Decoding Metastasis: Molecular Mechanisms, Therapeutic Targeting, and Clinical Translation in Cancer Progression
This article provides a comprehensive analysis of the deep molecular mechanisms driving cancer progression and metastasis, a process responsible for the majority of cancer-related deaths.
Decoding Metastasis: Molecular Mechanisms, Therapeutic Targeting, and Clinical Translation in Cancer Progression
Abstract
This article provides a comprehensive analysis of the deep molecular mechanisms driving cancer progression and metastasis, a process responsible for the majority of cancer-related deaths. Tailored for researchers, scientists, and drug development professionals, we explore the complex interplay of genetic, epigenetic, and tumor microenvironmental factors that enable invasion and dissemination. The content systematically progresses from foundational concepts like epithelial-mesenchymal transition (EMT) and signaling pathway dysregulation to methodological approaches for studying metastasis, strategies to overcome therapeutic resistance, and the validation of novel targets through emerging technologies. By integrating recent insights into cuproptosis, metabolic reprogramming, and immune evasion, this review aims to bridge fundamental research with clinical application, offering a roadmap for developing precise and effective anti-metastatic therapies.
The Cellular and Molecular Blueprint of Metastasis
Deconstructing the Multi-Step Metastatic Cascade
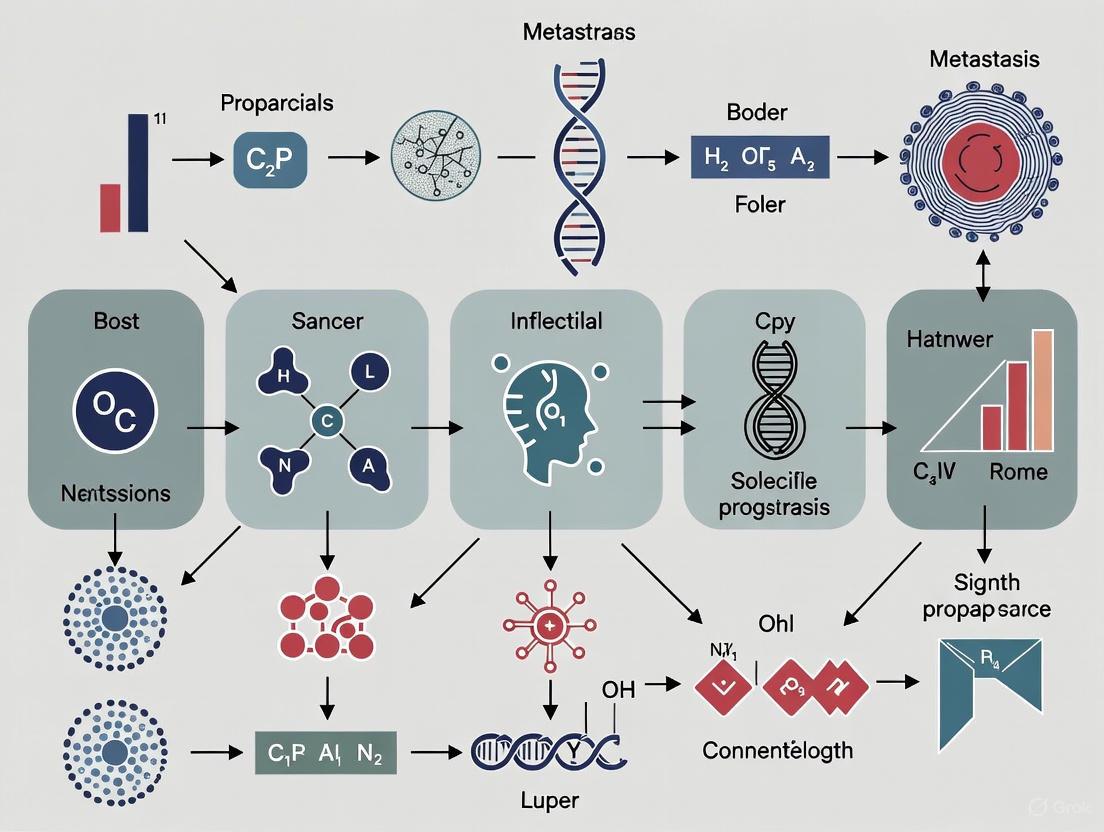
Cancer metastasis is a multifaceted and dynamic process responsible for the majority of cancer-related fatalities. The metastatic cascade involves a series of sequential, interconnected steps through which tumor cells disseminate from the primary tumor to colonize distant organs. This whitepaper deconstructs these stages, examining the molecular mechanisms, including the pivotal role of the pre-metastatic niche (PMN), tumor-derived extracellular vesicles (EVs), and cellular plasticity programs like epithelial-mesenchymal transition (EMT). Furthermore, it explores the experimental models utilized for investigation and discusses emerging therapeutic strategies designed to intercept metastasis at various points in the cascade, providing a molecular roadmap for researchers and drug development professionals.
Cancer metastasis represents the most formidable challenge in oncology, accounting for approximately 90% of cancer-related mortality [1]. It is a highly inefficient, multi-step process where cancer cells must successfully complete each step to form a secondary tumor [2]. The cascade is driven by intense evolutionary pressures, where tumor cells develop mechanisms to cope with numerous stresses encountered during their journey [2]. A critical feature of metastasis is organotropism—the non-random, preferential spread of cancer cells to specific distant organs, a phenomenon first articulated by Stephen Paget's "seed and soil" hypothesis in 1889 [3]. For instance, breast cancer commonly metastasizes to bone, while colorectal cancer often spreads to the liver [3]. Modern research has refined this concept, revealing that organ-specific metastasis relies on the formation of a pre-metastatic niche (PMN), where primary tumor-derived factors precondition a distant site to be receptive for circulating tumor cell (CTC) colonization [1] [3]. A deep molecular understanding of this cascade is paramount for developing effective anti-metastatic therapies.
The Metastatic Cascade: A Stage-by-Stage Molecular Deconstruction
The journey of a metastatic cell is a relentless series of challenges. The following stages outline this complex process.
Genesis of Invasion: Primary Tumor Progression
The initial steps of metastasis occur within the primary tumor, characterized by significant genetic intratumoral heterogeneity. Genomic analyses reveal that driver gene mutations (e.g., in TP53, KRAS, EGFR) not only promote unchecked cell growth but also regulate tumor cell migration and invasion [1]. For example, in lung cancer, upregulation of c-Myc promotes metastasis by enhancing the expression of ZEB1, ZEB2, and SNAIL genes, which are central to the invasive phenotype [1]. Concurrently, crosstalk between cancer stem cells (CSCs) and their microenvironment activates key signaling pathways such as RAS-MAPK and PI3K-AKT-mTOR, driving the progression from benign to invasive malignancy [1].
Local Invasion and Intravasation
To disseminate, tumor cells must breach the basement membrane and invade the surrounding stroma. A key regulator of this process is the Epithelial-Mesenchymal Transition (EMT), where cells lose their epithelial characteristics and acquire a mesenchymal, migratory phenotype [1] [2]. The tumor microenvironment (TME) plays an active role; for instance, Cancer-Associated Fibroblasts (CAFs) facilitate invasion by releasing matrix metalloproteinases (MMPs) and chemokines like SDF-1α/CXCL12, which remodel the extracellular matrix (ECM) and guide cell movement [2]. Furthermore, increased ECM stiffness activates mechanotransduction pathways, including the TWIST1-G3BP2 axis and the Hippo pathway effectors YAP/TAZ, to promote EMT and local invasion [2]. Following invasion, cells enter the circulation through intravasation.
Survival in Circulation and Travel to Distant Sites
Once in the bloodstream, cells are termed Circulating Tumor Cells (CTCs) and face immense stresses, including fluid shear stress and immune surveillance [1]. CTCs enhance their survival through homotypic clustering or heterotypic interactions with other cells, such as platelets [1]. Platelets can form aggregates around CTCs, providing physical shielding and enhancing immune evasion [1]. Only a small fraction of CTCs with specific metastatic properties, including the ability to evade anoikis (a form of cell death upon detachment), survive this phase [1] [2].
Pre-Metastatic Niche (PMN) Formation
Prior to the arrival of CTCs, the primary tumor actively prepares distant organs through the formation of a pre-metastatic niche (PMN) [1] [3]. This concept adds a new dimension to the traditional metastatic cascade. The priming of the PMN is largely orchestrated by tumor-derived extracellular vesicles (EVs), including exosomes, which carry proteins, lipids, and nucleic acids [1]. These EVs travel to specific organs and initiate processes such as ECM remodeling, altered vascular permeability, and the establishment of an immunosuppressive microenvironment [1] [3]. Key molecular players include EVs carrying integrins that interact with the ECM and inflammatory factors that suppress local immunity, creating a "fertile soil" for subsequent colonization [1].
Extravasation and Colonization
CTCs arrest in the capillary beds of distant organs and exit the circulation through extravasation. This step is influenced by vascular permeability and mechanical constraints, such as capillary size and shear stress [3]. Upon extravasation, disseminated tumor cells (DTCs) must adapt to the new microenvironment to survive and proliferate. However, many DTCs may enter a dormant state, persisting for years before potentially forming a clinically detectable macrometastasis [1]. Successful colonization requires DTCs to overcome local stresses, evade immune destruction, and co-opt the supportive functions of the niche's stromal components [2].
Table 1: Key Molecular Players in the Metastatic Cascade
| Metastatic Stage | Key Molecular Players | Primary Function |
|---|---|---|
| Invasion & Intravasation | EMT transcription factors (ZEB1, SNAIL), CAFs, MMPs, YAP/TAZ | Enables local invasion, ECM degradation, and entry into circulation |
| Circulation | CTC clusters, Platelets, Anti-apoptotic signals (e.g., BCL-2) | Promotes survival against shear stress and immune surveillance |
| Pre-Metastatic Niche | Tumor-derived EVs (exosomes), Integrins, Immunosuppressive factors (e.g., PD-L1) | Remodels distant site to be permissive for colonization |
| Extravasation & Colonization | Dormancy-inducing signals, Metabolic reprogramming factors, Local stromal cells (e.g., CAFs) | Facilitates exit from vasculature and adaptation to/outgrowth in new organ |
Molecular Mechanisms and Signaling Pathways
The Role of the Tumor Microenvironment (TME) and Cellular Stresses
The TME exerts significant selective pressure on tumor cells. Key stresses include:
- Hypoxia: Regions of low oxygen within solid tumors stabilize Hypoxia-Inducible Factors (HIFs), master regulators that trigger adaptive responses promoting invasion, EMT, and metabolic reprogramming to facilitate metastasis [2].
- ECM Stiffness: A stiff ECM, commonly found in tumors, promotes pro-metastatic signaling. For example, it can induce miR-18a expression, which downregulates the tumor suppressor PTEN, and can silence miR-9 via promoter methylation, leading to elevated VEGF-A and enhanced metastasis [2].
Organotropism: The "Seed and Soil" Hypothesis Revisited
Organotropism is governed by anatomical constraints, molecular crosstalk, and microenvironmental compatibility [3]. While circulatory patterns explain initial dissemination routes (e.g., colorectal cancer cells traveling via the portal vein to the liver), they cannot fully account for metastatic patterns [3]. The molecular basis lies in the specific compatibility between tumor cell receptors ("seed") and ligands expressed in the target organ's vasculature and ECM ("soil"). Tumor-derived EVs are instrumental in this process, as their surface molecules, such as integrins, dictate their homing to specific organs and initiate PMN formation [1] [3].
Experimental Models for Metastasis Research
A variety of models are employed to study the complex metastatic cascade, each with distinct advantages and limitations. The choice of model depends on the specific research question, whether it is investigating molecular mechanisms, screening for drugs, or validating therapeutic targets.
Table 2: Comparison of Experimental Metastasis Models
| Model Type | Key Features | Advantages | Limitations |
|---|---|---|---|
| Genetically Engineered Mouse Model (GEMM) | Spontaneous tumor formation in immunocompetent host [4] | Recapitulates natural tumor progression; intact immune system [4] | Long development time; high cost; technically complex [4] |
| Orthotopic Xenograft | Human tumor cells injected into corresponding mouse organ [4] | Better mimics tumor microenvironment; allows study of metastasis [4] | Technically demanding; requires immunocompromised mice [4] |
| Patient-Derived Xenograft (PDX) | Human tumor tissue transplanted into immunocompromised mouse [4] | Preserves patient tumor heterogeneity; personalized medicine applications [4] | Limited human immune system interaction; costly and time-consuming [4] |
| Zebrafish Xenograft | Human cancer cells injected into transparent zebrafish embryo [4] | Real-time, high-resolution imaging; high-throughput drug screening [4] | Evolutionary distance from mammals; limited immune relevance at larval stage [4] |
| Microfluidic "Organs-on-Chip" | Micro-engineered system to simulate metastatic steps in vitro [5] | Precise control of microenvironment; allows real-time observation of intravasation/extravasation [5] | May oversimplify in vivo complexity; lacks full systemic interaction [5] |
Detailed Experimental Protocol: Plug-and-PlayIn VitroMetastasis System
This protocol outlines the use of a modular microfluidic system to recapitulate key metastatic steps [5].
- Objective: To investigate cancer cell proliferation, migration, intravasation, and detachment into circulating flow in a controlled 3D microenvironment.
- Materials:
- U-well inserts with porous membranes.
- Microfluidic metastasis chip housing and perfusion system.
- Cell lines: e.g., A549-GFP (human lung adenocarcinoma) and HPMECs (human pulmonary microvascular endothelial cells).
- Culture reagents: Appropriate medium, TGF-β1 (a biochemical inducer of invasion), and hydrogel (e.g., Matrigel).
- Methodology:
- Cell Seeding in U-well: Seed A549-GFP cells onto the porous membrane of the U-well insert. For co-culture studies, seed HPMECs on the opposite side of the membrane.
- Hydrogel Embedding (Optional): For 3D migration studies, mix A549-GFP cells with a hydrogel and load into the U-well chamber.
- Plug-and-Play Assembly: After cells attach (e.g., 6 hours), insert the U-well into the metastasis chip housing.
- Perfusion and Induction: Connect the chip to a perfusion system (e.g., peristaltic pump) to establish circulating flow. Introduce biochemical inducers like TGF-β1 into the circulating medium.
- Monitoring and Analysis: The U-well can be removed for imaging under a microscope without disturbing the setup. Monitor over time (e.g., 3-20 days) for:
- Proliferation and Migration in 3D matrix.
- Intravasation: Cells crossing the membrane into the flow channel, enhanced by TGF-β1 or endothelial co-culture.
- Detachment: Cells transforming into CTCs within the circulating flow after long-term culture.
Therapeutic Strategies and Research Toolkit
Targeting the Metastatic Cascade
Therapeutic intervention can be aimed at different stages of the metastatic cascade:
- Targeting the PMN: Strategies focus on disrupting the formation of the pre-metastatic niche by inhibiting tumor-derived EV release or function, or by targeting specific components like fibronectin deposition or the recruitment of bone marrow-derived cells [1] [3].
- Inhibiting Stress-Relief Pathways: Tumor cells rely on "metastasis fitness genes" to cope with stresses. Targeting these pathways, such as HIFs under hypoxia or anti-apoptotic signals during circulation, represents a promising strategy [2].
- Anti-Platellet Therapy: Drugs like aspirin are being investigated for their potential to disrupt the protective interaction between platelets and CTCs, thereby reducing metastatic potential [1].
- Eradicating Dormant Cells: A major challenge is targeting minimal residual disease. Understanding the molecular signals that maintain dormancy or trigger awakening is crucial for preventing late-term recurrences [1].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Reagents and Materials for Metastasis Research
| Reagent / Material | Function in Experimental Design |
|---|---|
| TGF-β1 (Transforming Growth Factor-Beta 1) | A potent biochemical inducer used to trigger Epithelial-Mesenchymal Transition (EMT) and enhance cell invasion and intravasation in in vitro assays [5]. |
| Hydrogel/ECM Matrix (e.g., Matrigel) | Provides a three-dimensional (3D) scaffold for cell culture, more accurately mimicking the in vivo tumor microenvironment for studying cell migration and invasion [5]. |
| Human Pulmonary Microvascular Endothelial Cells (HPMECs) | Used in co-culture models to create a biologically relevant endothelial barrier for studying the intravasation and extravasation steps of the metastatic cascade [5]. |
| Fluorescently-Labeled Cell Lines (e.g., A549-GFP) | Enable real-time tracking and high-resolution visualization of cancer cell behavior, including migration, invasion, and circulation, in live-cell imaging systems [5]. |
| Tumor-Derived Extracellular Vesicles (EVs) | Isolated from patient serum or cancer cell cultures, they are used to study the molecular mechanisms of PMN formation and organotropism [1] [3]. |
| Dipotassium N-acetyl-DL-aspartate | Dipotassium N-acetyl-DL-aspartate|CAS 3397-52-2 |
| 2-(Allyloxy)-3-bromobenzaldehyde | 2-(Allyloxy)-3-bromobenzaldehyde|241.08 g/mol|RUO |
Deconstructing the multi-step metastatic cascade reveals a complex biological process governed by dynamic molecular interactions between tumor cells and their microenvironments. From the initial acquisition of invasive capabilities at the primary site to the orchestration of a receptive pre-metastatic niche and the ultimate challenge of colonization in a distant organ, each step presents unique molecular vulnerabilities. The integration of advanced experimental models—from GEMMs to sophisticated microfluidic systems—along with multi-omics technologies and bioinformatics, is rapidly accelerating our understanding. For researchers and drug developers, this detailed molecular map of metastasis is indispensable, offering a foundation for rational drug design and the development of novel therapeutic strategies aimed at intercepting this lethal cascade, thereby transforming the clinical outlook for patients with advanced cancer.
Epithelial-Mesenchymal Transition (EMT) as a Master Driver of Invasion
Epithelial-mesenchymal transition (EMT) represents a fundamental cellular reprogramming event wherein polarized, adhesive epithelial cells undergo biochemical changes to assume a mesenchymal phenotype characterized by enhanced migratory capacity, invasiveness, and resistance to apoptosis [6]. This dynamic process, essential during embryogenesis and wound healing, is co-opted by carcinoma cells to facilitate local invasion and metastatic dissemination [7]. During EMT, epithelial cells lose their characteristic apical-basal polarity and intercellular junctions, dramatically reorganize their cytoskeleton, and acquire front-rear polarity with associated migratory protrusions [8]. The transition is governed by complex molecular networks involving specific transcription factors, signaling pathways, epigenetic regulators, and post-translational modifications that collectively enable tumor cells to detach from primary sites, invade surrounding tissues, and ultimately metastasize [9] [7].
The invasive capabilities conferred by EMT make it a critical determinant of cancer progression and patient outcomes. In colorectal cancer, EMT drives metastasis and progression, contributing to invasion, intravasation, and colonization of distant organs [7]. Similarly, in breast cancer—particularly aggressive subtypes like triple-negative breast cancer—EMT promotes tumor aggressiveness, metastatic spread, and therapy resistance [10]. Understanding EMT's role as a master driver of invasion requires elucidating its core molecular mechanisms, regulatory networks, and the experimental approaches used to investigate this critical process in cancer biology.
Core Molecular Mechanisms of EMT
Transcriptional Regulation and Key Signaling Pathways
The molecular machinery of EMT is orchestrated by a core set of transcription factors and signaling pathways that reprogram gene expression to dismantle epithelial characteristics and install mesenchymal features. Key EMT-transcription factors (EMT-TFs) include members of the SNAIL (SNAIL1/Snail, SNAIL2/Slug), ZEB (ZEB1, ZEB2), and TWIST (TWIST1, TWIST2) families [7]. These master regulators rep epithelial genes while simultaneously activating mesenchymal genes through binding to E-box sequences in target gene promoters [7].
SNAIL family transcription factors contain zinc finger motifs that enable binding to E-box sequences in target gene promoters. SNAIL1 predominantly utilizes ZF1 and ZF2 for transcriptional repression, while SNAIL2 relies more on ZF3 and ZF4, suggesting distinct regulatory targets despite functional redundancy [7]. Both factors potently repress CDH1 (E-cadherin) expression, disrupting adherens junctions critical for epithelial integrity [7].
ZEB family proteins (ZEB1 and ZEB2) also function as transcriptional repressors of E-cadherin but can exhibit contextual transcriptional activation properties. ZEB1 can interact with coactivator p300 to activate mesenchymal genes through chromatin remodeling, while ZEB2 collaborates with TWIST1 to synergistically repress E-cadherin transcription [7]. In colorectal cancer, elevated ZEB expression correlates significantly with reduced overall and disease-free survival [7].
TWIST family basic helix-loop-helix transcription factors regulate EMT by heterodimerizing with E-proteins to enable DNA binding and transcriptional repression of epithelial genes [7]. Non-acetylated TWIST1 recruits the NuRD repressor complex, while diacetylated TWIST1 interacts with BRD4 to activate mesenchymal gene loci and MYC expression [7]. TWIST1 also induces chromosomal instability during EMT, enhancing cellular heterogeneity and tumor progression [7].
Multiple signaling pathways converge to regulate these EMT-TFs in response to developmental cues, tissue damage, or oncogenic signaling:
- TGF-β pathway: A potent inducer of EMT that activates SMAD proteins, which translocate to the nucleus and stimulate expression of SNAIL, SLUG, and TWIST [9] [6].
- Wnt/β-catenin pathway: Stabilized β-catenin translocates to the nucleus and associates with TCF/LEF transcription factors to activate EMT-TFs including SNAIL and TWIST [9] [6].
- Receptor Tyrosine Kinase (RTK) pathways: Growth factor signaling through ERK, PI3K/AKT, and other kinase cascades phosphorylates and modulates the activity of EMT-TFs [9].
- Notch pathway: Cleaved Notch intracellular domain (NICD) translocates to the nucleus and forms a complex with CSL to activate transcription of EMT-TFs including SNAIL and SLUG [9].
- Hypoxia-induced pathways: HIF-1α activation under low oxygen conditions promotes expression of TWIST, SNAIL, and ZEB [9].
Table 1: Major Signaling Pathways in EMT-Driven Invasion
| Pathway | Key Inducers | Major EMT-TFs Regulated | Primary Cellular Outcomes |
|---|---|---|---|
| TGF-β | TGF-β ligand, SMAD phosphorylation | SNAIL, SLUG, TWIST | Cytoskeletal reorganization, ECM production |
| Wnt/β-catenin | WNT ligands, β-catenin stabilization | SNAIL, TWIST | Loss of cell adhesion, enhanced motility |
| RTK | EGF, FGF, HGF via ERK, PI3K/AKT | SNAIL, ZEB | Increased proliferation, survival |
| Notch | Ligand-receptor interaction, NICD release | SNAIL, SLUG | Cell fate decisions, invasion |
| Hypoxia | Low O₂, HIF-1α stabilization | TWIST, ZEB | Angiogenesis, metabolic adaptation |
Matrix Metalloproteinases and Extracellular Matrix Remodeling
Matrix metalloproteinases (MMPs) sit at the nexus of EMT by dismantling physical barriers to invasion and activating pro-EMT signaling pathways [6]. These zinc-dependent endopeptidases degrade structural components of the extracellular matrix (ECM) and basement membranes, critical events that enable epithelial cell detachment and migration [6]. MMPs are classified into subgroups based on substrate specificity:
- Collagenases (MMP-1, -8, -13): Degrade fibrillar collagens (types I, II, III) [6]
- Gelatinases (MMP-2, -9): Target gelatin and collagen type IV, major basement membrane components [6]
- Stromelysins (MMP-3, -10, -11): Exhibit broad substrate specificity against proteoglycans, laminins, and other ECM components [6]
- Membrane-type MMPs (MMP-14): Activate pro-MMP-2 and directly degrade ECM at cell surfaces [6]
Beyond ECM degradation, MMPs facilitate EMT through multiple mechanisms: (1) releasing latent growth factors like TGF-β sequestered within the ECM; (2) cleaving junctional proteins such as E-cadherin to dismantle epithelial adhesion; and (3) activating integrin signaling pathways that promote mesenchymal characteristics [6]. Specific MMPs have distinct EMT-promoting functions—MMP-3 induces expression of mesenchymal markers while repressing epithelial markers; MMP-7 cleaves E-cadherin directly, disrupting cell-cell adhesion; and MMP-14 activates pro-MMP-2 while facilitating cell migration [10]. The urokinase plasminogen activator (uPA) system works concertedly with MMPs, activating plasminogen to plasmin, which in turn activates MMP-2 and MMP-9, creating a proteolytic cascade that degrades basement membranes and facilitates intravasation [11].
Metabolic Reprogramming and Cytoskeletal Reorganization
EMT involves profound changes in cellular metabolism and architecture that support an invasive phenotype. Cancer cells undergoing EMT exhibit metabolic plasticity, adapting their energy production to meet the demands of migration and survival in challenging microenvironments [8]. A key adaptation is the shift toward glycolysis, known as the Warburg effect, which provides rapid ATP generation and metabolic intermediates for biosynthetic pathways even under oxygen-replete conditions [8]. This metabolic reprogramming supports the increased energy requirements of cytoskeletal reorganization and membrane dynamics during cell migration.
The actin cytoskeleton undergoes extensive remodeling during EMT, transforming from a cortical arrangement supporting epithelial integrity to stress fibers that enable contraction and movement [9]. Small GTPases including RhoA, Rac1, and Cdc42 regulate this cytoskeletal reorganization—Rac1 promotes lamellipodia formation for cell-front extension, while Cdc42 induces filopodia for environmental sensing [9]. Actin-binding proteins including cofilin (which destabilizes actin filaments) and profilin (which promotes actin polymerization) facilitate the dynamic cytoskeletal changes required for motility [9]. EMT transcription factors directly influence these processes; TWIST1 induces formation of invadopodia, actin-rich protrusions that recruit MMPs to degrade ECM at the leading edge of invading cells [12].
Table 2: Key Molecular Changes During EMT-Driven Invasion
| Cellular Component | Epithelial Characteristics (Lost) | Mesenchymal Characteristics (Gained) |
|---|---|---|
| Cell Adhesion | E-cadherin, occludin, claudins, desmoplakin | N-cadherin, fibronectin, vitronectin |
| Cytoskeleton | Cortical actin, cytokeratins | Stress fibers, vimentin, moesin |
| ECM Interaction | Basement membrane attachment via hemidesmosomes | Focal adhesions with α5β1, αvβ3 integrins |
| Transcription Factors | Low SNAIL, ZEB, TWIST | High SNAIL, ZEB, TWIST |
| Proteolytic Enzymes | Low MMP-2, MMP-9, uPA | High MMP-2, MMP-9, uPA |
| Metabolic Profile | Oxidative phosphorylation | Glycolysis, glutamine metabolism |
Experimental Models and Methodologies for Studying EMT
In Vitro Models and Functional Assays
Investigating EMT-driven invasion requires experimental models that recapitulate key aspects of the transition and its functional consequences. Classical migration and invasion assays provide quantitative measurements of these hallmarks:
Transwell Migration/Invasion Assays: Cells are seeded in the upper chamber of a transwell insert, with a chemoattractant in the lower chamber. For invasion assays, the membrane is coated with Matrigel or collagen to simulate ECM penetration [11]. After incubation, cells that migrate through the pores (and degrade the matrix in invasion assays) are fixed, stained, and quantified microscopically.
Scratch/Wound Healing Assay: A confluent cell monolayer is scratched with a pipette tip, creating a cell-free zone. Migration into the wound is monitored over time via live-cell imaging or fixed time points, quantifying closure rates [11].
3D Spheroid Invasion Assays: Cells are cultured as spheroids in low-attachment plates or hanging drops, then embedded in ECM components like collagen or Matrigel. Invasion from the spheroid into the surrounding matrix is quantified over several days, providing a more physiologically relevant model of tumor cell behavior [11].
Microfluidic Devices: Advanced platforms create controlled chemical gradients and microenvironments to study cancer cell migration and invasion with high spatial and temporal resolution [11]. These systems can incorporate multiple cell types and ECM conditions to better mimic the tumor microenvironment.
Organoid Cultures: Patient-derived or cell line-derived organoids grown in 3D matrices preserve tissue architecture and cellular heterogeneity, enabling study of EMT in contexts that more closely resemble in vivo conditions [11].
In Vivo Models and Imaging Approaches
In vivo models provide essential physiological context for studying EMT and metastasis, capturing complex interactions within the tumor microenvironment:
Chicken Chorioallantoic Membrane (CAM) Assay: The vascularized CAM of chicken embryos serves as a host for tumor xenografts, allowing observation of tumor cell invasion, intravasation, and metastasis within a naturally immunodeficient environment [11]. This model is particularly useful for studying early metastatic events.
Genetically Engineered Mouse Models (GEMMs): These models develop spontaneous tumors through tissue-specific activation of oncogenes and/or deletion of tumor suppressors, enabling study of EMT in authentic tumor microenvironments with intact immune systems [11].
Cell Line-Derived and Patient-Derived Xenografts: Human cancer cells or tissue fragments are transplanted into immunodeficient mice, with patient-derived xenografts (PDXs) maintaining tumor heterogeneity and therapeutic responses observed in patients [11].
Lineage Tracing and Dynamic Imaging: Genetically encoded fluorescent reporters under control of EMT-TF promoters (e.g., SNAIL, TWIST) enable visualization of EMT dynamics in live animals. Intravital imaging techniques allow real-time observation of cancer cell invasion, intravasation, and metastatic seeding [11].
Diagram 1: Core Signaling Network Driving EMT and Invasion. This diagram illustrates the principal signaling pathways, transcription factors, and functional outcomes in EMT-driven cancer invasion. Key EMT-inducing signals activate intracellular pathways that converge on master transcription factors, which coordinately regulate cellular changes enabling invasion.
Quantitative Biomarker Analysis and Clinical Implications
EMT Biomarkers and Signatures
The molecular changes during EMT provide biomarkers for tracking this process in experimental systems and clinical samples. These biomarkers fall into several categories:
Epithelial markers (downregulated): E-cadherin, occludin, claudins, cytokeratins, and desmoplakin [7] [11]. Loss of E-cadherin, a critical component of adherens junctions, represents a hallmark event in EMT.
Mesenchymal markers (upregulated): N-cadherin, vimentin, fibronectin, α-smooth muscle actin, and matrix metalloproteinases [9] [7]. The "cadherin switch" from E-cadherin to N-cadherin expression is particularly characteristic of EMT.
Transcription factors: SNAIL1/2, ZEB1/2, and TWIST1/2 serve as functional biomarkers of EMT activation [7]. These are often assessed through nuclear localization in immunohistochemistry or mRNA expression levels.
Intermediate state biomarkers: Recent single-cell RNA sequencing studies have identified genes upregulated in hybrid E/M states, including SFN (stratifin), ITGB4, ITGA6, SNCG, and WNT9A [13]. These markers identify cells in partial EMT states that may have enhanced metastatic potential.
Multi-omics approaches integrating genomics, transcriptomics, proteomics, and metabolomics provide comprehensive EMT signatures rather than relying on individual markers [10]. Machine learning algorithms applied to these datasets can identify EMT-related gene expression patterns with prognostic significance across cancer types [10] [14].
Table 3: Quantitative EMT Biomarkers in Specific Cancers
| Cancer Type | EMT-Related Biomarkers | Detection Method | Clinical/Prognostic Significance |
|---|---|---|---|
| Hepatocellular Carcinoma | LAMA4, C7, KPNA2, STMN1, SF3B4 [15] | Transcriptomics, RT-qPCR | Predictive of survival outcomes |
| Clear Cell Renal Cell Carcinoma | AFM, CYS1, FAM171A1, GSTM3, FKBP10, MALL, RGS5, TIMP1 [14] | Bulk & single-cell RNA-seq | Prognostic model predicting immunotherapy response |
| Colorectal Cancer | SNAIL, SLUG, ZEB1, ZEB2, TWIST1 [7] | IHC, mRNA expression | Associated with metastatic potential and poor survival |
| Breast Cancer | MMP3, MMP9, MMP14, SNAI1, VIM, CDH2 [10] | Multi-omics, machine learning | Predict invasion and poor prognosis |
| Pan-Cancer Intermediate States | SFN, NRG1, ITGB4, ITGA6, SNCG [13] | scRNA-seq, mathematical modeling | Associated with metastatic competence |
Therapeutic Targeting of EMT
The critical role of EMT in invasion and metastasis makes it an attractive therapeutic target. Several strategic approaches are under investigation:
Signaling pathway inhibitors: Small molecule inhibitors targeting TGF-β receptors, Wnt pathway components, Notch signaling, and receptor tyrosine kinases can block EMT induction [9] [7]. Many are in clinical trials, often in combination with conventional therapies.
MMP inhibitors: Despite challenges in clinical translation due to toxicity and lack of specificity, new generation MMP inhibitors with improved selectivity are being developed [6]. Engineered tissue inhibitors of metalloproteinases (TIMPs) and CRISPR/Cas-based approaches offer more targeted strategies [6].
EMT-TF targeting: Direct targeting of transcription factors like SNAIL, TWIST, and ZEB remains challenging but approaches include disrupting their interactions with cofactors or promoting their degradation [7].
Inducing mesenchymal-epithelial transition (MET): Therapeutic strategies that reverse EMT may reduce invasiveness and sensitize cells to conventional therapies [7]. However, caution is needed as MET induction may potentially promote proliferative outgrowth at metastatic sites.
The relationship between EMT and therapy resistance underscores the potential of EMT-targeting agents to enhance conventional cancer treatments. EMT contributes to radioresistance through multiple mechanisms, including enhanced DNA repair capacity, reduced proliferation, and increased free radical scavenging [9]. Similarly, EMT confers resistance to chemotherapy and targeted therapies through various mechanisms, including increased drug efflux, enhanced survival signaling, and metabolic adaptations [9] [7]. Combining EMT inhibitors with standard treatments may therefore overcome resistance and improve outcomes.
The Scientist's Toolkit: Essential Research Reagents and Models
Table 4: Essential Research Tools for Investigating EMT-Driven Invasion
| Category | Specific Reagents/Models | Key Applications | Experimental Considerations |
|---|---|---|---|
| Cell Lines | MDCK (Madin-Darby Canine Kidney), MCF10A (human mammary), NMuMG (murine mammary) | Basic EMT mechanisms, TGF-β-induced EMT | Species-specific responses, variation between laboratories |
| EMT Inducers | Recombinant TGF-β1, EGF, FGF, HGF; Wnt3a; TNF-α | Controlled induction of EMT in vitro | Concentration optimization, combination effects |
| Inhibitors | SB431542 (TGF-β receptor), XAV939 (Wnt), DAPT (Notch) | Pathway-specific EMT inhibition | Off-target effects, cytotoxicity assessment |
| 3D Culture Matrices | Matrigel, collagen I, fibrin, synthetic hydrogels | Spheroid invasion, organoid models | Batch variability (Matrigel), stiffness effects |
| Migration/Invasion Assays | Transwell inserts, Boyden chambers, Ibidi Culture-Inserts | Quantitative migration and invasion measurement | Coating consistency, imaging methodology |
| Molecular Detection | E-cadherin, N-cadherin, vimentin antibodies; SNAIL, TWIST primers | Immunofluorescence, Western blot, RT-qPCR | Validation of antibody specificity, normalization controls |
| Advanced Models | Patient-derived organoids, microfluidic devices, GEMMs | Physiological relevance, therapeutic testing | Technical complexity, resource requirements |
| Live-Cell Imaging | GFP-tagged EMT reporters, Incucyte systems, confocal microscopy | Dynamic EMT tracking, single-cell analysis | Phototoxicity, reporter perturbation |
| 5,5-Difluoro-6-hydroxyhexanoic acid | 5,5-Difluoro-6-hydroxyhexanoic acid, CAS:2247107-02-2, MF:C6H10F2O3, MW:168.14 | Chemical Reagent | Bench Chemicals |
| Ethyl 1-oxoisochroman-3-carboxylate | Ethyl 1-oxoisochroman-3-carboxylate|3-Carboxylate | Ethyl 1-oxoisochroman-3-carboxylate is a chemical reagent for research purposes only (RUO). It is not for human or veterinary use. | Bench Chemicals |
Diagram 2: Experimental Workflow for EMT and Invasion Studies. This diagram outlines a systematic approach for investigating EMT-driven invasion, from initial induction to functional validation, incorporating both in vitro and in vivo assessment methods.
Epithelial-mesenchymal transition stands as a master driver of cancer invasion through its ability to coordinately regulate multiple cellular processes—dissolving cell-cell junctions, reorganizing the cytoskeleton, activating ECM-degrading enzymes, and enhancing motility. The molecular understanding of EMT has expanded considerably, revealing complex regulatory networks centered on core transcription factors but extending to epigenetic modifiers, post-translational mechanisms, and metabolic adaptations. While significant challenges remain in selectively targeting EMT for therapeutic benefit without disrupting its physiological functions, ongoing research using increasingly sophisticated experimental models continues to elucidate context-specific aspects of this critical process. Integrating single-cell technologies, mathematical modeling, and advanced imaging with functional studies promises to further unravel the complexities of EMT plasticity and its contribution to metastatic progression, potentially identifying new vulnerabilities for therapeutic intervention in advanced cancers.
The tumor microenvironment (TME) is a complex and dynamic ecosystem that surrounds cancer cells, playing a pivotal role in tumor initiation, progression, metastasis, and therapy resistance [16]. It represents a paradigm shift in oncology, moving the focus from the cancer cell alone to a holistic understanding of the tumor as a multicellular organ. As a major health issue worldwide responsible for nearly one in six global fatalities, cancer's complexity and heterogeneity are largely governed by the TME [16]. This multifaceted niche comprises diverse cellular components, including stromal cells and immune cells, alongside non-cellular elements such as the extracellular matrix (ECM) and soluble factors like cytokines and chemokines [16]. These components interact through intricate signaling networks to precisely regulate interactions that enable cancer cells to proliferate continuously, resist apoptosis, evade immune surveillance, and metastasize to distant regions [17]. The TME is not merely a passive bystander but actively contributes to the malignant phenotype, making it a critical frontier for understanding cancer biology and developing novel therapeutic strategies [16] [18].
Cellular and Structural Components of the TME
The TME consists of a sophisticated network of cellular and structural components that collectively support tumor growth and dissemination. Understanding these constituents is essential for comprehending TME functionality.
Core Cellular Constituents
Table 1: Major Cellular Components of the Tumor Microenvironment
| Cell Type | Subtypes/Functions | Pro-Tumorigenic Effects | Key Molecular Mediators |
|---|---|---|---|
| Cancer Cells | Genetically/ epigenetically heterogeneous populations [16] | Tumor initiation, progression, metastasis [16] | KRAS, TP53, EGFR mutations; EMT program activation [16] [19] |
| Immune Cells | Tumor-Associated Macrophages (TAMs) - M2 phenotype [16] [18] | Immunosuppression, angiogenesis, ECM remodeling [16] [18] | CCL2, IL-10, TGF-β, VEGF, MMPs [16] [18] |
| Regulatory T-cells (Tregs) [16] | Suppress anti-tumor immune responses [16] | IL-10, TGF-β [16] | |
| Myeloid-Derived Suppressor Cells (MDSCs) [16] | Inhibit T-cell function, promote immunosuppression [16] | Arginase, ROS, IFN-γ suppression [16] | |
| Natural Killer (NK) cells [16] | Dysfunctional in TME, impaired tumor cell killing [16] | Inhibitory receptors, TGF-β [16] | |
| Stromal Cells | Cancer-Associated Fibroblasts (CAFs) [16] | ECM remodeling, tumor invasion, therapy resistance [16] | TGF-β, FGF, HGF, ECM proteins [16] |
| Mesenchymal Stem Cells (MSCs) [18] | Differentiate into CAFs, promote metastasis via exosomes [16] [18] | Growth factors, cytokines, exosomes [16] [18] | |
| Endothelial Cells [16] | Angiogenesis, nutrient supply, intravasation/extravasation [16] | VEGF, Angiopoietins [16] |
Non-Cellular Components and Physical Properties
The structural backbone of the TME is the extracellular matrix (ECM), a complex network of proteins including collagen, fibronectin, and hyaluronan that provides physical scaffolding and biochemical signals [18]. The ECM is dynamically remodeled by matrix metalloproteinases (MMPs) and other enzymes produced by cancer and stromal cells, facilitating invasion and metastasis [18]. Beyond the ECM, the TME exhibits distinct physical properties:
- Hypoxia: Low oxygen tension (partial pressure <10 mmHg) develops due to imbalanced oxygen supply and consumption [17]. This activates hypoxia-inducible factors (HIFs) that drive adaptive responses including angiogenesis, metabolic reprogramming, and metastasis [17].
- Acidity: The "Warburg effect" describes how tumor cells preferentially utilize anaerobic glycolysis even under aerobic conditions, producing large amounts of lactic acid [17]. Coupled with poor vascular clearance, this creates an acidic microenvironment (pH 6.5-7.0) that promotes invasion and immune suppression [17].
- Mechanical Forces: Increased tissue stiffness and interstitial fluid pressure resulting from ECM remodeling and vascular abnormalities influence cancer cell behavior and hinder drug delivery [18].
Molecular Mechanisms and Signaling Pathways in TME-Driven Metastasis
Metastasis is a multi-step process responsible for approximately 90% of cancer mortality, with the TME playing an indispensable role at every stage [19] [18]. The metastasis cascade encompasses local invasion, intravasation, survival in circulation, extravasation, and colonization of distant organs [19].
Key Signaling Pathways in TME-Mediated Metastasis
Diagram 1: TME Signaling Pathways in Metastasis
The diagram above illustrates three major signaling axes through which the TME promotes metastasis. The hypoxia pathway stabilizes HIF-α subunits, which dimerize with HIF-β to activate transcription of genes involved in epithelial-mesenchymal transition (EMT) and angiogenesis [17]. Meanwhile, TGF-β secreted by CAFs and TAMs activates SMAD signaling to drive EMT and ECM remodeling [16] [18]. Parallelly, immune checkpoint activation through PD-1/PD-L1 interactions leads to T-cell exhaustion and immune evasion [16] [20]. These pathways collectively enable metastatic progression.
The Metastasis Cascade: TME Interactions at Each Stage
Local Invasion and EMT: Cancer cells at the invasive front undergo epithelial-mesenchymal transition (EMT), a transdifferentiation program often activated by TME-derived signals like TGF-β, TNF-α, and EGF from TAMs and CAFs [18] [1]. During EMT, cells lose epithelial markers (E-cadherin) and gain mesenchymal markers (vimentin, N-cadherin), enhancing motility and invasiveness [18]. The concept of "tumor microenvironment of metastasis" (TMEM) describes a tripartite structure comprising a cancer cell, a TAM, and an endothelial cell, which serves as a portal for intravasation [18].
