dPCR vs qPCR for Mutant Allele Detection: A Strategic Guide for Precision Analysis
This article provides a comprehensive comparison of digital PCR (dPCR) and quantitative PCR (qPCR) for the detection and quantification of mutant alleles, a critical task in oncology, biomarker validation, and...
dPCR vs qPCR for Mutant Allele Detection: A Strategic Guide for Precision Analysis
Abstract
This article provides a comprehensive comparison of digital PCR (dPCR) and quantitative PCR (qPCR) for the detection and quantification of mutant alleles, a critical task in oncology, biomarker validation, and drug development. We explore the foundational principles of both technologies, detail methodological approaches for specific applications like rare variant detection and copy number variation analysis, and offer practical troubleshooting and optimization strategies. By synthesizing recent comparative data and validation guidelines, this guide empowers researchers and drug development professionals to select the optimal PCR strategy for their specific sensitivity, precision, and throughput requirements in mutant allele analysis.
Core Principles: How dPCR and qPCR Work for Nucleic Acid Quantification
In the fields of molecular biology, clinical diagnostics, and drug development, accurately measuring nucleic acids is fundamental to understanding disease mechanisms, validating therapeutic targets, and developing diagnostic assays. The emergence of targeted nucleases like CRISPR/Cas9 has dramatically accelerated the pace of generating mutant cell lines and animal models, making efficient and accurate genotyping a critical step in the research pipeline [1]. At the core of this quantification challenge lies a fundamental methodological divide: absolute quantification versus relative quantification. These approaches differ not merely in calculation method, but in their underlying principles, technical requirements, and applications.
Absolute quantification determines the exact number of target DNA or RNA molecules in a sample, expressed as copies per unit volume [2] [3]. In contrast, relative quantification expresses the amount of target relative to a reference sample or control gene, typically presented as fold-change differences [2]. This distinction becomes particularly significant in the context of detecting mutant alleles, where precise measurement of allele frequencies can inform disease prognosis and treatment strategies. The choice between digital PCR (dPCR) and quantitative real-time PCR (qPCR) often hinges on this quantification paradigm, with each technology offering distinct advantages for specific applications in research and drug development.
Core Principles: A Comparative Framework
Absolute Quantification
Absolute quantification provides a direct count of target molecules without comparison to external standards or endogenous controls. In digital PCR, this is achieved through limiting dilution and Poisson statistical analysis. The sample is partitioned into thousands of individual reactions, some of which contain the target molecule (positive) while others do not (negative). The ratio of negative to total reactions enables precise calculation of the absolute target concentration [2] [4].
Key Characteristics:
- Does not require standard curves [4] [3]
- Provides direct copy number concentration [3]
- Independent of amplification efficiency [3]
- Uses endogenous controls only for sample quality assessment, not quantification [2]
Relative Quantification
Relative quantification measures changes in gene expression or nucleic acid concentration in a given sample relative to another reference sample, such as an untreated control. The comparative CT (ΔΔCT) method is commonly used, which compares the cycle threshold (CT) value of the target gene to a reference gene (e.g., a housekeeping gene) [2].
Key Characteristics:
- Requires stable reference genes for normalization [2] [3]
- Results expressed as n-fold difference relative to a calibrator [2]
- Dependent on amplification efficiency [2]
- Standard curves can be used, but units drop out in final calculation [2]
Table 1: Fundamental Differences Between Absolute and Relative Quantification
| Parameter | Absolute Quantification | Relative Quantification |
|---|---|---|
| Output | Exact copy number/μL | Fold-change relative to control |
| Standard Curve | Not required | Optional for calibration |
| Reference Genes | Not needed for quantification | Essential for normalization |
| Efficiency Compensation | Not required | Critical for ΔΔCT method |
| Primary Applications | Viral load quantification, copy number variation, rare mutation detection | Gene expression studies, response to therapeutic treatment |
Technological Implementation: dPCR vs qPCR
Digital PCR for Absolute Quantification
Digital PCR represents a transformative approach for absolute quantification. The technology partitions a PCR reaction into thousands of nanodroplets or nanowells, effectively creating a digital array of individual PCR reactions. Following amplification, the system counts the positive and negative partitions to provide absolute quantification through Poisson statistics [4] [5].
Recent advancements include real-time dPCR systems that further enhance sensitivity by using amplification curve analysis to eliminate false positive partitions. This approach combines the absolute quantification of dPCR with the analytical benefits of real-time amplification curve analysis, significantly improving the limit of detection for rare allele assays [5].
A key performance advantage of dPCR is its tolerance to inhibitors and capacity to analyze complex mixtures. By partitioning the sample, potential inhibitors are diluted in the positive partitions, minimizing their impact on amplification efficiency [2] [4].
Quantitative PCR for Relative Quantification
Quantitative PCR has long been the gold standard for relative quantification of nucleic acids. The two primary calculation methods are the standard curve method and the comparative CT method. While the standard curve method can approximate absolute quantification if calibrated with standards of known concentration, it remains fundamentally a relative technique when used for gene expression analysis [2].
The comparative CT method offers practical advantages for screening applications, as it does not require standard curves, increases throughput by eliminating standard wells, and allows for multiplexing target and reference genes in the same reaction [2]. However, this method requires rigorous validation to ensure that the amplification efficiencies of target and reference genes are approximately equal [2].
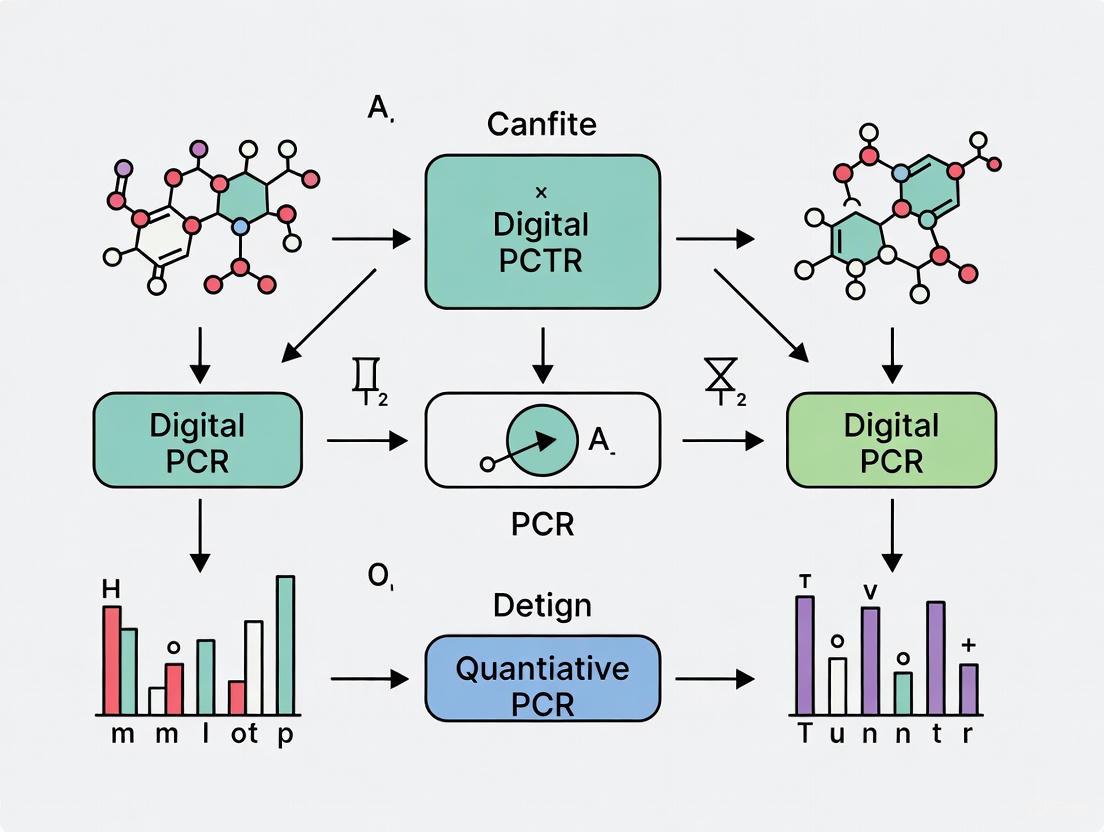
Diagram 1: Comparative Workflows of Digital PCR and Quantitative PCR
Performance Comparison: Experimental Data
Precision and Reproducibility
Multiple studies have directly compared the precision and reproducibility of dPCR and qPCR. In a controlled experiment comparing Crystal Digital PCR (cdPCR) technology to qPCR, researchers analyzed 23 technical replicates from a single PCR master mix spiked with human genomic DNA (175 cp/μl). The results demonstrated that the measurement variability of cdPCR (%CV = 2.3) was more than two-fold lower than that of qPCR (%CV = 5.0) [4].
When cdPCR replicates were pooled and analyzed as single larger samples, the precision advantage increased further, with cdPCR variability (%CV = 1.5) becoming almost three-fold lower (65.9%) than that of qPCR duplicate averages (%CV = 4.4) [4]. This enhanced precision is attributed to dPCR's endpoint determination, direct quantification method, and the high number of partitions generated per sample.
Table 2: Experimental Performance Comparison Between dPCR and qPCR
| Performance Metric | Digital PCR | Quantitative PCR | Experimental Context |
|---|---|---|---|
| Measurement Variability (%CV) | 2.3% | 5.0% | 23 technical replicates of human genomic DNA [4] |
| Pooled Sample Variability (%CV) | 1.5% | 4.4% | Pooled vs. averaged duplicates [4] |
| Sensitivity for Rare Alleles | Improved detection at lower allele frequencies | Limited by standard curve and efficiency | EGFR mutation detection [5] |
| Effect of Inhibitors | Highly tolerant | Sensitive | Complex biological samples [2] [4] |
| Dynamic Range | 1-100,000 copies/20μL [3] | Broader dynamic range | Manufacturer specifications and experimental data |
Sensitivity in Mutant Allele Detection
The ability to accurately detect and quantify mutant alleles is particularly important in cancer research and personalized medicine. A study comparing real-time dPCR to endpoint dPCR for detecting EGFR mutations (T790M, L858R, and exon 19 deletions) demonstrated that real-time dPCR improved sensitivity by establishing a lower baseline for wild-type samples [5].
For EGFR exon 19 deletion assays, samples with only 2 or more FAM-labeled positive partitions were reliably determined as positive by real-time dPCR, while endpoint dPCR required a minimum of 5 FAM-positive partitions for the same confidence level [5]. This enhanced sensitivity is crucial for liquid biopsy applications, where circulating tumor DNA (ctDNA) often represents a small fraction of total cell-free DNA.
In another study focusing on allele-specific quantitative PCR (ASQ), researchers achieved 98-100% concordance in genotype scoring with traditional methods like RFLP or Sanger sequencing while significantly reducing processing time and cost [1]. The open-source ASQ system utilized allele-specific primers, a locus-specific reverse primer, universal fluorescent probes and quenchers, and hot start DNA polymerase to genotype germline mutants through either threshold cycle (Ct) or end-point fluorescence reading [1].
Application in Mutant Allele Research
Genotyping and Mutation Detection
The accelerated pace of generating mutant alleles using customizable endonucleases like TALENs and CRISPR/Cas9 has made traditional genotyping methods a bottleneck in research pipelines [1]. While classic restriction fragment length polymorphism (RFLP) or sequencing is labor-intensive and expensive, allele-specific qPCR methods offer rapid, cost-effective alternatives.
The ASQ (allele-specific qPCR) protocol represents a significant advancement for genotyping applications. This one-step open-source method can genotype germline mutants through either threshold cycle (Ct) or end-point fluorescence reading without post-PCR processing [1]. The system has been successfully validated to genotype alleles in five different genes with high concordance to established methods, making it particularly valuable for high-throughput functional validation of disease-associated alleles [1].
Viral Load Quantification and Co-infections
In respiratory virus diagnostics, accurate quantification is essential for understanding infection dynamics, particularly during co-circulation of multiple pathogens like influenza A, influenza B, RSV, and SARS-CoV-2. A 2025 study comparing dPCR and Real-Time RT-PCR found that dPCR demonstrated superior accuracy, particularly for high viral loads of influenza A, influenza B, and SARS-CoV-2, and for medium loads of RSV [6].
dPCR showed greater consistency and precision than Real-Time RT-PCR, especially in quantifying intermediate viral levels. This precision is critical for monitoring antiviral efficacy, particularly in immunocompromised patients or those with prolonged viral shedding [6]. The absolute quantification provided by dPCR also facilitates the identification of co-infections and assessment of their relative contribution to disease burden, which is not possible with qualitative detection alone [6].
Practical Implementation: Methodologies and Reagents
Experimental Protocols
Allele-Specific Quantitative PCR (ASQ) Protocol [1]:
- Genomic DNA Preparation: Use hot sodium hydroxide (NaOH) extraction method for rapid preparation (25 min incubation in 50 mM NaOH at 95°C with shaking) followed by neutralization with Tris buffer.
- Primer Design: Design allele-specific primers (ASPs) with the discriminatory nucleotide at the 3' end, combined with a locus-specific reverse primer.
- Reaction Setup: Combine ASPs with universal fluorescent probes (FAM or HEX conjugated) and corresponding quenchers (Black Hole Quencher 1).
- Thermal Cycling: Use hot start DNA polymerase with optimized cycling conditions.
- Analysis: Genotype through either threshold cycle (Ct) method in a qPCR machine or end-point fluorescence reading in a plate reader.
Digital PCR Protocol for Rare Allele Detection [5]:
- Sample Preparation: Mix wild-type and mutant genomic DNA in desired ratios based on fluorometric quantification.
- Partitioning: Load samples into dPCR system (chip-based or droplet-based) creating 20,000+ individual partitions.
- Amplification: Perform endpoint PCR with target-specific assays.
- Data Analysis: For real-time dPCR, use amplification curves to eliminate false positive partitions; for endpoint dPCR, use fluorescence thresholds.
- Quantification: Apply Poisson statistics to calculate absolute copy numbers and mutant allele frequencies.
Research Reagent Solutions
Table 3: Essential Research Reagents for Absolute and Relative Quantification
| Reagent/Instrument | Function | Application Notes |
|---|---|---|
| Allele-Specific Primers | Specifically amplify mutant or wild-type alleles | Design with discriminatory base at 3' end; critical for ASQ [1] |
| Universal Fluorescent Probes | Detection of amplified products | FAM and HEX conjugated; used with shorter quenchers [1] |
| Hot Start DNA Polymerase | Prevents non-specific amplification | Essential for both dPCR and qPCR assays [1] |
| Digital PCR Systems | Partitioning and absolute quantification | Includes chip-based (QIAcuity) and droplet-based (ddPCR) platforms [4] [6] |
| Reference Gene Assays | Normalization for relative quantification | β-actin, GAPDH, rRNA; must demonstrate stable expression [2] [3] |
The choice between absolute and relative quantification methodologies depends fundamentally on the research question and application requirements. Absolute quantification using digital PCR provides superior precision, sensitivity for rare alleles, and tolerance to inhibitors, making it ideal for liquid biopsy applications, viral load quantification, and copy number variation studies [4] [6] [5]. Relative quantification using qPCR remains a robust, cost-effective solution for gene expression studies, particularly when screening large sample sets where fold-change differences provide sufficient biological insight [2] [3].
