ddPCR for Rare Mutation Detection: A Comprehensive Guide for Precision Oncology and Biomarker Research
Droplet Digital PCR (ddPCR) has emerged as a powerful technology for the precise detection and absolute quantification of rare mutations, revolutionizing applications in liquid biopsies, cancer monitoring, and disease research.
ddPCR for Rare Mutation Detection: A Comprehensive Guide for Precision Oncology and Biomarker Research
Abstract
Droplet Digital PCR (ddPCR) has emerged as a powerful technology for the precise detection and absolute quantification of rare mutations, revolutionizing applications in liquid biopsies, cancer monitoring, and disease research. This article provides a comprehensive overview for researchers and drug development professionals, covering the foundational principles of ddPCR, its core methodology and diverse applications in detecting circulating tumor DNA (ctDNA) and monitoring treatment response, practical troubleshooting and optimization strategies, and a critical validation against other technologies like qPCR and NGS. By synthesizing the latest evidence and future directions, this guide aims to equip scientists with the knowledge to leverage ddPCR's high sensitivity and reproducibility for advancing precision medicine.
The Power of Precision: Understanding ddPCR and Its Role in Rare Mutation Analysis
Digital PCR (dPCR) represents a paradigm shift in nucleic acid quantification, moving from the relative measurements of its predecessors to a calibration-free method of absolute quantification. This capability is particularly transformative for detecting rare mutations in cancer research and drug development, where sensitivity and precision are paramount [1] [2]. This guide details the core technical principles of dPCR, from sample partitioning to final calculation, framing them within the context of advanced research applications.
The Evolution of PCR: From qPCR to Digital Absolute Quantification
The journey to dPCR began with conventional Polymerase Chain Reaction (PCR), an endpoint method that provides semi-quantitative information. The development of quantitative real-time PCR (qPCR) introduced relative quantification by monitoring amplification in real-time and comparing results to a standard curve [1] [2]. However, qPCR's reliance on calibration curves makes it susceptible to efficiency variations, impacting accuracy and reproducibility [2].
Digital PCR addresses these limitations by redefining the approach to measurement. The foundational concept—partitioning a sample to isolate individual molecules—was explored in the 1990s and early 2000s using limiting dilutions in multi-well plates [1]. The term "digital PCR" was coined in 1999 by Bert Vogelstein's team, who used this method to detect cancer mutations [1] [3]. Subsequent advancements in microfluidics enabled the practical partitioning of samples into thousands to millions of nanoliter- or picoliter-scale reactions, leading to the modern dPCR platforms widely used today [1] [3].
The table below summarizes the key distinctions between qPCR and dPCR.
Table: Fundamental Differences Between qPCR and dPCR
| Feature | Quantitative PCR (qPCR) | Digital PCR (dPCR) |
|---|---|---|
| Quantification Basis | Relative to a standard curve | Absolute, based on Poisson statistics |
| Calibration | Requires calibration curve | Calibration-free |
| Measurement Type | Real-time (kinetic) | End-point |
| Signal Output | Continuous (Ct value) | Digital (positive/negative partition count) |
| Tolerance to Inhibitors | Lower | Higher [2] |
| Ideal Application | High-abundance target quantification | Rare event detection, absolute copy number [4] |
Core Technical Principles of dPCR
The power of dPCR stems from a simple yet powerful workflow that converts a continuous analog signal into a discrete digital one.
The Four-Step Workflow
The dPCR process can be broken down into four key steps:
- Partitioning: The PCR reaction mixture—containing the sample, primers, probes, mastermix, and enzymes—is randomly partitioned into a large number of individual reactions [1] [3]. Two main partitioning methods are used:
- Amplification: The partitioned samples undergo standard PCR thermal cycling. Partitions containing at least one copy of the target sequence will amplify it exponentially, while those without a target will not [2].
- End-point Fluorescence Analysis: After amplification, each partition is analyzed for fluorescence. In a probe-based assay, a fluorescent signal indicates a "positive" partition, while no signal indicates a "negative" partition [1] [2].
- Absolute Quantification using Poisson Statistics: The ratio of positive to total partitions is used to calculate the absolute concentration of the target in the original sample, applying Poisson statistics to account for the random distribution of molecules [1] [2].
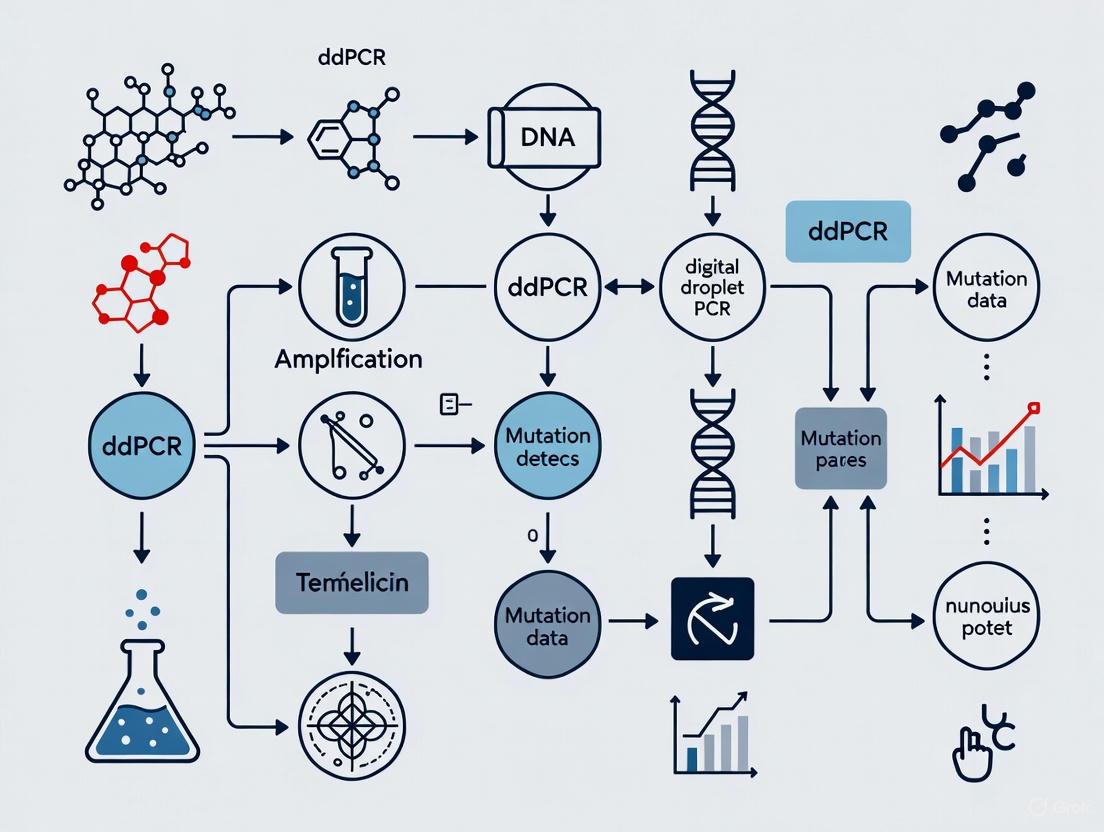
Diagram: The Core dPCR Workflow
The Statistical Foundation: Poisson Distribution
The absolute quantification in dPCR hinges on the fact that the distribution of target molecules across many partitions follows a Poisson distribution. This statistical model accounts for the randomness of the distribution, ensuring that some partitions will contain more than one target molecule, while others will contain none [2].
The fundamental formula for calculating the average number of target molecules per partition (λ) is: λ = -ln(1 - p) where p is the proportion of positive partitions (p = number of positive / total number of partitions) [2].
The absolute concentration in the original sample is then calculated as: Concentration = λ / (Partition Volume × Number of Partitions)
The precision of this measurement is intrinsically linked to the total number of partitions analyzed. A higher number of partitions yields a more precise and confident measurement, which is critical for detecting low-frequency mutations [4] [2]. The confidence interval for the estimated concentration can be determined using statistical methods like the Wilson score interval, which is preferred for its accuracy across all values of p [2].
A Practical Guide for Rare Mutation Detection
The following section provides a detailed experimental protocol for detecting a rare mutation, using the EGFR T790M mutation in non-small cell lung cancer (NSCLC) as a model. This mutation confers resistance to first-generation tyrosine kinase inhibitors, and its early detection is crucial for guiding treatment [4].
Assay and Experimental Design
- Assay Configuration: For rare mutation detection, a duplex probe-based assay is typically used. A single set of primers amplifies the region of interest. Two hydrolysis probes (e.g., TaqMan), each labeled with a different fluorophore, are used: one specific to the wild-type sequence and the other specific to the mutant allele [4].
- DNA Input and Sensitivity Calculation: Accurate DNA quantification is vital. The amount of input DNA directly determines the theoretical limit of detection (LOD) for the rare allele. For human genomic DNA, the number of copies can be calculated as: Number of copies = mass of DNA (in ng) / 0.003 (where 0.003 ng is the approximate mass of a single haploid human genome) [4].
- The theoretical sensitivity can be calculated as: Sensitivity = (Theoretical LOD of the system in copies/μL) / (Total concentration of target copies in the sample in copies/μL). For example, with 10 ng of human genomic DNA and a system LOD of 0.2 copies/μL, the theoretical sensitivity for detecting a mutant allele is approximately 0.15% [4].
Step-by-Step Protocol: EGFR T790M Detection
Table: Research Reagent Solutions for ddPCR
| Reagent / Component | Function / Description | Example Final Concentration |
|---|---|---|
| dPCR Mastermix | Provides DNA polymerase, dNTPs, reaction buffer, and MgCl₂. | 1X |
| Primer Set | Forward and reverse primers flanking the EGFR T790 locus. | 500 nM each [4] |
| Wild-Type Probe | Hydrolysis probe binding to the wild-type EGFR sequence. Labeled with fluorophore 1 (e.g., FAM). | 250 nM [4] |
| Mutant Probe | Hydrolysis probe binding to the mutant EGFR T790M sequence. Labeled with fluorophore 2 (e.g., Cy3). | 250 nM [4] |
| Reference Dye | Passive dye for normalization; required by some instruments. | As per manufacturer |
| Nuclease-Free Water | Solvent to achieve the final reaction volume. | - |
- PCR Mix Preparation: In a nuclease-free tube, assemble the reaction mixture according to the table above. Include necessary controls: a Non-Template Control (NTC), and monocolor controls for each probe to correct for fluorescence spillover [4].
- Partitioning: Load the PCR mix into the dedicated consumable of your dPCR system (e.g., a cartridge or chip) and perform the partitioning according to the manufacturer's protocol [4].
- Thermal Cycling: Transfer the partitions to a thermal cycler and run the following program, optimized for the EGFR T790M assay:
- Initial Denaturation: 95°C for 10 minutes (1 cycle)
- Amplification: 95°C for 30 seconds, then 62°C for 15 seconds (45 cycles) [4]
- Data Acquisition and Analysis:
- Read the partitions using your dPCR system's analyzer (either by planar imaging or in-line detection) [4].
- Apply a compensation matrix to correct for fluorescence spillover between channels if necessary [4].
- The software will automatically apply Poisson statistics to calculate the absolute concentration of both wild-type and mutant sequences in copies/μL. The mutant allelic frequency is then given by: (Mutant concentration / (Mutant + Wild-type concentration)) × 100.
Diagram: Rare Mutation Detection Logic
Advanced Applications in Research and Drug Development
The unique advantages of dPCR make it indispensable in modern biomedical research.
- Oncology and Liquid Biopsy: dPCR is exceptionally suited for analyzing circulating tumor DNA (ctDNA) from liquid biopsies. It can monitor treatment response by tracking the rise or fall of specific mutations and detect the emergence of resistance mutations (like EGFR T790M) with high sensitivity, enabling timely therapy switches [1] [5].
- Infectious Disease and Viral Load Monitoring: dPCR provides absolute quantification of pathogen load without standard curves, proving valuable for monitoring low-level persistent infections like HIV and for the precise detection of antibiotic-resistance genes in bacteria [1].
- Gene Therapy and Vector QC: In AAV-based gene therapy development, dPCR kits (e.g., VeriCheck) are used to precisely measure the titer of full versus empty viral capsids, a critical quality attribute that impacts therapeutic efficacy and safety [6].
- Mutation Scanning: Advanced techniques like COLD-ddPCR combine dPCR with co-amplification at lower denaturation temperature PCR. This method uses two wild-type probes with different fluorophores; a mutation anywhere under either probe causes a deviation in the FAM/HEX ratio, enabling scanning for unknown mutations within a target region [5].
Table: Commercial dPCR Platforms (Representative Examples)
| Brand | Instrument | Partitioning Method | Key Characteristics |
|---|---|---|---|
| Thermo Fisher Scientific | QuantStudio Absolute Q | Microchambers | Microfluidic Array Plate (MAP) with up to 20,480 partitions per sample [1]. |
| Bio-Rad Laboratories | QX Continuum ddPCR System | Droplets | Droplet-based system for a wide range of applications; for research use only [7]. |
| Qiagen | QIAcuity | Microchambers | Integrated instrument for partitioning, amplification, and imaging [1]. |
Digital PCR's core principle of partitioning samples for absolute, calibration-free quantification represents a significant advancement in molecular analysis. By combining physical partitioning with robust Poisson statistics, it provides researchers and drug developers with a tool of exceptional sensitivity and precision. As the technology continues to evolve with more integrated platforms and novel assays, its role in pushing the boundaries of rare mutation detection, disease monitoring, and advanced therapy development is set to expand further.
The polymerase chain reaction (PCR) represents one of the most transformative technologies in molecular biology, enabling exponential amplification of specific DNA sequences. From its inception as a qualitative tool, PCR technology has evolved through generations that progressively enhanced its quantitative capabilities. This evolution culminated in digital PCR (dPCR), a third-generation technology that provides absolute quantification of nucleic acids without requiring standard curves [3]. For researchers in rare mutation detection, this technological progression has been crucial, as it has steadily improved the sensitivity, accuracy, and precision required to identify genetic variants present in minute quantities within complex biological samples.
The journey from conventional PCR to digital PCR reflects a fundamental shift from relative to absolute quantification, with particular significance for applications like liquid biopsies, cancer biomarker detection, and monitoring minimal residual disease. This article traces the historical development, technical milestones, and practical implications of this evolution, with special emphasis on its critical role in advancing rare mutation research.
The Historical Progression of PCR Technologies
Conventional PCR: The Foundation of DNA Amplification
Conventional PCR, pioneered by Kary Mullis in 1986, revolutionized molecular biology by allowing specific DNA sequences to be amplified exponentially through repeated thermal cycling [3]. The fundamental process consists of three main steps per cycle: denaturation (separating DNA strands), annealing (binding primers to target sequences), and extension (synthesizing new DNA strands). This process relies on essential components including synthetic oligonucleotide primers, a thermostable DNA polymerase enzyme, and deoxyribonucleotide triphosphate monomers (dNTPs) [3].
Despite its revolutionary impact, conventional PCR presented significant limitations:
- End-point detection: Analysis occurred after all amplification cycles were complete, typically using gel electrophoresis with ethidium bromide staining to visualize amplified products [8]
- Semi-quantitative nature: Results were based on band intensity, providing only approximate quantification [3]
- Limited dynamic range: Detection relied on post-amplification processing, restricting accurate quantification [8]
- Low sensitivity: Difficulty detecting rare mutations in a background of wild-type sequences
These limitations restricted conventional PCR primarily to qualitative applications, such as confirming the presence or absence of specific DNA sequences, with limited utility for precise quantification needed in research and clinical diagnostics.
Quantitative PCR: Introducing Real-Time Monitoring
The development of quantitative PCR (qPCR), also known as real-time PCR, in 1992 by Russell Higuchi addressed several limitations of conventional PCR by enabling monitoring of amplification progress as it occurred [3]. This second-generation PCR technology incorporated fluorescent detection systems—either DNA-intercalating dyes like SYBR Green or sequence-specific fluorescent probes (TaqMan probes)—to track DNA accumulation during each cycle [8].
The key innovation of qPCR was the introduction of the threshold cycle (Cт) value, defined as the PCR cycle number at which the fluorescence signal crosses a predetermined threshold above background levels [8]. This value correlates inversely with the starting quantity of the target nucleic acid, enabling relative quantification when compared to standards of known concentration [9].
qPCR offered significant advantages over conventional PCR:
- Generation of quantitative data: Enabled measurement of DNA concentration across a wide dynamic range [8]
- Increased sensitivity: Capable of detecting down to a single copy of the target sequence [8]
- Elimination of post-PCR processing: Reduced hands-on time and contamination risk [8]
- Higher throughput capabilities: Allowed screening of more samples in less time
However, qPCR maintained important limitations, particularly its dependence on standard curves for quantification and susceptibility to amplification efficiency variations caused by PCR inhibitors [10]. These constraints motivated the development of more precise quantification technologies.
Digital PCR: Absolute Quantification at the Single-Molecule Level
Digital PCR (dPCR) represents the third generation of PCR technology, fundamentally changing the approach to nucleic acid quantification. The conceptual foundation for dPCR was established in 1992 when Morley and Sykes combined limiting dilution PCR with Poisson statistics to isolate, detect, and quantify single nucleic acid molecules [3]. In this pioneering work, the authors successfully detected mutated IgH rearranged heavy chain genes at frequencies as low as 2 targets in 160,000 wild-type sequences within bone marrow samples from leukemia patients [3].
The term "digital PCR" was formally coined in 1999 by Bert Vogelstein and colleagues, who developed a workflow using limiting dilution distributed across 96-well plates combined with fluorescence readout to detect RAS oncogene mutations in stool samples from colorectal cancer patients [3]. This milestone publication established the core principle of dPCR: partitioning a sample into many individual reactions such that each contains either zero or one (or a few) target molecules, followed by amplification and binary scoring of each partition as positive or negative for the target [3].
The period from 1999 to 2006 saw critical refinements to dPCR technology. In 2003, Vogelstein's group introduced the BEAMing technology (Beads, Emulsion, Amplification, and Magnetics), which simplified compartmentalization using water-in-oil droplets [3]. This approach involved encapsulating individual DNA molecules with magnetic beads coated with primers, permitting PCR amplification within droplets, with subsequent analysis by flow cytometry. This methodology significantly advanced rare mutation detection capabilities.
Technical Principles and Methodological Advances
Fundamental Working Principle of Digital PCR
Modern dPCR protocols follow four essential steps that enable absolute quantification of nucleic acids. The process begins with sample partitioning, where the PCR mixture containing the sample is distributed across thousands to millions of separate compartments [3]. This step relies on random distribution of target molecules among partitions according to Poisson statistics. The second step involves amplifying target molecules within each partition through conventional PCR thermal cycling. Unlike qPCR, which monitors amplification in real-time, dPCR uses end-point fluorescence detection as its third step, analyzing each partition after amplification is complete [3]. The final step applies Poisson statistical analysis to the ratio of positive to negative partitions, calculating the absolute concentration of the target nucleic acid in the original sample without requiring standard curves [3].
The mathematical foundation of dPCR relies on Poisson distribution statistics, which describe the probability of a target molecule being present in any given partition. The formula for calculating target concentration is:
[ \text{Concentration} = -\ln(1 - p) / V ]
Where "p" represents the proportion of positive partitions, and "V" is the volume of each partition. This approach enables absolute quantification, as the calculation depends only on the binary readout of each partition and the known partition volume.
Partitioning Methodologies: Droplet vs. Chip-Based Systems
Two primary partitioning methodologies have emerged in dPCR platforms, each with distinct advantages and applications:
Droplet Digital PCR (ddPCR) utilizes a water-oil emulsion system to create thousands of nanoliter-sized droplets, typically generating 20,000 or more partitions per sample [11]. The process involves microfluidic chips that leverage passive or active forces to break the aqueous/oil interface at high speeds (1-100 kHz) [3]. A critical consideration in ddPCR is droplet stability during thermal cycling, which requires appropriate surfactants to prevent coalescence, especially during temperature variations [3]. Bio-Rad's QX200/QX600/QX700 systems represent commercially successful implementations of this technology [11].
Chip-Based dPCR employs fixed arrays of microscopic wells or chambers embedded in solid chips. Examples include Applied Biosystems' AbsoluteQ system with approximately 20,000 fixed microwells and QIAGEN's QIAcuity system using nanoplates with similar partition counts [11]. This approach offers higher reproducibility and easier automation but is typically limited by fixed partition numbers and higher costs per run compared to droplet-based systems [3].
Detection and Analysis Systems
dPCR platforms utilize two primary readout methodologies for analyzing partitions. In-line detection, commonly used in ddPCR systems, involves flowing droplets sequentially through a microfluidic channel or capillary past a detection system consisting of a light source coupled with fluorescence detectors [3]. This approach allows analysis of a large number of droplets but requires precise flow control. Alternatively, planar imaging systems capture static snapshots of microchambers or microdroplets using fluorescence microscopy or scanning technologies [3]. Recent advances include 3D imaging and analysis techniques that enable faster assessment of larger numbers of droplets within reduced timeframes [3].
Comparative Analysis of PCR Generations
Technical Performance Comparison
The evolution from conventional PCR to qPCR and finally to dPCR has resulted in progressive improvements in key performance metrics, particularly for demanding applications like rare mutation detection.
Table 1: Comparative Analysis of PCR Technologies
| Parameter | Conventional PCR | Quantitative PCR (qPCR) | Digital PCR (dPCR) |
|---|---|---|---|
| Quantification Approach | Semi-quantitative (end-point) | Relative (requires standard curve) | Absolute (no standard curve) |
| Detection Method | Gel electrophoresis | Real-time fluorescence | End-point fluorescence |
| Sensitivity | Low | Moderate (can detect single copies) | High (detects rare mutations <0.1%) |
| Precision | Low | Moderate | High (CV < 10% common) |
| Tolerance to Inhibitors | Low | Moderate | High |
| Dynamic Range | Limited | 5-6 logs | 5 logs |
| Multiplexing Capability | Limited | Moderate | High (4-12 targets) |
Practical Workflow Comparison
The practical implementation of these technologies differs significantly in hands-on time, equipment requirements, and analytical workflows.
Table 2: Workflow Comparison Between dPCR and ddPCR
| Parameter | Chip-Based dPCR | Droplet Digital PCR (ddPCR) |
|---|---|---|
| Partitioning Mechanism | Fixed array/nanoplate | Emulsion droplets |
| Time to Results | < 90 minutes | 6-8 hours (multiple steps) |
| Multiplexing Capability | Available for 4-12 targets | Limited (newer models up to 12 targets) |
| Ease of Use | Integrated automated system | Multiple steps and instruments |
| Ideal Environment | QC and clinical settings | Research and development labs |
| Throughput | High | Moderate |
Experimental Protocols for Rare Mutation Detection
Sample Preparation and DNA Isolation
Effective rare mutation detection begins with optimal sample preparation. For liquid biopsy applications, blood samples should be collected in cell-stabilization tubes to prevent genomic DNA release from nucleated blood cells. Plasma separation via centrifugation (800-1600 × g for 10 minutes) should occur within 6 hours of collection, followed by a second centrifugation at 16,000 × g for 10 minutes to remove residual cells [12]. DNA extraction can be performed using commercially available kits optimized for cell-free DNA recovery, such as the MagMax Viral/Pathogen kit used with KingFisher Flex automated extraction systems [10]. DNA quantification should use fluorescence-based methods rather than UV spectrophotometry, as the latter lacks sensitivity for low-concentration cell-free DNA samples.
Assay Design Considerations
Effective dPCR assays for rare mutation detection require careful design to maximize specificity and sensitivity. Key considerations include:
- Amplicon Length: Shorter amplicons (60-100 bp) are preferred for fragmented DNA sources like formalin-fixed paraffin-embedded (FFPE) tissue or cell-free DNA
- Probe Design: Dual-labeled hydrolysis probes (TaqMan-style) should be designed with the variant nucleotide positioned centrally in the probe sequence to maximize discrimination
- Primer Placement: Primers should flank the target mutation with their 3' ends positioned to minimize mispriming to homologous sequences
- Validation: Assays should be validated using synthetic oligonucleotides or cell lines with known mutation status to establish limit of detection and limit of quantification
dPCR Setup and Optimization
For rare mutation detection, reaction setup must be optimized to maximize the number of partitions while maintaining amplification efficiency. A typical 20μL reaction mixture contains:
- 1× dPCR master mix
- 900 nM forward and reverse primers
- 250 nM wild-type and mutation-specific probes
- 5-50 ng DNA template
- Nuclease-free water to volume
Probe-based assays should utilize different fluorescent dyes (FAM, HEX/VIC, CY5) with non-overlapping emission spectra for wild-type and mutation-specific probes. Appropriate negative controls (no-template controls) and positive controls (synthetic oligonucleotides with known mutation status) must be included in each run.
Partitioning follows reaction setup, with methods varying by platform. For droplet-based systems, cartridges generate approximately 20,000 droplets per sample, while chip-based systems use pre-formed wells. Following partitioning, PCR amplification proceeds with standard thermal cycling conditions, though extension times may be optimized based on amplicon length.
Data Analysis and Interpretation
Post-amplification analysis involves several critical steps. First, fluorescence data from each partition is collected, typically using a two-dimensional plot of fluorescence amplitudes for each channel. Second, clusters corresponding to different populations (wild-type-only, mutation-only, double-positive, negative) are identified using appropriate gating strategies. For rare mutation detection, the threshold for mutant-positive partitions should be established using negative controls to determine background signals.