Intravasation and Circulation: Tumor cells enter the circulation through leaky, abnormal tumor vasculature. Platelets play a crucial role by forming protective emboli with circulating tumor cells (CTCs), shielding them from shear stress and natural killer (NK) cell-mediated cytotoxicity [19]. Platelets also release TGF-β to further drive EMT, enhancing the invasive capacity of CTCs [19].
Pre-Metastatic Niche Formation: Primary tumor-derived extracellular vesicles (EVs), particularly exosomes, prepare distant organ sites for metastasis by creating a pre-metastatic niche (PMN) [1]. These EVs carry proteins, lipids, and nucleic acids that remodel the local microenvironment through ECM modification, angiogenesis, and immunosuppression [1].
Extravasation and Colonization: At secondary sites, CTCs exit circulation (extravasation) and may enter a dormant state, surviving as micrometastases [19]. Reactivation from dormancy depends on non-autonomous mechanisms, including inflammatory signals and remodeling by myeloid-derived suppressor cells (MDSCs) [19]. Metastasis-associated macrophages (MAMs) facilitate extravasation and outgrowth through VEGF expression and other trophic factors [18].
Advanced Research Methodologies for TME Investigation
Experimental Models and Mathematical Frameworks
Table 2: Key Research Reagent Solutions for TME Investigation
| Category | Specific Reagents/Assays | Research Application | Key Insights Enabled |
|---|---|---|---|
| Single-Cell Omics | scRNA-seq (10x Genomics) [21] | Cellular heterogeneity mapping in TME | Identification of 55 distinct cell states in glioma TME [21] |
| EcoTyper computational framework [21] | Cell state and ecosystem discovery from bulk data | Deconvolution of cellular communities in bulk transcriptomes [21] | |
| Spatial Profiling | Multiplex immunofluorescence (mIHC) [20] | Simultaneous detection of multiple markers (CD8, CD68, PD-L1, etc.) | TME classification into immune-rich, intermediate, and scarce phenotypes [20] |
| Digital pathology/AI-based analysis [22] | Automated quantification of TME features from histology | Identification of TME-derived digital biomarkers predicting metastasis [22] | |
| Molecular Imaging | PET radiotracers (e.g., [18F]FDG) [23] | Metabolic imaging of tumor lesions | Whole-body assessment of tumor burden and heterogeneity [23] |
| Targeted PET ligands (e.g., immune cell markers) [23] | Specific molecular targeting of TME components | Visualization of immune cell distribution and checkpoint expression [23] | |
| Mathematical Modeling | Reaction-diffusion equations [24] | Quantifying cell dynamics and interactions in TME | Simulation of tumor-immune interactions and immunoediting phases [24] |
Detailed Methodological Protocols
Single-Cell RNA Sequencing for TME Deconstruction
Protocol Purpose: To comprehensively characterize cellular heterogeneity and identify novel cell states within the TME [21].
Workflow:
- Tissue Processing: Dissociate fresh tumor samples into single-cell suspensions using enzymatic digestion (collagenase/hyaluronidase cocktail) with viability maintained >80% [21].
- Cell Quality Control: Filter out low-quality cells using criteria: <500 or >10,000 genes detected, >10% mitochondrial gene content [21].
- Library Preparation: Use 10x Genomics platform to capture cells and barcode transcripts. Target cell recovery: 5,000-10,000 cells per sample [21].
- Bioinformatic Analysis: Process data using Seurat v4. Normalize with 'NormalizeData' function, identify highly variable genes ('FindVariableFeatures'), perform dimensionality reduction (PCA, UMAP), and cluster cells ('FindClusters') [21].
- Cell State Identification: Apply Non-negative Matrix Factorization (NMF) to transformed gene expression matrices to identify distinct cell states. Validate state stability using co-occurrence coefficient threshold of 0.95 [21].
Expected Outcomes: This approach identified 55 distinct cell states in glioma, with each major cell type (e.g., macrophages, T cells, cancer cells) exhibiting 2-8 sub-states with unique functional programs [21].
Multiplex Immunofluorescence for Spatial TME Profiling
Protocol Purpose: To simultaneously quantify multiple cell types and phenotypic markers while preserving spatial context in the TME [20].
Workflow:
- Sample Preparation: Cut 4μm formalin-fixed paraffin-embedded (FFPE) tissue sections. Perform deparaffinization in xylene and rehydration in graded ethanols [20].
- Antigen Retrieval: Use pH9 HIER buffer in a decloaking chamber at 110°C for 10 minutes [20].
- Sequential Staining:
- Block with 3% hydrogen peroxide in Tris-buffered saline with Tween (TBST) for 5 minutes
- Incubate with primary antibody (e.g., CD68, 1:500) for 30 minutes
- Detect with Opal Polymer HRP Ms+Rb and visualize with Opal520 TSA (1:100) for 5 minutes
- Repeat antigen retrieval and staining cycle for additional markers (CD8, PD-L1, CD16, SOX10) with different Opal fluorophores [20]
- Image Acquisition: Scan slides using a multispectral imaging system (e.g., Vectra/Polaris) [20].
- Quantitative Analysis: Use image analysis software to segment tissue into intratumoral and peritumoral regions. Calculate cell densities and phenotypic marker expression [20].
Expected Outcomes: This methodology enabled classification of metastatic melanoma TME into three distinct classes: immune-rich (favorable prognosis), immune-intermediate, and immune-scarce (poor prognosis), with significant predictive value for response to immune checkpoint inhibitors [20].
Therapeutic Implications and Concluding Perspectives
The TME represents a promising therapeutic frontier for combating cancer metastasis. Several targeting strategies have emerged:
Table 3: TME-Targeted Therapeutic Approaches
| Therapeutic Strategy | Molecular Targets | Mechanism of Action | Representative Agents |
|---|---|---|---|
| Imm Microenvironment | PD-1/PD-L1 [16] [20] | Block immune checkpoint, reactivate T cells | Pembrolizumab, Nivolumab [20] |
| CTLA-4 [20] | Enhance T-cell priming and activation | Ipilimumab [20] | |
| CAF Targeting | FAP-directed therapies [16] | Deplete or reprogram CAFs | FAP-targeting CAR-T cells [16] |
| TGF-β signaling [18] | Inhibit CAF activation and ECM production | TGF-β inhibitors [18] | |
| TAM Targeting | CSF-1/CSF-1R [18] | Deplete pro-tumorigenic M2 TAMs | CSF-1R inhibitors [18] |
| CCR2/CCL2 axis [18] | Block monocyte recruitment to tumors | CCR2 antagonists [18] | |
| Vascular Normalization | VEGF/VEGFR [16] [17] | Restructure abnormal tumor vasculature | Bevacizumab, Aflibercept [16] |
| Metabolic Targeting | HIF pathway [17] | Counteract hypoxia-driven malignancy | HIF inhibitors [17] |
| Carbonic anhydrases [17] | Counteract tumor acidosis | CA IX inhibitors [17] |
The TME is increasingly recognized as an indispensable determinant of cancer metastasis, functioning as a dynamic ecosystem that orchestrates each step of the metastatic cascade. Advances in single-cell technologies, spatial profiling, and computational modeling are rapidly decoding the extraordinary complexity of cellular interactions within the TME. Future research directions should focus on understanding the spatial organization of TME components, the dynamic evolution of the TME during therapy, and the development of multi-targeted approaches that simultaneously address multiple TME compartments. As our comprehension of this intricate ecosystem deepens, targeting the TME will undoubtedly yield more effective strategies to combat metastatic cancer, ultimately improving outcomes for cancer patients worldwide.
Cancer metastasis, the process where tumor cells disseminate from the primary site to colonize distant organs, remains the principal cause of cancer-related mortality. This complex, multi-step cascade is orchestrated by intracellular signaling pathways that regulate cell motility, invasion, survival, and adaptation to foreign microenvironments. Among the myriad of molecular networks implicated in metastatic progression, the Wnt/β-catenin and PI3K/Akt/mTOR pathways stand out as central regulators. However, beyond these well-characterized pathways, several additional signaling axes—including RAS/RAF/MEK/ERK, VEGF/VEGFR, and MAP4K—contribute significantly to the metastatic phenotype. Understanding the intricate mechanisms, crosstalk, and therapeutic targeting of these pathways provides the foundational knowledge required to develop effective strategies against advanced cancer. This review synthesizes current knowledge of these key signaling pathways, emphasizing their roles in metastasis, quantitative dynamics in human cancers, experimental methodologies for their investigation, and emerging therapeutic approaches that target these molecular networks.
Core Signaling Pathways in Metastasis
Wnt/β-Catenin Signaling Pathway
The Wnt/β-catenin pathway, often referred to as the canonical Wnt pathway, is a highly conserved signaling cascade that governs numerous cellular processes including embryonic development, tissue homeostasis, and stem cell maintenance. In the context of cancer, its aberrant activation is a driving force behind tumor initiation, progression, and metastasis [25] [26].
Pathway Mechanism: In the absence of Wnt ligands (the "Wnt-off" state), cytoplasmic β-catenin is constitutively phosphorylated by a destruction complex comprising Adenomatous Polyposis Coli (APC), Axin, Casein Kinase 1α (CK1α), and Glycogen Synthase Kinase 3β (GSK3β). This phosphorylation marks β-catenin for ubiquitination by the E3 ubiquitin ligase β-TrCP and subsequent proteasomal degradation. When Wnt ligands bind to Frizzled (Fzd) receptors and LRP5/6 co-receptors (the "Wnt-on" state), this destruction complex is disrupted. The key effector, β-catenin, accumulates in the cytoplasm and translocates to the nucleus. There, it partners with T-cell factor/lymphoid enhancer factor (TCF/LEF) transcription factors to activate the expression of a plethora of target genes implicated in metastasis, such as c-MYC, Cyclin D1, and matrix metalloproteinases (MMPs) [25] [27] [26].
Role in Metastasis: The Wnt/β-catenin pathway promotes metastasis through multiple mechanisms. It induces Epithelial-Mesenchymal Transition (EMT), a critical early step in metastasis, by upregulating transcription factors like Snail and Slug, thereby enhancing cell motility and invasion. Furthermore, it regulates cancer cell stemness, allowing a subset of cells to acquire self-renewal capacity crucial for colonization at distant sites. The pathway also remodels the tumor microenvironment (TME); for instance, it upregulates Vascular Endothelial Growth Factor (VEGF) to stimulate angiogenesis, creating new vasculature for tumor dissemination. Notably, in non-small cell lung cancer (NSCLC), Wnt/β-catenin signaling activation is directly linked to metastasis and recurrence [27]. Additionally, it contributes to immune evasion by fostering an immunosuppressive TME, often resulting in "cold tumors" that are resistant to immunotherapy [26].
PI3K/Akt/mTOR Signaling Pathway
The Phosphoinositide 3-Kinase (PI3K)/Protein Kinase B (Akt)/Mammalian Target of Rapamycin (mTOR) axis is one of the most frequently dysregulated signaling pathways in human cancers, acting as a master regulator of cell growth, survival, metabolism, and motility [28] [29].
Pathway Mechanism: The pathway is typically activated by upstream signals from Receptor Tyrosine Kinases (RTKs) like EGFR and IGF-1R. Upon activation, the p110 catalytic subunit of PI3K phosphorylates the lipid phosphatidylinositol 4,5-bisphosphate (PIP2) to generate phosphatidylinositol 3,4,5-trisphosphate (PIP3). This lipid second messenger recruits Akt to the plasma membrane, where it is activated by phosphorylation at two key residues (Thr308 by PDK1 and Ser473 by mTORC2). Activated Akt then phosphorylates numerous downstream substrates. A critical downstream effector is the mTOR complex 1 (mTORC1), which is activated when Akt inhibits the TSC1/TSC2 complex. mTORC1 drives protein synthesis, lipid biogenesis, and inhibits autophagy, thereby promoting cell growth and proliferation. The pathway is negatively regulated by the phosphatase PTEN, which dephosphorylates PIP3 back to PIP2 [28] [29] [30].
Role in Metastasis: The PI3K/Akt/mTOR pathway fuels metastatic progression by inhibiting apoptosis and enhancing cancer cell survival under stressful conditions, such as during detachment from the extracellular matrix. It potently stimulates cell proliferation and tumor growth. Furthermore, it regulates metabolic reprogramming, shifting cancer cells toward glycolysis (the Warburg effect) to meet the high energy and biosynthetic demands of rapid growth and invasion. This pathway is also a key modulator of the response to cellular stress and a major contributor to therapy resistance against chemotherapy, targeted therapy, and immunotherapy. Its activation is often associated with accelerated tumor growth and poor patient outcomes [28] [29].
Additional Key Pathways
Beyond Wnt/β-catenin and PI3K/Akt/mTOR, several other pathways play indispensable roles in metastatic dissemination.
RAS/RAF/MEK/ERK Pathway: This mitogen-activated protein kinase (MAPK) pathway is a classic regulator of cell proliferation and is hyperactivated in many cancers, often via mutations in RAS or BRAF. When activated by RTKs or other signals, membrane-bound RAS GTPase activates RAF kinases (ARAF, BRAF, CRAF), which then phosphorylate and activate MEK, which in turn phosphorylates and activates ERK. Activated ERK translocates to the nucleus to regulate transcription factors. In metastasis, this pathway enhances cell cycle progression, cell survival, and expression of proteases that facilitate invasion through the basement membrane and extracellular matrix [31].
VEGF/VEGFR Pathway: This pathway is the principal regulator of tumor angiogenesis, the formation of new blood vessels, which is essential for supplying oxygen and nutrients to growing tumors and providing a conduit for metastatic spread. VEGF-A (the most prominent ligand) binding to its primary receptor VEGFR2 triggers receptor dimerization and autophosphorylation, initiating downstream signaling cascades like PI3K-Akt and RAF-MEK-ERK. This promotes endothelial cell proliferation, survival, migration, and vascular permeability. VEGF-C and VEGF-D, signaling predominantly through VEGFR3, drive lymphangiogenesis, facilitating spread through the lymphatic system, a common route for metastasis in cancers like ovarian cancer [32] [33].
MAP4K Signaling: The MAP4K family (MAP4K1-MAP4K7) acts as upstream regulators of key pathways including JNK, MAPK, and Hippo signaling. These kinases influence diverse cellular processes such as proliferation, migration, and apoptosis. For example, MAP4K1 (HPK1) functions as a negative regulator of T-cell receptor signaling, thereby modulating anti-tumor immunity. MAP4K4, on the other hand, is implicated in cancer cell motility, invasion, and tumor growth. Their diverse roles make them emerging targets for cancer therapy, with inhibitors being explored to enhance T-cell responses against tumors [34].
Table 1: Key Signaling Pathways in Cancer Metastasis
| Pathway | Core Components | Primary Activators/ Mutations | Major Downstream Effectors | Role in Metastasis |
|---|---|---|---|---|
| Wnt/β-Catenin | Wnt, Fzd, LRP5/6, β-catenin, APC, Axin, GSK3β, TCF/LEF | Wnt ligand overexpression, CTNNB1, APC, AXIN mutations | c-MYC, Cyclin D1, MMPs, VEGF, Snail | EMT, stemness, immune evasion, angiogenesis [25] [27] [26] |
| PI3K/Akt/mTOR | PI3K (p110, p85), Akt, mTOR (mTORC1/2), PTEN | PIK3CA, AKT1 mutations; PTEN loss | TSC2, GSK3β, FOXO, S6K, 4E-BP1 | Cell survival, proliferation, metabolic reprogramming, therapy resistance [28] [29] |
| RAS/RAF/MEK/ERK | RAS, RAF, MEK, ERK | KRAS, NRAS, BRAF mutations | c-Fos, c-Jun, c-Myc | Cell cycle progression, proliferation, survival, invasion [31] |
| VEGF/VEGFR | VEGF-A/C/D, VEGFR1/2/3, NRP1/2 | VEGF overexpression, hypoxia | PI3K-Akt, RAF-MEK-ERK | Angiogenesis, lymphangiogenesis, vascular permeability [32] [33] |
| MAP4K | MAP4K1-7 | Overexpression in various cancers | JNK, LATS1/2 (Hippo) | Immune modulation, cell migration, apoptosis [34] |
Quantitative Data and Mutational Landscape
The impact of signaling pathway dysregulation in human cancers is quantifiable through their mutation prevalence and association with clinical outcomes. The PI3K/Akt/mTOR pathway is notably one of the most frequently altered pathways in human cancers, with abnormalities present in approximately 50% of solid tumors [29]. Specific mutations include PIK3CA mutations and PTEN loss, which are common drivers in breast cancer and other malignancies [28] [30]. In hepatocellular carcinoma (HCC), about half of the patients exhibit activated Wnt signaling, frequently accompanied by mutations in CTNNB1 (encoding β-catenin), AXIN, and APC [26]. CTNNB1 gain-of-function mutations are also prevalent in various other cancers, leading to stabilized β-catenin and constitutive signaling [26]. The RAS/RAF/MEK/ERK pathway is heavily implicated, with BRAF mutations being strongly associated with malignancies such as melanoma, thyroid cancer, and colorectal cancer [31]. VEGF expression is a significant prognostic marker; in ovarian cancer, high VEGF levels are linked with advanced disease and poorer survival, and it serves as an independent predictor for malignant ascites formation [33].
Table 2: Prevalence of Pathway Alterations in Human Cancers
| Cancer Type | Wnt/β-catenin Alterations | PI3K/Akt/mTOR Alterations | Other Pathway Alterations |
|---|---|---|---|
| Hepatocellular Carcinoma (HCC) | ~50% have activated signaling; CTNNB1, AXIN, APC mutations [26] | Frequently altered | RAS/RAF mutations common [31] |
| Colorectal Cancer (CRC) | >80% have APC mutations [26] | Common (e.g., PIK3CA mutations) | High frequency of KRAS mutations [31] |
| Breast Cancer | Less frequent | High frequency of PIK3CA mutations and PTEN loss [30] | BRAF mutations less common |
| Ovarian Cancer | Implicated in progression | Commonly activated | High VEGF expression correlated with advanced stage [33] |
| Melanoma | Less frequent | Common | ~50% harbor BRAF mutations [31] |
| Lung Cancer (NSCLC) | Associated with metastasis and recurrence [27] | Abnormal in ~50% of tumors [29] | KRAS and EGFR mutations common |
Experimental Protocols for Pathway Analysis
Studying these complex pathways requires a multifaceted experimental approach. Below is a detailed methodology for investigating the Wnt/β-catenin pathway, which can be adapted for other signaling cascades.
Detailed Protocol: Investigating Wnt/β-catenin Signaling in Vitro
Objective: To assess the activation status of the Wnt/β-catenin pathway in a cancer cell line and investigate the functional consequences of its modulation on metastatic phenotypes.
Materials and Reagents:
- Cell line of interest (e.g., SW480 [CRC with APC mutation] or HEK293T [for high transfection efficiency])
- Recombinant Wnt-3a protein (a canonical Wnt pathway activator)
- Small-molecule inhibitors: e.g., XAV939 (Tankyrase inhibitor, stabilizes Axin and promotes β-catenin degradation) [26]
- siRNA or CRISPR/Cas9 reagents targeting CTNNB1 (β-catenin) or a control sequence
- Antibodies for Western Blot: anti-β-catenin (total), anti-phospho-β-catenin (Ser33/37/Thr41), anti-active-β-catenin (non-phospho Ser33/37/Thr41), anti-c-MYC, anti-Lamin B1 (nuclear marker), anti-α-Tubulin (loading control)
- Antibodies for Immunofluorescence: anti-β-catenin, fluorescently-labeled secondary antibodies, DAPI (for nuclear staining)
- qPCR reagents and primers for target genes (e.g., AXIN2, c-MYC, CCND1)
- Matrigel-coated Transwell inserts (for invasion assay)
- Cell culture plates and standard reagents (DMEM/RPMI, FBS, penicillin/streptomycin)
Methodology:
1. Pathway Modulation and Cell Lysis: - Culture cells in standard conditions. Seed cells in multiple plates for different analyses (protein, RNA, functional assays). - Treatment Groups: - Group 1 (Control): Vehicle-treated cells (e.g., DMSO for inhibitors). - Group 2 (Activation): Stimulate with recombinant Wnt-3a (e.g., 50-100 ng/mL) for 6-24 hours. - Group 3 (Inhibition): Treat with XAV939 (e.g., 5-10 µM) for 24-48 hours. - Group 4 (Genetic Knockdown): Transfect cells with siRNA targeting CTNNB1 using a standard transfection reagent. Include a non-targeting siRNA control. Assay 48-72 hours post-transfection. - After treatment, lyse cells for protein and RNA extraction. For nuclear-cytoplasmic fractionation, use a commercial kit to separate cellular compartments.
2. Analyzing Pathway Activity: - Western Blotting: Resolve 20-30 µg of total, cytoplasmic, and nuclear protein extracts by SDS-PAGE. Transfer to a PVDF membrane and probe with the relevant antibodies. Key observations: - Total β-catenin: May increase with Wnt activation. - Phospho-β-catenin (Ser33/37/Thr41): Should decrease with pathway activation. - Active β-catenin: Should increase with pathway activation. - Nuclear β-catenin: The most critical readout; a clear increase indicates pathway activation. - c-MYC protein: A key downstream target; its level indicates transcriptional output. - Quantitative PCR (qPCR): Extract total RNA, synthesize cDNA, and perform qPCR for canonical target genes like AXIN2 (a direct feedback target) and c-MYC. Normalize to housekeeping genes (e.g., GAPDH, ACTB). A significant upregulation in treated groups indicates pathway activation. - Immunofluorescence: Seed cells on glass coverslips. After treatments, fix, permeabilize, and stain with anti-β-catenin antibody and DAPI. Visualize using a confocal microscope. Pathway activation is indicated by the robust translocation of β-catenin signal from the membrane/cytoplasm to the nucleus.
3. Functional Metastasis Assays: - Invasion Assay: Use Matrigel-coated Transwell chambers. Serum-starve treated/transfected cells and seed them in the top chamber with serum-free medium. Place complete medium with 10% FBS in the lower chamber as a chemoattractant. After 24-48 hours, fix the cells that have invaded through the Matrigel and migrated to the lower side of the membrane, stain them, and count them under a microscope. Inhibition of Wnt signaling is expected to reduce the number of invaded cells. - Proliferation Assay: Perform a colorimetric assay like MTT or CCK-8 at 0, 24, 48, and 72 hours post-treatment/modulation. Monitor the rate of cell proliferation. Pathway inhibition should slow down proliferation.
Data Analysis: Quantify Western blot bands and normalize to loading controls. Graph qPCR data as fold-change relative to the control group. For invasion and proliferation assays, plot the absolute counts or absorbance over time. Perform statistical analyses (e.g., Student's t-test, ANOVA) to determine significance between groups. A comprehensive analysis should demonstrate that Wnt/β-catenin pathway activation (by Wnt-3a) increases nuclear β-catenin, target gene expression, and invasive capacity, while its inhibition (by XAV939 or siRNA) produces the opposite effects.
Table 3: The Scientist's Toolkit: Key Research Reagents for Pathway Analysis
| Reagent Category | Specific Examples | Function/Application in Experiments |
|---|---|---|
| Recombinant Proteins | Recombinant Wnt-3a protein | Activates the canonical Wnt pathway in cell-based assays [25]. |
| Small Molecule Inhibitors | XAV939 (Tankyrase inhibitor), CGX1321 (PORCN inhibitor) [25] [26] | Inhibits Wnt/β-catenin signaling by stabilizing Axin or preventing Wnt secretion. |
| Buparlisib (PI3Ki), MK2206 (AKTi), Sirolimus (mTORi) [29] | Inhibit specific nodes of the PI3K/Akt/mTOR pathway for functional studies. | |
| Vemurafenib (BRAFi), Trametinib (MEKi) [31] | Target the RAF/MEK/ERK pathway in mutation-specific contexts. | |
| Genetic Tools | siRNA, shRNA, CRISPR/Cas9 targeting CTNNB1, PIK3CA, etc. | For stable or transient genetic knockdown/knockout of pathway components [26]. |
| Antibodies for Detection | Anti-β-catenin (total, phospho, active), anti-pAKT (Ser473), anti-pERK | Detect protein levels, phosphorylation (activation), and localization via Western Blot, IF, IHC [26]. |
| Assay Kits | Matrigel-coated Transwell inserts | Standardized system for measuring cell invasion capacity in vitro. |
Pathway Visualization and Crosstalk
The signaling pathways driving metastasis do not operate in isolation. They form a complex, interconnected network characterized by extensive crosstalk, allowing for signal integration and amplification. For instance, the Wnt/β-catenin pathway can upregulate VEGF expression, thereby stimulating the VEGF/VEGFR angiogenic pathway [26]. Conversely, VEGF signaling through VEGFR2 activates the PI3K-Akt and RAF-MEK-ERK pathways in endothelial cells [32]. Furthermore, the PI3K/Akt pathway can cross-talk with the MAPK pathway and influence β-catenin activity through inhibitory phosphorylation of GSK3β, mimicking Wnt signaling. This intricate web of interactions means that targeting a single pathway may be insufficient due to compensatory mechanisms, underscoring the rationale for combination therapies.
Diagram 1: Crosstalk between key signaling pathways driving metastasis. This network illustrates how external signals (Wnt, Growth Factors, VEGF) activate their respective membrane receptors, triggering intracellular cascades (Wnt/β-catenin, PI3K/Akt, RAF/MEK/ERK). Key effectors (β-catenin, Akt, ERK) translocate to the nucleus to regulate gene programs essential for metastatic traits. Critical crosstalk mechanisms, such as Akt-mediated inhibition of GSK3β (linking PI3K to Wnt) and ERK-mediated stabilization of β-catenin (linking MAPK to Wnt), are highlighted, demonstrating the integrated nature of these pathways.
Concluding Perspectives and Future Directions
The intricate dance of metastasis is directed by a symphony of signaling pathways, with Wnt/β-catenin, PI3K/Akt/mTOR, RAS/RAF/MEK/ERK, VEGF/VEGFR, and others playing lead roles. Their frequent dysregulation in cancer, complex crosstalk, and role in driving every step of the metastatic cascade make them prime therapeutic targets. While significant progress has been made in developing inhibitors, particularly for the PI3K and MAPK pathways, challenges remain. These include therapeutic resistance, pathway redundancy, and on-target toxicities due to the pathways' critical roles in normal physiology.
Future directions are focused on overcoming these hurdles. Strategies include the development of next-generation inhibitors with improved specificity and safety profiles, and the rational design of combination therapies that target multiple pathways or nodes simultaneously to prevent resistance [29] [31]. The emergence of novel therapeutic modalities like targeted protein degradation (TPD), including proteolysis-targeting chimeras (PROTACs), offers a promising strategy to completely eliminate oncogenic proteins like β-catenin, potentially overcoming the "undruggable" nature of some targets [26]. Furthermore, integrating pathway inhibitors with immunotherapy is a particularly exciting avenue; for example, combining MAP4K1 inhibition with anti-PD-L1 therapy has shown synergistic effects in enhancing T-cell responses against poorly immunogenic tumors [34]. As our understanding of the deep molecular mechanisms of these pathways continues to evolve, it will undoubtedly pave the way for more effective, personalized therapeutic strategies to halt metastasis and improve outcomes for cancer patients.
Genetic Instability and Epigenetic Reprogramming in Pro-Metastatic Evolution
Tumor metastasis represents the culmination of a complex evolutionary process wherein cancer cells acquire the ability to disseminate from the primary site and colonize distant organs. This pro-metastatic evolution is orchestrated through the dynamic interplay of two fundamental mechanisms: genetic instability that generates diversity and epigenetic reprogramming that enables phenotypic plasticity. While genetic mutations provide the initial oncogenic drivers, the metastatic cascade requires continuous adaptation to diverse microenvironments—a process largely governed by reversible epigenetic modifications. The cooperation between these mechanisms facilitates the acquisition of hallmark metastatic capabilities, including invasion, immune evasion, and metabolic adaptation [35] [36].
The conceptual framework of metastasis has evolved significantly since Stephen Paget's seminal "seed and soil" hypothesis in 1889, which proposed that successful metastasis requires compatible interactions between cancer cells ("seeds") and the microenvironment of distant organs ("soil") [37] [35]. Contemporary research has substantiated this theory by revealing how genetic and epigenetic alterations collectively equip cancer cells to overcome the numerous barriers along the metastatic cascade. This whitepaper synthesizes current molecular insights into how genetic instability and epigenetic reprogramming cooperate to drive pro-metastatic evolution, providing a foundation for developing novel therapeutic strategies aimed at interrupting this process.
Molecular Mechanisms Linking Genetic Instability and Epigenetic Reprogramming
Drivers of Genetic Instability in Metastatic Evolution
Genetic instability manifests through multiple mechanisms that increase mutation rates and generate cellular diversity, providing the raw material for metastatic selection. Key drivers include:
- DNA repair deficiencies: Inactivation of pathways such as homologous recombination (BRCA1/2), mismatch repair, and nucleotide excision repair creates hypermutable states that accelerate the accumulation of pro-metastatic mutations [35].
- Epigenetic modulation of repair systems: Aberrant DNA methylation can silence DNA repair genes like MLH1 and MGMT, while histone modifications alter chromatin accessibility at DNA damage sites, further compounding genetic instability [38] [36].
- Oncogene-induced replication stress: Activated oncogenes like MYC and Cyclin E drive aberrant replication initiation and fork stalling, leading to DNA breakage and chromosomal rearrangements characteristic of advanced cancers [35].
This genetic heterogeneity creates subpopulations with varying metastatic potential, enabling selection for traits conducive to invasion, circulation survival, and colonization.
Epigenetic Reprogramming as a Metastatic Catalyst
Epigenetic mechanisms provide the plasticity necessary for cancer cells to navigate the diverse challenges of the metastatic cascade without permanent genetic alterations. The major epigenetic modalities include:
DNA methylation alterations in metastatic cells exhibit a paradoxical pattern of global hypomethylation coupled with localized hypermethylation at specific promoters. Global hypomethylation activates pro-metastatic genes such as ANO1, enhancing invasion and bone metastasis in prostate cancer, while also promoting chromosomal instability through demethylation of repetitive elements [38] [36]. Conversely, promoter hypermethylation silences tumor suppressor genes including HIN-1, RASSF1A, and CDH13 in breast cancer metastases, with TIMP3 hypermethylation facilitating extracellular matrix degradation through increased MMP activity [38].
Histone modifications dramatically alter chromatin architecture and gene accessibility in metastatic cells. Key modifications include the gain of activating marks such as H4K16Ac and loss of repressive marks including H4K20me3, mediated by histone acetyltransferases (HATs) and demethylases like KDM4/6 [39]. Histone modifiers such as EZH2 (catalytic subunit of PRC2) and KDM5 family members are frequently dysregulated in metastasis, promoting invasive phenotypes through aberrant repression of differentiation programs and cell adhesion genes [38] [40].
Chromatin remodeling complexes, particularly SWI/SNF family members, are recurrently mutated in metastatic cancers. Subunits like BRG1 and BRM reconfigure enhancer-promoter interactions that promote bone tropism, while their loss can drive alternative transcriptional programs conducive to metastasis [38] [39].
Non-coding RNA networks including miRNAs, lncRNAs, and circRNAs function as critical epigenetic regulators. For instance, miR-34a is frequently silenced by promoter hypermethylation in metastatic cells, permitting increased expression of its targets c-MET and SNAIL that drive invasion [36]. Exosomal circIKBKB and lncRNA NORAD circulate systemically to modulate the RANKL/OPG axis, conditioning the bone microenvironment for metastatic colonization [38].
Table 1: Major Epigenetic Alterations in Metastatic Progression
| Epigenetic Mechanism | Molecular Alteration | Functional Consequence | Therapeutic Targeting |
|---|---|---|---|
| DNA Methylation | Global hypomethylation; promoter hypermethylation of HIN-1, RASSF1A, CDH13 | Genomic instability; silencing of tumor suppressors; enhanced invasion | DNMT inhibitors (decitabine, guadecitabine) |
| Histone Modification | EZH2 overexpression; KDM4/6 activation; altered H4K16Ac/H4K20me3 balance | Repression of differentiation genes; enhanced plasticity; activated EMT | EZH2 inhibitors; HDAC inhibitors; KDM1A inhibitors |
| Chromatin Remodeling | SWI/SNF complex mutations (BRG1, BRM); enhancer-promoter reconfiguration | Altered transcriptional programs; bone tropism | BET inhibitors; synthetic lethality approaches |
| Non-coding RNA | miR-34a silencing; NORAD, circIKBKB overexpression | Dysregulated RANKL/OPG axis; enhanced colonization | RNA-targeted therapies; antisense oligonucleotides |
Interplay Between Genetic and Epigenetic Mechanisms
The boundary between genetic and epigenetic regulation is highly permeable, with each influencing the other in metastatic progression. Genetic mutations in epigenetic regulators create widespread epigenetic dysregulation—for example, EZH2 gain-of-function mutations or DNMT3A mutations are common in advanced cancers and drive transcriptional programs favoring invasion and stem-like properties [39]. Conversely, epigenetic alterations can predispose to genetic instability, as seen when hypermethylation silences DNA repair genes or hypomethylation activates transposable elements that cause DNA damage [36].
This reciprocal relationship establishes a self-reinforcing cycle wherein genetic mutations in epigenetic regulators create epigenetic instability, which in turn promotes further genetic alterations. This "vicious cycle" accelerates the evolution of metastatic competency by simultaneously increasing cellular diversity and phenotypic plasticity [38] [39].
Experimental Models and Methodologies for Metastasis Research
In Vivo and In Vitro Metastasis Models
Research into pro-metastatic evolution employs sophisticated experimental models that recapitulate specific stages of the metastatic cascade:
Animal models including patient-derived xenografts (PDX), genetically engineered mouse models (GEMMs), and metastasis assays provide physiologically relevant systems for studying the entire metastatic process. Intracardiac or intraosseous injection models specifically investigate bone metastasis tropism, while intracarotid injection enables study of brain metastasis [38] [35]. These models allow for temporal analysis of metastatic progression and assessment of organ-specific colonization patterns.
3D culture systems such as organoids and spheroids mimic key aspects of the tumor microenvironment, including oxygen and nutrient gradients, cell-cell interactions, and spatial organization. When combined with extracellular matrix components, these models enable investigation of invasion and early dissemination events while allowing precise experimental manipulation [40].
Microfluidic and organ-on-a-chip platforms provide unprecedented control over microenvironmental parameters, enabling real-time observation of metastatic behaviors like extravasation and niche formation under controlled conditions [35].
Molecular Profiling Technologies
Comprehensive molecular profiling technologies are essential for deciphering the genetic and epigenetic alterations driving metastasis:
Genomic approaches including whole-exome sequencing, whole-genome sequencing, and targeted sequencing identify mutations, copy number alterations, and structural variations associated with metastatic progression. Single-cell DNA sequencing resolves intratumoral heterogeneity and traces clonal evolution during metastasis [35] [40].
Epigenomic mapping techniques such as whole-genome bisulfite sequencing (WGBS), ChIP-seq for histone modifications, ATAC-seq for chromatin accessibility, and Hi-C for 3D genome architecture provide comprehensive views of the epigenetic landscape in metastatic cells. These approaches have identified metastatic-specific epigenomic signatures including differentially methylated regions and altered enhancer activities [38] [41].
Multi-omics integration combines genomic, epigenomic, transcriptomic, and proteomic datasets to construct comprehensive molecular networks driving metastasis. This approach has revealed coordinated genetic and epigenetic programs that enable metastatic adaptation to different organ microenvironments [36] [40].
Figure 1: Metastatic Cascade with Genetic and Epigenetic Influences. The diagram illustrates the sequential steps of metastasis, with dashed lines indicating how genetic instability (red) and epigenetic reprogramming (green) influence specific stages.
Functional Validation Approaches
CRISPR-based screening enables genome-scale identification of genetic and epigenetic dependencies for metastatic traits. Pooled in vivo CRISPR screens have identified essential genes for organ-specific colonization, while CRISPRi/a screens pinpoint epigenetic regulators of metastatic phenotypes [41].
Epigenome editing technologies including CRISPRoff/CRISPRon systems allow precise manipulation of epigenetic marks at specific genomic loci. These tools establish causal relationships between epigenetic alterations and metastatic behaviors without permanent genetic changes [41].
Lineage tracing and barcoding techniques track the fate and contribution of different subclones to metastatic lesions, revealing the dynamics of clonal selection during metastatic evolution [35].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Investigating Genetic and Epigenetic Mechanisms in Metastasis
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Epigenetic Editors | CRISPRoff-V2.3 mRNA, CRISPRon (dCas9-TET1) | Locus-specific epigenetic programming; stable gene silencing/activation without DNA damage | Requires CpG island-containing promoters for optimal efficiency; highly specific DNA methylation changes [41] |
| DNMT Inhibitors | Decitabine, Guadecitabine | DNA hypomethylating agents; reverse hypermethylation-induced gene silencing | Global effects require careful interpretation; can reactivate silenced tumor suppressors but may also activate oncogenes [38] [36] |
| HDAC & HMT Inhibitors | Entinostat (HDAC inhibitor), EZH2 inhibitors (GSK126, Tazemetostat) | Modulate histone acetylation/methylation; counteract repressive chromatin states | Context-dependent effects on metastasis; may influence both tumor cells and microenvironment [38] [40] |
| Metastasis-Associated Antibodies | Anti-RANKL, anti-SNAIL, anti-E-cadherin, anti-vimentin | Detect EMT markers; validate metastatic phenotypes; target critical pathways | EMT markers show dynamic expression during metastasis; multiple markers recommended for verification [35] [42] |
| Epigenomic Profiling Kits | Whole-genome bisulfite sequencing kits, ChIP-seq grade antibodies, ATAC-seq kits | Comprehensive epigenetic mapping; identify metastasis-associated epigenetic alterations | Single-cell epigenomic kits enable resolution of heterogeneous cell states in metastatic populations [41] [40] |
| 2-(2-Methylazetidin-2-yl)ethanol | 2-(2-Methylazetidin-2-yl)ethanol | 2-(2-Methylazetidin-2-yl)ethanol is a chemical building block for research. This product is for laboratory research use only and not for human or veterinary use. | Bench Chemicals |
| 2-[(3-Fluorobenzyl)oxy]benzoic acid | 2-[(3-Fluorobenzyl)oxy]benzoic acid|CAS 360778-48-9 | Bench Chemicals |
Signaling Networks and Pathway Visualization in Metastasis
The metastatic process is governed by complex signaling networks that integrate genetic and epigenetic information to coordinate cellular behaviors. Key pathways include:
The RANKL/RANK/OPG axis plays a central role in bone metastasis by coupling tumor cells with the bone remodeling system. Epigenetic regulation of RANKL expression in stromal cells and RANK in tumor cells creates a "vicious cycle" wherein bone resorption releases growth factors that further promote tumor growth [38] [35]. Epigenetic modifiers including EZH2 and histone demethylases regulate this pathway, while non-coding RNAs such as circIKBKB and miR-34a fine-tune its activity.
TGF-β signaling exhibits context-dependent roles in metastasis, initially suppressing tumor growth but subsequently promoting EMT, invasion, and metastatic colonization. The pathway influences epigenetic regulation through SMAD proteins that recruit histone modifiers and DNA methyltransferases to specific genomic loci [38] [35]. Conversely, epigenetic mechanisms control TGF-β pathway activity through methylation of pathway components and modifiers.
Wnt/β-catenin signaling drives metastatic progression through multiple mechanisms, including stemness maintenance, EMT induction, and microenvironment modification. Epigenetic silencing of Wnt antagonists like SFRPs through promoter hypermethylation commonly activates this pathway in metastatic cells [35] [42]. β-catenin also recruits epigenetic regulators to activate pro-metastatic transcriptional programs.
Integrin signaling mediates cell-matrix interactions critical for invasion and colonization of distant organs. Genetic alterations in integrins and their downstream effectors cooperate with epigenetic mechanisms that control integrin expression patterns, enabling adaptation to different tissue microenvironments [35] [42].
Figure 2: Genetic and Epigenetic Regulation of Pro-Metastatic Signaling Networks. Key signaling pathways (red) integrate genetic alterations and epigenetic reprogramming to drive specific metastatic processes (blue), ultimately promoting dissemination and colonization.
Therapeutic Implications and Clinical Translation
Epigenetic Therapies in Metastatic Disease
The reversible nature of epigenetic alterations presents compelling therapeutic opportunities for metastatic cancer:
DNMT inhibitors including decitabine and guadecitabine have shown promise in attenuating osteoclast differentiation and potentially reversing hypermethylation-induced silencing of metastasis suppressor genes. These agents are being evaluated in combination with bisphosphonates or immune checkpoint inhibitors for bone metastasis [38] [36].
HDAC inhibitors display context-dependent effects on tumor progression and bone remodeling. While generally effective in hematological malignancies, their utility in solid tumor metastasis is being explored in combination regimens [38] [40].
EZH2 inhibitors such as tazemetostat and GSK126 target the catalytic subunit of PRC2 that mediates H3K27 trimethylation. These agents have shown particular promise in cancers with EZH2 gain-of-function mutations or SMARCB1 deletions [38] [39].
BET protein inhibitors target bromodomain-containing proteins that "read" acetylated histones, disrupting the transcription of key oncogenes and metastasis drivers. These agents are advancing through early-phase clinical trials, often in combination with other epigenetic therapies [38].
KDM1A inhibitors target histone demethylases that remove repressive marks, potentially reactivating silenced differentiation programs in metastatic cells [38].
Emerging Therapeutic Platforms
CRISPR/dCas9-based epigenome editing offers locus-specific reprogramming potential without permanent genetic alterations. The CRISPRoff and CRISPRon systems enable stable gene silencing or activation through targeted DNA methylation or demethylation, respectively [41]. This approach provides unprecedented precision for modulating specific epigenetic marks driving metastasis while avoiding the global effects of pharmacological inhibitors.
RNA-targeted therapies including antisense oligonucleotides and small molecule RNA binders are being developed to target non-coding RNAs involved in metastatic progression. These approaches could modulate the function of oncogenic lncRNAs, circRNAs, and miRNAs that establish pro-metastatic regulatory networks [38] [36].
Combination strategies that target both genetic and epigenetic vulnerabilities represent the frontier of metastatic cancer treatment. Rational combinations might include PARP inhibitors with DNMT inhibitors in BRCA-deficient cancers, or immune checkpoint inhibitors with HDAC inhibitors to enhance antitumor immunity [42] [40].
Biomarker Development and Clinical Challenges
Epigenetic alterations show promise as biomarkers for predicting metastatic risk and treatment response. DNA methylation patterns in primary tumors may predict metastatic proclivity, with "metastatic methylation signatures" proposed for specific cancers [36] [40]. Hypermethylated gene promoters can serve as blood-based DNA methylation biomarkers in circulating tumor DNA, signaling occult metastatic disease or recurrence [36].
