction to addressing the root causes of therapeutic resistance and disease recurrence. The comparative analysis presented herein demonstrates that while significant challenges remain in selectively eliminating CSCs without damaging normal stem cell compartments, emerging approaches—particularly biomarker-driven strategies, nanotechnology, and immunotherapies—show considerable promise. The integration of advanced OMICS technologies, AI-driven biomarker discovery, and sophisticated experimental models will be crucial for advancing CSC-targeted therapies from bench to bedside. Future success in overcoming CSC-mediated treatment failure will likely depend on combinatorial approaches that simultaneously target multiple CSC vulnerabilities while preserving normal tissue function, ultimately enabling more durable responses and improved outcomes for cancer patients.
Conclusion
The pivotal role of cancer stem cells in fostering tumor heterogeneity and driving therapeutic resistance is unequivocal. Effectively targeting this resilient subpopulation is no longer a supplementary approach but a fundamental necessity for achieving durable cancer remissions and preventing relapse. The path forward requires an integrative strategy that combines foundational knowledge of CSC biology with advanced diagnostic tools and innovative therapeutic modalities. Future progress will depend on overcoming key challenges, including the dynamic plasticity of CSCs, the lack of universal biomarkers, and the need for therapies that selectively target CSCs without harming normal stem cells. The integration of AI-driven multi-omics analysis, the refinement of patient-derived organoid models, and the clinical development of combination therapies—such as dual metabolic inhibition with nanotechnology-based delivery—hold immense promise. By dismantling the defenses of CSCs, the biomedical research community can make transformative strides towards overcoming therapy resistance and ultimately improving survival for cancer patients.
References
- 1. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 2. Cancer stem cells: Bridging microenvironmental interactions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264091/]
- 3. Cancer stem cells: understanding tumor hierarchy and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5599210/]
- 4. Drug resistance and Cancer stem cells [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-020-00627-5]
- 5. Drug resistance mechanisms of cancer stem-like cells and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8992527/]
- 6. Deciphering Cancer Stem Cell Self-Renewal Pathways [https://pubmed.ncbi.nlm.nih.gov/40765762/]
- 7. Biomarkers and Targeted Therapy for Cancer Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842814/]
- 8. Cancer stem cells as a biomarker – A mini review [https://www.probiologists.com/article/cancer-stem-cells-as-a-biomarker-a-mini-review]
- 9. The spatial landscape of cancer hallmarks reveals patterns ... [https://www.sciencedirect.com/science/article/pii/S2211124724015808]
- 10. Recent advances in drug delivery systems for targeting ... [https://www.sciencedirect.com/science/article/pii/S2211383520307322]
- 11. The Role of Cancer Stem Cell Markers in Ovarian Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10778113/]
- 12. Cancer Stem Cell Markers, CD44 and ALDH1, for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9187836/]
- 13. Evaluation of CD44 and CD133 as cancer stem cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3981033/]
- 14. Prognostic impact of the expression of putative cancer stem ... [https://www.nature.com/articles/6605762]
- 15. The Clinical Significance of Cancer Stem Cell Markers ... [https://ar.iiarjournals.org/content/37/5/2541]
- 16. ALDH1-Bright Epithelial Ovarian Cancer Cells Are ... [https://www.sciencedirect.com/science/article/pii/S0002944011010790]
- 17. Drug resistance in cancer: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623568/]
- 18. Deciphering the Role of Cancer Stem Cells: Drivers of Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11815874/]
- 19. Cancer stem cells and tumor heterogeneity [https://www.sciencedirect.com/science/article/abs/pii/S1043466622001776]
- 20. Pharmacological modulation of stem cells signaling pathway ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04438-8]
- 21. Key roles of ubiquitination in regulating critical ... [https://www.sciencedirect.com/science/article/pii/S2352304224001089]
- 22. Hippo/YAP signaling's multifaceted crosstalk in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12263953/]
- 23. Dissecting Tumor Growth: The Role of Cancer Stem Cells ... [https://www.mdpi.com/2072-6694/14/4/976]
- 24. Hippo/YAP signaling pathway in colorectal cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1545952/full]
- 25. Cancer stem cells in focus: Deciphering the dynamic ... [https://www.sciencedirect.com/science/article/pii/S0304419X25001829]
- 26. Cancer Stem Cell Plasticity – A Deadly Deal [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2020.00079/full]
- 27. Dynamic equilibrium between cancer stem cells and non- ... [https://www.nature.com/articles/bjc2012126]
- 28. Tumor cell plasticity in targeted therapy-induced resistance [https://www.nature.com/articles/s41392-023-01383-x]
- 29. Mathematical Modeling of Plasticity and Heterogeneity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8178376/]
- 30. Patient-Derived Tumor Organoids to Model Cancer Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469014/]
- 31. Deciphering the Role of Cancer Stem Cells [https://www.mdpi.com/2072-6694/17/3/382]
- 32. A review of the role of CSCs and CSC-EXOs in increasing ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842825001623]