For mutant allele research, emerging technologies like real-time dPCR and allele-specific qPCR are addressing critical bottlenecks in genotyping workflows. Real-time dPCR significantly improves the limit of detection for rare alleles by eliminating false positives through amplification curve analysis [5], while ASQ provides a rapid, open-source platform for high-throughput genotyping of engineered mutants [1]. As these technologies continue to evolve, they will further empower researchers and drug development professionals in their pursuit of precision medicine and personalized therapeutic strategies.
Quantitative PCR (qPCR) is a powerful molecular biology technique that enables the detection and quantification of nucleic acids in real-time during the amplification process. The core principle of qPCR lies in monitoring the fluorescence emitted during each PCR cycle, which is directly proportional to the amount of amplified DNA product. The calibration curve, also known as the standard curve, serves as the fundamental mathematical model that translates the fluorescence detection data into meaningful quantitative results. This curve is generated by amplifying a dilution series of known template concentrations and plotting their quantification cycle (Cq) values against the logarithm of their initial concentrations.
The relationship is described by the linear equation: Cq = slope × log(N₀) + intercept, where the slope is used to calculate the amplification efficiency via the formula E = 10^(-1/slope) - 1 [7] [8]. An ideal PCR reaction with 100% efficiency corresponds to a slope of -3.32, though in practice, reactions with efficiencies between 90-110% (slope of -3.58 to -3.10) are generally considered acceptable [8]. The reliability of this standard curve method has been validated through extensive testing, such as in studies measuring the expression of 6 genes in 42 breast cancer biopsies, demonstrating its utility in routine laboratory practice [7].
The qPCR Workflow: From Fluorescence to Quantification
The transformation of raw fluorescence signals into quantitative data involves a multi-step data processing procedure. The following diagram illustrates this complete workflow:
Data Processing and Noise Filtering
The initial phase of qPCR data analysis focuses on noise filtering to enhance data quality. Raw fluorescence readings often contain non-specific cycle-to-cycle scattering that requires correction. The standard processing approach includes three sequential steps [7]:
- Smoothing: Random cycle-to-cycle noise is reduced using a 3-point moving average (with two-point averages applied at the first and last data points)
- Baseline Subtraction: Background fluorescence is eliminated by subtracting the minimal fluorescence value observed through the entire run
- Amplitude Normalization: Plateau scattering is addressed by normalizing to the maximal fluorescence value in each reaction well over the complete PCR run
This noise filtering process transforms raw fluorescence data into clean amplification curves suitable for reliable crossing point determination [7].
Crossing Point Determination and Standard Curve Generation
The crossing point (CP), also referred to as quantification cycle (Cq), represents the cycle number at which the fluorescence signal intersects a predetermined threshold line. In standard curve methodology, the optimal threshold is typically selected automatically by identifying the position that yields the maximum coefficient of determination (r²) for the standard curve, often exceeding 99% [7]. The standard curve itself is generated by performing linear regression on the plot of CP values against the logarithm of known template concentrations for the dilution series.
The statistical assessment of intra-assay variation is a critical advantage of this approach. Means and variances are calculated for CP values in PCR replicates, and these variances are propagated through subsequent calculations using error propagation principles, providing confidence intervals for final quantitative results [7].
Comparative Performance: qPCR vs. dPCR for Mutant Allele Detection
In the context of detecting mutant alleles, particularly for cancer research and personalized medicine applications, the limitations and strengths of qPCR become apparent when compared with digital PCR (dPCR). The following table summarizes key performance characteristics based on experimental data:
Table 1: Performance comparison between qPCR and dPCR for mutant allele detection
| Performance Characteristic | qPCR (ARMS-based) | Droplet Digital PCR (dPCR) | Experimental Context |
|---|---|---|---|
| Detection Limit | ~1% mutation rate [9] | ≤0.1% mutation rate [9] [10] | EGFR T790M mutation detection in plasmid samples [9] |
| Quantification Type | Relative (requires standard curve) [10] [8] | Absolute (no standard curve needed) [9] [10] | Direct comparison using identical samples [9] |
| Dynamic Range | Broad [11] | Limited by partition number [11] | Detection of Xanthomonas citri subsp. citri [11] |
| Precision at Low Concentration | Higher CV (coefficient of variation) [11] | Lower CV, especially at low target concentration [11] | Pathogen quantification in plant samples [11] |
| Tolerance to PCR Inhibitors | Moderate [10] | High (due to sample partitioning) [10] | Analysis of environmental and clinical samples [10] [11] |
| Practical Agreement | 91.7% overall agreement with dPCR [12] | Reference method for discordant samples [9] [12] | EGFR T790M detection in clinical NSCLC samples [12] |
Experimental Evidence in Mutant Allele Detection
The comparative performance of qPCR and dPCR has been extensively evaluated in mutation detection studies, particularly for epidermal growth factor receptor (EGFR) mutations in non-small cell lung cancer (NSCLC). In one study comparing amplification refractory mutation system-based qPCR (ARMS-qPCR) and droplet digital PCR (ddPCR) for detecting EGFR T790M mutation, the ARMS-qPCR method reliably detected plasmid samples with 5% and 1% mutation rates, while ddPCR consistently detected mutation rates as low as 0.1% (approximately 6 mutant copies in 6,000 wild-type copies) [9].
Clinical validation using 10 formalin-fixed paraffin-embedded (FFPE) tumor samples from NSCLC patients revealed concordance in 9 samples between the two methods. Notably, sample N006, identified as EGFR wild-type by ARMS-qPCR, was shown to harbor a clear EGFR T790M mutation using ddPCR technology, with 7 copies of mutant alleles detected against a background of 6,000 wild-type copies [9]. This demonstrates ddPCR's superior sensitivity for detecting low-abundance mutations in clinical samples, which is crucial for early detection of resistance mutations during tyrosine kinase inhibitor therapy.
A larger study of 72 NSCLC patients comparing QuantStudio 3D dPCR and droplet dPCR for detecting T790M mutation in cell-free DNA found 91.7% overall agreement (66/72 samples). The 6 discordant samples showed low mutation abundance (~0.1%), with the discrepancy attributed to stricter threshold settings for QS3D dPCR [12].
Methodological Protocols for qPCR Calibration Curve Assays
Standard Curve Generation Protocol
The following diagram outlines the experimental workflow for establishing a qPCR calibration curve:
The standard curve generation begins with preparation of a serial dilution series of known template concentration, typically spanning 5-6 orders of magnitude (e.g., 10-fold dilutions). The template can be purified PCR product, plasmid DNA constructs, or synthetic oligonucleotides spanning the PCR amplicon [8]. Each dilution should be amplified in multiple replicates (typically 3+ replicates) to account for technical variability.
During the qPCR run, fluorescence data is collected at each cycle. Following amplification, the raw fluorescence data undergoes processing as described in Section 2.1. The optimal threshold for Cq determination is selected to maximize the coefficient of determination (r²) of the standard curve [7]. Linear regression of Cq values versus the logarithm of initial template concentrations generates the standard curve equation, from which amplification efficiency is calculated [8].
Advanced Calibration Approaches
Recent methodological advances have addressed limitations in traditional standard curve approaches. The Pairwise Efficiency method represents a novel mathematical approach to qPCR data analysis that improves the precision of calibration curve assays. This method uses a modified formula describing pairwise relationships between data points on separate amplification curves from a dilution series, enabling extensive statistical analysis. Compared to the standard calibration curve method, Pairwise Efficiency demonstrates nearly double the precision in qPCR efficiency determinations and a 2.3-fold improvement in precision of gene expression ratio estimations using the same experimental dataset [13].
For applications requiring correction of variations in amplification efficiency between standards and samples, the One-Point Calibration (OPC) method has been developed. This approach corrects for efficiency differences and has shown superior accuracy compared to the standard curve method when quantifying artificial template mixtures with differing amplification efficiencies. In validation studies, while the standard curve method deviated from the expected nifH gene copy number by 3- to 5-fold, the OPC method quantified template mixtures with high accuracy [14].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Essential research reagents and materials for qPCR calibration curve assays
| Reagent/Material | Function/Purpose | Specification Notes |
|---|---|---|
| Standard Template | Provides known concentration reference for standard curve | Purified PCR product, plasmid DNA, or synthetic oligonucleotides; must span the amplicon [8] |
| qPCR Master Mix | Contains enzymes, dNTPs, buffer for amplification | SYBR Green or probe-based; optimized for efficiency [7] |
| Primer Pairs | Sequence-specific amplification | Designed for target specificity; optimal GC content [14] |
| Probe (if applicable) | Sequence-specific detection | Hydrolysis (TaqMan) or hybridization formats; FAM-labeled common [8] |
| Nuclease-free Water | Reaction reconstitution | Free of contaminants and nucleases |
| qPCR Plates/Tubes | Reaction vessel | Optically clear; compatible with instrument [9] |
| Sealing Materials | Prevents evaporation | Optical seals or caps [7] |
| Positive Control | Assay validation | Known positive sample for quality control |
| No Template Control (NTC) | Contamination check | Water instead of template; should not amplify [9] |
The qPCR calibration curve method remains a fundamental tool for nucleic acid quantification, providing a reliable approach for relative quantification in gene expression analysis and mutation detection. While the method is well-established and widely used, its limitations in detecting very low-abundance mutations (<1%) have become apparent in applications requiring high sensitivity, such as cancer resistance mutation monitoring. The emergence of digital PCR platforms offers complementary capabilities with absolute quantification and enhanced sensitivity for rare variant detection.
The continuing development of improved calibration methods, such as Pairwise Efficiency and One-Point Calibration, demonstrates that innovation in qPCR methodology remains active. For researchers and clinical diagnosticians, the choice between qPCR and dPCR technologies depends on the specific application requirements, with qPCR maintaining advantages in dynamic range and established workflows, while dPCR provides superior sensitivity for low-abundance targets and absolute quantification without standard curves.
Digital PCR (dPCR) represents a significant advancement in nucleic acid quantification, enabling the absolute detection and measurement of target DNA sequences without reliance on standard curves. This technology's core principles—sample partitioning, end-point analysis, and Poisson statistical analysis—provide unmatched precision for applications requiring high sensitivity, particularly in detecting rare mutant alleles in cancer research and liquid biopsies. This guide explores the fundamental mechanics of dPCR and provides an objective comparison with quantitative PCR (qPCR) through experimental data, offering researchers a comprehensive resource for selecting appropriate molecular detection methods.
Digital PCR (dPCR) has emerged as a powerful technique for absolute quantification of nucleic acids, operating on three fundamental principles: sample partitioning, end-point detection, and Poisson statistics [15]. Unlike quantitative PCR (qPCR) that measures amplification in real-time relative to standard curves, dPCR physically partitions a sample into thousands to millions of individual reactions where amplification occurs independently [16]. This partitioning process effectively dilutes the template molecules such that each partition contains either zero, one, or a few target molecules [15]. Following PCR amplification to endpoint, each partition is analyzed for the presence or absence of a fluorescent signal, with positive partitions indicating the presence of at least one target molecule [17]. The binary data generated (positive/negative partitions) is then subjected to Poisson statistical analysis to calculate the absolute concentration of the target sequence in the original sample [18]. This mechanistic approach provides dPCR with significant advantages for detecting low-abundance targets and achieving precise quantification without external references.
The application of dPCR has become particularly valuable in fields requiring high sensitivity and precision, such as cancer research and liquid biopsy analysis, where it can detect rare mutations with mutant allele frequencies as low as 0.1% [19]. Additionally, dPCR has demonstrated superior performance in viral load quantification and copy number variation analysis, often outperforming traditional qPCR in reproducibility and resistance to PCR inhibitors [6] [16]. As research continues to demand higher sensitivity for detecting rare mutations and quantifying slight genetic variations, understanding the core mechanics of dPCR becomes essential for selecting appropriate molecular detection methods.
Core Mechanical Principles of dPCR
Sample Partitioning Strategies
The foundation of dPCR lies in its ability to partition a single PCR reaction into numerous individual reactions, a process achieved through different technological approaches:
Droplet-based Partitioning (ddPCR): This method utilizes microfluidics to partition the sample into thousands to millions of nanoliter-sized oil-emulsion droplets [15] [20]. The QX200 droplet digital PCR (ddPCR) system from Bio-Rad represents this approach, where each droplet functions as an individual PCR microreactor [18]. The random distribution of template molecules into droplets follows Poisson distribution, with most droplets containing either zero or one template molecule at appropriate dilutions.
Chip-based/Nanoplate-based Partitioning (cdPCR): This alternative approach employs microfluidic chips with fixed nanowells or microchambers to partition the sample [15] [20]. Systems like the QIAcuity from QIAGEN use nanoplate technology with approximately 26,000 individual wells [6] [18], while the QuantStudio Absolute Q system utilizes microfluidic array plates (MAP) technology [19]. These systems offer simplified workflows by integrating partitioning and thermal cycling into single steps.
The partitioning process effectively enriches low-abundance targets by separating them from abundant background DNA, significantly enhancing detection sensitivity for rare alleles [21] [19]. The number of partitions directly impacts precision, with higher partition counts providing better statistical confidence and lower detection limits [18].
End-Point Analysis and Detection
Following partitioning and thermal cycling, dPCR employs end-point detection to analyze each partition:
Fluorescence Detection: After PCR amplification is complete, each partition is analyzed for fluorescence using either laser scanning or imaging systems [18]. Probe-based chemistries (such as TaqMan probes) are typically used, with different fluorescent labels for various targets enabling multiplexing capabilities [19].
Signal Classification: Partitions are classified as positive or negative based on their fluorescence intensity exceeding a predetermined threshold [17]. This binary classification is fundamental to the digital nature of the technology, enabling absolute quantification without reference to amplification kinetics [16].
Real-time dPCR Enhancement: Recent advancements have introduced real-time dPCR, which collects amplification data throughout the thermal cycling process rather than just at endpoint [5]. This approach enables the identification and elimination of false positive signals based on their atypical amplification profiles, further improving detection sensitivity and accuracy, particularly for rare allele detection [5].
Poisson Statistics and Absolute Quantification
The mathematical foundation of dPCR relies on Poisson statistics to calculate target concentration from the binary partition data:
Principle of Poisson Distribution: Poisson statistics account for the random distribution of template molecules across partitions [15] [18]. The model assumes that template molecules follow a Poisson distribution during partitioning, meaning some partitions will contain multiple copies while others contain none or one.
Concentration Calculation: The fundamental Poisson equation used in dPCR is: [ C = -\ln(1 - p) \times V^{-1} ] Where (C) is the target concentration, (p) is the proportion of positive partitions, and (V) is the partition volume [18]. This calculation provides absolute quantification without standard curves, a significant advantage over qPCR.
Limitations and Considerations: The accuracy of Poisson statistics depends on having sufficient partitions and appropriate template dilution to avoid saturation effects [18]. When too many partitions are positive (typically >90%), the Poisson model becomes less accurate due to an increasing number of partitions containing multiple template molecules [16].