Despite these advances, significant challenges remain in translating epigenetic therapies to metastatic disease. Tumor heterogeneity necessitates sophisticated patient stratification strategies, while the plasticity of epigenetic regulation can lead to adaptive resistance. Furthermore, the complex interplay between genetic and epigenetic mechanisms requires comprehensive diagnostic approaches that capture both dimensions of metastatic evolution [38] [35] [40].
The pro-metastatic evolution of cancer cells represents a dynamic interplay between genetic instability that generates diversity and epigenetic reprogramming that enables adaptive plasticity. This cooperative relationship accelerates the acquisition of metastatic traits by providing both the diversity for selection and the flexibility for rapid adaptation to new microenvironments. Understanding the molecular mechanisms underlying this cooperation provides not only fundamental insights into cancer biology but also novel therapeutic opportunities aimed at interrupting the metastatic process.
Future research directions will likely focus on several key areas: First, single-cell multi-omics technologies will enable unprecedented resolution of the genetic and epigenetic heterogeneity within metastatic populations and their dynamic evolution during disease progression. Second, spatial mapping of epigenetic states within the tissue context will reveal how microenvironmental cues shape and are shaped by the epigenetic landscape of metastatic cells. Third, advanced epigenetic engineering tools with improved specificity and efficiency will facilitate functional dissection of specific epigenetic alterations in metastasis and enable the development of more targeted epigenetic therapies. Finally, computational integration of multidimensional genomic, epigenomic, and transcriptomic data will generate predictive models of metastatic progression and treatment response, ultimately guiding personalized therapeutic strategies.
As our understanding of the genetic and epigenetic dimensions of metastasis deepens, so too will our ability to develop interventions that prevent or reverse this devastating aspect of cancer progression. By targeting the cooperative mechanisms that drive pro-metastatic evolution, we may ultimately transform metastatic cancer from a terminal condition to a manageable disease.
Advanced Models and Translational Strategies for Intervention
The high failure rate of anticancer drugs in clinical trials, often due to weak efficacy or adverse events, underscores a critical deficiency in conventional preclinical models [43]. Traditional two-dimensional (2D) cell cultures and animal models have historically formed the cornerstone of cancer biology research. However, the simplistic 2D environment, characterized by unnatural cell polarity and uniform nutrient exposure, fails to recapitulate the complex tumor microenvironment (TME), leading to distorted gene expression, metabolic profiles, and drug responses [44] [45] [46]. Although animal models provide an in vivo system, they are hampered by species-specific differences, low throughput, high costs, and ethical controversies, with an average concordance rate with human clinical trials that is remarkably low [44] [43].
These limitations have driven the development of advanced models that can more accurately bridge the gap between in vitro studies and human clinical applications. Among these, three-dimensional (3D) culture systems and microfluidic Organ-on-a-Chip (OoC) platforms have emerged as transformative technologies. By mimicking the three-dimensional architecture, cell-cell and cell-matrix interactions, and diffusion gradients of in vivo tumors, these models provide a more physiologically relevant context for studying the deep molecular mechanisms of cancer progression, metastasis, and treatment resistance [44] [47] [46]. The integration of these models with patient-derived cells further positions them as powerful tools for advancing precision oncology and accelerating drug development.
The Rise of Three-Dimensional (3D) Culture Models
Core 3D Model Typologies: Spheroids and Organoids
3D models are primarily categorized into spheroids and organoids, which differ in their cellular origin and functional complexity.
- Spheroids are simple, spherical aggregates of cells that can be derived from cell lines, primary cells, or tissue fragments. They form through self-assembly and are characterized by their multi-layered, compact structure. While they excel at modeling nutrient and oxygen gradients that create proliferative, quiescent, and necrotic zones akin to in vivo tumors, they typically lack specific tissue-like organization or function [47] [46] [48].
- Organoids are more complex structures that are derived from stem cells (embryonic, induced pluripotent, or adult stem cells) or patient-derived tumor cells. They possess the capacity for self-renewal and self-organization, differentiating into multiple cell types to form structures that recapitulate the key architectural and functional aspects of the organ or tumor from which they originate [49] [47]. Patient-derived tumor organoids (PDOs) are particularly valuable as they retain the genetic, phenotypic, and heterogeneity profiles of the parent tumor, making them exceptional tools for personalized drug screening and studying tumor heterogeneity [49] [50].
Methodologies for Generating 3D Cultures
The establishment of robust 3D models relies on scaffold-based and scaffold-free techniques, each with distinct protocols and applications.
Scaffold-Based Techniques: These methods utilize a supportive 3D matrix that mimics the native extracellular matrix (ECM).
- Natural Hydrogels: Materials like Matrigel, collagen, and fibrin are commonly used. They are rich in integrin-binding sites and biological cues that support cell adhesion, proliferation, and differentiation. The protocol involves embedding cells within the hydrogel matrix and culturing them with specialized media to promote 3D growth [49] [48].
- Synthetic Hydrogels: Polymers such as polyethylene glycol (PEG) offer greater control over mechanical properties and biochemical composition but may require functionalization with adhesion peptides (e.g., RGD) to improve cell attachment [48].
Scaffold-Free Techniques: These methods promote cell aggregation without an external scaffold.
- Hanging Drop Method: A cell suspension is dispensed as droplets on the lid of a culture dish. Gravity forces the cells to aggregate at the bottom of the droplet, forming a spheroid [48].
- Low-Adhesion Plates: Multi-well plates coated with non-adherent polymers force cells to aggregate in the center of the well [45] [48].
- Agitation-Based Methods: Bioreactors that maintain constant agitation prevent cells from adhering to the vessel walls, encouraging them to form aggregates in suspension [48].
Microfluidic Organs-on-Chips: Engineering the Tumor Microenvironment
Organ-on-a-Chip technology represents a significant leap forward by integrating microfluidics, 3D cell culture, and tissue engineering to create dynamic, physiologically relevant models [50] [43].
Design Principles and Fabrication
OoC devices are typically fabricated using soft lithography, a process that creates microfluidic channels from the silicone-based polymer polydimethylsiloxane (PDMS). PDMS is optically clear, gas-permeable, and biocompatible, making it ideal for live-cell imaging and culture [43]. The core design principles include:
- Microfluidic Channels: These tiny channels house cells and hydrogels, allowing for precise control over the spatial organization of co-cultures.
- Perfusion Systems: The continuous flow of culture medium through the channels introduces fluid shear stress, enables efficient nutrient delivery and waste removal, and models vascular perfusion and drug delivery in a way static cultures cannot [50] [43].
- Porous Membranes: These often separate adjacent microchannels, allowing for the study of complex biological processes like cancer cell extravasation during metastasis and the interaction between different tissue compartments (e.g., vascular lumen and tumor parenchyma) [43].
Key Applications in Cancer Research
- Studying Metastasis: Metastasis-on-a-chip models have been developed to dissect the multi-step process of cancer spread. For instance, a lung cancer brain metastasis chip with upstream "lung" and downstream "brain" units revealed that intrinsic cellular changes, including enhanced GSH metabolism and inactivated EGFR, are primary drivers of drug resistance in metastatic cells [50]. Similarly, bone-on-a-chip models have shown that osteoblasts and signals like CXCL5/CXCR2 significantly enhance the extravasation and migration of breast cancer cells [50].
- Vascularized Tumor Models: A major innovation is the development of vascularized patient-derived tumor organoid chips. These models feature a stratified, tumor-specific microvascular system, providing a versatile platform for exploring tumor vascular dynamics and the efficacy of anti-angiogenic drugs like bevacizumab [51] [50].
- Drug Screening and Therapy Assessment: The FDA Modernization Act 2.0 (2022) now permits OoC data to serve as sole preclinical evidence for clinical trials, underscoring the technology's predictive power [50]. For example, PDOs have demonstrated over 87% accuracy in predicting patient responses to colorectal cancer treatments [50]. Tumor-on-a-chip models have also been pivotal in overcoming drug resistance, such as in ovarian cancer, where the platform revealed the efficacy of combining bevacizumab and siRNA to overcome carboplatin resistance within a fibrotic microenvironment [51].
Comparative Analysis: Quantitative and Functional Differences
Metabolic and Proliferative Disparities
Quantitative comparisons between 2D and 3D models reveal profound differences in cancer cell behavior. A 2025 study using a microfluidic chip to monitor metabolites daily provided critical insights, summarized in the table below.
Table 1: Quantitative Comparison of 2D vs. 3D Cancer Cell Cultures
| Parameter | 2D Culture Findings | 3D Culture Findings | Biological Implication |
|---|---|---|---|
| Proliferation Rate | High, glucose-dependent; cells stop proliferating and die rapidly under glucose deprivation [45]. | Reduced, less glucose-dependent; cells survive longer under glucose deprivation by activating alternative pathways [45]. | Better models tumor regions with nutrient limitation; reduced proliferation mirrors in vivo growth kinetics. |
| Glucose Consumption (per cell) | Lower [45]. | Higher, indicating fewer but more metabolically active cells [45]. | Recapitulates the heightened metabolic activity of tumors (Warburg effect). |
| Lactate Production | Lower [45]. | Higher, indicating an enhanced Warburg effect [45]. | Reflects the glycolytic phenotype prevalent in many solid tumors. |
| Glutamine Metabolism | Standard consumption [45]. | Elevated consumption under glucose restriction [45]. | Highlights metabolic flexibility and use of alternative nutrient sources in stress conditions. |
| Gene Expression | Altered profiles; does not mimic in vivo state [45]. | Upregulation of genes like CD44, OCT4, SOX2, and ALDH1 [45]. | Promotes a stem-cell-like, drug-resistant phenotype more representative of in vivo tumors. |
| Drug Response (IC50) | Lower, more sensitive [43]. | Higher, more resistant [43]. | More accurately predicts in vivo drug resistance due to diffusion barriers and cellular heterogeneity. |
Choosing the appropriate model depends on the research question, required throughput, and available resources.
Table 2: Strategic Comparison of Preclinical Cancer Models
| Model Type | Key Advantages | Key Limitations | Ideal Applications |
|---|---|---|---|
| 2D Cell Culture | Cost-effective, straightforward, high-throughput, highly reproducible [44]. | Overly simplistic, loses TME complexity and tumor heterogeneity, altered gene expression [44] [46]. | Initial high-throughput drug screening, basic mechanistic studies. |
| Animal Models | Provides a complete living system, partially recapitulates TME, gold standard for in vivo validation [44]. | Expensive, low-throughput, ethically challenging, species-specific differences limit predictive value [44] [43]. | Studying systemic effects, complex immune interactions, final preclinical validation. |
| 3D Spheroids | Simple to generate, model diffusion gradients and basic TME architecture, cost-effective for 3D screening [47] [46]. | Limited tissue complexity, no vascularization, heterogeneity in size and shape [49] [47]. | Studying tumor metabolism, hypoxia, and preliminary drug penetration. |
| Patient-Derived Organoids (PDOs) | Preserves patient-specific tumor heterogeneity, genetics, and drug responses; high predictive accuracy (>87%) [49] [50]. | Lack vascular and immune components (in basic form), technically demanding, can be costly [49] [47]. | Personalized drug screening, biomarker discovery, studying tumor heterogeneity. |
| Organ-on-a-Chip | Recapitulates dynamic TME, vascular perfusion, and multi-organ interactions; high physiological relevance [50] [43]. | Technically complex, low- to medium-throughput, requires specialized expertise and equipment [47] [50]. | Studying metastasis, drug delivery, pharmacokinetics, and complex cell-cell interactions in the TME. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of 3D and OoC technologies requires specific reagents and equipment.
Table 3: Essential Research Reagent Solutions for Advanced Models
| Item Category | Specific Examples | Function in Experiment |
|---|---|---|
| Natural Hydrogels | Matrigel, Collagen I, Fibrin | Provides a biologically active scaffold that mimics the native extracellular matrix for 3D cell growth and organization [49] [48]. |
| Synthetic Hydrogels | Polyethylene Glycol (PEG), Polylactic Acid (PLA) | Offers a defined, tunable scaffold with controllable mechanical properties; often modified with bioactive peptides [48]. |
| Microfluidic Chips | PDMS-based chips with single or multiple channels | Serves as the physical platform for housing cells and hydrogels, enabling perfusion and dynamic control of the microenvironment [50] [43]. |
| Stem Cell Media Supplements | Noggin, R-spondin, EGF, Wnt-agonists | Critical for the establishment and long-term maintenance of patient-derived organoids by mimicking niche signaling pathways [49]. |
| Low-Adhesion Plates | Ultra-low attachment (ULA) spherical plates | Enables scaffold-free formation of spheroids by preventing cell attachment to the well surface [45] [48]. |
| 2,4-Dimethylpentane-1,2-diamine | 2,4-Dimethylpentane-1,2-diamine|C7H18N2|RUO | |
| N-(3-aminopyridin-4-yl)benzamide | N-(3-aminopyridin-4-yl)benzamide|CAS 918550-20-6 | N-(3-aminopyridin-4-yl)benzamide (CAS 918550-20-6), a chemical building block for research. This product is For Research Use Only. Not for human or therapeutic use. |
Experimental Workflow and Signaling Pathways
The following diagram illustrates a generalized, integrated workflow for establishing a vascularized tumor-on-a-chip model to study drug response, incorporating key biological pathways.
Diagram Title: Workflow for Vascularized Tumor-on-a-Chip Modeling
This workflow highlights the convergence of patient-derived materials, microfabrication, and tissue engineering. The molecular pathways depicted are frequently dysregulated in cancer and are critical targets for therapeutic intervention. For instance, the VEGF/VEGFR axis drives angiogenesis, while the CXCL5/CXCR2 axis has been implicated in promoting cancer cell migration during bone metastasis [50]. The EGFR signaling pathway is a classic driver of proliferation and a key target in head and neck cancers [44]. These pathways are not isolated; extensive crosstalk between them contributes to tumor progression and therapy resistance, which can be effectively modeled in these advanced systems.
Innovative preclinical models, including 3D spheroids, patient-derived organoids, and microfluidic Organ-on-a-Chip systems, are fundamentally reshaping cancer research. By providing a more physiologically relevant context that mirrors the structural, biochemical, and dynamic properties of human tumors, these models offer unprecedented insights into the molecular mechanisms driving cancer progression and metastasis. The integration of these platforms with artificial intelligence for data analysis and high-throughput screening holds the promise of further accelerating the discovery of novel therapeutic targets and biomarkers [44].
The future of this field lies in increasing model complexity and standardization. Key directions include the robust integration of immune cells to create a fully functional tumor immune microenvironment, the development of more sophisticated multi-organ systems to study metastatic spread and systemic drug effects, and the establishment of standardized protocols to ensure reproducibility across laboratories [47] [50]. As these technologies continue to mature and gain regulatory acceptance, they are poised to significantly reduce the reliance on animal models, lower drug development costs, and ultimately, pave the way for more effective and personalized cancer therapies.
Targeting Angiogenesis and Lymphangiogenesis with VEGF Inhibitors
The vascular endothelial growth factor (VEGF) signaling pathway represents a master regulatory system controlling both angiogenesis (the formation of new blood vessels) and lymphangiogenesis (the formation of new lymphatic vessels). In the context of cancer biology, this pathway is hijacked by tumors to establish blood supply and facilitate metastatic spread. VEGF ligands and their receptors orchestrate endothelial cell proliferation, migration, and survival, playing a pivotal role in dynamic vascular remodeling within the tumor microenvironment [32]. Dysregulated VEGF signaling drives diverse pathological conditions, with excessive VEGF activity promoting tumor growth, invasion, and metastasis, while also contributing to the development of abnormal, leaky vasculature characteristic of malignant tumors [32] [52].
The critical relationship between angiogenesis and tumor growth was first hypothesized by Judah Folkman in 1971, who proposed that tumor growth is angiogenesis-dependent [32]. This foundational concept has since been validated through decades of research, leading to the development of therapeutic strategies targeting VEGF signaling. The discovery of VEGF by Harold Dvorak's team (initially as vascular permeability factor) and its subsequent isolation by Napoleone Ferrara in 1989 catalyzed the identification of additional VEGF family members and their receptors, unveiling a complex regulatory network that extends beyond simple blood vessel formation to include lymphatic system development and immune modulation [32].
Within the tumor microenvironment, VEGF-mediated pathways control multiple aspects of cancer progression. Tumor cells and stromal cells secrete factors that stimulate both angiogenesis and lymphangiogenesis, resulting in the formation of peri-tumoral lymphatic vessels that often serve as conduits for metastatic spread [53]. The structural characteristics of lymphatic capillaries—including a thin, discontinuous basement membrane, lack of pericyte coverage, and frequent endothelial cell gaps—make them particularly susceptible to invasion by tumor cells, facilitating their journey to regional lymph nodes and beyond [53]. Understanding the deep molecular mechanisms governing VEGF signaling in both vascular and lymphatic endothelial compartments provides the foundation for developing targeted therapeutic interventions aimed at suppressing tumor progression and metastasis.
Molecular Mechanisms of VEGF Signaling
VEGF Ligands and Receptor Interactions
The VEGF family comprises multiple ligands with distinct structural features and receptor binding specificities. The primary members include VEGF-A, VEGF-B, VEGF-C, and VEGF-D, which interact with three tyrosine kinase receptors—VEGFR1, VEGFR2, and VEGFR3—as well as neuropilin (NRP) co-receptors that modulate signaling specificity and intensity [32]. These ligands share a characteristic cystine-knot motif critical for receptor binding and dimerization, but differ significantly in their bioavailability, receptor affinity, and biological functions due to alternative splicing and proteolytic processing [32].
Table 1: VEGF Family Ligands and Their Characteristics
| Ligand | Primary Receptors | Key Isoforms | Structural Features | Biological Functions |
|---|---|---|---|---|
| VEGF-A | VEGFR1, VEGFR2, NRP1 | VEGF-A121, VEGF-A165, VEGF-A189, VEGF-A206 | VEGF homology domain (VHD), heparin-binding domain (HBD) in some isoforms [32] | Angiogenesis, vascular permeability, endothelial cell survival and proliferation [32] |
| VEGF-B | VEGFR1 | VEGF-B167, VEGF-B186 | VHD, heparin-binding or hydrophobic C-terminal domain [32] | Tissue protection, metabolic regulation, minimal angiogenic activity [32] |
| VEGF-C | VEGFR2, VEGFR3 | Full-length (58kDa), processed (21kDa) | Requires proteolytic processing by ADAMTS3/PC for activation [32] | Lymphangiogenesis, angiogenesis, vascular remodeling [32] [54] |
| VEGF-D | VEGFR2, VEGFR3 | Full-length (50kDa), processed (31kDa) | Structural similarity to VEGF-C with unique N- and C-terminal extensions [32] | Lymphangiogenesis, metastatic spread [32] [54] |
VEGF-A exists as multiple isoforms generated through alternative splicing of exons, resulting in proteins with distinct heparin-binding capacities and extracellular matrix retention properties [32]. VEGF-A165, the predominant isoform, features both a receptor-binding domain and a heparin-binding domain, enabling controlled distribution through ECM interactions [32]. In contrast, VEGF-A121 lacks the heparin-binding domain and diffuses more freely but has reduced receptor activation capacity [32]. VEGF-C and VEGF-D undergo sophisticated proteolytic processing to achieve full activation and receptor binding affinity, with their mature forms preferentially activating VEGFR3 to drive lymphangiogenesis [32] [54].
VEGF Receptor Activation and Downstream Signaling
VEGF receptors are transmembrane tyrosine kinases that undergo ligand-induced dimerization and autophosphorylation, initiating downstream signaling cascades that control endothelial cell behavior. VEGFR2 serves as the primary mediator of angiogenic signaling, while VEGFR3 is predominantly involved in lymphangiogenesis, though there is significant crossover in their functions [32] [54].
The following diagram illustrates the core VEGF signaling pathway and its downstream effects:
Figure 1: Core VEGF Signaling Pathway Activation and Cellular Outcomes
Upon VEGF binding, VEGFR2 undergoes dimerization and autophosphorylation at specific tyrosine residues, including Tyr1175, which serves as a docking site for downstream adaptor proteins [32] [52]. This initiates two primary signaling cascades: the MAPK pathway (driving proliferation and migration) and the PI3K-AKT pathway (promoting survival and additional migratory signals) [52]. In physiological conditions, this signaling is transient and tightly regulated; however, in tumor contexts, oncogenic pathways such as RAS-RAF-MEK and PI3K-AKT can lock VEGFR2 in a constitutively activated state, fueling unchecked endothelial proliferation and generating the malformed, leaky vasculature characteristic of tumors [52].
VEGFR3 signaling follows similar principles but demonstrates distinct downstream effectors that preferentially stimulate lymphatic endothelial cell migration and tube formation. The balanced activation of both receptor types and their complex interplay with co-receptors such as neuropilins allows for precise control of vascular versus lymphatic endothelial responses, though this balance is frequently disrupted in cancer [32] [54].
Therapeutic Targeting Strategies
Established VEGF Inhibitors and Their Mechanisms
VEGF-targeted therapies have revolutionized cancer treatment by providing mechanisms to suppress tumor angiogenesis and lymphangiogenesis. These interventions can be broadly categorized into several classes based on their molecular targets and mechanisms of action.
Table 2: Classes of VEGF-Targeted Therapeutics and Their Properties
| Therapeutic Class | Representative Agents | Molecular Targets | Mechanism of Action | Key Clinical Applications |
|---|---|---|---|---|
| Monoclonal Antibodies | Bevacizumab [55] | VEGF-A | Ligand neutralization, prevents receptor binding [32] [55] | Colorectal cancer, NSCLC, ovarian cancer [55] |
| VEGF Traps | Aflibercept, AVT06 (biosimilar) [56] | VEGF-A, VEGF-B, PlGF | Soluble receptor decoy, binds multiple ligands with high affinity [56] | nAMD, metastatic colorectal cancer [54] [56] |
| Tyrosine Kinase Inhibitors | Sunitinib [55] | VEGFR, PDGFR, c-KIT | Intracellular kinase domain inhibition, multi-targeted approach [55] | Renal cell carcinoma, GIST [55] |
| Novel Bispecific Antibodies | BNT327/PM8002 [57], CTX-10726 [58] | VEGF-A + PD-L1/PD-1 | Dual targeting of angiogenesis and immune checkpoint [57] [58] | Investigational for multiple solid tumors [57] [58] |
| Selective Ligand Inhibitors | Sozinibercept [54] | VEGF-C, VEGF-D | Ligand trap specifically targeting lymphangiogenesis drivers [54] | Investigational for nAMD [54] |
Bevacizumab, a humanized monoclonal antibody against VEGF-A, received FDA approval in 2004 for metastatic colorectal cancer, marking the beginning of clinical anti-angiogenesis therapy [55]. It functions by sequestering VEGF-A, preventing its interaction with VEGFR2 and thereby inhibiting downstream signaling. VEGF traps such as aflibercept employ a different strategy, utilizing engineered soluble receptor domains that bind multiple VEGF family members with high affinity, creating a broader inhibition profile [56]. Tyrosine kinase inhibitors like sunitinib target the intracellular kinase domains of VEGF receptors, but their specificity varies, with many agents inhibiting multiple tyrosine kinases simultaneously [55].
Emerging Therapeutic Approaches and Combination Strategies
The limitations of current VEGF-targeted therapies—including resistance development, suboptimal efficacy in certain contexts, and adverse effects—have driven the development of next-generation approaches [32]. Two promising strategies include bispecific antibodies that simultaneously target VEGF and immune checkpoints, and selective inhibitors targeting specific VEGF family members beyond VEGF-A.
BNT327 (PM8002) is an investigational bispecific antibody that combines PD-L1 checkpoint inhibition with VEGF-A neutralization, addressing both immunosuppressive and angiogenic pathways in the tumor microenvironment [57]. Preclinical characterization demonstrates that BNT327 exhibits high binding affinity to both PD-L1 and VEGF-A, efficiently blocking PD-1/PD-L1 and VEGF-A/VEGFR2 interactions simultaneously [57]. This dual mechanism results in anti-tumor activity superior to single PD-1/PD-L1 blockade or anti-VEGF-A treatment alone in multiple tumor models [57]. Similarly, CTX-10726, a tetravalent bispecific antibody targeting PD-1 and VEGF-A, has shown potent immunomodulatory activity and superior anti-tumor efficacy compared to selective VEGF-A inhibition in preclinical models [58].
Another emerging approach involves targeted inhibition of specific VEGF ligands beyond VEGF-A. Sozinibercept, an investigational trap biologic that selectively binds and neutralizes VEGF-C and VEGF-D, has demonstrated promising efficacy in neovascular age-related macular degeneration when combined with standard anti-VEGF-A therapy [54]. This suggests that targeting the VEGF-C/VEGF-D axis may provide additional therapeutic benefits in pathologies involving lymphangiogenesis and vascular remodeling.
Experimental Methodologies for VEGF Research
Pharmacovigilance and Clinical Adverse Event Analysis
Understanding the clinical effects and adverse event profiles of VEGF inhibitors requires systematic analysis of real-world data. The following methodology outlines approaches for evaluating VEGF inhibitor-induced adverse events, such as arthritis, using pharmacovigilance databases:
Figure 2: Pharmacovigilance Analysis Workflow for VEGF Inhibitor Adverse Events
This methodology was employed in a recent study analyzing VEGF(R) inhibitor-induced arthritis [55]. Researchers extracted adverse event data from the FDA Adverse Event Reporting System (FAERS) and VigiBase (WHO's global database), spanning from 2013-2023 and 1968-2023, respectively [55]. Inclusion criteria encompassed adverse drug event reports from cancer patients, with primary suspected medications limited to VEGF inhibitors, VEGFR inhibitors, or standard chemotherapy agents. Reports were deduplicated based on gender, age, reporting country, date, adverse events, and medications [55].
Signal detection employed disproportionality analysis using Reporting Odds Ratio (ROR) and Proportional Reporting Ratio (PRR) methods. Positive signals for VEGF(R) inhibitor-related arthritis adverse events were defined as simultaneously satisfying three conditions: (1) number of ADE reports ≥3 cases; (2) lower limit of the 95% confidence interval for ROR (ROR025) > 1; (3) PRR ≥ 2 and χ² ≥ 4 [55]. Subgroup analyses were conducted based on demographic factors and specific therapeutic agents to identify risk patterns. Clinical validation included assessment of inflammatory markers in cancer patients receiving VEGF(R) inhibitor therapy and transcriptomic analysis of bone tissue in mouse models to investigate molecular mechanisms [55].
Preclinical Evaluation of Novel VEGF-Targeting Agents
The development of novel VEGF-targeting therapies requires comprehensive preclinical assessment utilizing both in vitro and in vivo models. The following experimental approaches are representative of current methodologies:
For bispecific antibodies such as BNT327 and CTX-10726, in vitro characterization typically includes:
- High-affinity binding assays to determine dissociation constants (Kd) for both targets (e.g., VEGF-A and PD-L1) using surface plasmon resonance or similar techniques [57] [58]
- Functional blockade assays measuring dose-dependent inhibition of VEGF-A/VEGFR2 and PD-1/PD-L1 interactions [57] [58]
- Immunomodulatory activity assessment through IFN-γ production assays in co-culture systems with immune and target cells [58]
In vivo evaluation employs multiple tumor models to assess anti-tumor efficacy:
- Human tumor xenograft models (e.g., HCC827 lung cancer xenografts) in immunocompromised mice to evaluate direct anti-angiogenic effects [57] [58]
- Syngeneic tumor models in immunocompetent mice or humanized mouse models (e.g., human PD-1/PD-L1/VEGF-A triple knock-in mice) to assess combined anti-angiogenic and immunomodulatory activity [58]
- Comparative efficacy studies against standard-of-care agents (e.g., bevacizumab) and competitive bispecific antibodies to establish therapeutic advantage [58]
Additional specialized assessments include:
- Histological analysis of tumor vasculature (CD31 staining for blood vessels, LYVE-1 for lymphatic vessels) to quantify vascular normalization and density changes [53]
- Lymph node metastasis models to evaluate anti-lymphangiogenic and anti-metastatic activity [53]
- Transcriptomic analysis of treated tissues (e.g., bone, tumor) using RNA sequencing to identify pathway alterations and potential mechanisms of adverse effects [55]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for VEGF Signaling and Inhibition Studies
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Recombinant VEGF Ligands | VEGF-A165, processed VEGF-C, VEGF-D [32] | Endothelial cell stimulation, receptor binding studies, signaling assays | Consider isoform-specific effects; VEGF-C/D require proper proteolytic processing for full activity [32] |
| VEGF Receptor Assays | Phospho-specific VEGFR2 antibodies, soluble VEGFR extracellular domains [32] | Receptor phosphorylation analysis, ligand-receptor interaction studies | VEGFR2 Tyr1175 phosphorylation is a key activation marker; systemic soluble VEGFR2 as potential biomarker [32] [52] |
| Endothelial Cell Models | Human umbilical vein endothelial cells (HUVEC), lymphatic endothelial cells (LEC) [53] | Angiogenesis assays, lymphangiogenesis studies, permeability measurements | LEC express VEGFR3 and respond preferentially to VEGF-C/D; 3D cultures better mimic physiological conditions [53] |
| Animal Tumor Models | Xenograft models, syngeneic models, genetically engineered models [57] [58] | In vivo efficacy testing, metastasis assessment, toxicology studies | Humanized mouse models enable evaluation of immunomodulatory agents; orthotopic models may better replicate metastatic spread [57] [58] |
| Angiogenesis Assays | Tube formation assay, chick chorioallantoic membrane (CAM) assay, Matrigel plug assay [53] | Functional assessment of angiogenic potential, inhibitor screening | Multiple complementary assays recommended; in vivo assays incorporate complex microenvironmental factors [53] |
| Lymphangiogenesis Markers | LYVE-1, podoplanin, VEGFR3 antibodies [53] | Identification and quantification of lymphatic vessels, metastasis tracking | LYVE-1 is a specific marker for lymphatic endothelium; combined markers improve specificity in pathological tissues [53] |
| 1-Methyl-3-pyrrolidinyl Benzoate | 1-Methyl-3-pyrrolidinyl Benzoate|CAS 13220-17-2 Supplier | 1-Methyl-3-pyrrolidinyl Benzoate (CAS 13220-17-2), a high-purity pharmaceutical intermediate for synthesis. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| Isoquinolin-7-amine dihydrochloride | Isoquinolin-7-amine dihydrochloride, CAS:2172185-59-8, MF:C9H10Cl2N2, MW:217.09 | Chemical Reagent | Bench Chemicals |
Clinical Implications and Future Directions
VEGF-targeted therapies have fundamentally transformed the treatment landscape for multiple cancers, but significant challenges remain. Resistance mechanisms, adaptive bypass signaling pathways, and heterogeneous patient responses continue to limit the efficacy of current approaches [32] [52]. The emergence of novel agents targeting VEGF family members beyond VEGF-A, particularly those involved in lymphangiogenesis (VEGF-C, VEGF-D), represents a promising direction for overcoming these limitations [54].
The integration of VEGF inhibition with complementary therapeutic strategies—particularly immune checkpoint blockade—has demonstrated synergistic anti-tumor activity in preclinical models and is undergoing extensive clinical evaluation [57] [58]. This combination approach addresses both the angiogenic and immunosuppressive components of the tumor microenvironment, potentially breaking cycles of mutual reinforcement that drive tumor progression. Additionally, biomarker-driven patient selection strategies, potentially incorporating VEGF isoform ratios, soluble VEGFR2 levels, or Ang-2 expression, may enable more precise targeting of these therapies to patient subsets most likely to benefit [52].
Beyond oncology, understanding VEGF signaling has important implications for managing treatment-related adverse effects. Recent pharmacovigilance studies have identified significant associations between VEGF(R) inhibitor therapy and inflammatory adverse events such as arthritis, with higher incidence in females and individuals under 65 years [55]. Transcriptomic analyses of bone tissue from VEGF(R) inhibitor-treated mice show altered inflammation-related pathways, providing mechanistic insights into these clinical observations [55]. Such findings highlight the importance of continued monitoring and investigation of VEGF inhibition effects across multiple biological systems to optimize therapeutic efficacy while minimizing adverse outcomes.
As research continues to unravel the complexity of VEGF signaling in both physiological and pathological contexts, the development of increasingly sophisticated targeting strategies holds promise for improved patient outcomes across multiple disease states, particularly in advanced cancers where angiogenesis and lymphangiogenesis drive progression and metastasis.
Leveraging Immune Checkpoint Inhibitors (PD-1/PD-L1) to Reverse Immunosuppression
Immune checkpoint inhibitors (ICIs) targeting the PD-1/PD-L1 axis represent a paradigm shift in cancer therapy, designed to reverse tumor-induced immunosuppression and reactivate anti-tumor immunity. Despite remarkable clinical success, therapeutic efficacy remains limited by primary and acquired resistance mechanisms. This in-depth technical guide explores the sophisticated molecular machinery of PD-1/PD-L1 signaling, delineates the multifaceted mechanisms of immune resistance within the tumor microenvironment (TME), and outlines advanced experimental approaches for developing novel combination strategies. We integrate the latest preclinical and clinical evidence to provide researchers and drug development professionals with a comprehensive framework for advancing next-generation immunotherapies that effectively overcome immunosuppressive barriers in cancer.
The programmed death protein 1 (PD-1, CD279) and its primary ligand PD-L1 (CD274) constitute a critical immune checkpoint pathway that tumors exploit to evade host immune surveillance. Under physiological conditions, this interaction maintains peripheral tolerance and prevents autoimmunity. However, in the TME, persistent antigen exposure leads to sustained PD-1 expression on T cells, while inflammatory signals upregulate PD-L1 on tumor and myeloid cells [59] [60]. This results in T-cell exhaustion, characterized by impaired effector function, proliferative capacity, and cytokine production. Blockade of this pathway with monoclonal antibodies restores T-cell activity and enhances anti-tumor immunity, demonstrating profound clinical benefits across diverse malignancies [60].
The molecular regulation of PD-1/PD-L1 is complex, involving genetic, epigenetic, post-transcriptional, and post-translational mechanisms. Cancer cells manipulate this pathway through various strategies, including genomic alterations, promoter hypomethylation, microRNA dysregulation, and protein stability modifications [60]. Understanding these regulatory networks is essential for developing strategies to overcome resistance and expand the therapeutic efficacy of ICIs.
Molecular Mechanisms of PD-1/PD-L1-Mediated Immunosuppression
Intracellular Signaling and T-Cell Inhibition
The immunosuppressive function of PD-1 primarily operates through the SHP-2 phosphatase-mediated disruption of T-cell activation signals. Upon PD-1 engagement with PD-L1, phosphorylation of the ITSM and ITIM tyrosine motifs in PD-1's cytoplasmic tail recruits and activates SHP-2 [60]. The activated SHP-2 then dephosphorylates key signaling molecules in the TCR and CD28 pathways. Critical targets include:
- CD3ζ chain and ZAP70 in the TCR signalosome, attenuating proximal TCR signaling.
- CD28, a crucial co-stimulatory receptor, reducing PI3K/Akt activation and metabolic reprogramming essential for T-cell function [60].
This coordinated dephosphorylation ultimately leads to:
- Cell cycle arrest and reduced clonal expansion
- Impaired cytokine production (e.g., IL-2, IFN-γ, TNF-α)
- Metabolic dysregulation through inhibition of glycolysis and aerobic metabolism
- Altered differentiation toward exhausted T-cell states [60]
Non-Canonical Functions and Regulatory Mechanisms
Beyond T-cell inhibition, PD-1/PD-L1 interactions influence multiple cellular processes:
- Cellular migration: PD-1 signaling regulates T-cell trafficking across endothelial barriers via PI3K/Akt-dependent mechanisms [60].
- Memory formation: The pathway impacts the development and maintenance of tissue-resident memory T cells [60].
- Metabolic adaptation: Tumor cell-intrinsic PD-L1 signaling can promote resistance to metabolic stress through mTOR activation [60].
- Stem cell function: PD-L1 expression in mammary stem cells facilitates tissue development and regeneration, suggesting broader physiological roles beyond immunity [60].
Mechanisms of Resistance to PD-1/PD-L1 Blockade
Resistance to ICI therapy is categorized as primary (de novo) or acquired, with overlapping mechanisms involving tumor-intrinsic and -extrinsic factors [59].
Tumor-Intrinsic Resistance Mechanisms
Defective Antigen Presentation and Recognition
- MHC-I Downregulation: Mutations in β2-microglobulin (β2M) prevent proper MHC-I complex assembly and surface expression, rendering tumor cells invisible to CD8+ T cells [59].
- Epigenetic Silencing: Hyper methylation of antigen processing machinery genes (e.g., TAP, proteasome subunits) and MHC-I components further disrupts antigen presentation [59].
- Low Mutational Burden: Tumors with low neoantigen load (e.g., prostate, pancreatic cancers) fail to elicit sufficient T-cell infiltration and activation [59].
Alternative Checkpoint Activation and Signaling Pathways
- Compensatory Checkpoints: Upregulation of alternative inhibitory receptors (LAG-3, TIM-3, TIGIT) maintains T-cell exhaustion despite PD-1/PD-L1 blockade [61].
- Oncogenic Signaling: β-catenin/Wnt pathway activation drives T-cell exclusion through reduced CCL4 chemokine production and impaired dendritic cell recruitment [59]. Similar mechanisms involve PI3K-Akt, RAS-MAPK, and MYC signaling networks.
Table 1: Tumor-Intrinsic Resistance Mechanisms and Functional Consequences
| Resistance Mechanism | Key Molecular Alterations | Impact on Anti-Tumor Immunity |
|---|---|---|
| Defective Antigen Presentation | β2M mutations, MHC-I loss, TAP deficiency | Impaired tumor recognition by CD8+ T cells |
| Epigenetic Silencing | Promoter hypermethylation of antigen processing genes | Reduced tumor immunogenicity |
| Low Neoantigen Burden | Minimal somatic mutations, few immunogenic antigens | Inadequate T-cell priming and activation |
| T-cell Exclusion | Wnt/β-catenin activation, reduced CCL4 | Impaired T-cell and dendritic cell infiltration |
| Alternative Checkpoints | Upregulation of LAG-3, TIM-3, TIGIT | Sustained T-cell exhaustion despite PD-1 blockade |
Tumor-Extrinsic Resistance Mechanisms
Immunosuppressive Cellular Networks
- Myeloid-Derived Suppressor Cells (MDSCs): These cells expand dramatically in tumor-bearing hosts and utilize multiple suppressive mechanisms:
- Metabolic Disruption: Production of arginase-1 depletes L-arginine, while iNOS generates nitric oxide, collectively impairing T-cell receptor signaling and promoting apoptosis [62].
- Reactive Oxygen Species: PMN-MDSCs produce peroxynitrite, which nitrates TCRs and chemokines, disrupting T-cell migration and function [62].
- Checkpoint Expression: MDSCs express PD-L1, enabling direct suppression of T-cells through PD-1 engagement [62].
- Regulatory T Cells (Tregs): PD-1/PD-L1 signaling enhances Treg suppression and stability while inhibiting effector T-cell function [60].
- Tumor-Associated Macrophages (TAMs): MDSCs promote M2 macrophage polarization, further reinforcing an immunosuppressive TME [62].
Metabolic and Spatial Constraints
The TME creates metabolic competition through nutrient depletion (glucose, tryptophan, arginine) and accumulation of waste products (lactate, kynurenines). Hypoxia induces HIF-1α, driving PD-L1 expression and enhancing immunosuppressive functions of MDSCs and TAMs [62]. Spatial architecture of tumors also impacts ICI efficacy, with excluded or stromal-barricaded T-cells showing reduced cytotoxicity compared to infiltrated patterns [63].
Table 2: Cellular Mediators of Tumor-Extrinsic Resistance
| Cell Population | Suppressive Mechanisms | Impact on ICI Response |
|---|---|---|
| MDSCs | Arg-1, iNOS, ROS production; PD-L1 expression; Treg induction | Correlates with ICI resistance; depletes essential T-cell nutrients |
| Tregs | IL-10, TGF-β secretion; CTLA-4 expression; metabolic competition | Inhibits effector T-cell function; limits therapeutic activation |
| M2 Macrophages | Immunosuppressive cytokines; tissue remodeling; angiogenesis promotion | Creates barrier to T-cell infiltration and function |
| Cancer-Associated Fibroblasts | Physical barriers; ECM remodeling; chemokine sequestration | Excludes T-cells from tumor islets; limits drug penetration |
Experimental Models and Methodologies
Preclinical Models for ICI Mechanism and Resistance Studies
In Vivo Tumor Models
- Syngeneic Mouse Models: Immunocompetent mice implanted with murine tumor cells (e.g., MC38, B16, CT26) enable evaluation of ICI efficacy and immune correlates of response.
- Genetically Engineered Mouse Models (GEMMs): Spontaneous tumor models with intact immune systems recapitulate tumor-immune evolution and editing.
- Humanized Mouse Models: NSG mice engrafted with human hematopoietic stem cells or PBMCs support human immune cell reconstitution and evaluation of human-specific ICIs [64].
In Vitro and Ex Vivo Systems
- 3D Organoid-PBMC Co-cultures: Patient-derived organoids co-cultured with autologous PBMCs model human-specific tumor-immune interactions and ICI effects [64].
- Air-Liquid Interface Cultures: Recreate tissue-specific architecture for studying irAEs in epithelial tissues [64].
- Microfluidic Devices: "Organ-on-a-chip" platforms enable spatial-temporal analysis of immune cell trafficking and function.
Protocol: Organoid-PBMC Co-culture for ICI Screening
Purpose: Evaluate tumor-immune interactions and ICI efficacy using patient-derived systems.
Materials:
- Patient-derived tumor organoids
- Autologous PBMCs isolated via Ficoll density gradient centrifugation
- Anti-PD-1/PD-L1 neutralizing antibodies (e.g., nivolumab, pembrolizumab, atezolizumab)
- Advanced DMEM/F12 culture medium supplemented with growth factors
Procedure:
- Organoid Generation: Digest tumor tissue enzymatically, embed in Matrigel, and culture in tissue-specific medium with Wnt3a, R-spondin, Noggin, and growth factors.
- PBMC Isolation: Collect peripheral blood, separate mononuclear cells via density gradient centrifugation, and cryopreserve until use.
- Co-culture Establishment: Seed organoids in 96-well plates, add activated PBMCs at 10:1 effector:target ratio, and treat with ICIs (10μg/mL).
- Endpoint Analysis:
- Viability: Measure organoid metabolism using CellTiter-Glo 3D.
- Cytotoxicity: Quantify caspase-3/7 activation and LDH release.
- Cytokine Profiling: Analyze supernatant for IFN-γ, IL-6, IL-1β, TNF-α via Luminex.