- 33. Intratumoral heterogeneity and drug resistance in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11917089/]
- 34. Intratumoral heterogeneity and drug resistance in cancer [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03734-w]
- 35. The interplay of DNA damage, epigenetics and tumour ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12484684/]
- 36. Unveiling the mechanisms and challenges of cancer drug ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01302-1]
- 37. Cancer cell plasticity and therapeutic resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465352/]
- 38. of Glioblastoma Isolation with Stem Cells Flow Cytometry [https://pubmed.ncbi.nlm.nih.gov/29392691/]
- 39. Fluorescence-activated cell sorting: An overview | Abcam [https://www.abcam.com/en-us/knowledge-center/flow-cytometry/fluorescence-activated-cell-sorting-overview]
- 40. Generating Quantitative Cell Identity Labels with Marker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5774653/]
- 41. Nanomaterials targeting cancer stem cells to overcome ... [https://pubmed.ncbi.nlm.nih.gov/40548119/]
- 42. Tumorsphere Formation Assay: A Cancer Stem-Like Cell Characterization in Pediatric Brain Cancer Medulloblastoma | SpringerLink [https://link.springer.com/protocol/10.1007/978-1-0716-3373-1_17]
- 43. High-Throughput Single-Cell Derived Sphere Formation for Cancer Stem-Like Cell Identification and Analysis | Scientific Reports [https://www.nature.com/articles/srep27301]
- 44. Chemoresistance is associated with cancer stem cell-like properties and epithelial-to-mesenchymal transition in pancreatic cancer cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/22993328/]
- 45. 4.10. Sphere Formation Assay [https://bio-protocol.org/exchange/minidetail?id=6806703&type=30]
- 46. ALDEFLUOR™ Kit for ALDH Assays [https://www.stemcell.com/products/brands/aldefluor-aldh-assay.html]
- 47. PET-leveraged ALDH probe toward cancer stem cells [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb01253h]
- 48. Predicting resistance to chemotherapy using chromosomal ... [https://www.nature.com/articles/s41588-025-02233-y]
- 49. Assessing Tumorigenicity in Stem Cell-Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376867/]
- 50. Limiting dilution assay to quantify the self-renewal potential ... [https://www.sciencedirect.com/science/article/abs/pii/S0091679X22000577]
- 51. NAD(P)H Quinone Oxidoreductase-1 Expression Promotes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10047941/]
- 52. The strategies to cure cancer patients by eradicating cancer ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01867-y]
- 53. Targeting cancer stem cells for reversing therapy resistance [https://www.nature.com/articles/s41392-020-00430-1]
- 54. Single-cell multi-omics and machine learning for dissecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570030/]
- 55. Clinical application of single‐cell RNA sequencing in disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576031/]
- 56. Unraveling the future of genomics: CRISPR, single-cell omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12021818/]
- 57. Use of CRISPR-based screens to identify mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10722205/]
- 58. Base editing screens define the genetic landscape of ... [https://www.nature.com/articles/s41588-024-01948-8]
- 59. A CRISPR/Cas9-based enhancement of high-throughput ... [https://www.nature.com/articles/s41467-025-59880-2]
- 60. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 61. 3D tumor cultures for drug resistance and screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11927140/]
- 62. Breaking the mold: 3D cell cultures reshaping the future of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1507388/full]
- 63. Organoids as Next-Generation Models for Tumor ... [https://www.mdpi.com/2674-1172/4/4/23]
- 64. Cancer Organoids as reliable disease models to drive ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-024-03258-7]
- 65. Implications for Therapy Resistance and Tumor Recurrence [https://www.sciencedirect.com/science/article/abs/pii/S1368764625001189]
- 66. Cancer cell plasticity and therapeutic resistance - Hereditas [https://hereditasjournal.biomedcentral.com/articles/10.1186/s41065-025-00564-8]
- 67. Patient-derived organoids in precision cancer medicine [https://www.sciencedirect.com/science/article/pii/S266663402400343X]
- 68. Patient-derived tumor organoids: a new avenue for ... [https://www.nature.com/articles/s12276-024-01272-5]
- 69. Biology of stem cell paradox: a double-edged sword ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03981-x]
- 70. ABC Transporters in Cancer Stem Cells - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5713331/]
- 71. Cancer Stem Cells as a Potential Target to Overcome ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.00764/full]
- 72. Revisiting the role of efflux pumps in multidrug-resistant cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC6622180/]
- 73. New trends for overcoming ABCG2/BCRP-mediated ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-015-0275-x]
- 74. The role of ABCG2 in health and disease: Linking cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S002432052400835X]
- 75. Strategies to Inhibit ABCB1- and ABCG2-Mediated Efflux ... [https://jnm.snmjournals.org/content/58/1/117]
- 76. Revisiting strategies to target ABC transporter-mediated ... [https://pubmed.ncbi.nlm.nih.gov/41024626/]
- 77. Structural Basis of the Allosteric Inhibition of Human ... [https://www.sciencedirect.com/science/article/pii/S0022283623003443]
- 78. Metabolic Plasticity and Cancer Stem Cell ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504402/]