The concentration of mutant and wild-type targets is calculated using Poisson statistics applied to the fraction of positive partitions. The variant allele frequency (VAF) is then determined as:
[ \text{VAF} = \frac{[\text{Mutant}]}{[\text{Mutant}] + [\text{Wild-type}]} \times 100\% ]
The limit of detection for rare variants depends on the total number of partitions analyzed. With 20,000 partitions, typical sensitivity reaches 0.1% VAF, while higher partition numbers (100,000+) can achieve 0.01% sensitivity.
The Scientist's Toolkit: Essential Reagents and Platforms
Research Reagent Solutions
Successful dPCR experimentation requires specific reagents optimized for partitioning and amplification. The following table outlines essential components and their functions:
Table 3: Essential Research Reagents for dPCR
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| dPCR Master Mixes | ddPCR Supermix, QIAcuity PCR Master Mix | Provides DNA polymerase, dNTPs, buffer | Optimized for partition stability and efficient amplification |
| Fluorescent Probes | TaqMan probes, Double-stranded DNA binding dyes | Target-specific detection | FAM/HEX/CY5 dyes for multiplexing |
| Partitioning Reagents | Droplet Generation Oil, Nanoplate Reagents | Create stable partitions | Platform-specific formulations |
| DNA Extraction Kits | MagMax Viral/Pathogen Kit | Nucleic acid purification | Optimized for yield and inhibitor removal |
| Assay Design Tools | Custom TaqMan Assay Design Tool | Primer/probe design | Ensures specificity and efficiency |
Commercial dPCR Platforms
The dPCR landscape includes several commercial platforms implementing different partitioning and detection technologies:
- Bio-Rad ddPCR Systems: QX200, QX600, and QX700 systems utilizing droplet technology with 2-6 color detection capabilities [11]
- QIAGEN QIAcuity: Integrated nanoplate-based system with 4-5 plex capability and automated workflow [11]
- Thermo Fisher Absolute Q: Chip-based system with automated analysis and 4-color detection [11]
- RainDrop Systems: High-partition-count droplet systems generating millions of partitions per sample
Platform selection depends on application needs, with droplet-based systems typically offering higher partition counts and chip-based systems providing more streamlined, automated workflows better suited for clinical quality control environments [11].
Application in Rare Mutation Detection Research
Minimal Residual Disease Monitoring
dPCR has demonstrated superior performance for minimal residual disease (MRD) monitoring in hematological malignancies. A blinded prospective study comparing dPCR with qPCR in acute lymphoblastic leukemia (ALL) demonstrated that dPCR significantly outperformed qPCR, with a better quantitative limit of detection and sensitivity [13]. The number of critical MRD estimates below the quantitative limit was reduced by sixfold in retrospective cohorts and threefold in prospective cohorts when using dPCR compared to qPCR [13]. Furthermore, concordance between dPCR and flow cytometry (another absolute quantification method) was higher than between dPCR and qPCR, likely because both dPCR and flow cytometry provide absolute quantification independent of diagnostic samples [13].
Cancer Liquid Biopsy Applications
In liquid biopsy applications, dPCR enables non-invasive monitoring of tumor-associated mutations in cell-free DNA. The technology's high sensitivity allows detection of cancer-derived DNA fragments present at very low frequencies in blood samples. This capability has proven valuable for treatment response monitoring, resistance mutation detection, and cancer recurrence surveillance. dPCR's absolute quantification provides more reliable tracking of mutation levels over time compared to relative quantification methods, enabling more accurate assessment of disease progression or treatment response.
Analysis of DNA Methylation Patterns
dPCR has also been adapted for DNA methylation analysis, providing sensitive quantification of epigenetic markers. A comparison between ddPCR and qPCR for assessing T-cell proportions via CD3Z promoter methylation status demonstrated that ddPCR exhibited significantly better reproducibility (3.5% coefficient of variation) compared to qPCR (25% coefficient of variation) [14]. Both technologies correlated with flow cytometry measurements, but statistical measures of agreement showed linear concordance was stronger for ddPCR, with absolute values closer to flow cytometry results [14]. This enhanced precision makes dPCR particularly valuable for methylation-based biomarker applications.
Visualizing the Evolution: A Technical Workflow
Diagram 1: Technological Evolution from Conventional PCR to Digital PCR
The evolution from conventional PCR to digital PCR represents a paradigm shift in nucleic acid quantification, moving from qualitative detection to absolute single-molecule counting. For rare mutation detection research, this progression has been particularly significant, enabling applications previously limited by technical constraints. dPCR's ability to provide absolute quantification without standard curves, combined with exceptional sensitivity and precision, has established it as the technology of choice for challenging detection scenarios including minimal residual disease monitoring, liquid biopsy applications, and rare allele detection in heterogeneous samples.
Current trends suggest continued refinement of dPCR technologies, with emphasis on increasing partition density, enhancing multiplexing capabilities, and improving workflow automation. Integration of dPCR with microfluidic systems and development of novel detection chemistries promise to further expand applications in both research and clinical diagnostics. As these advancements continue, dPCR is poised to remain at the forefront of nucleic acid analysis, providing researchers with increasingly powerful tools to address complex biological questions and clinical challenges in rare mutation detection and beyond.
Rare mutations, defined as genetic variants present at very low frequencies within a cellular population or biological sample, hold profound clinical significance in oncology and genetic diseases. The ability to detect these mutations is critical for early cancer diagnosis, monitoring minimal residual disease (MRD), assessing tumor heterogeneity, and enabling personalized treatment strategies [3]. In non-cancerous genetic disorders, detecting rare mutations allows for prenatal diagnosis and carrier screening. The emergence of Droplet Digital PCR (ddPCR) represents a transformative advancement in this field, providing the sensitivity and precision required to identify and quantify these critical but elusive biomarkers [15]. This whitepaper details the clinical impact of rare mutations and the instrumental role of ddPCR in their detection within a research context focused on improving patient outcomes.
Digital PCR: A Paradigm Shift in Detection Technology
Digital PCR (dPCR) is a third-generation PCR technology that enables the absolute quantification of nucleic acid targets without the need for a standard curve. Its principle relies on partitioning a PCR reaction mixture into thousands to millions of nanoliter-scale reactions, so that each partition contains zero, one, or a few target molecules [3]. Following end-point PCR amplification, the fraction of positive partitions is counted, and the target concentration is calculated using Poisson statistics. This fundamental approach provides several powerful advantages over quantitative PCR (qPCR):
- Absolute Quantification: Eliminates the reliance on external standards, providing direct copy number concentration [3] [15].
- High Sensitivity and Precision: Capable of detecting single molecules, making it ideal for rare mutation detection [3].
- Superior Tolerance to Inhibitors: The partitioning of samples dilutes PCR inhibitors present in the reaction mix, enhancing robustness [3].
Droplet Digital PCR (ddPCR) is a widely adopted implementation of this technology that uses a water-in-oil emulsion to generate partitions. Recent innovations have focused on miniaturizing and automating ddPCR systems, making them suitable for rapid, on-site diagnostics without compromising the performance of bulky, conventional platforms [15].
Experimental ddPCR Protocol for Rare Mutation Detection
The following protocol, adapted from a study on detecting IDH1 mutations in gliomas, outlines a standard ddPCR workflow [15]:
1. Reaction Mixture Preparation:
- Combine
10 μLof 2x ddPCR Supermix for Probes. - Add
1 μLof ddPCR Mutation Detection Assay (20X) containing target-specific and wild-type-specific primers and probes. - Include
1 μLof restriction enzyme (e.g., HaeIII,10 U/μL) to digest genomic DNA and reduce viscosity for improved partitioning. - Add
50 ng/μLof template DNA (e.g., from patient-derived tissue). - Adjust the final volume to
20 μLwith nuclease-free water.
2. Droplet Generation:
- Transfer the
20 μLreaction mixture into an individual well of a droplet generation cartridge. - Add
70 μLof Droplet Generation Oil to the adjacent oil well. - Place the cartridge in a droplet generator. The device uses a flow-focusing method to create thousands of monodisperse, nanoliter-sized water-in-oil droplets, effectively partitioning the sample.
3. PCR Amplification:
- Transfer
40 μLof the generated droplets to a 96-well PCR plate. - Seal the plate with pierceable foil.
- Perform PCR amplification on a thermal cycler using optimized cycling conditions. A typical protocol includes:
- Enzyme activation at
95°Cfor10 minutes. 40 cyclesof:- Denaturation:
94°Cfor30 seconds. - Annealing/Extension:
55–60°Cfor60 seconds.
- Denaturation:
- Enzyme deactivation:
98°Cfor10 minutes. - Hold at
4°C.
- Enzyme activation at
4. Droplet Reading and Analysis:
- Load the PCR-amplified plate into a droplet reader.
- The reader aspirates droplets one-by-one, passing them through a fluorescence detector.
- Fluorescence signals (e.g., FAM for mutant targets, HEX/VIC for wild-type targets) are measured for each droplet.
- Data analysis software (e.g., Quantasoft) classifies droplets as positive or negative for each fluorescence channel and calculates the absolute concentration of the target (copies/μL) based on the fraction of positive droplets and Poisson statistics [15] [16].
Clinical Applications and Quantitative Impact
The application of ddPCR for rare mutation detection has yielded substantial clinical benefits across multiple domains, particularly in oncology. The following table summarizes key clinical applications and their documented impact.
Table 1: Clinical Applications and Performance of ddPCR in Rare Mutation Detection
| Clinical Application | Target | Clinical Significance | Reported Performance | Source/Model |
|---|---|---|---|---|
| Glioma Diagnosis & Prognosis | IDH1 R132H mutation | Differentiates IDH-mutant glioma (median survival: ~11.4 yrs) from IDH-wildtype glioblastoma (median survival: ~14.6 mos) [15]. | 92% Sensitivity, 100% Specificity [15] | Portable ddPCR System [15] |
| Liquid Biopsy & MRD | RAS oncogene mutations | Enables non-invasive detection of tumor DNA in blood; monitoring of treatment response and recurrence in colorectal cancer [3]. | Detected 2 mutant sequences in 160,000 wild-type sequences [3] | Early dPCR (Limiting Dilution) [3] |
| Infectious Disease | HIV provirus | Quantifies viral load by detecting single copies of HIV provirus in infected cells, correlating with disease stage [3]. | Detected 1 infected cell per 5000-80,000 PBMCs in asymptomatic patients [3] | Early dPCR (Limiting Dilution) [3] |
The Scientist's Toolkit: Essential Research Reagents
Successful ddPCR assays depend on a suite of specialized reagents and instruments. The table below details key components used in the featured IDH mutation detection study and their functions.
Table 2: Essential Research Reagents and Materials for ddPCR Mutation Detection
| Item | Function / Role in the Assay | Example from Protocol |
|---|---|---|
| ddPCR Supermix | Provides optimized buffer, dNTPs, DNA polymerase, and other reagents essential for PCR amplification in a droplet format. | Bio-Rad ddPCR Supermix for Probes [15] [16] |
| Mutation Detection Assay | Target-specific primers and fluorescently-labeled probes (e.g., TaqMan) that distinguish between wild-type and mutant sequences. | ddPCR Mutation Detection Assay for IDH1-R132H [15] |
| Restriction Enzyme | Digests long genomic DNA fragments to prevent entanglement and ensure efficient and random partitioning into droplets. | HaeIII restriction enzyme [15] |
| Droplet Generation Oil | Creates a stable water-in-oil emulsion, forming the individual partitions in which PCR reactions occur. | Bio-Rad Droplet Generation Oil [15] [16] |
| Template DNA | The sample containing the nucleic acid target of interest; quality and quantity are critical for accurate quantification. | 50 ng/μL of patient-derived glioma tissue DNA [15] |
Visualizing the ddPCR Workflow and Data Analysis
The following diagrams, created using the specified color palette and contrast-compliant design rules, illustrate the core workflow and data analysis logic of ddPCR.
Diagram 1: Core ddPCR Workflow. The process involves sample preparation, partitioning into droplets, PCR amplification, fluorescence reading, and data analysis.
Diagram 2: ddPCR Data Analysis Logic. Fluorescence data is used to classify droplets, and the count of positive and negative droplets is used for absolute quantification via Poisson statistics.
The detection of rare mutations is no longer a research curiosity but a clinical necessity for advancing personalized medicine. ddPCR technology, with its unparalleled sensitivity, precision, and robustness, provides a critical tool for researchers and clinicians to uncover these mutations in various contexts, from guiding cancer therapy to diagnosing genetic disorders. As the technology continues to evolve toward greater automation, miniaturization, and integration, its role in routine clinical diagnostics and drug development is poised to expand significantly, offering new hope for early intervention and improved patient outcomes.
Droplet Digital PCR (ddPCR) represents a transformative advancement in molecular diagnostics, offering unparalleled precision for detecting rare genetic mutations. This technical guide elucidates the core principles underpinning ddPCR's superior sensitivity, specificity, and reproducibility, framed within the context of oncology research and rare allele detection. By providing absolute quantification without standard curves, demonstrating resilience to PCR inhibitors, and enabling single-molecule detection, ddPCR establishes a new paradigm for biomarker discovery, liquid biopsy applications, and clinical diagnostics. We present experimental validation data, detailed methodologies, and analytical frameworks that confirm ddPCR's robust performance in detecting rare mutations, quantifying gene copy number variations, and identifying low-abundance pathogens, solidifying its critical role in advancing personalized medicine.
Digital PCR (dPCR), the third generation of PCR technology after conventional PCR and real-time quantitative PCR (qPCR), operates on a fundamentally different principle than its predecessors [3] [1]. By partitioning a PCR reaction mixture into thousands to millions of nanoliter-sized reactions, dPCR enables the absolute quantification of nucleic acid targets through Poisson statistical analysis of the binary positive/negative endpoint signals [3] [1]. This partitioning strategy allows dPCR to achieve single-molecule sensitivity, making it particularly powerful for applications requiring the detection of rare genetic events. Droplet Digital PCR (ddPCR) specifically utilizes a water-in-oil emulsion system to generate these partitions, typically creating thousands of droplets that function as individual microreactors [17] [3]. The technology's development, pioneered by Bert Vogelstein and colleagues who coined the term "digital PCR" in 1999, has evolved through significant microfabrication and microfluidics advances to become a robust, commercially available platform that provides calibration-free quantification with exceptional accuracy and reproducibility [3] [1].
The core workflow encompasses four critical steps: (1) partitioning the sample-PCR mixture into numerous discrete compartments; (2) endpoint PCR amplification within each partition; (3) fluorescence detection to classify partitions as positive or negative; and (4) absolute quantification of target concentration based on the fraction of positive partitions using Poisson statistics [3] [1]. This process eliminates the reliance on external standard curves and cycle threshold (Ct) values inherent to qPCR, thereby reducing quantification variability and enhancing measurement precision [17] [10]. For rare mutation detection—where identifying a few mutant alleles amidst a vast background of wild-type sequences is critical—ddPCR's partitioning approach provides a decisive advantage by effectively concentrating rare targets into detectable positive signals through massive sample fractionation [3].
Unmatched Sensitivity
The exceptional sensitivity of ddPCR stems directly from its ability to partition samples into thousands of individual reactions, effectively concentrating rare targets and enabling single-molecule detection. This section details the quantitative evidence and methodological approaches that establish ddPCR's superior sensitivity for rare mutation detection.
Single-Molecule Detection and Limits of Detection
ddPCR achieves remarkable sensitivity through statistical partitioning, allowing detection of rare mutations at frequencies as low as 0.001%–0.0001% in optimal conditions [3]. In practical applications, this sensitivity translates to reliable detection of minimal residual disease, circulating tumor DNA, and occult infections that remain undetectable by conventional methods. A comparative study of ddPCR platforms demonstrated a Limit of Detection (LOD) of approximately 0.17 copies/μL input for the QX200 system, equivalent to 3.31 copies per 20μL reaction [18]. The same study established a Limit of Quantification (LOQ) of 4.26 copies/μL input (85.2 copies/reaction), confirming ddPCR's ability to both detect and precisely quantify minimal target concentrations [18].
Table 1: Sensitivity Performance Metrics Across ddPCR Applications
| Application Domain | Detection Limit | Quantification Limit | Platform | Reference |
|---|---|---|---|---|
| Synthetic Oligonucleotides | 0.17 copies/μL | 4.26 copies/μL | QX200 ddPCR | [18] |
| Pathogen Detection (Plasma) | 0.5 copies/μL (most bacteria) | N/R | Auto-Pure System | [19] |
| Fungal Detection (Plasma) | 1.0 copies/μL (Candida) | N/R | Auto-Pure System | [19] |
Experimental Protocol for Sensitivity Validation
The validation of ddPCR sensitivity follows a standardized approach utilizing serial dilutions to establish detection boundaries. The protocol involves:
- Sample Preparation: Create a dilution series of the target nucleic acid, spanning from clinically relevant concentrations to near-zero concentrations [18].
- Partitioning: Utilize microfluidic chips to generate approximately 20,000 droplets per reaction, ensuring optimal Poisson distribution [17] [18].
- Thermal Cycling: Perform endpoint PCR with target-specific primers and probes under optimized cycling conditions (e.g., 50°C for 10 min, 95°C for 10 min, followed by 40 cycles of 95°C for 10s and 58°C for 45s) [17].
- Droplet Reading: Analyze droplets using a fluorescent detector to distinguish positive from negative partitions [17] [18].
- Statistical Analysis: Apply Poisson statistics to calculate target concentration, determining LOD and LOQ through regression analysis of the dilution series [18].
This methodological framework ensures that sensitivity claims are empirically validated and reproducible across laboratories, establishing ddPCR as the preferred technology for detecting rare mutations in complex biological samples.
Exceptional Specificity
ddPCR achieves exceptional specificity through a combination of optimized probe chemistry, thermal cycling conditions, and dual-signature verification within individual partitions. This multi-layered approach ensures accurate discrimination between closely related sequences, which is paramount for reliable rare mutation detection.
Probe-Based Discrimination and Experimental Validation
The specificity of ddPCR is fundamentally enhanced through TaqMan probe chemistry, which requires both primer annealing and probe hybridization for fluorescent signal generation [17]. This dual requirement significantly increases specificity compared to intercalating dye-based methods. In a bladder cancer study targeting FRS2 copy number variation, researchers designed specific primers (FRS2 forward: 5'-GCCTACAACTCCCCTTCCAC-3', reverse: 5'-TCATCTCGTGGCAGTGCTTT-3') and a FAM-labeled probe (5'-FAM-TTGACATAGCAGCAGTTCTCTCGA-BHQ-3') that clearly distinguished target sequences from homologous regions [17]. The assay demonstrated no interference between primers and probes when performing duplex detection of FRS2 and the reference gene RPP30 within the same reaction, confirming target specificity [17].
Validation against fluorescence in situ hybridization (FISH) demonstrated 100% sensitivity and 100% specificity for detecting FRS2 amplification, with a kappa value of 1 indicating perfect agreement between the methods [17]. This level of specificity is critical for clinical applications where false positives could lead to inappropriate treatment decisions. The binary nature of ddPCR readout—where partitions are unequivocally classified as positive or negative based on fluorescence amplitude—further enhances specificity by eliminating the subjective interpretation often associated with analog signals [17] [3].
Specificity Optimization Techniques
Several technical approaches can further enhance ddPCR specificity:
- Thermal Gradient Optimization: Empirical determination of optimal annealing temperatures for each primer-probe set significantly reduces non-specific amplification [17].
- Restriction Enzyme Digestion: Pre-digestion with enzymes such as HaeIII or EcoRI improves precision, especially for targets with high copy numbers or complex structures [18].
- Multi-Color Probe Design: Utilizing different fluorescent dyes (FAM, HEX/VIC, Cy5) for multiple targets enables specific detection within the same reaction while monitoring potential cross-reactivity [17] [18].
Table 2: Specificity Validation in Clinical Applications
| Application | Specificity Metric | Validation Method | Performance | Reference |
|---|---|---|---|---|
| FRS2 CNV in Bladder Cancer | Agreement with FISH | Fluorescence In Situ Hybridization | 100% Specificity | [17] |
| Pathogen Detection in Febrile Patients | Clinical Correlation | Conventional Microbiological Testing | 26.3% Specificity (vs. CMT) | [19] |
| Platform Comparison | Restriction Enzyme Impact | EcoRI vs. HaeIII Digestion | HaeIII Improved Specificity | [18] |
Superior Reproducibility
The reproducibility of ddPCR represents one of its most compelling advantages for research and clinical applications. By eliminating variations associated with standard curves and amplification efficiency, ddPCR delivers consistent, precise measurements across different instruments, laboratories, and timepoints.
Quantitative Precision Metrics
ddPCR demonstrates exceptional precision across technical and biological replicates, as evidenced by low coefficients of variation (CV%) in multiple studies. In the FRS2 copy number assay, researchers reported intra-assay CV% of 2.58% and 3.75%, and inter-assay CV% of 2.68% and 3.79% across 20 ng and 2 ng input DNA levels, respectively [17]. These remarkably low variation coefficients confirm the technology's robustness for serial monitoring applications, such as tracking treatment response through liquid biopsies.
A comprehensive platform comparison study further validated ddPCR's reproducibility, demonstrating that both droplet-based (QX200) and nanoplate-based (QIAcuity) systems achieved high precision across most analyses, with CVs ranging between 6% to 13% for ddPCR across various concentration levels [18]. The study noted that precision could be further optimized through restriction enzyme selection, with HaeIII demonstrating superior performance compared to EcoRI, particularly for the QX200 system where CVs improved to below 5% for all cell numbers tested [18].
Factors Enhancing Reproducibility
Several technological features contribute to ddPCR's superior reproducibility:
- Absolute Quantification Without Standard Curves: By counting discrete molecules rather than comparing to standard curves, ddPCR eliminates a major source of inter-laboratory variability [3] [1].
- Endpoint Detection: Measuring fluorescence after PCR completion avoids variations associated with amplification efficiency differences that affect Ct values in qPCR [10] [3].
- Partitioning Normalization: The massive sample partitioning minimizes the impact of PCR inhibitors, generating more consistent results across challenging sample matrices [10] [19].
- Poisson Statistical Foundation: The mathematical framework accounts for random distribution effects, providing statistically robust concentration calculations [3] [18].
The Scientist's Toolkit: Research Reagent Solutions
Implementing ddPCR for rare mutation detection requires specific reagents and optimized experimental components. The following table details essential materials and their functions based on validated protocols from recent research.
Table 3: Essential Research Reagents for ddPCR Rare Mutation Detection
| Reagent/Component | Function | Example Specification | Application Note |
|---|---|---|---|
| Target-Specific Primers | Amplification of target sequence | FRS2: 5'-GCCTACAACTCCCCTTCCAC-3' and 5'-TCATCTCGTGGCAGTGCTTT-3' [17] | HPLC purification recommended for long primers |
| Fluorescent Probes (TaqMan) | Sequence-specific detection | FRS2: 5'-FAM-TTGACATAGCAGCAGTTCTCTCGA-BHQ-3' [17] | FAM/HEX/Cy5 dyes for multiplexing; BHQ quenchers |
| Reference Gene Assay | Normalization control | RPP30: 5'-ROX-CTGACCTGAAGGCTCT-BHQ1-3' [17] | Different fluorescent channel than target |
| Restriction Enzymes | Enhance DNA accessibility | HaeIII or EcoRI [18] | HaeIII showed superior precision in comparative studies |
| Digital PCR Supermix | Partition stability & amplification | 2× Aplµs Digital PCR Mix [17] | Contains polymerase, dNTPs, optimized buffers |
| Microfluidic Chips | Partition generation | C4 chips (DropXpert S6 system) [17] | Generates ~20,000 droplets per reaction |
| Negative Controls | Contamination monitoring | DNase-free water [19] | Essential for establishing background signals |
| Synthetic DNA Standards | Assay validation | Custom oligonucleotides with target sequence [18] | Verify LOD, LOQ, and linearity |
Droplet Digital PCR establishes a new standard for sensitivity, specificity, and reproducibility in molecular detection, particularly for challenging applications like rare mutation detection in cancer research. The technology's unparalleled performance stems from its fundamental partitioning approach, which enables absolute quantification of nucleic acids without standard curves, reduces susceptibility to inhibitors, and provides statistically robust counting of individual molecules. As evidenced by the rigorous validation studies cited herein, ddPCR consistently demonstrates the ability to detect rare mutations with precision unattainable by conventional PCR methods. The detailed experimental protocols and reagent specifications provided in this technical guide offer researchers a framework for implementing ddPCR in their own laboratories, potentially accelerating discoveries in biomarker identification, liquid biopsy development, and personalized therapeutic monitoring. With ongoing advancements in microfluidics, multiplexing capabilities, and automated workflows, ddPCR is poised to remain at the forefront of molecular diagnostics, providing the precision necessary to decipher biological complexity and guide clinical decision-making.
From Theory to Practice: Implementing ddPCR in Liquid Biopsies and Disease Monitoring
Droplet Digital PCR (ddPCR) represents a third-generation polymerase chain reaction technology that enables absolute quantification of nucleic acids without the need for a standard curve [3] [20]. This revolutionary approach is based on the concept of sample partitioning and endpoint PCR analysis, fundamentally transforming capabilities for rare mutation detection in modern research laboratories [20]. The core technological advantage of ddPCR lies in its physical segregation of the sample into thousands of tiny, uniform water-in-oil emulsion droplets—typically 20,000 or more per reaction—with each droplet acting as an independent micro-reactor [20]. This partitioning process converts a continuous measurement of concentration into a digital readout, conferring the technology's characteristic robustness and sensitivity essential for detecting rare genetic mutations that constitute less than 0.1% of the total nucleic acid population [3] [20].