- Imaging: Fix and stain for CD8, Granzyme B, PD-1, PD-L1, and Ki67.
Applications: Preclinical drug screening, biomarker discovery, and patient stratification strategies.
Strategic Approaches to Overcome Resistance
Rational Combination Therapies
Enhancing Tumor Immunogenicity
- Epigenetic Modulators: DNMT inhibitors (azacitidine) and HDAC inhibitors (vorinostat) upregulate tumor antigen presentation, MHC expression, and Th1-type chemokines, priming tumors for ICI response [59].
- Targeted Therapies: Zanzalintinib (VEGFR, MET, TAM kinase inhibitor) reverses immunosuppression and, when combined with atezolizumab, significantly improves overall survival in metastatic colorectal cancer (10.9 vs. 9.4 months, HR 0.80) [65].
Counteracting Immunosuppressive Cells
- MDSC-Targeted Approaches:
- Checkpoint Blockade: Targeting novel MDSC checkpoints (e.g., IL-1β, TNF-α, PGE2 pathways) [62].
- Differentiation Agents: All-trans retinoic acid promotes MDSC differentiation into mature dendritic cells and macrophages.
- Recruitment Inhibitors: CCR2 and CXCR2 antagonists block monocytic and granulocytic MDSC trafficking to tumors [62].
Oncolytic Viruses and Vaccines
Intralesional talimogene laherparepvec (T-VEC) combined with pembrolizumab enhances T-cell infiltration and significantly improves response rates in melanoma (62% ORR, 33% CR) [59]. Neoantigen vaccines prime de novo T-cell responses against tumor-specific epitopes.
Clinical Evidence for Combination Strategies
Table 3: Clinical Trial Outcomes of Selected ICI Combination Therapies
| Trial/Phase | Cancer Type | Intervention | Key Efficacy Outcomes | Reference |
|---|---|---|---|---|
| STELLAR-303 Phase 3 | Metastatic Colorectal Cancer | Zanzalintinib + Atezolizumab vs. Regorafenib | mOS: 10.9 vs. 9.4 mo (HR 0.80); mPFS: 3.7 vs. 2.0 mo | [65] |
| KEYNOTE-189 Phase 3 | NSCLC | Pembrolizumab + Carboplatin/Pemetrexed | Improved OS (HR 0.49) and PFS (HR 0.52) | [66] |
| IMpassion130 Phase 3 | Metastatic TNBC | Atezolizumab + nab-Paclitaxel | Improved PFS (HR 0.62) and OS (HR 0.67) in PD-L1+ | [66] |
| AtezoTRIBE Phase 2 | Metastatic Colorectal Cancer | Atezolizumab + FOLFOXIRI + Bevacizumab | Improved PFS (HR 0.69) | [66] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating PD-1/PD-L1 Biology
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Anti-PD-1 Antibodies | Nivolumab, Pembrolizumab (clinical); RMP1-14 (mouse) | ICI efficacy studies; immune cell functional assays | Mouse cross-reactivity varies; validate species specificity |
| Anti-PD-L1 Antibodies | Atezolizumab, Durvalumab (clinical); 10F.9G2 (mouse) | Blockade experiments; immunohistochemistry | Different clones may recognize distinct epitopes and domains |
| PD-1/PD-L1 Binding Assays | Biolayer interferometry; ELISA; SPR | Compound screening; affinity measurements | Use recombinant human/mouse proteins; consider glycosylation |
| Recombinant Proteins | hPD-1-Fc, hPD-L1-Fc (extracellular domains) | Binding studies; T-cell activation assays | Fc portions may cause non-specific binding in some assays |
| Multicolor Flow Cytometry Panels | CD3, CD4, CD8, CD45, PD-1, TIM-3, LAG-3, Ki67 | Immune phenotyping; exhaustion marker assessment | Include viability dye; titrate antibodies; use compensation beads |
| Phospho-Specific Antibodies | pSHP-2, pZAP70, pCD3ζ | Signaling studies by Western blot, phospho-flow | Require rapid fixation; optimize permeabilization conditions |
| 4-Nitropyridine-2-sulfonyl fluoride | 4-Nitropyridine-2-sulfonyl Fluoride|CAS 2090446-25-4 | Research-grade 4-Nitropyridine-2-sulfonyl fluoride for antibiotic development. This product is For Research Use Only (RUO). Not for personal or diagnostic use. | Bench Chemicals |
| 2-bromoethyl N,N-dimethylcarbamate | 2-bromoethyl N,N-dimethylcarbamate, CAS:82524-20-7, MF:C5H10BrNO2, MW:196.044 | Chemical Reagent | Bench Chemicals |
Signaling Pathway Visualization
Diagram 1: PD-1/PD-L1 inhibitory signaling in T cells. The engagement of PD-1 with its ligand PD-L1 recruits SHP-2 phosphatase, which dephosphorylates key signaling molecules in both the TCR (CD3ζ, ZAP70) and CD28 co-stimulatory (PI3K/Akt) pathways. This results in suppressed T-cell proliferation, cytokine production, and metabolic reprogramming.
Diagram 2: Multifaceted mechanisms of resistance to PD-1/PD-L1 blockade. Resistance arises from tumor-intrinsic factors (impaired antigen presentation, low immunogenicity, alternative signaling) and tumor-extrinsic components (immunosuppressive cellular networks, metabolic constraints). These mechanisms often interact synergistically within the TME.
The strategic targeting of PD-1/PD-L1 to reverse cancer-associated immunosuppression has fundamentally transformed oncology therapeutics. However, the complexity of resistance mechanisms demands sophisticated, multi-faceted approaches. Future advances will require:
- Spatiotemporal profiling of the TME using single-cell and spatial transcriptomics to decipher dynamic immune evasion programs [63].
- Rational combination therapies that simultaneously target multiple resistance pathways while minimizing toxicity [62] [65].
- Advanced biomarker development beyond PD-L1 IHC, incorporating mutational burden, immune gene signatures, and MDSC frequencies to guide patient selection [67] [62].
- Novel ICI sequencing strategies, as evidenced by recent real-world data showing that ICIs continuation beyond progression can provide survival benefit in SCLC (2L-OS: 8.66 vs 7.90 months, P=0.016) [68].
The continued elucidation of PD-1/PD-L1 biology and resistance mechanisms at molecular, cellular, and systems levels will enable researchers and drug developers to create increasingly effective immunotherapeutic strategies that overcome immunosuppressive barriers across diverse cancer types.
CRISPR and Single-Cell Sequencing for Target Discovery and Validation
The integration of CRISPR-based gene editing with single-cell sequencing technologies is redefining the landscape of oncological research and therapeutic development. This powerful synergy provides an unprecedented platform for systematically identifying and validating the deep molecular mechanisms that drive cancer progression and metastasis. By enabling high-resolution functional genomics at single-cell resolution, researchers can now move beyond associative studies to establish direct causal links between genetic perturbations, transcriptional programs, and phenotypic outcomes within complex tumor ecosystems [69] [70]. This technical guide examines the current methodologies, applications, and experimental frameworks that combine these technologies to uncover novel therapeutic targets and resistance mechanisms in cancer.
CRISPR screening technology accelerates therapeutic target identification and drug discovery by providing a precise and scalable platform for functional genomics [71]. The development of extensive single-guide RNA (sgRNA) libraries enables high-throughput screening (HTS) that systematically investigates gene-drug interactions across the entire genome [71]. When coupled with single-cell readouts, this approach allows researchers to dissect tumor heterogeneity with remarkable resolution while simultaneously mapping the genetic dependencies that underlie cancer vulnerability [70] [72]. This technical synergy has found broad applications in identifying drug targets for various cancers and plays a crucial role in elucidating drug mechanisms of action and facilitating targeted therapy development [71].
Technological Foundations
CRISPR Systems for Functional Genomics
The CRISPR-Cas system has evolved from a simple gene-editing tool to a sophisticated functional genomics platform. The system comprises two essential components: the Cas nuclease, which induces targeted DNA breaks, and a guide RNA (gRNA) that directs Cas to specific genomic loci [69]. DNA cleavage triggers repair mechanisms, primarily non-homologous end joining (NHEJ), which often introduces insertion or deletion mutations (indels) that result in frameshifts and effectively disrupt gene function [70]. This property has facilitated the widespread use of CRISPR-Cas9-based knockout screens to efficiently identify genetic determinants of cancer phenotypes [69].
The CRISPR toolkit has expanded significantly beyond standard knockout approaches:
- CRISPR interference (CRISPRi): Nuclease-dead Cas9 (dCas9) fused to transcriptional repressors like KRAB enables gene silencing without DNA cleavage [69]
- CRISPR activation (CRISPRa): dCas9 fused to activator domains (VP64, VPR, SAM) enables targeted gene activation [69]
- Base editing: Cas9 variants fused to deaminase enzymes enable precise nucleotide conversions without double-strand breaks [70]
- Prime editing: Cas9-reverse transcriptase fusions enable targeted insertions, deletions, and all possible base-to-base conversions [70]
- CRISPR-Cas13: RNA-targeting systems enable specific degradation of mRNA transcripts [69]
These advanced CRISPR systems have broadened the scope of perturbomic studies to include non-coding regions, epigenetic modifications, and precise mutation modeling, thereby enabling more comprehensive functional annotation of cancer genomes [69] [70].
Single-Cell Sequencing Modalities
Single-cell technologies resolve cellular heterogeneity by profiling individual cells across multiple molecular layers:
- Single-cell RNA sequencing (scRNA-seq): Enables unbiased characterization of gene expression programs, identification of rare cell types, and reconstruction of developmental trajectories [73]
- Single-cell ATAC-seq (scATAC-seq): Maps chromatin accessibility landscapes to identify regulatory elements and transcription factor binding sites [73]
- Single-cell proteomics: Quantifies protein abundance using antibody-based methods (CITE-seq, ECCITE-seq) providing crucial phenotypic information [74] [73]
- Multi-omics integration: Combined modalities (G&T-seq, SIDR-seq, DNTR-seq) enable correlated analysis of genomic, transcriptomic, and proteomic features within the same cell [73]
Recent technological advances have significantly enhanced the sensitivity and scalability of these approaches. Platforms such as 10x Genomics Chromium X and BD Rhapsody HT-Xpress now enable profiling of over one million cells per run with improved sensitivity and multimodal compatibility [73]. Methods like single-cell CRISPRclean (scCLEAN) further improve resolution by using CRISPR/Cas9 to remove highly abundant transcripts from sequencing libraries, thereby redistributing sequencing reads toward less abundant but biologically distinct molecules [75].
Table 1: Single-Cell Sequencing Technologies and Applications
| Technology | Molecular Target | Key Applications in Cancer Research | Throughput |
|---|---|---|---|
| scRNA-seq | mRNA transcriptome | Cell type identification, trajectory inference, differential expression | High (10,000-1,000,000+ cells) |
| scATAC-seq | Accessible chromatin | Regulatory element mapping, TF activity inference | Medium to High |
| CITE-seq | Surface proteins + transcriptome | Immune profiling, cell state validation | Medium to High |
| scTCR/BCR-seq | Immune receptor sequences | Clonality analysis, antigen specificity | Medium |
| Spatial transcriptomics | mRNA with spatial context | Tumor microenvironment architecture | Low to Medium |
Integrated Experimental Frameworks
Core Workflow for Target Discovery
The integration of CRISPR screening with single-cell sequencing follows a structured workflow that enables systematic target identification and validation:
Diagram 1: Integrated CRISPR-single-cell screening workflow for target discovery.
In Vivo Single-Cell CRISPR Screening
Advanced screening approaches now enable functional genomics directly in physiological contexts. In vivo single-cell CRISPR screening combines ultrasound-guided in utero lentiviral microinjections, single-cell RNA sequencing, and guide capture to longitudinally monitor clonal expansions and document their underlying gene programmes at single-cell resolution [72]. This approach was used to systematically investigate tissue-wide clonal dynamics of 150 frequently mutated squamous cell carcinoma genes, revealing distinct tumor necrosis factor (TNF) signaling programs in tumor evolution [72].
The experimental protocol for in vivo screening involves:
- Library Design: Select 150-500 genes relevant to the cancer type with 3-5 sgRNAs per gene plus non-targeting controls [72]
- In Utero Delivery: Inject lentiviral sgRNA library into embryonic day 9.5 (E9.5) mouse embryos to infect the surface ectoderm of Cas9-expressing embryos [72]
- Temporal Sampling: Collect tissues at multiple timepoints (e.g., postnatal day 4 and 60) to monitor clonal evolution [72]
- Cell Sorting: Isolate infected cells using FACS based on fluorescent markers (e.g., mCherry) [72]
- Single-Cell Sequencing: Profile cells using scRNA-seq with simultaneous sgRNA capture [72]
- Computational Analysis: Identify enriched/depleted sgRNAs and correlate with transcriptional phenotypes [72]
This approach demonstrated that Notch1, Fat1, and Trp53 mutant clones expand in normal epidermis, and revealed a paracrine TNF signaling module involving macrophages that drives clonal expansions, while cancer cells switch to an autocrine TNF program associated with epithelial-mesenchymal transition [72].
High-Content Screening in Immune Cells
Genome-wide CRISPR screening in primary immune cells represents a powerful approach for immunotherapy target discovery. A recently developed platform called PreCiSE enables pooled retroviral library delivery and Cas9 electroporation in primary human natural killer (NK) cells [76]. This system has been used to systematically interrogate genetic regulators of NK cell fitness and antitumor activity under immunosuppressive conditions.
The optimized protocol for NK cell screening includes:
- NK Cell Isolation: Isolate primary human NK cells from cord blood or peripheral blood [76]
- Library Transduction: Transduce cells with genome-wide sgRNA library (77,736 guides targeting 19,281 genes) using retroviral vectors [76]
- Cas9 Delivery: Electroporate cells with Cas9 protein using optimized pulse codes [76]
- Selection: Apply puromycin selection to eliminate non-transduced cells [76]
- Tumor Challenge: Subject edited NK cells to multiple rounds of tumor cell challenge to model exhaustion [76]
- Phenotypic Sorting: Sort cells based on functional markers (e.g., CD107a degradation) or allow clonal outgrowth [76]
- Sequencing & Analysis: Extract genomic DNA, sequence sgRNA regions, and analyze guide abundance [76]
This approach identified MED12, ARIH2, and CCNC as critical checkpoints regulating NK cell resistance to immunosuppressive pressures, demonstrating that ablation of these genes significantly improved NK cell antitumor activity against multiple treatment-refractory human cancers both in vitro and in vivo [76].
Table 2: Key Screening Approaches in Cancer Research
| Screening Type | Model System | Readout | Key Applications | Case Example |
|---|---|---|---|---|
| In vivo single-cell CRISPR | Mouse models | scRNA-seq + gRNA capture | Clonal evolution, Tumor-microenvironment interactions | Identification of TNF programs in SCC [72] |
| Genome-wide immune cell screening | Primary human NK cells | Bulk sgRNA abundance | Immunotherapy optimization | MED12, ARIH2, CCNC as NK cell enhancers [76] |
| Perturb-seq | Cell lines, organoids | scRNA-seq | Gene regulatory networks, Drug mechanisms | Mapping transcriptional responses to genetic perturbations [77] |
| TF-focused screening | NK cells, T cells | Bulk sgRNA abundance | Transcriptional regulation | PRDM1, RUNX3 as NK cell regulators [76] |
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of integrated CRISPR-single-cell approaches requires carefully selected reagents and tools. The following table summarizes key components of the experimental toolkit:
Table 3: Essential Research Reagents for CRISPR-single-cell Studies
| Reagent Category | Specific Examples | Function | Technical Considerations |
|---|---|---|---|
| CRISPR Libraries | Genome-wide (GeCKO), TF-focused, Custom libraries | Enable parallel perturbation of multiple genes | Ensure high coverage (500x), include non-targeting controls |
| Cas9 Systems | Wild-type Cas9, dCas9-KRAB, dCas9-VPR | DNA cleavage or transcriptional modulation | Optimize delivery method (lentivirus, AAV, protein) |
| Delivery Vectors | Lentivirus, AAV, Lipid nanoparticles (LNPs) | Introduce CRISPR components into cells | Balance efficiency, immunogenicity, packaging capacity |
| Single-Cell Platforms | 10X Genomics, Drop-seq, Smart-seq2 | Partition individual cells for sequencing | Choose based on cell throughput, sequencing depth, cost |
| Cell Sorting Systems | FACS, MACS | Isulate specific cell populations | Antibody quality critical for purity and viability |
| Analysis Tools | Seurat, Monocle, MAGeCK, mixscape | Process sequencing data, identify hits | Computational resources, expertise requirements |
| N-(2-chloroethyl)carbamoyl chloride | N-(2-Chloroethyl)carbamoyl chloride | 15872-02-3 | High-purity N-(2-Chloroethyl)carbamoyl chloride for research. CAS 15872-02-3. A key electrophilic reagent for synthesis. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| 6-Bromoquinoline-8-carbonitrile | 6-Bromoquinoline-8-carbonitrile|CAS 1563017-39-9 | Bench Chemicals |
Data Analysis and Interpretation
Computational Pipelines
The analysis of integrated CRISPR-single-cell data requires specialized computational approaches. A typical pipeline includes:
- Single-Cell Data Processing: Quality control, normalization, batch correction, and cell clustering using tools like Seurat or Scanpy [78] [74]
- sgRNA Assignment: Associate cells with their perturbed genes using CROP-seq, Perturb-seq, or other barcode recovery methods [72]
- Differential Analysis: Identify genes whose perturbation affects cell abundance (differential abundance) or transcriptional state (differential expression) [78] [72]
- Pathway Analysis: Enrichment testing (GSEA, ORA) to map hits to biological processes and signaling pathways [78]
- Network Inference: Reconstruction of gene regulatory networks using WGCNA or similar approaches to identify shared programs [72]
Benchmarking studies have evaluated numerous clustering algorithms for single-cell data, recommending scAIDE, scDCC, and FlowSOM for top performance across transcriptomic and proteomic data types [74]. These tools enable robust cell type identification which is crucial for interpreting perturbation effects in heterogeneous samples.
Visualization and Interpretation
Effective visualization is essential for interpreting complex perturbation data. Key approaches include:
- UMAP/t-SNE plots: Visualize cell states colored by sgRNA identity or perturbation phenotype [72]
- Violin/ridge plots: Display expression changes of key genes across perturbations [78]
- Heatmaps: Show expression patterns of differentially expressed genes [78]
- Trajectory analysis: Pseudotime ordering to model differentiation or progression [78]
Diagram 2: Computational analysis pipeline for CRISPR-single-cell data.
Application in Cancer Mechanism Studies
Dissecting Tumor Heterogeneity
The integration of CRISPR screening with single-cell sequencing has proven particularly powerful for dissecting tumor heterogeneity and plasticity. In triple-negative breast cancer (TNBC), researchers combined DEPMAP CRISPR dependency data with single-cell transcriptomics to identify four tumor dependency genes (TONSL, TIMELESS, RFC3, RAD51) that define a tumor dependency-associated subpopulation (TDAS) with elevated proliferation and metabolic activity [78]. This subpopulation resided at the differentiation terminus of epithelial/tumor cells and was linked to energy metabolism and cell cycle pathways [78]. Patients with high TDAS infiltration abundance were found to be unsuitable for surgery alone and benefited from combined radiotherapy or chemotherapy [78].
The experimental methodology for such studies typically involves:
- Dependency Analysis: Identify tumor dependency genes using CRISPR screening data from DEPMAP [78]
- Bulk Analysis: Validate expression and prognostic significance in TCGA and METABRIC cohorts [78]
- Single-Cell Profiling: Map dependency genes to cell subpopulations using scRNA-seq data [78]
- Trajectory Analysis: Position target populations within differentiation trajectories using pseudotime algorithms [78]
- Therapeutic Screening: Use Connectivity Map (CMAP) to identify potential targeting compounds [78]
- Functional Validation: Perform in vitro assays (colony formation, CCK-8) to confirm gene function [78]
Elucidating Resistance Mechanisms
CRISPR-single-cell approaches have dramatically accelerated the identification of therapy resistance mechanisms. By subjecting cancer cells to drug selection pressure during CRISPR screening, researchers can identify genetic drivers of resistance while simultaneously profiling the associated transcriptional adaptations. This approach has been used to identify resistance mechanisms to targeted therapies, chemotherapy, and immunotherapy across diverse cancer types.
For example, prime-editor-based tiling screens have systematically evaluated the functional impact of EGFR mutations on tyrosine kinase inhibitor resistance, identifying both known and novel resistance variants [69]. Similarly, base editor screens have uncovered MEK1 variants that confer resistance to MEK inhibitors, revealing unexpected resistance mechanisms that inform drug design and combination strategies [69].
Diagram 3: Key applications of CRISPR-single-cell integration in cancer research.
The integration of CRISPR screening with single-cell multi-omics technologies represents a paradigm shift in cancer target discovery and validation. This powerful combination enables researchers to move beyond correlation to causation, systematically linking genetic perturbations to molecular and phenotypic outcomes within relevant physiological contexts. As these technologies continue to evolve, several exciting directions are emerging:
The field is advancing toward more physiologically relevant model systems, including patient-derived organoids and complex coculture systems that better recapitulate the tumor microenvironment [71] [69]. Computational methods are becoming increasingly sophisticated, with machine learning and artificial intelligence approaches being deployed to predict optimal sgRNA designs, integrate multimodal data, and prioritize the most promising therapeutic targets [77] [70]. Delivery technologies are improving with the development of microenvironment-responsive nanoparticles and cell-type-specific vectors that enhance the precision and efficiency of CRISPR component delivery [77].
Looking ahead, the continued convergence of CRISPR screening, single-cell multi-omics, and computational analytics promises to accelerate the development of personalized cancer therapies tailored to the unique genetic and molecular makeup of individual patients' tumors. As these technologies become more accessible and scalable, they will undoubtedly uncover deeper insights into the molecular mechanisms driving cancer progression and metastasis, ultimately leading to more effective and targeted therapeutic interventions.
Therapeutic Applications of Antibody-Drug Conjugates (ADCs) and Nanoplatforms
Antibody-Drug Conjugates (ADCs) represent a transformative class of biopharmaceuticals that combine the precision targeting of monoclonal antibodies with the potent cytotoxicity of small-molecule chemotherapeutic agents [79] [80]. Often described as "biological missiles" or "magic bullets," ADCs are engineered to selectively deliver highly cytotoxic payloads to tumor cells while minimizing damage to healthy tissues, thereby improving the therapeutic index compared to traditional chemotherapy [80] [81]. The conceptual foundation for ADCs was first proposed by Paul Ehrlich over a century ago, but this vision has only been realized in the past two decades with advancements in antibody engineering, linker chemistry, and potent cytotoxic payloads [81]. The year 2000 marked a pivotal milestone with the approval of gemtuzumab ozogamicin for acute myeloid leukemia, establishing the first commercially available ADC [80]. Since then, ADC technology has evolved through multiple generations, with significant improvements in stability, potency, and therapeutic window [79]. As of June 2025, 19 ADCs have gained global regulatory approval for treating various hematological malignancies and solid tumors, with hundreds more in clinical development [80]. This review examines the structural components, mechanisms of action, and therapeutic applications of ADCs within the context of cancer metastasis, while exploring innovative nanoplatform strategies to overcome current limitations in targeted cancer therapy.
Molecular Architecture of ADCs: Core Components and Design Principles
Structural Framework and Component Integration
ADCs comprise three essential elements: a monoclonal antibody serving as the targeting moiety, a potent cytotoxic payload, and a specialized chemical linker that connects these components [79] [80]. The coordinated interaction among these elements is critical to determining the overall therapeutic efficacy, pharmacokinetics, and safety profile of the conjugate [79]. Figure 1 illustrates the basic structure of an ADC and its mechanism of action.
Table 1: Core Components of Antibody-Drug Conjugates
| Component | Key Features | Representative Examples | Function in ADC Design |
|---|---|---|---|
| Antibody | Humanized/human IgG1; High antigen specificity; Extended half-life; Effector functions (ADCC, CDC) | Trastuzumab (anti-HER2); Brentuximab (anti-CD30) | Target recognition and binding; Fc-mediated immune activation; Prolonged circulation |
| Linker | Cleavable (acid-labile, protease-sensitive) or Non-cleavable (thioether); Plasma-stable, Tumor-activatable | mc-VC-PABC (protease-cleavable); SMCC (non-cleavable) | Circulatory stability; Controlled payload release in target cells |
| Payload | High potency (IC50 ~10^-11–10^-9 M); Defined mechanism; Modifiable functional groups | MMAE/MMAF (tubulin inhibitors); Deruxtecan (TOP1 inhibitor); Calicheamicin (DNA damage) | Tumor cell killing; Bystander effect (depending on permeability) |
Antibody Component: Target Selection and Optimization
The antibody moiety serves as the tumor-targeting vector, enabling selective delivery of cytotoxic payloads to malignant cells while sparing normal tissues [79]. Most clinically approved ADCs utilize humanized or fully human IgG1 antibodies, which offer extended serum half-lives through neonatal Fc receptor (FcRn)-mediated recycling and preserve effector functions such as antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC) [79] [80]. An optimal tumor-associated antigen typically fulfills three criteria: (1) high and homogeneous expression on malignant cells with minimal presence in normal tissues, (2) efficient internalization upon antibody binding to facilitate intracellular drug delivery, and (3) biological relevance to tumorigenesis, which reduces immune escape and supports durable therapeutic responses [79]. Clinically validated targets satisfying these criteria include HER2 (breast, gastric cancers), CD30 (lymphomas), CD33 (acute myeloid leukemia), and TROP2 (various solid tumors), which have been successfully utilized in approved ADC therapies [79]. While conventional monospecific antibodies currently dominate ADC design, structural optimization strategies are gaining traction, including biparatopic antibodies that recognize two distinct epitopes on the same antigen, demonstrating enhanced binding avidity and improved internalization kinetics [79].
Linker Design: Balancing Stability and Payload Release
The linker component plays a dual role in ADC function: maintaining conjugate stability in systemic circulation and enabling efficient payload release within tumor cells [79]. An ideal linker remains intact in plasma to prevent premature cleavage and off-target toxicity, yet is selectively cleaved in the tumor microenvironment (TME) or within cancer cells to enable targeted drug release [79]. Linker physicochemical properties, including hydrophilicity and charge, substantially affect solubility, systemic stability, volume of distribution, and clearance kinetics, thereby influencing efficacy, safety, and the therapeutic index [79]. Cleavable linkers exploit physiological differences between the circulation and tumor cells, including acidic pH in endosomes/lysosomes (hydrazone linkers), high intracellular protease activity (valine-citrulline dipeptide linkers), and reducing environments with elevated glutathione levels (disulfide linkers) [79] [80]. Non-cleavable linkers (e.g., thioether linkers) rely on complete antibody degradation within lysosomes to release the payload, typically resulting in charged, membrane-impermeable metabolites that may reduce bystander effects but potentially increase intracellular retention and specificity [80]. Incorporating hydrophilic polyethylene glycol (PEG) chains into linker structures has been shown to improve aqueous solubility, reduce hydrophobic aggregation, and prolong circulation time [79].
Cytotoxic Payloads: Mechanisms of Action and Evolution
The payload component of ADCs consists of highly potent cytotoxic agents that ultimately kill target cells upon internalization and release [80]. First-generation ADCs used conventional chemotherapeutic agents (e.g., methotrexate, doxorubicin) with limited potency, but contemporary ADCs employ compounds with 100-1000-fold greater cytotoxicity than traditional chemotherapy drugs [80]. Payloads are categorized based on their mechanism of action, primarily as tubulin inhibitors or DNA-damaging agents [80].
Tubulin inhibitors, including auristatins (MMAE, MMAF) and maytansinoids (DM1, DM4), disrupt microtubule assembly during cell division, leading to cell cycle arrest at G2/M phase and apoptosis [80] [82]. These agents are particularly effective against rapidly dividing cells but may have limited efficacy against quiescent cancer cell populations [80]. DNA-damaging agents include topoisomerase I inhibitors (DXd, SN-38), calicheamicins, and pyrrolobenzodiazepines (PBDs), which cause DNA single-strand or double-strand breaks, disrupting DNA replication and transcription [80] [82]. These payloads can target cells throughout the cell cycle, making them effective against both proliferating and slow-cycling cells [80]. Third-generation ADCs increasingly utilize DNA-damaging agents, with 8 ADCs based on this mechanism approved as of 2025 [80].
Figure 1: ADC Mechanism of Action. ADCs bind to target antigens on tumor cells, undergo internalization and lysosomal trafficking, where linkers are cleaved to release cytotoxic payloads that induce apoptosis. Permeable payloads can diffuse into neighboring cells, creating a bystander effect.
ADC Mechanisms of Action: From Target Engagement to Cell Death
Molecular Orchestration of ADC Efficacy
The therapeutic activity of ADCs involves a meticulously coordinated sequence of molecular events beginning with specific antigen recognition and culminating in target cell elimination [79] [80]. The process initiates when the antibody component binds to its cognate cell surface antigen, typically followed by internalization of the ADC-antigen complex via receptor-mediated endocytosis [79]. The internalized complex traffics through endosomal compartments that progressively acidify, ultimately fusing with lysosomes containing proteolytic enzymes and acidic environments that trigger linker cleavage or antibody degradation [79]. For cleavable linkers, the lysosomal environment (low pH, high protease activity, or reducing conditions) liberates the cytotoxic payload, while non-cleavable linkers require complete antibody degradation to release payload attached to amino acid residues [80]. The released payload then diffuses throughout the cell to engage its molecular target—microtubules for auristatins and maytansinoids, or nuclear DNA for calicheamicin and topoisomerase inhibitors [80]. This interaction disrupts essential cellular processes, leading to cell cycle arrest and initiation of apoptotic pathways [80]. A critical feature of certain ADCs is the "bystander effect," wherein membrane-permeable payloads (e.g., MMAE, SN-38) diffuse out of the target cell and kill adjacent tumor cells regardless of their antigen expression, overcoming challenges posed by tumor heterogeneity [79] [82]. Additionally, the Fc domain of IgG1 antibodies can engage immune effector mechanisms including ADCC and CDC, potentially recruiting immune cells to contribute to tumor cell killing [79].
Payload Mechanisms at the Molecular Level
Tubulin inhibitors employ distinct molecular mechanisms to disrupt microtubule dynamics. Auristatins (MMAE, MMAF) bind to tubulin near the vinca domain, suppressing polymerization and accelerating disassembly, which reduces microtubule density and impairs spindle assembly during mitosis [80]. This triggers prophase/metaphase arrest and induces apoptosis through oxidative stress and mitochondrial membrane potential loss [80]. In contrast, maytansinoids (DM1, DM4) bind to β-tubulin and promote polymerization while inhibiting depolymerization, leading to abnormal microtubule stabilization, mitotic spindle disruption, chromosome segregation errors, and G2/M phase arrest [80]. This triggers apoptosis via mitochondria-dependent pathways [80].
DNA-damaging agents employ alternative mechanisms to induce lethal cellular damage. Topoisomerase I inhibitors (DXd, SN-38) form stable ternary complexes with TOP1 and DNA, preventing religation of DNA single-strand breaks and generating replication-associated double-strand breaks during DNA replication [80] [82]. Calicheamicin binds to the DNA minor groove and generates double-strand breaks via diradical formation, causing sequence-selective DNA damage [80]. Pyrrolobenzodiazepines (PBDs) cross-link DNA at specific sequences, creating irreversible interstrand cross-links that block DNA replication and transcription [82].
Advanced ADC Platforms and Nanoplatform Integration
Next-Generation ADC Architectures
The evolving understanding of ADC limitations has spurred development of innovative platforms with enhanced therapeutic properties [79] [83]. Bispecific ADCs incorporate antibodies that simultaneously target two different tumor antigens or epitopes, improving binding specificity and potential for enhanced internalization while addressing tumor heterogeneity [79]. Examples include platforms co-targeting HER2 and EGFR, which demonstrate improved targeting precision and efficacy against heterogeneous tumors [79]. Immune-stimulatory ADCs (ISACs) represent a paradigm shift from conventional cytotoxic payloads to immune-modulating agents such as TLR7/8 or STING agonists [79] [83]. These compounds stimulate innate immune responses within the tumor microenvironment, potentially converting "cold" tumors into "hot" tumors that are more susceptible to immune checkpoint inhibitors and other immunotherapies [79]. Proteolysis-targeting chimeras (PROTAC)-based ADCs leverage the ubiquitin-proteasome system to induce degradation of intracellular target proteins, offering strategies for traditionally "undruggable" oncoproteins [79]. These degrader-antibody conjugates (DACs) expand the scope of ADC targets beyond surface antigens to include intracellular oncoproteins [83]. Dual-payload ADCs deliver two different cytotoxic agents with complementary mechanisms to overcome resistance and enhance tumor cell killing, while radionuclide-drug conjugates (RDCs) combine radioactive isotopes with targeted antibodies for both diagnostic imaging and therapeutic applications [80].
RNA Delivery Nanoplatforms for Cancer Therapy
Nanoplatforms have emerged as crucial enabling technologies for RNA-based cancer therapeutics, addressing inherent challenges of RNA delivery including size constraints, low stability, surface charge hindering direct cell entry, short circulatory half-life, and rapid clearance [84]. Lipid nanoparticles (LNPs), polymeric nanoparticles, and inorganic nanoparticles provide designed solutions for RNA delivery and cellular uptake [84]. These platforms protect RNA payloads from degradation, enhance tumor accumulation through enhanced permeability and retention (EPR) effects or active targeting, and facilitate intracellular delivery through endosomal escape mechanisms [84]. RNA-based approaches include mRNA vaccines encoding tumor-associated antigens, neoantigens, or chimeric antigen receptors for T-cell reprogramming, as well as RNA interference tools (siRNA, miRNA) that enable highly effective post-transcriptional gene silencing of key molecular players in tumor progression and drug resistance [84]. The convergence of ADC technology with RNA nanoplatforms represents a promising frontier in targeted cancer therapy, combining precise targeting with versatile mechanisms of action.
Table 2: Approved ADC Drugs in Clinical Use (Selected Examples)
| ADC Drug | Target | Payload | Linker Type | Approved Indications |
|---|---|---|---|---|
| Gemtuzumab Ozogamicin | CD33 | Calicheamicin | Cleavable (hydrazone) | Acute Myeloid Leukemia |
| Brentuximab Vedotin | CD30 | MMAE | Cleavable (dipeptide) | Hodgkin Lymphoma, sALCL |
| Trastuzumab Emtansine (T-DM1) | HER2 | DM1 | Non-cleavable (SMCC) | HER2+ Breast Cancer |
| Trastuzumab Deruxtecan (T-DXd) | HER2 | Deruxtecan (TOP1 inhibitor) | Cleavable (tetrapeptide) | HER2+ Breast, Gastric Cancer |
| Sacituzumab Govitecan | TROP-2 | SN-38 (TOP1 inhibitor) | Cleavable (CL2A) | Triple-Negative Breast Cancer, HR+ Breast Cancer |
| Enfortumab Vedotin | Nectin-4 | MMAE | Cleavable (mc-VC-PABC) | Advanced Urothelial Carcinoma |
| Belantamab Mafodotin | BCMA | MMAF | Non-cleavable | Multiple Myeloma |
Experimental Protocols for ADC Development and Evaluation
ADC Conjugation and Characterization Workflow
The development of novel ADC entities requires rigorous analytical characterization to ensure optimal drug-to-antibody ratio (DAR), stability, and binding functionality [79]. The following protocol outlines key steps in ADC synthesis and evaluation:
Step 1: Antibody Engineering and Modification Engineer monoclonal antibodies to introduce specific conjugation sites using cysteine mutagenesis (THIOMAB technology) or unnatural amino acid incorporation [79]. Reduce endogenous interchain disulfide bonds for cysteine conjugation using tris(2-carboxyethyl)phosphine (TCEP) or dithiothreitol (DTT) in phosphate buffer (pH 7.0-7.4) at 25-37°C for 1-2 hours [79]. Alternatively, utilize engineered cysteines or incorporated unnatural amino acids with orthogonal chemical handles for site-specific conjugation [79].
Step 2: Payload-Linker Conjugation Activate cytotoxic payloads with maleimide (for cysteine conjugation) or NHS ester (for lysine conjugation) functional groups [79]. For maleimide-based conjugation, maintain reaction pH between 6.5-7.5 to minimize thioether exchange and ensure consistent DAR [79]. Incubate activated payload-linker complexes with modified antibodies at 4-25°C for 1-4 hours with gentle agitation [79].
Step 3: Purification and Characterization Purify conjugated ADCs using tangential flow filtration or size exclusion chromatography to remove unconjugated payload and aggregates [79]. Characterize DAR using hydrophobic interaction chromatography (HIC) or reversed-phase HPLC methods [79]. Confirm antigen-binding capacity using surface plasmon resonance (SPR) or ELISA, and assess aggregation status by size exclusion chromatography with multi-angle light scattering (SEC-MALS) [79].
Step 4: In Vitro Functional Assessment Evaluate ADC cytotoxicity using cell viability assays (e.g., CellTiter-Glo) across antigen-positive and antigen-negative cell lines to determine specificity [79]. Measure internalization kinetics using pH-sensitive fluorescent dyes or antibody-based detection methods [79]. Assess bystander killing effect using transwell co-culture systems with antigen-positive and antigen-negative cells [79].
Figure 2: ADC Development Workflow. Key stages in ADC development from antibody engineering through preclinical validation, highlighting the systematic approach required for successful ADC creation.
In Vivo Efficacy and Pharmacokinetic Studies
Animal Model Selection and Dosing Select immunodeficient mice (e.g., NSG, nude) for human tumor xenograft models or immunocompetent syngeneic models for immune function assessment [79]. Implant tumor cells subcutaneously or establish orthotopic models that better recapitulate the tumor microenvironment [79]. Administer ADCs via intravenous injection (tail vein) at doses typically ranging from 1-10 mg/kg, with dosing schedules varying from weekly to every three weeks based on ADC half-life and toxicity profile [79].
Tumor Monitoring and Pharmacodynamic Analysis Monitor tumor volume by caliper measurements 2-3 times weekly, calculating volume using the formula: V = (length × width²)/2 [79]. For pharmacokinetic analysis, collect serial blood samples at predetermined time points (e.g., 5 minutes, 4 hours, 24 hours, 72 hours, 1 week post-administration) [79]. Process samples to isolate plasma and quantify ADC concentrations using ELISA methods with detection antibodies specific to the payload or antibody component [79].
Tissue Analysis and Biomarker Assessment At study endpoint, collect tumors and normal tissues (liver, heart, lung, kidney) for histopathological examination [79]. Analyze antigen expression by immunohistochemistry and assess payload distribution using specialized detection methods (e.g., laser capture microdissection coupled with LC-MS/MS for payload quantification) [79]. Evaluate pharmacodynamic biomarkers including cleaved caspases for apoptosis, γH2AX for DNA damage, and phospho-histone H3 for mitotic arrest [79].
Research Reagent Solutions for ADC Development
Table 3: Essential Research Reagents for ADC Development
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Conjugation Reagents | Maleimide crosslinkers; NHS esters; Tetrazine/TCO for bioorthogonal chemistry | Site-specific ADC conjugation | Controlled DAR; Minimal heterogeneity; Improved stability |
| Cytotoxic Payloads | MMAE/MMAF; DM1/DM4; Pyrrolobenzodiazepines (PBDs); Camptothecin derivatives | ADC payload construction | High potency (pM-nM IC50); Defined mechanism; Modifiable functional groups |
| Specialized Linkers | mc-VC-PABC; SMCC; SPDB; Hydrazone linkers | Connecting antibodies to payloads | Plasma stability; Tumor-specific cleavage; Reduced premature release |
| Analytical Standards | DAR standards; Aggregation markers; Free payload controls | ADC characterization and QC | Benchmark for HIC/RP-HPLC; Quantification reference; Purity assessment |
| Cell-Based Assays | Antigen-positive/negative cell pairs; Reporter gene assays; 3D spheroid models | ADC functionality screening | Target specificity; Bystander effect; Penetration in tumor models |
Future Perspectives and Concluding Remarks
The ADC landscape continues to evolve rapidly, with ongoing innovations addressing key challenges including target heterogeneity, resistance mechanisms, and therapeutic index limitations [79] [83]. Future directions include the development of conditionally active "probody" ADCs that remain inert until activated by tumor-associated proteases, expanding the targetable antigen repertoire to include targets expressed in healthy tissues [83]. Artificial intelligence (AI)-guided ADC design is accelerating the identification of optimal antibody sequences, conjugation sites, and linker-payload combinations, potentially reducing development timelines and improving success rates [79] [81]. The integration of ADC technology with other therapeutic modalities, particularly immunotherapy, represents a promising strategy to overcome resistance and enhance durable responses [79] [82]. Additionally, the application of ADCs beyond oncology—including autoimmune diseases, infectious diseases, and other pathological conditions—is gaining traction as ADC platforms demonstrate versatility in targeted delivery [81]. As the molecular mechanisms driving cancer progression and metastasis continue to be elucidated, ADCs and advanced nanoplatforms will play an increasingly central role in the precision medicine arsenal, offering targeted therapeutic strategies aligned with the genetic and molecular profiles of individual tumors. The convergence of these technologies holds exceptional promise for addressing the formidable challenge of metastatic cancer, which remains the primary cause of cancer-related mortality worldwide [85] [37] [35].
Overcoming Drug Resistance and Tumor Heterogeneity
Therapies for metastatic cancer are profoundly limited by the development of resistance, a multifaceted challenge underpinning approximately 90% of cancer-related deaths. This whitepaper delineates three core molecular mechanisms—efflux pump-mediated drug expulsion, metabolic reprogramming, and evasion of apoptosis—that collectively enable tumor cells to survive therapeutic assault. Within the context of cancer progression and metastasis, we explore how these mechanisms are integrated into the tumor's biology, review current experimental methodologies for their study, and discuss emerging therapeutic strategies aimed at overcoming resistance. The objective is to provide a foundational resource for researchers and drug development professionals dedicated to creating next-generation oncology therapeutics.
The progression from a primary tumor to metastatic disease represents the most formidable challenge in clinical oncology. While advancements have been made in treating localized tumors, metastatic disease accounts for approximately 90% of cancer-related deaths [85]. A central driver of this mortality is the development of resistance to systemic therapies. The mechanisms of resistance are not merely cellular defects but are often emergent properties of a complex host-tumor ecosystem, intricately linked to the processes of dissemination and colonization of distant organs [85].
The efficacy of mainstay treatments—including chemotherapy, targeted therapy, and immunotherapy—is frequently undermined by intrinsic or acquired resistance. This paper focuses on three well-established yet critically relevant pillars of therapy resistance: the active efflux of drugs, the rewiring of cellular metabolism to support survival, and the disabling of programmed cell death pathways. Understanding these mechanisms within the broader framework of metastasis research is paramount for developing strategies to circumvent treatment failure and improve patient outcomes.