Table 1: Comparison of dPCR Partitioning Technologies
| Feature | Droplet-based (ddPCR) | Chip/Nanoplate-based (cdPCR) |
|---|---|---|
| Partition Mechanism | Oil-emulsion droplets | Fixed nanowells/microchambers |
| Typical Partition Count | 20,000 (QX200) [18] | 26,000 (QIAcuity) [6] |
| Throughput | Moderate | High with automation |
| Reaction Assembly | Separate partitioning step | Integrated partitioning and cycling |
| Detection Method | Flow cytometry | Imaging |
Experimental Comparison: dPCR vs qPCR for Mutant Allele Detection
Methodology for Performance Comparison
To objectively evaluate the performance of dPCR against qPCR for detecting mutant alleles, we designed a comparative analysis based on published experimental approaches:
Sample Preparation: Contrived samples were prepared using mixed genomic DNA from wild-type and mutant cell lines to simulate clinical samples with known mutant allele frequencies (MAF) [5]. For EGFR mutation detection, DNA from mutant cell lines (NCI-H1975 for T790M and L858R; HCC827 for exon 19 deletions) was mixed with wild-type human genomic DNA at varying ratios [5].
Instrumentation and Platforms: Experiments compared leading dPCR systems including the QIAcuity One nanoplate-based system (QIAGEN) and QX200 droplet-based system (Bio-Rad) against standard qPCR platforms [6] [18]. The novel real-time dPCR system was also evaluated against endpoint dPCR for rare allele detection [5].
Data Analysis: For dPCR, absolute quantification was performed using Poisson statistics [18]. qPCR analysis utilized standard curve-based quantification with serial dilutions of known standards [16]. Sensitivity, specificity, limit of detection (LOD), and precision were calculated for both technologies across multiple replicates.
Table 2: Key Research Reagent Solutions for dPCR Mutation Detection
| Reagent/Equipment | Function | Example Products |
|---|---|---|
| Digital PCR System | Partitioning, amplification, and detection | QIAcuity One, QX200 ddPCR, QuantStudio Absolute Q |
| Assay Kits | Target-specific detection | Absolute Q Liquid Biopsy dPCR Assays [19] |
| Master Mix | PCR reagents and enzymes | dPCR-specific master mixes with optimized buffers |
| Restriction Enzymes | Improve DNA accessibility | HaeIII, EcoRI (for complex genomes) [18] |
| Nucleic Acid Extraction Kits | Sample preparation | MagMax Viral/Pathogen kit [6] |
Quantitative Performance Data
Experimental results demonstrate distinct performance characteristics between dPCR and qPCR technologies:
Sensitivity and Limit of Detection: dPCR consistently shows superior sensitivity for rare allele detection. In respiratory virus detection, dPCR demonstrated significantly improved accuracy for high viral loads of influenza A, influenza B, and SARS-CoV-2, and for medium loads of RSV [6]. For EGFR mutation detection, real-time dPCR achieved a lower limit of detection compared to endpoint dPCR, requiring only 2 positive partitions for positive calling compared to 5 for endpoint systems [5].
Precision and Reproducibility: dPCR exhibits enhanced precision, particularly at low target concentrations. A comparative study of dPCR platforms found coefficient of variation (CV) values below 5% for optimal systems, with generally higher precision observed when using specific restriction enzymes like HaeIII instead of EcoRI [18]. This precision advantage is most pronounced at low template concentrations where qPCR variability increases substantially.
Quantification Accuracy: dPCR provides more accurate quantification at low allele frequencies. For EGFR mutations, real-time dPCR generated mutant allele frequencies closer to expected values at very low MAF compared to endpoint dPCR [5]. However, at high target concentrations or for gene amplification assays, both technologies show comparable performance [5].
Table 3: Performance Comparison of dPCR vs qPCR for Mutation Detection
| Parameter | Digital PCR | Quantitative PCR |
|---|---|---|
| Detection Limit | 0.1% mutant allele frequency [19] | Typically 1-5% mutant allele frequency |
| Quantification Method | Absolute (Poisson statistics) | Relative (standard curve required) |
| Precision at Low Concentration | CV: 5-13% [18] | CV: 15-25% or higher |
| Impact of Inhibitors | Reduced effect due to partitioning [16] | Significant impact on amplification efficiency |
| Dynamic Range | Limited at high concentrations [16] | Broad with optimized assays |
| Multiplexing Capability | Moderate (2-5 plex) [6] | High with different reporter dyes |
dPCR Workflow Visualization
The following diagram illustrates the complete experimental workflow for digital PCR analysis, from sample preparation through data interpretation:
Diagram 1: dPCR Experimental Workflow. Key distinguishing steps of dPCR (partitioning, binary classification, and Poisson analysis) are highlighted.
Discussion and Technical Considerations
Applications and Practical Implementation
The mechanical principles of dPCR make it particularly suitable for specific research applications:
Rare Mutation Detection: dPCR's partitioning mechanics enable detection of rare mutations down to 0.1% allele frequency, making it invaluable for liquid biopsy applications in oncology [19] [5]. The technology can identify emerging resistance mutations (e.g., EGFR T790M) and monitor minimal residual disease with sensitivity exceeding qPCR.
Copy Number Variation (CNV) Analysis: dPCR provides absolute quantification for precise CNV determination without reference standards, offering advantages over qPCR for detecting subtle copy number differences [15] [18].
Viral Load Quantification: dPCR's absolute quantification capability improves accuracy in viral load measurements, as demonstrated in respiratory virus studies where it outperformed qPCR across different viral load categories [6].
Limitations and Practical Challenges
Despite its advantages, dPCR presents several practical limitations:
Throughput and Cost: dPCR typically has lower throughput and higher per-sample cost compared to qPCR, making it less suitable for high-volume screening [16] [17]. The specialized equipment and consumables contribute to higher operational costs.
Dynamic Range Limitations: While excellent for low-abundance targets, dPCR has a more limited dynamic range at high target concentrations due to partition saturation effects [16] [18].
Technical Complexity: The requirement for partitioning and more complex data analysis presents a steeper learning curve compared to qPCR, though newer integrated systems are addressing this challenge [19].
The core mechanics of dPCR—sample partitioning, end-point analysis, and Poisson statistics—provide a fundamentally different approach to nucleic acid quantification compared to traditional qPCR. This mechanistic foundation enables absolute quantification without standard curves and superior sensitivity for rare target detection. Experimental data consistently demonstrates dPCR's advantages for applications requiring high precision at low concentrations, particularly in mutant allele detection for cancer research.
For researchers investigating rare mutations or requiring absolute quantification, dPCR offers significant performance benefits despite its higher cost and lower throughput. Continued technological advancements, including real-time dPCR and improved multiplexing capabilities, are further expanding dPCR's applications in both research and clinical diagnostics. The choice between dPCR and qPCR ultimately depends on specific application requirements, with dPCR representing the optimal tool for challenging detection scenarios where sensitivity and precision are paramount.
Digital PCR (dPCR) represents a fundamental shift in nucleic acid quantification from quantitative PCR (qPCR). While qPCR relies on relative quantification by comparing the amplification cycle number (Cq) to a standard curve, dPCR provides absolute quantification by partitioning a sample into thousands of individual reactions and applying Poisson statistics to count target molecules directly [11] [22]. This core difference in methodology underlies the significant performance advantages dPCR offers for detecting rare mutant alleles, particularly in applications like liquid biopsy and oncogene monitoring where sensitivity and precision are paramount [9] [22].
The partitioning process in dPCR enables single-molecule detection, making it possible to identify rare mutations present at very low abundances within a background of wild-type sequences [22]. This technical advancement has positioned dPCR as a crucial tool in precision medicine, where early detection of treatment resistance mutations can inform clinical decisions before acquired resistance becomes clinically evident [9].
Comparative Performance Metrics
Direct comparisons between dPCR and qPCR across multiple studies reveal consistent patterns of performance differences in key metrics essential for mutant allele detection.
Table 1: Direct Performance Comparison between dPCR and qPCR
| Performance Metric | Digital PCR Performance | Quantitative PCR Performance | Experimental Context |
|---|---|---|---|
| Sensitivity | Detects EGFR T790M mutations at 0.1% mutation rate [9] | Requires ≥1% mutation rate for reliable detection [9] | Plasmid DNA samples with defined mutation rates [9] |
| Precision | Intra-assay CV: 4.5% (periodontal pathobionts) [23] | Higher intra-assay variability than dPCR (p=0.020) [23] | Subgingival plaque samples from periodontitis patients [23] |
| Dynamic Range | Broader dynamic range for Xanthomonas citri detection [11] | Good linearity but narrower dynamic range [11] | Plant pathogen detection in citrus crops [11] |
| Tolerance to Inhibitors | Reduced susceptibility to PCR inhibitors [11] | More significantly affected by inhibitors [11] | Analysis of plant-derived inhibitors in environmental samples [11] |
| Limit of Detection | 0.17 copies/μL (QX200 ddPCR) [18] | Higher detection limits, varies by assay [11] | Synthetic oligonucleotide dilutions [18] |
| Limit of Quantification | 4.26 copies/μL (QX200 ddPCR) [18] | Higher quantification limits [9] | Synthetic oligonucleotide dilutions [18] |
Sensitivity and Limit of Detection
dPCR demonstrates substantially superior sensitivity for detecting low-abundance targets. In a landmark study comparing EGFR T790M mutation detection, dPCR reliably identified mutations at 0.1% mutation rates (approximately 6 mutant copies among 6,000 wild-type copies), while the ARMS-qPCR method required 1-5% mutation rates for stable detection [9]. This enhanced sensitivity has direct clinical relevance, as researchers identified one clinical sample (N006) with a clear T790M mutation using dPCR that was classified as wild-type by ARMS-qPCR [9].
This sensitivity advantage extends beyond oncology applications. In periodontal microbiology, dPCR demonstrated superior detection of low bacterial loads, particularly for P. gingivalis and A. actinomycetemcomitans, resulting in qPCR false negatives at concentrations below 3 log₁₀ genomic equivalents/mL [23]. The fundamental partitioning approach enables dPCR to detect single molecules, with studies reporting limits of detection as low as 0.17 copies/μL for the QX200 ddPCR system [18].
Precision and Reproducibility
dPCR exhibits significantly better precision, especially at low target concentrations. In periodontal pathogen quantification, dPCR showed lower intra-assay variability (median CV: 4.5%) compared to qPCR [23]. This precision advantage is most pronounced near the detection limit, where qPCR results typically show higher coefficients of variation [11].
Precision in dPCR is influenced by platform choice and experimental conditions. A 2025 study comparing the QX200 droplet dPCR and QIAcuity One nanoplate dPCR found both platforms provided high precision, though performance varied with restriction enzyme selection [18]. When using the HaeIII restriction enzyme, the QX200 system achieved exceptional precision with all CV values below 5% across various cell numbers of Paramecium tetraurelia [18].
Dynamic Range
The dynamic range characteristics of dPCR and qPCR differ significantly. While qPCR typically demonstrates a broader dynamic range in some applications [11], dPCR provides excellent linearity across its effective range. One study reported high linearity (R² > 0.99) for dPCR across measurable concentrations [23].
A key consideration in dPCR analysis is the optimal partition occupancy rate. According to Poisson statistics, the optimal range for accurate quantification is between 0.1 and 5 copies per partition [22]. Beyond approximately 6-7 copies per partition, saturation effects occur, reducing quantification accuracy. This fundamental limitation defines the effective dynamic range of dPCR systems, though sample dilution can extend the measurable range.
Tolerance to PCR Inhibitors
dPCR demonstrates superior tolerance to PCR inhibitors commonly found in clinical and environmental samples. In plant pathogen detection, the influence of PCR inhibitors was "considerably reduced" in dPCR compared to qPCR assays [11]. This advantage stems from the partitioning process, which effectively dilutes inhibitors across thousands of individual reactions, reducing their local concentration and minimizing interference with amplification [22].
The endpoint measurement approach in dPCR also contributes to its resilience against inhibitors. Unlike qPCR, which depends on the efficiency of amplification throughout all cycles, dPCR only requires sufficient amplification to generate a fluorescent signal above background in positive partitions, making it less vulnerable to inhibitors that reduce amplification efficiency [11].
Experimental Protocols for Performance Validation
Protocol for Sensitivity and Limit of Detection Determination
To evaluate detection sensitivity for mutant alleles, researchers can employ plasmid models with defined mutation rates:
- Plasmid Standard Preparation: Construct plasmid standards containing wild-type and mutant sequences (e.g., EGFR T790M). Create dilution series with defined mutation rates (0.1%, 0.5%, 1%, 5%) by mixing mutant and wild-type plasmids [9].
- Sample Processing: Adjust templates to a unified concentration (e.g., 10 ng/μL). For dPCR, prepare 25 μL reactions using 2X Master Mix, primer-probe mix, and template [9].
- Partitioning and Amplification: For ddPCR, generate droplets using a droplet generator cartridge. Thermal cycling conditions: 95°C for 10 minutes, followed by 40 cycles of 94°C for 30 seconds and 58°C for 1 minute, then 98°C for 10 minutes [9].
- Data Analysis: Calculate mutant allele frequency using Poisson statistics from positive and negative partitions [22].
Protocol for Precision Assessment
Method for determining inter-assay and intra-assay precision:
- Sample Preparation: Use synthetic oligonucleotides or DNA extracted from reference cell lines. Prepare replicate samples across multiple runs [18].
- Experimental Design: For intra-assay precision, analyze multiple replicates within the same run. For inter-assay precision, analyze replicates across different runs, days, or operators [23].
- Statistical Analysis: Calculate coefficient of variation (CV%) for replicate measurements. Apply statistical frameworks like Generalized Linear Models (GLM) or Multiple Ratio Tests (MRT) for comparing multiple dPCR experiments [24].
Protocol for Inhibitor Tolerance Evaluation
Assessing inhibitor resistance using environmental or clinical samples:
- Sample Collection: Collect samples with inherent inhibitors (e.g., plant tissues, FFPE samples, blood) [11].
- Inhibitor Spiking: Add known PCR inhibitors (humic acids, heparin, IgG) to purified DNA samples in increasing concentrations [11].
- Parallel Analysis: Process identical samples with dPCR and qPCR simultaneously. For dPCR, use 40 μL reactions with restriction enzymes if needed to improve DNA accessibility [23] [18].
- Quantification Comparison: Compare quantification results between platforms, noting the concentration at which qPCR fails while dPCR continues to provide accurate quantification [11].
dPCR Platform Comparisons
Different dPCR platforms exhibit distinct performance characteristics that researchers should consider when selecting instrumentation.
Table 2: Comparison of dPCR Platforms and Technologies
| Platform/Technology | Partitioning Method | Key Advantages | Typical Partitions | Optimal Applications |
|---|---|---|---|---|
| Droplet dPCR | Water-in-oil emulsion [22] | High partition count, well-established | Up to 20,000 partitions [9] | High sensitivity applications, rare variant detection [9] |
| Nanoplate dPCR | Microfabricated chips [22] | Simplified workflow, reduced cross-contamination | ~26,000 partitions [23] | Routine clinical tests, multiplex applications [23] |
| BEAMing Technology | Emulsion with magnetic beads [22] | Combination with flow cytometry, high multiplexing | Variable | Rare cell detection, single-cell analysis [22] |
| Microfluidic Chip | Fixed microchambers [22] | Excellent reproducibility, consistent volumes | Thousands to millions [22] | Regulatory applications, lot release testing [25] |
A 2025 comparative study of the QX200 ddPCR (Bio-Rad) and QIAcuity One nanoplate dPCR (QIAGEN) systems found both platforms demonstrated similar detection and quantification limits with high precision across most analyses [18]. The QX200 system showed a limit of detection of approximately 0.17 copies/μL, while the QIAcuity system's LOD was approximately 0.39 copies/μL [18]. However, precision was influenced by restriction enzyme selection, with HaeIII providing better precision than EcoRI, especially for the QX200 system [18].