The complete ddPCR workflow encompasses three critical phases: sample preparation, partitioning, and end-point analysis [3]. Each phase must be meticulously optimized to ensure the high sensitivity, accuracy, and precision required for rare mutation detection in research and drug development applications [21]. The fundamental mechanism relies on Poisson statistics, where the random distribution of template molecules into partitions ensures that most droplets contain either zero or one copy of the target molecule, allowing for absolute quantification through binary endpoint detection [3] [20]. This technical guide provides an in-depth examination of each workflow component, with particular emphasis on methodological considerations for rare mutation detection research.
Sample Preparation: Optimizing Input Material
Conventional Nucleic Acid Extraction
Sample preparation constitutes the most variable phase of the ddPCR workflow and profoundly impacts assay performance, especially for rare target detection [21]. Conventional approaches utilize commercially available genomic DNA extraction kits that include purification steps through silica columns, magnetic beads, or ethanol precipitation [21]. These methods work effectively for cultured cells or samples with abundant cellular material (typically greater than 100,000 cells) but present significant challenges for clinical samples with limited cell numbers [21]. When working with limited samples containing fewer than 1,000 cells, target loss during extraction becomes a substantial concern that can compromise rare mutation detection sensitivity [21].
For circulating tumor DNA (ctDNA) analysis in liquid biopsy applications, specific considerations for cell-free DNA (cfDNA) extraction must be implemented. The recommended serum input volume for optimal sensitivity in viral load detection has been demonstrated at 200μL, which is lower than most conventional real-time PCR assays require [22]. This reduced input requirement is particularly advantageous when analyzing precious clinical samples or when additional blood collection from patients is challenging [22]. Extraction methods that maximize recovery of short-fragment cfDNA are essential for oncology applications where ctDNA may represent less than 0.01% of total cfDNA [20].
Innovative Approaches for Limited Samples
Recent methodological advances address the challenges of limited sample material. A novel crude lysate approach eliminates the DNA extraction and purification steps entirely, thereby preventing target loss during extraction [21]. This method is particularly valuable for quantifying rare targets from minimal cell samples, such as T stem cell memory cells that constitute only 2-4% of the total T cell population or antigen-specific T cells that may be present at frequencies of 1 per 100 to 100,000 cells [21].
The crude lysate protocol incorporates a critical viscosity breakdown (VB) step prior to droplet generation to address the challenge of intact oligonucleotides in cellular lysates increasing viscosity and impairing droplet formation [21]. Research demonstrates that samples processed without the VB protocol exhibited unexpected droplet spreading on the 2D plot, making threshold determination challenging, and showed significant differences in generated droplet numbers compared to VB-processed samples [21]. Importantly, the VB step eliminated systematic overestimation of target copies observed in non-VB protocols (0.046 TRECs/cell without VB versus 0.029 with standard ddPCR), establishing its essential role in ensuring measurement accuracy [21].
The performance of crude lysate methods depends heavily on lysis buffer composition. Comparative studies identified Buffer 2 (from SuperScript IV CellsDirect cDNA Synthesis Kit) as superior to Buffer 1 (from Ambion Cell-to-Ct kit), with Buffer 2 demonstrating excellent linearity (r² > 0.99) across a range of 200-16,000 cells and accurate quantification without systematic overestimation [21]. This optimized crude lysate protocol achieved a limit of detection of 0.0001 TRECs/cell, enabling reliable rare target detection from as few as 200 cells [21].
Sample Quality Assessment
Robust sample quality control is prerequisite for reliable ddPCR analysis, particularly in rare mutation detection where suboptimal sample quality can profoundly impact results. A ddPCR-based cell counting assay targeting the single-copy RPP30 gene has been developed to accurately quantify cell numbers, overcoming the high variability associated with traditional cell counting methods that depend on site, methodology, and operator expertise [23]. This approach demonstrates exceptional reproducibility across laboratories, with applications extending to normalization of tissue homogenates from various sources [23].
For monitoring DNA sample integrity during storage, ddPCR provides significant advantages over traditional methods like gel electrophoresis, UV absorbance, and qPCR [23]. The technology's absolute quantification capability without standard curves enables precise assessment of DNA degradation and quantification of losses due to tube binding, facilitating improved sample storage protocols [23].
Partitioning: Microfluidic Droplet Generation
Principles of Partitioning
Partitioning constitutes the defining step of the ddPCR workflow, where the PCR mixture is physically segregated into thousands to millions of discrete reaction compartments [3]. This partitioning process follows Poisson distribution statistics, where nucleic acid targets are randomly distributed among the partitions such that each compartment contains either 0, 1, or a few target molecules [3]. The statistical foundation of this approach was established in early work combining limiting dilution PCR with Poisson statistics to isolate, detect, and quantify single nucleic acid molecules [3].
Two major partitioning methodologies have emerged: water-in-oil droplet emulsification (ddPCR) and microchamber-based systems [3]. Droplet-based systems offer greater scalability and cost-effectiveness, while microchamber platforms provide higher reproducibility and ease of automation but are limited by fixed partition numbers and typically higher costs [3]. The number of partitions directly impacts quantification accuracy, with higher partition counts enabling more precise rare allele detection by ensuring adequate representation of low-frequency targets within the statistical sample [20].
Microfluidic Technology
Microfluidic technology is central to creating the uniform, stable droplets that define the ddPCR process [3] [20]. Monodisperse droplets are typically generated at high speed (1-100 kHz) using microfluidic chips that leverage passive forces or actively break the aqueous/oil interface [3]. Modern commercial systems like the QX ONE Droplet Digital PCR System have automated this process, integrating droplet generation, PCR amplification, and droplet reading into a single platform capable of analyzing 480 samples daily [23] [24].
Droplet stability represents a critical technical consideration throughout the workflow. Water-in-oil droplets are prone to coalescence, particularly during the rigorous temperature variations of PCR thermocycling [3]. Appropriate surfactant formulations are essential for maintaining droplet integrity, with specialized Droplet Generation Oil formulations containing proprietary surfactants that prevent droplet merging while ensuring compatibility with biochemical reactions [22]. Empirical validation of droplet volume is recommended, as studies have demonstrated actual droplet volumes (0.70nL) may differ from manufacturer specifications (0.85nL), necessitating adjustment of concentration calculations to maintain accurate quantification [21].
Digital PCR Partitioning Workflow
End-point Analysis: Detection and Quantification
Fluorescence Detection Technologies
Following endpoint PCR amplification, droplets undergo individual fluorescence analysis to determine target presence or absence [3] [20]. Two primary readout methodologies exist: in-line detection and planar imaging [3]. In-line detection, commonly employed in ddPCR systems, involves flowing droplets sequentially through a microfluidic channel or capillary where fluorescence is measured using a light source coupled to detectors [3]. This approach enables analysis of large droplet numbers but requires precise flow control [3]. Planar imaging captures static snapshots of microchamber arrays or deposited microdroplets using fluorescence microscopy or scanners [3]. Advanced 3D imaging and analysis techniques have been developed to assay larger droplet numbers in reduced timeframes [3] [25].
Modern ddPCR platforms feature multi-channel fluorescence detection capabilities essential for multiplex applications. While earlier systems like the QX200 were limited to two-color fluorescence, restricting multiplex detection complexity, newer platforms including the QX ONE incorporate four independent fluorescence channels, enabling simultaneous detection of multiple targets in a single reaction [24]. This advancement facilitates development of sophisticated multiplex assays, such as the automated high-throughput quadruplex RT-ddPCR assay (AHQR-ddPCR) that simultaneously detects influenza A, influenza B, respiratory syncytial virus, and SARS-CoV-2 [24].
Data Analysis and Poisson Statistics
The fundamental principle of ddPCR quantification relies on Poisson statistics applied to the binary readout of positive versus negative partitions [3] [20]. The fraction of positive partitions enables computation of the target concentration based on Poisson distribution parameters, providing absolute quantification without external calibration [3]. This statistical approach accounts for the random distribution of targets among partitions, including the probability that some partitions received multiple copies, thereby enabling accurate back-calculation of the true starting concentration [20].
The Poisson model is expressed mathematically as:
[C = -\frac{\ln(1 - p)}{V}]
Where (C) represents the target concentration (copies/μL), (p) is the proportion of positive partitions, and (V) is the partition volume [20]. This calculation is automatically performed by instrument software such as Bio-Rad's QuantaSoft, which applies automatic thresholding based on fluorescence amplitude to classify partitions as positive or negative [22]. For rare mutation detection, the high degree of partitioning (20,000+ droplets) ensures that even minimal target concentrations are reliably detected and quantified, enabling discrimination of mutant allele frequencies below 0.1% [20].
Advanced Analysis and Artificial Intelligence
Emerging analytical approaches incorporate artificial intelligence to enhance ddPCR data interpretation. AI-driven fluorescence image analysis represents a significant advancement, with evolution from classical classifiers to modern deep learning and foundation models (e.g., SAM, ViT, GPT-4o) improving analytical precision [25]. These computational methods address challenges in partition diversity, signal interpretation, and workflow integration, particularly for point-of-care testing applications [25]. Structured frameworks redefining dNAAT into five stages (Sample Preparation, Partition, Amplification, Detection, and Analysis) highlight opportunities for AI-enhanced precision, scalability, and automation at each workflow step [25].
Quantitative Performance Metrics
The exceptional analytical performance of ddPCR is demonstrated through rigorous validation studies across diverse applications. The tables below summarize key performance metrics established through recent research.
Table 1: Analytical Sensitivity of ddPCR Assays Across Applications
| Application | Target | Limit of Detection (LOD) | Lower Limit of Quantification (LLOQ) | Sample Input | Citation |
|---|---|---|---|---|---|
| Hepatitis B Viral Load | HBV X gene | 1.6 IU/mL | 9.4 IU/mL | 200 μL serum | [22] |
| Respiratory Virus Detection | Influenza A | 0.65 copies/μL | N/R | 5 μL RNA | [24] |
| Respiratory Virus Detection | Influenza B | 0.78 copies/μL | N/R | 5 μL RNA | [24] |
| Rare DNA Circles | TRECs | 0.0001 copies/cell | N/R | 200 cells | [21] |
Table 2: Precision and Reproducibility Metrics
| Application | Intra-run Variability (CV) | Inter-run Variability (CV) | Linearity (R²) | Specificity | Citation |
|---|---|---|---|---|---|
| Hepatitis B Viral Load | 0.69% | 4.54% | 0.988 | 96.2% | [22] |
| Copy Number Variation | N/R | N/R | N/R | 95% concordance with PFGE | [26] |
| Rare Target Detection | High reproducibility across laboratories | N/R | >0.99 (Buffer 2) | No false positives with VB protocol | [21] [23] |
Research Reagent Solutions
Table 3: Essential Reagents and Kits for ddPCR Workflow
| Reagent/Kits | Function | Application Notes | Citation |
|---|---|---|---|
| QX ONE ddPCR System | Integrated partitioning, thermocycling, reading | Automated high-throughput (480 samples/day); 4-color detection | [23] [24] |
| One-Step RT–ddPCR Advanced Kit for Probes | Reverse transcription and PCR amplification | Enables direct RNA detection; includes reverse transcriptase and supermix | [24] |
| Droplet Generation Oil | Forms stable water-in-oil emulsion | Critical for droplet integrity; contains proprietary surfactants | [22] |
| Cell Lysis Buffer (Buffer 2) | Cellular lysis without DNA purification | Superior performance for crude lysate preparations from limited samples | [21] |
| QIAamp MinElute Virus Spin Kit | Nucleic acid extraction | Optimized for viral DNA/RNA from serum/plasma; elution volume 16μL | [22] |
| RPP30 Assay | Reference gene for cell counting | Absolute quantification of cell numbers; normalizes sample input | [23] |
The integrated workflow of sample preparation, partitioning, and end-point analysis in ddPCR provides researchers with an exceptionally powerful tool for rare mutation detection. The technology's absolute quantification capability, independence from standard curves, and exceptional sensitivity enable applications previously challenging with conventional PCR methods [20]. Ongoing advancements in sample preparation methodologies, particularly for limited samples, microfluidic partitioning technologies, and AI-enhanced data analysis continue to expand the frontiers of molecular detection [21] [25]. For research and drug development professionals focused on high-stakes applications such as liquid biopsy, viral load monitoring, and genetic variation studies, mastery of the complete ddPCR workflow is essential for generating reliable, reproducible, and clinically actionable data [27] [20]. As the technology continues to evolve with improved automation, multiplexing capabilities, and analytical sophistication, its role in precision medicine and molecular diagnostics is poised for significant expansion [25] [27].
Liquid biopsy represents a transformative approach in oncology, shifting the paradigm from traditional tissue biopsy to minimally invasive detection of tumor-derived components in body fluids. Among these components, circulating tumor DNA (ctDNA) has emerged as a predominant biomarker due to its ability to provide a real-time snapshot of tumor genomics [28] [29]. ctDNA consists of short fragments of DNA released into the bloodstream primarily through apoptosis and necrosis of tumor cells, carrying tumor-specific genetic and epigenetic alterations [30] [31]. Unlike conventional tissue biopsy, which captures a single spatial and temporal point, ctDNA analysis reflects tumor heterogeneity and evolving genomic landscapes, enabling dynamic monitoring throughout the disease course [29] [31].
The clinical significance of ctDNA stems from its correlation with tumor burden and cellular turnover [31]. In patients with advanced cancer, ctDNA can constitute upwards of 90% of total cell-free DNA (cfDNA), though this percentage drops significantly in early-stage disease, often falling below 1% [31]. The half-life of ctDNA is remarkably short, estimated between 15 minutes to several hours, allowing for near real-time assessment of treatment response and disease progression [30] [31]. These characteristics make ctDNA an exceptionally dynamic biomarker for precision oncology applications, including treatment selection, response monitoring, minimal residual disease (MRD) detection, and identification of resistance mechanisms [32] [31].
Biological Foundations and Technical Challenges
Origin and Characteristics of ctDNA
ctDNA originates from tumor cells through various mechanisms, with apoptosis and necrosis being the primary sources [30]. Apoptosis produces uniformly short DNA fragments (approximately 160-180 base pairs), while necrosis generates more variable fragment sizes [29]. Additional release mechanisms include phagocytosis, active secretion, and neutrophil extracellular traps [30]. A key distinguishing feature of tumor-derived DNA is its fragmentation pattern; ctDNA fragments are typically shorter than non-tumor cfDNA, with enrichment of fragments between 90-150 base pairs [29] [30]. This fragmentation signature, along with end-motif patterns, provides additional discriminative power for detecting tumor-derived DNA amidst the background of normal cfDNA [28] [31].
The concentration of ctDNA in circulation varies significantly based on cancer type, stage, and tumor location [30]. While ctDNA levels generally correlate with tumor burden, this relationship is not absolute, as some tumors exhibit higher shedding rates than others independent of size [30] [31]. Additionally, ctDNA is not uniformly distributed throughout the bloodstream, presenting analytical challenges for reliable detection, particularly in early-stage disease where tumor DNA represents only a minute fraction of total cfDNA [33] [31].
Technical Hurdles in ctDNA Analysis
The detection and analysis of ctDNA face several significant technical challenges that must be addressed for successful implementation:
Low Abundance: In early-stage cancers, ctDNA can represent as little as 0.01% of total cfDNA, requiring exceptionally sensitive detection methods [34]. This low variant allele frequency (VAF) demands techniques capable of distinguishing true mutations from background noise and technical artifacts [33] [31].
Pre-analytical Variables: Sample collection, processing, and storage conditions significantly impact ctDNA integrity and yield [28]. Variables including blood collection tube type, time-to-processing, centrifugation protocols, and storage temperature can introduce biases that affect downstream analysis [35]. Standardization of these pre-analytical steps is crucial for reproducible results [28].
Tumor Heterogeneity: The genetic diversity within and between tumor sites presents challenges for designing assays that comprehensively capture the molecular landscape [34]. While ctDNA theoretically represents the entire tumor ecosystem, in practice, low-frequency subclones may evade detection if assay sensitivity is insufficient [31].
Clonal Hematopoiesis: Age-related mutations in blood cells can contribute cfDNA variants that mimic tumor-derived mutations, potentially leading to false positive results [33]. Distinguishing somatic tumor mutations from clonal hematopoiesis of indeterminate potential (CHIP) requires careful bioinformatic filtering or matched analysis of white blood cells [33].
Table 1: Key Technical Challenges in ctDNA Analysis and Potential Mitigation Strategies
| Challenge | Impact on Analysis | Mitigation Strategies |
|---|---|---|
| Low Abundance | Limits detection sensitivity in early-stage cancer | Unique molecular identifiers (UMIs), error-suppressed sequencing, deep sequencing |
| Pre-analytical Variability | Introduces bias and affects reproducibility | Standardized collection protocols, plasma separation within 4h, use of stabilizing tubes |
| Tumor Heterogeneity | Incomplete representation of molecular landscape | Large gene panels, whole-genome approaches, multi-analyte integration |
| Clonal Hematopoiesis | False positive variant calls | Matched white blood cell sequencing, bioinformatic filtering, epigenetic profiling |
Detection Methodologies and Platforms
PCR-Based Approaches
Polymerase chain reaction (PCR) methods form the foundation of ctDNA detection, offering rapid turnaround times and high sensitivity for known mutations [28] [31]. Digital droplet PCR (ddPCR) and BEAMing (beads, emulsion, amplification, and magnetics) technologies enable absolute quantification of mutant alleles by partitioning reactions into thousands of individual droplets, allowing for detection of rare variants with variant allele frequencies as low as 0.001% in some optimized assays [28]. These methods are particularly valuable for monitoring specific driver mutations in genes such as BRAF (melanoma), KRAS (lung and colorectal cancer), ESR1 (breast cancer), and AR (prostate cancer) [31]. The primary limitation of PCR-based approaches is their restriction to a small number of predefined mutations, making them less suitable for discovery applications or heterogeneous tumors with diverse mutation profiles [31].
Next-Generation Sequencing Strategies
Next-generation sequencing (NGS) has dramatically expanded the scope of ctDNA analysis, enabling comprehensive profiling of multiple genomic alterations simultaneously [30] [31]. NGS approaches for ctDNA can be broadly categorized into targeted and untargeted methods:
Targeted NGS focuses on specific genes or regions of interest, achieving high sensitivity through deep sequencing (often >10,000x coverage) [30] [33]. Common targeted approaches include TAm-Seq (tagged-amplicon deep sequencing), CAPP-Seq (cancer personalized profiling by deep sequencing), and Safe-SeqS (safe-sequencing system) [30] [31]. These methods typically employ unique molecular identifiers (UMIs) to distinguish true mutations from PCR and sequencing errors, with some advanced error-correction methods like Duplex Sequencing and CODEC (concatenating original duplex for error correction) achieving up to 1000-fold higher accuracy than conventional NGS [31].
Untargeted NGS includes whole-genome sequencing (WGS) and whole-exome sequencing (WES), which provide a hypothesis-free approach for discovering novel alterations but at lower sensitivity due to reduced sequencing depth [30]. These methods are particularly valuable for identifying copy number alterations, chromosomal rearrangements, and unexpected mutational signatures [31].
Table 2: Comparison of Major ctDNA Detection Platforms
| Technology | Detection Limit | Advantages | Limitations | Best Use Cases |
|---|---|---|---|---|
| ddPCR/BEAMing | 0.01%-0.1% | High sensitivity, quantitative, fast turnaround | Limited multiplexing, predefined targets | Therapy monitoring, MRD tracking |
| Targeted NGS | 0.1%-0.5% | Multiplexing capability, patient-specific panels | Longer turnaround, higher cost | Comprehensive profiling, heterogeneous tumors |
| Whole-Genome NGS | 1%-5% | Genome-wide coverage, discovery potential | Lower sensitivity, higher cost & bioinformatics burden | Novel biomarker discovery, structural variant detection |
| Methylation Analysis | Varies by assay | Tissue-of-origin identification, early detection | Complex analysis, requires reference databases | Cancer screening, recurrence monitoring |
Emerging Approaches: Fragmentomics and Methylation Analysis
Beyond mutation detection, novel approaches are expanding the analytical capabilities of liquid biopsy. Fragmentomics analyzes the size distribution and fragmentation patterns of cfDNA to distinguish tumor-derived fragments without relying on specific mutations [28]. The DELFI (DNA evaluation of fragments for early interception) method uses machine learning to identify cancer-associated fragmentation profiles across the genome, demonstrating 91% sensitivity for cancer detection in one study [28].
Methylation analysis detects cancer-specific epigenetic patterns that often occur early in tumorigenesis [28] [35]. Both bisulfite conversion-based methods (e.g., whole-genome bisulfite sequencing) and bisulfite-free approaches (e.g., MeDIP-Seq) can identify hypermethylated or hypomethylated regions characteristic of malignancy [28]. In a 2025 comparative study, MeD-Seq (a genome-wide methylation profiling assay) detected ctDNA in 57.5% of early breast cancer patients, outperforming mutation-based approaches [35]. Multimodal integration of genomic, fragmentomic, and epigenetic analyses further enhances detection sensitivity, with one study reporting a 25-36% increase in recurrence detection when combining epigenomic signatures with genomic alterations [28].
Experimental Workflows and Protocols
Sample Collection and Processing
Robust pre-analytical protocols are essential for reliable ctDNA analysis. The following workflow represents current best practices for blood-based ctDNA collection and processing:
Blood Collection: Draw blood into cell-stabilizing tubes (e.g., Streck, CellSave, or EDTA) [35]. The choice of collection tube impacts processing timelines, with EDTA tubes requiring processing within 4 hours and specialized cell-stabilizing tubes allowing for extended storage up to 96 hours [35].
Plasma Separation: Perform two-step centrifugation - first at 1711×g for 10 minutes at room temperature to separate cellular components, followed by a second centrifugation at 12,000×g for 10 minutes at 4°C to remove remaining cellular debris [35]. Aliquot plasma carefully to avoid disturbing the buffy coat or pellet.
cfDNA Extraction: Use commercially available kits (e.g., QiaAmp cfDNA Kit) to isolate cfDNA from plasma according to manufacturer's instructions [35]. Extraction efficiency varies significantly between methods, with one comparative study reporting efficiencies ranging from 16% to near-complete recovery across different platforms [33].
Quality Control and Quantification: Quantify cfDNA using fluorescence-based methods (e.g., Quant-iT dsDNA HS Assay) rather than UV spectrophotometry to ensure accurate measurement of low-concentration samples [35]. Assess DNA integrity through fragment analysis if fragmentomic applications are planned.
Library Preparation and Sequencing
Library preparation methods vary significantly based on the intended analysis, with key considerations including input DNA quantity, target region size, and required sensitivity:
Targeted Amplification Approaches: For PCR-based NGS methods like TAm-Seq, library preparation begins with an initial multiplex PCR amplification using primers designed for regions of interest, followed by a second amplification to attach platform-specific adapters and sample barcodes [30]. Unique molecular identifiers (UMIs) are incorporated during this step to enable error correction and accurate quantification [30] [31]. Even a 2% reduction in variant calling error rate can improve sensitivity by 15% for low-frequency variants, making UMI implementation critical for ctDNA applications [31].
Hybrid Capture-Based Approaches: For larger target regions or whole-genome analysis, hybrid capture methods are preferred. Following library preparation with adapter ligation, biotinylated probes complementary to the target regions are used to enrich sequences of interest [30]. This approach requires more input DNA but provides more uniform coverage and better performance for detecting structural variants and copy number alterations [31].
Sequencing Configuration: The appropriate sequencing depth depends on the application and expected variant allele frequency. For MRD detection where VAF may be <0.1%, ultra-deep sequencing (>30,000x) is often necessary, while for monitoring known mutations in advanced disease, moderate depth (5,000-10,000x) may suffice [33]. A 2024 analytical evaluation found that sequencing depth varied widely across commercial ctDNA assays, with some achieving >10,000x deduplicated mean depth while others operated at <5,000x, significantly impacting sensitivity particularly at lower VAFs [33].
Analytical Validation and Quality Metrics
Rigorous validation is essential for implementing ctDNA testing in research and clinical contexts. Key performance metrics include:
Limit of Detection (LOD): Determine the lowest VAF that can be reliably detected with 95% confidence. LOD varies by variant type, with SNVs typically having lower detection limits than indels or structural variants [33].
Sensitivity and Specificity: Calculate based on known positive and negative reference materials. In a 2024 multi-assay evaluation, sensitivity for SNV detection at 0.5% VAF ranged from approximately 0.8 to >0.95 across different platforms, with specificity generally exceeding 99% for most assays [33].
Reproducibility: Assess intra-run, inter-run, and inter-operator variability using replicate samples. The same evaluation found substantial variability in reproducibility across platforms, particularly at lower DNA inputs (<20 ng) [33].