Efflux Pump-Mediated Drug Resistance
Mechanisms and Key Players
Multidrug efflux pumps are transmembrane transporters that utilize energy to expel a wide spectrum of structurally unrelated chemotherapeutic drugs from cancer cells, thereby reducing intracellular drug accumulation and conferring multidrug resistance (MDR) [86] [87] [88]. The most extensively studied among these is P-glycoprotein (P-gp), a 170-kDa glycoprotein encoded by the ABCB1 gene and a member of the ATP-binding cassette (ABC) transporter superfamily [88]. P-gp is composed of two nucleotide-binding domains (NBDs) that hydrolyze ATP and two transmembrane domains (TMDs) that form the substrate-binding pocket [88].
The physiological expression of efflux pumps in organs like the intestine, liver, kidney, and blood-brain barrier serves a protective role by eliminating toxins [86]. However, overexpression of P-gp has been detected in various chemoresistant cancers, including osteosarcoma, hepatocellular carcinoma, breast cancer, gastric cancer, and lung cancer, where it actively expels drugs such as cisplatin, paclitaxel, 5-fluorouracil (5-FU), and doxorubicin [88]. Beyond P-gp, other ABC transporters like Multidrug Resistance-Associated Protein 1 (MRP1) and Breast Cancer Resistance Protein (BCRP/ABCG2) also contribute significantly to the MDR phenotype [89].
Regulation and Role in Metastasis
The expression of efflux pumps is often induced by the selective pressure of chemotherapy. However, it can also be upregulated by specific tumor microenvironmental conditions, such as hypoxia. In liver cancer cells, a hypoxic environment can induce P-gp expression via the transcription factor Nrf2 [88]. Similarly, in non-small cell lung cancer (NSCLC), hypoxia-inducible factor (HIF) can drive P-gp overexpression, promoting cisplatin resistance [88]. Key signaling pathways involved in regulating P-gp expression include NF-κB and STAT3 [88].
The role of efflux pumps extends beyond mere drug resistance. In the metastatic cascade, circulating tumor cells (CTCs) must survive in the circulation to seed distant sites. The expression of efflux pumps may provide a survival advantage by protecting these "seeds" from various toxic compounds, thereby facilitating successful metastasis.
Table 1: Key ATP-Binding Cassette (ABC) Efflux Pumps in Cancer Drug Resistance
| Transporter | Gene | Common Substrates | Cancers with Documented Role |
|---|---|---|---|
| P-glycoprotein (P-gp) | ABCB1 | Doxorubicin, Paclitaxel, Cisplatin, Vinblastine | Liver cancer, Lung cancer, Breast cancer, Osteosarcoma [88] |
| Multidrug Resistance-Associated Protein 1 (MRP1) | ABCC1 | Doxorubicin, Etoposide, Vincristine, Methotrexate | Acute Myeloid Leukemia, Lung cancer [89] |
| Breast Cancer Resistance Protein (BCRP) | ABCG2 | Mitoxantrone, Topotecan, Doxorubicin | Breast cancer, Gastric cancer, Colon cancer [89] |
Experimental Analysis of Efflux Pumps
Protocol: Functional Assessment of Efflux Pump Activity via Flow Cytometry
This protocol measures the intracellular retention of a fluorescent P-gp substrate (e.g., Rhodamine 123 or Calcein-AM) with and without inhibitors.
- Cell Preparation: Harvest drug-resistant and parental sensitive cancer cells (e.g., HepG2/DOX vs. HepG2). Wash with PBS and resuspend in serum-free media.
- Dye Loading: Divide cell suspensions into aliquots.
- Test Group: Incubate with the fluorescent substrate (e.g., 0.5 µg/mL Rhodamine 123) for 60 minutes at 37°C.
- Inhibition Control: Pre-incubate with a specific P-gp inhibitor (e.g., 10 µM Verapamil) for 20 minutes, then co-incubate with the inhibitor and the fluorescent dye for 60 minutes.
- Background Control: Keep on ice without dye.
- Wash and Analyze: Wash cells twice with ice-cold PBS to remove extracellular dye. Resuspend in cold PBS and analyze immediately via flow cytometry.
- Data Interpretation: A higher mean fluorescence intensity (MFI) in the inhibition control compared to the test group indicates active efflux. The Efflux Ratio can be calculated as (MFI with inhibitor) / (MFI without inhibitor). A ratio >1 confirms functional efflux pump activity.
Research Reagent Solutions for Efflux Pump Studies
| Research Reagent | Function/Application |
|---|---|
| Rhodamine 123 | Fluorescent P-gp substrate for functional efflux assays. |
| Verapamil | First-generation P-gp inhibitor used as a control in inhibition experiments. |
| Anti-P-gp Antibody (e.g., UIC2) | For detecting P-gp cell surface expression via flow cytometry or immunofluorescence. |
| Tariquidar | Third-generation, highly specific P-gp inhibitor for potent efflux blockade. |
| siRNA against ABCB1 | For genetic knockdown of P-gp to confirm its role in resistance. |
Diagram 1: P-gp Mediated Drug Efflux. The diagram illustrates how P-gp uses ATP hydrolysis to actively pump chemotherapeutic drugs out of the cancer cell, maintaining sub-therapeutic intracellular concentrations and leading to multidrug resistance.
Metabolic Reprogramming as a Resistance Mechanism
The Warburg Effect and Beyond
Cancer metabolic reprogramming, a hallmark of cancer, describes the rewiring of energy production and biosynthetic pathways to support rapid proliferation, survival, and metastasis [90]. A cardinal feature is the Warburg effect (aerobic glycolysis), wherein cancer cells preferentially metabolize glucose to lactate even in the presence of ample oxygen [90] [91]. This shift from efficient oxidative phosphorylation to seemingly inefficient glycolysis provides several advantages: it generates ATP rapidly, and crucially, glycolytic intermediates are diverted into biosynthetic pathways for nucleotides, amino acids, and lipids, fuelling cell growth [90].
This metabolic adaptation directly contributes to therapy resistance. For instance, the upregulation of glucose transporters (e.g., GLUT1) and glycolytic enzymes (e.g., HK2, LDHA) not only increases energy production but also provides precursors for synthesizing molecules that combat oxidative stress, such as NADPH via the pentose phosphate pathway (PPP) [90]. This enhanced antioxidant capacity helps cells withstand the oxidative damage induced by many chemotherapeutic agents.
Glutaminolysis and Mitochondrial Dynamics
Beyond glycolysis, many tumors exhibit a dependency on glutaminolysis. Glutamine is catabolized to glutamate and then to α-ketoglutarate to fuel the tricarboxylic acid (TCA) cycle, a process regulated by oncogenes like c-Myc [90]. This pathway provides nitrogen for amino acid and nucleotide synthesis and NADPH for redox homeostasis, supporting tumor survival under stress [90].
Mitochondria, the central organelles for energy metabolism and apoptosis regulation, play a key role in resistance. They undergo constant mitochondrial dynamics—fusion and fission—and mitophagy (selective removal of damaged mitochondria) to maintain a functional network [91]. Through fusion, fission, and mitophagy, tumor cells ensure a population of healthy mitochondria capable of meeting energy demands and resisting drug-induced apoptosis, thereby increasing tolerance to chemotherapeutic drugs [91]. For example, dysregulation of fusion proteins (MFN1/MFN2, OPA1) and fission protein (DRP1) is linked to proliferation and chemoresistance in various tumors [91].
Table 2: Key Features of Metabolic Reprogramming in Therapy-Resistant Cancers
| Metabolic Pathway | Key Molecular Players | Role in Resistance & Tumor Survival |
|---|---|---|
| Aerobic Glycolysis (Warburg Effect) | GLUT1, HK2, LDHA, c-Myc, HIF-1α | Rapid ATP generation; provides precursors for biosynthesis (nucleotides, lipids); lactate secretion acidifies TME, promoting invasion [90]. |
| Glutaminolysis | ASCT2, GLS1, c-Myc | Fuels TCA cycle (anaplerosis); generates antioxidants (NADPH) to detoxify ROS from chemotherapy [90]. |
| Pentose Phosphate Pathway (PPP) | G6PD | Produces ribose-5-phosphate for nucleotide synthesis and NADPH for redox balance and drug detoxification [90]. |
| Mitochondrial Dynamics | MFN1/2, OPA1, DRP1 | Maintains mitochondrial health and function; enhances bioenergetic capacity and stress tolerance, promoting cell survival [91]. |
Experimental Analysis of Metabolic Reprogramming
Protocol: Assessing Glycolytic Flux with the Seahorse XF Analyzer
This protocol measures the Extracellular Acidification Rate (ECAR), a proxy for glycolytic flux, in real-time.
- Cell Culture: Seed drug-resistant and sensitive cells (e.g., 20,000-50,000 cells/well) into a Seahorse XF cell culture microplate and culture overnight.
- Assay Medium: Prior to the assay, replace growth media with Seahorse XF Base Medium (pH 7.4) supplemented with 2 mM L-glutamine. Incubate for 1 hour at 37°C in a non-CO₂ incubator.
- Sensor Cartridge Loading: Load the Seahorse XFp Glycolysis Stress Test Kit reagents into the sensor cartridge:
- Port A: 10 mM Glucose
- Port B: 1 µM Oligomycin (ATP synthase inhibitor)
- Port C: 50 mM 2-Deoxy-D-glucose (2-DG, a glycolytic inhibitor)
- Run Assay: Calibrate the cartridge and run the Glycolysis Stress Test program. The instrument sequentially injects the compounds while measuring ECAR.
- Data Interpretation: Key parameters are derived:
- Glycolysis: Baseline ECAR after glucose injection.
- Glycolytic Capacity: Maximum ECAR after oligomycin injection.
- Glycolytic Reserve: The difference between glycolytic capacity and glycolysis.
Research Reagent Solutions for Metabolic Studies
| Research Reagent | Function/Application |
|---|---|
| 2-Deoxy-D-glucose (2-DG) | Competitive inhibitor of glycolysis; used to block glycolytic flux. |
| Oligomycin | ATP synthase inhibitor; used to measure glycolytic capacity. |
| UK5099 | Inhibitor of the mitochondrial pyruvate carrier; forces reliance on glycolysis. |
| CB-839 | Clinical-stage inhibitor of glutaminase (GLS1); targets glutaminolysis. |
| Seahorse XF Glycolysis Stress Test Kit | Standardized kit for real-time measurement of ECAR and glycolytic function. |
Diagram 2: Metabolic Reprogramming in Cancer. This map illustrates key alterations in cancer cell metabolism, including the Warburg Effect (conversion of glucose to lactate despite oxygen availability), upregulated glutaminolysis, and shunting of carbons into the pentose phosphate pathway. These changes provide energy, biomass, and redox balance, collectively supporting survival under therapeutic stress.
Evasion of Apoptosis
Core Apoptotic Pathways and Their Dysregulation
Apoptosis, or programmed cell death, is a critical defense mechanism that eliminates damaged cells. The evasion of apoptosis is a hallmark of cancer and a major contributor to therapy resistance, as most chemotherapeutic agents ultimately act by inducing apoptotic cell death [92]. There are two principal apoptosis signaling pathways: the extrinsic (death receptor) pathway and the intrinsic (mitochondrial) pathway [92].
The extrinsic pathway is initiated by the binding of ligands (e.g., FasL, TRAIL) to death receptors on the cell surface, leading to the formation of the Death-Inducing Signaling Complex (DISC) and activation of caspase-8. The intrinsic pathway is triggered by cellular stress (e.g., DNA damage, oxidative stress) and is regulated by the B-cell lymphoma 2 (Bcl-2) protein family. This stress leads to Mitochondrial Outer Membrane Permeabilization (MOMP), releasing cytochrome c and forming the apoptosome, which activates caspase-9 [92]. Both pathways converge on the execution phase, mediated by caspase-3 and -7.
Cancer cells evade these pathways through multiple mechanisms. The extrinsic pathway can be impaired by downregulation of death receptor surface expression (e.g., CD95 in chemoresistant leukemia) or by overexpression of decoy receptors and inhibitory proteins like cellular FLICE-inhibitory protein (c-FLIP) [92]. The intrinsic pathway is frequently blocked by the overexpression of anti-apoptotic Bcl-2 family members (e.g., Bcl-2, Bcl-XL, Mcl-1), which prevent the pro-apoptotic proteins Bax and Bak from inducing MOMP [92]. An imbalance in the ratio of anti-apoptotic to pro-apoptotic proteins is a common feature in therapy-resistant cancers.
Experimental Analysis of Apoptosis Evasion
Protocol: Differentiating Apoptosis Pathways via Caspase Activation and Flow Cytometry
This protocol uses caspase-specific inhibitors and flow cytometry to distinguish the pathway of drug-induced apoptosis.
- Cell Treatment: Divide drug-resistant and sensitive cells into four treatment groups:
- Untreated Control: Vehicle only.
- Drug Treatment: Incubate with a chemotherapeutic agent (e.g., 1 µM Doxorubicin) for 12-24 hours.
- Drug + Extrinsic Inhibitor: Pre-treat with a caspase-8 specific inhibitor (e.g., Z-IETD-FMK, 20 µM) for 1 hour, then add the chemotherapeutic drug.
- Drug + Intrinsic Inhibitor: Pre-treat with a caspase-9 specific inhibitor (e.g., Z-LEHD-FMK, 20 µM) for 1 hour, then add the chemotherapeutic drug.
- Apoptosis Detection: Harvest cells and stain with an Annexin V-FITC / Propidium Iodide (PI) kit according to the manufacturer's instructions. Annexin V binds to phosphatidylserine externalized on the outer leaflet of the plasma membrane in early apoptosis, while PI stains cells with compromised membrane integrity (late apoptosis/necrosis).
- Flow Cytometry Analysis: Analyze all samples by flow cytometry. The percentage of Annexin V-positive cells indicates the level of apoptosis.
- Data Interpretation: Compare apoptosis levels across inhibitor-treated groups. A significant reduction in apoptosis in the caspase-9 inhibited group suggests the intrinsic pathway is the primary activation route for the drug. Conversely, protection by the caspase-8 inhibitor implicates the extrinsic pathway.
Research Reagent Solutions for Apoptosis Studies
| Research Reagent | Function/Application |
|---|---|
| Annexin V-FITC/PI Apoptosis Detection Kit | Standard kit for quantifying early and late apoptosis by flow cytometry. |
| Z-VAD-FMK | Pan-caspase inhibitor; confirms caspase-dependent apoptosis. |
| Z-IETD-FMK (Caspase-8 Inhibitor) | Specific inhibitor to probe the extrinsic apoptosis pathway. |
| Z-LEHD-FMK (Caspase-9 Inhibitor) | Specific inhibitor to probe the intrinsic apoptosis pathway. |
| ABT-263 (Navitoclax) | Bcl-2/Bcl-XL inhibitor; small molecule to restore intrinsic apoptosis. |
| Anti-Bcl-2 Antibody | For Western blot or ICC to measure anti-apoptotic protein levels. |
Diagram 3: Apoptosis Evasion Mechanisms. The map outlines the extrinsic (death receptor) and intrinsic (mitochondrial) apoptosis pathways. Key evasion strategies employed by cancer cells are highlighted, including overexpression of inhibitory proteins like c-FLIP and Bcl-2, which block caspase activation and prevent cell death, leading to therapy resistance.
Integrated View and Therapeutic Outlook
The three pillars of resistance—efflux, metabolism, and apoptosis evasion—do not operate in isolation. They form a coordinated defense network within the tumor cell. For instance, metabolic rewiring can supply the ATP needed for efflux pump function and promote the synthesis of anti-apoptotic proteins. Furthermore, successful metastasis relies on cancer cells that are inherently resistant to anoikis (a form of apoptosis) and can adapt their metabolism to thrive in new organ microenvironments [93] [35].
The future of overcoming therapy resistance lies in combination therapies that target these mechanisms simultaneously. Promising strategies include:
- Nanotechnology: Nanoparticles can be engineered to co-deliver chemotherapeutic drugs alongside efflux pump inhibitors (e.g., tariquidar) or pro-apoptotic molecules (e.g., BH3 mimetics), bypassing efflux and directly triggering cell death [89].
- Targeting Metabolism: Inhibitors of key glycolytic enzymes (e.g., LDHA) or glutaminase (e.g., CB-839) are in development to disrupt the metabolic adaptations that fuel resistance [90].
- Restoring Apoptosis: BH3 mimetics like venetoclax (a Bcl-2 inhibitor) have shown clinical success in hematological malignancies and are being explored in solid tumors to directly reactivate the blocked intrinsic apoptosis pathway [92].
A deep understanding of the molecular interplay between these resistance mechanisms, particularly within the context of the metastatic cascade, is essential for the rational design of these next-generation therapeutic regimens.
The Pivotal Role of Cancer Stem Cells in Relapse and Treatment Failure
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [94]. These cells possess the dual functional capacities of self-renewal and multi-lineage differentiation, enabling them to regenerate the heterogeneous cell populations within a tumor and initiate new tumor growth after conventional therapies have eliminated the bulk of cancer cells [95]. The ability of CSCs to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies [94]. Despite significant advances in cancer treatment, recurrence and metastasis remain the primary causes of cancer-related mortality, with CSCs identified as the key drivers of these recalcitrant behaviors [95]. Understanding the biological properties and molecular regulatory mechanisms of CSCs is therefore essential for developing more effective cancer therapies that can overcome treatment resistance and prevent disease recurrence.
Biological Characteristics and Identification of Cancer Stem Cells
Defining Properties of Cancer Stem Cells
CSCs exhibit several defining characteristics that distinguish them from the bulk of tumor cells and normal stem cells. These properties collectively enable CSCs to initiate tumors, drive disease progression, and survive therapeutic interventions [96] [95]:
- Self-renewal and differentiation: CSCs can undergo asymmetric division to produce both identical copies of themselves (self-renewal) and differentiated progeny that constitute the bulk of the tumor (multi-lineage differentiation) [95].
- Tumor-initiating capacity: When transplanted into immunodeficient mice, CSCs can initiate new tumors that recapitulate the heterogeneity of the original tumor, whereas non-CSC populations lack this capacity [95].
- Therapy resistance: CSCs possess intrinsic and adaptive mechanisms that allow them to survive conventional chemotherapy and radiotherapy [96].
- Metabolic plasticity: CSCs can switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids, enabling survival under diverse environmental conditions [94].
- Dynamic plasticity: CSCs can reversibly transition between epithelial and mesenchymal states, as well as between quiescent and proliferative phases, complicating therapeutic targeting [95].
CSC Markers and Signaling Pathways Across Cancer Types
CSCs are identified and isolated through specific surface markers and activated signaling pathways that vary across different cancer types. The table below summarizes key markers and pathways associated with CSCs in various malignancies.
Table 1: Cancer Stem Cell Markers and Signaling Pathways in Different Cancer Types
| Cancer Type | Key CSC Markers | Activated Signaling Pathways | Functional Significance |
|---|---|---|---|
| Acute Myeloid Leukemia (AML) | CD34âºCD38â» [94] | Notch, Wnt/β-catenin [97] | Leukemia initiation and reconstitution capacity [94] |
| Breast Cancer | CD44âºCD24â»/ALDH1⺠[95] | Notch1, Wnt/β-catenin [96] [97] | Tumor initiation, trastuzumab resistance [96] [95] |
| Glioblastoma (GBM) | CD133âº/Prominin-1, Nestin, SOX2 [94] [96] | Hedgehog, Notch [97] | Radioresistance, DNA repair activation [96] |
| Colorectal Cancer | LGR5, CD166, CD133 [94] [95] | Wnt/β-catenin, Notch [97] | Tumor initiation, regulated by gut microbiota [95] |
| Pancreatic Cancer | CD133âº, CD44⺠[94] | Hedgehog, Wnt/β-catenin [97] | Therapy resistance, tumor maintenance |
| Prostate Cancer | EpCAM [94] | PI3K/Akt, Notch [97] | Target for CAR-T cell therapy [94] |
It is important to note that CSC markers are not universal across cancer types and may vary even within subtypes of the same cancer, reflecting the influence of tissue origin and microenvironmental context on CSC phenotypes [94]. Furthermore, the expression of these markers does not always strictly define the CSC population, as non-CSCs may also express some of these markers, and CSC phenotypes can be dynamically acquired by non-CSCs through processes such as epithelial-mesenchymal transition (EMT) [94] [98].
Molecular Mechanisms of CSC-Mediated Therapy Resistance
Intrinsic Resistance Mechanisms
CSCs employ multiple sophisticated mechanisms to resist conventional cancer therapies, enabling them to survive treatment and initiate disease recurrence. These intrinsic resistance properties include:
- Enhanced drug efflux capabilities: CSCs overexpress ATP-binding cassette (ABC) transporters such as P-glycoprotein, multidrug resistance-associated proteins, and breast cancer resistance protein, which actively expel chemotherapeutic agents from the cell, reducing intracellular drug accumulation [96] [42].
- Enhanced DNA damage response: CSCs exhibit heightened activation of DNA damage checkpoints (Chk1 and Chk2) and repair pathways, allowing them to efficiently repair therapy-induced DNA damage [96].
- Apoptosis evasion: CSCs upregulate anti-apoptotic proteins (e.g., Bcl-2, Bcl-xL) and disrupt apoptotic pathways, increasing their threshold for cell death induction [96] [42].
- Quiescence: A subset of CSCs can enter a dormant, non-dividing state (G0 phase), making them resistant to therapies that target rapidly dividing cells [96].
- Detoxifying enzymes: High expression of aldehyde dehydrogenase (ALDH1) in CSCs contributes to resistance by detoxifying chemotherapeutic agents and reactive oxygen species [96] [95].
Signaling Pathways Governing CSC Resistance
Several evolutionarily conserved signaling pathways play critical roles in maintaining CSC stemness and promoting therapy resistance. The intricate network of these pathways presents both challenges and opportunities for therapeutic targeting.
Table 2: Key Signaling Pathways in Cancer Stem Cell Maintenance and Resistance
| Signaling Pathway | Key Components | Role in CSCs | Therapeutic Targeting Approaches |
|---|---|---|---|
| Wnt/β-catenin | β-catenin, APC, GSK-3β, TCF/LEF | Self-renewal maintenance, EMT induction [97] [98] | Small molecule inhibitors, monoclonal antibodies [97] |
| Notch | Notch receptors (1-4), DLL, Jagged, γ-secretase | Stemness maintenance, chemotherapy resistance [96] [97] | γ-secretase inhibitors, monoclonal antibodies [96] |
| Hedgehog | PTCH, SMO, GLI | Self-renewal regulation, tumor initiation [96] [97] | SMO inhibitors (vismodegib), GLI antagonists [96] |
| PI3K/Akt/mTOR | PI3K, Akt, mTOR, PTEN | Survival, metabolism, proliferation [97] [42] | PI3K inhibitors, Akt inhibitors, mTOR inhibitors [42] |
| JAK/STAT | JAK, STAT | Immune evasion, inflammation response [96] | JAK inhibitors, STAT inhibitors [96] |
CSC Signaling Network: This diagram illustrates how major signaling pathways converge to maintain stemness properties in cancer stem cells, which in turn drive therapy resistance and metastatic progression through processes like epithelial-mesenchymal transition (EMT).
Microenvironmental Interactions and CSC Niche
The tumor microenvironment (TME) plays a crucial role in supporting CSC maintenance and promoting therapy resistance. CSCs engage in bidirectional interactions with various components of the TME [97] [95]:
- Cancer-associated fibroblasts (CAFs): CAFs secrete growth factors, cytokines, and extracellular matrix components that support CSC survival and self-renewal through pathways such as PDGFR-β/GPR91 [95].
- Tumor-associated macrophages (TAMs): TAMs polarized toward the M2 phenotype release immunosuppressive cytokines (TGF-β, IL-10) that shield CSCs from immune surveillance [95].
- Hypoxia: Hypoxic conditions within the TME stabilize hypoxia-inducible factors (HIFs), which enhance CSC stemness through metabolic and epigenetic alterations [97].
- Gut microbiota: In colorectal cancer, specific bacteria (e.g., colistin-producing Escherichia coli) induce genomic instability and upregulate stemness markers (CD133, OCT4) [95].
These microenvironmental interactions create specialized "niches" that protect CSCs from therapeutic insults and facilitate their persistence after treatment.
Experimental Models and Methodologies for CSC Research
Core Experimental Protocols in CSC Investigation
CSC Isolation and Characterization
Sphere Formation Assay:
- Purpose: To evaluate the self-renewal capacity of CSCs under non-adherent conditions.
- Methodology: Single-cell suspensions are plated in ultra-low attachment plates with serum-free medium supplemented with growth factors (EGF, bFGF). After 7-14 days, spheres (tumorspheres) are counted and analyzed.
- Interpretation: The number and size of spheres correlate with the self-renewal potential of the CSC population. Secondary and tertiary sphere formation assays can further assess self-renewal capacity [96] [95].
Limiting Dilution Transplantation Assay:
- Purpose: To quantify tumor-initiating cell frequency in vivo.
- Methodology: Serial dilutions of putative CSC populations are transplanted into immunodeficient mice (e.g., NOD/SCID, NSG). Tumor formation is monitored over several weeks to months.
- Interpretation: Tumor-initiating cell frequency is calculated using statistical methods (e.g., ELDA software) that compare the probability of tumor formation at different cell doses [95].
Targeting CSC Signaling Pathways
Notch Pathway Inhibition Assay:
- Purpose: To evaluate the effect of Notch signaling inhibition on CSC viability and stemness properties.
- Methodology: CSCs are treated with γ-secretase inhibitors (e.g., DAPT, RO4929097) or Notch-blocking antibodies. Effects on sphere formation, marker expression (by flow cytometry), and downstream target genes (Hes1, Hey1 by qRT-PCR) are assessed.
- Application: Particularly relevant in breast cancer models to overcome trastuzumab resistance [96].
Combined Checkpoint Inhibition and Radiotherapy:
- Purpose: To sensitize radioresistant CSCs to radiation treatment.
- Methodology: Glioblastoma CSCs are treated with Chk1/Chk2 inhibitors prior to or concurrently with radiation. DNA damage response is assessed by γH2AX staining, and apoptosis is measured by Annexin V staining.
- Interpretation: Enhanced radiosensitization indicates dependency on DNA checkpoint pathways in CSCs [96].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Cancer Stem Cell Investigations
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| CSC Surface Markers | Anti-CD44, Anti-CD133, Anti-CD34, Anti-ALDH1 | Flow cytometry, immunocytochemistry, cell sorting | CSC identification, isolation, and purification |
| Signaling Inhibitors | γ-Secretase inhibitors (DAPT), SMO antagonists (vismodegib), Wnt inhibitors (LGK974) | Pathway inhibition studies, combination therapies | Targeting stemness pathways to eliminate CSCs |
| Cytokines/Growth Factors | EGF, bFGF, BMP-4 | Sphere formation assays, in vitro culture | Maintaining CSC stemness in vitro |
| Apoptosis Detection | Annexin V, caspase inhibitors, JC-1 dye | Apoptosis assays, therapy response assessment | Measuring cell death in response to treatments |
| qRT-PCR Primers | Nanog, Oct4, Sox2, ALDH1A1 | Gene expression analysis | Stemness gene profiling |
| Nanocarriers | Liposomes, polymeric nanoparticles, exosomes | Targeted drug delivery to CSCs | Overcoming drug resistance mechanisms |
Emerging Therapeutic Strategies Targeting CSCs
Innovative Approaches to Overcome CSC-Mediated Resistance
Recent advances in our understanding of CSC biology have led to the development of several promising therapeutic strategies aimed at eradicating CSCs and overcoming treatment resistance:
Nanocarrier-based drug delivery systems: Nanoparticles (20-200 nm) leverage the enhanced permeability and retention (EPR) effect to passively accumulate in tumor tissues, allowing targeted delivery of therapeutic agents to CSCs while minimizing systemic toxicity [96]. These systems can co-deliver anticancer drugs, multiple drug resistance modulators, and CSC-targeting ligands to boost specificity and overcome drug resistance [96].
Immunotherapy approaches: Chimeric antigen receptor (CAR) T-cells targeting CSC-specific markers (e.g., EpCAM in prostate cancer) have shown preclinical efficacy in eliminating CSCs [94] [97]. Immune checkpoint inhibitors (e.g., anti-PD-1/PD-L1) are being investigated in combination with CSC-targeted therapies to enhance immune-mediated clearance of CSCs [42].
Photodynamic therapy (PDT): PDT uses light-activated photosensitizers to generate reactive oxygen species that selectively target and destroy tumor cells. Recent advancements include nanoparticle-based PDT systems that improve targeting and efficacy against CSCs, particularly in colorectal cancer models [99].
Metabolic interventions: Dual metabolic inhibition strategies target the metabolic plasticity of CSCs by simultaneously inhibiting glycolysis, oxidative phosphorylation, and alternative fuel source utilization [94]. Pro-oxidative therapies exploit the increased vulnerability of metastatic CSCs to oxidative stress during the metastatic cascade [37].
Boolean logic CAR T-cells: Next-generation CAR T-cells are engineered with multiple receptors that require recognition of at least two different leukemia markers for activation, enhancing specificity and sparing healthy cells [100].
Clinical Translation Challenges and Future Directions
Despite promising preclinical developments, several challenges remain in translating CSC-targeted therapies to clinical applications:
- Lack of universal CSC biomarkers: The absence of consistent markers across cancer types and the dynamic plasticity of CSCs complicate patient stratification and treatment monitoring [94].
- Toxicity to normal stem cells: Many CSC-targeted approaches may affect normal tissue stem cells due to shared signaling pathways and surface markers, potentially causing unacceptable side effects [94].
- Tumor heterogeneity and adaptive resistance: Intratumoral heterogeneity and the ability of CSCs to adaptively switch signaling pathways can lead to compensatory resistance mechanisms [97] [95].
- CSC plasticity and phenotypic switching: The ability of non-CSCs to acquire CSC properties through EMT and other plasticity mechanisms enables tumors to regenerate the CSC pool after initially successful targeted therapies [94] [98].
Future research directions include the integration of multi-omics technologies (single-cell sequencing, spatial transcriptomics, AI-driven analysis) to better understand CSC heterogeneity and identify novel vulnerabilities [94] [100]. Additionally, combination therapies that simultaneously target CSCs through multiple mechanisms (signaling pathways, metabolic vulnerabilities, immune activation) may be necessary to achieve durable treatment responses and prevent relapse [42] [95].
CSC Research Pipeline: This workflow outlines the comprehensive process from tumor sample collection through single-cell analysis and CSC identification to therapeutic targeting and response assessment, highlighting the integrated approach required for effective CSC research.
Strategies to Counteract Multi-Drug Resistance (MDR) Proteins
Multidrug resistance (MDR) represents a principal obstacle in oncology, frequently leading to the failure of chemotherapy and mortality in cancer patients. MDR is classically defined as the ability of cancer cells to withstand treatment with diverse anticancer drugs, irrespective of their structural or functional differences [101]. A cornerstone mechanism underpinning this phenotype is the elevated activity of ATP-binding cassette (ABC) transporter proteins, with P-glycoprotein (P-gp/ABCB1) being the most extensively characterized efflux pump [102] [103]. These transmembrane proteins actively expel a wide spectrum of chemotherapeutic agents from cancer cells, diminishing intracellular drug accumulation and cytotoxic efficacy [102]. Beyond efflux mechanisms, resistance is a multifaceted phenomenon, coordinated through a complex interplay of additional processes including altered drug targets, enhanced DNA repair, cell death inhibition, and the dynamic influence of the tumor microenvironment [101] [104]. This technical guide synthesizes current molecular understanding and outlines advanced, evolving strategies to counteract MDR proteins, providing a framework for ongoing research and therapeutic development.
Molecular Mechanisms of MDR Proteins
P-Glycoprotein and ABC Transporter Family
The ABC transporter superfamily comprises a class of membrane proteins that utilize ATP hydrolysis to energize the translocation of substrates across cellular membranes. In the context of MDR, P-glycoprotein (P-gp) is of paramount importance. It is a 170-kDa transmembrane glycoprotein encoded by the ABCB1 (or MDR1) gene, which functions as a polyspecific efflux pump for chemotherapeutic agents including anthracyclines, vinca alkaloids, taxanes, and epipodophyllotoxins [101] [103]. Its broad substrate specificity is a major driver of cross-resistance to unrelated drugs. The operational model involves drug binding to the transmembrane domains of P-gp, followed by ATP hydrolysis at its nucleotide-binding domains, which induces a conformational change that results in the extrusion of the drug substrate to the extracellular space [103]. This active efflux maintains intracellular drug concentrations below a critical therapeutic threshold, thereby protecting cancer cells from apoptosis.
Non-Efflux Mediated Mechanisms
While ABC transporters are pivotal, the MDR landscape is considerably broader. Cancer cells deploy a formidable arsenal of resistance strategies, often operating in concert with efflux pumps.
- Altered Drug Metabolism and Targets: Mutations in drug targets can reduce drug-binding affinity. For instance, mutations in the catalytic domain of EGFR (e.g., T790M) confer resistance to tyrosine kinase inhibitors like afatinib in non-small cell lung cancer (NSCLC) [105].
- Enhanced DNA Repair and Apoptotic Evasion: Upregulation of DNA damage repair pathways, such as homologous recombination repair, can counteract DNA-damaging chemotherapeutics. Additionally, cancer cells can evade programmed cell death by downregulating pro-apoptotic signals or upregulating anti-apoptotic proteins like Bcl-2 [101] [104].
- Role of the Tumor Microenvironment (TME) and Non-coding RNAs: Hypoxia and interactions with stromal cells in the TME can foster resistance [101]. Moreover, non-coding RNAs (ncRNAs), including microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), function as critical regulators of MDR. For example, exosomal transfer of miR-21 from M2-polarized macrophages can promote cisplatin resistance in gastric cancer by suppressing PTEN and enhancing PI3K/AKT signaling [105].
- The Emergent Concept of Protein Damage Response (PDR): Recent research has unveiled a novel, pervasive mechanism termed the Protein Damage Response (PDR). This process is initiated when anticancer drugs bind nonspecifically to newly synthesized proteins, causing misfolding, aggregation, and oxidative damage. In response, cancer cells mount a defense involving the ubiquitination of these damaged proteins and their subsequent clearance by the proteasome. Elevated proteasome activity has been clinically observed in drug-resistant metastatic breast and colon cancers, identifying the PDR as a potent, non-canonical facilitator of MDR [106].
Table 1: Key Mechanisms of Multidrug Resistance in Cancer
| Mechanism Category | Specific Example | Functional Consequence |
|---|---|---|
| Drug Efflux | Overexpression of P-glycoprotein (P-gp/ABCB1) | Active extrusion of chemotherapeutics (e.g., anthracyclines, taxanes) reducing intracellular accumulation [101] [103]. |
| Drug Target Alteration | EGFR T790M mutation in NSCLC | Reduced binding affinity of tyrosine kinase inhibitors (e.g., afatinib, dacomitinib) [105]. |
| DNA Repair Enhancement | Upregulation of Homologous Recombination (HR) pathway | Counteracts DNA damage induced by platinum-based agents and PARP inhibitors [105]. |
| Apoptosis Evasion | Downregulation of pro-apoptotic proteins; Upregulation of Bcl-2 | Increased threshold for cell death initiation upon drug exposure [101]. |
| Tumor Microenvironment | Hypoxia; Exosomal miRNA transfer (e.g., miR-21, miR-130a) | Promotes survival signaling and confers chemoresistance (e.g., cisplatin) via intercellular communication [101] [105]. |
| Protein Damage Response | Elevated proteasome activity | Clearance of drug-damaged proteins, enabling cell survival and fostering cross-resistance [106]. |
Advanced Strategies to Overcome MDR
Direct Inhibition of MDR Proteins
The direct pharmacological inhibition of P-gp has been a long-standing strategy to reverse MDR. The development of P-gp inhibitors has evolved through multiple generations.
- First-generation inhibitors (e.g., Verapamil, Cyclosporine A) were repurposed drugs that often resulted in dose-limiting toxicities due to off-target effects [103].
- Second-generation inhibitors (e.g., Valspodar, Biricodar) exhibited improved specificity but could unpredictably alter the pharmacokinetics of co-administered chemotherapeutics [103].
- Third-generation inhibitors (e.g., Tariquidar, Zosuquidar, Elacridar) were developed to be highly potent and specific to P-gp, with limited impact on cytochrome P450 enzymes, thereby minimizing undesirable drug-drug interactions [103]. Despite promising preclinical results, the clinical translation of P-gp inhibitors has been largely disappointing, attributed to factors such as systemic toxicity, the redundancy of other ABC transporters, and complex pharmacokinetic interplay [102] [103].
Nanomedicine and Advanced Drug Delivery Systems
Nanocarrier-based drug delivery systems offer a powerful workaround to MDR by bypassing efflux pumps and improving drug targeting.
- Mechanisms of Action: Nanoparticles can be internalized via endocytosis, avoiding recognition by P-gp, which is primarily active on the plasma membrane. Furthermore, they can be engineered for co-delivery of a chemotherapeutic agent and an MDR inhibitor, ensuring both compounds reach the same cell simultaneously [102].
- Nanocarrier Types: A variety of platforms have been explored, including polymeric nanoparticles, liposomes, micelles, and inorganic nanoparticles. These systems can be further functionalized with targeting ligands (e.g., antibodies, peptides) that bind to receptors overexpressed on cancer cells, enhancing tumor-specific delivery [102] [103].
- Stimuli-Responsive Systems: "Smart" nanocarriers can be designed to release their payload in response to specific tumor microenvironment triggers such as low pH, elevated glutathione levels, or overexpressed enzymes [102].
Emerging Molecular and Gene-Targeted Strategies
The arsenal against MDR is expanding with the advent of sophisticated molecular and genetic tools.
- Gene Editing Technology: The CRISPR-Cas9 system enables the precise knockout of the MDR1 gene, permanently abrogating P-gp expression and resensitizing cancer cells to chemotherapeutics [103]. While delivery to tumors in vivo remains a challenge, nanoparticle-based delivery of CRISPR components is an area of intense investigation [107].
- RNA Interference (RNAi): Small interfering RNAs (siRNAs) or short hairpin RNAs (shRNAs) can be used to selectively degrade MDR1 mRNA, achieving a transient but potent knockdown of P-gp [103].
- Combination Therapies Targeting Resistance Pathways: Rational combination therapies are showing significant promise. For example, in KRAS-G12C mutant cancers that develop resistance to adagrasib (a KRAS-G12C inhibitor), combination therapy with an SRC kinase inhibitor (e.g., dasatinib) was shown to effectively overcome resistance in preclinical models [108]. Similarly, in BRCA-deficient cancers, resistance to PARP inhibitors can be overcome by co-targeting the ATR/CHK1 DNA damage checkpoint pathway [105].
- Targeting the Protein Damage Response (PDR): The newly identified PDR pathway offers a compelling new therapeutic vulnerability. Clinical studies have demonstrated that proteasome inhibitors like bortezomib can effectively overcome multidrug resistance in colon and breast cancer patients exhibiting elevated proteasome activity, presumably by preventing the clearance of drug-damaged proteins and tipping the balance toward cytotoxicity [106].
Table 2: Advanced Strategies to Counteract MDR
| Strategy | Mechanism of Action | Representative Agents/Technologies | Development Status |
|---|---|---|---|
| 3rd Gen P-gp Inhibitors | High-affinity, non-competitive binding to P-gp to block drug efflux. | Tariquidar, Zosuquidar, Elacridar [103]. | Clinical trials (limited success). |
| Nanoparticle Co-delivery | Bypasses P-gp-mediated efflux via endocytosis; simultaneous delivery of drug + inhibitor. | Polymeric NPs loaded with Doxorubicin & Tariquidar [102]. | Preclinical & early clinical. |
| CRISPR-Cas9 Gene Editing | Precise knockout of the MDR1 gene to abolish P-gp expression. | CRISPR/Cas9 system targeting ABCB1 [103]. | Preclinical research. |
| RNA Interference (RNAi) | Sequence-specific degradation of MDR1 mRNA. | siRNA/shRNA against P-gp [103]. | Preclinical research. |
| Combination Targeted Therapy | Co-inhibition of a primary oncogenic driver and a key resistance pathway. | Adagrasib (KRAS-G12Ci) + Dasatinib (SRCi) [108]. | Preclinical validation. |
| Proteasome Inhibition (PDR) | Blocks clearance of drug-damaged proteins, leading to lethal proteotoxicity. | Bortezomib, other clinically approved proteasome inhibitors [106]. | Investigator-initiated clinical trials. |
Experimental and Technical Approaches
Key Research Reagent Solutions
A well-equipped toolkit is essential for investigating MDR mechanisms and evaluating novel therapeutic strategies.
Table 3: Essential Research Reagents for MDR Studies
| Reagent / Tool | Function / Application | Specific Example |
|---|---|---|
| P-gp Inhibitors | Pharmacological blockade of P-gp efflux activity for in vitro and in vivo resensitization studies. | Tariquidar (3rd generation) [103]. |
| Fluorescent Substrate Dyes | To measure P-gp transport activity via flow cytometry or fluorescence microscopy. | Calcein-AM, Rhodamine 123 [103]. |
| PROTEOSTAT Dye | Detection of protein aggregation and misfolding in the Protein Damage Response (PDR) [106]. | PROTEOSTAT Aggresome Detection Kit [106]. |
| Proteasome Activity Assays | Quantification of proteasome activity, a biomarker for PDR-mediated MDR. | Sensitive commercial kits (e.g., based on fluorogenic substrates) [106]. |
| CRISPR-Cas9 System | For genetic knockout of MDR-associated genes (e.g., ABCB1). | Cas9 nuclease and sgRNA targeting MDR1 [103]. |
| siRNA/shRNA | For transient knockdown of target gene expression to validate MDR targets. | siRNA targeting MDR1 mRNA [103]. |
| 3D Tumor Models | High-fidelity, clinically predictive models for drug sensitivity testing. | Tumor slice cultures, patient-derived organoids [106] [108]. |
Detailed Experimental Protocol: Assessing the Protein Damage Response
The following methodology, adapted from a seminal 2025 study, outlines a comprehensive approach to evaluate protein damage induced by anticancer drugs and the ensuing cellular response [106].
Objective: To characterize the induction of protein damage (misfolding/aggregation) by an anticancer drug and investigate the role of the proteasome in mitigating this damage.
Materials:
- Cancer cell line of interest (e.g., MDA-MB-231).
- Anticancer drug for testing (e.g., Cisplatin, Lapatinib).
- PROTEOSTAT staining solution or equivalent molecular rotor dye.
- Proteasome inhibitor (e.g., Bortezomib).
- Lysis buffer, proteinase K (for LiP-MS).