- 79. Cancer stem cell metabolism: target for cancer therapy [https://www.bmbreports.org/view.html?uid=1269&vmd=Full]
- 80. Cancer stem cells in personalized therapy [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1619597/full]
- 81. Altered metabolism in cancer: insights into energy pathways ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02119-3]
- 82. Mitochondrial and metabolic alterations in cancer cells [https://www.sciencedirect.com/science/article/pii/S0171933522000280]
- 83. EMT and cancer stem cells: Drivers of therapy resistance ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764625000792]
- 84. Epithelial-to-mesenchymal transition (EMT) and cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12144846/]
- 85. Advances in research regarding epithelial-mesenchymal ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1583255/full]
- 86. New Insights into the Crossroads between EMT and Stemness in the Context of Cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/26985909/]
- 87. Construction of the cancer cell continuum reveals hybrid ... [https://www.nature.com/articles/s41417-025-00991-9]
- 88. Communication Between Epithelial–Mesenchymal Plasticity and Cancer Stem Cells: New Insights Into Cancer Progression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8097085/]
- 89. EMT imparts cancer stemness and plasticity: new perspectives and therapeutic potential - PubMed [https://pubmed.ncbi.nlm.nih.gov/33049669/]
- 90. Hypoxic microenvironment in cancer [https://www.nature.com/articles/s41392-023-01332-8]
- 91. Breaking hypoxic barrier: Oxygen-supplied nanomaterials for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495343/]
- 92. Unraveling the immune evasion mechanisms in the tumor ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597202/full]
- 93. Statistical analysis of spatial patterns in tumor ... [https://www.nature.com/articles/s41467-025-57943-y]
- 94. Nanomaterials targeting cancer stem cells to overcome drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178904/]
- 95. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 96. Overcoming Physiological Barriers to Nanoparticle Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6928054/]
- 97. Nanotherapeutics in Neuropathologies - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8573747/]
- 98. Drug delivery | Nature Nanotechnology [https://www.nature.com/subjects/drug-delivery/nnano]
- 99. The role of stem cells in precision medicine: next-generation ... [https://jenci.springeropen.com/articles/10.1186/s43046-025-00328-5]
- 100. CAR-T cell therapy for cancer: current challenges and ... [https://www.nature.com/articles/s41392-025-02269-w]
- 101. CAR-T cell therapy: current limitations and potential ... [https://www.nature.com/articles/s41408-021-00459-7]
- 102. Combination Immunotherapy with CAR T Cells and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7171534/]
- 103. CAR-T cells and checkpoint inhibitors: ripping out the ... [https://www.fredhutch.org/en/news/spotlight/2024/02/crd-hirayama-bloodadv.html]
- 104. Cancer resistance to immunotherapy: What is the role ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9771758/]
- 105. Cancer stem cells and niches: challenges in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02265-2]
- 106. Cancer Stem Cells Decide the Fate of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12461067/]
- 107. Fully equipped CARs to address tumor heterogeneity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11180895/]
- 108. CAR-T cells in solid tumors: Challenges and breakthroughs [https://www.sciencedirect.com/science/article/pii/S2666379125004264]
- 109. Regulation and signaling pathways in cancer stem cells [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01877-w]
- 110. PI3K/AKT/mTOR signaling transduction pathway and targeted ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01827-6]
- 111. Dual PI3K and Wnt pathway inhibition is a synergistic ... [https://www.nature.com/articles/s41523-017-0016-8]
- 112. DUAL INHIBITION OF PI3K/AKT AND mTOR SIGNALING IN ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3267899/]
- 113. Targeting ferroptosis in cancer stem cells: A novel strategy to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12354820/]
- 114. Emerging strategies in engineering nanomaterials for ... [https://www.sciencedirect.com/science/article/pii/S1385894725119335]
- 115. Nanoparticle-Mediated Ferroptosis for Cancer Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570996/]
- 116. Advances in novel cell death mechanisms in breast cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02445-0]
- 117. Ferroptosis in ocular diseases: mechanisms, crosstalk with ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1608975/full]
- 118. Ferroptosis: The dawn of reversing drug resistance in ... [https://www.sciencedirect.com/science/article/pii/S2352304225003629]
- 119. Avenues for integrating photothermal therapy in cancer clinic [https://www.nature.com/articles/s42004-025-01705-w]
- 120. Targeting epigenetic regulators as a promising avenue to ... [https://www.nature.com/articles/s41392-025-02266-z]
- 121. Cancer Stem Cells (CSCs) in Drug Resistance and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5850899/]
- 122. Therapeutic Strategies Targeting Cancer Stem Cells and ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2019.01104/full]
- 123. Hypothesis-Free Biomarker Discovery in Oncology [https://blog.crownbio.com/hypothesis-free-biomarker-discovery-in-oncology]
- 124. Biomarkers, isolation methods, and therapeutic ... [https://www.sciencedirect.com/science/article/pii/S2949713225000060]