Application Workflows for Mutant Allele Detection
The detection of rare mutant alleles follows a structured workflow that leverages dPCR's strengths in partitioning and absolute quantification.
Figure 1: dPCR Workflow for Mutant Allele Detection
This workflow enables researchers to detect rare mutations with unparalleled sensitivity. In liquid biopsy applications for oncology, the process begins with cell-free DNA extraction from blood plasma, followed by dPCR reaction setup with mutation-specific probes [9] [12]. After partitioning and amplification, the analysis phase applies Poisson statistics to calculate mutant allele frequency, enabling detection of mutations present at frequencies as low as 0.1% [9].
Research Reagent Solutions
Successful dPCR experiments require carefully selected reagents and optimized reaction conditions.
Table 3: Essential Research Reagents for dPCR Experiments
| Reagent Category | Specific Examples | Function & Importance | Optimization Tips |
|---|---|---|---|
| DNA Extraction Kits | QIAamp DNA FFPE Tissue Kit [9], QIAamp DNA Mini Kit [23] | Obtain high-quality template DNA free of inhibitors | Ensure appropriate elution volume for target concentration [9] |
| dPCR Master Mixes | ddPCR 2X Master Mix [9], QIAcuity Probe PCR Kit [23] | Provide optimized buffer, enzymes, dNTPs for partitioning | Include restriction enzymes (e.g., HaeIII) for complex genomes [18] |
| Primers & Probes | TaqMan hydrolysis probes [9], Target-specific primers [23] | Enable specific detection of mutant vs. wild-type alleles | Optimize concentrations (e.g., 0.4μM primers, 0.2μM probes) [23] |
| Reference Assays | Reference genes (e.g., for total DNA quantification) [9] | Normalize for DNA input quantity and quality | Select reference targets with similar amplification efficiency [9] |
| Partitioning Reagents | Droplet Generation Oil [9], Nanoplate seals [23] | Create stable partitions for individual reactions | Ensure proper storage and handling to maintain partition integrity [9] |
Digital PCR demonstrates clear advantages over qPCR for detecting mutant alleles across all four key performance metrics. The technology provides superior sensitivity for rare variant detection, enhanced precision especially at low target concentrations, excellent linearity across its dynamic range, and greater resilience to PCR inhibitors. These performance characteristics make dPCR particularly valuable for applications requiring absolute quantification of rare mutations, such as liquid biopsy monitoring of cancer treatment resistance [9], early pathogen detection [23], and environmental monitoring [11].
While dPCR may have a more limited dynamic range compared to qPCR and requires specialized instrumentation, its performance benefits justify the adoption in research and clinical settings where detection of low-abundance targets is critical. As dPCR technology continues to evolve with improvements in multiplexing capabilities, workflow automation, and data analysis tools, its application in mutant allele detection is expected to expand further, potentially enabling new approaches in precision medicine and molecular diagnostics [25] [22].
For researchers detecting mutant alleles, the choice between quantitative PCR (qPCR) and digital PCR (dPCR) often comes down to a fundamental question: should results be interpreted through the Cycle Threshold (Ct), a relative and indirect measure, or the absolute copies/μL, a direct count of target molecules? This guide provides an objective comparison of these two quantification methods and the technologies that produce them.
Core Concepts: Ct and Copies/μL Defined
What is Cycle Threshold (Ct)?
In quantitative real-time PCR (qPCR), the Cycle Threshold (Ct) value is the PCR cycle number at which the amplification curve of a target sequence crosses a fluorescence threshold set above the background level [26] [27]. This value is inversely proportional to the starting amount of the target nucleic acid: a lower Ct value indicates a higher initial target concentration, while a higher Ct value indicates a lower concentration [26] [28].
Crucially, the Ct value is a relative measure. To convert a Ct value into a concentration, a standard curve with samples of known concentrations must be run alongside the experimental samples [28]. The quantitative relationship is described by the formula: Quantity ≈ e-Ct, where 'e' represents the amplification efficiency [26].
What is Copies/μL?
Copies per microliter (copies/μL) is a unit of absolute quantification. It represents the exact number of target DNA or RNA molecules present in a given volume of sample [22]. This measurement is the primary output of digital PCR (dPCR).
dPCR achieves this by partitioning a PCR reaction into thousands of individual nanoreactions. After amplification, the platform counts the number of partitions that contain the target sequence (positive partitions) and applies Poisson statistics to calculate the absolute concentration in the original sample, without the need for a standard curve [6] [22].
Technology Face-Off: qPCR vs. dPCR
The following table summarizes the fundamental differences between the two technologies that generate Ct values and copies/μL.
| Feature | Quantitative Real-Time PCR (qPCR) | Digital PCR (dPCR) |
|---|---|---|
| Quantification Type | Relative (requires standard curve) | Absolute (no standard curve) |
| Primary Output | Cycle Threshold (Ct) | Copies/μL |
| Principle | Monitors amplification in real-time | Partitions sample, uses end-point detection & Poisson statistics |
| Sensitivity & Precision | High | Superior, especially for low-abundance targets and rare mutations [6] [29] |
| Tolerance to Inhibitors | Moderate | High [30] |
| Throughput & Cost | High throughput, lower cost per sample | Lower throughput, higher cost per sample [6] |
| Ideal For | High-throughput screening, gene expression (relative), well-established diagnostic assays | Absolute quantification, rare allele detection (e.g., ctDNA, minor clones), copy number variation [29] [31] |
Experimental Performance in Mutant Allele Detection
Detection of JAK2V617F Mutation in Myeloproliferative Neoplasms
A 2025 study optimized a laboratory-developed droplet digital PCR (ddPCR) assay for the JAK2V617F mutation, a critical biomarker for MPNs [29].
- Methodology: The assay was optimized by fine-tuning five key parameters: primer/probe sequences and concentrations, annealing temperature, template amount, and PCR cycles [29].
- Key Finding on LoQ: The optimized ddPCR assay demonstrated an exceptional limit of quantification (LoQ) of 0.01% variant allele frequency (VAF). This means it could reliably quantify the mutant allele even when it constituted just 0.01% of the total DNA background, a level of sensitivity crucial for early detection and monitoring minimal residual disease [29].
Circulating Tumor DNA (ctDNA) Detection in Rectal Cancer
A 2025 comparative study directly pitted ddPCR against Next-Generation Sequencing (NGS) for detecting ctDNA in non-metastatic rectal cancer [31].
- Methodology: Pre-therapy plasma and tumor samples were collected from 41 patients. Mutations were identified in tumor tissue via NGS, and ctDNA detection in plasma was performed using both ddPCR and an NGS panel [31].
- Key Finding on Sensitivity: In the development group, ddPCR detected ctDNA in 58.5% (24/41) of baseline plasma samples, significantly outperforming the NGS panel, which detected ctDNA in only 36.6% (15/41). This highlights ddPCR's superior sensitivity for detecting low-frequency mutations in a background of wild-type DNA, a common challenge in liquid biopsy applications [31].
General Workflow Comparison for Inhibitor Tolerance
While not specific to mutant alleles, a key technical advantage of dPCR is its resilience to PCR inhibitors, which can severely impact qPCR accuracy [30].
- Principle: In qPCR, inhibitors present in the sample reduce the effective amplification efficiency, leading to higher Ct values and an underestimation of the true target concentration. In dPCR, because the sample is partitioned, the inhibitor molecules are also distributed. While some partitions may be affected, many others will amplify normally, preserving the accuracy of the absolute count derived from the ratio of positive to negative partitions [30].
Essential Research Reagent Solutions
The table below lists key materials and reagents required for implementing qPCR and dPCR workflows in a research setting.
| Item | Function in qPCR/dPCR |
|---|---|
| Primers & Probes | Target-specific oligonucleotides that define the sequence to be amplified. Fluorogenic probes (e.g., TaqMan) are essential for specific detection in both qPCR and dPCR [26]. |
| Thermostable DNA Polymerase | Enzyme that catalyzes DNA synthesis. Hot-start enzymes are preferred to prevent non-specific amplification during reaction setup [32] [33]. |
| dNTP Mix | Deoxynucleoside triphosphates (dATP, dCTP, dGTP, dTTP); the building blocks for new DNA strands [32]. |
| Reaction Buffer | Provides optimal chemical environment (pH, salts) for polymerase activity. MgCl₂ concentration is a critical component [33]. |
| dPCR Partitioning Oil/Chips | For ddPCR, this immiscible oil creates the droplet partitions. For systems like QIAcuity, microchamber chips are used [6] [22]. |
| Nucleic Acid Isolation Kits | For purification of high-quality DNA/RNA from samples (e.g., tumor tissue, blood). Purity is especially critical for qPCR accuracy [27] [29]. |
| Standard Curve Materials | For qPCR absolute quantification, a serial dilution of a sample with known concentration (e.g., gBlocks, plasmid DNA) is essential [28]. |
The choice between relying on Ct values from qPCR or copies/μL from dPCR hinges on the specific requirements of your research on mutant alleles.
- Use qPCR/Ct when your project involves high-throughput sample screening, relative quantification (e.g., gene expression fold-changes) is sufficient, and the target is not extremely rare. Its lower cost and established workflows are key advantages [6] [30].
- Choose dPCR/copies/μL when your goal is the absolute quantification of rare mutations (e.g., in liquid biopsy), precise measurement of copy number variations, or when working with complex samples that may contain PCR inhibitors. Its superior sensitivity, precision, and lack of reliance on a standard curve make it the superior tool for these demanding applications [6] [29] [31].
For drug development and clinical research, where accurately quantifying minor mutant clones or tracking minute changes in allele frequency can be critical for patient stratification and therapy monitoring, dPCR offers a level of performance that is often unmatched by traditional qPCR.
Targeted Applications: Implementing dPCR and qPCR in Mutant Allele Workflows
The detection of rare alleles, such as somatic mutations in circulating tumor DNA (ctDNA), is a significant challenge in molecular diagnostics and oncology research. While quantitative PCR (qPCR) has been the traditional method for nucleic acid quantification, digital PCR (dPCR) offers a transformative approach through sample partitioning. This guide objectively compares the performance of dPCR and qPCR for rare mutant allele detection, supported by experimental data demonstrating dPCR's superior sensitivity, precision, and ability for absolute quantification without standard curves. We detail specific methodologies that leverage dPCR's partitioning advantage to achieve detection sensitivities as low as 0.001% mutant allele frequency, enabling applications in liquid biopsy, cancer monitoring, and pathogen detection.
Accurate detection of low-abundance nucleic acid targets is crucial across biomedical research and clinical diagnostics. In oncology, for example, rare mutant alleles can indicate early cancer development, minimal residual disease, or emerging therapy-resistant subclones [22] [34]. These targets often appear at frequencies below 0.1% amidst a background of wild-type sequences, presenting a formidable detection challenge [35].
Traditional qPCR quantifies nucleic acids by measuring amplification fluorescence in real-time, with target concentration determined by the cycle threshold (Ct) relative to standard curves. While excellent for higher abundance targets, qPCR encounters sensitivity limitations at very low target concentrations due to background noise and amplification efficiency variations [36] [16].
Digital PCR addresses these limitations through a fundamental methodological shift: partitioning the sample into thousands of nanoscale reactions. This allows individual mutant molecules to be detected against the wild-type background, providing absolute quantification and dramatically enhancing sensitivity for rare allele detection [36] [22].
Technological Comparison: Partitioning as a Key Differentiator
Fundamental Working Principles
Quantitative PCR (qPCR) amplifies DNA in a bulk reaction, monitoring fluorescence accumulation during cycling. The cycle threshold (Ct) at which fluorescence crosses a background level correlates with initial DNA concentration, requiring standard curves for quantification [36] [16]. This approach works well for abundant targets but struggles with rare variants where signal differences are minimal.
Digital PCR (dPCR) incorporates a crucial partitioning step before amplification. The reaction mixture is divided into numerous individual partitions—either droplets or microchambers—so that each contains zero, one, or a few target molecules. Following end-point PCR amplification, partitions are scored as positive or negative based on fluorescence. The absolute target concentration is calculated using Poisson statistics based on the ratio of positive to negative partitions, eliminating the need for standard curves [22] [18].
Direct Performance Comparison
The partitioning methodology of dPCR provides distinct advantages for rare allele detection, as summarized in the performance comparison below.
Table 1: Performance comparison between qPCR and dPCR for rare allele detection
| Feature | qPCR (Quantitative PCR) | dPCR (Digital PCR) |
|---|---|---|
| Quantification Type | Relative (requires standard curve) | Absolute (no standard curve needed) |
| Sensitivity | High, but limited by background noise | Ultra-high, ideal for low-abundance targets |
| Precision & Reproducibility | Good, affected by PCR efficiency variations | Excellent, due to absolute quantification |
| Dynamic Range | 7–10 logs | 5 logs |
| Error Susceptibility | More variation due to amplification efficiency | Low error rate, robust for complex samples |
| Ideal Application | Gene expression, high-throughput pathogen detection | Rare mutation detection, copy number variation, liquid biopsy |
Partitioning enables dPCR's superior performance by effectively enriching mutant signals. When a sample containing rare mutants is partitioned, reactions containing mutant molecules become concentrated sources of mutant DNA after amplification, while the vast majority containing only wild-type sequences remain distinct. This physical separation prevents amplification competition and background interference that plagues bulk reactions in qPCR [37] [35].
Experimental Evidence: Quantifying dPCR Sensitivity
Sensitivity Limits for Cancer Mutations
Multiple studies have rigorously quantified dPCR's detection limits for clinically relevant mutations. In one comprehensive evaluation of EGFR mutations, dPCR demonstrated exceptional sensitivity with a false-positive rate of just 1 in 14 million molecules. The lower limit of detection (LoD) reached 1 mutant in 180,000 wild-type molecules (0.00056%) when analyzing 3.3 μg of genomic DNA. When processing larger DNA quantities (70 million copies), detection sensitivity reached an remarkable 1 mutant in over 4 million wild-type molecules [35].
Table 2: Experimentally determined detection limits for dPCR assays
| Target Mutation | Application Context | Lower Limit of Detection (LoD) | Reference |
|---|---|---|---|
| EGFR L858R | Non-small cell lung cancer | 1 in 180,000 (0.00056%) to 1 in 4,000,000 | [35] |
| EGFR T790M | Drug resistance in lung cancer | 1 in 13,000 (0.0077%) | [35] |
| Multiple TP53 mutations | Tumor suppressor gene scanning | 0.2% to 1.2% mutation abundance | [37] |
| COLD-ddPCR | Multiple mutation scanning | 0.2% to 1.2% mutation abundance | [37] |
Enhanced Mutation Scanning with COLD-ddPCR
Researchers have combined dPCR with COnvection and Liquid Denaturation PCR (COLD-PCR) to further enhance mutation detection. This hybrid approach enables scanning for unknown mutations within approximately 50-base pair regions of target amplicons. The method uses two differently colored hydrolysis probes (FAM/HEX) both matching the wild-type sequence. The ratio of FAM/HEX-positive droplets remains constant with wild-type templates but deviates when mutations occur under either probe binding site. COLD-PCR cycling conditions enrich mutation-containing sequences, enhancing the ratio change to achieve detection sensitivities between 0.2% to 1.2% mutation abundance for TP53 and EGFR mutations in cell-free DNA [37].