Essential Research Reagent Solutions
Successful ctDNA analysis requires carefully selected reagents and materials at each stage of the workflow. The following table details key research reagent solutions and their functions in ctDNA studies:
Table 3: Essential Research Reagent Solutions for ctDNA Analysis
| Reagent Category | Specific Examples | Function | Technical Considerations |
|---|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, EDTA tubes, CellSave | Cellular stabilization, prevention of lysis | Processing time varies (4h for EDTA, 96h for specialized tubes) [35] |
| Nucleic Acid Extraction Kits | QiaAmp cfDNA Kit, MagMAX Cell-Free DNA Isolation Kit | Isolation of high-quality cfDNA from plasma | Extraction efficiency varies (16% to near-complete recovery across platforms) [35] [33] |
| Library Preparation Kits | AVENIO ctDNA kits, Oncomine Breast cfDNA assay, custom UMI kits | Preparation of NGS libraries with minimal bias | UMI incorporation reduces errors by 70-fold in Safe-SeqS [30] [31] |
| Target Enrichment Systems | IDT xGen Lockdown Probes, Twist Human Core Exome | Hybrid capture-based target enrichment | Critical for large panels; improves uniformity [30] |
| Quantification Assays | Quant-iT dsDNA HS Assay, Qubit fluorometer | Accurate measurement of low-concentration DNA | Fluorescence-based methods preferred over spectrophotometry [35] |
| Sequencing Controls | Seraseq ctDNA Reference Materials, Horizon Multiplex I cfDNA | Process monitoring, quality control, assay validation | Essential for determining LOD and reproducibility [33] |
Current Applications and Clinical Validation
Minimal Residual Disease and Recurrence Monitoring
The detection of minimal residual disease (MRD) represents one of the most promising applications of ctDNA analysis [32] [31]. Following curative-intent treatment, the presence of ctDNA indicates residual tumor cells that may lead to recurrence, often months before clinical or radiological evidence [32]. In the GALAXY arm of the CIRCULATE-Japan trial involving over 2000 patients with resectable stage II-IV colorectal cancer, recurrence occurred in 78% of MRD-positive patients compared to only 13% of those with negative ctDNA results [32]. At 36-month follow-up, disease-free survival was only 16% in ctDNA-positive patients versus 83% in the ctDNA-negative cohort, establishing ctDNA positivity as the single most significant prognostic factor for recurrence [32].
Similar findings have been reported across multiple cancer types. The DARE clinical trial presented at ASCO 2025 confirmed that ctDNA dynamics following surgery are strongly prognostic for patient outcomes [36]. Additionally, the PREDICT-DNA trial demonstrated that ctDNA assessment after neoadjuvant therapy may be more prognostic than pathological response at surgery [36]. These findings highlight the potential for ctDNA to guide adjuvant therapy decisions, though the DYNAMIC-III trial in stage III colon cancer showed that treatment escalation based solely on ctDNA positivity did not improve recurrence-free survival, suggesting that both assay refinement and more effective escalation therapies are needed [36].
Treatment Response Monitoring and Therapy Selection
ctDNA analysis enables real-time assessment of treatment response through serial monitoring of mutation levels [31]. The short half-life of ctDNA (approximately 15 minutes to several hours) allows for rapid evaluation of therapeutic efficacy, often within days or weeks of treatment initiation [30] [31]. In advanced disease, ctDNA monitoring can identify emerging resistance mechanisms, such as ESR1 mutations in hormone receptor-positive breast cancer during aromatase inhibitor therapy [36] [31].
The SERENA-6 clinical trial, a landmark study presented at ASCO 2025, demonstrated the clinical utility of ctDNA-guided treatment switching [36]. Patients with advanced HR-positive HER2-negative breast cancer receiving CDK4/6 inhibitors and aromatase inhibition were monitored for emerging ESR1 mutations via ctDNA. Those with detected mutations without radiological progression were randomized to switch to camizestrant (an oral SERD) or continue aromatase inhibition. The study showed significantly improved progression-free survival and quality of life in the switched group, establishing ctDNA monitoring as a strategy for anticipating resistance and modifying treatment before clinical progression [36].
Emerging Applications and Future Directions
While current clinical applications focus primarily on treatment monitoring and MRD detection in established cancers, emerging research is exploring additional applications:
Early Cancer Detection: Multicancer early detection tests using methylation patterns or fragmentomic profiles represent an exciting frontier [28] [36]. Current limitations include reduced sensitivity for early-stage cancers and potential overdiagnosis [36]. At ASCO 2025, researchers reported that pap-derived cell-free tumor DNA was more effective than plasma ctDNA for detecting endometrial cancer, suggesting alternative biofluids may enhance early detection for specific cancer types [36].
Novel Biofluid Sources: Beyond blood, ctDNA can be detected in urine, saliva, cerebrospinal fluid, and other bodily secretions, potentially improving detection for specific malignancies [28] [29]. Urine ctDNA shows particular promise for genitourinary cancers, while CSF analysis provides valuable information for central nervous system malignancies [28].
Multimodal Integration: Combining ctDNA with other liquid biopsy analytes, such as circulating tumor cells, extracellular vesicles, and protein biomarkers, may provide a more comprehensive disease picture [29] [31]. Integrated approaches could potentially overcome limitations of individual analytes and improve overall sensitivity and specificity.
As ctDNA analysis continues to evolve, standardization of pre-analytical procedures, analytical validation, and reporting standards will be crucial for broader clinical adoption [28] [33]. Ongoing prospective clinical trials will further define the appropriate contexts for ctDNA testing and establish evidence-based guidelines for implementation across different cancer types and clinical scenarios.
Quantifying Therapy Response and Monitoring Residual Disease
Minimal (or Measurable) Residual Disease (MRD) refers to the small number of cancer cells that persist in a patient after treatment, often at levels undetectable by conventional microscopy. Droplet Digital PCR (ddPCR) has emerged as a powerful third-generation PCR technology for MRD monitoring, enabling the absolute quantification of rare genetic mutations and fusion transcripts with ultra-high sensitivity [3]. This guide details the application of ddPCR for quantifying therapy response and monitoring residual disease in haematological malignancies, providing a technical framework for researchers and drug development professionals. By offering a highly sensitive and precise method for tracking specific molecular targets, ddPCR allows for the digitalization of serial MRD monitoring, which is critical for guiding treatment decisions and improving patient outcomes [37].
Technical Advantages of ddPCR in MRD Monitoring
Droplet Digital PCR revolutionizes nucleic acid quantification by partitioning a sample into thousands of nanoliter-sized water-in-oil droplets, effectively creating a massive array of individual PCR reactions. Following end-point amplification, the droplets are analyzed one-by-one in a flow cytometer to count the positive and negative reactions, allowing for absolute quantification of the target molecule without the need for a standard curve, based on Poisson statistics [37] [3]. This core principle underpins several key advantages for MRD monitoring.
- Absolute Quantification without Standard Curves: Unlike quantitative real-time PCR (qPCR), ddPCR does not rely on external standard curves for quantification, which improves accuracy and reproducibility, especially at very low target concentrations crucial for assessing deep molecular response [37] [13].
- Ultra-High Sensitivity and Precision: ddPCR demonstrates a significantly superior limit of detection compared to qPCR, reliably detecting variant allele frequencies (VAF) as low as 0.001% (1 mutant in 100,000 wild-type genomes) [38]. This reduces the number of non-quantifiable MRD measurements and provides more precise data in the critical low-positive range [13].
- Resistance to PCR Inhibitors: The partitioning step in ddPCR dilutes potential PCR inhibitors across many droplets, making the assay less susceptible to their effects compared to qPCR, thereby enhancing robustness, particularly when using complex sample matrices [37].
- Ideal for Rare Target Detection: The ability to effectively enrich low-abundance targets makes ddPCR exceptionally suited for detecting rare mutant alleles in a vast background of wild-type DNA, a fundamental requirement for effective MRD monitoring and liquid biopsy analysis [39].
Table 1: Comparison of MRD Monitoring Technologies
| Feature | ddPCR | qPCR | Multiparameter Flow Cytometry (MFC) | Next-Generation Sequencing (NGS) |
|---|---|---|---|---|
| Quantification Method | Absolute | Relative | Absolute | Relative (Variant Allele Frequency) |
| Sensitivity | 0.001% [38] | 0.01% | 0.01% [38] | Variable (0.1% - 1%) [37] |
| Throughput | Medium | High | High | Low to High |
| Requires Standard Curve? | No | Yes | No | Yes (for some applications) |
| Key Advantage | Superior sensitivity & precision for known targets | Established, gold standard for some markers | Broad applicability, no molecular target needed | Ability to discover novel mutations |
Clinical Application: MRD Monitoring in Haematological Malignancies
The clinical utility of ddPCR for MRD monitoring is well-established in acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), and chronic myeloid leukemia (CML). In AML and ALL, the presence of MRD at any point during treatment is a strong negative prognostic indicator for relapse and worse overall survival [37]. In CML, achieving a sustained deep molecular response with tyrosine kinase inhibitor therapy is a key treatment goal and a prerequisite for considering therapy discontinuation [37].
A key application is monitoring specific genetic aberrations. ddPCR assays have been successfully developed and validated for a range of rare fusion transcripts and mutations, including:
- Atypical BCR::ABL1 fusion transcripts (e.g., e19a2, e23a2ins52) [37]
- CBFB::MYH11 fusion types (G and I) [37]
- PCM1::JAK2 and KMT2A::ELL fusions [37]
- CEBPA frame-shift and insertion/duplication mutations [37]
A multicenter retrospective study on AML/MDS patients after allogeneic hematopoietic stem cell transplantation (allo-HSCT) demonstrated the robust prognostic power of ddPCR-MRD monitoring. The study, which included 152 patients, found that ddPCR-MRD positivity for non-DTA mutations (excluding age-related clonal hematopoiesis genes DNMT3A, TET2, and ASXL1) within four months post-transplant was an independent adverse predictor for relapse, relapse-free survival, and overall survival [38]. Furthermore, combining ddPCR with MFC provided an even more accurate prediction of relapse risk, highlighting the power of a multi-modal MRD assessment strategy [38].
Table 2: Selected ddPCR MRD Markers and Clinical Performance in Haematological Malignancies
| Disease Context | Molecular Target | Reported Sensitivity | Clinical/Prognostic Utility |
|---|---|---|---|
| AML/MDS (post-HSCT) | Non-DTA mutations (e.g., in NPM1, IDH1/2, RUNX1) | VAF ≥ 0.001% [38] | Independent predictor of higher relapse incidence and worse survival [38] |
| CML | Atypical BCR::ABL1 transcripts (e.g., e19a2) | High (precise LOD not stated) | Monitoring deep molecular response for TKI discontinuation consideration [37] |
| ALL | Immunoglobulin/T-cell receptor gene rearrangements | Better than qPCR; reduces BQL samples [13] | Better quantitative LOD and sensitivity than qPCR; high concordance with MFC [13] |
| AML | CBFB::MYH11 Type G and I fusions | High (precise LOD not stated) | Serial monitoring for early relapse detection [37] |
Figure 1: The core workflow for MRD monitoring using droplet digital PCR (ddPCR), from patient diagnosis to clinical decision-making.
Detailed Experimental Protocol for ddPCR-Based MRD Assay
Sample Preparation and Nucleic Acid Extraction
- Sample Type: Use bone marrow aspirates or peripheral blood samples collected in EDTA tubes. Process samples within 24-48 hours of collection.
- Nucleic Acid Extraction: Extract DNA or RNA using commercial kits (e.g., QIAamp DNA Blood Mini Kit or equivalent for DNA; acid-phenol guanidinium thiocyanate-based methods for RNA). For RNA, include a DNase digestion step. Precisely quantify the extracted nucleic acids using a spectrophotometer (e.g., NanoDrop) or fluorometer (e.g., Qubit). For MRD detection, input 50-200 ng of DNA or cDNA per ddPCR reaction [37] [38].
Assay Design and Optimization
- Primers and Probes: Design primers and hydrolysis probes (e.g., TaqMan) following manufacturer guidelines (e.g., Bio-Rad Droplet Digital PCR Application Guide). Amplicon size should ideally be <200 bp for optimal amplification efficiency. The probe for the mutant or fusion transcript is typically labeled with FAM, while the reference gene (e.g., ABL1, GUSB) probe is labeled with HEX or VIC [37].
- Validation: Confirm assay specificity using conventional PCR and Sanger sequencing on patient diagnostic samples or synthetic gBLOCK gene fragments before deploying for MRD monitoring [37].
- Thermal Cycling Optimization: A generalized two-step protocol is common, but optimization is critical:
- Enzyme Activation: 95°C for 10 minutes.
- Amplification (40 cycles): Denaturation at 94°C for 30 seconds; Annealing/Extension at a temperature between 58-64°C for 1-1.5 minutes [37].
- Enzyme Deactivation: 98°C for 10 minutes.
- Hold at 4-12°C.
- The optimal annealing/extension temperature must be determined empirically for each assay. For instance, the PICALM::MLLT10 fusion required a lower temperature (58°C) for higher PCR efficiency, while a CEBPA deletion assay required a higher denaturation temperature (96°C) to reduce "raindrops" (suboptimal amplification) and increase total copy number [37].
ddPCR Reaction Setup and Data Analysis
- Reaction Mixture: Prepare a 20-22 μL reaction volume containing ddPCR supermix (e.g., Bio-Rad ddPCR Supermix for Probes), forward and reverse primers (final concentration typically 900 nM each), FAM and HEX-labeled probes (final concentration typically 250 nM each), and the template DNA/cDNA.
- Droplet Generation: Load the reaction mixture into a droplet generator cartridge along with droplet generation oil. Generate droplets according to the instrument manufacturer's protocol (e.g., using a QX200 Droplet Generator, Bio-Rad).
- PCR Amplification: Transfer the emulsified samples to a 96-well PCR plate. Seal the plate and perform PCR amplification in a thermal cycler using the optimized protocol.
- Droplet Reading and Analysis: After amplification, load the plate into a droplet reader (e.g., QX200 Droplet Reader, Bio-Rad). The reader streams droplets single-file past a fluorescence detector. Analyze the data using vendor software (e.g., QuantaSoft, Bio-Rad). Set thresholds to distinguish positive and negative droplets for FAM and HEX channels. The software uses Poisson statistics to calculate the absolute concentration of the target (copies/μL) and the control gene, from which the target ratio or VAF is derived [37] [38] [3].
Figure 2: A clinical decision pathway based on ddPCR MRD monitoring results, particularly in the post-transplant setting.
Essential Reagents and Research Solutions
A successful ddPCR MRD assay relies on a suite of specialized reagents and instruments. The following table details key components and their functions in the experimental workflow.
Table 3: Research Reagent Solutions for ddPCR MRD Assays
| Item Category | Specific Examples | Function/Brief Explanation |
|---|---|---|
| ddPCR System | QX200 System (Bio-Rad), QuantStudio Absolute Q (Thermo Fisher) | Instrument platform for droplet generation, thermal cycling, and droplet reading. The Absolute Q system uses a microfluidic array plate (MAP) technology instead of droplets [39] [3]. |
| ddPCR Supermix | ddPCR Supermix for Probes (Bio-Rad) | Optimized PCR master mix containing DNA polymerase, dNTPs, buffers, and stabilizers formulated for the ddPCR environment. |
| Primers & Probes | Custom TaqMan Assays | Target-specific oligonucleotides. Primers flank the region of interest, while hydrolysis probes (FAM/HEX labeled) enable specific detection. Can be pre-designed (e.g., Absolute Q Liquid Biopsy Assays) or custom-made [39]. |
| Nucleic Acid Kits | QIAamp DNA Blood Mini Kit (Qiagen) | For high-quality and consistent extraction of DNA or RNA from patient samples, which is critical for assay sensitivity and reproducibility [38]. |
| Droplet Generation Oil | Droplet Generation Oil for Probes (Bio-Rad) | Immiscible oil used to create the water-in-oil emulsion for partitioning the sample. Contains surfactants for droplet stability during thermal cycling. |
| Restriction Enzymes | EcoRI-HF (NEB) | Sometimes required for mutation detection assays to cleave wild-type sequences and improve specificity or to overcome amplicon size limitations [37]. |
Droplet Digital PCR represents a significant advancement in the technological arsenal for monitoring minimal residual disease. Its exceptional sensitivity, precision, and ability to provide absolute quantification without standard curves make it an indispensable tool for personalizing patient management, particularly in haematological malignancies. The technology enables clinicians to detect early signs of molecular relapse, assess deep molecular responses, and make informed decisions about treatment intensification or cessation. As research continues to validate new markers and standardize protocols, ddPCR is poised to become an even more central pillar in the framework of precision oncology, ultimately improving survival and quality of life for patients.
Droplet Digital PCR (ddPCR) represents a transformative advancement in molecular diagnostics, enabling absolute quantification of nucleic acids with exceptional sensitivity. This technology partitions a PCR reaction into thousands of nanoliter-sized water-in-oil droplets, effectively creating individual micro-reactors where amplification occurs independently [3]. The fundamental principle relies on Poisson statistics applied to the fraction of positive and negative droplets post-amplification, allowing for precise, calibration-free quantification of target sequences without standard curves [37] [3]. This technical capability positions ddPCR as an ideal platform for detecting rare genetic variants in complex biological samples—a critical requirement in oncology for monitoring tumor dynamics through liquid biopsies.
In the context of cancer research, ddPCR addresses two significant challenges: the need for ultrasensitive detection of minimal residual disease (MRD) and the requirement for monitoring treatment response through circulating tumor DNA (ctDNA). Its ability to detect mutant alleles at frequencies as low as 0.01%-0.4% variant allele frequency (VAF) surpasses conventional quantitative PCR and, in certain applications, even next-generation sequencing (NGS) [40] [41]. This technical review examines two specific cancer models—rectal and lung cancer—where ddPCR implementation has yielded substantial insights into disease monitoring and treatment personalization, highlighting experimental protocols, performance metrics, and practical implementation frameworks.
Rectal Cancer Case Study: ddPCR for ctDNA Detection and Monitoring
Study Design and Performance Metrics
A comprehensive 2025 study directly compared ddPCR against next-generation sequencing (NGS) for detecting circulating tumor DNA (ctDNA) in localized rectal cancer [40]. The research employed a rigorous approach, analyzing pre-therapy plasma and tumor samples from a development cohort (n=41) and a validation cohort (n=26). Tumor tissue underwent NGS analysis using the Ion AmpliSeq Cancer Hotspot Panel v2 to identify patient-specific mutations. Researchers then designed personalized ddPCR assays targeting one to two mutations exhibiting the highest variant allele frequencies in matched tumors.
The performance comparison revealed ddPCR's superior sensitivity in baseline plasma detection:
Table 1: Detection Rate Comparison Between ddPCR and NGS in Rectal Cancer
| Patient Cohort | ddPCR Detection Rate | NGS Detection Rate | Statistical Significance |
|---|---|---|---|
| Development Cohort (n=41) | 24/41 (58.5%) | 15/41 (36.6%) | p = 0.00075 |
| Validation Cohort (n=26) | 21/26 (80.8%) | Not reported | Not applicable |
The significantly higher detection rate with ddPCR underscores its enhanced sensitivity for low-abundance mutations in plasma. Furthermore, ctDNA positivity correlated strongly with advanced disease features, including higher clinical tumor stage and lymph node positivity identified on MRI [40]. This association suggests potential clinical utility for ddPCR in stratifying patients based on tumor aggressiveness before treatment initiation.
Experimental Protocol and Technical Implementation
The methodological framework for this study followed a standardized workflow:
Sample Collection: Blood samples (3 × 9 mL) were collected in Streck Cell-Free DNA BCT tubes before neoadjuvant therapy and processed within a strict pre-analytical window.
cfDNA Extraction: Plasma was separated via centrifugation (2,000 × g for 10 minutes), followed by cfDNA extraction using the QIAamp Circulating Nucleic Acid Kit (Qiagen). DNA was eluted in 100 μL of AVE buffer.
Tumor Genotyping: DNA from tumor specimens (surgical resections or pre-therapy biopsies) was analyzed using the Ion AmpliSeq Cancer Hotspot Panel v2 (Thermo Fisher) to identify somatic mutations.
ddPCR Assay Design: Patient-specific ddPCR assays were designed for one to two predominant mutations identified in tumor tissue. The reaction mixture (20 μL) included:
- 8 μL of extracted cfDNA
- 10 μL of 2× ddPCR Supermix
- 1 μL of each primer/probe set (FAM/HEX labeled)
- 1 μL of restriction enzyme (if required)
Droplet Generation and Amplification: Samples were partitioned into approximately 20,000 droplets using the QX200 Droplet Generator (Bio-Rad). PCR amplification followed this protocol:
- Enzyme activation: 95°C for 10 minutes
- 40-45 cycles of:
- Denaturation: 94°C for 30 seconds
- Annealing/Extension: Primer-specific temperature (52-60°C) for 1 minute
- Enzyme deactivation: 98°C for 10 minutes
- 4°C hold
Droplet Reading and Analysis: Droplets were analyzed using the QX200 Droplet Reader (Bio-Rad), with data interpretation via QuantaSoft software (Bio-Rad). Mutant allele frequency was calculated based on Poisson statistics of positive and negative droplets [40].
Figure 1: Rectal Cancer ctDNA Analysis Workflow. This diagram illustrates the complete process from sample collection to result interpretation in the rectal cancer ctDNA study.
Lung Cancer Case Study: EGFR Mutation Detection for Treatment Guidance
Detection of Primary and Treatment-Emergent Mutations
A pivotal 2018 study demonstrated ddPCR's clinical utility for detecting EGFR mutations in non-small cell lung cancer (NSCLC) patients [41]. The research stratified 133 patients into three distinct groups to evaluate different clinical scenarios:
Table 2: ddPCR Performance in EGFR Mutation Detection Across Patient Groups
| Patient Group | Clinical Context | ddPCR Detection Rate | Key Findings |
|---|---|---|---|
| Group 1 (n=40) | Treatment-naïve, tissue-positive for EGFR Del19/L858R | 35/40 (87.5%) for primary mutations | 4 cases with T790M detected in plasma but not in initial tissue biopsy |
| Group 2 (n=73) | TKI-treated with radiographic progression | 39/73 (53.4%) for T790M resistance mutation | ddPCR detected T790M in 7/11 cases where tissue biopsy was negative |
| Group 3 (n=20) | Treatment-naïve, tissue-negative for EGFR mutations | 0/20 (100% specificity) | No false positives, confirming assay specificity |
The study yielded several critical insights. In Group 1, ddPCR detected primary EGFR mutations with 87.5% sensitivity and 100% specificity compared to tissue biopsy, demonstrating excellent concordance (Cohen's kappa = 0.82) [41]. Notably, ddPCR identified T790M mutations—a known resistance mechanism to first-generation TKIs—in four treatment-naïve patients whose initial tissue biopsies were negative, suggesting potential for identifying de novo resistance clones.
In the TKI-resistant cohort (Group 2), ddPCR detected the T790M mutation in 53.4% of cases, aligning with established literature that approximately 50-60% of TKI resistance is mediated by this mechanism [41]. Importantly, in a subset of 11 patients who underwent secondary tissue biopsy, ddPCR detected T790M in seven cases where tissue testing was negative, highlighting its superior capability to capture tumor heterogeneity non-invasively.
Technical Methodology and Validation Framework
The lung cancer study implemented a rigorous technical approach:
Sample Processing: Blood samples (10 mL) were collected in EDTA tubes and processed within 1 hour. Plasma was separated via centrifugation, and cfDNA was extracted using the QIAamp Circulating Nucleic Acid Kit (Qiagen).
ddPCR Assay Configuration: Commercially available primer/probe sets (Bio-Rad) specifically targeting EGFR Del19, L858R, and T790M mutations were employed. Each 20 μL reaction mixture contained:
- 8 μL of template cfDNA
- 10 μL of 2× ddPCR Supermix
- 1 μL of EGFR mutation assay (FAM-labeled)
- 1 μL of reference assay (HEX-labeled)
Thermal Cycling Conditions: The amplification protocol followed manufacturer recommendations:
- Initial denaturation: 95°C for 10 minutes
- 40 cycles of:
- Denaturation: 94°C for 30 seconds
- Annealing/Extension: 55°C for 60 seconds
- Signal stabilization: 98°C for 10 minutes
- 4°C hold
Quality Control and Analysis: Thresholds for positive/negative droplet calls were established using control samples. Mutant allele frequency was calculated as: [mutant copies / (mutant copies + wild-type copies)] × 100. Samples with ≥3 mutant droplets were considered positive, based on Poisson statistics confidence limits [41].
Figure 2: Lung Cancer EGFR Mutation Monitoring Pathway. This clinical decision pathway illustrates how ddPCR integrates into patient management from initial diagnosis through treatment resistance monitoring.