- Equipment: Flow cytometer or fluorescence microscope, LC-MS/MS system.
Procedure:
- Cell Treatment and Induction of Damage:
- Seed cells and allow to adhere overnight.
- Treat cells with the IC~50~ concentration of the anticancer drug for a short duration (e.g., 1 hour). Include a DMSO vehicle control.
- For rescue experiments, pre-treat cells with a proteasome inhibitor (e.g., 100 nM Bortezomib) for 2-4 hours prior to the addition of the anticancer drug.
Detection of Protein Aggregation (at 1-hour post-treatment):
- Harvest drug-treated and control cells by trypsinization.
- Wash cells with PBS and stain with PROTEOSTAT dye according to the manufacturer's instructions.
- Analyze the level of fluorescence, which corresponds to protein aggregation, immediately using flow cytometry or fluorescence microscopy.
Limited Proteolysis-coupled Mass Spectrometry (LiP-MS) for Detecting Protein Structural Changes (at 1-hour post-treatment):
- Lyse the drug-treated and control cells in a non-denaturing buffer.
- Subject the lysates to limited proteolysis with a broad-spectrum protease like proteinase K.
- Quench the proteolysis reaction and denature the proteins.
- Digest the resulting peptide fragments with trypsin following a standard proteomics workflow.
- Analyze the peptides via Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS).
- Data Analysis: Identify peptides with significantly altered abundance between drug-treated and control samples. Peptides with increased abundance indicate drug-induced structural alterations that made them more accessible to proteinase K, while decreased abundance suggests protection due to drug binding.
Interpretation: An increase in PROTEOSTAT signal upon drug treatment indicates rapid protein misfolding/aggregation. Attenuation of this signal over time (e.g., by 12 hours) suggests active clearance of damaged proteins, which can be blocked by proteasome inhibitors. The LiP-MS data provides a proteome-wide map of specific proteins and domains undergoing structural changes or direct drug binding, enabling the identification of key vulnerable pathways, such as mitochondrial metabolism [106].
Pathway and Workflow Visualizations
Diagram 1: This workflow illustrates the logical relationship between different strategies to overcome MDR, their molecular mechanisms, and the ultimate goal of resensitizing cancer cells to therapy. Key emerging approaches include combination targeted therapy and targeting the Protein Damage Response (PDR) [106] [108] [103].
Diagram 2: This pathway diagram details the sequential steps of the Protein Damage Response (PDR), a recently elucidated mechanism of MDR. It also highlights the therapeutic intervention point—proteasome inhibition—which can disrupt this survival pathway and reverse resistance [106].
The battle against multidrug resistance in cancer is being waged on multiple fronts, from refining the inhibition of classical efflux pumps like P-gp to exploiting new vulnerabilities such as the Protein Damage Response. The future of overcoming MDR lies in personalized medicine approaches, where therapeutic strategies are informed by the specific resistance mechanisms operative in an individual patient's tumor. This necessitates the development of robust biomarkers—such as assays for proteasome activity to identify PDR-high cancers—to guide patient stratification [106] [103]. Furthermore, the complexity of MDR suggests that rational combination therapies that simultaneously target the primary oncogenic drive and key resistance pathways will be more effective than monotherapies. The integration of advanced tools like CRISPR for target validation, nanomedicine for precision delivery, and sophisticated models like organoids for clinically predictive testing will continue to accelerate the discovery and translation of next-generation strategies to counteract MDR proteins, ultimately improving outcomes for cancer patients.
The landscape of cancer treatment has been revolutionized by the development of targeted therapies and immunotherapies, yet both therapeutic classes face significant limitations as monotherapies. Targeted therapies, which inhibit specific oncogenic signaling pathways, often achieve high initial response rates but are frequently limited by the development of resistance within months of treatment [109]. Conversely, immune checkpoint inhibitors (ICIs), which reactivate the anti-tumor immune response, can achieve durable long-term responses but only in a subset of patients, with low overall response rates across many cancer types [109] [110]. This therapeutic landscape has catalyzed the development of rational combination strategies designed to synergize the rapid tumor regression enabled by targeted agents with the durable response potential of immunotherapy [109].
The fundamental rationale for these combinations lies in the ability of many targeted therapies and chemotherapeutic agents to modulate the tumor microenvironment (TME), transforming "cold" immunologically ignorant tumors into "hot" tumors susceptible to immune attack [109] [111]. Specific inhibitors of oncogenic signaling pathways and tumor-associated angiogenesis can activate anti-tumor immune responses by increasing tumor antigen presentation, enhancing intratumoral T cell infiltration, and reversing immunosuppressive mechanisms [109]. Furthermore, emerging research demonstrates that chemotherapy can synergize with immunotherapy by shifting anti-PD-1 resistance phenotypes in tumor cells, potentially overcoming one of the most significant challenges in immuno-oncology [111]. This in-depth technical guide explores the molecular mechanisms, clinical applications, and experimental frameworks underlying these sophisticated combination approaches, providing researchers and drug development professionals with a comprehensive resource for advancing the field of synergistic cancer therapy.
Molecular Mechanisms of Synergism
Modulation of the Tumor Microenvironment
The immunosuppressive tumor microenvironment represents a major barrier to effective anti-tumor immunity. Combination therapies can reverse this immunosuppression through multiple mechanisms. Targeted kinase inhibitors against the MAPK pathway (BRAF and MEK inhibitors) counteract the immunosuppressive TME by increasing the expression of melanoma differentiation antigens, which in turn primes antigen-specific T cells [109]. These inhibitors also augment anti-tumor immunity by increasing intratumoral T cell infiltration and altering the immune status of the TME, likely through blocking signals that elicit T cell exhaustion or apoptosis while downregulating immune suppressive factors or chemokines [109].
Angiogenesis inhibitors targeting VEGFA/VEGFR signaling remodel the tumor vasculature to enhance T cell infiltration while reducing immunosuppressive cell populations [109]. The abnormal tumor vasculature limits immune cell infiltration into tumors; VEGF inhibition can normalize this vasculature, improving drug delivery and enabling more efficient T cell trafficking into the tumor bed [109]. Additionally, epigenetic modulators including DNA methyltransferase inhibitors (e.g., azacitidine) and histone deacetylase inhibitors (e.g., entinostat) enhance tumor immunogenicity by upregulating major histocompatibility complex molecules and natural killer cell receptor ligands while increasing proinflammatory cytokine activity [109].
Table 1: Molecular Mechanisms of TME Modulation by Therapeutic Agents
| Therapeutic Class | Specific Agents | Key Immunomodulatory Effects | Impact on TME |
|---|---|---|---|
| MAPK Pathway Inhibitors | BRAF/MEK inhibitors (e.g., dabrafenib/trametinib) | Increased tumor antigen presentation, enhanced T cell infiltration | Reversal of T cell exhaustion, reduced immunosuppressive factors |
| Angiogenesis Inhibitors | Bevacizumab, lenvatinib, ziv-aflibercept | Vascular normalization, reduced immunosuppressive cell populations | Improved T cell trafficking, altered cytokine/chemokine profile |
| Epigenetic Modulators | Azacitidine, entinostat | Upregulation of MHC molecules, NK cell receptor ligands | Decreased myeloid-derived suppressor cells, enhanced proinflammatory signaling |
Induction of Immunogenic Cell Death and Antigen Presentation
Chemotherapy and targeted agents can stimulate anti-tumor immunity through the induction of immunogenic cell death (ICD), a form of cell death that activates an adaptive immune response against dead cell-associated antigens. Several chemotherapeutic agents, including gemcitabine, induce ICD characterized by the surface exposure of calreticulin, release of high mobility group box 1 (HMGB1), and ATP secretion [111]. These damage-associated molecular patterns (DAMPs) facilitate dendritic cell maturation and cross-presentation of tumor antigens to T cells, essentially turning tumor cells into in situ vaccines [111].
The type I interferon (IFN) pathway serves as a critical mediator of therapy-induced immune activation. Recent research has revealed that a mitochondrial RNA-dependent activation of type I interferon signaling represents a promising mechanism for chemo-immunotherapy synergism [111]. This pathway can be triggered by certain DNA-damaging agents that cause mitochondrial stress and the release of endogenous nucleic acids that activate the cGAS-STING pathway, ultimately leading to IFN production and enhanced dendritic cell cross-priming of tumor-specific CD8+ T cells.
Overcoming Tumor Cell Plasticity and Resistance Mechanisms
Tumor cell plasticity enables cancer cells to evade treatments through phenotypic switching, including epithelial-to-mesenchymal transition (EMT) and transdifferentiation [112]. This plasticity represents a major non-genetic mechanism of resistance to targeted therapies. Combination approaches can target this plasticity by simultaneously inhibiting the primary oncogenic driver and preventing escape pathway activation. For instance, in cancers such as prostate cancer and lung adenocarcinoma, therapy-induced neuroendocrine transdifferentiation (NET) causes resistance to targeted agents; combining these agents with immunomodulators may prevent or reverse this transition [112].
The emergence of drug-tolerant persisters (DTPs) represents another resistance mechanism whereby a subpopulation of tumor cells enters a reversible dormant, stem-like state to survive therapeutic pressure [112]. These DTPs are characterized by their ability to switch between proliferative and dormant states, evading drug targeting. Immunotherapeutic approaches may effectively target these populations by engaging immune surveillance mechanisms that recognize and eliminate these persistent cells before they can cause disease relapse.
Strategic Combination Approaches
Targeted Therapy-Immunotherapy Combinations
Rational combination of targeted agents with immunotherapy leverages the specific molecular vulnerabilities of tumors while engaging the immune system for sustained response. The MAPK pathway represents a prime target for such combinations, as its inhibition not only directly suppresses tumor growth but also reverses immune escape mechanisms. In BRAF-mutant melanoma models, combining BRAF inhibitors with adoptive T cell transfer resulted in stronger anti-tumor responses compared to either modality alone [109]. Similarly, immune checkpoint blockade augments the effect of BRAF inhibitors in metastatic melanoma while activating tumor-infiltrating T cells [109].
The integration of angiogenesis inhibition with immunotherapy represents another promising strategy. VEGF-targeted agents including bevacizumab, lenvatinib, and ziv-aflibercept are being extensively investigated in combination with PD-1/PD-L1 inhibitors across multiple cancer types [109]. The synergistic effect arises from the dual action of vascular normalization (facilitating T cell infiltration) and direct immunomodulatory effects on T cell function.
Table 2: Clinically Investigated Targeted Therapy-Immunotherapy Combinations
| Target | Targeted Therapy | Immunotherapy | Cancer Indications | Phase | NCT Number |
|---|---|---|---|---|---|
| BRAF/MEK | Dabrafenib + Trametinib | Pembrolizumab | Melanoma | II | NCT02858921 |
| BRAF/MEK | Vemurafenib + Cobimetinib | Atezolizumab | Melanoma | II | NCT02303951 |
| MEK | Cobimetinib | Atezolizumab | NSCLC | II | NCT03660701 |
| VEGF | Lenvatinib | Pembrolizumab | Hepatobiliary tumors | II | NCT03895970 |
| VEGF | Bevacizumab | Atezolizumab | HNSCC | II | NCT03818061 |
| PI3K | Duvelisib | Pembrolizumab | HNSCC | I/II | NCT04193293 |
| HDAC | Entinostat | Pembrolizumab | MIBC | II | NCT03978624 |
Chemotherapy-Immunotherapy Combinations
Chemo-immunotherapy combinations represent one of the most practical approaches to improve immunotherapy response rates. Systematic investigation of chemo-immunotherapy synergism has identified specific chemotherapeutic agents that can shift anti-PD-1 resistance in tumor cells [111]. Computational approaches analyzing treatment-induced gene expression changes have enabled the development of a "shift ability score" to quantify a treatment's capability of improving anti-PD-1 response [111].
Gemcitabine, a synthetic pyrimidine nucleoside analog, exemplifies the potential of chemotherapy to enhance immunotherapy efficacy. Beyond its direct cytotoxic effects, gemcitabine induces immunogenic cell death, enhances dendritic cell-dependent cross-presentation of tumor antigens to cytotoxic T cells, and depletes immunosuppressive cell populations in the TME [111]. These immunomodulatory properties make it an ideal partner for immune checkpoint inhibitors.
The FDA has approved several chemo-immunotherapy regimens based on demonstrated clinical benefit, including atezolizumab/pembrolizumab combined with taxanes in triple-negative breast cancer and nivolumab with fluoropyrimidine/platinum regimens in gastric and esophageal adenocarcinomas [111]. These approvals underscore the translational potential of rationally designed chemo-immunotherapy combinations.
Epigenetic Therapy-Immunotherapy Combinations
Epigenetic therapies can reverse cancer-associated epigenetic silencing and enhance tumor immunogenicity. DNA methyltransferase inhibitors (e.g., azacitidine) and histone deacetylase inhibitors (e.g., entinostat) activate both intrinsic and extrinsic apoptosis pathways while enhancing immune recognition [109]. These agents increase the expression of cancer-testis antigens and viral mimicry pathways that enhance tumor cell visibility to the immune system.
Preclinical models demonstrate compelling synergy between epigenetic modulators and immunotherapy. The combination of entinostat and azacitidine with PD-1 and CTLA-4 checkpoint blockers led to complete tumor regression and prevented metastasis in 4T1 tumor mouse models [109]. This combination therapy enhanced anti-tumor response by decreasing the number of granulocytic myeloid-derived suppressor cells in the TME [109]. Similarly, histone deacetylase inhibitors augmented the anti-tumor activity of high-dose interleukin-2 in lung and renal cancer models [109].
Biomarker-Driven Patient Selection and Resistance
Predictive Biomarkers for Combination Therapy
Biomarker-guided patient selection is critical for maximizing the efficacy of combination therapies. While single biomarkers have shown utility, comprehensive biomarker integration better predicts treatment response. A retrospective analysis of advanced cancer patients treated with dual-matched therapy (both gene-targeted agents and ICIs selected based on distinct biomarkers) demonstrated a disease control rate of 53% despite 29% of patients having undergone ≥3 prior therapies [113]. This approach yielded a median progression-free survival of 6.1 months and median overall survival of 9.7 months, with three patients (~18%) achieving prolonged benefit exceeding 3 years [113].
Beyond conventional biomarkers like PD-L1 expression and tumor mutational burden, inflammatory markers and metastatic patterns provide additional predictive value. In advanced non-small cell lung cancer (NSCLC) patients receiving ICIs, serum globulin (GLB) >26.6 g/L, absolute neutrophil count (ANC) >5×10â¹/L, and bone metastasis were independent factors affecting both progression-free and overall survival [114]. These readily measurable clinical parameters offer accessible tools for predicting combination therapy outcomes.
Table 3: Predictive Biomarkers for Combination Therapy Response
| Biomarker Category | Specific Markers | Predictive Value | Clinical Application |
|---|---|---|---|
| Genomic | BRAF V600E, HER2 amplification, KRAS G12C | Selection for targeted therapy component | Guides targeted agent selection within combinations |
| Immunological | PD-L1 expression, TMB, MSI status | Predicts immunotherapy responsiveness | Identifies patients likely to benefit from ICI component |
| Inflammatory | ANC >5×10â¹/L, GLB >26.6 g/L | Negative prognostic indicators | Identifies patients who may require additional interventions |
| Clinical | Bone metastasis, ECOG performance status | Associated with treatment outcomes | Informs overall prognosis and expected benefit |
Molecular Mechanisms of Resistance
Despite the promise of combination approaches, resistance remains a significant challenge. Tumor cell plasticity enables cancer cells to evade targeted therapies through non-genetic mechanisms including phenotypic switching, epithelial-mesenchymal transition (EMT), and transdifferentiation [112]. In cancers such as prostate cancer and lung adenocarcinoma, therapy-induced neuroendocrine transdifferentiation causes resistance to targeted agents [112]. This transition is characterized by the presence of neuroendocrine markers and the absence of original lineage markers, resulting in heightened therapeutic resistance and worse prognosis.
The tumor microenvironment also plays a crucial role in therapeutic resistance. In pancreatic ductal adenocarcinoma, the extensive fibrotic stroma creates a physical barrier to drug delivery, while in glioblastoma, the blood-brain barrier and overexpression of efflux pumps reduce drug concentrations at the tumor site [115]. Additionally, metabolic reprogramming of tumor cells and immune cells within the TME can create an immunosuppressive metabolic landscape characterized by hypoxia, nutrient depletion, and accumulation of toxic metabolites that inhibit anti-tumor immune function [115].
Experimental Approaches and Methodologies
Computational Framework for Identifying Synergistic Combinations
High-throughput computational approaches enable systematic identification of promising chemo-immunotherapy combinations. A recently developed framework integrates transcriptomics data from anti-PD-1-treated tumors and compound-treated cancer cell lines to screen for synergistic interactions in silico [111]. This method analyzes anti-PD-1-induced expression changes in patient tumors to develop a "shift ability score" that quantifies whether a chemotherapy or small molecule inhibitor treatment can shift anti-PD-1 resistance in tumor cells.
The experimental workflow involves several key steps:
- Identification of treatment-induced expression signatures associated with anti-PD-1 response using pre- and post-treatment paired transcriptomic data from patient tumors
- Development of resistance (R) and sensitivity (S) signatures through bootstrapping and cross-validation feature selection
- Integration of compound-treated cancer cell line transcriptomes from large-scale pharmacological datasets (e.g., Connectivity Map)
- Calculation of shift ability scores to quantify a treatment's ability to simultaneously suppress R signature genes and induce S signature genes
This approach has been applied to 41,321 compound-treated and 16,853 shRNA-treated cell line expression profiles, identifying treatments that can potentially shift anti-PD-1 resistance [111]. The methodology has revealed that a mitochondrial RNA-dependent activation of type I interferon signaling may be a promising mechanism for chemo-immunotherapy synergism.
In Vivo and In Vitro Validation Models
Robust experimental models are essential for validating combination therapies. Syngeneic mouse models enable evaluation of combination treatments in immunocompetent settings, allowing researchers to assess both direct anti-tumor effects and immunomodulatory activities. The 4T1 mammary carcinoma model has been used to demonstrate that epigenetic modulators combined with immune checkpoint blockade can achieve complete tumor regression and prevent metastasis by modulating myeloid-derived suppressor cells [109].
Patient-derived organoids and xenografts preserve the tumor heterogeneity and microenvironment characteristics of human cancers, providing more clinically relevant platforms for testing combination strategies. These models are particularly valuable for assessing therapies targeting specific molecular subsets defined by genomic alterations or immune phenotypes.
Functional genomics approaches including CRISPR screens conducted in combination treatment settings can identify genetic determinants of response and resistance. For example, integrated analysis of shRNA-mediated gene inhibition and transcriptomic changes has identified potential targets whose inhibition would induce resistant-to-sensitive (R-to-S) shifting in anti-PD-1 response [111].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating Combination Therapies
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Immune Checkpoint Inhibitors | Anti-PD-1, anti-PD-L1, anti-CTLA-4 antibodies | Blockade of immune inhibitory pathways | Restore T cell-mediated killing of tumor cells |
| Targeted Therapy Compounds | BRAF/MEK inhibitors (dabrafenib/trametinib), VEGF inhibitors (bevacizumab) | Specific pathway inhibition | Directly target oncogenic drivers or tumor-supporting processes |
| Epigenetic Modulators | DNMT inhibitors (azacitidine), HDAC inhibitors (entinostat) | Alteration of epigenetic landscape | Enhance tumor immunogenicity, reverse silencing of tumor suppressor genes |
| Cell Death Assays | Annexin V/PI staining, caspase activation assays | Quantification of cell death | Distinguish immunogenic vs. non-immunogenic cell death |
| Immune Monitoring Tools | Multiplex cytokine assays, multicolor flow cytometry panels, IHC markers (CD8, CD4, FoxP3) | Comprehensive immune profiling | Characterize immune cell populations and functional states in TME |
Visualization of Core Concepts
Signaling Pathways in Combination Therapy Synergism
Diagram 1: Molecular Mechanisms of Combination Therapy Synergism. This diagram illustrates how targeted therapies (MAPK pathway inhibition, VEGF pathway inhibition, epigenetic modulation) and immunotherapy (immune checkpoint inhibition) converge to enhance anti-tumor immunity through multiple complementary mechanisms in the tumor microenvironment.
Computational Screening for Combination Therapy
Diagram 2: Computational Framework for Identifying Synergistic Combinations. This workflow illustrates the in silico screening process for identifying chemotherapy-immunotherapy combinations that can shift anti-PD-1 resistance phenotypes, incorporating transcriptomic data from both patient tumors and compound-treated cell lines.
Combination therapies represent the forefront of oncology research, integrating chemotherapy, targeted therapy, and immunotherapy to achieve synergistic anti-tumor effects. The molecular basis for these synergisms includes enhanced antigen presentation, reversal of immunosuppression, induction of immunogenic cell death, and targeting of tumor cell plasticity. Advanced computational frameworks now enable systematic identification of promising combinations through analysis of treatment-induced gene expression changes and calculation of "shift ability scores" that predict capacity to overcome immunotherapy resistance [111].
Future progress in the field will require deeper understanding of resistance mechanisms and more sophisticated patient selection approaches. The development of dual-matched therapies - selecting both targeted agents and immunotherapies based on distinct biomarkers in individual patients - represents a promising precision oncology strategy [113]. Currently, only 1.3% of clinical trials combining targeted therapies with immune checkpoint inhibitors employ biomarkers for both therapeutic components [113], highlighting a significant opportunity for methodological refinement.
Additionally, overcoming tumor cell plasticity - the ability of cancer cells to switch phenotypes and evade targeted therapies - will require novel combination strategies that simultaneously inhibit primary drivers and prevent escape pathways [112]. As our understanding of the deep molecular mechanisms driving cancer progression and metastasis expands, so too will our capacity to design increasingly effective combination therapies that transform cancer from a lethal to a manageable chronic disease.
Addressing Tumor Heterogeneity Through Personalized Medicine and Re-biopsy Strategies
Tumor heterogeneity represents a fundamental challenge in clinical oncology, contributing significantly to treatment failure, disease progression, and the development of therapeutic resistance. This complexity manifests across multiple dimensions, including spatial heterogeneity (variations across different tumor regions), temporal heterogeneity (evolution over time), and molecular heterogeneity (divergence at genetic, epigenetic, and phenotypic levels) [116] [117]. The profound implications of this diversity are evident in metastatic disease, which accounts for over 90% of cancer-related mortality [35] [42]. The emerging paradigm in precision oncology necessitates a dynamic approach to cancer management, moving beyond static molecular profiling to adaptive strategies that address the evolving nature of malignant tumors through advanced technologies and re-biopsy protocols.
The clinical ramifications of tumor heterogeneity are particularly evident in the context of therapeutic resistance. Intratumoral genetic heterogeneity and non-genetic plasticity represent two major mechanisms through which cancers evade targeted therapies [118]. The former involves the selection and expansion of resistant subclones harboring genetic mutations that confer survival advantages under therapeutic pressure, while the latter encompasses reversible, adaptive changes that allow cancer cells to tolerate treatment without permanent genetic alterations [118]. This comprehensive review examines the current landscape of personalized medicine and re-biopsy strategies designed to overcome these challenges, with particular emphasis on their application within cutting-edge cancer research and drug development.
Molecular Foundations of Tumor Heterogeneity
Genetic and Non-Genetic Diversity in Cancer Ecosystems
The genomic landscape of tumors is characterized by extensive diversity driven by multiple mechanisms. Intra-tumoral heterogeneity (ITH) refers to the genetic diversity present within a single tumor, where distinct subclones carrying different driver mutations can exhibit variations in tumor growth, therapy response, and metastatic potential [116] [117]. Conversely, inter-tumoral heterogeneity describes the genetic diversity observed among tumors of the same histopathological type in different patients, resulting from differences in underlying mutations or microenvironmental contexts [116]. This genetic variability is further complicated by temporal heterogeneity, which emerges as tumors evolve over time through accumulating additional mutations or environmental selection pressures [116] [117].
Beyond genetic alterations, epigenetic regulation significantly contributes to tumor heterogeneity. Epigenetic modifications—including DNA methylation, histone modifications, and chromatin remodeling—enable heritable changes in gene expression without altering the underlying DNA sequence [117]. These modifications allow cancer cells to adapt to microenvironmental stimuli such as oxygen tension, nutrient availability, and therapeutic interventions [117]. The bidirectional crosstalk between genetic and epigenetic mechanisms further amplifies diversity, with somatic mutations occurring in genes encoding epigenetic regulators (DNMT3A, IDH1, H3F3A) and epigenetic silencing of DNA repair genes (MLH1, BRCA1) promoting genomic instability [117].
Table 1: Dimensions of Tumor Heterogeneity and Clinical Implications
| Heterogeneity Type | Definition | Clinical Implications | Detection Methods |
|---|---|---|---|
| Spatial Heterogeneity | Genetic and phenotypic variations across different geographic regions of a single tumor or between primary and metastatic lesions | Incomplete molecular profiling from single biopsies; sampling bias affecting treatment decisions | Multi-region sequencing; liquid biopsy; advanced imaging |
| Temporal Heterogeneity | Evolution of tumor cell features during disease progression under environmental or therapeutic pressure | Emergence of treatment-resistant clones; limited efficacy of initial targeted therapies | Longitudinal liquid biopsy; serial tissue sampling |
| Intra-tumoral Heterogeneity | Presence of distinct subclones with different genotypes and phenotypes within an individual tumor | Differential drug sensitivity within same tumor; partial treatment response | Single-cell sequencing; multi-region analysis |
| Inter-tumoral Heterogeneity | Molecular differences among tumors of same histopathological type in different patients | Variable treatment responses among patients with same cancer type; need for personalized approaches | Comprehensive genomic profiling; molecular subtyping |
The Metastatic Cascade and Organotropism
The process of metastasis exemplifies the functional consequences of tumor heterogeneity, with circulating tumor cells (CTCs) successfully colonizing distant organs through a complex multistep cascade. The "seed and soil" hypothesis, first proposed by Stephen Paget in 1889, provides a framework for understanding the non-random patterns of metastatic dissemination, wherein cancer cells ("seeds") exhibit specific affinities for particular organ microenvironments ("soil") [37] [35]. Modern oncology has substantiated this theory with molecular insights, identifying specific signaling pathways and cellular interactions that drive organotropism [35].
Breast cancer subtypes demonstrate distinct metastatic patterns that illustrate the principles of organotropism. Bone represents the most common site for breast cancer metastasis, accounting for approximately 65-75% of metastatic cases, with ER+ luminal A and B subtypes exhibiting particular predisposition to skeletal colonization [37]. In contrast, HER2+ and triple-negative breast cancers (TNBCs) demonstrate preference for visceral organs, including the brain and lungs [37]. Liver metastasis develops in 40-50% of breast cancer patients, with HER2-positive subtypes showing increased propensity for hepatic colonization [37]. These patterns reflect underlying molecular compatibilities between specific cancer cell populations and organ microenvironments, mediated through adhesion molecules, chemokine receptors, and growth factor interactions [35].
Technological Advances in Heterogeneity Assessment
Genomic Profiling and Sequencing Technologies
Next-generation sequencing (NGS) technologies have revolutionized our capacity to characterize tumor heterogeneity at unprecedented resolution. Comprehensive genomic profiling (CGP) enables the simultaneous detection of multiple clinically relevant genomic alterations, including single nucleotide variants (SNVs), insertions and deletions (indels), copy number alterations (CNAs), and structural variants (SVs) across hundreds of cancer-related genes [119]. The clinical utility of this approach is evidenced by studies demonstrating that patients receiving genomic profiling-matched targeted therapies experience significantly improved response rates (11% vs. 5%), longer failure-free survival (3.4 vs. 2.9 months), and extended overall survival (8.4 vs. 7.3 months) compared to those receiving unmatched therapies [119].
The evolution of sequencing technologies has progressed from bulk tumor analysis to sophisticated single-cell approaches. Single-cell multiomics enables the concurrent measurement of multiple molecular modalities (genomics, epigenomics, transcriptomics, proteomics) within individual cells, providing unprecedented resolution of cellular diversity and revealing rare cell populations that drive tumor evolution and therapeutic resistance [120]. Technological platforms such as microfluidics, droplet-based sequencing, and combinatorial indexing have dramatically increased the scale and precision of these analyses, facilitating the construction of comprehensive cellular atlases for both diseased and healthy tissues [120].
Table 2: Advanced Technologies for Assessing Tumor Heterogeneity
| Technology | Application | Resolution | Key Advantages | Limitations |
|---|---|---|---|---|
| Next-Generation Sequencing (NGS) | Detection of mutations, CNAs, fusions across cancer genes | Tissue-level | Comprehensive profiling of known cancer genes; established clinical validity | May miss rare subclones; requires sufficient tumor content |
| Single-Cell RNA Sequencing (scRNA-seq) | Transcriptome profiling of individual cells | Single-cell | Identifies rare cell populations; reveals cellular heterogeneity | Technical artifacts from tissue dissociation; high cost |
| Single-Nuclei RNA Sequencing (snRNA-seq) | Gene expression analysis from isolated nuclei | Single-nucleus | Compatible with frozen/archived tissues; reduces dissociation bias | Limited cytoplasmic RNA detection |
| Liquid Biopsy | Detection of ctDNA, CTCs in blood | Molecule/cell | Non-invasive; enables serial monitoring; captures spatial heterogeneity | Lower sensitivity for early-stage disease; analytical challenges |
| Spatial Transcriptomics | Gene expression within tissue architecture | Tissue region with spatial context | Preserves spatial information; correlates morphology with molecular features | Lower resolution than single-cell methods; complex data analysis |
Liquid Biopsy and Minimally Invasive Monitoring
Liquid biopsy has emerged as a transformative approach for assessing tumor heterogeneity through minimally invasive blood collection. This methodology encompasses the analysis of multiple biomarkers, including circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), extracellular vesicles (EVs), and cell-free RNA (cfRNA) [121]. The clinical applications of liquid biopsy span early detection, prognostic stratification, therapy selection, resistance monitoring, and surveillance for recurrence [121].
CtDNA analysis offers particular advantages for tracking tumor evolution, with fragments typically ranging from 20-50 base pairs and representing only 0.1-1.0% of total cell-free DNA [121]. The short half-life of ctDNA (approximately 1-2 hours) enables real-time assessment of tumor burden and molecular alterations, providing a dynamic picture of clonal evolution under therapeutic pressure [121]. Studies in colorectal cancer have demonstrated that monitoring specific mutations (APC, KRAS, TP53, PIK3CA) in ctDNA can effectively track disease progression and treatment response [121]. Similarly, in non-small cell lung cancer (NSCLC), ctDNA analysis has shown utility for detecting EGFR mutations and monitoring emerging resistance mechanisms, with clinical guidelines now supporting its use when tissue sampling is insufficient [119] [121].
CTC analysis provides complementary information by enabling functional characterization of viable tumor cells in circulation. Despite their rarity (approximately 1 CTC per 1 million leukocytes), CTCs play crucial roles in the metastatic cascade and can be enriched using various technologies, including the FDA-cleared CellSearch system [121]. The clinical significance of CTC enumeration is well-established in breast cancer, where elevated levels correlate with reduced progression-free and overall survival, leading to incorporation into prognostic guidelines [121]. Emerging technologies now enable molecular characterization of CTCs, including genomic, transcriptomic, and protein-level analyses that provide insights into metastatic potential and therapeutic vulnerabilities.
Liquid Biopsy Analysis Workflow
Personalized Medicine Strategies for Heterogeneous Tumors
Dynamic Precision Medicine and Treatment Sequencing
The limitations of conventional precision medicine, which typically matches therapies to static molecular profiles at single timepoints, have prompted the development of dynamic approaches that explicitly address tumor evolution. Dynamic Precision Medicine (DPM) represents an advanced framework that designs individualized treatment sequences by simulating genetic evolutionary dynamics and non-genetic plasticity within heterogeneous tumors [118]. This approach balances the immediate objective of tumor reduction with the long-term goal of preventing or delaying the emergence of resistant subclones through strategic drug sequencing.
Mathematical modeling frameworks that incorporate both irreversible genetic resistance and reversible non-genetic resistance mechanisms demonstrate that DPM strategies significantly outperform conventional personalized medicine approaches [118]. In simulations involving over 6 million virtual patients, DPM-based protocols achieved substantial improvements in survival outcomes by strategically alternating between targeted agents to manage competing resistant populations [118]. For example, in NSCLC with EGFR mutations, DPM principles can guide the sequential use of EGFR tyrosine kinase inhibitors (afatinib, osimertinib) to address divergent resistance mechanisms, including T790M gatekeeper mutations, HER2 amplification, and RAS-MAPK pathway activation [118].
Targeting the Tumor Microenvironment
The tumor microenvironment (TME) constitutes a critical component of tumor heterogeneity, comprising diverse non-malignant cell types (immune cells, fibroblasts, endothelial cells) and non-cellular elements (extracellular matrix, cytokines) that collectively influence cancer progression and therapeutic response [116] [117]. The composition and functional state of TME components exhibit substantial spatial and temporal heterogeneity, contributing to variations in drug delivery, immune evasion, and metastatic potential [117].
Therapeutic strategies targeting the TME include immune checkpoint inhibitors (anti-PD-1/PD-L1, anti-CTLA-4), antiangiogenic agents (VEGF inhibitors), and stromal modifying therapies [35] [42]. The complex interplay between cancer cells and their microenvironment also enables novel combination approaches, such as combining TME-targeting therapies with genomic alteration-matched targeted agents to address both cellular compartments simultaneously [42]. Emerging evidence suggests that the TME not only responds to but actively shapes tumor evolution through selective pressures that favor specific subclones, creating dynamic feedback loops that necessitate comprehensive therapeutic targeting [116].
Dynamic Precision Medicine Addressing Heterogeneity
Re-biopsy Strategies and Longitudinal Monitoring
Protocol for Comprehensive Re-biopsy Implementation
The dynamic nature of tumor evolution under therapeutic pressure necessitates longitudinal molecular assessment through repeat tissue sampling and liquid biopsy. Re-biopsy protocols should be strategically timed to capture clinically relevant transitions, including initial resistance emergence (radiographic progression or biomarker elevation), histologic transformation (e.g., small cell conversion in lung adenocarcinoma), and metastatic progression (new lesion development) [122] [121]. Tissue sampling should prioritize metastatic sites accessible through minimally invasive approaches while considering lesion viability and potential procedural risks.
Multi-region sampling within heterogeneous lesions enhances the detection of resistant subclones that may be geographically restricted. For example, in glioblastoma, spatial heterogeneity contributes to substantial molecular divergence between tumor regions, with subclonal mutations present in only specific geographic areas [122]. Advanced imaging guidance (MRI, CT, PET) can target regions with distinct radiographic features (enhancement patterns, metabolic activity) to maximize the representation of molecular diversity [122]. When tissue sampling is infeasible or high-risk, liquid biopsy provides a complementary approach for capturing heterogeneity, though with limitations in detecting structural variants and representing the complete genomic landscape [121].
Analytical Considerations for Longitudinal Samples
The computational analysis of longitudinal samples requires specialized bioinformatic approaches to distinguish meaningful clonal evolution from technical artifacts. Sequencing data from serial samples should be processed through integrated pipelines that enable accurate variant calling while accounting for differences in tumor content, DNA quality, and sequencing depth [119] [120]. Phylogenetic reconstruction algorithms can model evolutionary relationships between subclones across timepoints, identifying patterns of linear progression, branching evolution, or neutral drift [120].
The interpretation of molecular changes between biopsies must differentiate between driver alterations that confer selective advantages and passenger alterations that represent collateral genetic damage. Functional validation of putative resistance mechanisms through experimental models (patient-derived organoids, xenografts) strengthens clinical translation [122] [120]. For example, in recurrent glioblastoma, patient-derived organoids enable functional drug screening to identify active agents against therapy-resistant populations, guiding subsequent treatment selection [122].
Table 3: Re-biopsy Strategy Implementation Framework
| Clinical Scenario | Recommended Approach | Sampling Method | Analytical Priorities | Therapeutic Implications |
|---|---|---|---|---|
| Progression on Targeted Therapy | Tissue biopsy of progressing lesion + liquid biopsy | Image-guided core biopsy or liquid biopsy | Identification of on-target vs. off-target resistance mechanisms | Selection of next-line targeted therapy or combination approach |
| Metastatic Relapse After Period of Control | Biopsy of new metastatic site + liquid biopsy | Least invasive accessible site + blood collection | Assessment for clonal evolution and new driver alterations | Adaptation of treatment strategy based on molecular evolution |
| Mixed Response to Therapy | Multi-region sampling of responding and progressing sites | Multiple image-guided biopsies if feasible | Comparison of molecular profiles across different regions | Locally ablative therapy for resistant foci + systemic therapy modification |
| Histologic Transformation Suspected | Tissue biopsy with adequate sample for histology | Core biopsy preserving architecture | Pathological confirmation + molecular profiling of transformed cells | Switch to histology-appropriate treatment regimen |
The Scientist's Toolkit: Essential Research Reagents and Technologies
Table 4: Essential Research Reagents and Platforms for Heterogeneity Studies
| Category | Specific Reagents/Platforms | Research Application | Key Considerations |
|---|---|---|---|
| Single-Cell Isolation | 10X Genomics Chromium, Fluidigm C1, DEPArray | High-throughput single-cell analysis, rare cell population isolation | Recovery efficiency, viability maintenance, representation bias |
| Spatial Biology | 10X Visium, NanoString GeoMx, Multiplexed IF/IHC | Tissue context preservation, tumor-immune interactions mapping | Resolution limits, multiplexing capacity, data integration complexity |
| Liquid Biopsy Technologies | CellSearch (CTCs), ddPCR, NGS panels (ctDNA) | Non-invasive monitoring, resistance mechanism tracking | Sensitivity for rare variants, standardization needs, blood collection protocols |
| Organoid Culture | Matrigel-based 3D culture, defined media formulations | Functional studies, drug screening, personalized therapy testing | Culture success rates, representation of original heterogeneity, scalability |
| Multi-omics Integration | Seurat, Monocle, CITE-seq, ATAC-seq | Combined genomic, transcriptomic, epigenomic profiling | Data harmonization, computational resources, analytical expertise |
| CRISPR Screening | Pooled libraries, base editing, CRISPRi/a | Functional genomics, resistance mechanism identification | Delivery efficiency, off-target effects, validation requirements |
The relentless evolution of cancer ecosystems demands equally dynamic approaches to diagnosis and treatment. Addressing tumor heterogeneity through advanced personalized medicine and systematic re-biopsy strategies represents a paradigm shift in oncology, moving from static molecular profiling to adaptive therapeutic approaches that acknowledge and anticipate cancer evolution. The integration of comprehensive genomic characterization, longitudinal monitoring through liquid biopsy, and computational modeling of tumor dynamics provides a framework for staying ahead of the evolutionary trajectories that underlie treatment failure.
Future progress will depend on several critical advancements: (1) the development of more sophisticated single-cell and spatial technologies that capture multidimensional heterogeneity with greater resolution and throughput; (2) the validation of functional precision medicine approaches using patient-derived models that preserve tumor heterogeneity for drug testing; (3) the implementation of artificial intelligence algorithms that integrate complex molecular, clinical, and radiographic data to predict evolutionary trajectories and optimize therapeutic sequences; and (4) the establishment of standardized protocols for longitudinal sampling and analysis that enable robust comparison across studies and institutions [122] [120]. As these innovations mature, they will progressively transform cancer management from reactive to proactive, ultimately improving outcomes for patients with heterogeneous and evolving malignancies.
Evaluating Therapeutic Efficacy and Emerging Clinical Targets
Comparative Analysis of Monotherapy vs. Combination Regimen Efficacy
Therapeutic resistance represents a defining challenge in modern oncology, directly contributing to disease relapse and poor patient outcomes [115]. The selection between monotherapy and combination regimens is a critical decision point in cancer drug development and clinical practice. While monotherapy can be effective, its utility is often limited by diverse resistance mechanisms, including genetic alterations, epigenetic reprogramming, and tumor microenvironment interactions [115]. Combination therapies have emerged as a promising strategy to overcome these limitations through multi-targeted attacks on cancer cell signaling, potentially delaying resistance and improving therapeutic efficacy [105]. This analysis systematically examines the molecular foundations, clinical evidence, and methodological frameworks guiding the evaluation of these treatment paradigms within the context of cancer progression and metastasis research.
Molecular Mechanisms of Therapeutic Resistance and Rationale for Combination Approaches
Fundamental Resistance Mechanisms Limiting Monotherapy
Cancer cells employ sophisticated biological strategies to evade single-agent therapies through both intrinsic and acquired resistance mechanisms. At the genetic level, mutations in drug targets—such as the T790M and C797S mutations in epidermal growth factor receptor (EGFR) in non-small cell lung cancer (NSCLC)—directly impair drug binding and efficacy [115]. Tumor heterogeneity further enables the selection of resistant subclones under therapeutic pressure, leading to disease progression [115].
Beyond genetic alterations, resistance is reinforced through parallel survival pathway activation, metabolic reprogramming, and dynamic interactions with the tumor microenvironment. The dense fibrotic stroma in malignancies like pancreatic ductal adenocarcinoma creates physical barriers to drug delivery, while cancer-associated fibroblasts (CAFs) secrete factors that promote tumor survival [115]. Additionally, non-coding RNA networks and epigenetic modifications contribute to the establishment of resistant phenotypes that can withstand monotherapy approaches [115].
Scientific Rationale for Combination Therapy
Combination regimens are designed to simultaneously target multiple oncogenic dependencies and resistance pathways, creating synthetic lethal interactions that enhance cancer cell killing while potentially delaying the emergence of resistance [105]. The theoretical foundations for combination approaches include:
- Horizontal Blockade: Targeting parallel signaling pathways that compensate for inhibited drivers
- Vertical Blockade: Concurrent inhibition of upstream and downstream elements within a single pathway
- Microenvironment Modulation: Disrupting tumor-stroma interactions that support cancer cell survival
- Immome Activation: Overcoming immune evasion mechanisms while enhancing antitumor immunity
The critical challenge lies in identifying optimal drug pairings that maximize synergistic efficacy while maintaining manageable toxicity profiles.