Experimental Protocols: Implementing dPCR for Rare Allele Detection
Core dPCR Workflow Methodology
The fundamental dPCR workflow consists of four key steps, with the partitioning step being crucial for rare allele enrichment:
- Sample Partitioning: The PCR reaction mixture containing the sample DNA is partitioned into thousands of nanoliter-sized droplets or microchambers, randomly distributing target molecules according to Poisson distribution.
- Endpoint PCR Amplification: Thermal cycling amplifies target sequences within each partition until completion, without real-time monitoring.
- Fluorescence Detection: Each partition is analyzed for fluorescence signals using specific probes (e.g., FAM, HEX) to determine positive/negative status.
- Absolute Quantification: The fraction of positive partitions is used with Poisson statistics to calculate the absolute concentration of target molecules in the original sample [22] [18].
COLD-Digital PCR Protocol for Mutation Scanning
This advanced protocol combines COLD-PCR with dPCR to detect multiple unknown mutations within a target region:
- Primer and Probe Design: Design two hydrolysis probes (FAM and HEX-labeled) complementary to different segments of the wild-type target sequence within a 50-100 bp region.
- Pre-amplification (Optional): Perform target-specific pre-amplification when analyzing limited samples like cell-free DNA (20 cycles for genomic DNA, 30 cycles for cfDNA) [37].
- Partitioning and COLD-PCR Amplification:
- Partition the sample using droplet or microchamber dPCR systems.
- Implement COLD-PCR cycling conditions: Denature at lower critical temperature (Tc) to preferentially denature and amplify heteroduplex DNA containing mutations, thereby enriching mutation-containing sequences [37].
- Endpoint Fluorescence Detection: Measure fluorescence in both FAM and HEX channels for each partition.
- Ratio Analysis and Mutation Calling:
- Calculate the FAM/HEX fluorescence ratio for each partition.
- Partitions with wild-type sequences will maintain a consistent FAM/HEX ratio.
- Partitions containing mutations under either probe binding site will show deviant ratios.
- Statistical analysis of ratio distributions identifies samples containing mutant alleles [37].
Essential Research Reagent Solutions
Successful implementation of dPCR for rare allele detection requires specific reagents and systems. The following table details key components and their functions in the experimental workflow.
Table 3: Essential research reagents and systems for dPCR-based rare allele detection
| Reagent/System | Function in Rare Allele Detection | Implementation Example |
|---|---|---|
| Partitioning Systems | Creates thousands of individual reactions for single-molecule detection | Droplet generators (Bio-Rad QX200), nanoplate systems (QIAGEN QIAcuity) [18] |
| Hydrolysis Probes | Target-specific detection with fluorescent reporters (FAM, HEX) | TaqMan probes wild-type and mutant-specific [35] |
| Digital PCR Master Mix | Optimized enzyme and buffer system for partitioned amplification | Contains DNA polymerase, dNTPs, MgCl₂, and stabilizers [35] |
| Reference Standard Sets | Controls for assay validation and sensitivity determination | EGFR Multiplex cfDNA standards with known mutation frequencies [34] |
| Bisulfite Conversion Kits | DNA treatment for methylation-specific detection | EZ DNA Methylation-Lightning Kit for methylation marker analysis [38] |
Comparative Applications in Clinical Research
Liquid Biopsy and Cancer Monitoring
dPCR's partitioning advantage makes it particularly suited for liquid biopsy applications where ctDNA is extremely scarce. Studies have validated methylation-specific ddPCR assays for lung cancer detection, demonstrating ctDNA-positive rates of 38.7-46.8% in non-metastatic disease and 70.2-83.0% in metastatic cases. The method enabled monitoring of treatment response through longitudinal ctDNA quantification [38].
Alternative Technologies for Rare Variant Detection
While dPCR offers exceptional performance for targeted detection, alternative technologies exist for different application needs:
Next-Generation Sequencing with Molecular Barcodes: This approach tags individual DNA molecules with unique barcodes before amplification and deep sequencing. It enables detection of variants at 0.17% allele frequency while covering multiple genomic regions simultaneously, making it suitable for unknown mutation discovery across larger target areas [34].
BEAMing Technology: Combines emulsion PCR with magnetic beads and flow cytometry to detect rare mutations down to 0.1% variant allele frequency, demonstrating similar sensitivity to dPCR for known mutations [22] [34].
Digital PCR's partitioning methodology provides a fundamental advantage for rare allele detection by physically separating target molecules and enabling absolute quantification at the single-molecule level. Experimental data consistently demonstrates dPCR's ability to detect mutant alleles at frequencies as low as 0.001%, outperforming qPCR particularly for challenging applications like liquid biopsy, rare mutation detection, and analysis of heterogenous samples. While qPCR remains suitable for high-throughput quantification of more abundant targets, dPCR has established itself as the superior technology for detecting low-abundance mutations critical for cancer research, non-invasive prenatal testing, and pathogen detection.
Quantitative PCR (qPCR) remains a cornerstone technology for gene expression analysis and validation of disease biomarkers, particularly when dealing with known targets. For researchers validating a defined genetic signature, the choice of high-throughput platform is critical, balancing factors such as sensitivity, reproducibility, and practical workflow efficiency. This guide objectively compares the performance of established qPCR platforms, focusing on their application in screening workflows. Within the broader context of digital PCR (dPCR) versus quantitative PCR for detecting mutant alleles, understanding these qPCR capabilities is fundamental for selecting the appropriate technology. While dPCR offers superior sensitivity for low-abundance mutations [10], qPCR platforms provide robust, cost-effective solutions for high-throughput expression profiling of known transcripts, making them indispensable for large-scale screening studies and biomarker validation pipelines.
Platform Comparison: Throughput, Sensitivity, and Practical Workflow
Several advanced qPCR platforms have been developed to meet the demands of large-scale studies, each with distinct technical specifications and operational workflows.
Table 1: Comparison of High-Throughput qPCR Platforms for miRNA Validation
| Platform | Reaction Volume | Throughput | Median CV (Precision) | Sensitivity for Low Copy Numbers | Key Applications |
|---|---|---|---|---|---|
| Standard 96-Well (ViiA7) | 5 μl | 96 wells/run | 0.6% (Range: 0.1-1.9%) | High | Gold standard for sensitivity; low-variability replicates [39] |
| TaqMan Low Density Array (TLDA) | 1 μl | 384 assays/card | 8.3% (Range: 0.3-19.1%) | Moderate | Fixed-panel biomarker validation [39] |
| OpenArray (OA) | 33 nl | 3,072 assays/array | 2.1% (Range: 0.7-4.6%) | High (inverse to volume) | Ultra-high-throughput gene expression [39] |
| Dynamic Array (DA) | 15 nl | 9,216 reactions/chip | 9.5% (Range: 2.2-27.6%) | Variable (platform-dependent) | High-flexibility, custom panel screening [39] |
The data reveal a critical trade-off: platforms with smaller reaction volumes (OpenArray, Dynamic Array) enable massive parallelism but can exhibit higher technical variability, especially for low-abundance targets [39]. The 96-well platform, while lower in throughput, sets the "gold standard" for precision, with a median coefficient of variation (CV) of just 0.6% [39]. CV is a key metric for precision, calculated as the standard deviation divided by the mean quantity of replicates, with lower percentages indicating more consistent results [40].
Performance Metrics: Reproducibility and Detection Fidelity
Beyond basic specifications, performance in detecting real-world biomarker signatures varies significantly across platforms.
Table 2: Performance Metrics in Signature Detection
| Performance Metric | 96-Well (ViiA7) | OpenArray (OA) | Dynamic Array (DA) | Implication for Screening |
|---|---|---|---|---|
| Fidelity (<1 CT difference) | 99.23% | 88.1% | 77.78% | High fidelity reduces false positives/negatives [39] |
| Fidelity (<2 CT difference) | 99.23% | 96.29% | 91.27% | Critical for reliable fold-change calculations [39] |
| Reproducibility (Run-to-Run) | Highest | Moderate (up to 2.06 CT variation) | Lower (up to 8.17 CT variation) | Impacts longitudinal study reliability [39] |
| Detection of miRNA Signature | Accurate profile | Accurate profile | Skewed profile | Platform choice affects biological conclusions [39] |
The 96-well platform maintained CT variation of less than 1 cycle until the target transcript was expressed at very low levels (CT >30.01), whereas the high-throughput platforms showed substantially increased replicate variability for moderate and low-expression transcripts [39]. This has direct implications for detecting small fold-changes, as excessive variability can reduce a statistical test's ability to discriminate meaningful biological differences [40].
Experimental Protocols for Platform Evaluation and miRNA Signature Validation
Systematic Comparison of qPCR Platforms
The comparative data presented in this guide were derived from a systematic study designed to evaluate platform performance in a real-world research scenario [39].
1. Sample Preparation:
- Source: RNA was extracted from both human islet cells and human plasma/serum to represent cellular and circulating miRNA analysis.
- Target Selection: An unbiased small RNA sequencing approach was first used on plasma samples from diabetic individuals with and without retinopathy (DR vs. NDR) to identify a candidate miRNA signature.
2. cDNA Synthesis and Pre-amplification:
- cDNA was synthesized from the RNA samples.
- Pre-amplification was performed with platform-specific protocols:
- OpenArray: 14 cycles of pre-amplification followed by a 1:40 dilution.
- Dynamic Array: 14 cycles of pre-amplification followed by a 1:10 dilution. This lower dilution factor contributes to the overall lower CT values observed on the DA platform [39].
3. qPCR Execution:
- The same cDNA samples were run on four platforms: ViiA7 (96-well), TLDA, OpenArray, and Dynamic Array.
- Experiments were performed in multiple replicates and were repeated by two different users to assess inter-user reproducibility.
- Raw CT values were collected using each manufacturer's software with default parameters.
4. Data Analysis:
- Variability Analysis: The coefficient of variation (CV) was calculated for each miRNA assay across replicates.
- Fidelity Scoring: The percentage of replicates differing by less than 1, 2, or 3 CT values was computed.
- Reproducibility Assessment: The average difference between two independent runs was plotted.
- Signature Detection: A five-miRNA signature identified by sequencing was assessed for its detection profile across the four qPCR platforms [39].
Protocol for High-Throughput Multiplexing with 2D Labeling
For applications requiring mid-level multiplexing (10-50-plex) on standard qPCR instruments, a combinatorial approach using fluorescence color and melting temperature (Tm) as a virtual 2D label has been developed [41].
Workflow for 2D Multiplex qPCR Assay
1. Library Construction (2D Label Setup):
- Combine multiple fluorophores (e.g., FAM, HEX, ROX, CAL Fluor Red 635, Quasar 705) with a series of oligonucleotide "Tm tags" [41].
- Design each Tm tag to hybridize to a universal fluorogenic probe with a predicated Tm value ranging from 40°C to 80°C in 1°C–5°C intervals. This creates a library of unique 2D labels (e.g., 5 colors × 10 Tm = 50 unique labels) [41].
2. Target-Specific Ligation:
- For each target (e.g., HPV genotype or SNP), design a pair of ligation oligonucleotides.
- One oligonucleotide in the pair harbors one of the unique artificial Tm tag sequences.
- In a 10 μl reaction containing sample DNA, hybridize and ligate the oligonucleotides using a thermostable DNA ligase (e.g., Taq DNA ligase) with a thermal cycling protocol tailored for multiple targets [41].
3. Universal PCR with Melting Curve Analysis:
- Amplify all ligated products in a single tube using a single universal primer pair.
- Include all relevant fluorogenic probes in the PCR reaction mix.
- Perform real-time PCR followed by a high-resolution melting curve analysis, raising the temperature from 40°C to 85°C at 1°C increments [41].
4. Data Interpretation:
- Identify each target by its unique combination of fluorescence color (detection channel) and Tm value (peak position in the melting curve) [41].
- This method has been validated for genotyping 15 high-risk human papillomaviruses in a single 16-plex reaction and for 48-plex SNP genotyping [41].
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of high-throughput qPCR workflows depends on careful selection of reagents and materials.
Table 3: Essential Research Reagent Solutions for High-Throughput qPCR
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Fluorogenic Probes (TaqMan-style) | Sequence-specific detection of amplified targets. | Use dark quenchers (e.g., Iowa Black FQ) and double-quenched probes to minimize background in multiplex reactions [42]. |
| HEX (Hexachlorofluorescein) | Fluorescent reporter dye for multiplexing. | Excitation/emission: 533/549 nm. Compatible with FAM, ROX in multiplex assays; check instrument calibration [43] [42]. |
| Passive Reference Dye (e.g., ROX) | Normalizes for pipetting volume variations and optical anomalies. | Included in the reaction mix at a fixed concentration; essential for improving precision [40]. |
| Taq DNA Ligase | Enzymatically joins sequence-specific oligonucleotides. | Critical for ligation-based multiplex assays (e.g., 2D labeling workflow) [41]. |
| Pre-amplification Master Mix | Pre-amplifies cDNA for low-input or high-throughput applications. | Platform-specific cycles and dilution factors are required (e.g., 1:10 for DA vs. 1:40 for OA) [39]. |
Strategic Implementation and Analysis
To ensure data quality, researchers should adhere to several key practices. Precision Optimization: System variation can be minimized through good pipetting technique, instrument maintenance, using a passive reference dye, and avoiding optical mixing by ensuring sample volume does not exceed 20% of the PCR reaction volume [40]. Replicate Strategy: Employ both technical replicates (repetitions of the same sample) to estimate system precision and biological replicates (different samples from the same group) to account for true biological variation. The number of replicates is a balance between cost, throughput, and the required statistical power [40]. Data Analysis: Use the correct statistical approaches. For comparisons between groups, statistical tests (e.g., t-test) determine if an observed fold change is significant. Reducing variation through careful experimentation allows these tests to discriminate smaller, more biologically relevant fold changes [40].
Technology Selection Workflow
The selection of a qPCR platform for high-throughput gene expression and screening is a strategic decision that directly impacts data quality and biological interpretation. For the validation of known miRNA or gene expression signatures, the standard 96-well platform offers unmatched precision, while ultra-high-throughput systems like OpenArray provide a compelling balance of throughput and data quality for large-scale studies. The development of advanced multiplexing techniques, such as 2D labeling, further extends the capabilities of standard qPCR instruments. When positioned within the broader thesis of dPCR versus qPCR, it is clear that while dPCR excels in absolute quantification and ultrasensitive detection of rare alleles, high-throughput qPCR remains the superior tool for the rapid, cost-effective profiling of known targets across vast sample sets. The optimal choice is thus not a question of which technology is universally better, but which is precisely suited to the specific biological question and experimental constraints at hand.