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of ddPCR in cancer research requires specific reagents and instrumentation. The following table details essential components referenced in the case studies:
Table 3: Essential Research Reagents for ddPCR in Oncology Applications
| Reagent/Material | Specific Product Examples | Application Function |
|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, EDTA tubes | Preserves blood cells and prevents genomic DNA contamination during transport and storage |
| cfDNA Extraction Kit | QIAamp Circulating Nucleic Acid Kit (Qiagen) | Isolves cell-free DNA from plasma with high efficiency and minimal fragmentation |
| ddPCR Supermix | ddPCR Supermix for Probes (Bio-Rad) | Provides optimized buffer, nucleotides, and polymerase for droplet-based PCR reactions |
| Mutation Assays | Bio-Rad ddPCR Mutation Assays, Custom TaqMan Assays | Target-specific primers and fluorescent probes (FAM/HEX) for mutant and wild-type alleles |
| Droplet Generation Oil | Droplet Generation Oil for Probes (Bio-Rad) | Creates stable water-in-oil emulsion for partitioning PCR reactions |
| Restriction Enzymes | EcoRI-HF (NEB) | Digests wild-type sequences in certain assay designs to enhance mutation detection sensitivity |
| Bisulfite Conversion Kit | EZ DNA Methylation-Lightning Kit (Zymo Research) | Converts unmethylated cytosine to uracil for methylation-specific ddPCR applications |
| Instrument Platform | QX200 Droplet Digital PCR System (Bio-Rad) | Integrated system for droplet generation, thermal cycling, and droplet reading |
Discussion: Technical Advantages and Implementation Considerations
The case studies demonstrate distinct technical advantages of ddPCR in oncology applications. For rectal cancer monitoring, ddPCR showed significantly higher detection rates (58.5-80.8%) compared to NGS (36.6%) in pre-therapy plasma [40]. This enhanced sensitivity stems from ddPCR's ability to detect rare mutations against a background of wild-type DNA without requiring the extensive sequencing depths necessary for NGS. Furthermore, the 5-8.5-fold lower operational costs of ddPCR compared to NGS enhance its practicality for serial monitoring applications [40].
In lung cancer management, ddPCR provided excellent concordance with tissue biopsy (kappa = 0.82) while additionally detecting resistance mutations missed by standard tissue testing [41]. This capability is particularly valuable for assessing tumor heterogeneity and identifying resistant clones early during treatment. The technology's precision enables reliable detection at variant allele frequencies as low as 0.01%-0.4%, crucial for monitoring minimal residual disease and early recurrence [40] [41].
Methodological optimization remains essential for successful ddPCR implementation. Key considerations include:
Primer/Probe Design: Following manufacturer guidelines for amplicon size (<200 bp) and avoiding sequences with secondary structures improves amplification efficiency [37].
Thermal Cycling Optimization: Gradient testing of annealing temperatures (58-68°C range) enhances cluster separation and signal intensity [37]. The addition of restriction enzymes can improve assay specificity for challenging targets [37].
Sample Quality Control: Implementing extraction controls (exogenous spike-ins) and assessing genomic DNA contamination ensures result reliability [42] [43].
Data Interpretation: Establishing appropriate thresholds for positive calls (typically ≥3 mutant droplets) and applying Poisson confidence intervals ensures accurate quantification at low target concentrations [41].
Emerging applications continue to expand ddPCR's utility in cancer research. Methylation-specific ddPCR assays, such as those detecting methylated SEPT9 in colorectal cancer [43] or multi-marker panels in lung cancer [42], enable epigenetic profiling from liquid biopsies. The combination with coamplification at lower denaturation temperature PCR (COLD-PCR) enables mutation scanning across genomic regions, further expanding ddPCR's capabilities [44].
These case studies firmly establish ddPCR as a robust, sensitive, and clinically applicable technology for molecular analysis in rectal and lung cancers. Its superior sensitivity over NGS for detecting low-frequency mutations in rectal cancer ctDNA and its exceptional performance in monitoring EGFR treatment resistance in lung cancer highlight its dual value in both diagnostic and monitoring contexts. The technical protocols, reagent frameworks, and implementation guidelines presented herein provide researchers with practical pathways for incorporating ddPCR into their oncology research programs. As liquid biopsy applications continue to evolve, ddPCR's unique combination of sensitivity, precision, and practical efficiency positions it as an indispensable tool in the advancing era of precision oncology.
Maximizing Assay Performance: ddPCR Troubleshooting and Optimization Strategies
The accurate detection of rare mutations is a cornerstone of modern precision medicine, influencing prognostic evaluation and treatment selection in fields like oncology. However, this critical task is often hampered by the inherent complexity of clinical specimens. Samples such as blood, formalin-fixed paraffin-embedded (FFPE) tissue, and tumor biopsies frequently contain substances that inhibit polymerase activity, complicating nucleic acid quantification [20]. These inhibitors include hemoglobin, bile salts, humic acids, and residual proteins or chemicals from sample processing reagents [45] [20]. In traditional quantitative PCR (qPCR), the presence of such substances can delay amplification, reduce reaction efficiency, and lead to significant underestimation of target concentration, an effect that is particularly detrimental when quantifying low-abundance targets [45] [46].
Droplet Digital PCR (ddPCR) presents a paradigm shift in managing this challenge. As a third-generation PCR technology, ddPCR's unique partitioning workflow and endpoint detection confer a naturally higher tolerance to inhibitors compared to qPCR [47] [20]. This technical guide explores the mechanisms behind this robustness and provides detailed methodologies for leveraging ddPCR to achieve precise and reliable rare mutation detection in even the most complex clinical samples.
Theoretical Basis: How ddPCR Mitigates Inhibition Effects
The fundamental difference between ddPCR and qPCR lies in their approach to quantification. qPCR relies on measuring the amplification kinetics during the exponential phase of PCR, where the cycle threshold (Cq) is profoundly sensitive to any factor that slows down amplification [48] [46]. In contrast, ddPCR partitions a single PCR reaction into tens of thousands of nanoliter-sized water-in-oil droplets, effectively creating independent micro-reactors [3] [20]. Each droplet undergoes endpoint amplification, and the readout is simply binary: positive or negative for the target sequence. The absolute concentration of the target nucleic acid is then calculated using Poisson statistics based on the fraction of positive droplets, without reference to a standard curve [48] [20].
This digital approach confers two key advantages against inhibitors:
- Effective Dilution of Inhibitors: During partitioning, inhibitor molecules are randomly distributed across the thousands of droplets. This drastically reduces their local concentration within any single droplet, minimizing their impact on the polymerase enzyme [20]. In a bulk qPCR reaction, inhibitors affect the entire reaction volume, whereas in ddPCR, they only affect a subset of droplets.
- Endpoint Detection Independence: Since ddPCR quantification depends on a final, binary fluorescence measurement and not the kinetics of amplification (Cq), it is unaffected by a delayed or slowed amplification. A droplet will be counted as positive as long as sufficient amplification occurs to cross the fluorescence threshold by the end of the cycling process, even if the amplification is slower due to partial inhibition [45] [20].
The following diagram illustrates this core concept of sample partitioning and how it manages inhibitors.
Experimental Evidence: Quantitative Comparison of qPCR and ddPCR Performance
Direct comparisons between qPCR and ddPCR under controlled conditions of contamination consistently demonstrate the superior resilience of the digital method. A seminal study using synthetic DNA samples spiked with variable amounts of reverse transcription (RT) mix—a common source of PCR inhibitors—revealed stark differences in performance [45].
When the RT mix volume was increased from 4 µL to 5 µL, qPCR reaction efficiency dropped significantly from approximately 89.6% to 67.1%. This efficiency loss translated into an approximate 2 Cq shift, corresponding to a perceived four-fold reduction in the calculated relative quantity of the target, despite the actual DNA concentration remaining unchanged [45]. In contrast, ddPCR analysis of the identical reaction mixtures showed minimal variability in the calculated absolute concentration at each DNA dilution, successfully converting what was "uninterpretable" qPCR data into highly quantitative and reproducible results [45].
The table below summarizes the core performance differences between the two technologies in the presence of inhibitors.
Table 1: Comparative Performance of qPCR vs. ddPCR in Inhibitor-Rich Environments
| Parameter | Quantitative PCR (qPCR) | Droplet Digital PCR (ddPCR) |
|---|---|---|
| Quantification Method | Relative (based on Cq from standard curve) | Absolute (based on Poisson statistics of positive partitions) |
| Impact of Inhibitors | High; delays Cq, reduces amplification efficiency, causes underestimation | Low; inhibitors are diluted, endpoint detection minimizes impact [20] |
| Data Quality with Low-Abundance Targets (Cq ≥29) | Highly variable, artifactual, and non-reproducible [45] | Precise, reproducible, and statistically significant [45] |
| Best Use Case for Rare Allele Detection | Limited due to sensitivity to efficiency variations | Ideal; high sensitivity and precision for rare mutations in a wild-type background [47] [20] |
Detailed Experimental Protocol: IDH Mutation Detection in Glioma
The following section details a validated experimental protocol for detecting Isocitrate Dehydrogenase 1 (IDH1) mutations in patient-derived glioma samples, a key application in neuro-oncology with significant prognostic implications [15]. This protocol exemplifies a real-world implementation of ddPCR for rare mutation detection in a clinical specimen.
Research Reagent Solutions and Materials
Table 2: Essential Reagents and Materials for ddPCR Mutation Detection
| Item | Function | Example/Details |
|---|---|---|
| ddPCR Supermix for Probes | Provides optimized buffer, dNTPs, and polymerase for probe-based digital PCR. | Bio-Rad's ddPCR Supermix for Probes (No dUTP) [15]. |
| Mutation Detection Assay | Target-specific primers and fluorescently labeled probes for wild-type and mutant alleles. | 20X ddPCR Mutation Detection Assays (e.g., for IDH1-R132H) [15]. |
| Restriction Enzyme | Can be used to digest wild-type sequences and improve assay specificity for rare mutant detection. | HaeIII (10 U/µL) [15]. |
| Genomic DNA | The analyte; template nucleic acids extracted from the clinical specimen. | 50 ng/µL of patient-derived tissue DNA [15]. |
| Droplet Generation Oil | Immiscible oil phase for creating stable water-in-oil emulsions. | Bio-Rad Droplet Generation Oil [15]. |
| DG8 Cartridges and Gaskets | Microfluidic consumables for generating uniform droplets. | Used with the QX200/QS600 Droplet Generator [15]. |
Step-by-Step Workflow
Reaction Mixture Preparation:
- In a sterile tube, combine the following components to a final volume of 20 µL:
- 10 µL of 2X ddPCR Supermix for Probes.
- 1 µL of 20X ddPCR Mutation Detection Assay (containing both wild-type and mutant-specific primers/probes).
- 1 µL of restriction enzyme HaeIII (10 U/µL).
- 50 ng of patient-derived genomic DNA.
- Nuclease-free water to adjust the volume.
- Gently mix the reaction mixture by pipetting. Do not vortex, as it may cause foam formation [15].
- In a sterile tube, combine the following components to a final volume of 20 µL:
Droplet Generation:
- Transfer 20 µL of the reaction mixture into the middle well of a DG8 cartridge.
- Carefully add 70 µL of Droplet Generation Oil to the bottom wells of the cartridge.
- Place a DG8 gasket over the cartridge.
- Load the cartridge assembly into the droplet generator. The instrument will automatically create thousands of nanoliter-sized droplets, which will collect in the designated outlet well [15].
PCR Amplification:
- Carefully transfer 40 µL of the generated droplet emulsion into a semi-skirted 96-well PCR plate. Seal the plate with a foil heat seal.
- Place the plate in a conventional thermal cycler and run the following standard PCR protocol:
- Enzyme activation: 95°C for 10 minutes.
- 40 cycles of:
- Denaturation: 94°C for 30 seconds.
- Annealing/Extension: 55-60°C (assay-specific) for 60 seconds.
- Enzyme deactivation: 98°C for 10 minutes.
- Hold at 4°C.
- Note: A ramping rate of 2°C/second is recommended to maintain droplet integrity [15].
Droplet Reading and Data Analysis:
- After amplification, place the plate in a droplet reader. The instrument will aspirate each sample sequentially, flowing droplets single-file past a two-color optical detection system.
- The reader counts the total number of droplets and identifies each as positive for the mutant channel (e.g., FAM), wild-type channel (e.g., HEX), both, or neither.
- Using the raw count data, the instrument's software applies Poisson statistics to calculate the absolute concentration (in copies/µL) of the wild-type and mutant targets in the original sample.
- Set validated cut-off values for positive calls (e.g., 7.0 copies/reaction for IDH1 mutation and 5.0 copies/reaction for wildtype IDH1, as used in one study) to distinguish true positives from background [15].
The entire workflow, from sample partitioning to final result, is visualized below.
Droplet Digital PCR technology provides a robust and powerful solution for overcoming the challenge of PCR inhibitors in complex clinical specimens. Its fundamental principles of massive sample partitioning and endpoint detection effectively dilute the impact of inhibitors and decouple quantification from amplification efficiency, enabling a level of precision and sensitivity that is difficult to achieve with qPCR, especially for low-abundance targets [45] [20]. As demonstrated in the IDH1 glioma assay, this makes ddPCR exceptionally suited for critical clinical applications like rare mutation detection, liquid biopsy, and minimal residual disease monitoring [15] [20].
The ongoing evolution of ddPCR, including the development of more portable, integrated systems and advanced data analysis algorithms, promises to further solidify its role in molecular diagnostics [3] [15]. For researchers and drug development professionals, adopting and optimizing ddPCR protocols is key to generating publication-quality data and making reliable clinical decisions based on accurate genetic information extracted from even the most challenging samples.
Digital PCR (dPCR) represents a transformative technology in molecular diagnostics, particularly for the detection and quantification of rare mutations in cancer and genetic disease research. Unlike quantitative PCR (qPCR), which relies on relative quantification against a standard curve, dPCR provides absolute quantification of target nucleic acid sequences by partitioning a sample into thousands of individual reactions, with each partition functioning as a separate PCR vessel [49]. This partitioning enables the detection of rare mutations present at frequencies as low as 0.1% or even lower, making it an indispensable tool for applications such as liquid biopsy analysis, where minute quantities of circulating tumor DNA (ctDNA) must be detected against a background of abundant wild-type DNA [39].
The exceptional sensitivity and specificity of dPCR for rare mutation detection are fundamentally dependent on optimal primer and probe design. Properly designed assays can distinguish single-nucleotide polymorphisms (SNPs) with high precision, enabling researchers to identify emerging treatment-resistant clones in cancer patients or detect minimal residual disease after therapy [4]. The design process must account for numerous factors, including target sequence characteristics, secondary structures, GC content, and potential off-target binding sites. This technical guide provides comprehensive strategies for designing primers and probes that maximize specificity and efficiency in dPCR assays, with particular emphasis on applications in rare mutation detection for research and drug development.
Core Principles of dPCR Assay Design
Fundamental Design Parameters
The design of primers and probes for dPCR follows similar principles to qPCR but demands even greater stringency due to the digital nature of the quantification. Key design considerations include amplicon length, melting temperature (Tm), specificity checks, and avoidance of secondary structures. For dPCR applications, amplicon length should generally be kept between 60-150 base pairs to ensure efficient amplification within the partitioned reactions [49]. Shorter amplicons typically amplify more efficiently, which is particularly important when working with degraded samples such as formalin-fixed, paraffin-embedded (FFPE) tissues or cell-free DNA (cfDNA) from plasma.
The melting temperatures of forward and reverse primers should be carefully balanced, with ideally less than 1°C difference between them. The Tm for probes should be 5-10°C higher than the primers to ensure probe hybridization prior to primer extension. Probe-based assays using hydrolysis chemistry (such as TaqMan) are generally preferred for dPCR applications because they provide greater specificity than intercalating dyes, which is crucial when distinguishing mutant from wild-type sequences that may differ by only a single nucleotide [49]. This enhanced specificity comes from the requirement that the probe must bind to its exact complementary sequence for fluorescence to be generated.
Design Strategies for Challenging Targets
Some genetic targets present particular challenges for PCR amplification due to their sequence characteristics. GC-rich regions, such as the TERT promoter (approximately 80% GC content), can form stable secondary structures that inhibit DNA polymerase progression [50]. In such cases, specialized reagents can be incorporated into the reaction mix to improve amplification efficiency. As demonstrated in TERT promoter mutation assays, the addition of betaine (5 M final concentration) and disodium EDTA (20 mM final concentration) can significantly enhance amplification efficiency by reducing secondary structure formation and inhibiting enzymes that may degrade the DNA template [50].
For multiplex dPCR assays, where multiple targets are detected simultaneously, careful design is essential to prevent cross-reactivity and ensure accurate quantification. Since dPCR partitions individual template molecules, the primers and probes for different targets do not compete in the same way they might in a conventional multiplex qPCR reaction [49]. However, all primer pairs and probes in a multiplex reaction must function efficiently under identical thermal cycling conditions, requiring careful Tm matching and comprehensive specificity validation.
Table 1: Core Design Parameters for dPCR Primers and Probes
| Parameter | Optimal Range | Considerations for Rare Mutation Detection |
|---|---|---|
| Amplicon Length | 60-150 bp | Shorter amplicons preferred for degraded samples (cfDNA, FFPE) |
| Primer Tm | 58-60°C | <1°C difference between forward and reverse primers |
| Probe Tm | 65-70°C | 5-10°C higher than primers |
| GC Content | 30-80% | Additives like betaine may be needed for high GC targets |
| Primer Length | 18-25 bases | Balance between specificity and Tm requirements |
| Probe Length | 15-30 bases | Must not overlap with primer binding sites |
Specialized Design Strategies for Rare Mutation Detection
Dual-Probe Approach for SNP Detection
The detection of rare single-nucleotide variants requires specialized design strategies to achieve the necessary specificity. The most common approach utilizes a dual-probe system, where two hydrolysis probes target the same genomic locus but are specific to either the wild-type or mutant sequence [4]. These probes are labeled with different fluorophores (e.g., FAM for mutant and HEX/VIC for wild-type) to enable discrimination in the dPCR platform's detection channels.
For the EGFR T790M mutation detection assay, researchers used one FAM-labeled hydrolysis probe to detect the mutant sequence (T790M) and one Cy3-labeled probe to detect the wild-type sequence [4]. Both probes were used with a single set of primers that amplified the region of interest, ensuring that amplification efficiency was identical for both targets. This approach is critical for accurate quantification of mutation allele frequency, as any difference in amplification efficiency between separate reactions would introduce quantification errors.
The positioning of the mutation within the probe sequence significantly impacts discrimination capability. Ideally, the variant nucleotide should be positioned near the center of the probe sequence to maximize the difference in hybridization efficiency between matched and mismatched probes. Mismatches near the center of the probe have a more dramatic effect on Tm than those near the ends, enhancing the ability to distinguish between wild-type and mutant sequences. Additionally, locked nucleic acid (LNA) modifications can be incorporated into probes to increase binding specificity, particularly for challenging SNP detection applications [51].
Optimization for Maximum Specificity
Achieving optimal specificity in rare mutation detection requires careful optimization of both probe design and reaction conditions. For the TERT promoter mutation assays, researchers developed nine different primer pairs before identifying three that produced amplicons of 88, 113, or 163 bp that worked robustly in the dPCR format [50]. This extensive optimization process highlights the empirical nature of assay development for challenging targets.
The annealing temperature is a critical parameter that must be optimized to maximize the difference in hybridization efficiency between perfectly matched and mismatched probes. Using a temperature gradient during validation can help identify the optimal annealing temperature that provides clear separation between positive and negative droplets while maintaining robust amplification efficiency. For the Salmonella detection ddPCR assay, researchers tested a temperature gradient from 55-63°C before establishing 60°C as the optimal annealing temperature [52].
The concentration of primers and probes also requires optimization to ensure efficient amplification while minimizing non-specific signals. For the validated Salmonella assay, the optimal primer concentration was determined to be 600 nM with probes at 300 nM [52]. Higher primer concentrations may improve amplification efficiency but can also increase the formation of primer-dimers or non-specific amplification products, particularly in complex samples.
Diagram 1: Rare Mutation Detection Workflow
Experimental Protocols and Validation
Step-by-Step Assay Design and Optimization Protocol
Developing a validated dPCR assay for rare mutation detection requires a systematic approach to design, optimization, and validation. The following protocol outlines the key steps based on successful implementations from the literature:
Step 1: In Silico Design Begin by retrieving the target sequence from a reliable database such as GenBank. For the TERT promoter assays, researchers used the sequence with GenBank accession numbers for reference [50]. Design primers to amplify a 60-150 bp region surrounding the mutation of interest, ensuring they do not contain polymorphisms or span intron-exon boundaries (when working with gDNA). Design two hydrolysis probes that are identical except for the nucleotide at the mutation position, with fluorophores that are compatible with your dPCR system and can be spectrally distinguished.
Step 2: Primary Optimization Test the initial designs using a temperature gradient to determine the optimal annealing temperature. Prepare reaction mixtures containing 1X dPCR supermix, 300-900 nM primers, 100-300 nM probes, and template DNA in a total volume of 20-25 μL depending on the platform specifications [52] [50]. For challenging GC-rich targets, include additives such as betaine (1-1.5 M final concentration) and EDTA (1-2 mM final concentration) in the optimization process [50]. Cycle conditions should include an initial denaturation at 95°C for 5-10 minutes, followed by 40-50 cycles of denaturation at 95°C for 30 seconds and annealing/extension at the gradient temperatures for 30-60 seconds.
Step 3: Limit of Detection (LOD) Determination Once optimal conditions are established, determine the assay's limit of detection by testing serial dilutions of mutant DNA in a background of wild-type DNA. For the TERT promoter assays, the LOD was determined to be 0.051% and 0.062% mutant allele fraction for the C250T and C228T assays, respectively [50]. Calculate the theoretical LOD based on the number of partitions and the total DNA input using the formula: Sensitivity = Theoretical LOD of the system / Total target concentration in the sample [4].
Step 4: Specificity Testing Validate assay specificity using orthogonal methods such as Sanger sequencing or SNaPShot analysis. The TERT promoter assays demonstrated 100% concordance with sequencing-based methods across 32 FFPE melanoma tumors [50]. Test against samples with known mutations in similar sequences to check for cross-reactivity.
Troubleshooting Common Issues
Even with careful design, dPCR assays may require troubleshooting to achieve optimal performance. Common issues and their solutions include:
Rain Effect (Intermediate Fluorescence): The presence of partitions with fluorescence intensity between clearly positive and negative clusters can complicate analysis. This "rain" effect may be caused by incomplete amplification, probe degradation, or suboptimal thermal cycling conditions. To address this, ensure complete droplet generation, optimize annealing temperature, and consider using different probe chemistry or additives [53].
Poor Partition Separation: If the positive and negative populations are not well separated, consider increasing the probe concentration or adjusting the annealing temperature. For the Salmonella detection assay, researchers used a kernel density estimation algorithm to categorize partitions into positive, negative, and rain populations based on their fluorescence readings [53].
Low Amplification Efficiency: For targets with high GC content or secondary structure, incorporate additives such as DMSO (2-5%), trehalose (0.2 M), or Tween-20 (0.5%) to improve amplification efficiency [53]. Restriction enzymes can also be used to linearize the template and improve accessibility, as demonstrated in the TERT promoter assays where CviQI was included in the reaction mixture [50].
Table 2: Troubleshooting Guide for dPCR Rare Mutation Assays
| Problem | Potential Causes | Solutions |
|---|---|---|
| High background in negative controls | Contaminated reagents | Prepare fresh master mix; use UV treatment |
| Poor separation between positive and negative clusters | Suboptimal annealing temperature | Perform temperature gradient optimization |
| Low mutant signal in known positives | Inhibition or inefficient amplification | Add enhancers (betaine, DMSO); optimize primer concentration |
| High rain effect | Incomplete amplification; probe issues | Extend elongation time; check probe quality and storage |
| Inconsistent results between replicates | Pipetting errors; droplet generation issues | Use automated liquid handling; check droplet generator performance |
Reagent Solutions and Practical Implementation
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of dPCR for rare mutation detection requires careful selection of reagents and materials. The following toolkit summarizes essential components based on validated protocols from the literature:
Table 3: Research Reagent Solutions for dPCR Rare Mutation Detection
| Reagent/Material | Function | Examples & Specifications |
|---|---|---|
| dPCR Mastermix | Provides essential components for amplification | ddPCR Supermix for Probes (Bio-Rad); Contains DNA polymerase, dNTPs, buffer, MgCl₂ [52] |
| Hydrolysis Probes | Sequence-specific detection | FAM/HEX-labeled TaqMan probes; LNA-modified for enhanced specificity [51] [49] |
| Primer Sets | Target amplification | HPLC-purified; 18-25 bp; designed to avoid secondary structures [50] |
| Restriction Enzymes | Template linearization | CviQI for GC-rich targets; improves template accessibility [50] |
| Chemical Enhancers | Overcome amplification barriers | Betaine (1-1.5 M), EDTA (1-2 mM) for GC-rich targets [50] |
| Droplet Generation Oil | Partitioning agent | Generator Oil (Bio-Rad) for water-in-oil emulsion formation [52] |
| DNA Extraction Kits | Sample preparation | QIAamp DNA Mini Kit (tissues); Circulating NA Kit (plasma) [50] |
| Quantification Standards | Quality control | Synthetic oligonucleotides with known mutations [4] |
Practical Considerations for Implementation
When implementing dPCR for rare mutation detection in a research or drug development setting, several practical considerations can significantly impact the success and reproducibility of the assays:
Sample Preparation and DNA Input: The quality and quantity of input DNA are critical factors in rare mutation detection. For liquid biopsy applications, cell-free DNA should be extracted from plasma using specialized kits designed for low-abundance targets [50]. The amount of DNA input should be calculated based on copy number requirements rather than mass, using the formula: Number of copies = mass of DNA (in ng) / 0.003 (for human gDNA) [4]. Sufficient DNA input is necessary to ensure adequate representation of rare targets; for detection of mutations at 0.1% allele frequency, approximately 100,000 haploid genome equivalents are required to have 95% confidence of detecting at least one mutant molecule.