Clinical Efficacy Comparison Across Cancer Types
Table 1: Clinical Outcomes of Monotherapy vs. Combination Regimens in Solid Tumors
| Cancer Type | Therapeutic Context | Monotherapy Outcomes | Combination Regimen | Combination Outcomes |
|---|---|---|---|---|
| HR+/HER2- Breast Cancer | ESR1-mutated after AI + CDK4/6i | Fulvestrant: mPFS 2.1 months [123] | Vepdegestrant (PROTAC) | mPFS 5.0 months [123] |
| HR+/HER2- Breast Cancer | PIK3CA-mutated, endocrine-resistant | Palbociclib + Fulvestrant: mOS 27 months [123] | Inavolisib + Palbociclib + Fulvestrant | mOS 34 months [123] |
| HER2+ Metastatic Breast Cancer | First-line treatment | THP regimen: 2-yr PFS 52% [123] | T-DXd + Pertuzumab | 2-yr PFS 70% [123] |
| TNBC | First-line, PD-L1+ | Chemotherapy + Pembrolizumab: 12-mo PFS rate 63% [123] | Sacituzumab Govitecan + Pembrolizumab | 12-mo PFS rate 72% [123] |
| KRAS G12C NSCLC | Adagrasib monotherapy | Overall response: 32% [124] | Adagrasib + mTOR inhibitor (preclinical) | Improved efficacy in KEAP1/STK11 co-mutation models [124] |
| Refractory Lymphoma | Post-CAR T failure | Poor prognosis [124] | Olaparib + HDC + ASCT | ORR 100%, CR 90%, EFS 71% in prior CAR T failure [124] |
Table 2: Efficacy of Combination Immune Checkpoint Inhibition
| Cancer Type | Combination Approach | Mechanistic Rationale | Key Efficacy Findings |
|---|---|---|---|
| Multiple Cancers | Anti-LAG-3/TIGIT bispecific antibody (ZGGS15) + Anti-PD-1 | Dual immune checkpoint blockade enhances T-cell activation and reverses exhaustion [105] | Synergistic tumor growth inhibition without cytokine release syndrome in preclinical models [105] |
| HNSCC | X-ray/proton radiotherapy + Anti-PD-L1 | Radiation induces immunogenic cell death and enhances tumor antigen presentation [105] | Synergistic effects in both immunogenic and less immunogenic models; proton radiotherapy + ICI superior in poorly differentiated tumors [105] |
| Metastatic Uveal Melanoma | Pembrolizumab + Lenvatinib | PD-1 inhibition reverses T-cell exhaustion while TKI modulates immunosuppressive microenvironment [125] | Preliminary results show promising efficacy (PLUME trial) [125] |
Experimental Methodologies for Evaluating Treatment Strategies
Resistance Mechanism Elucidation
Single-Cell RNA Sequencing (scRNA-seq) Protocol:
- Cell Preparation: Harvest viable tumor cells from patient-derived xenografts or fresh tissue specimens using collagenase-based dissociation
- Library Construction: Utilize 10X Genomics Chromium platform for droplet-based encapsulation and barcoding with unique molecular identifiers (UMIs)
- Sequencing: Perform high-depth sequencing on Illumina platforms (minimum 50,000 reads/cell)
- Bioinformatic Analysis: Process raw data using Cell Ranger pipeline, followed by dimensionality reduction (UMAP/t-SNE) and cluster identification using Seurat or Scanpy workflows
- Application: Identified transcription factors (FOSL1, NFE2L2, ELF3) driving paclitaxel resistance in TNBC through cell cycle dysregulation and innate immune pathway activation [105]
Circulating Tumor DNA (ctDNA) Monitoring Protocol:
- Blood Collection: Draw Streck tubes (10mL) and process within 6 hours with double centrifugation protocol
- Cell-Free DNA Extraction: Use QIAamp Circulating Nucleic Acid Kit with elution in 45μL AE buffer
- Library Preparation: Employ hybrid capture-based methods targeting cancer-specific mutations (e.g., ESR1, PIK3CA, EGFR)
- Sequencing & Analysis: Perform ultra-deep sequencing (>10,000X coverage) with duplex molecular barcoding; variant calling using custom algorithms accounting for clonal hematopoiesis
- Clinical Application: SERENA-6 trial demonstrated ctDNA-guided ESR1 mutation detection enables early therapy switching to camizestrant, significantly improving progression-free survival [123]
Combination Therapy Screening
High-Throughput Synergy Screening Workflow:
- Platform Setup: Utilize 384-well plates with automated liquid handling systems
- Compound Administration: Implement checkerboard design with serial dilutions of both agents (typically 8 concentrations each)
- Viability Assessment: Measure cell viability at 72-96 hours using CellTiter-Glo luminescent assay
- Data Analysis: Calculate combination indices using Chou-Talalay method with CompuSyn software; values <0.9 indicate synergy, 0.9-1.1 additive effect, >1.1 antagonism
- Validation: Confirm synergistic interactions in 3D spheroid models and patient-derived organoids
Predictive Biomarkers and Computational Approaches
Biomarker-Driven Patient Stratification
The development of predictive biomarkers is essential for optimizing patient selection for both monotherapy and combination approaches. Key biomarker classes include:
- Genomic Alterations: Specific mutations (e.g., KRAS G12C, ESR1, PIK3CA) that determine drug sensitivity
- Gene Expression Signatures: Transcriptomic profiles predictive of pathway dependence
- Microenvironmental Factors: Immune contexture scores, fibroblast activation markers
- Dynamic Biomarkers: ctDNA mutation clearance as early indicator of treatment response
In KRAS G12C-mutant NSCLC, co-mutations in KEAP1 and STK11 are associated with reduced survival to adagrasib monotherapy (32% response rate), identifying a patient population that may benefit from combination strategies with mTOR inhibition [124]. Similarly, in breast cancer, ESR1 mutations detected via ctDNA monitoring predict resistance to aromatase inhibitor/CDK4/6 inhibitor combinations and identify candidates for early transition to next-generation SERDs like camizestrant [123].
Computational Biology Platforms
Advanced computational approaches are revolutionizing treatment strategy prediction. The Genialis Supermodel, a foundation model trained on nearly 1 million harmonized transcriptomic samples, maps individual patient tumors into biologically meaningful subspaces to predict therapeutic response [126]. This large molecular model can distinguish contexts where monotherapy is sufficient versus those requiring combination approaches by capturing biology linked to responses across multiple therapeutic classes, including KRAS inhibitors, EGFR inhibitors, and immune checkpoint inhibitors [126].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms for Therapy Evaluation Studies
| Reagent/Platform | Primary Function | Research Application |
|---|---|---|
| 10X Genomics Chromium | Single-cell partitioning and barcoding | Enables scRNA-seq analysis of tumor heterogeneity and resistance mechanisms [105] |
| CellTiter-Glo Assay | Luminescent measurement of ATP content | Quantifies cell viability in high-throughput drug screening [105] |
| Circulating Nucleic Acid Kits | Stabilization and extraction of cell-free DNA | Facilitates ctDNA analysis for resistance mutation monitoring [123] |
| Patient-Derived Organoids | 3D culture systems from patient tumors | Provides physiologically relevant models for drug testing [115] |
| Genialis Supermodel | Foundation model of cancer biology | Predicts monotherapy and combination therapy responses using transcriptomic data [126] |
| Combinatorial Drug Screening Platforms | Automated liquid handling and readout systems | Enables systematic evaluation of drug interactions in matrix designs [105] |
The comparative analysis of monotherapy versus combination regimens reveals a complex therapeutic landscape where optimal strategy selection depends on understanding the multidimensional nature of cancer biology. While monotherapy remains appropriate for molecularly defined populations without pre-existing resistance mechanisms, combination approaches demonstrate superior efficacy in overcoming diverse resistance pathways and delaying disease progression across multiple cancer types. The future of cancer therapeutics lies in biomarker-driven, adaptive treatment strategies that leverage real-time molecular monitoring, computational prediction platforms, and rationally designed combinations targeting both cancer cell-intrinsic and microenvironmental resistance mechanisms. As our understanding of cancer evolution under therapeutic pressure deepens, the strategic integration of monotherapy and combination approaches throughout the treatment continuum will be essential for achieving durable disease control.
The metastasis of malignant tumors accounts for over 90% of cancer-related deaths, posing a formidable challenge in clinical oncology [35]. This intricate process, driven by cancer stem cells (CSCs) with properties such as self-renewal, differentiation, invasion, and drug resistance, represents a pivotal biological bottleneck in treatment efficacy [127]. The validation of novel therapeutic targets against cancer progression and metastasis thus constitutes an urgent priority in translational cancer research. Current pharmacological interventions face significant limitations including high toxicity, development of resistance, and inconsistent patient outcomes, highlighting the critical need for target validation frameworks that can reliably bridge fundamental biological discoveries to clinical application [127] [35]. This technical guide provides a comprehensive roadmap for validating novel molecular targets, from initial discovery through sophisticated preclinical assessment to clinical trial design, with particular emphasis on targets relevant to metastasis and CSC biology.
Phase 1: Target Discovery and Preliminary Validation
Leveraging Molecular Insights into Metastasis and Stemness
Target discovery begins with elucidating the deep molecular mechanisms governing cancer progression. Key processes include epithelial-mesenchymal transition (EMT), organ-specific tropism governed by the "seed and soil" hypothesis, and CSC maintenance pathways [127] [35]. The "seed and soil" theory posits that successful metastasis requires compatible interactions between circulating tumor cells (the "seed") and microenvironments of distant organs (the "soil"), creating permissive niches for colonization [35]. Understanding these dynamics reveals potential vulnerabilities for therapeutic intervention.
Research should prioritize targets with demonstrable roles in these fundamental processes, such as proteases involved in invasion, cytokines mediating microenvironment crosstalk, and stemness maintenance pathways. For example, PSMD14 has been identified as highly expressed across multiple cancers where it functions as an oncogene by promoting deubiquitination of SNAIL, thereby stabilizing this key EMT regulator [127]. Similarly, BMI-1 serves as a critical regulator of CSC stemness, with overexpression correlating with tumor progression and poor prognosis in colorectal cancer [127].
Leverage established pathway databases to contextualize potential targets within broader molecular networks. The KEGG PATHWAY database provides manually drawn pathway maps representing molecular interaction, reaction, and relation networks, including cancer-relevant pathways such as MAPK signaling, Ras signaling, and HIF-1 signaling [128]. These resources enable researchers to identify critical nodes within pathological processes and predict potential compensatory mechanisms that might limit therapeutic efficacy.
Table 1: Key Bioinformatics Resources for Target Discovery
| Resource Name | Primary Application | Utility in Target Validation |
|---|---|---|
| KEGG PATHWAY [128] | Pathway mapping and analysis | Contextualizing targets within signaling networks and disease mechanisms |
| PubMedQA [129] | Biomedical literature retrieval | Accessing current research on potential targets and their biological roles |
| BioGPT [129] | Biomedical text generation | Synthesizing information across scientific literature |
Phase 2: Preclinical Validation Strategies
In Vitro Functional Assays
Rigorous in vitro assessment establishes causal relationships between target modulation and phenotypic outcomes. The following methodologies are essential for validating targets involved in metastasis and CSC biology:
3.1.1 Invasion and Migration Assays
- Transwell/Boyden Chamber Assays: Quantify invasive capacity through Matrigel-coated membranes toward chemoattractants. Calculate invasion index as percentage of cells traversing matrix.
- Scratch/Wound Healing Assays: Measure 2D migration capacity. Create uniform wound, image at 0, 12, 24, and 48 hours, and quantify closure percentage using image analysis software.
- 3D Spheroid Invasion Assays: Embed tumor spheroids in collagen matrices and quantify invasive protrusions over 72-96 hours.
3.1.2 Cancer Stem Cell Functional Assays
- Sphere Formation Assays: Plate single-cell suspensions in ultra-low attachment plates with serum-free media supplemented with EGF, bFGF, and B27. Quantify primary and secondary sphere formation efficiency after 7-14 days.
- ALDH Activity Assessment: Use ALDEFLUOR assay to identify and sort ALDH-high population via FACS. Validate stemness properties through in vitro and in vivo limiting dilution assays.
- Drug Resistance Profiling: Compare viability of CSC-enriched populations versus bulk tumor cells after exposure to standard chemotherapeutics.
Molecular Validation Techniques
3.2.1 Target Engagement Assessment
- Cellular Thermal Shift Assay (CETSA): Measure target protein thermal stability changes following compound treatment to confirm direct binding.
- Drug Affinity Responsive Target Stability (DARTS): Evaluate protease sensitivity changes in target proteins after compound binding.
- Surface Plasmon Resonance (SPR): Quantify binding kinetics and affinity between therapeutic compounds and purified target proteins.
3.2.2 Downstream Pathway Modulation
- Western Blot Analysis: Detect changes in phosphorylation status and expression levels of pathway components following target inhibition.
- RNA Sequencing: Conduct transcriptomic profiling to identify differentially expressed genes and pathway enrichment after target modulation.
- Proteomic Analysis: Utilize mass spectrometry-based approaches to quantify global protein expression and phosphorylation changes.
In Vivo Validation Models
3.3.1 Experimental Metastasis Models
- Tail Vein Injection Models: Inject luciferase-tagged tumor cells intravenously to monitor metastatic colonization to specific organs via bioluminescent imaging.
- Orthotopic Implantation Models: Implant tumor cells into their native organ microenvironment (e.g., mammary fat pad for breast cancer) to recapitulate the complete metastatic cascade.
- Patient-Derived Xenograft (PDX) Models: Establish tumors from patient samples in immunocompromised mice to maintain tumor heterogeneity and predictive value.
3.3.2 Spontaneous Metastasis Models
- Resection-Based Models: Surgically remove primary orthotopic tumors after establishment and monitor for spontaneous metastasis development.
- Genetically Engineered Mouse Models (GEMMs): Utilize tissue-specific inducible systems to initiate tumorigenesis and study metastasis in immunocompetent settings.
Phase 3: Translational Development and Clinical Trial Design
The Bench to Bedside Pipeline
Translating validated targets into clinical candidates requires navigating a complex, multi-stage process typically spanning 10-15 years at an average cost of £1 billion [130]. Only approximately 10% of potential drugs successfully complete this journey from preclinical discovery to clinical application [130]. The pipeline consists of several distinct phases:
Diagram 1: Drug Development Pipeline
4.1.1 Discovery Phase Identify therapeutic targets and screen compound libraries (often thousands of candidates) to find lead compounds with desired activity. Approaches include high-throughput screening and rational drug design utilizing artificial intelligence [130] [131].
4.1.2 Preclinical Development Conduct rigorous testing of candidate compounds using computer models, human cells, and animal studies to establish proof-of-concept, initial safety profile, and pharmacological properties [130]. This phase focuses on identifying potential toxicity issues and determining appropriate starting doses for human trials.
Clinical Trial Design Considerations for Novel Targets
4.2.1 Phase I Trial Design
- Primary Objective: Establish safety profile, recommended Phase II dose (RP2D), and maximum tolerated dose (MTD).
- Patient Population: Typically patients with advanced, treatment-refractory malignancies.
- Key Endpoints: Incidence and severity of adverse events, dose-limiting toxicities, pharmacokinetic parameters.
- Design Options: 3+3 dose escalation, accelerated titration, or model-based designs.
4.2.2 Phase II Trial Design
- Primary Objective: Preliminary efficacy assessment and further safety evaluation.
- Patient Population: Molecularly selected patients likely sensitive to target inhibition.
- Key Endpoints: Objective response rate, progression-free survival, biomarker correlates.
- Design Options: Single-arm versus randomized designs, with potential for biomarker-stratified enrollment.
4.2.3 Phase III Trial Design
- Primary Objective: Confirm efficacy in randomized setting and establish benefit-risk profile.
- Patient Population: Broadly representative population with strict inclusion/exclusion criteria.
- Key Endpoints: Overall survival, quality of life measures, time to metastasis.
- Design Options: Randomized controlled trials, potentially with adaptive features.
Biomarker-Driven Clinical Development
Incorporate biomarker strategies throughout clinical development to establish proof-of-mechanism and identify responsive populations:
4.3.1 Pharmacodynamic Biomarkers
- Assess target modulation in tumor tissue or surrogate tissues.
- Examples: phosphorylation status of downstream effectors, pathway component expression.
4.3.2 Predictive Biomarkers
- Identify patient subsets most likely to respond to therapy.
- Examples: PSMD14 expression levels for Thiolatia response, BMI-1 status for PTC-209 sensitivity [127].
4.3.3 Monitoring Biomarkers
- Track emergence of resistance and disease evolution during treatment.
- Examples: circulating tumor DNA analysis, CSC frequency in serial biopsies.
Case Studies: Emerging Therapeutic Strategies
Novel Agents in Development
Table 2: Promising Novel Agents Targeting Metastasis and Cancer Stem Cells
| Agent | Molecular Target | Mechanism of Action | Development Stage |
|---|---|---|---|
| Thiolatia (THL) [127] | PSMD14 (JAMM domain-containing protease) | Zinc chelator that inhibits deubiquitination of SNAIL, reversing EMT and enhancing chemotherapy sensitivity | Preclinical |
| Sulfarotene (WYC-209) [127] | RARα-SOS2-RAS axis | Upregulates RARα, inhibiting SOS2 expression and blocking RAS activation in tumor-repopulating cells | Preclinical |
| PTC-209 (HA-NPs formulation) [127] | BMI-1 | Nanodelivery system inhibiting key stemness regulator in colorectal cancer stem cells | Preclinical |
| HY1-Pt and Salvigenin-Pt [127] | Multiple targets | Platinum hybrids designed to overcome resistance through dual mechanisms | Preclinical |
| Cantharidin (CTD) [127] | Multiple targets including PP2A | Natural compound inhibiting metastasis but requiring toxicity optimization | Preclinical |
Technical Challenges and Solutions
5.2.1 Cancer Stem Cell Targeting CSCs mediate therapeutic resistance through multiple mechanisms including transport protein expression, DNA repair capacity, and metabolic adaptations [127]. Successful CSC-targeting approaches must address this heterogeneity through combination strategies or multi-targeting agents.
5.2.2 Metastasis Microenvironment Modulation The metastatic niche presents physical and biochemical barriers to therapeutic efficacy. Nanotechnology approaches like hyaluronic acid nanoparticles for PTC-209 delivery demonstrate improved targeting to CSCs in colorectal cancer [127].
5.2.3 Combination Therapy Design Rational combination strategies should target both bulk tumor populations and CSCs while minimizing overlapping toxicities. Thiolatia demonstrates potential for combination approaches by enhancing sensitivity to conventional chemotherapeutics like cisplatin [127].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Target Validation
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| PSMD14 Inhibitors [127] | Thiolatia (disulfide-containing antibiotic) | Zinc chelator that inhibits JAMM domain-containing proteases; reverses EMT by decreasing SNAIL stability |
| CSC Stemness Inhibitors [127] | PTC-209 (BMI-1 inhibitor) | Targets self-renewal capacity of cancer stem cells; formulated in hyaluronic acid nanoparticles for improved delivery |
| EMT Modulators [127] | Thiolatia, Cantharidin | Suppress epithelial-mesenchymal transition; regulate E-cadherin expression and cytoskeletal reorganization |
| Signaling Pathway Inhibitors [127] | Sulfarotene (WYC-209) | Targets RARα-SOS2-RAS axis in hepatocellular carcinoma TRCs; overcomes sorafenib resistance |
| Platinum Hybrids [127] | HY1-Pt, Salvigenin-Pt | Dual-mechanism platinum complexes designed to circumvent conventional resistance pathways |
| Animal Metastasis Models [35] | Tail vein injection, Orthotopic implantation | Quantify metastatic burden and organ-specific colonization in vivo |
| CSC Functional Assays [127] | Sphere formation, ALDEFLUOR | Isolate and characterize cancer stem cell populations from tumor specimens |
Validating novel targets from bench-side discovery to clinical trial design requires integrated approaches that address the complexity of cancer progression and metastasis. Success depends on rigorous preclinical models that recapitulate human disease, strategic clinical development plans incorporating biomarker strategies, and innovative therapeutic platforms such as nanotechnology and combination approaches. As our understanding of the molecular mechanisms driving metastasis and stemness continues to evolve, so too must our validation frameworks, ensuring that promising discoveries successfully navigate the challenging path from fundamental biology to patient benefit.
The Role of Biomarkers and Genetic Profiling in Patient Stratification
In modern oncology, patient stratification is the systematic process of classifying cancer patients into distinct subgroups based on the specific molecular characteristics of their disease to guide prognostic assessment and therapeutic intervention. This approach moves beyond traditional organ- or histology-based classification to a paradigm where treatment decisions are informed by the deep molecular mechanisms driving cancer progression and metastasis. The foundational elements enabling this precision medicine approach are biomarkers—objective biological measures of pathogenic processes or pharmacological responses—and comprehensive genetic profiling technologies that decode the genomic, transcriptomic, and epigenomic alterations underlying tumor behavior [132] [133].
The critical distinction between biomarker types forms the conceptual bedrock of effective stratification. Prognostic biomarkers provide information about a patient's overall cancer outcome, such as disease recurrence or overall survival, regardless of specific therapy. In contrast, predictive biomarkers give information about the expected effect of a therapeutic intervention, identifying patients more likely to benefit from a particular treatment [132] [134]. Some biomarkers can serve both functions, though this dual role can present analytical challenges. Mastery of this distinction is essential for researchers designing stratification strategies and interpreting biomarker data in both clinical and research settings [134].
Biomarker Classification and Molecular Mechanisms
The molecular diversity of biomarkers reflects the complex biological pathways involved in oncogenesis and metastasis. Understanding this classification provides researchers with a framework for selecting appropriate biomarkers for specific stratification goals.
Table 1: Classification of Key Cancer Biomarkers and Their Clinical Applications
| Biomarker Category | Molecular Basis | Exemplary Biomarkers | Primary Stratification Utility |
|---|---|---|---|
| Genetic Biomarkers | Somatic mutations, gene fusions, copy number alterations | KRAS, EGFR, BRAF mutations; HER2 amplification; NTRK fusions | Predicting response to targeted therapies (e.g., EGFR inhibitors, TRK inhibitors) [135] [133] |
| Epigenetic Biomarkers | DNA methylation patterns, histone modifications | MGMT promoter methylation; RASSF1A methylation | Predicting chemotherapy response (e.g., temozolomide in glioblastoma); prognostic stratification [132] [133] |
| Transcriptomic Biomarkers | Gene expression signatures | 70-gene MammaPrint signature; 21-gene Oncotype DX recurrence score | Prognostic stratification in breast cancer; predicting chemotherapy benefit [132] |
| Protein Biomarkers | Protein expression or overexpression | HER2/ER/PR protein expression; PD-L1 | Predicting response to targeted therapies (e.g., trastuzumab) and immunotherapy [132] [133] |
| Circulating Biomarkers | ctDNA, CTCs, exosomes | ctDNA mutations; CTC count | Non-invasive monitoring; early detection of resistance; assessing tumor heterogeneity [133] [136] |
Molecular Mechanisms Linking Biomarkers to Metastasis
Recent research has illuminated how specific molecular mechanisms, identifiable through biomarkers, drive cancer progression and metastasis. A pivotal 2025 study analyzing genomic profiles of over 3,700 patients across 24 cancer types revealed that metastatic tumors undergo distinct evolutionary paths characterized by increased genomic complexity [137]. The research demonstrated that whole-genome duplication (WGD)—the doubling of the entire chromosome set—occurs in nearly one-third of patients during metastasis, creating redundant gene copies that allow cancer cells to accumulate damaging mutations while preserving essential functions [137].
This study further established a critical divergence in evolutionary patterns: while metastatic tumors accumulate copy-number alterations (CNAs), they do not proportionally increase their mutational burden. This strategic adaptation maximizes cellular adaptability and treatment resistance through CNAs while avoiding excessive mutations that would increase tumor immunogenicity and visibility to the immune system [137]. This mechanistic insight explains why CNA-rich metastatic tumors may be less responsive to immunotherapies and suggests that targeting genetic instability represents a promising therapeutic strategy for advanced disease.
Advanced Technologies for Genetic Profiling and Biomarker Discovery
The revolution in patient stratification has been propelled by technological advances that enable comprehensive molecular characterization at multiple biological levels.
Multi-Omics Profiling Platforms
Next-generation sequencing (NGS) technologies form the cornerstone of modern genetic profiling, allowing simultaneous assessment of numerous genetic alterations across the genome. The most sophisticated stratification approaches now integrate multiple omics technologies:
Whole Genome/Exome Sequencing: Provides complete cataloguing of coding and non-coding mutations, copy-number alterations, and structural variants. The CATCH trial in metastatic breast cancer demonstrated that combining whole-genome/exome with RNA-sequencing significantly expanded actionable biomarker detection compared to targeted sequencing alone [138].
Transcriptomic Profiling: RNA-sequencing enables detection of gene fusions, alternative splicing, and gene expression signatures that refine prognostic classification and identify therapeutic vulnerabilities [138].
Epigenomic Analysis: Array-based or sequencing-based methylation profiling identifies clinically significant epigenetic alterations such as MGMT promoter methylation in glioblastoma, which predicts response to temozolomide [132] [133].
Liquid Biopsy and Circulating Biomarkers
Liquid biopsy represents a transformative approach for non-invasive biomarker assessment through analysis of circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and exosomes. This technology enables real-time monitoring of tumor evolution and treatment response, capturing spatial and temporal heterogeneity that may be missed by single tissue biopsies [133]. Key applications include:
Early Detection of Resistance: In hormone receptor-positive metastatic breast cancer, serial ctDNA analysis can detect emerging ESR1 mutations before radiographic progression, allowing early intervention with targeted agents like camizestrant [136].
Minimal Residual Disease Monitoring: In soft tissue sarcoma, personalized ctDNA assays using whole-genome sequencing to identify structural variants can predict recurrence risk following surgery, stratifying patients who may benefit from adjuvant chemotherapy [136].
Therapy Selection: In metastatic prostate cancer, dual-platform testing analyzing both cell-free DNA and circulating tumor cell DNA (HERCULES test) provides comprehensive mutation profiling to guide precision oncology strategies as cancers evolve resistance mechanisms [136].
Artificial Intelligence in Biomarker Discovery
Artificial intelligence (AI) and machine learning (ML) are accelerating biomarker discovery by mining complex multidimensional datasets to identify patterns beyond human analytical capability. AI algorithms integrate multi-omics data with clinical outcomes to identify novel biomarker signatures and improve predictive accuracy [133]. Recent applications include:
Multimodal AI Predictors: In high-risk non-metastatic prostate cancer, an MMAI algorithm successfully identified patients who would benefit from intensified hormone therapy, sparing non-responders unnecessary toxicity [136].
Image-Based Biomarkers: AI analysis of digital pathology images and radiomics features can extract subtle morphological patterns predictive of molecular subtypes and treatment response [133].
Table 2: Experimental Protocols for Biomarker Discovery and Validation
| Experimental Goal | Recommended Protocol | Key Analytical Methods | Technical Considerations |
|---|---|---|---|
| Comprehensive Genomic Profiling | Whole genome/exome and transcriptome sequencing of tumor-normal pairs [138] | MSK-IMPACT or similar large panel NGS; variant calling pipelines; RNA-seq alignment and fusion detection | Minimum 150x coverage for tumor; 60x for normal; FFPE-friendly protocols needed for clinical samples |
| Liquid Biopsy Analysis | Blood collection in cell-stabilizing tubes; plasma separation within 2 hours; ctDNA extraction [136] | ddPCR for variant tracking; NGS panels for mutation detection; structural variant analysis | Pre-analytical variables critical; optimize blood volume and processing delays; use unique molecular identifiers |
| Methylation Profiling | Bisulfite conversion of tumor DNA; library preparation and sequencing [132] | Array-based methylation platforms; bisulfite sequencing; methylation-specific PCR | Bisulfite conversion efficiency monitoring; appropriate normalization to control samples |
| Gene Expression Signatures | RNA extraction from fresh-frozen or stabilized tissue; quality control [132] | Nanostring nCounter; RT-qPCR; RNA-seq; microarray platforms | RIN >7 for RNA quality; avoid excessive cycle thresholds in qPCR; normalize to reference genes |
The Scientist's Toolkit: Essential Reagents and Technologies
Table 3: Essential Research Reagent Solutions for Biomarker Studies
| Reagent/Category | Specific Examples | Research Application | Technical Function |
|---|---|---|---|
| NGS Library Prep Kits | Illumina TruSight Oncology; Thermo Fisher Oncomine | Comprehensive genomic profiling; targeted sequencing | Target enrichment; adapter ligation; library amplification for sequencing [138] |
| ctDNA Isolation Kits | QIAGEN Circulating Nucleic Acid Kit; Roche cfDNA System | Liquid biopsy applications; minimal residual disease detection | Cell-free DNA purification from plasma; removal of genomic DNA contamination [136] |
| Multiplex Immunoassay Panels | R&D Systems Luminex; MSD Multi-Spot Assays | Cytokine profiling; protein biomarker validation | Simultaneous measurement of multiple analytes in small sample volumes [133] |
| Single-Cell RNA-seq Kits | 10x Genomics Chromium; BD Rhapsody | Tumor heterogeneity studies; tumor microenvironment characterization | Single-cell encapsulation; barcoding; reverse transcription; library prep [137] |
| Methylation Analysis Kits | Illumina Infinium MethylationEPIC; Zymo Research Bisulfite Kits | Epigenetic biomarker discovery; methylation signature development | Bisulfite conversion; array hybridization; sequencing library preparation [132] |
Clinical Implementation and Validation Frameworks
Translating biomarker discoveries into clinically validated tools for patient stratification requires rigorous evaluation frameworks and consideration of practical implementation challenges.
Evidence Generation and Clinical Trial Designs
Robust validation of stratification biomarkers requires study designs that can definitively establish clinical utility. While early-phase biomarker studies often use tumor-agnostic designs that enroll patients based on molecular alterations regardless of cancer type, these approaches have limitations for establishing definitive efficacy [135]. More rigorous frameworks include:
Biomarker-Stratified Randomized Trials: The gold-standard design where all patients are tested for the biomarker and randomized to biomarker-directed or control therapy, allowing assessment of both predictive and prognostic value [135].
ctDNA-Guided Intervention Trials: Exemplified by the SERENA-6 trial in breast cancer, where patients with emerging ESR1 mutations detected in ctDNA were randomized to continue current therapy or switch to targeted agents before radiographic progression [136].
Real-World Evidence Generation: Registry studies like the CATCH trial in metastatic breast cancer provide complementary evidence on biomarker implementation in routine care settings, with the CATCH study reporting a 44.4% implementation rate of molecular tumor board recommendations and one-third of patients experiencing significantly prolonged progression-free survival with molecularly guided therapy [138].
Analytical Validation and Quality Assurance
Before clinical deployment, stratification biomarkers require rigorous analytical validation to ensure reliability and reproducibility across laboratory settings. Key considerations include:
Assay Performance Metrics: Establishing sensitivity, specificity, precision, and reproducibility using well-characterized reference materials and control samples [133].
Limit of Detection Determination: Particularly critical for liquid biopsy applications where variant allele fractions may be low (<0.5% for minimal residual disease detection) [136].
Platform Standardization: Harmonizing procedures across testing laboratories through initiatives like the FDA's Bioanalytical Method Validation guidance and CLIA certification requirements for laboratory-developed tests [133].
Future Directions and Emerging Research Paradigms
The field of patient stratification continues to evolve with several emerging trends poised to further refine precision oncology approaches:
Multi-Modal Biomarker Integration: Future stratification strategies will increasingly integrate genomic, transcriptomic, proteomic, and imaging biomarkers to create comprehensive molecular portraits. Research indicates that adding computational biomarkers and gene expression signatures to genomic data can expand treatment options in up to 50% of patients [138].
Dynamic Biomarker Monitoring: The recognition that tumors evolve under therapeutic pressure is driving shift toward serial biomarker assessment rather than single timepoint testing. Liquid biopsy technologies enable this dynamic monitoring to detect resistance mechanisms as they emerge [136].
Artificial Intelligence-Enhanced Stratification: AI algorithms that continuously learn from real-world patient outcomes and multi-omics data will create increasingly sophisticated stratification models that adapt as new evidence accumulates [133].
Equitable Access Implementation: As biomarker-guided therapies demonstrate improved outcomes, ensuring equitable access across diverse populations and healthcare systems represents a critical challenge. Shared infrastructures for biomarker testing at national and international levels are being explored to expand availability [135].
The ongoing refinement of biomarkers and genetic profiling technologies continues to enhance our ability to stratify cancer patients with increasing precision, ultimately enabling more effective targeting of therapies to individual molecular vulnerabilities and improving outcomes across the cancer spectrum.
The targeting of oncogenic drivers such as MET, KRAS, and PIK3CA represents both the promise and challenge of precision oncology. These genes encode critical signaling proteins that regulate cellular proliferation, survival, and metastasis. While significant advances have been made in developing inhibitors against these targets, the clinical outcomes have varied dramatically, revealing complex molecular interdependencies and resistance mechanisms. This review analyzes key case studies that highlight both the successes and setbacks in targeting these molecules, providing insights into the sophisticated molecular circuitry underlying cancer progression and treatment response. The journey from initial target validation to effective therapeutic implementation requires a deep understanding of pathway interactions, mutational profiles, and adaptive resistance mechanisms that characterize advanced malignancies.
MET Targeting: From Promising Target to Combination Strategies
MET as an Oncogenic Driver
The MET receptor tyrosine kinase, upon activation by its ligand hepatocyte growth factor (HGF), initiates signaling cascades that promote cell growth, invasiveness, and metastatic potential. Aberrant activation of the HGF-MET axis occurs through various mechanisms, including gene amplification, protein overexpression, and activating mutations, making it a compelling therapeutic target across multiple cancer types. The MET M1268T mutation represents one such activating mutation that constitutively stimulates downstream pathways, including both the MAPK and PI3K signaling networks, which are critical for tumor maintenance and progression [139].
Case Study: PIK3CA Mutations Confer Resistance to MET Inhibition
Experimental Overview: A pivotal investigation examined how concurrent PIK3CA mutations impact response to MET inhibition in MET-driven cancer models. Researchers utilized NIH3T3 cells harboring the MET M1268T activating mutation with and without ectopic expression of two common PIK3CA hotspot mutations (E545K and H1047R). Additional studies were conducted in head and neck cancer cell lines endogenously expressing MET with and without PIK3CA mutations [139].
Methodology:
- Cell Lines and Transfection: NIH3T3 MET M1268T cells were transfected with PIK3CA E545K, H1047R, or empty vector control using Lipofectamine 2000 and selected with puromycin [139].
- Inhibitors and Treatments: Cells were treated with the MET tyrosine kinase inhibitor tepotinib (EMD1214063) and/or the PI3K inhibitor pictilisib (GDC-0941) across a concentration range [139].
- Assessments: Endpoints included immunoblotting for pathway activation (p-MET, p-AKT, p-ERK), cell viability (resazurin assay), colony-forming ability, apoptosis detection, wound-healing migration assays, and in vivo tumor growth studies [139].
Key Findings:
- Both PIK3CA E545K and H1047R mutations conferred resistance to MET inhibition in MET-driven models
- PIK3CA H1047R conferred stronger resistance than E545K across multiple endpoints: PI3K pathway activation, proliferation, colony formation, apoptosis induction, and migration capacity
- Resistance was overcome by combined MET and PI3K inhibition, with synergistic effects observed in vitro and enhanced anti-tumor activity in vivo
- In head and neck cancer models with ligand-induced MET activation, the combination of MET and PI3K inhibitors produced more-than-additive effects, particularly in PIK3CA-mutated cells [139]
Table 1: Impact of PIK3CA Mutations on Response to MET Inhibition
| Experimental Endpoint | PIK3CA E545K | PIK3CA H1047R | Wild-type Control |
|---|---|---|---|
| AKT Phosphorylation Post-MET Inhibition | Moderately Sustained | Strongly Sustained | Abolished |
| Cell Viability EC50 to MET Inhibitor | High (Resistant) | Very High (Highly Resistant) | Low (Sensitive) |
| Colony Formation with MET Inhibitor | Reduced but Present | Minimally Affected | Abolished |
| Synergy with PI3K Inhibitor | Strong | Strong | Additive |
Clinical Implications and Ongoing Challenges
These findings demonstrate that concurrent PIK3CA mutations can function as a potent resistance mechanism to MET-targeted therapies. The persistence of PI3K signaling upon MET inhibition maintains survival signals that allow cancer cells to withstand treatment. This molecular insight supports the clinical evaluation of combination therapies targeting both MET and PI3K in tumors featuring aberrant MET expression alongside PIK3CA mutations, particularly in head and neck cancers where both alterations are frequently observed [139].
KRAS: From "Undruggable" Target to Clinical Breakthrough
KRAS as a Master Oncogene in Solid Tumors
The KRAS oncogene represents one of the most frequently mutated drivers in human cancer, with particularly high prevalence in pancreatic ductal adenocarcinoma (PDAC), where it is mutated in approximately 95% of cases [140]. For decades, KRAS was considered "undruggable" due to its smooth surface topology and picomolar affinity for GTP, which complicated the development of selective inhibitors. This perception shifted dramatically with the development of allele-specific KRAS inhibitors that target the G12C mutation, leading to FDA approvals for non-small cell lung cancer (NSCLC) and colorectal cancer [140].
Case Study: Mutation-Specific KRAS Inhibition in PDAC
Experimental Overview: The development of KRASG12C inhibitors represented a breakthrough in targeted therapy; however, their efficacy varies significantly across cancer types. In PDAC, KRASG12C mutations occur in less than 2% of cases, in contrast to NSCLC where they comprise approximately 40% of KRAS mutations [140]. The most common KRAS mutations in PDAC are G12D (41%), G12V (32%), and G12R (16%), creating a therapeutic challenge that requires mutation-specific approaches [140].
Methodology:
- Genetic Models: Genetically engineered mouse models (GEMMs) of PDAC with conditional KrasG12D expression have been instrumental in establishing KRAS as both an initiating and maintenance driver [140].
- Dependency Studies: RNA interference and genetic silencing of mutant Kras in established PanINs and PDAC tumors demonstrated tumor regression, validating KRAS as a therapeutic target [140].
- Therapeutic Targeting: Covalent inhibitors targeting KRASG12C (sotorasib, adagrasib) exploit a specific cysteine residue for selective binding, while alternative strategies are needed for non-G12C mutations [140].
Key Findings:
- Mutational activation of KRAS is the initiating genetic event in PDAC, followed by sequential loss of tumor suppressors CDKN2A, TP53, and SMAD4 [140]
- GEMMs demonstrated that mutant Kras is necessary for tumor maintenance, as its inactivation causes regression of primary and metastatic tumors [140]
- The KRAS mutational profile in PDAC is distinct from other cancers, with predominance of G12D, G12V, and G12R mutations, while G12C is rare (<2%) [140]
- Despite the success of KRASG12C inhibitors in lung cancer, their limited applicability in PDAC has driven development of broader targeting approaches, including pan-KRAS and combination strategies [140]
Table 2: KRAS Mutation Distribution Across Cancer Types
| Cancer Type | G12C Prevalence | G12D Prevalence | G12R Prevalence | Other Mutations |
|---|---|---|---|---|
| Pancreatic Ductal Adenocarcinoma | ~2% | ~41% | ~16% | ~41% |
| Non-Small Cell Lung Cancer | ~40% | Low | Low | ~60% |
| Colorectal Cancer | Low | Variable | Low | High (G13 18%) |
Emerging Strategies and Clinical Translation
The development of direct KRAS inhibitors has catalyzed extensive drug discovery efforts, with more than 50 mutation-selective and pan/multi-KRAS inhibitors currently in clinical evaluation [140]. However, the clinical efficacy of KRAS inhibitors in PDAC has been limited by several factors, including intrinsic resistance mechanisms, tumor heterogeneity, and the complex tumor microenvironment of pancreatic cancer. Current research focuses on combination strategies that target both KRAS and parallel survival pathways or microenvironmental components to improve therapeutic outcomes.
PIK3CA: Context-Dependent Efficacy and Combination Approaches
PIK3CA in the Oncogenic Signaling Network
The PIK3CA gene encodes the p110α catalytic subunit of PI3K, which plays a central role in the PI3K/AKT/mTOR pathway, regulating cell survival, growth, and metabolism. PIK3CA is among the most frequently mutated oncogenes in human cancer, with hotspot mutations clustering in the helical (E542K, E545K) and kinase (H1047R) domains. These mutations lead to constitutive PI3K pathway activation and are found in approximately 15-20% of colorectal cancers and a significant proportion of breast, endometrial, and other solid tumors [141].
Case Study: Limited Efficacy of PI3K Inhibition in Colorectal Cancer
Experimental Overview: Despite the high prevalence of PIK3CA mutations in colorectal cancer (CRC), PI3K inhibitors have demonstrated limited clinical efficacy as monotherapy. This contrasts with their success in PIK3CA-mutant breast cancer, where alpelisib is approved in combination with endocrine therapy. Investigation of this discrepancy revealed critical differences in co-occurring mutations and pathway dependencies between cancer types [142].
Methodology:
- Clinical Trial Analysis: Evaluation of early-phase trials of PI3K inhibitors in CRC, including a first-in-human trial of alpelisib in 134 mostly PIK3CA-mutated metastatic cancer patients (35 with CRC) [142].
- Molecular Profiling: Assessment of concurrent genetic alterations in KRAS, BRAF, and PTEN in patient samples [142].
- Preclinical Modeling: Use of genetically engineered models to dissect the contribution of PI3K signaling in KRAS-driven cancers [143].
Key Findings:
- In the alpelisib trial, the objective response rate in CRC was only 5.7% despite 84.2% of patients having centrally confirmed PIK3CA mutations [142]
- 76.5% of evaluated CRC patients had concurrent KRAS mutations, representing a potential resistance mechanism [142]
- The NCI-MATCH trial of taselisib in PIK3CA-mutated tumors (excluding KRAS/PTEN mutations) showed no objective responses in 6 CRC patients, though 3 had stable disease [142]
- Copanlisib in another NCI-MATCH cohort showed no responses or clinical benefit in 4 CRC patients despite 16% ORR in the overall cohort [142]
- Preclinical studies demonstrated that while PI3K activity is important for KRAS-induced tumorigenesis, it is not essential for maintenance of established KRAS-driven tumors [143]
Case Study: Differential Signaling Properties of PIK3CA Hotspots
Experimental Overview: Research has revealed that different PIK3CA hotspot mutations may exhibit distinct signaling properties and differential sensitivities to targeted therapies. This molecular nuance may explain some of the variable treatment responses observed in the clinic [139].
Key Findings:
- PIK3CA H1047R demonstrated stronger resistance to MET inhibition than E545K across multiple cellular assays [139]
- In mammary tumor models, PIK3CA H1047R-induced tumors were more aggressive than E545K-driven tumors [139]
- In lung cancer models, PIK3CA H1047R alone was insufficient to promote tumor initiation, requiring cooperation with BRAFV600E [139]
Therapeutic Implications and Future Directions
The limited efficacy of PI3K inhibitor monotherapy in CRC, despite PIK3CA mutation prevalence, underscores the necessity for rational combination strategies. The high frequency of concurrent KRAS mutations (35-60% of PIK3CA-mutated CRC) represents a major resistance mechanism, as KRAS can activate PI3K-independent survival pathways [142]. Future therapeutic approaches require combination strategies that address the complex pathway interactions and feedback mechanisms that maintain tumor survival despite PI3K inhibition.