The molecular analysis of circulating tumor DNA (ctDNA) present in a patient's bloodstream, a practice known as liquid biopsy, represents a transformative approach in oncology. This non-invasive technique provides a dynamic snapshot of the tumor's genetic landscape, enabling applications in early cancer detection, treatment selection, and monitoring of therapy response and resistance. A significant challenge in this field is the reliable detection of rare mutant DNA molecules, which can be present at exceedingly low frequencies amidst a high background of wild-type DNA. While quantitative PCR (qPCR) has been a workhorse for nucleic acid analysis, its limitations in sensitivity and absolute quantification can hinder its effectiveness for liquid biopsy.
Digital PCR (dPCR) has emerged as a powerful alternative, redefining the limits of detection for rare mutant alleles. This case study will objectively compare the performance of dPCR against qPCR for detecting tumor DNA in circulation. We will delve into experimental data that highlights the superior analytical performance of dPCR, provide a detailed protocol for a representative experiment detecting cancer-associated mutations, and situate these findings within the broader thesis that dPCR offers unparalleled advantages for precise, sensitive, and absolute quantification of ctDNA.
Performance Comparison: dPCR vs. qPCR
The fundamental difference between the two technologies lies in their approach to quantification. qPCR relies on measuring amplification in a bulk reaction and comparing results to a standard curve, providing a relative quantification. In contrast, dPCR partitions a sample into thousands of individual reactions, counts the positive and negative endpoints, and uses Poisson statistics to calculate an absolute quantification without the need for a standard curve [44] [10] [45]. This partitioning confers key advantages in sensitivity, precision, and tolerance to inhibitors.
The following tables summarize key performance metrics from recent studies, illustrating the distinct strengths of dPCR in molecular diagnostics.
Table 1: Overall Technical Comparison of dPCR and qPCR
| Feature | Digital PCR (dPCR) | Quantitative PCR (qPCR) |
|---|---|---|
| Quantification Method | Absolute, without standard curves [10] [45] | Relative, requires standard curve [44] [10] |
| Principle | End-point detection of partitioned reactions [44] [22] | Real-time detection of bulk reaction [44] [45] |
| Precision & Reproducibility | High precision, superior for fractional abundance analysis [10] [23] | Well-established protocols, but lower precision for rare targets [10] |
| Sensitivity for Rare Mutations | Detects mutation rates ≥ 0.1% (high signal-to-noise) [10] [35] | Typically detects mutation rates > 1% [10] |
| Tolerance to PCR Inhibitors | High, due to partitioning [10] [46] | Lower, inhibitors affect amplification efficiency [10] |
| Best Suited Applications | Liquid biopsy, rare mutation detection, copy number variation, viral load monitoring [10] [22] | Gene expression analysis, pathogen detection (high viral load), microbiome analysis [10] |
Table 2: Comparative Experimental Data from Recent Studies
| Study Context | Key Performance Metric | Digital PCR Performance | qPCR Performance |
|---|---|---|---|
| Respiratory Virus Detection (2024) [6] | Accuracy (Viral Load Quantification) | Superior accuracy for high viral loads (Influenza A/B, SARS-CoV-2) and medium loads (RSV) | Lower accuracy compared to dPCR |
| Periodontal Pathobiont Detection (2025) [23] | Intra-assay Variability (Precision) | Median CV%: 4.5% | Higher than dPCR (p=0.020) |
| Periodontal Pathobiont Detection (2025) [23] | Sensitivity (Detection of Low Loads) | Superior sensitivity; identified qPCR false negatives at low concentrations (< 3 log10 Geq/mL) | Underestimated prevalence of A. actinomycetemcomitans by 5-fold |
| EGFR Mutation Detection (2014) [35] | Limit of Detection (LoD) | L858R: 1 mutant in 180,000 wild-type (in 3.3 μg DNA) [35] | Not comparable for rare alleles |
| Wastewater SARS-CoV-2 Surveillance (2023) [46] | Sensitivity in Complex Matrices | Highly sensitive, robust | Highly sensitive, but slightly more variable |
Experimental Protocol: Detecting EGFR Mutations via dPCR
To illustrate a real-world application, we detail a landmark dPCR experiment for detecting cancer-associated mutations in the epidermal growth factor receptor (EGFR) gene, a key biomarker in non-small cell lung cancer [35]. The following diagram outlines the core workflow of a droplet-based dPCR assay.
Materials and Reagents
Table 3: Key Research Reagent Solutions for dPCR Assay
| Item | Function/Description | Example/Details |
|---|---|---|
| dPCR System | Instrument for partitioning, thermocycling, and imaging. | RainDance RainDrop System [35]; QIAcuity nanoplate system (Qiagen) [6] [23] |
| PCR Master Mix | Provides enzymes, dNTPs, and optimized buffer for amplification. | TaqMan Genotyping Master Mix [35]; QIAcuity Probe PCR Kit [23] |
| Primers & Probes | Target-specific oligonucleotides for amplification and detection. | Hydrolysis probes (e.g., TaqMan) labeled with FAM/VIC; specific for mutant and wild-type alleles [35] |
| DNA Template | Sample containing the nucleic acids to be analyzed. | Genomic DNA from patient plasma (ctDNA) or tumor tissue; can include synthetic controls [35] |
| Restriction Enzyme | Optional, used to digest genomic DNA and improve access to target sequences. | HaeIII or EcoRI; choice can impact precision [18] |
| Droplet Stabilizer | For ddPCR, ensures droplet integrity during thermocycling. | Included in specific ddPCR kits [35] |
Step-by-Step Procedure
- Assay Design: Design and validate primer and probe sets specific for the mutant (e.g., EGFR L858R) and wild-type alleles. Hydrolysis probes for different alleles are typically labeled with distinct fluorophores (e.g., FAM for mutant, VIC for wild-type) [35].
- Sample and Reaction Preparation: Extract DNA from patient plasma (ctDNA) or other samples. Prepare the dPCR reaction mix containing master mix, primers, probes, and the DNA template. In the referenced study, a 50 μL reaction volume contained approximately 3.3 μg of genomic DNA [35].
- Partitioning: Load the reaction mixture into the dPCR instrument. The system will automatically partition each sample into thousands of individual reactions—either as droplets in droplet digital PCR (ddPCR) or in nanowells in nanoplate-based dPCR [22] [35]. For example, the QIAcuity system creates ~26,000 partitions per well [6] [23].
- Endpoint PCR Amplification: Perform PCR on the partitioned sample using a standard thermocycling protocol. The reaction runs to completion (end-point), and partitions containing the target sequence amplify and generate a fluorescent signal [45] [35].
- Fluorescence Reading and Analysis: After cycling, the instrument reads the fluorescence in each partition. Partitions are classified as positive (for mutant, wild-type, or both) or negative. Software (e.g., QIAcuity Suite) then applies Poisson statistics to the count of positive and negative partitions to calculate the absolute concentration of the target molecule in the original sample, expressed as copies per microliter [6] [35].
Discussion and Future Perspectives
The experimental data and protocol clearly demonstrate that dPCR outperforms qPCR in key metrics essential for liquid biopsy, particularly sensitivity, precision, and absolute quantification. The ability of dPCR to detect a single mutant molecule among hundreds of thousands of wild-type molecules [35] is a game-changer for detecting minimal residual disease or emerging therapy-resistant clones long before they become clinically apparent through imaging or symptoms. Furthermore, its higher tolerance to PCR inhibitors makes it exceptionally robust for analyzing ctDNA from blood-based samples, which can contain various substances that interfere with traditional PCR [10] [46].
While qPCR remains a valuable, cost-effective tool for applications where high sensitivity for rare alleles is not required, the evidence strongly supports the adoption of dPCR for advanced oncological research and clinical diagnostics focused on ctDNA analysis. The future of dPCR in clinics is bright, with ongoing developments aimed at increasing throughput, reducing costs, and standardizing protocols. As the technology continues to evolve, its integration into routine patient management promises to usher in an era of more personalized, precise, and proactive cancer care [22].
Copy Number Variations (CNVs), defined as gains or losses of DNA segments larger than 50 base pairs, represent a major source of genetic diversity and are critically implicated in a wide range of diseases, including cancer and hereditary disorders [47] [48]. The accurate detection and precise quantification of these variations are paramount for both basic research and clinical diagnostics. In the context of detecting mutant alleles, the choice of analytical platform is crucial, as it directly impacts the sensitivity, specificity, and reliability of the results. While quantitative PCR (qPCR) has been a longstanding workhorse for gene quantification, digital PCR (dPCR) has emerged as a powerful third-generation technology that enables absolute quantification of nucleic acids without the need for standard curves [16]. This guide provides an objective, data-driven comparison of the precision and performance of current CNV analysis platforms, with a particular focus on their application in digital versus quantitative PCR workflows, to inform researchers and drug development professionals in selecting the optimal tool for their specific needs.
Platform Comparison: Methodologies and Performance Metrics
A variety of platforms are available for CNV analysis, each with distinct underlying technologies and performance characteristics. The following table summarizes the primary technologies and their key attributes.
Table 1: Key Platforms and Technologies for CNV Analysis
| Platform Category | Examples | Key Technology/Method | Primary Use Case |
|---|---|---|---|
| Digital PCR (dPCR) | QIAcuity One (Nanoplate-based), QX200/QX600 (Droplet-based) [18] | Partitioning of sample into thousands of individual reactions for absolute quantification [16] | Absolute quantification, rare allele detection, quality control in manufacturing [49] |
| Quantitative PCR (qPCR) | Standard real-time PCR systems | Relative quantification based on standard curves and cycle threshold (Ct) values [16] | High-throughput screening, gene expression analysis where absolute copy number is not critical |
| Next-Generation Sequencing (NGS) | CNVkit, Control-FREEC, Delly [50] | Read-depth, split-read, read-pair, and assembly methods [51] | Genome-wide discovery of CNVs and other structural variants |
| Microarray | CytoScan HD, SNP arrays [47] | Hybridization to genome-wide probes | Clinical cytogenetics, detection of large CNVs and aneuploidy |
Digital PCR vs. Quantitative PCR: A Direct Comparison of Precision
Direct comparisons between dPCR and qPCR reveal fundamental differences in their precision and accuracy, especially for CNV analysis. A 2025 study focusing on the multiallelic DEFA1A3 gene, whose copy number ranges from 2 to 16 per genome, provided a rigorous benchmark. The study compared Droplet Digital PCR (ddPCR) and qPCR against Pulsed-Field Gel Electrophoresis (PFGE), considered a gold standard for CNV enumeration. The results demonstrated a stark contrast in performance: ddPCR showed 95% concordance with PFGE, with a strong Spearman correlation of r=0.90. In contrast, qPCR results were only 60% concordant with a moderate correlation of r=0.57. The precision of qPCR was notably poorer at higher copy numbers, with its results differing from PFGE by an average of 22%, compared to just 5% for ddPCR [48]. This establishes dPCR as a superior method for applications requiring high precision in absolute copy number determination.
Comparing dPCR Platforms: Nanoplate vs. Droplet-Based Systems
Within dPCR technologies, different partitioning methods exist. A 2025 study directly compared the QX200 droplet-based system (ddPCR) from Bio-Rad with the QIAcuity One nanoplate-based system (ndPCR) from QIAGEN. Using synthetic oligonucleotides and DNA from the ciliate Paramecium tetraurelia, the study found that both platforms exhibited similar limits of detection (LOD) and quantification (LOQ) and high precision across most analyses [18].
Table 2: Performance Metrics of dPCR Platforms [18]
| Performance Metric | QIAcuity One (ndPCR) | QX200 (ddPCR) |
|---|---|---|
| Limit of Detection (LOD) | ~0.39 copies/µL input | ~0.17 copies/µL input |
| Limit of Quantification (LOQ) | 1.35 copies/µL input | 4.26 copies/µL input |
| Precision (Coefficient of Variation) | 7-11% (across dilution series) | 6-13% (across dilution series) |
| Key Finding | Less affected by choice of restriction enzyme | Precision significantly improved using HaeIII over EcoRI |
From an operational standpoint, chip- or nanoplate-based dPCR systems offer a streamlined "sample-in, results-out" process that is highly suited for quality control (QC) environments. This integrated workflow reduces hands-on time and minimizes the risk of human error and contamination compared to droplet-based systems, which often involve multiple instruments and steps taking 6-8 hours [49].
Next-Generation Sequencing and Microarray Platforms
For genome-wide CNV discovery, NGS and microarrays are the dominant technologies. A comprehensive 2025 benchmarking study of 12 NGS-based CNV detection tools evaluated their performance across different variant lengths, sequencing depths, and tumor purities. The study found that tool performance varies significantly based on these factors, with no single method being optimal for all scenarios. For instance, tools like CNVkit and Control-FREEC (read-depth based) are generally robust, but their ability to detect CNVs is influenced by sequencing depth and the size of the variation [50].
Microarray technology remains a first-line test in clinical cytogenetics. A 2025 comparative study of medium-coverage genome sequencing (GS) and SNP array found 100% concordance between the two methods for identifying clinically relevant CNVs. However, GS demonstrated better precision in defining CNV breakpoints and a lower false-positive rate [52]. Similarly, another study noted that while nanopore sequencing could detect CNVs with advantages over microarray, such as identifying inversions, its variant calling algorithms still require improvement for maximum robustness [47].
Experimental Protocols for Platform Assessment
To ensure reliable and reproducible CNV data, rigorous experimental protocols must be followed. The methodologies below are derived from the cited comparative studies.
Protocol: Assessing dPCR Performance for CNV Quantification
This protocol is adapted from studies comparing dPCR platforms and validating ddPCR against PFGE [18] [48].
Sample Preparation:
- DNA Extraction: Use high-quality genomic DNA, quantified using a fluorometer. Assess purity via spectrophotometry (A260/A280 ratio ~1.8-2.0).
- Restriction Digestion: Digest 1-10 µg of genomic DNA with a suitable restriction enzyme (e.g., HaeIII or EcoRI) to fragment the DNA and improve access to the target locus. Incubate for 15-30 minutes at the enzyme's optimal temperature, followed by enzyme inactivation.
- Dilution: Serially dilute the digested DNA in nuclease-free water or TE buffer to a concentration suitable for the dPCR reaction (typically 1-100 ng/µL).
dPCR Assay Setup:
- Reaction Mix: Prepare a master mix containing dPCR supermix, fluorescently labeled target assay (FAM-labeled) for the CNV of interest, and fluorescently labeled reference assay (HEX/VIC-labeled) for a diploid control gene.
- Partitioning: Load the reaction mix onto the chosen dPCR platform.
- PCR Amplification: Transfer the plate or droplets to a thermal cycler and run endpoint PCR with optimized cycling conditions.
Data Acquisition and Analysis:
- Fluorescence Reading: After PCR, analyze each partition using a droplet reader (ddPCR) or plate imager (ndPCR) to classify it as positive or negative for the target and reference signals.
- Concentration Calculation: The instrument's software will apply Poisson statistics to calculate the absolute copy concentration (in copies/µL) of both the target and reference from the fraction of positive partitions.
- CNV Determination: Calculate the copy number of the target locus per diploid genome using the formula:
CN = (Target concentration / Reference concentration) × 2.
Protocol: Benchmarking scRNA-seq CNV Callers
This protocol is based on a large-scale benchmarking study of computational tools that infer CNVs from single-cell RNA sequencing data [53].