Platform Selection and Multiplexing: Different dPCR platforms offer varying numbers of partitions, which directly impacts the theoretical limit of detection. Platforms generating 20,000 partitions can typically detect allele frequencies of 0.1%, while those with 100,000+ partitions may detect even rarer mutations [39]. Most modern dPCR systems support multiplexing with 2-5 colors, allowing for simultaneous detection of multiple mutations or inclusion of reference genes [49]. When designing multiplex assays, ensure that the fluorophores have minimal spectral overlap or implement compensation algorithms to correct for spillover [4].
Data Analysis and Quality Control: Proper data analysis is crucial for accurate mutation detection and quantification. Establish clear thresholds for positive/negative classification, and implement quality control measures including no-template controls (NTC), wild-type controls, and positive controls with known mutation allele frequencies [4]. For the TERT promoter assays, researchers established a minimum of 10,000 droplets as a quality threshold and required zero positive droplets in NTCs to avoid false positives [50]. Use Poisson statistics to calculate confidence intervals for the measured mutant allele frequencies, particularly when dealing with very low abundance targets where sampling error can significantly impact results [53].
Diagram 2: dPCR Reagent Workflow
The exceptional sensitivity and precision of digital PCR for rare mutation detection hinge on meticulously designed primers and probes. By adhering to the fundamental design parameters outlined in this guide—including appropriate amplicon length, careful Tm balancing, and strategic probe placement—researchers can develop robust assays capable of detecting mutant alleles at frequencies as low as 0.1%. The dual-probe approach for SNP detection, coupled with optimization of reaction conditions and the strategic use of enhancers for challenging targets, enables the specific quantification required for advanced applications in cancer research, liquid biopsy development, and therapeutic monitoring.
As dPCR technology continues to evolve, these design principles will remain foundational for harnessing its full potential in basic research and drug development. The rigorous validation protocols and troubleshooting strategies presented here provide a roadmap for researchers to implement publication-quality dPCR assays that generate reproducible, statistically significant data for rare mutation detection.
In the realm of droplet digital PCR (ddPCR) for rare mutation detection, establishing robust cut-off values is not merely a technical formality but a fundamental determinant of assay success. Unlike quantitative real-time PCR (qPCR), which relies on cycle threshold (Cq) values derived from amplification curves, ddPCR employs a binary readout of positive and negative partitions based on fluorescence thresholds [54] [55]. This binary quantification approach makes threshold determination particularly crucial for applications such as detecting circulating tumor DNA (ctDNA), where distinguishing true mutant signals from background noise can have direct clinical implications for cancer monitoring and treatment selection [56].
The challenge intensifies when targeting rare mutations present at frequencies below 1% of the wild-type sequence, where false positive signals can significantly impact quantification accuracy and clinical interpretation [4]. A data-driven approach to cut-off establishment provides the statistical rigor necessary to maximize detection specificity while maintaining sensitivity, ensuring that results remain reliable even at the extreme limits of detection. This technical guide outlines a comprehensive framework for establishing, validating, and implementing robust cut-off values specifically within the context of ddPCR-based rare mutation detection research.
Statistical Foundations for Cut-off Determination
Performance Metrics and Calculation Methods
The establishment of statistically sound cut-off values requires the determination of key analytical performance parameters through rigorous experimental testing. These metrics provide the quantitative foundation for threshold setting and assay validation.
Table 1: Key Performance Metrics for Cut-off Determination
| Metric | Definition | Calculation Method | Acceptance Criteria |
|---|---|---|---|
| Limit of Blank (LoB) | Highest apparent analyte concentration in blank samples | 60 measurements on blank samples at different times [57] | Target: 0 false positives in no-template controls |
| Limit of Detection (LoD) | Lowest concentration detectable with 95% confidence | Probit regression analysis of 70 measurements across dilution series [57] | 95% detection rate at LoD concentration |
| Limit of Quantification (LoQ) | Lowest concentration quantifiable with acceptable precision | 20 measurements across serial dilutions; CV < 25% [57] | CV ≤ 25% with acceptable accuracy |
The LoB establishes the baseline fluorescence threshold by testing blank samples (containing no DNA template) to define the background signal level [57]. For rare mutation detection, this is particularly critical as it helps distinguish true mutant signals from background noise in wild-type-dominated samples. The LoD then builds upon this foundation by determining the minimum mutant allele concentration that can be reliably detected, typically using probit regression analysis to establish the concentration with a 95% detection rate [57].
Addressing the "Rain" Phenomenon in ddPCR
A characteristic challenge in ddPCR analysis is the "rain" phenomenon—droplets that exhibit intermediate fluorescence signals falling between explicit positive and negative populations [58]. This phenomenon can arise from various sources including delayed PCR onset, partial PCR inhibition in individual droplets, or damaged droplets with altered fluorescence characteristics [58]. For rare mutation detection, misclassification of these intermediate signals can disproportionately impact results due to the low abundance of true mutant targets.
Advanced approaches to address rain include computer-based algorithms that evaluate both fluorescence channels simultaneously and calculate a droplet separation value based on both absolute fluorescence signal distance between positive and negative populations and the variation within these populations [58]. This objective metric facilitates the optimization of assay parameters to maximize separation and minimize ambiguous classifications, thereby enhancing the reliability of cut-off values.
Experimental Protocol for Cut-off Establishment
Assay Design and Optimization Phase
The foundation for robust cut-off values begins with careful assay design and optimization. For rare mutation detection, this typically involves a probe-based approach with two different hydrolysis probes—one targeting the wild-type sequence and another targeting the mutant allele, both using the same primer set [4].
Step 1: Primer and Probe Design
- Design primers to amplify the region of interest containing the mutation site
- Design hydrolysis probes with the mutant probe spanning the mutation site
- Incorporate locked nucleic acid (LNA) bases into probes to enhance discrimination between wild-type and mutant sequences [56]
- Select fluorophores with minimal spectral overlap (e.g., FAM and HEX/Cy3) compatible with your ddPCR system [4]
Step 2: Initial Assay Validation
- Verify specificity using control templates with known mutation status
- Optimize annealing temperature using gradient PCR
- Determine optimal primer and probe concentrations (typically 500 nM for primers and 250 nM for probes) [57]
- Validate discrimination between wild-type and mutant templates
Threshold Establishment and Validation Phase
Once the assay is optimized, the following protocol establishes data-driven cut-off values:
Step 1: Define Limit of Blank (LoB)
- Prepare no-template controls (NTCs) containing all reaction components except DNA template
- Include elution buffer controls to account for potential background from extraction reagents [56]
- Run 60 measurements across multiple batches and operators [57]
- Analyze fluorescence amplitude in both channels to establish the background distribution
- Set initial fluorescence threshold above the maximum background signal observed in NTCs
Step 2: Establish Analytical Sensitivity
- Prepare serial dilutions of mutant DNA in wild-type background DNA
- Include concentrations spanning the expected detection range (e.g., 0.01%, 0.1%, 1%, 5%)
- Run multiple replicates (n ≥ 8) at each concentration [56]
- Perform probit regression analysis to determine LoD with 95% confidence [57]
Step 3: Validate with Control Materials
- Include positive template controls (PTCs) with known mutation percentages [56]
- Use certified reference materials when available [58]
- Include sample process controls spiked with synthetic DNA sequences to monitor extraction efficiency [56]
Table 2: Example Validation Data for EGFR T790M Detection
| Sample Type | Mutation Percentage | Replicates (n) | Positive Partitions | False Positive Rate |
|---|---|---|---|---|
| No-template control | 0% | 16 | 0 | 0% |
| Wild-type gDNA | 0% | 12 | 0.17 ± 0.41 | 0.0008% |
| 0.1% mutant | 0.1% | 8 | 15.5 ± 3.2 | N/A |
| 0.5% mutant | 0.5% | 8 | 78.3 ± 12.1 | N/A |
Special Considerations for Rare Mutation Detection
Determining DNA Input Requirements
The sensitivity for rare mutation detection is directly influenced by the total DNA input, which determines the number of mutant allele copies available for detection. The required DNA input can be calculated based on the desired detection sensitivity:
This calculation assumes human genomic DNA with approximately 3 pg per haploid genome [4]. For a desired sensitivity of 0.1% mutant allele frequency with 95% confidence level using a system with theoretical LOD of 0.2 copies/μL:
This calculation ensures sufficient genome equivalents are analyzed to detect the target mutation at the desired frequency with statistical confidence.
Multiplex Assay Considerations
For efficient screening of multiple mutations, singleplex assays can be combined into multiplex formats, though this introduces additional challenges for threshold setting [56]. Key considerations include:
- Spectral Compensation: Implement fluorescence spillover compensation using monocolor controls for each fluorophore [4]
- Assay Compatibility: Verify that all assays perform efficiently under unified cycling conditions
- Signal Separation: Ensure sufficient separation between all fluorescence clusters in multidimensional space
Multiplexing requires careful validation of each individual assay within the multiplex format, as performance characteristics may differ between singleplex and multiplex configurations even when using identical reagent concentrations and cycling conditions [56].
Implementation and Quality Control
Ongoing Monitoring and Threshold Adjustment
Establishing robust cut-off values is not a one-time event but requires ongoing monitoring and potential adjustment. Implement a quality control system that includes:
- Batch-specific controls: Include NTCs and PTCs in every ddPCR run [56]
- Process controls: Spike synthetic control sequences to monitor extraction efficiency [56]
- Reference materials: Use certified reference materials with known mutation percentages for periodic assay validation [58]
- Operator training: Ensure consistent technique across all personnel, particularly for droplet generation and handling
Regular review of quality control data allows for detection of assay drift and facilitates proactive adjustment of cut-off values when necessary.
Data Analysis and Interpretation
Implement standardized analysis procedures including:
- Two-dimensional clustering: Analyze fluorescence data in both channels simultaneously to distinguish true mutant signals from background [56]
- Rain management: Apply consistent algorithms for handling intermediate signals [58]
- Statistical confidence reporting: Include confidence intervals for mutation frequency measurements based on Poisson statistics
For clinical applications, establish a clear decision threshold that considers both analytical performance and biological significance, particularly for guiding treatment decisions based on mutation detection [4] [56].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for ddPCR Rare Mutation Detection
| Reagent / Material | Function | Considerations |
|---|---|---|
| ddPCR Supermix | Provides optimized buffer, enzymes, and dNTPs for partition PCR | Choose "no dUTP" version if not using UDG carryover prevention [56] |
| Hydrolysis Probes | Sequence-specific detection with fluorescent reporters | FAM/HEX common; consider LNA modifications for enhanced specificity [56] |
| Reference Genes | Control for DNA quantity and quality | RPP30 recommended for human DNA; single-copy genes preferred [56] |
| gBlock Gene Fragments | Synthetic DNA controls for assay validation | Design to match amplicon size of target; use for spike-in controls [56] |
| Certified Reference Materials | Assay validation with known mutation percentages | Horizon Discovery and IRMM provide GM materials [58] |
Workflow Visualization
Data-Driven Cut-off Establishment Workflow
Establishing robust cut-off values in ddPCR for rare mutation detection requires a systematic, data-driven approach that spans assay design, statistical validation, and ongoing quality monitoring. By implementing the protocols and considerations outlined in this guide, researchers can achieve the high level of assay robustness necessary for reliable detection of low-frequency mutations in challenging sample types such as circulating tumor DNA. The framework presented here emphasizes statistical rigor while providing practical guidance for implementation in the research setting, ultimately supporting the generation of reliable, reproducible data for drug development and clinical research applications.
Droplet Digital PCR (ddPCR) has established itself as a powerful technology for the quantitative detection of rare genetic mutations, which is critical for applications in cancer research, liquid biopsy analysis, and genetic disease monitoring. This technology operates by partitioning a PCR reaction into thousands to millions of nanoliter-sized droplets, effectively creating a massive array of independent, parallel PCR reactions. The fundamental principle relies on the statistical distribution of target DNA molecules across these partitions, enabling absolute quantification of nucleic acids without the need for a standard curve [1]. For rare mutation detection, this partitioning process effectively enriches low-level targets, allowing ddPCR to detect mutant alleles with frequencies as low as 0.1% against a background of wild-type sequences [39]. This exceptional sensitivity makes it particularly valuable for monitoring circulating tumor DNA (ctDNA) in liquid biopsies, where the concentration of tumor-derived fragments is typically low and the fragments are often short [39].
Despite its impressive capabilities, researchers must navigate significant practical limitations when implementing ddPCR in their workflows. The technology presents a unique set of challenges related to sample input requirements, analytical throughput, and operational costs that can impact experimental design, feasibility, and scalability. These constraints are particularly pronounced in large-scale clinical studies or population screening programs where processing thousands of samples quickly and cost-effectively is essential. Understanding these limitations and the emerging solutions to address them is crucial for optimizing ddPCR applications in rare mutation detection and expanding its utility in both research and potential clinical diagnostics [59].
Technical Limitations and Strategic Mitigations
Sample Input and Partitioning Constraints
The analytical sensitivity of ddPCR is fundamentally governed by Poisson statistics, which necessitates careful consideration of sample input requirements. According to Poisson distribution principles, the optimal number of target molecules per partition should be less than 1 to ensure that most positive partitions contain only a single molecule, thereby enabling accurate quantification. This statistical foundation creates practical constraints on the amount of sample that can be effectively analyzed in a single reaction, particularly for rare mutation detection where the target sequence is present in very low abundance [1].
Table 1: Sample Input Considerations in ddPCR
| Factor | Impact on Rare Mutation Detection | Recommended Optimization |
|---|---|---|
| Partition Count | Lower partition counts reduce sensitivity for rare targets; most systems generate 20,000 droplets [60]. | Use systems with higher partition counts when maximum sensitivity is required. |
| Input DNA Concentration | Excessive DNA can lead to multiple targets per droplet, violating Poisson assumptions [1]. | Dilute samples to maintain 0.001-6 copies per partition for accurate quantification [61]. |
| Sample Volume | Limited by droplet generation capacity; typically 20-40μL per reaction [60]. | Use concentrated DNA extracts to maximize target input within volume constraints. |
| Target Abundance | For 0.1% variant detection, approximately 100,000 wild-type genomes are needed for statistical confidence [39]. | Increase sample input through multiple reactions if necessary for ultra-rare targets. |
For environmental and complex biological samples, additional challenges emerge that can further complicate sample input optimization. Inhibitors present in these samples, such as humic acids in soil or heparin in blood samples, can reduce amplification efficiency even within partitions, leading to intermediate fluorescence signals known as "rain" [60]. This phenomenon makes clear discrimination between positive and negative droplets challenging and can compromise quantification accuracy. To address this, researchers can implement modified cycling conditions, including adjusted annealing temperatures and extension times, to improve amplification efficiency in compromised samples [60]. Furthermore, DNA fragmentation, which commonly occurs in clinical samples like formalin-fixed paraffin-embedded (FFPE) tissues or cell-free DNA, can reduce the effective number of amplifiable target molecules, potentially leading to an underestimation of the true target concentration [60].
Throughput Limitations in Population-Scale Applications
Throughput represents a significant constraint in ddPCR technology, particularly when compared to alternative molecular detection methods. Current droplet systems typically plateau at approximately 480 samples per day, creating a substantial bottleneck for applications requiring population-scale testing, such as newborn screening programs, epidemiological studies, or large clinical trials [59]. This limitation stems from both the physical process of droplet generation and the time-intensive nature of the thermal cycling and droplet reading steps, which collectively extend the total processing time per batch of samples.
The throughput constraint becomes particularly problematic when ddPCR is considered for applications traditionally dominated by qPCR or next-generation sequencing (NGS). Epidemiological demands driven by aging demographics are doubling assay volumes every decade, a trend that favors qPCR arrays or NGS in population-health laboratories where high-throughput capabilities are essential [59]. While manufacturers have responded with 384-sample microfluidic cartridges, these systems still face fundamental limitations related to partition-count ceilings before matching the scalability of competing technologies [59]. Consequently, ddPCR currently maintains its strongest position in applications requiring high sensitivity for low-throughput but ultra-sensitive applications rather than high-volume screening.
Table 2: Throughput Comparison of Nucleic Acid Detection Technologies
| Technology | Theoretical Maximum Throughput | Practical Limitations | Suitable Applications for Rare Mutation Detection |
|---|---|---|---|
| Droplet ddPCR | ~480 samples/day [59] | Physical partition generation and analysis time | Low-to-medium throughput studies requiring high precision |
| qPCR | Thousands of samples/day [59] | Requires standard curves; less sensitive for rare variants | High-throughput screening where extreme sensitivity is not critical |
| Next-Generation Sequencing | Varies by platform; generally high | Higher cost per sample; complex data analysis | Comprehensive mutation profiling beyond known variants |
| Microfluidic cdPCR | Emerging technology | Fixed partition counts; less flexible | Point-of-care applications; resource-limited settings |
Strategic approaches to mitigate throughput limitations include the development of multiplexed ddPCR assays that enable simultaneous detection of multiple targets within a single reaction. Recent advances have demonstrated the feasibility of 8-plex ddPCR systems for DNA methylation analysis, allowing quantification of four CpG sites within a single reaction by employing a strategy that utilizes different probe concentrations to distinguish targets based on varied fluorescence amplitudes [62]. This multiplexing capacity substantially improves efficiency and cost-effectiveness while reducing sample requirements and labor-intensive procedures. For age prediction models based on DNA methylation patterns, this 8-plex approach demonstrated a mean absolute error of just 4.59 years, highlighting the analytical precision achievable with multiplexed ddPCR despite throughput constraints [62].
Economic Considerations: Capital and Per-Sample Costs
The implementation of ddPCR technology carries significant economic considerations that impact its accessibility and scalability, particularly for resource-limited settings. Instrument entry prices typically start around $38,000, with costs escalating substantially when annual maintenance contracts, proprietary consumables, and specialized staff training are included in the total cost of ownership [59]. This high capital investment creates a substantial barrier to entry, especially for smaller laboratories or research groups with limited funding resources.
The per-sample reagent costs present an additional economic challenge for laboratories considering ddPCR implementation. Even with newer reagent bundles that consolidate multiple assays into single runs and reportedly reduce costs by up to 43%, the total per-test expense still exceeds high-throughput qPCR by 2-3 times in community hospital settings [59]. This cost differential becomes particularly significant in large-scale studies where hundreds or thousands of samples require processing, making qPCR a more economically viable option despite its lower sensitivity for rare variant detection.
Table 3: Cost Structure Analysis for ddPCR Implementation
| Cost Component | Financial Impact | Mitigation Strategies |
|---|---|---|
| Instrument Acquisition | ~$38,000 entry price [59] | Leverage core facility sharing; utilize vendor financing programs |
| Proprietary Consumables | High recurring cost; vendor lock-in [59] | Bulk purchase agreements; evaluate total cost per data point |
| Per-Sample Reagents | 2-3x more expensive than qPCR [59] | Implement reagent-saving protocols; optimize reaction volumes |
| Specialized Staff Training | Often overlooked in budgeting | Cross-train existing personnel; utilize vendor training resources |
| Maintenance Contracts | Annual recurring expense (10-15% of instrument cost) | Consider third-party service providers; self-maintenance if feasible |
The capital intensity required for ddPCR development and implementation is further highlighted by the fact that startups in this field often need to raise nine-figure venture rounds to cover the long research and development cycles needed to reach cost parity with established technologies [59]. This financial reality underscores why emerging-market budgets frequently prioritize multipurpose hematology or chemistry analyzers unless vendors introduce tiered pricing models or reagent-rental schemes that can make the technology more accessible across diverse economic settings [59].
Emerging Solutions and Future Directions
The limitations of current ddPCR systems have stimulated significant innovation aimed at addressing the challenges of sample input, throughput, and cost. Microfluidic technology plays a pivotal role in this evolution, enabling the development of integrated systems that consolidate droplet generation, thermal cycling, and signal detection into single, automated platforms [61]. This integration minimizes manual handling, reduces contamination risk, and improves overall workflow efficiency, potentially addressing both throughput and operational cost concerns.
Technological Innovations
Benchtop ddPCR systems represent one important direction in the evolution of this technology, offering decentralization of molecular testing capabilities that were previously confined to centralized reference laboratories. These compact platforms achieve impressive heating rates of 8°C/s and cooling rates of -9.3°C/s, supporting 40-cycle assay runs in under 35 minutes [59]. The accompanying workflow automation reduces sample preparation time from hours to minutes, enabling general hospitals and even outpatient clinics to operate sophisticated oncology or infection-control assays that once required specialized molecular facilities. Further simplification is achieved through artificial intelligence optimization that adjusts thermal profiles dynamically, eliminating manual parameter tuning and supporting reliable operation by novice users [59].
Microfluidic chip platforms are posting a remarkable 17.78% CAGR, advancing through the machining of microchambers directly into glass or polymer substrates [59]. This architectural approach eliminates the need for oil suspensions, reduces reagent volumes per reaction, and enables point-of-care cartridges that consolidate sample preparation, amplification, and readout within credit-card-sized cassettes. From an economic perspective, these microfluidic readers cost approximately 30% less than traditional droplet generators, making entry into digital PCR technology feasible for first-time purchasers in middle-income economies [59]. While droplet systems remain entrenched in high-volume oncology laboratories, microfluidics is attracting new users who prioritize portability, ease of use, and lower per-sample costs over maximum partition counts.
Multiplexing Strategies for Enhanced Efficiency
The development of sophisticated multiplexing strategies represents another promising approach to overcoming throughput and cost limitations in ddPCR. Traditional ddPCR methodologies have been restricted to detecting only two targets simultaneously in most instruments, leading to inefficient resource utilization, sample wastage, and labor-intensive procedures [62]. Recent advances have demonstrated the feasibility of higher-plex detection systems that substantially improve the information yield per reaction.
The implementation of 8-plex ddPCR for DNA methylation-based age prediction illustrates the power of advanced multiplexing. This system employs a novel strategy utilizing four distinct fluorophores (FAM, Cy5, ROX, and VIC) combined with different probe concentrations to distinguish targets based on varied fluorescence amplitudes [62]. This approach enables the simultaneous absolute quantification of four CpG sites within a single reaction, creating substantial efficiencies in terms of reagent consumption, technician time, and required sample input. The successful application of this 8-plex system, with its demonstrated mean absolute error of 4.59 years in age prediction, validates the practical utility of advanced multiplexing for complex analytical challenges [62].
Future developments in multiplexing are likely to focus on expanding the number of detectable targets while maintaining clear discrimination between different signals. This will require innovations in both fluorescence chemistry and signal detection algorithms. The combination of multiple fluorophores with varying probe concentrations and the development of novel statistical approaches for signal deconvolution will further enhance the multiplexing capabilities of ddPCR systems, making them increasingly efficient and cost-effective for complex analytical applications requiring detection of multiple rare mutations simultaneously.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of ddPCR for rare mutation detection requires careful selection and optimization of research reagents. The following table outlines essential materials and their specific functions in the experimental workflow, particularly focusing on the innovative 8-plex system discussed previously as a model for advanced ddPCR applications.
Table 4: Essential Research Reagents for Advanced ddPCR Applications
| Reagent Category | Specific Function | Application Notes |
|---|---|---|
| TaqMan Hydrolysis Probes | Sequence-specific detection with fluorescent signal release | 4-plex detection (FAM, Cy5, ROX, VIC) with varying concentrations for target discrimination [62] |
| Primer Sets | Target-specific amplification | Optimized primer:probe ratio (5:1 recommended) critical for multiplex assay performance [62] |
| Droplet Generation Oil | Creates stable water-in-oil emulsion | Requires specific surfactants to prevent droplet coalescence during thermal cycling [1] |
| SuperMix for Probes | Provides optimized buffer, nucleotides, and enzyme | Must maintain efficiency across multiple targets in multiplex reactions [60] |
| Microfluidic Array Plates | Solid substrate with predefined partitions | 20,480 partitions per sample in Absolute Q system; eliminates need for oil [59] |
| Bisulfite-Converted DNA | Preserves methylation status while converting unmethylated C to U | Recommended input: 10-50 ng for optimal performance in methylation assays [62] |
The selection and optimization of these reagents are particularly critical for complex multiplexed applications. In the development of the 8-plex ddPCR system for DNA methylation analysis, researchers conducted comprehensive linear regression analyses to determine optimal primer and probe ratios, tested diverse inputs of single CpG sites with distinct primers and probes, and validated various plex assay configurations [62]. This systematic approach to reagent optimization ensured stable DNA methylation values for four CpGs and consistent measurement precision across distinct multiplex systems. The resulting protocol demonstrated remarkable concordance with alternative technologies like SNaPshot while offering the advantages of absolute quantification without standard curves [62].
Droplet Digital PCR represents a powerful analytical tool for rare mutation detection with exceptional sensitivity and precision, yet practical implementation requires careful navigation of its limitations in sample input, throughput, and cost. The fundamental constraints imposed by Poisson statistics dictate specific sample input parameters that must be optimized for each application, while throughput limitations naturally position ddPCR as a preferred technology for low-to-medium throughput applications requiring high sensitivity rather than population-scale screening. The economic considerations of both capital investment and per-sample costs further shape the appropriate use cases for this technology.