Integrated Analysis: Cross-Talk and Therapeutic Integration
Signaling Network Interdependencies
The MET, KRAS, and PIK3CA signaling axes exhibit extensive cross-talk and compensatory mechanisms that have profound therapeutic implications. KRAS directly binds to the p110α catalytic subunit of PI3K, providing a biochemical link between these pathways [143]. Feedback reactivation of ERBB3/PI3K signaling represents a common resistance mechanism to targeted therapies against upstream receptors [143]. The presence of concurrent genetic alterations in these pathways often dictates therapeutic responses and resistance patterns.
Table 3: Clinical Development Status of Targeted Agents
| Therapeutic Target | Representative Agents | Approval Status | Key Limitations |
|---|---|---|---|
| KRAS G12C | Sotorasib, Adagrasib | Approved (NSCLC, CRC) | Limited efficacy in PDAC (low prevalence) |
| PI3K p110α | Alpelisib, Inavolisib | Approved (Breast Cancer) | Limited efficacy in CRC with KRAS co-mutations |
| MET | Tepotinib, Cabozantinib | Approved (NSCLC, Thyroid) | Resistance via PIK3CA mutations |
Combination Therapy Rationale
Preclinical and clinical evidence strongly supports combination approaches for targeting these interconnected pathways:
PI3K/MEK Combinations: Concurrent inhibition of PI3K and MEK has demonstrated synergistic effects in KRAS-mutant cancers, including dramatic responses in established KRAS-driven lung adenocarcinomas [143]. This combination promotes apoptosis through concomitant down-regulation of Mcl-1 (PI3K inhibition) and up-regulation of BIM (MEK inhibition) [143].
MET/PI3K Combinations: In models with MET activation and PIK3CA mutations, combined MET and PI3K inhibition synergistically overcomes resistance and enhances anti-tumor activity in vitro and in vivo [139].
Context-Specific Combinations: The efficacy of combination strategies is highly dependent on the genetic context, requiring careful patient selection based on comprehensive molecular profiling.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Key Research Reagent Solutions
Table 4: Essential Research Reagents for Investigating MET, KRAS, and PIK3CA Signaling
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cell Line Models | NIH3T3 MET M1268T; Detroit-562 (HNC, PIK3CA H1047R); CRC lines with KRAS/PIK3CA mutations | Mechanistic studies, drug screening | Modeling specific genetic alterations and their functional consequences |
| Inhibitors | Tepotinib (MET); Pictilisib (PI3K); Sotorasib (KRAS G12C) | Target validation, combination studies | Selective inhibition of specific pathway components to assess functional roles |
| Expression Plasmids | PIK3CA E545K, H1047R (Addgene #12524, #12525) | Genetic manipulation studies | Introducing specific mutations to investigate their biological impact |
| Antibodies | p-Y1234/Y1235 MET, p-Ser473 AKT, p-ERK, p-S6 | Pathway activation assessment | Detecting phosphorylation status and pathway activity through immunoblotting |
| In Vivo Models | GEMMs of PDAC (KrasG12D; Trp53-/-); Xenograft models | Preclinical therapeutic evaluation | Assessing drug efficacy and resistance mechanisms in physiological contexts |
Experimental Workflows and Methodologies
Comprehensive Molecular Profiling Workflow:
- Sample Acquisition: Tumor tissue or liquid biopsy collection from patients
- DNA/RNA Extraction: Quality control for downstream applications
- Mutation Detection: Next-generation sequencing covering hotspot mutations in 50+ cancer-related genes [144]
- Pathway Activation Assessment: Immunoblotting for phosphorylated signaling proteins (p-MET, p-AKT, p-ERK, p-S6) [139]
- Functional Validation: In vitro and in vivo models to confirm biological significance of identified alterations
Drug Combination Screening Protocol:
- Single-Agent Testing: Determine IC50 values for individual inhibitors across a concentration range
- Matrix Combination Design: Systematically combine inhibitors at multiple concentrations
- Synergy Analysis: Calculate combination indices using Chou-Talalay or Bliss independence models
- Mechanistic Follow-up: Assess effects on downstream pathway components and apoptosis markers
- In Vivo Validation: Evaluate most promising combinations in appropriate animal models
Visualizing Signaling Pathways and Experimental Approaches
MET/PIK3CA Signaling Network and Therapeutic Intervention
Signaling Network and Therapeutic Targeting
Experimental Workflow for Combination Therapy Assessment
Combination Therapy Assessment Workflow
The case studies presented herein illustrate both the remarkable progress and persistent challenges in targeting MET, KRAS, and PIK3CA mutations in cancer. Key lessons emerge from these experiences: (1) Monotherapy approaches against single oncogenic drivers are frequently insufficient due to pathway redundancies and adaptive resistance mechanisms; (2) The genetic context, including concurrent mutations, dramatically influences therapeutic response; (3) Mutation location and type within a gene can significantly impact biological behavior and drug sensitivity; and (4) Rational combination strategies informed by molecular mechanisms offer the most promising path forward.
Future advances will require increasingly sophisticated approaches to patient stratification, considering not only individual mutations but also their functional interactions within signaling networks. The development of novel therapeutic modalities, including allosteric inhibitors, protein degradation strategies, and mutation-agnostic approaches, may expand the scope of targetable alterations. Additionally, a deeper understanding of adaptive resistance mechanisms and the role of the tumor microenvironment will be essential for designing durable treatment strategies. As we continue to decipher the complex molecular circuitry of cancer, targeted therapy combinations matched to specific molecular contexts offer the potential to transform cancer treatment outcomes across diverse malignancies characterized by MET, KRAS, and PIK3CA alterations.
Integrating Multi-Omics Data and AI for Prognostic and Predictive Modeling
Cancer's complex pathophysiology is shaped by diverse genetic, environmental, and molecular factors, leading to considerable variability in patient outcomes even within the same cancer types, which complicates treatment strategies [145]. The advent of large-scale molecular profiling methods, collectively known as omics technologies, has revolutionized our understanding of disease mechanisms, uncovering novel pathways, disease-associated loci, biomarkers, and therapeutic targets [146]. While early research focused on single-omics layers, it has become increasingly clear that a comprehensive understanding of disease and normal physiology requires integrative, multi-omics analyses [146]. Biological systems operate through complex, interconnected layers including the genome, transcriptome, proteome, metabolome, microbiome, and lipidome, with genetic information flowing through these layers to shape observable traits [146].
The integration of artificial intelligence (AI) with multi-omics data represents a transformative approach in oncology, enabling researchers to decode cancer's intricate molecular mechanisms and address critical clinical challenges. Tumor metastasis and drug resistance are two major challenges in cancer treatment, accounting for over 90% of cancer mortalities [147]. These processes involve sophisticated molecular reprogramming that allows cancer cells to colonize distant organs, evade the immune system, and develop resistance to therapeutic interventions [115] [147]. Multi-omics technologies provide a systems-level understanding of these processes by combining information from genomics, transcriptomics, epigenomics, proteomics, and metabolomics [147]. When powered by AI's analytical capabilities, these integrated datasets reveal critical prognostic biomarkers, predict therapeutic responses, and identify novel targets for personalized treatment strategies, ultimately advancing precision oncology and improving patient outcomes [148] [149].
Multi-Omics Data Types and Their Biological Significance
Multi-omics approaches integrate complementary molecular perspectives to construct comprehensive models of tumor biology. Each omics layer provides unique insights into the molecular events driving cancer progression, metastasis, and therapeutic resistance.
Table 1: Multi-Omics Components and Their Applications in Cancer Research
| Omics Component | Description | Key Features in Cancer | Clinical Applications |
|---|---|---|---|
| Genomics | Study of the complete set of DNA, including all genes | Driver/passenger mutations, copy number variations (CNVs), single-nucleotide polymorphisms (SNPs) | Disease risk assessment, identification of genetic disorders, pharmacogenomics [146] |
| Transcriptomics | Analysis of RNA transcripts produced by the genome | Differential gene expression, alternative splicing, non-coding RNAs | Gene expression profiling, biomarker discovery, drug response studies [146] |
| Proteomics | Study of protein structure, function, and interactions | Post-translational modifications, protein-protein interactions, signaling pathways | Biomarker discovery, drug target identification, functional studies [146] |
| Epigenomics | Study of heritable changes in gene expression without DNA sequence changes | DNA methylation, histone modifications, chromatin accessibility | Cancer research, developmental biology, environmental impact studies [146] |
| Metabolomics | Comprehensive analysis of metabolites within biological samples | Metabolic reprogramming, oncometabolites, nutrient sensing | Disease diagnosis, nutritional studies, toxicology and drug metabolism [146] |
Genetic and Genomic Variations in Cancer
Genetic alterations represent one of the hallmarks of cancer cells, changing the sequence or amount of resulting mRNA and protein, thus disrupting normal protein function and contributing to cancer development [150]. These alterations can be inherited from parents (germline mutations) or acquired throughout a person's lifetime (somatic mutations) [150]. Mutations in cancer are broadly categorized into driver mutations that provide growth advantage and are directly involved in oncogenic processes, and passenger mutations that do not confer selective advantage [146]. Approximately 10% of cancer cases are caused by germline mutations, which occur in reproductive cells and are passed from parents to children, becoming incorporated into the DNA of every cell in the offspring's body [150].
Copy number variations (CNVs) represent another fundamental form of genetic diversity in cancers, involving duplications or deletions of large DNA regions that lead to variations in gene copies [146]. These variations significantly influence cancer development by altering gene dosage, potentially leading to overexpression of oncogenes or under-expression of tumor suppressor genes [146]. A well-established example is the amplification of the HER2 gene in approximately 20% of breast cancers, leading to aggressive tumor behavior and poor prognosis [146]. Single-nucleotide polymorphisms (SNPs), the most common genetic variation among people, can also affect how cancers develop or respond to drugs by altering genes involved in critical cellular processes such as DNA repair, cell growth, and apoptosis [146].
Artificial Intelligence Methodologies for Multi-Omics Integration
AI technologies, particularly machine learning (ML) and deep learning (DL), have demonstrated remarkable capabilities in analyzing complex multi-omics datasets to extract biologically meaningful patterns and clinically actionable insights. These approaches are especially valuable for addressing the high dimensionality, noise, and heterogeneity inherent in multi-omics data [145] [148].
AI-Driven Workflows for Multi-Omics Analysis
A robust AI-driven workflow for multi-omics analysis involves several critical stages, each requiring specialized computational approaches and rigorous validation:
Data Acquisition and Preprocessing: Multi-modal acquisitions capture complementary molecular information from various omics technologies. Protocol harmonization following community guidance ensures consistency, while preprocessing typically includes normalization, noise reduction, and handling of missing values [148]. For genomic data, this may involve variant calling; for transcriptomics, normalization methods such as TPM or FPKM; and for proteomics, intensity normalization and peak alignment [145].
Feature Engineering and Selection: From processed omics data, feature extraction derives quantitative descriptors including shape, distribution, and higher-order patterns [148]. Due to the high dimensionality of omics data, rigorous feature reduction is essential, employing univariate filtering, correlation pruning, stability checks, embedded sparsity methods, and tree-based importance ranking [148]. Common practice includes selecting the most variable features or those with biological relevance to specific cancer types [145].
Model Construction and Training: Classifiers and regressors for multi-omics integration typically include logistic regression, support vector machines, random forests, gradient boosting (e.g., XGBoost), and deep neural networks [148]. Survival tasks frequently use Cox-based or deep survival models [148]. The model choice should balance discrimination, calibration, interpretability, and computational efficiency, with case-level explanations to support clinical acceptance [148].
Validation and Clinical Translation: Generalizability must be demonstrated through nested cross-validation, temporal splits, and external multi-center testing [148]. Beyond discrimination metrics (e.g., AUC), best practices include calibration assessment, reporting of clinical utility metrics, and decision-analytic evaluation to show net clinical benefit over standard approaches [148]. Successful deployment requires continuous monitoring of performance across scanners, sites, and demographics [148].
AI-Driven Multi-Omics Integration Workflow: This diagram illustrates the comprehensive pipeline for integrating multi-omics data using artificial intelligence, from raw data acquisition to clinical application.
Advanced Machine Learning Approaches
Innovative machine learning frameworks specifically designed for multi-omics integration have demonstrated remarkable success in cancer research. The PRISM (PRognostic marker Identification and Survival Modelling through Multi-omics Integration) framework represents a comprehensive approach aimed at improving survival prediction and discovering minimal yet robust biomarker panels across multiple omics modalities [145]. PRISM systematically evaluates various feature selection methods and survival models through a robust pipeline that selects features within single-omics datasets before integrating them via feature-level fusion and multi-stage refinement [145].
Another advanced approach employed integrative machine learning comprising 111 algorithms to construct a proliferating cell risk score (SPRS) for lung adenocarcinoma [151]. This model demonstrated superior performance in predicting prognosis and clinical outcomes compared to 30 previously published models, highlighting the power of combining multiple algorithmic approaches [151]. The role of SPRS and five pivotal genes in immunotherapy response was evaluated, and their expression was experimentally verified, confirming SPRS as an independent prognostic factor affecting LUAD patient survival [151].
Experimental Protocols and Methodologies
Multi-Omics Data Acquisition and Processing
Comprehensive multi-omics analysis requires standardized protocols for data generation across different molecular layers. The following methodologies represent current best practices derived from recent cancer studies:
Genomic and Transcriptomic Profiling:
- DNA and RNA are typically extracted from tumor tissues or liquid biopsies using quality-controlled kits
- Next-generation sequencing (NGS) enables comprehensive analysis of entire genomes, exomes, or transcriptomes with high accuracy [146]
- For RNA sequencing, the Illumina HiSeq 2000 RNA-seq platform is commonly used, with data provided as log2(x + 1) transformed RSEM-normalized counts representing gene-level expression of protein-coding genes [145]
- Single-cell RNA sequencing (scRNA-seq) technology enables high-resolution dissection of cellular heterogeneity within tumors and their associated microenvironments, allowing identification and characterization of different subpopulations of tumor cells, stromal components, and immune cells [147]
Epigenomic Analysis:
- DNA methylation data consist of beta values (0-1) from Illumina 450K/27K assays, where 0 signifies no methylation and 1 indicates full methylation [145]
- Data are typically restricted to specific CpG probes to enable cross-cancer analysis consistency [145]
Proteomic and Metabolomic Approaches:
- Mass spectrometry-based methods enable high-throughput protein and metabolite identification and quantification
- Advanced proteogenomic approaches correlate molecular profiles with clinical features, refining prediction of therapeutic responses [146]
Table 2: Key Analytical Methods in Multi-Omics Cancer Research
| Method Category | Specific Techniques | Key Applications | Considerations |
|---|---|---|---|
| Sequencing Technologies | Whole-genome sequencing (WGS), Whole-exome sequencing, RNA-seq, scRNA-seq | Mutation discovery, CNV analysis, gene expression profiling, cellular heterogeneity | Library preparation quality, sequencing depth, batch effects [147] |
| Epigenomic Profiling | DNA methylation arrays, ChIP-seq, ATAC-seq | Methylation patterns, histone modifications, chromatin accessibility | Tissue specificity, dynamic nature of modifications [146] |
| Proteomic Analysis | Mass spectrometry, protein arrays, RPPA | Protein expression, post-translational modifications, signaling pathways | Protein complexity, dynamic range, quantification challenges [146] |
| Spatial Technologies | Spatial transcriptomics, multiplex immunofluorescence | Tissue architecture, cellular localization, tumor-immune interactions | Resolution limitations, data integration complexity [151] |
Data Integration and Computational Analysis
The integration of multi-omics datasets requires sophisticated computational approaches to extract meaningful biological insights:
Multi-Omics Integration Framework:
- Data Preprocessing: Each omics dataset is processed independently with quality control, normalization, and batch effect correction. For gene expression data, features with excessive missing values are removed, and the most variable genes are selected using variance thresholds [145]. For miRNA data, features with over 20% missing values are excluded, and only miRNAs present in sufficient samples are retained [145].
- Feature Selection: Dimensionality reduction is critical for handling high-dimensional omics data. Methods include univariate/multivariate Cox filtering, Random Forest importance, and recursive feature elimination (RFE) to enhance robustness and minimize signature panel size without compromising performance [145].
- Multi-Stage Integration: The PRISM framework employs a two-stage approach: (1) selecting features within single-omics datasets, and (2) integrating them via feature-level fusion and multi-stage refinement [145]. This method has revealed that different cancer types benefit from unique combinations of omics modalities reflecting their molecular heterogeneity [145].
Validation Strategies:
- Cross-validation, bootstrapping, and ensemble voting enhance robustness [145]
- External validation using independent cohorts is essential for verifying generalizability [149]
- Experimental validation using cell lines, animal models, or clinical samples confirms biological relevance [151]
Signaling Pathways in Cancer Progression and Therapeutic Resistance
The molecular mechanisms driving cancer progression and therapeutic resistance involve complex interactions between multiple signaling pathways within tumor cells and their microenvironment. Multi-omics approaches have been instrumental in elucidating these networks and their clinical implications.
Key Signaling Pathways in Cancer Progression: This diagram illustrates the major molecular pathways involved in cancer metastasis and therapeutic resistance, highlighting potential targets for intervention.
Critical Molecular Mechanisms in Metastasis and Resistance
Genetic Alterations and Driver Mutations: Genomic studies have identified numerous key genes that frequently undergo mutations or copy number variations during the metastatic process [147]. TP53, a classical tumor suppressor gene, is highly mutated across various cancer types, leading to cell cycle dysregulation and defective DNA damage repair pathways that increase tumor cell migration, invasiveness, and proliferation [147]. Activating mutations in oncogenes such as KRAS and PIK3CA also play pivotal roles in metastasis [147]. KRAS mutations cause constitutive activation of the MAPK signaling pathway, promoting cell proliferation, survival, and motility, while PIK3CA mutations activate the PI3K/Akt signaling pathway that controls cellular metabolism, proliferation, and cytoskeletal remodeling [147].
Tumor Microenvironment and Immune Evasion: The metastatic tumor microenvironment is a highly dynamic and heterogeneous ecosystem that plays a critical role in promoting cancer cell colonization, immune escape, and resistance to therapy [147]. Transcriptomic studies employing RNA sequencing have uncovered extensive alterations in gene expression profiles within metastatic tumor tissues compared to their primary counterparts [147]. Metastatic tumor cells show marked increase in expression of immune regulatory pathways, with key immune checkpoint molecules such as PD-L1 and CTLA-4 frequently overexpressed, serving to suppress T cell activation and promote immune tolerance [147]. Additionally, the tumor immune microenvironment is transformed by recruitment of regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs), which secrete immunosuppressive cytokines like IL-10, TGF-β, and IL-6, creating an immunosuppressive niche that promotes tumor survival and metastasis [147].
Therapeutic Resistance Mechanisms: Tumor drug resistance fundamentally limits the clinical benefits of cancer therapy, with approximately 90% of chemotherapy failures and more than 50% of targeted or immunotherapy failures directly attributable to resistance [115]. Resistance can be classified as intrinsic (primary) resistance, referring to lack of response to initial treatment, or acquired (secondary) resistance that develops during or after treatment [115]. Mechanisms include drug efflux pumps such as P-glycoprotein that expel chemotherapy drugs from tumor cells; gene mutations including PIK3CA, KRAS, EGFR, p53 and OCT4; metabolic reprogramming; enhanced DNA repair capabilities; deregulation of apoptotic pathways; and tumor stem cells with self-renewal capabilities [42].
Table 3: Key Research Reagent Solutions for Multi-Omics and AI Studies
| Reagent/Resource Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Sequencing Platforms | Illumina HiSeq 2000 RNA-seq, Illumina 450K/27K methylation arrays | Genome-wide profiling of gene expression, DNA methylation, genetic variations | Platform-specific normalization, batch effect correction [145] |
| Single-Cell Technologies | 10X Genomics, Drop-seq, in situ sequencing | Cellular heterogeneity analysis, rare cell population identification, trajectory inference | Cell viability, amplification bias, computational resources [147] |
| Spatial Biology Tools | Multiplex immunofluorescence, spatial transcriptomics platforms | Tissue architecture preservation, cell-cell interaction mapping, spatial gene expression | Resolution limitations, data integration complexity [151] |
| Computational Tools | UCSCXenaTools R package, PyRadiomics, Scissor algorithm, CellChat | Data retrieval and integration, radiomic feature extraction, single-cell analysis, cell-cell communication | Reproducibility, version control, documentation [145] [151] |
| AI/ML Frameworks | TensorFlow, PyTorch, scikit-learn, XGBoost | Model development, feature selection, predictive modeling, survival analysis | Hyperparameter tuning, overfitting prevention, interpretability [148] [149] |
| Validation Reagents | CRISPR-based screening libraries, antibodies for IHC, qPCR assays | Functional validation of biomarkers, protein expression confirmation, gene expression verification | Specificity, sensitivity, reproducibility across platforms [150] |
Experimental Models for Functional Validation
A comprehensive multi-omics and AI research pipeline requires robust experimental models for validating computational predictions:
- Cell Line Models: Established cancer cell lines enable mechanistic studies of specific genetic alterations, drug responses, and molecular pathways. Recent studies have employed CRISPR-based screening to test nearly all possible single base substitutions, allowing direct assessment of mutation impact [150].
- Animal Models: Genetically engineered mouse models and patient-derived xenografts provide in vivo systems for studying tumor progression, metastasis, and therapeutic responses in a physiological context.
- Patient-Derived Organoids: These 3D culture systems maintain tumor heterogeneity and microenvironment characteristics, enabling personalized drug sensitivity testing and functional validation of biomarkers [152].
- Microgravity Models: Innovative approaches such as simulated microgravity environments have been used to investigate cancer induction in mesothelial cells, revealing changes in cytoskeleton and adhesion proteins that switch normal cells toward tumor phenotypes [152].
Clinical Applications and Translational Implications
The integration of multi-omics data with AI methodologies has produced significant advances in clinical cancer research, with demonstrable impact on prognostic modeling, therapeutic selection, and personalized treatment strategies.
Prognostic and Predictive Biomarker Discovery
AI-driven analysis of multi-omics data has enabled the identification of robust prognostic and predictive biomarkers across multiple cancer types:
- PRISM Framework Applications: Applied to TCGA cohorts of Breast Invasive Carcinoma (BRCA), Cervical Squamous Cell Carcinoma and Endocervical Adenocarcinoma (CESC), Ovarian Serous Cystadenocarcinoma (OV), and Uterine Corpus Endometrial Carcinoma (UCEC), PRISM revealed that miRNA expression consistently provided complementary prognostic information across all cancers, enhancing integrated model performance (C-index: BRCA 0.698, CESC 0.754, UCEC 0.754, OV 0.618) [145].
- Lung Cancer Biomarkers: A systematic review and meta-analysis of AI models for biomarker identification in lung cancer demonstrated pooled sensitivity and specificity of 0.77 and 0.79, respectively, for predicting biomarker status including EGFR, PD-L1, and ALK [149]. These models facilitate non-invasive assessment of prognostic and predictive biomarkers, potentially revolutionizing personalized oncology [149].
- Breast Cancer Stratification: AI technologies have enabled robust subtype identification, immune tumor microenvironment quantification, and prediction of immunotherapy response and drug resistance in breast cancer, supporting individualized treatment design and drug discovery [148].
Therapeutic Targeting and Personalized Treatment
Multi-omics and AI approaches have identified novel therapeutic targets and strategies for overcoming drug resistance:
- KRAS Targeting: Decades of basic research culminated in the development of sotorasib and adagrasib, FDA-approved KRAS inhibitors for KRAS G12C-mutated cancers [150]. Multi-omics studies identified factors within tumor cells and the surrounding environment that render KRAS-targeted treatments less effective, leading to new strategies for overcoming resistance [150].
- Immunotherapy Optimization: Multi-omics analysis of the tumor microenvironment after metastasis provides scientific rationale for designing novel immunotherapeutic strategies tailored to the metastatic niche [147]. By identifying patient-specific neoantigens and immune suppression mechanisms, multi-omics analysis can personalize immunotherapy, improving efficacy of immune checkpoint inhibitors [147].
- Drug Resistance Overcoming: Integrative multi-omics approaches have revealed critical functions of proliferating cells in prognosis and personalized treatment of lung adenocarcinoma [151]. High- and low-risk patient groups identified through these approaches exhibit different biological functions and immune cell infiltration in the tumor microenvironment, with high-risk patients showing resistance to immunotherapy but increased sensitivity to chemotherapeutic and targeted therapeutic agents [151].
The integration of multi-omics data with artificial intelligence represents a paradigm shift in cancer research, enabling unprecedented insights into the molecular mechanisms driving cancer progression, metastasis, and therapeutic resistance. These approaches have moved beyond proof-of-concept to deliver tangible advances in prognostic modeling, biomarker discovery, and personalized treatment strategies.
Future research directions will likely focus on several key areas: standardization of multi-omics data generation and analysis pipelines to enhance reproducibility; development of more sophisticated AI algorithms capable of modeling temporal dynamics and spatial relationships; integration of real-world evidence and digital pathology to complement molecular profiling; and implementation of privacy-preserving federated learning approaches to enable multi-institutional collaboration while protecting patient data [148]. Additionally, as basic research continues to uncover novel molecular mechanisms, such as the role of cuproptosis in tumor metastasis and the complex functions of adhesion molecules like Desmoglein-2, multi-omics and AI approaches will be essential for translating these discoveries into clinical applications [42].
The remarkable progress in targeting previously "undruggable" targets like KRAS demonstrates the power of fundamental research combined with advanced technologies [150]. As these approaches continue to mature, they hold the promise of transforming cancer care by enabling truly personalized therapeutic strategies based on comprehensive molecular profiling and predictive AI modeling, ultimately improving survival rates and quality of life for cancer patients worldwide.
Conclusion
The battle against cancer metastasis requires a multifaceted approach that targets not only the cancer cells themselves but also the dynamic tumor microenvironment and the complex molecular networks that drive progression. Key takeaways include the critical roles of EMT, metabolic rewiring, and immune evasion as core therapeutic vulnerabilities. Overcoming drug resistance and tumor heterogeneity remains a central challenge, necessitating the continued development of sophisticated models and combination strategies. The future of anti-metastatic therapy lies in the precise integration of multi-omics data, artificial intelligence, and novel technologies like CRISPR to uncover deeper mechanistic insights and deliver personalized, effective treatments that ultimately improve patient survival and quality of life.
References
- 1. Multi-stage mechanisms of tumor metastasis and ... [https://www.nature.com/articles/s41392-024-01955-5]
- 2. Stresses in the metastatic cascade: molecular mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7706714/]
- 3. Deciphering organotropism reveals therapeutic targets in ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1677481/full]
- 4. Approaches to modeling cancer metastasis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370506/]
- 5. Plug-and-Play In Vitro Metastasis System toward ... [https://www.nature.com/articles/s41598-019-54711-z]
- 6. Matrix metalloproteinase-driven epithelial-mesenchymal ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06447-w]
- 7. Epithelial-mesenchymal transition in colorectal cancer ... [https://www.nature.com/articles/s41420-025-02593-8]
- 8. Epithelial-mesenchymal transition [https://www.sciencedirect.com/science/article/abs/pii/S0092867425010256]
- 9. Epithelial–Mesenchymal Transition in Cancer: Insights Into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394892/]
- 10. Innovative Approaches to EMT-Related Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467340/]
- 11. Epithelial-to-mesenchymal transition (EMT) and cancer ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02338-2]
- 12. Contribution of Extracellular Matrix to EMT [https://www.cellsignal.com/pathways/contribution-extracellular-matrix-emt?srsltid=AfmBOop8fVmFSr5ClUroSRIt8PUcy4d3wbVZkuKYIKBvxUYD-qOju7Ca]
- 13. Modeling the dynamics of EMT reveals genes associated ... [https://www.nature.com/articles/s41540-025-00512-2]
- 14. A robust EMT-related prognostic model for ccRCC ... [https://link.springer.com/article/10.1007/s12672-025-03911-3]
- 15. Identification of prognostic biomarkers related to epithelial ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1600546/full]
- 16. Tumor Microenvironment: A Complex Landscape of Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066109/]
- 17. The solid tumor microenvironment and related targeting ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1563858/full]
- 18. The Role of Tumor Microenvironment in Cancer Metastasis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8122975/]
- 19. Mechanism insights and therapeutic intervention of tumor ... [https://www.nature.com/articles/s41392-024-01885-2]
- 20. Classification of the tumor immune microenvironment and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10603328/]
- 21. Leveraging TME features and multi-omics data with an ... [https://www.nature.com/articles/s41598-025-98565-0]
- 22. Multimodal AI and tumour microenvironment integration ... [https://www.nature.com/articles/s41467-025-65051-0]
- 23. The development process of 'fit-for-purpose' imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11138661/]
- 24. Data-driven mathematical modeling and quantitative ... [https://www.sciencedirect.com/science/article/abs/pii/S0898122122000967]
- 25. Wnt/β-catenin mediated signaling pathways in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150590/]
- 26. Targeted protein degradation of Wnt/β-catenin signaling ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07333-1]
- 27. Roles of the WNT/β-catenin signaling pathway in ... [https://www.sciencedirect.com/science/article/pii/S2667394025000310]
- 28. PI3K/AKT/mTOR Axis in Cancer - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308072/]
- 29. Targeting the PI3K/AKT/mTOR pathway in lung cancer [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1516583/full]
- 30. Strategic advancements in targeting the PI3K/AKT/mTOR ... [https://www.sciencedirect.com/science/article/pii/S0006295225001121]
- 31. Targeting the RAS/RAF/MAPK pathway for cancer therapy [https://www.nature.com/articles/s41392-023-01705-z]
- 32. Vascular endothelial growth factor signaling in health and ... [https://www.nature.com/articles/s41392-025-02249-0]
- 33. Vascular endothelial generating factor pathway in ovarian ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01864-3]
- 34. MAP4K signaling pathways in cancer: roles, mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586695/]
- 35. Invasion and metastasis in cancer: molecular insights and ... [https://www.nature.com/articles/s41392-025-02148-4]
- 36. Rewriting the Fate of Cancer: Epigenetic and ... [https://www.mdpi.com/2218-273X/15/11/1573]
- 37. Cancer metastasis: molecular mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11977077/]
- 38. Epigenetic Modulation and Bone Metastasis - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389651/]
- 39. Epigenetic regulators in cancer therapy and progression [https://www.nature.com/articles/s41698-025-01003-7]
- 40. Progress in epigenetic research of breast cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446028/]
- 41. Integrated epigenetic and genetic programming of primary ... [https://www.nature.com/articles/s41587-025-02856-w]
- 42. Editorial: Molecular mechanisms and therapeutic targets of ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1571403/full]
- 43. Tumor-on-a-chip: from bioinspired design to biomedical ... [https://www.nature.com/articles/s41378-021-00277-8]
- 44. Innovative organ-on-a-chip platforms for exploring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12269115/]
- 45. 2D versus 3D tumor-on-chip models to study the impact of ... [https://www.nature.com/articles/s41598-025-03504-8]
- 46. Breaking the mold: 3D cell cultures reshaping the future of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1507388/full]
- 47. Three-Dimensional Culture System: A New Frontier in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292892/]
- 48. 3D Cell Culture Methods and Applications [https://elveflow.com/microfluidic-reviews/3d-cell-culture-methods-and-applications-a-short-review/]
- 49. Organoid models in oncology: advancing precision cancer ... [https://www.cancerbiomed.org/content/early/2025/07/24/j.issn.2095-3941.2025.0127]
- 50. Application and development of Organ-on-a-Chip ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1643230/full]
- 51. Cancer-metastasis-on-a-chip reveals efficacy of ... [https://www.sciencedirect.com/science/article/pii/S2590006425008105]
- 52. Dual faces of angiogenesis: Mechanisms and therapeutic ... [https://www.sciencedirect.com/science/article/pii/S0304419X25002367]
- 53. POTENTIAL THERAPEUTIC STRATEGIES FOR LYMPHATIC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2525453/]
- 54. Novel targets beyond vascular endothelial growth factor-A ... [https://www.nature.com/articles/s41433-025-04042-3]
- 55. Insights from pharmacovigilance databases, clinical ... [https://www.nature.com/articles/s43856-025-01169-y]
- 56. A randomized, double-masked parallel-group, multicenter ... [https://pubmed.ncbi.nlm.nih.gov/40512025/]
- 57. BioNTech to Present Clinical and Preclinical Data Across ... [https://investors.biontech.de/news-releases/news-release-details/biontech-present-clinical-and-preclinical-data-across-mrna-and]
- 58. News Release Details [https://investors.compasstherapeutics.com/news-releases/news-release-details/compass-therapeutics-presents-preclinical-data-ctx-10726]
- 59. Mechanisms of Resistance to PD-1 and PD-L1 blockade - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5785093/]
- 60. Regulatory mechanisms of PD-1/PD-L1 in cancers [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02023-w]
- 61. Molecular mechanisms and therapies of immune ... [https://www.sciencedirect.com/science/article/abs/pii/S1044579X25001221]
- 62. MDSC checkpoint blockade therapy: a new breakthrough ... [https://www.nature.com/articles/s41417-025-00886-9]
- 63. Insights into the Mechanisms of Immune-Checkpoint ... [https://pubmed.ncbi.nlm.nih.gov/40874420/]
- 64. Preclinical models of immune checkpoint inhibitors-related ... [https://www.sciencedirect.com/science/article/pii/S017129852500018X]
- 65. ESMO 2025: Combination of immunotherapy and targeted ... [https://ecancer.org/en/news/27160-esmo-2025-combination-of-immunotherapy-and-targeted-therapy-improves-survival-for-patients-with-advanced-colorectal-cancer]
- 66. Preclinical studies performed in appropriate models could ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10512939/]
- 67. Progression-Free Survival Under Immune Checkpoint ... [https://pubmed.ncbi.nlm.nih.gov/40759835/]
- 68. Immune checkpoint inhibitors continuation beyond ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1666373/full]
- 69. Perturbomics: CRISPR–Cas screening-based functional ... [https://www.nature.com/articles/s12276-025-01487-0]
- 70. Unraveling the future of genomics: CRISPR, single-cell ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1565387/full]
- 71. CRISPR screening redefines therapeutic target ... [https://www.sciencedirect.com/science/article/pii/S2095177925001741]
- 72. In vivo single-cell CRISPR uncovers distinct TNF ... [https://www.nature.com/articles/s41586-024-07663-y]
- 73. Single-cell multi-omics in cancer immunotherapy: from tumor ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02426-3]
- 74. Comparative benchmarking of single-cell clustering ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03719-y]
- 75. A CRISPR/Cas9-based enhancement of high-throughput ... [https://www.nature.com/articles/s41467-025-59880-2]
- 76. Genome-wide CRISPR screens identify critical targets to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12396527/]
- 77. CRISPR enabled precision oncology: from gene editing to ... [https://www.eurekalert.org/news-releases/1105244]
- 78. Integrating single-cell transcriptomics and whole-genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575124/]
- 79. Antibody–drug conjugates in cancer therapy [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02489-2]
- 80. Antibody-drug conjugates in cancer therapy [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1669592/full]
- 81. The next frontier in antibody-drug conjugates - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366496/]
- 82. The evolving landscape of antibody-drug conjugates ... [https://www.nature.com/articles/s41698-025-01131-0]
- 83. Antibody-drug conjugates: Current challenges and ... [https://pubmed.ncbi.nlm.nih.gov/41033317/]
- 84. Advances and prospects of RNA delivery nanoplatforms for ... [https://pubmed.ncbi.nlm.nih.gov/40041887/]
- 85. Editorial: Cancer Metastases: Mechanisms of Tumor ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1746602/full]
- 86. Efflux Pump-Mediated Resistance in Chemotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3573517/]
- 87. Function and Inhibitory Mechanisms of Multidrug Efflux ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.737288/full]
- 88. International Journal of Oncology - Spandidos Publications [https://www.spandidos-publications.com/10.3892/ijo.2023.5567]
- 89. Frontiers | Nanotechnology in cancer treatment: revolutionizing... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1548588/full]
- 90. Cancer metabolic reprogramming: importance, main features ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3969803/]
- 91. The molecular mechanisms mitochondrial dynamics and mitophagy... of [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07078-x]
- 92. Evasion of Apoptosis as a Cellular Stress Response in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2825553/]
- 93. Progression and Metastasis of Lung Cancer: Clinical Features ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618860/]
- 94. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 95. Cancer stem cells: Bridging microenvironmental interactions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264091/]
- 96. Nanomaterials targeting cancer stem cells to overcome drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178904/]
- 97. Biology of stem cell paradox: a double-edged sword ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03981-x]
- 98. Stem Cells in Cancer: From Mechanisms to Therapeutic ... [https://www.mdpi.com/2073-4409/14/7/538]
- 99. Overcoming colorectal cancer and cancer stem cell ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra07380d]
- 100. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 101. Multidrug Resistance in Cancer: Understanding Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9262248/]
- 102. Overcoming Cancer Multi-drug Resistance (MDR) [https://www.sciencedirect.com/science/article/pii/S0753332223004316]
- 103. progress in P-glycoprotein inhibitors, drug delivery, and ... [https://pubmed.ncbi.nlm.nih.gov/40892191/]
- 104. Progress in the studies on the molecular mechanisms ... [https://www.sciencedirect.com/science/article/pii/S2211383522004208]
- 105. Therapeutic resistance and combination therapy for cancer [https://www.nature.com/articles/s41598-025-12725-w]
- 106. Suppressing protein damage response to overcome ... [https://www.nature.com/articles/s41421-025-00826-9]
- 107. Recent Advances in Understanding the Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10859101/]
- 108. New target to thwart multidrug resistance in cancer treatment [https://www.utsouthwestern.edu/newsroom/articles/year-2025/feb-thwart-multidrug-resistance-cancer-treatment.html]
- 109. Combined targeted therapy and immunotherapy for cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8462242/]
- 110. Advances and challenges in cancer immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12202542/]
- 111. Systematic investigation of chemo-immunotherapy ... [https://www.nature.com/articles/s41467-024-47433-y]
- 112. Tumor cell plasticity in targeted therapy-induced resistance [https://www.nature.com/articles/s41392-023-01383-x]
- 113. Gene- and immune-targeted therapy combinations using ... [https://www.nature.com/articles/s41698-025-01038-w]
- 114. A Cohort Study on Dual Predictive Markers of Immune ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11829304/]
- 115. Drug resistance in cancer: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623568/]
- 116. Decoding Cancer Heterogeneity for Enhanced Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10525472/]
- 117. Deciphering Tumour Heterogeneity: From Tissue to Liquid ... [https://www.mdpi.com/2072-6694/14/6/1384]
- 118. Personalized cancer treatment strategies incorporating ... [https://www.nature.com/articles/s41540-025-00547-5]
- 119. Advances in personalized medicine: translating genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106117/]
- 120. Precision Oncology: Current Landscape, Emerging Trends ... [https://www.mdpi.com/2073-4409/14/22/1804]
- 121. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 122. Advances and challenges in personalized diagnosis ... [https://www.sciencedirect.com/science/article/pii/S2950523225000387]
- 123. ASCO 2025 Metastatic Breast Cancer Updates [https://www.bcrf.org/blog/asco-2025-metastatic-breast-cancer-updates/]
- 124. MD Anderson Research Highlights for January 22, 2025 [https://www.mdanderson.org/newsroom/featuring-novel-treatment-strategies-lymphomas-kidney-cancers-insights-inflammatory-pain-promising-trial-results-breast-cancer-NSCLC.h00-159773289.html]
- 125. ESMO 2025: Institut Curie at the forefront of innovation against ... [https://institut-curie.org/esmo2025]
- 126. Genialisâ„¢ Supermodel: Predicting monotherapy and ... [https://www.genialis.com/2025/04/17/genialis-supermodel-predicting-monotherapy-and-combination-therapy-responses-in-kras-mutated-cancers-using-a-large-molecular-model-of-cancer-biology/]
- 127. Novel drug research and therapeutic strategies targeting ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1643183/full]
- 128. KEGG PATHWAY Database [https://www.genome.jp/kegg/pathway.html]
- 129. Large language model trained on clinical oncology data ... [https://www.nature.com/articles/s41746-025-01780-2]
- 130. From bench to bedside: how we turn science into medicine [https://www.bhf.org.uk/informationsupport/heart-matters-magazine/research/bench-to-bedside]
- 131. Bench to Bedside [https://www.idorsia.com/our-innovation/bench-to-bedside.html]
- 132. Prognostic and Predictive Biomarkers: Tools in Personalized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4031398/]
- 133. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 134. Prognostic versus predictive value of biomarkers in oncology [https://pubmed.ncbi.nlm.nih.gov/18396036/]
- 135. Precision cancer medicine 2025: some concerns - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439214/]
- 136. Molecular Profiling Insights from ASCO 2025 [https://privatehealth.com/molecular-profiling-insights-from-asco-2025-advancing-personalized-cancer-care/]
- 137. Study Provides New Insights into the Genetic Complexity of ... [https://news.weill.cornell.edu/news/2025/06/study-provides-new-insights-into-the-genetic-complexity-of-cancer-metastasis]
- 138. Delivering precision oncology in metastatic breast cancer [https://pubmed.ncbi.nlm.nih.gov/41170836]
- 139. PIK3CA hotspot mutations differentially impact responses to ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-017-0660-5]
- 140. KRAS: the Achilles' heel of pancreas cancer biology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12352898/]
- 141. The role of PIK3CA gene mutations in colorectal cancer ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1494802/full]
- 142. From PIK3CA Mutations to Rational PI3K Inhibition for the ... [https://link.springer.com/article/10.1007/s40291-025-00815-4]
- 143. Targeting the PI3K signaling pathway in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2822054/]
- 144. Differential Responses to Targeted Therapies in Non-Small ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12323794/]
- 145. Multi-omics prognostic marker discovery and survival ... [https://www.nature.com/articles/s41598-025-20572-y]
- 146. Navigating Cancer Complexity: Integrative Multi-Omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553891/]
- 147. Multi-omics analysis of the tumor microenvironment after ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1648987/full]
- 148. Artificial intelligence integrates multi-omics data for precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12463597/]
- 149. AI models for the identification of prognostic and predictive ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1424647/full]
- 150. Understanding the Path to Cancer Development [https://cancerprogressreport.aacr.org/progress/cpr25-contents/cpr25-understanding-the-path-to-cancer-development/]
- 151. Integrative multi-omics and machine learning reveal critical ... [https://www.nature.com/articles/s41698-025-01027-z]
- 152. Advances in Molecular Pathogenesis Regulation in Cancer ... [https://www.mdpi.com/journal/cimb/special_issues/MZUFBY182M]