Data Preparation:
- Dataset Selection: Obtain scRNA-seq datasets with orthogonal ground truth CNV data (e.g., from matched single-cell or bulk whole-genome sequencing).
- Data Preprocessing: Process raw sequencing data through a standard scRNA-seq pipeline (e.g., Cell Ranger) to obtain a count matrix.
- Cell Annotation: Manually annotate cell types (e.g., tumor vs. normal) using marker genes and clustering algorithms. These annotations are used to define reference "normal" cells for the CNV callers.
CNV Calling Execution:
- Tool Selection and Execution: Run the selected CNV callers (e.g., InferCNV, CaSpER, CopyKAT) on the scRNA-seq data according to their respective tutorials and default parameters. Provide each tool with the same set of reference normal cells.
- Output Generation: Collect the outputs, which may include per-cell or per-subclone CNV profiles, either as discrete calls or continuous expression scores.
Performance Evaluation:
- Pseudobulk Creation: For cell line mixtures or tumor samples, combine per-cell results to create an average "pseudobulk" CNV profile for comparison with bulk WGS/WES ground truth.
- Metric Calculation:
- Correlation: Calculate correlation coefficients between the pseudobulk profile and the ground truth.
- AUC/Partial AUC: Evaluate the ability to classify genomic regions as gains or losses using Area Under the Curve (AUC) metrics.
- F1 Score: Determine optimal thresholds for gain/loss calling and calculate the multi-class F1 score to assess sensitivity and specificity [53].
Visualizing Workflows and Relationships
The following diagrams illustrate the core workflows for dPCR analysis and the logical relationships in the benchmarking of CNV detection methods.
Digital PCR Workflow for CNV Analysis
CNV Method Benchmarking Logic
The Scientist's Toolkit: Essential Reagents and Materials
Successful CNV analysis requires a suite of reliable reagents and materials. The following table details key solutions used in the experiments cited in this guide.
Table 3: Essential Research Reagents for CNV Analysis
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| High-Quality Genomic DNA | The source material for CNV analysis; purity and integrity are critical for accurate quantification. | Used as the starting template in all dPCR, qPCR, and NGS protocols [18] [48]. |
| Restriction Enzymes (e.g., HaeIII, EcoRI) | Fragment genomic DNA to ensure the target locus is accessible for primer/probe binding. | Used in dPCR to improve precision and accuracy of gene copy number estimation [18]. |
| dPCR Supermix | A optimized chemical mixture containing DNA polymerase, dNTPs, and buffer necessary for PCR amplification. | Forms the base of the reaction mix in all dPCR assays [18] [48]. |
| Hydrolysis (TaqMan) Probes | Sequence-specific, fluorescently labeled probes that bind to the target and reference sequences, enabling detection. | Used for specific target detection in dPCR and qPCR assays for CNV quantification [48]. |
| Nuclease-Free Water | A pure, enzyme-free solvent for diluting DNA and preparing reaction mixes to prevent nucleic acid degradation. | Used throughout experimental protocols for consistent and reproducible results. |
| Reference Locus Assay | A probe/primer set targeting a known diploid single-copy gene in the genome (e.g., RNase P, RPP30). | Serves as an internal control for normalizing target gene copy number in dPCR and qPCR [48]. |
The choice of platform for CNV analysis is highly dependent on the specific research or clinical question. For applications demanding the highest possible precision in absolute quantification of mutant alleles or copy number—such as quality control in cell and gene therapy manufacturing or studying genes with complex copy number ranges—digital PCR is the unequivocal leader. Its superiority over qPCR is clearly demonstrated in direct comparisons, with dPCR providing >95% concordance with gold-standard methods [48]. Between dPCR platforms, both droplet-based and nanoplate-based systems offer similar and excellent analytical performance [18], though nanoplate systems may provide workflow advantages in regulated environments [49]. For discovery-based research aiming to identify novel CNVs across the genome, NGS and microarray technologies remain the tools of choice, with the understanding that computational methods for NGS data continue to evolve and improve [50]. Ultimately, researchers must weigh factors such as required precision, throughput, cost, and workflow integration to select the most appropriate platform for their needs.
Multiplexing Strategies for Simultaneous Wild-Type and Mutant Allele Detection
The analysis of specific mutations in genes such as KRAS and BRAF has become a prerequisite for anti-epidermal growth factor receptor therapy in patients with metastatic colorectal cancers. KRAS mutations are associated with resistance to treatment by monoclonal antibodies such as cetuximab and panitumumab and thus are correlated with a shorter progression-free survival. BRAF mutations also play a crucial role in treatment decisions, with approximately 10% of advanced colorectal cancer tissue blocks harboring BRAF codon 600 mutations [54]. The widespread use of these targeted therapies has generated the need to develop cost-effective, multiplexed methods for routine molecular analysis that can simultaneously detect both wild-type and mutant alleles from limited clinical samples.
In modern clinical practice, detecting somatic low-abundance mutations in early cancer development requires methodologies that are discriminatory, specific, and high-throughput [55]. This technical comparison guide examines the leading multiplexing strategies for simultaneous wild-type and mutant allele detection, with particular focus on the evolving roles of quantitative PCR (qPCR) and digital PCR (dPCR) platforms. Each technology offers distinct advantages for research and clinical applications, with significant implications for drug development professionals seeking to implement robust biomarker detection protocols.
Technical Comparison of Multiplex Detection Platforms
Performance Characteristics Across Platforms
Table 1: Performance Comparison of Multiplex Detection Methods
| Method | Sensitivity (VAF) | Multiplexing Capacity | Throughput | Best Applications |
|---|---|---|---|---|
| Sanger Sequencing | ~15-20% | Low | Moderate | Research validation, high DNA quality samples |
| qPCR/HRM | 1-5% | Moderate | High | Rapid screening, cost-effective routine testing |
| Multiplex SNaPshot | 1-5% | High (up to 50 SNPs) | Moderate | Research with multiple targets, FFPE samples |
| dPCR | 0.1-0.001% | Moderate | Moderate | Liquid biopsies, rare mutation detection, absolute quantification |
| NGS | 1-5% | Very High | Variable | Comprehensive profiling, novel discovery |
VAF: Variant Allele Frequency
Key Technology Working Principles
The mitogen-activated protein kinase (MAPK) and phosphatidylinositol-3'-OH kinase (PI3K) signaling pathways form a network that participates in tumorigenesis. Activation by mutation of different adaptors of this molecular network deregulates proliferation, differentiation, and cell survival. In colorectal cancers (CRCs), the KRAS, BRAF, and PIK3CA genes are mutated in approximately 30% to 50% of cases, leading to the activation of Ras/Raf/MAPK and PI3K signaling pathways [54]. This pathway significance underscores why multiplex detection of mutations in these genes has become clinically essential.
Figure 1: KRAS/BRAF Signaling Pathway and Therapeutic Impact
Digital PCR Platforms for Multiplex Detection
Single-Color dPCR for Mutation Detection
Single-color digital PCR represents an innovative approach that detects and quantifies cancer mutations directly from circulating DNA collected from plasma of cancer patients. This method uses a double-stranded DNA intercalator dye and paired allele-specific DNA primer sets to determine an absolute count of both mutation and wild-type-bearing DNA molecules present in the sample. The cell-free DNA assay uses an input of 1 ng of nonamplified DNA (approximately 300 genome equivalents) and has a molecular limit of detection of three mutation DNA genome-equivalent molecules per assay reaction [56].
The primer design strategy for single-color dPCR involves creating mutation- or wild-type-specific reverse primers paired with a common target forward primer. For the paired-allele assay, the mutation-specific primer has a configurable extension tail that differentiates the mutation amplicons from the wild-type amplicons, producing different size amplicon products. When the droplet fluorescence data are visualized, this difference leads to the separation of fluorescent clusters composed of either mutation or wild-type amplicons [56]. This design flexibility allows efficient configuration across different cancer mutations without extensive optimization required for multi-color probe-based systems.
Figure 2: Digital PCR Workflow for Mutation Detection
dPCR Performance Characteristics
Digital PCR demonstrates exceptional sensitivity in detecting rare mutations against abundant wild-type sequences. When using more genome equivalents as input, researchers have demonstrated a sensitivity of 0.10% for detecting BRAF V600E and KRAS G12D mutations [56]. This level of sensitivity enables detection of mutant alleles in liquid biopsy specimens where circulating tumor DNA (ctDNA) is typically short and very low in concentration.
A cross-sectional study assessing the sensitivity of chip-based dPCR to detect and quantify PIK3CA mutations compared its performance with Sanger sequencing. While Sanger sequencing identified PIK3CA mutations in six patients (10.5%), dPCR confirmed those mutations and identified 19 additional patients with at least one mutation. The comparison showed a sensitivity of 100% (95% CI 53-100%) and specificity of 84.2% (95% CI 83-84.2%) for dPCR [57]. The technology's ability to detect low-rate mutations and tumor subpopulations not detected by Sanger sequencing makes it particularly valuable for clinical research applications.
Quantitative PCR Platforms for Multiplex Detection
Multiplex SNaPshot Methodology
The multiplex SNaPshot assay represents a robust technique for molecular diagnostic practices and patient selection. This method employs a primer extension-based approach that can be adapted for simultaneous analysis of up to 50 biallelic single nucleotide polymorphisms (SNPs) in a single reaction [54]. In one validation study, SNaPshot analysis detected KRAS and BRAF codon 600 mutations in 34.5% (n = 38) and 10% (n = 11) of formalin-fixed, paraffin-embedded (FFPE) tissue blocks, respectively. These results were confirmed by direct DNA sequencing and by high-resolution melting (HRM) analysis [54].
The experimental protocol for SNaPshot analysis begins with a multiplex PCR assay designed to amplify fragments of KRAS exon 2 (200 bp) and BRAF exon 15 (250 bp). Multiplex PCR is performed with the Qiagen Multiplex PCR Kit in a total volume of 25 μL containing 1× Qiagen Multiplex PCR Master Mix (providing a final concentration of 3 mmol/L MgCl2), 0.5 μmol/L of each primer, and DNA extracted from paraffin-embedded material. PCR conditions consist of: 94°C for 5 minutes, 35 cycles of 94°C for 30 seconds, 58°C for 1 minute, 72°C for 1 minute, and finally 10 minutes at 72°C [54].
High-Resolution Melting (HRM) Analysis
HRM analysis is a cost-efficient, closed-tube system without any post-PCR processing that shows greater sensitivity and specificity than Sanger sequencing for KRAS and BRAF mutation detection [54]. This method detects mutations based on the subtle differences in melting temperatures between wild-type and mutant amplicons. While HRM doesn't specifically identify the exact mutation, it serves as an effective screening tool to identify samples requiring further analysis.
The comparison of costs and time constraints among detection methods reveals that HRM and SNaPshot provide favorable profiles for routine diagnostic use. While DNA sequencing offers comprehensive mutation identification, its relatively high cost and limited sensitivity present limitations for clinical implementation [54].
Comparative Experimental Data
Direct Method Comparison Studies
Table 2: Experimental Validation Data Across Detection Platforms
| Study Reference | Method Comparison | Sensitivity | Specificity | Key Findings |
|---|---|---|---|---|
| PMC3157611 [54] | SNaPshot vs. Sequencing vs. HRM | 100% concordance | 100% concordance | SNaPshot identified all mutations confirmed by other methods |
| PMC6593258 [56] | dPCR vs. Reference Methods | 0.1% VAF | High specificity for SNVs | Detected 3 mutant molecules in 300 genome equivalents |
| ScienceDirect [57] | dPCR vs. Sanger Sequencing | 100% | 84.2% | dPCR identified 19 additional mutations missed by Sanger |
| PMC4495218 [58] | qPCR vs. ddPCR | Higher sensitivity for qPCR | Lower variability for ddPCR | ddPCR handled PCR inhibition better in duplex assays |
Multiplexing Efficiency and Limitations
Multiplex qPCR represents a valuable tool that allows researchers to simultaneously amplify and detect multiple target sequences in a single reaction. This capability streamlines workflow and increases qPCR efficiency. However, comparisons between qPCR and ddPCR techniques have shown that while qPCR has higher sensitivity, a wider linear dynamic range, shorter analysis time, and better cost-effectiveness (making it suitable for initial screening), the ddPCR approach has lower variability and is able to handle the PCR inhibition and competitive effects found in duplex assays, thus providing more precise and accurate analysis [58].
For fragment analysis-based methods like MultiFRAGing, multiplexing can be achieved through several strategies: (1) amplicons separated by two/three different sizes amplified in a single reaction; (2) amplicons separated by two/three different colors amplified in a single reaction; (3) amplicons separated by three/four different sizes amplified separately, then pooled for capillary electrophoresis; or (4) amplicons separated by three different colors and two sizes amplified separately, then pooled together [59]. This approach can identify indels in up to four targets from a single reaction, representing a four-fold increase in genotyping throughput.
Essential Research Reagent Solutions
Table 3: Research Reagent Toolkit for Multiplex Detection
| Reagent/Kit | Function | Application Context |
|---|---|---|
| QIAamp DNA Mini Kit | DNA extraction from FFPE tissues | Sample preparation for all platforms |
| Qiagen Multiplex PCR Master Mix | Multiplex PCR amplification | SNaPshot, fragment analysis |
| Platinum Taq Polymerase | High-fidelity amplification | Fragment analysis, dPCR |
| TaqMan Assays | Sequence-specific detection | qPCR, dPCR mutation detection |
| pGEM-T Easy Vector | Cloning for plasmid standards | Assay validation and controls |
| EvaGreen dye | DNA intercalator for detection | Single-color dPCR |
| Absolute Q Liquid Biopsy dPCR Assays | Predesigned mutation panels | Liquid biopsy research |
The comparative analysis of multiplexing strategies for simultaneous wild-type and mutant allele detection reveals a dynamic technological landscape where each platform offers distinct advantages for specific research and clinical contexts. Digital PCR emerges as the superior technology for applications requiring ultra-sensitive detection of rare mutations, particularly in liquid biopsy samples where variant allele frequencies can be extremely low. The ability to detect mutations at frequencies as low as 0.1% without standard curves provides significant advantages for absolute quantification [19] [56].
Conversely, qPCR-based methods including SNaPshot and HRM analysis maintain importance for cost-effective routine testing scenarios where highest sensitivity is not required but throughput and established workflows are prioritized [54]. The choice between these platforms ultimately depends on specific research requirements, including sensitivity thresholds, sample quantity and quality, multiplexing needs, and available resources.
As molecular diagnostics continue to evolve, the integration of these complementary technologies offers the most robust approach for comprehensive mutation profiling. Drug development professionals should consider implementing orthogonal validation strategies that leverage the unique strengths of both dPCR and qPCR platforms to ensure accurate, reliable detection of clinically relevant mutations in both tissue and liquid biopsy specimens.
Optimizing Assay Performance: Critical Steps for Robust Mutant Detection
The detection of low-frequency mutant alleles is a cornerstone of modern precision medicine, directly impacting diagnostic accuracy, treatment selection, and therapeutic monitoring. This process hinges on robust assay design and rigorous validation, with primer/probe specificity and the strategic use of controls being paramount. Within this framework, a significant methodological evolution is underway, shifting from traditional quantitative PCR (qPCR) to more sensitive digital PCR (dPCR) platforms. This guide provides an objective comparison of these two technologies, focusing on their performance in detecting challenging mutant alleles like the epidermal growth factor receptor (EGFR) T790M mutation, a key marker of treatment resistance in non-small cell lung cancer (NSCLC). The data demonstrate that while qPCR remains a reliable workhorse, dPCR offers superior sensitivity and absolute quantification, particularly for samples with mutant allele frequencies below 1% [9] [10].