Despite these limitations, ongoing technological innovations are progressively expanding the capabilities and accessibility of ddPCR. The development of integrated microfluidic systems, advanced multiplexing strategies, and decentralized benchtop platforms is actively addressing many current constraints. For researchers focused on rare mutation detection, particularly in applications like liquid biopsy for cancer monitoring, the exceptional sensitivity and absolute quantification capabilities of ddPCR often outweigh its limitations when appropriate experimental designs and strategic implementations are employed. As the technology continues to evolve toward greater automation, integration, and cost-effectiveness, ddPCR is poised to play an increasingly important role in both basic research and clinical applications requiring precise quantification of rare genetic targets.
ddPCR vs. qPCR and NGS: A Critical Comparative Analysis for Biomarker Detection
Droplet Digital PCR (ddPCR) represents a paradigm shift in nucleic acid quantification, offering transformative advantages for rare mutation detection in research and drug development. This technical guide delineates the core principles, experimental protocols, and quantitative data establishing ddPCR's superiority over real-time quantitative PCR (qPCR) in precision, sensitivity, and reproducibility. By partitioning samples into thousands of nanoliter-sized droplets, ddPCR achieves absolute quantification without standard curves and detects rare mutations below 0.1% allele frequency—a critical threshold for oncological research and minimal residual disease monitoring. This whitepaper provides researchers and drug development professionals with methodologies and data frameworks to implement ddPCR for demanding applications requiring the highest quantification accuracy and minimal variability.
Digital PCR (dPCR), the third generation of PCR technology after conventional PCR and quantitative PCR (qPCR), fundamentally redefines nucleic acid quantification [3] [1]. While qPCR provides relative quantification based on extrapolation from standard curves during the exponential amplification phase, ddPCR employs a digital approach based on endpoint measurement of partitioned reactions [63] [64]. This partition-based methodology enables absolute quantification by applying Poisson statistics to count discrete positive and negative reactions, eliminating reliance on external standards and inherent calibration inaccuracies [3] [65].
For rare mutation detection research—the core thesis context—this paradigm shift is particularly impactful. The ability to precisely quantify low-abundance targets within a wild-type background enables applications previously constrained by technological limitations, including cancer liquid biopsies, minimal residual disease monitoring, and asymmetric expression analysis [66] [37]. The following sections provide technical validation of ddPCR's superior performance characteristics through experimental data, methodological protocols, and comparative analyses.
Fundamental Principles and Quantification Methodology
Core Technological Differentiation
The fundamental distinction between qPCR and ddPCR lies in their quantification approaches. qPCR is an "analog" method that measures fluorescence intensity at each amplification cycle, with quantification based on the cycle threshold (Ct) value relative to a standard curve [63] [64]. This approach is inherently relative and susceptible to efficiency variations throughout the amplification process.
In contrast, ddPCR is a "digital" method that partitions each sample into approximately 20,000 nanoliter-sized droplets, with each droplet functioning as an individual PCR reactor [63]. Following endpoint amplification, droplets are classified as positive or negative based on fluorescence detection, enabling binary counting of target molecules rather than indirect fluorescence measurement [3] [65].
Absolute vs. Relative Quantification
The quantification methodologies underscore a critical distinction between the two technologies:
qPCR - Relative Quantification:
- Requires standard curves with known concentrations
- Measures cycle threshold (Ct) values relative to standards
- Expressed as relative fold-changes or extrapolated concentrations
- Subject to calibration variability and amplification efficiency artifacts [64]
ddPCR - Absolute Quantification:
- Requires no standard curves or reference samples
- Directly counts target molecules using Poisson distribution
- Provides absolute copy numbers per unit volume (e.g., copies/μL)
- Unaffected by amplification efficiency variations [63] [64]
This absolute quantification capability proves particularly valuable for rare mutation detection, where precise determination of mutant allele frequency is crucial for clinical decision-making in oncology [66] [37].
Experimental Data: Quantitative Performance Comparison
Sensitivity and Detection Limit Validation
Multiple studies have systematically compared the detection limits of ddPCR versus qPCR methodologies, with consistent findings demonstrating ddPCR's superior sensitivity for low-abundance targets.
Table 1: Comparative Detection Limits for EGFR T790M Mutation Detection
| Method | Detection Limit | Mutation Rate Detected | Copy Number Sensitivity | Reference |
|---|---|---|---|---|
| ARMS-qPCR | ~1% | 1-5% | 57-398 copies | [66] |
| ddPCR | <0.1% | 0.1-5% | 6-398 copies | [66] |
In a landmark 2015 study comparing amplification refractory mutation system-based qPCR (ARMS-qPCR) and ddPCR for EGFR T790M mutation detection, ddPCR demonstrated significantly enhanced sensitivity [66]. The ARMS-qPCR method reliably detected plasmid samples with 5% and 1% mutation rates, while ddPCR consistently identified mutations at 5%, 1%, 0.5%, and 0.1% mutation rates [66]. Critically, in clinical validation, ddPCR detected an EGFR T790M mutation with just seven copies of mutant alleles in a background of 6,000 wild-type copies in a sample previously classified as wild-type by ARMS-qPCR [66].
Precision and Reproducibility Metrics
The partitioning approach of ddPCR provides superior precision and reduced variability compared to qPCR, particularly for low-abundance targets where quantification precision is most challenging.
Table 2: Precision and Variability Comparison
| Performance Parameter | qPCR Performance | ddPCR Performance | Application Impact |
|---|---|---|---|
| Detection Precision | 2-fold differences | <30% differences [63] | Enhanced measurement of small expression changes |
| Rare Allele Detection | ~1% [65] | ≤0.1% [63] [65] | Early detection of treatment resistance mutations |
| Copy Number Variation | Multi-copy differences | Single-copy resolution [63] | Precise genotyping and haplotype analysis |
| Inhibitor Tolerance | Highly susceptible | High tolerance [65] [67] | Reliable results with challenging samples (e.g., FFPE, soil) |
The precision advantage stems from ddPCR's digital counting nature and statistical power from thousands of replicate reactions per sample. This provides superior reproducibility across laboratories and operators, a critical consideration for multi-center clinical trials and regulatory submissions [65].
Methodological Implementation: Experimental Protocols
Core ddPCR Workflow for Rare Mutation Detection
The standard ddPCR protocol for rare mutation detection involves several critical steps that differ significantly from qPCR approaches:
Step 1: Assay Design and Validation
- Design primers and TaqMan probes targeting mutation and wild-type sequences
- Validate specificity using control samples with known mutation status
- Optimize annealing temperatures through gradient PCR [37]
Step 2: Reaction Mixture Preparation
- Prepare 20-25μL reaction volumes containing:
Step 3: Droplet Generation
- Load reaction mixture into droplet generator cartridge
- Add 70μL of droplet generation oil
- Process through microfluidic droplet generator
- Typically generate ~20,000 droplets per sample [66] [63]
Step 4: PCR Amplification
- Transfer droplets to 96-well PCR plate and seal
- Amplify using optimized thermal cycling conditions:
Step 5: Droplet Reading and Analysis
- Load PCR plate into droplet reader
- Measure fluorescence in each droplet (FAM and HEX/VIC channels)
- Analyze using Poisson statistics to calculate absolute copy numbers
- Calculate mutant allele frequency as: [mutant copies/(mutant + wild-type copies)] × 100% [3] [65]
Optimization Strategies for Challenging Targets
Successful implementation for rare mutation detection often requires target-specific optimization:
Thermal Cycling Optimization:
- For GC-rich targets: Increase denaturation temperature to 96-98°C
- For complex secondary structures: Incorporate longer denaturation times or temperature gradients
- For specific applications like PICALM::MLLT10 fusion detection: Lower annealing temperatures (58°C) may improve PCR efficiency and cluster separation [37]
Assay Design Considerations:
- Amplicon size ideally <200bp for degraded samples (e.g., FFPE, cfDNA)
- Position mutation site centrally within amplicon for optimal probe binding
- For highly homologous sequences: Consider restriction enzyme digestion pre-treatment to improve specificity [37]
Troubleshooting Suboptimal Partitions:
- "Rain" (intermediate fluorescence droplets): Optimize annealing temperature, improve probe design, or adjust template quality
- Poor cluster separation: Validate probe specificity, optimize probe concentration, or implement touchdown thermal protocols [37]
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for ddPCR
| Category | Specific Product/Platform | Function/Application | Technical Considerations |
|---|---|---|---|
| ddPCR Systems | Bio-Rad QX200 Droplet Digital PCR System | Rare mutation detection, copy number variation | Water-in-oil droplet technology; 20,000 droplets/sample [66] [67] |
| QIAcuity (Qiagen) | High-throughput nanoplated dPCR | Integrated partitioning, thermocycling, imaging; <2 hour workflow [65] | |
| QuantStudio Absolute Q (Thermo Fisher) | Automated digital PCR | Microfluidic array plates; 20,480 partitions/sample [1] | |
| Core Reagents | ddPCR Supermix | Reaction foundation | Contains DNA polymerase, dNTPs, optimized buffers [66] |
| TaqMan Probe/Primer Sets | Target-specific detection | FAM-labeled for mutant; HEX/VIC-labeled for wild-type [37] | |
| Droplet Generation Oil | Partition stabilization | Creates stable water-in-oil emulsions during thermal cycling [66] | |
| Sample Prep Kits | QIAamp DNA FFPE Tissue Kit | Extraction from challenging samples | Optimized for cross-linked, fragmented DNA [66] |
| Circulating Nucleic Acid Kit | Cell-free DNA extraction | High-sensitivity recovery for liquid biopsy applications |
Application Scope: Advancing Rare Mutation Research
The superior quantification capabilities of ddPCR have enabled breakthroughs across multiple research domains:
Oncology and Liquid Biopsy:
- EGFR T790M resistance mutation detection in non-small cell lung cancer [66]
- Minimal residual disease monitoring via rare fusion transcripts in hematological malignancies [37]
- Tumor heterogeneity analysis through low-frequency mutation detection
Infectious Disease Monitoring:
- HIV reservoir quantification with precision unattainable by qPCR [67]
- Viral load monitoring for treatment response assessment
- Antibiotic resistance gene detection in bacterial pathogens [3]
Environmental and Conservation Genetics:
- Species detection from soil environmental DNA (eDNA) with 86.84% success rate [68]
- Cryptic species identification for biodiversity assessment
- Non-invasive monitoring of endangered terrestrial vertebrates [68]
Droplet Digital PCR represents a significant technological advancement over qPCR, providing researchers and drug development professionals with unparalleled quantification accuracy, sensitivity for rare targets, and experimental reproducibility. The absolute quantification capability without standard curves, coupled with detection sensitivity below 0.1% mutant allele frequency, positions ddPCR as the emerging gold standard for applications requiring precise nucleic acid measurement. As the technology continues to evolve with increased automation and throughput, its implementation will undoubtedly expand, driving discoveries in rare mutation research and transforming our approach to molecular quantification across diverse scientific disciplines.
Next-generation sequencing (NGS) and droplet digital PCR (ddPCR) represent two pillars of modern molecular diagnostics and life sciences research. While NGS offers an unbiased, high-throughput platform for the discovery of novel genetic variants, ddPCR provides an exceptionally precise and sensitive method for validating and absolutely quantifying those findings [69]. This guide details the technical framework for leveraging these technologies in concert, with a specific focus on detecting rare somatic mutations—a critical application in cancer research, therapy monitoring, and drug development. The synergy between NGS's broad discovery power and ddPCR's focused validation capabilities creates a robust workflow for generating high-confidence data, ultimately accelerating scientific discovery and clinical assay development.
Understanding the core principles and performance characteristics of each technology is fundamental to deploying them effectively.
Next-Generation Sequencing (NGS)
NGS is a massively parallel sequencing technology that enables the comprehensive analysis of entire genomes, exomes, or targeted gene panels. It works by fragmenting DNA samples, attaching adapters, and simultaneously sequencing millions of these fragments. The resulting data allows for the identification of known and novel genetic variants, including single nucleotide variants (SNVs), insertions/deletions (indels), and copy number variations (CNVs). Its primary strength in the discovery phase is its ability to screen a vast genetic landscape without prior knowledge of specific mutations.
Droplet Digital PCR (ddPCR)
The ddPCR technology partitions a single PCR reaction into thousands to millions of nanoliter-sized water-in-oil droplets, effectively creating a massive array of individual PCR reactions [69]. After endpoint PCR amplification, each droplet is analyzed for fluorescence. The fraction of positive droplets is then used to calculate the absolute concentration of the target nucleic acid sequence in the original sample using Poisson statistics [69]. This partitioning makes ddPCR highly resistant to PCR inhibitors and reduces template competition, allowing for the precise detection and quantification of rare target sequences in a wild-type background with a sensitivity that can reach a variant allele frequency of 0.001% [69].
Table 1: Key Performance Characteristics of NGS and ddPCR
| Feature | Next-Generation Sequencing (NGS) | Droplet Digital PCR (ddPCR) |
|---|---|---|
| Primary Role | Discovery, Hypothesis Generation | Validation, Absolute Quantification |
| Throughput | High (Multiple samples/genes in parallel) | Medium (Typically 1-4 targets per reaction) |
| Sensitivity | ~1-5% Variant Allele Frequency (VAF) | ~0.001-0.01% VAF [69] |
| Quantification | Relative (Requires standard curves/bioinformatics) | Absolute (No need for calibrators) [69] |
| Precision | Moderate | High |
| Key Advantage | Unbiased detection of novel variants | Ultra-sensitive quantification of known variants |
The Integrated Workflow: From Discovery to Validation
The complementary relationship between NGS and ddPCR is best exemplified in a structured workflow that moves from broad screening to focused, high-confidence validation. This pipeline is essential for applications like rare mutation detection in cancer.
Figure 1: Integrated NGS-ddPCR Workflow. The process flows from discovery using NGS to targeted validation using ddPCR.
Phase 1: Discovery with NGS
The process begins with NGS analysis of patient samples (e.g., tumor biopsies) to identify potential driver mutations. This is typically performed using targeted panels, whole exome, or whole genome sequencing. Bioinformatic pipelines are then used to align sequences to a reference genome and call variants. The output is a list of candidate somatic mutations with a variant allele frequency (VAF) typically above 1-5%.
Phase 2: Validation with ddPCR
Specific mutations of interest identified by NGS are then transitioned to a ddPCR validation phase. For each candidate mutation, a specific probe-based ddPCR assay is designed. These assays are used to interrogate the original and/or longitudinal samples (e.g., during therapy or for minimal residual disease monitoring). ddPCR's superior sensitivity and absolute quantification confirm the presence of the mutation and provide precise data on its abundance, even at levels far below the detection limit of NGS [69] [70].
Quantitative Comparison of Detection Sensitivity
A direct comparison of technologies highlights the critical advantage of ddPCR in detecting low-frequency variants, which is paramount for monitoring disease burden and treatment response.
Table 2: Detection of BRAF V600E Mutation in Papillary Thyroid Carcinoma (PTC)
| Detection Method | Number of Positive Samples | Positive Rate | Reported Sensitivity (LoD) | Notes |
|---|---|---|---|---|
| Sanger Sequencing | 67 / 150 | 44.67% | ~7-20% Mutant Alleles [70] | Failed to detect mutations in samples with VAF ≤5% [70] |
| Droplet Digital PCR | 92 / 150 | 61.33% | 0.0005% [70] | Detected 25 additional positive cases missed by Sanger; mutant allele frequency ranged from 0.28% to 45.40% [70] |
The data in Table 2 underscores a key finding: ddPCR significantly outperforms traditional sequencing methods in detecting low-abundance mutations. In this study, all 25 samples where the two methods disagreed had a mutant allele frequency of 5% or lower, firmly within ddPCR's range of reliable detection but below the sensitivity threshold of Sanger sequencing [70]. This capability is directly transferable to validating NGS findings that hover near its limit of detection.
Application in Hematologic Malignancies and MRD Monitoring
The NGS-ddPCR synergy is powerfully demonstrated in the management of hematologic cancers, particularly for monitoring minimal residual disease (MRD)—the small number of cancer cells that persist after treatment and can lead to relapse.
ddPCR has proven particularly useful for the accurate detection and quantification of low-abundance nucleic acids, highlighting its advantages in cancer diagnosis and in predicting recurrence and monitoring minimal residual disease [69]. For instance, in Acute Myeloid Leukemia (AML), ddPCR has been used to track mutation-specific markers (e.g., in DNMT3A, TET2, ASXL1, RUNX1, and IDH1/2) with a sensitivity that allows the detection of as few as 1 malignant cell in 15,000 normal cells (0.0067%) [69]. This enables clinicians to detect molecular relapse long before it becomes clinically apparent.
Furthermore, in Philadelphia-negative chronic Myeloproliferative Neoplasms (MPNs), ddPCR provides a highly precise method for quantifying the allelic burden of driver mutations like JAK2V617F and various CALR mutations, with assays reliably achieving a sensitivity of 0.01% to 0.02% [69]. This allows for highly accurate assessment of tumor burden and response to therapy.
Essential Protocols and Reagents
Implementing this integrated approach requires robust experimental protocols and carefully selected reagents.
Protocol: ddPCR Assay for Mutation Validation
This protocol outlines the key steps for validating an NGS-identified mutation using a probe-based ddPCR assay.
1. Assay Design:
- Design primers and two TaqMan probes (one wild-type-specific, one mutation-specific).
- The probes must be labeled with different fluorescent dyes (e.g., FAM for mutant, HEX/VIC for wild-type).
- Verify assay specificity in silico.
2. Reaction Setup:
- Prepare a 20 μL reaction mix containing:
- 1× ddPCR Supermix (no dUTP).
- Forward and Reverse Primers (e.g., 0.5 μmol/L each).
- Wild-type and Mutation-specific Probes (e.g., 0.25 μmol/L each).
- Template DNA (e.g., 20 ng).
- Gently mix and avoid introducing bubbles [70].
3. Droplet Generation:
- Load the reaction mix into a droplet generator.
- This partitions the sample into ~20,000 nanoliter-sized droplets.
- Carefully transfer the generated droplets to a 96-well PCR plate and seal it.
4. PCR Amplification:
- Perform endpoint PCR on a thermal cycler using optimized conditions. An example profile:
- Hold: 95°C for 10 minutes (1 cycle).
- Amplify: 94°C for 30 seconds and 55-60°C for 1 minute (40 cycles).
- Enzyme Deactivation: 98°C for 10 minutes (1 cycle).
- Hold: 4°C ∞.
5. Droplet Reading and Analysis:
- Load the plate into a droplet reader.
- The reader counts the number of positive and negative droplets for each fluorescence channel.
- Use the instrument's software (e.g., QuantaSoft) to analyze the data and calculate the absolute concentration of mutant and wild-type alleles in copies/μL using Poisson statistics.
Figure 2: ddPCR Workflow. Key steps from sample partitioning to absolute quantification.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for ddPCR-based Validation
| Item | Function | Example/Note |
|---|---|---|
| ddPCR Supermix | Provides optimized buffer, dNTPs, and polymerase for the PCR reaction. | Select a supermix without dUTP if using UDG carryover prevention is not required [70]. |
| Sequence-Specific Primers | Amplifies the genomic region containing the mutation of interest. | Must be designed for high amplification efficiency. |
| Fluorescent Probes (FAM/HEX) | Specifically binds to and reports the presence of wild-type or mutant alleles. | Two differentially labeled probes are needed for a single-plex assay. |
| DNA Template | The sample containing the nucleic acid target to be quantified. | Can be derived from various sources (e.g., FFPE tissue, blood). |
| Droplet Generation Oil | Creates the water-in-oil emulsion necessary for partitioning the sample. | Specific to the ddPCR system being used (e.g., Bio-Rad QX200). |
| Droplet Generator & Reader | Instrumentation for creating droplets and analyzing fluorescence post-PCR. | Essential hardware (e.g., Bio-Rad QX200 system). |
NGS and ddPCR are not competing technologies but rather complementary forces in the molecular toolkit. NGS provides the wide-angle lens for discovery, uncovering the complex genetic landscape of diseases like cancer. ddPCR then acts as the telephoto lens, allowing researchers and clinicians to zoom in with immense precision on specific, clinically relevant mutations for validation and longitudinal monitoring. This synergy is indispensable for advancing rare mutation detection research, enabling robust biomarker validation, accurate MRD assessment, and ultimately, the development of more effective, personalized therapeutic strategies. By adopting this integrated workflow, scientists can maximize data confidence and translational impact.
The accurate detection of rare mutant alleles隐藏在 a background of abundant wild-type DNA represents one of the most significant challenges in molecular diagnostics and clinical research. The ability to identify mutations present at frequencies of 0.1% or lower has profound implications for cancer management, treatment monitoring, and early disease detection. Digital PCR (dPCR), particularly droplet digital PCR (ddPCR), has emerged as a leading technology in this arena, enabling researchers to achieve unprecedented sensitivity in quantifying rare mutations. This technical guide explores the methodologies, experimental protocols, and analytical frameworks that make such sensitive detection possible, with particular focus on applications in liquid biopsy analysis and cancer research where monitoring rare mutations can directly impact patient outcomes [39].
The clinical importance of this capability is exemplified in scenarios such as monitoring EGFR T790M mutations in non-small cell lung cancer (NSCLC) patients. This mutation, which often emerges during treatment with tyrosine kinase inhibitors, confers therapeutic resistance and is rarely detected during initial tumor characterization. Early detection of its appearance is therefore critical for directing patients toward more effective treatments [4]. Similarly, the detection of circulating tumor DNA (ctDNA) in liquid biopsies requires exceptional sensitivity, as these fragments are typically short and exist in very low concentrations amidst a background of normal cell-free DNA [39].
Digital PCR achieves its exceptional sensitivity through a fundamental methodological shift from conventional quantitative PCR. Rather than relying on amplification curves and standard curves for quantification, dPCR partitions sample DNA into thousands to millions of individual reactions, effectively "enriching" low-level targets by reducing background interference [39]. This partitioning allows for binary endpoint detection (positive or negative) for each partition, followed by Poisson statistical analysis to determine absolute target concentration without the need for standard curves [39] [71].
The statistical power of dPCR stems from the law of large numbers—as partition count increases, so does the probability of detecting rare events. With partition numbers reaching 20,000-50,000 in modern systems, the technology can reliably detect mutant allele frequencies (MAFs) as low as 0.1% with 95% confidence [39] [4] [72]. This represents a significant advancement over traditional qPCR, which typically achieves sensitivity in the 1-5% range. The elimination of standard curves not only improves accuracy but also enhances reproducibility across experiments and laboratories [39].
Table 1: Key Advantages of Digital PCR for Rare Mutation Detection
| Feature | Advantage | Impact on Rare Mutation Detection |
|---|---|---|
| Sample Partitioning | Effectively enriches low-abundance targets | Enables detection of rare sequences against wild-type background |
| Absolute Quantification | No standard curves required | Improves accuracy and reproducibility of measurements |
| High Partition Count | Provides robust statistical power | Allows detection of mutant allele frequencies as low as 0.1% |
| Multiplexing Capability | Simultaneous detection of mutant and wild-type alleles | Enables direct calculation of variant allele frequency |
| Resistance to Inhibitors | Individual reactions are less affected by PCR inhibitors | Maintains sensitivity in challenging samples like FFPE and cfDNA |
Experimental Design and Workflow for Rare Mutation Detection
Core Principles of Assay Design
Successful detection of rare mutations begins with careful assay design. For optimal performance, researchers typically employ dual-probe hydrolysis assays (TaqMan-style) with a single set of primers amplifying the region of interest, plus two differently labeled probes—one targeting the wild-type sequence and another targeting the mutant allele [4]. This approach requires careful selection of fluorophores with compatible excitation and emission spectra that match the detection capabilities of the dPCR system being used [4].
The placement of probes and primers follows similar rules to qPCR, with particular attention to ensuring that the mutant-specific probe binds exclusively to the mutant sequence. The wild-type probe should be designed to compete effectively for binding to ensure accurate discrimination between populations. This design strategy creates the foundation for the distinct clustering patterns observed in two-dimensional ddPCR scatter plots, where droplets segregate into FAM-positive, HEX-positive, double-positive, and double-negative populations [71].
Critical Sample Preparation Considerations
The sensitivity of any rare mutation detection assay is fundamentally limited by input DNA quality and quantity. For human genomic DNA applications, the following calculation determines the theoretical detection limit:
Number of copies in reaction volume = mass of DNA in reaction volume (in ng)/0.003 [4]
This calculation is based on the approximate mass of 3 pg per haploid human genome. The theoretical limit of detection can then be calculated by dividing the system's theoretical LOD (e.g., 0.2 copies/μL for some systems) by the final concentration of target copies in the reaction [4]. For example, with 10ng of human genomic DNA in a 25μL reaction, the total EGFR copies would be approximately 3,333, with a final concentration of 133 copies/μL. The theoretical sensitivity would therefore be 0.2/133 = 0.15% with 95% confidence [4].
When working with cell-free DNA from liquid biopsies, specialized extraction methods are required to maximize yield while minimizing genomic DNA contamination. Technologies such as the MagBind cfDNA Kit have demonstrated extraction efficiencies of 60-70%, significantly higher than the 30% efficiency of some alternative methods [72]. The quality of extracted cfDNA can be verified using tools like the Agilent 4150 TapeStation system with Cell-Free DNA ScreenTape Assays, which should show prominent bands between 150-200 base pairs, indicating high-quality cfDNA suitable for rare mutation detection [72].
Diagram 1: Comprehensive ddPCR Workflow for Rare Mutation Detection
Detailed Experimental Protocol: EGFR T790M Case Study
Reagent Preparation and PCR Mix Formulation
The following protocol, optimized for detection of the EGFR T790M mutation, illustrates a robust approach to rare mutation detection. This example utilizes the Naica System and Sapphire chip, though principles apply across platforms [4].
Table 2: PCR Mix Formulation for EGFR T790M Detection
| Reagent | Final Concentration | Function |
|---|---|---|
| PCR Mastermix (2X or 5X) | 1X | Provides essential components for amplification |
| Reference Dye | Per manufacturer instructions | Internal control for partition quality |
| EGFR T790 Reverse & Forward Primers | 500 nM each | Amplify target region containing mutation |
| EGFR T790WT Probe | 250 nM | Detects wild-type allele sequence |
| EGFR T790M Probe | 250 nM | Detects mutant allele sequence |
| Human Genomic DNA | Calculated based on sensitivity requirements | Template for amplification |
| Nuclease-Free Water | Volume to achieve 25μL final reaction | Diluent and volume adjustment |
When preparing the PCR mix, it is crucial to account for pipetting errors by preparing a master mix for n+1 samples (e.g., for 7 samples, prepare for 8). All components should be thoroughly homogenized before loading into partitioning consumables. Proper controls must be included: a non-template control (NTC) containing all components except DNA, plus monocolor controls for each probe to facilitate fluorescence spillover compensation during analysis [4].
Thermal Cycling Conditions and Data Acquisition
The EGFR T790M assay described here was optimized using the QuantaBio PerfeCTa Multiplex mastermix with the following thermal cycling program [4]:
Table 3: Thermal Cycling Conditions for EGFR T790M Assay
| Cycles | Temperature | Time | Purpose |
|---|---|---|---|
| 1 | 95°C | 10 minutes | Initial denaturation and enzyme activation |
| 45 | 95°C | 30 seconds | Denaturation |
| 45 | 62°C | 15 seconds | Primer annealing and extension |
Following amplification, data acquisition methods vary by platform. Some systems capture images of the entire chip (Naica System, QuantStudio 3D Digital PCR System), while others read partitions sequentially in a process similar to flow cytometry (QX200 Droplet Digital PCR System, Raindrop Digital PCR System) [4]. In all cases, manufacturer protocols should be followed precisely to ensure optimal data quality.
Data Analysis and Interpretation Framework
Cluster Identification and Quality Control
ddPCR data is typically visualized as two-dimensional scatter plots where fluorescence amplitudes for both channels are plotted against each other for every droplet [71]. In ideal experiments with two templates, droplets segregate into four distinct populations: HEX-positive, FAM-positive, double-positive, and double-negative clusters [71]. In practice, however, some droplets exhibit intermediate fluorescence signals and fall between distinct populations—a phenomenon termed "rain"—which must be properly accounted for during analysis [71].
Two critical quality control parameters should be assessed before proceeding with analysis:
- Non-Template Control (NTC): Should display only negative partitions, with few or no positive signals indicating contamination or non-specific amplification [4]
- Partition Count: Since rare mutation detection benefits from higher partition numbers, experiments should achieve between 19,000-22,000 analyzable partitions (or as recommended for the specific system) to ensure statistical confidence in results [4]
Analysis Algorithms and Software Solutions
The assignment of droplets to specific clusters can be performed through manual gating, proprietary automated algorithms (such as those in QuantaSoft), or open-source solutions like the ddpcr R package [71]. This package uses kernel density estimation and Gaussian mixture models applied to droplet fluorescence amplitudes to automatically gate droplets into appropriate clusters while accounting for rain [71]. The algorithm follows several key steps:
- Identify and exclude wells with failed ddPCR reactions
- Identify and exclude outlier droplets with aberrant fluorescence signals
- Identify and exclude empty droplets lacking DNA template
- Assign droplets to clusters through automated gating
- Calculate starting template concentration using Poisson statistics [71]
Diagram 2: Data Analysis Workflow for Rare Mutation Detection
Experimental Validation and Concordance Analysis
In validation studies, researchers have demonstrated excellent concordance between expected and observed mutant allele frequencies using ddPCR. For example, in experiments detecting NRAS and EGFR mutations at varying allelic frequencies, the following results were obtained [72]:
Table 4: Experimental Validation of Rare Mutation Detection by ddPCR
| Target Gene | Expected MAF | Observed MAF | Concordance |
|---|---|---|---|
| NRAS | 0% (Wildtype) | 0% | Perfect |
| NRAS | 0.1% | 0.17% | Excellent |
| NRAS | 1% | 1.5% | Excellent |
| NRAS | 5% | 7.6% | Good |
| EGFR | 0% (Wildtype) | 0% | Perfect |
| EGFR | 0.1% | 0.17% | Excellent |
| EGFR | 1% | 1.12% | Excellent |
| EGFR | 5% | 4.66% | Excellent |
These results demonstrate that ddPCR consistently detects mutant alleles at frequencies as low as 0.1% with high accuracy, confirming its utility for rare mutation detection in clinical research settings [72].
Essential Research Reagent Solutions
Successful rare mutation detection requires careful selection of reagents and consumables optimized for digital PCR applications. The following table summarizes key components and their functions:
Table 5: Essential Research Reagents for Rare Mutation Detection by ddPCR
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Digital PCR Systems | QuantStudio Absolute Q, Naica, QX200 | Platform for partitioning and amplification |
| Specialized Master Mixes | ddPCR Supermix for Probes, PerfeCTa Multiplex | Optimized for partition-based amplification |
| Hydrolysis Probes | TaqMan, Absolute Q Liquid Biopsy Assays | Sequence-specific detection with fluorophores |
| Nucleic Acid Extraction Kits | MagBind cfDNA Kit | High-efficiency recovery of target DNA |
| Reference Dyes | Instrument-specific compounds | Internal controls for partition quality |
| Partitioning Consumables | Chips, cartridges, droplet generators | Create isolated reaction environments |
The detection of mutant allele frequencies as low as 0.1% represents a significant advancement in molecular diagnostics, enabled by the precision, sensitivity, and accuracy of digital PCR technologies. As demonstrated through the EGFR T790M case study and validation data, properly optimized ddPCR workflows can reliably quantify rare mutations that have profound clinical implications for cancer management and treatment monitoring. The continued refinement of assay designs, extraction methods, and analysis algorithms promises to further enhance the sensitivity and reproducibility of rare mutation detection, solidifying ddPCR's role as an indispensable tool in clinical research and personalized medicine.
Digital PCR (dPCR), and specifically droplet digital PCR (ddPCR), has emerged as a powerful third-generation PCR technology for the absolute quantification of nucleic acids. Its unique capability to detect rare genetic mutations down to 0.1% allele frequency or lower makes it indispensable in oncology, liquid biopsy applications, prenatal diagnosis, and pathogen identification [1] [4]. Unlike quantitative real-time PCR (qPCR), dPCR partitions a sample into thousands of individual reactions, allowing for the detection and absolute quantification of target sequences without the need for a standard curve [2]. This calibration-free technology offers superior sensitivity, accuracy, and reproducibility, making it particularly suitable for identifying rare somatic mutations in a background of wild-type sequences, monitoring minimal residual disease, and analyzing tumor heterogeneity [1] [5].
However, the successful implementation of a ddPCR workflow for rare mutation detection requires careful consideration of multiple interconnected parameters. Assay sensitivity, which determines the lowest mutant allele frequency detectable, is directly influenced by factors such as total DNA input, partition count, and assay design [4]. Suboptimal choices at any stage can compromise data quality, leading to false negatives or inaccurate quantification. This guide provides a systematic decision framework to help researchers navigate these critical choices, ensuring that their experimental design is robustly aligned with their specific research goals in rare mutation detection.
Core Principles of ddPCR for Rare Mutation Detection
Statistical Foundation for Absolute Quantification
The absolute quantification capability of dPCR hinges on its statistical foundation. The technique involves partitioning a PCR mixture into a large number of nano-liter or pico-liter volume reactions, so that each partition contains either 0, 1, or a few target molecules according to a Poisson distribution [1] [2]. Following end-point PCR amplification, the fraction of positive partitions (those containing the amplified target) is used to calculate the absolute concentration of the target nucleic acid in the original sample using Poisson statistics [1].
The precision of this quantification is intrinsically linked to the number of partitions analyzed. The confidence in estimating target concentration is highest when approximately 20% of partitions are empty, which corresponds to a Poisson distribution parameter (λ) of about 1.6 [2]. This statistical relationship means that increasing the number of partitions directly enhances the sensitivity of rare allele detection, allowing for the reliable identification of mutant alleles present at frequencies below 1% in a wild-type background [2].
Key Advantages Over qPCR
- Absolute Quantification Without Standards: dPCR provides direct nucleic acid counting without requiring standard curves, eliminating concerns about differential amplification efficiencies between standards and samples [2].
- Enhanced Sensitivity for Rare Variants: Sample partitioning effectively concentrates rare targets within isolated microreactors, reducing template competition and enabling detection of rare mutations in a background of wild-type sequences [2] [5].
- Superior Tolerance to Inhibitors: The partitioning process dilutes PCR inhibitors across thousands of reactions, making dPCR more resilient to substances that would typically inhibit conventional PCR [2].
- Precise Quantification at Low Concentrations: dPCR excels at accurately quantifying target sequences present at very low copy numbers, where qPCR typically shows high variability [2].
Decision Framework: Critical Experimental Parameters
DNA Input and Theoretical Sensitivity
The relationship between DNA input, partition count, and theoretical detection sensitivity is fundamental to experimental design. The required DNA input depends directly on the desired sensitivity for detecting rare mutations.
Table 1: Relationship Between DNA Input, Partition Number, and Theoretical Detection Limit
| Target Sensitivity | Required DNA Mass (Human gDNA) | Approximate DNA Copies | Minimum Partitions |
|---|---|---|---|
| 1% Mutant Allele Frequency | 3.3 ng | ~1,000 copies | 20,000 |
| 0.1% Mutant Allele Frequency | 33 ng | ~10,000 copies | 20,000 |
| 0.01% Mutant Allele Frequency | 330 ng | ~100,000 copies | 100,000 |
The calculation for determining the theoretical limit of detection (LOD) follows this formula [4]:
Where P is the desired confidence level (typically 0.95 for 95% confidence) and V is the partition volume. The sensitivity for rare mutation detection can be calculated as [4]:
For example, with 10 ng of human genomic DNA input and a system LOD of 0.2 copies/μL, the theoretical sensitivity would be approximately 0.15% for a haploid target [4].
Assay Design Strategy Selection
The choice of assay design depends on the mutation type and the need for multiplexing or mutation scanning capabilities.
Table 2: ddPCR Assay Design Strategies for Rare Mutation Detection
| Assay Type | Principle | Best For | Limitations |
|---|---|---|---|
| Hydrolysis Probes (TaqMan) | Two probes with different fluorophores target wild-type and mutant alleles [4] | Known point mutations at predetermined positions | Requires prior knowledge of exact mutation; specific probe needed for each mutation |
| COLD-ddPCR | COLD-PCR enriches mutations; two wild-type probes detect ratio changes [5] | Scanning for unknown mutations in a ~50bp region | Requires optimization of critical temperature; limited to specific amplicon regions |
| SuperSelective Primers | Special primers with long anchor and short foot sequences for selectivity [73] | Validating rare SNVs identified by NGS; cost-sensitive applications | Requires extensive optimization and validation; complex design process |
Platform and Partitioning Technology
The choice between droplet-based and microchamber-based dPCR systems involves trade-offs between partition density, cost, and workflow convenience.
Table 3: Comparison of ddPCR Partitioning Technologies
| Parameter | Droplet-based ddPCR | Microchamber-based dPCR |
|---|---|---|
| Number of Partitions | 20,000-100,000+ | 5,000-30,000 |
| Partition Volume | Picoliter to nanoliter scale | Typically larger volumes (nanoliter) |
| Scalability | High | Limited by fixed chip design |
| Cost per Reaction | Generally lower | Generally higher |
| Ease of Automation | Moderate | High |
| Reproducibility | Requires precise emulsification | High, with fixed chambers |
Decision Framework for ddPCR Experimental Design
Detailed Experimental Protocols
Hydrolysis Probe Protocol for Known Mutations (e.g., EGFR T790M)
This protocol is adapted from established methods for detecting the EGFR T790M mutation in non-small cell lung cancer [4].
PCR Mix Preparation (25 μL total volume):
- Mastermix: 1X concentration (check manufacturer's recommendation)
- Primers: 500 nM each forward and reverse primer
- Probes: 250 nM each for wild-type and mutant-specific probes
- DNA Input: 10-100 ng human genomic DNA (depending on required sensitivity)
- Reference Dye: If required by platform
- Nuclease-free water: To volume
Essential Controls:
- Non-Template Control (NTC): All components except DNA template
- Wild-type Control: Only wild-type DNA with both probes
- Mutant Control: Mutant DNA with both probes (if available)
- Monocolor controls for fluorescence compensation if required by platform
Thermal Cycling Conditions:
- Initial Denaturation: 95°C for 10 minutes
- 45 Cycles:
- Denaturation: 95°C for 30 seconds
- Annealing/Extension: 62°C for 15 seconds
- Final Hold: 4-12°C indefinitely
Data Analysis:
- Apply fluorescence compensation if necessary to correct for spectral overlap
- Set thresholds to distinguish positive and negative partitions
- Calculate mutant allele frequency using the formula:
COLD-ddPCR Protocol for Mutation Scanning
This protocol enables detection of unknown mutations within approximately 50bp of a target amplicon [5].
Workflow:
- Design Two Wild-type Probes: Labeled with different fluorophores (e.g., FAM and HEX) targeting adjacent regions of the wild-type sequence
- Incorporate COLD-PCR: Implement modified thermal cycling conditions that enrich mutation-containing sequences by exploiting the reduced denaturation temperature of heteroduplexes
- Analyze Fluorescence Ratios: The ratio of FAM/HEX-positive droplets remains constant for wild-type amplicons but deviates when mutations are present under either probe
Key Considerations:
- Requires optimization of the critical temperature (Tc) for the specific amplicon
- Validated for detection of multiple mutations in TP53 and EGFR with sensitivity down to 0.2-1.2% mutation abundance [5]
- Enables detection of mutations without prior knowledge of the exact nucleotide change
SP-ddPCR with SuperSelective Primers
This approach combines SuperSelective primers with ddPCR for quantifying rare single nucleotide variants (SNVs) [73].
Primer Design:
- 5' Anchor: ~20 nucleotides complementary to the target sequence
- 3' Foot: 4-6 nucleotides containing the interrogated mutant nucleotide at the 3' end
- Bridge: Non-complementary sequence that forms a single-stranded bubble
Validation Steps:
- Test primer selectivity using control templates with 100% and 0% variant allele frequency (VAF)
- Establish limit of detection (LOD) using serial dilutions of mutant in wild-type background
- Calculate LOD as the average signal plus three standard deviations of measurements at 0% VAF
- Average LOD across assays is approximately 0.18% [73]
Advantages:
- Requires only one fluorescent channel
- Cost-effective compared to dual-probe approaches
- Suitable for validating SNVs identified by next-generation sequencing
Research Reagent Solutions
Table 4: Essential Reagents for ddPCR Rare Mutation Detection
| Reagent/Category | Function | Key Considerations |
|---|---|---|
| Digital PCR Mastermix | Provides DNA polymerase, dNTPs, buffer, MgCl₂ | Use manufacturer-recommended formulations; some are optimized for multiplexing |
| Hydrolysis Probes (TaqMan) | Sequence-specific detection of wild-type and mutant alleles | Fluorophores must be compatible with detection system (e.g., FAM, HEX/VIC, Cy5) |
| SuperSelective Primers | Selective amplification of mutant alleles over wild-type | Complex design with anchor, bridge, and foot regions; requires extensive validation |
| Reference Dye | Normalization for partition volume variation | Required for some platforms (e.g., ROX) |
| Partitioning Oil/Stabilizer | Creates stable emulsion for droplet-based systems | Prevents droplet coalescence during thermal cycling |
| Positive Control Templates | Assay validation and quality control | Synthetic oligonucleotides or characterized genomic DNA with known mutations |
Advanced Applications and Future Directions
The application of ddPCR for rare mutation detection continues to evolve with emerging methodologies. Recent advances include the integration of artificial intelligence for automated droplet classification, with one study reporting 99.05% accuracy in processing complex ddPCR images containing over 300 droplets per image with varying signal-to-noise ratios [74]. This intelligent interpretable ddPCR (I2ddPCR) approach combines specialized neural networks with large language models to provide a robust framework for absolute molecular quantification, achieving sensitivity for detecting low-abundance targets as low as 90.32 copies/μL [74].
Furthermore, ddPCR is increasingly recognized as a gold-standard method for characterizing reference materials, given its ability to provide absolute quantification of specific nucleic acid sequences without calibration curves [75]. This application underscores the technology's precision and reliability for critical measurement tasks where accuracy is paramount.
As rare mutation detection becomes increasingly important in clinical diagnostics, cancer monitoring, and personalized medicine, the strategic implementation of ddPCR workflows following this structured decision framework will enable researchers to maximize data quality, optimize resource utilization, and generate clinically actionable results from challenging samples.
Conclusion
Droplet Digital PCR stands as a cornerstone technology in the modern molecular diagnostics toolkit, offering unparalleled precision for rare mutation detection that is critical for advancing precision oncology and clinical research. Its ability to provide absolute, calibration-free quantification of targets like ctDNA enables robust monitoring of treatment response and minimal residual disease, outperforming qPCR in reproducibility and offering a practical, highly sensitive complement to NGS for validating known biomarkers. Future directions will likely focus on overcoming current limitations in throughput and cost through technological innovations, expanding standardized and reimbursable clinical test menus, and deeper integration with NGS in multi-modal diagnostic workflows. For researchers and drug developers, mastering ddPCR is not just an option but a necessity for driving the next wave of discoveries in personalized medicine.
References
- 1. Digital PCR: from early developments to its future application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278255/]
- 2. dPCR: A Technology Review [https://www.mdpi.com/1424-8220/18/4/1271]
- 3. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 4. Rare Mutation Detection Digital PCR Tutorial [https://www.stillatechnologies.com/digital-pcr/primer-design/rare-mutation-detection/]
- 5. Enhanced Ratio of Signals Enables Digital Mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4411249/]
- 6. Measuring AAV capsids using VeriCheck ddPCR technology [https://www.news-medical.net/health/Measuring-AAV-capsids-using-VeriCheck-ddPCR-technoloy-A-guide.aspx]
- 7. Emerging Technologies Guide: Fall 2025 [https://www.clinicallab.com/emerging-technologies-guide-fall-2025-28397]
- 8. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 9. Comparison of Analytic Methods for Quantitative Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4642823/]
- 10. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 11. dPCR vs. ddPCR: Why Precision Matters in Cell and Gene ... [https://www.roslinct.com/insights/dpcr-vs-ddpcr/]
- 12. Correlation Between Chimeric Antigen Receptor T‐Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12445920/]
- 13. A New View on Minimal Residual Disease Quantification in ... [https://www.sciencedirect.com/science/article/pii/S1525157822001453]
- 14. A comparison of DNA methylation specific droplet digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4622657/]
- 15. Portable Duplex Digital PCR for On-Site Detection of IDH ... [https://www.sciencedirect.com/science/article/abs/pii/S095656632501084X]
- 16. dPCR Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/genomics/qpcr/dpcr?srsltid=AfmBOoo9T5Xd3G0CgctQKLE3bMFjbVDho-qSkM9aqpRX_J8-THYI3F-v]
- 17. Droplet digital PCR assay for precise determination of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291395/]
- 18. Comparing the precision of two digital PCR applications for ... [https://www.nature.com/articles/s41598-025-13143-8]
- 19. Plasma cell-free DNA Droplet Digital PCR provides rapid ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1522426/full]
- 20. Droplet Digital PCR: Advantages and Applications in ... [https://www.labx.com/resources/droplet-digital-pcr-advantages-and-applications-in-molecular-diagnostics/5581]
- 21. Absolute quantification of rare gene targets in limited ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11928631/]
- 22. Development and Validation of a High‐Sensitivity Droplet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11909581/]
- 23. A quality control revolution for droplet digital PCR [https://www.nature.com/articles/d42473-020-00123-x]
- 24. Development and validation of an automated and high ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1529336/full]
- 25. From droplets to diagnosis: AI-driven imaging and system ... [https://www.sciencedirect.com/science/article/pii/S0956566325006177]
- 26. Digital droplet PCR is an accurate and precise method to ... [https://www.nature.com/articles/s41598-025-20944-4]
- 27. Digital PCR Assays and Kits Analysis 2025 and Forecasts ... [https://www.archivemarketresearch.com/reports/digital-pcr-assays-and-kits-762372]
- 28. A Review of Circulating Tumor DNA (ctDNA) and the Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032849/]
- 29. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 30. Liquid Biopsy, ctDNA Diagnosis through NGS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8468354/]
- 31. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 32. Integrating Circulating Tumor DNA into Clinical Management ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346868/]
- 33. Analytical evaluation of circulating tumor DNA sequencing ... [https://www.nature.com/articles/s41598-024-54361-w]
- 34. ctDNA Analysis using Liquid Biopsy [https://sequencing.roche.com/us/en/article-listing/liquid-biopsy.html]
- 35. A comparative study of four cell-free DNA assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217890/]
- 36. Circulating tumour DNA assays in focus: highlights from ... [https://www.nature.com/articles/s44276-025-00181-y]
- 37. Application of droplet digital PCR in minimal residual ... [https://www.nature.com/articles/s41598-024-57016-y]
- 38. Measurable residual disease monitoring by ddPCR in the ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05114-w]
- 39. Digital PCR for Rare Mutation Detection [https://www.thermofisher.com/us/en/home/life-science/pcr/digital-pcr/mutation-detection.html]
- 40. Performance Comparison of Droplet Digital PCR and Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062871/]
- 41. The detection of primary and secondary EGFR mutations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6120312/]
- 42. Development and validation of a methylation-specific ... [https://www.nature.com/articles/s41598-025-15228-w]
- 43. Application of droplet digital polymerase chain reaction ... [https://www.nature.com/articles/s41598-021-02879-8]
- 44. Enhanced Ratio of Signals Enables Digital Mutation ... [https://www.sciencedirect.com/science/article/pii/S1525157815000409]
- 45. Droplet Digital PCR versus qPCR for gene expression ... [https://www.nature.com/articles/s41598-017-02217-x]
- 46. qPCR vs. ddPCR: Which Is Best for You? [https://www.bioradiations.com/qpcr-vs-ddpcr-assays-select-the-best-gene-expression-analysis-method-for-your-application1125/]
- 47. The Role of Digital PCR in Enhancing Diagnostic Power ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11311727/]
- 48. dPCR: A Technology Review - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5948698/]
- 49. Digital PCR | IDT [https://eu.idtdna.com/pages/technology/qpcr-and-pcr/digital-pcr]
- 50. Development of Novel Mutation-Specific Droplet Digital PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6419583/]
- 51. Custom dPCR Assay Design [https://geneglobe.qiagen.com/us/customize/dpcr]
- 52. Validation of Droplet Digital Polymerase Chain Reaction ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.01512/full]
- 53. Measuring Digital PCR Quality: Performance Parameters ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4858304/]
- 54. Commonly used terms in PCR [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/commonly-used-terms-in-pcr/commonly-used-terms-in-pcr]
- 55. Understanding Cq values in PCR [https://www.idtdna.com/page/support-and-education/decoded-plus/understanding-cq-values-in-pcr/]
- 56. Optimisation of robust singleplex and multiplex droplet ... [https://www.nature.com/articles/s41598-019-49043-x]
- 57. Development and validation of a droplet digital PCR assay ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1573949/full]
- 58. Optimization of digital droplet polymerase chain reaction for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4827695/]
- 59. Digital PCR Market Size, Forecast Report [https://www.mordorintelligence.com/industry-reports/digital-pcr-market]
- 60. Challenges Using Droplet Digital PCR for Environmental ... [https://www.mdpi.com/2673-8007/1/1/7]
- 61. Droplet-based digital PCR (ddPCR) and its applications [https://www.sciencedirect.com/science/article/abs/pii/S0165993622003806]
- 62. A high-throughput droplet digital PCR system aiming eight ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708523007124]
- 63. What Are the Advantages of ddPCR Over Other PCR ... [https://mogene.com/what-are-the-advantages-of-ddpcr-over-other-pcr-variants/]
- 64. Absolute vs. Relative Quantification for qPCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/absolute-vs-relative-quantification-real-time-pcr.html]
- 65. dPCR vs qPCR [https://www.qiagen.com/us/applications/digital-pcr/beginners/dpcr-vs-qpcr]
- 66. Comparison of droplet digital PCR and conventional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4353752/]
- 67. Droplet digital PCR of viral DNA/RNA, current progress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8013307/]
- 68. Soil eDNA-based droplet digital PCR assay as a new ... [https://www.sciencedirect.com/science/article/pii/S2351989425003816]
- 69. Digital PCR: A Reliable Tool for Analyzing and Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7247671/]
- 70. Comparison of droplet digital PCR and direct Sanger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6642310/]
- 71. ddpcr: an R package and web application for analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5031129/]
- 72. Using ddPCR to Detect Rare Variant Alleles in cfDNA ... [https://omegabiotek.com/using-ddpcr-to-detect-rare-variant-alleles-in-cfdna-samples-on-the-magbinder-fit24-platform/]
- 73. Quantification of rare somatic single nucleotide variants by ... [https://www.nature.com/articles/s41598-023-39874-0]
- 74. [2501.09218] Interpretable Droplet Digital PCR Assay for ... [https://arxiv.org/abs/2501.09218]
- 75. Digital PCR for the characterization of reference materials [https://www.sciencedirect.com/science/article/pii/S0098299724000153]