The transition to dPCR is driven by the need for unparalleled sensitivity in applications such as liquid biopsy, where tumor DNA is scarce in a high background of wild-type DNA. This guide summarizes experimental data, details key methodologies, and provides a resource toolkit to help researchers and drug development professionals make informed decisions about assay design and platform selection for their specific research context.
Technology Comparison: qPCR versus dPCR
Fundamental Principles and Workflows
Quantitative PCR (qPCR) is a well-established method that quantifies nucleic acids relative to a standard curve. It monitors PCR amplification in real-time as fluorescence increases with each cycle. The cycle threshold (Ct) at which fluorescence crosses a predefined threshold is used for relative quantification. Its "bulk" reaction format means the entire sample is amplified in a single tube, making it susceptible to variations in amplification efficiency and the presence of PCR inhibitors [10].
In contrast, digital PCR (dPCR) provides absolute quantification without the need for a standard curve. It achieves this by partitioning a single PCR reaction into thousands to millions of nanoliter-sized reactions. Each partition effectively contains zero, one, or more target molecules. Following end-point PCR amplification, the partitions are analyzed to count the number of positive (fluorescent) and negative (non-fluorescent) reactions. The absolute copy number of the target sequence is then calculated using Poisson statistics [9] [10]. This partitioning confers higher tolerance to PCR inhibitors and eliminates the reliance on amplification efficiency, as data is collected at the end of the PCR cycles rather than during the exponential phase [10].
The following diagram illustrates the core workflows and logical differences between the two technologies:
Performance Comparison in Mutant Allele Detection
Direct comparative studies highlight the distinct advantages of dPCR for detecting low-abundance mutations. The following table synthesizes quantitative data from studies analyzing the EGFR T790M mutation, a critical resistance marker in NSCLC.
Table 1: Performance comparison of qPCR and dPCR in detecting EGFR T790M mutation
| Parameter | qPCR (ARMS-based) | Droplet Digital PCR (ddPCR) | QS3D Digital PCR | Experimental Context |
|---|---|---|---|---|
| Detection Limit | ~1% mutation rate [9] | ~0.1% mutation rate [9] | ~0.1% mutation rate [12] | Plasmid DNA samples with defined mutation rates [9] |
| Quantification Basis | Relative (requires standard curve) [10] | Absolute (Poisson statistics) [9] [10] | Absolute (Poisson statistics) [12] | N/A |
| Sensitivity in Clinical Samples | 15/72 T790M+ cfDNA samples [12] | 21/72 T790M+ cfDNA samples [12] | Highly consistent with ddPCR [12] | 72 NSCLC patient plasma cfDNA samples [12] |
| Precision & Robustness | Affected by PCR inhibitors and amplification efficiency changes [10] | High tolerance to inhibitors; unaffected by amplification efficiency changes [10] | High consistency with droplet methods [12] | Various sample types including FFPE and plasma [9] [10] |
| Key Finding | Missed a clinical sample (N006) with 7 mutant copies in 6,000 wild-type copies (~0.12%) [9] | Identified the T790M mutation in sample N006, missed by ARMS-qPCR [9] | 91.7% overall agreement with ddPCR for T790M in cfDNA [12] | 10 clinical FFPE samples [9] |
The data clearly shows that dPCR platforms offer a lower limit of detection (LOD), reliably identifying mutations at a 0.1% allele frequency compared to the 1% LOD of ARMS-qPCR [9]. This enhanced sensitivity has direct clinical relevance, as evidenced by the ability of ddPCR to identify a T790M mutation in a patient sample (N006) that was falsely classified as wild-type by ARMS-qPCR [9]. In a larger cohort study, both ddPCR and the QS3D dPCR system detected more positive samples than qPCR, with discordant results occurring at low mutation abundances around 0.1% [12].
Experimental Protocols for Assay Validation
Primer and Probe Design for Specificity
Achieving high specificity is the first critical step in detecting single-nucleotide variants. The following guidelines are essential for designing primers and probes for both qPCR and dPCR assays [60]:
Primer Design:
- Length: 18–30 bases.
- Melting Temperature (Tm): Optimal Tm of 60–64°C, with an ideal of 62°C. The Tm of forward and reverse primers should not differ by more than 2°C.
- GC Content: 35–65%, with an ideal of 50%. Avoid runs of four or more consecutive G residues.
- Complementarity: Screen designs for self-dimers, heterodimers, and hairpins. The ΔG for any secondary structure should be weaker (more positive) than -9.0 kcal/mol.
- Specificity Check: Perform an in silico NCBI BLAST alignment to ensure primers are unique to the target sequence.
TaqMan Probe Design:
- Location: Should be in close proximity to a primer but must not overlap with the primer-binding site.
- Tm: Should be 5–10°C higher than the primer Tm.
- GC Content: Same as primers (35–65%). Avoid a G at the 5’ end.
- Type: Double-quenched probes (e.g., using ZEN or TAO internal quenchers) are recommended over single-quenched probes to lower background and increase signal-to-noise ratio [60].
Amplicon Design:
- Length: 70–150 bp is ideal for efficient amplification.
- Location: When working with RNA or distinguishing genomic DNA, design assays to span an exon-exon junction.
The Use of Positive and Internal Controls
Controls are non-negotiable for validating results and identifying assay failure. The MIQE guidelines (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) provide a standardized framework for reporting all aspects of qPCR experiments, including the use of controls, to ensure reproducibility and credibility [61] [62].
Internal Control (IC): An IC is a non-target nucleic acid co-amplified with the target to monitor the entire process from extraction to amplification. A synthetic IC is designed with primer binding regions identical to the target and a unique, internal probe binding region for differentiation [63].
- Function: Distinguishes true target negativity from PCR failure due to inhibition or workflow error. A negative result is only valid if the IC amplifies correctly.
- Implementation: A low copy number (e.g., 20 copies) of the IC is spiked into each sample. Its amplification confirms that the reaction was efficient enough to detect a target present at the limit of detection [63].
- Impact: The use of an IC can increase test sensitivity by 1–6% by preventing the reporting of false negatives and allowing for the retesting of inhibitory specimens [63].
Positive Control: A positive control contains the target sequence of interest and is used to verify that the assay correctly identifies a known positive sample. It is crucial for confirming reagent integrity and correct instrument function.
Detailed dPCR Protocol for EGFR T790M Detection in cfDNA
The following protocol is adapted from a study comparing dPCR platforms for detecting EGFR T790M in cell-free DNA from lung cancer patients [12].
Table 2: Key research reagent solutions for dPCR mutation detection
| Reagent/Material | Function | Example Product/Specification |
|---|---|---|
| QX200 Droplet Generator | Partitions the PCR reaction into ~20,000 nanoliter-sized droplets | Bio-Rad QX200 System [9] |
| TaqMan Assay | Provides sequence-specific primers and a fluorescent probe for the target (T790M) and wild-type sequences | Human EGFR Gene Mutations Detection Kit or custom-designed assays [9] |
| ddPCR 2X Master Mix | Provides optimized buffer, dNTPs, and polymerase for digital PCR | Bio-Rrad ddPCR Master Mix [9] |
| Droplet Generation Oil | Creates the water-in-oil emulsion for droplet formation | Bio-Rad Droplet Generation Oil [9] |
| Cell-free DNA Sample | The analyte containing the mutant and wild-type alleles | Isolated from patient plasma using a kit like QIAamp DNA Blood Mini |
Step-by-Step Workflow:
Sample Collection and cfDNA Extraction: Collect patient blood in anticoagulant tubes. Isolate plasma by centrifugation and extract cfDNA using a commercial kit (e.g., QIAamp DNA Blood Mini Kit) according to the manufacturer's instructions. Quantify DNA using a spectrophotometer (e.g., Nanodrop) [9] [12].
Reaction Mix Preparation: For each sample, prepare a 25 µL reaction mixture containing:
- 12.5 µL of ddPCR 2X Master Mix
- 1.25 µL of 20X primer and TaqMan probe mix (for T790M and a reference gene)
- 8.75 µL of nuclease-free water
- 2.5 µL of extracted cfDNA template [9]
Droplet Generation: Load the entire reaction mixture into the middle well of a droplet generator cartridge. Add 70 µL of droplet generation oil to the lower well. Place the cartridge into the QX200 Droplet Generator. The instrument will automatically create the water-in-oil emulsion, yielding approximately 20,000 droplets per sample [9].
PCR Amplification: Carefully transfer 40 µL of the generated droplets to a 96-well PCR plate. Seal the plate and place it in a thermal cycler. Run the following program:
- 95°C for 10 min (enzyme activation)
- 40 cycles of:
- 94°C for 30 sec (denaturation)
- 58°C for 1 min (annealing/extension)
- 98°C for 10 min (enzyme deactivation)
- 4°C hold [9]
Droplet Reading and Analysis: Place the PCR plate in the QX200 Droplet Reader. The reader streams each droplet past a fluorescence detector, classifying it as positive (mutant), positive (wild-type), or negative. The raw data is then analyzed using companion software (e.g., QuantaSoft). The software applies Poisson statistics to the counts of positive and negative droplets to provide an absolute copy number per microliter of the input sample for both mutant and wild-type alleles, from which the mutant allele frequency is calculated [9].
The Scientist's Toolkit: Essential Reagent Solutions
Successful implementation of mutation detection assays requires a suite of reliable reagents and tools. The following table details essential components.
Table 3: Essential research reagents and materials for PCR-based mutation detection
| Category | Item | Critical Function |
|---|---|---|
| Nucleic Acid Isolation | DNA/RNA Extraction Kits (e.g., for FFPE, plasma) | Purifies high-quality, inhibitor-free nucleic acid from complex clinical samples. [9] |
| Assay Design | Primer & Probe Design Tools (e.g., IDT SciTools, PrimerQuest) | Ensures optimal specificity, Tm, and GC content for robust amplification. [60] |
| Assay Components | Predesigned TaqMan Assays | Provides pre-validated, highly specific primer/probe sets for known targets. [61] [60] |
| PCR Master Mix | dPCR or qPCR Master Mix | Provides optimized buffers, enzymes, and dNTPs for efficient amplification. [9] |
| Controls | Synthetic Internal Control & Positive Control Plasmid | Validates assay performance and distinguishes true negatives from assay failure. [63] |
| Reference Materials | Characterized Genomic DNA or Plasmid Samples | Serves as a gold standard for determining assay LOD and during validation. [9] [62] |
The choice between qPCR and dPCR is fundamentally dictated by the application's required sensitivity and precision. For the detection of mutant alleles at frequencies above 1%, qPCR remains a powerful, cost-effective, and well-standardized tool. However, for the growing number of applications demanding the detection of rare mutations—such as monitoring minimal residual disease or identifying emerging resistance mutations in circulating tumor DNA—dPCR is the unequivocal superior technology. Its ability to provide absolute quantification without a standard curve, coupled with its robust performance in the presence of inhibitors and its sensitivity down to 0.1% allele frequency, enables earlier and more accurate detection of biomarker status [9] [10] [12].
Regardless of the platform chosen, rigorous assay validation built on the principles of primer/probe specificity and the comprehensive use of controls is essential. Adherence to MIQE-inspired guidelines ensures that results are reliable, reproducible, and capable of supporting critical decisions in both research and clinical development [61] [62] [64].
Digital PCR (dPCR) has established itself as a powerful tool for the absolute quantification of nucleic acids, offering unparalleled sensitivity for applications like detecting rare mutant alleles in a background of wild-type sequences. However, the phenomenon of 'rain'—the appearance of intermediate fluorescent clusters that fall between clearly positive and negative populations—can compromise data resolution and accuracy. This guide objectively compares optimization strategies and performance data across key dPCR parameters and platforms to provide a clear roadmap for minimizing rain.
Understanding Rain and Its Impact on dPCR Performance
In dPCR, a sample is partitioned into thousands of individual reactions, each yielding a definitive positive or negative fluorescence signal after endpoint amplification. The term "rain" refers to partitions that exhibit ambiguous fluorescence, appearing as a scatter of data points between the high-positive and low-negative clusters. This phenomenon can lead to inaccurate quantification by increasing the technical variation in copy number estimates and raising the effective limit of detection.
The causes of rain are multifactorial, often stemming from suboptimal template quality, inefficient amplification within partitions, or non-specific probe chemistry. For instance, fragmented or degraded DNA, as often obtained from formalin-fixed paraffin-embedded (FFPE) tissue, can lead to truncated amplification products and incomplete fluorescent probe hydrolysis, generating intermediate signals. Similarly, imperfect thermal cycling conditions can cause uneven amplification efficiency across partitions. Recognizing and mitigating these sources is the first step toward achieving the high-precision data required for demanding applications like liquid biopsy and microbial quantification.
Comparative Data: dPCR Performance and Optimization
The following tables synthesize experimental data from recent studies, comparing platform performance and the impact of key reagents on assay precision.
Table 1: Comparison of dPCR Platform Performance and Rain Mitigation
| Platform (Technology) | Key Performance Metric | Impact on Rain/Precision | Experimental Context |
|---|---|---|---|
| QX200 (Droplet ddPCR) [18] | LOQ: 4.26 copies/µL input; CV: <5% (with optimized enzyme) | Higher precision achieved with HaeIII vs. EcoRI restriction enzyme [18] | Gene copy number quantification in protists; precision tested with two restriction enzymes. |
| QIAcuity (Nanoplate dPCR) [18] | LOQ: 1.35 copies/µL input; CV: ~8% for mid-range concentrations | Lower impact from enzyme choice; generally high precision [18] | Same study as above, allowing for direct cross-platform comparison. |
| Absolute Q, QIAcuity, QX600, Digital Light Cycler [65] | High linearity (R² ≥ 0.99) across 4 orders of magnitude | USE-PCR chemistry standardizes signals, reducing assay-specific rain [65] | Multiplex detection of 32 synthetic templates using universal probe system. |
| QS3D (Chip-based dPCR) [12] | 91.7% agreement with droplet dPCR for EGFR T790M | Stricter threshold settings can reduce sensitivity but improve cluster clarity [12] | Detection of T790M mutation in patient cfDNA; 6 discordant samples had ~0.1% abundance. |
Table 2: Optimizing Reagents to Minimize Rain and Improve Quantification
| Parameter | Standard Approach | Optimized Strategy | Experimental Outcome |
|---|---|---|---|
| Template Quality | Using fragmented DNA from FFPE samples [9] | Ensure high DNA purity (OD260/280 ~1.95); use restriction enzymes [9] [23] | ddPCR detected 7 mutant copies in 6,000 wild-type where ARMS-qPCR failed [9]. |
| Probe Chemistry | Target-specific hydrolysis probes for each assay [65] | Universal Signal Encoding PCR (USE-PCR) with color-coded tags [65] | Achieved 92.6%–97.6% target identification accuracy, simplifying analysis [65]. |
| Restriction Enzymes | Standard enzyme (e.g., EcoRI) | Enzyme selection (e.g., HaeIII over EcoRI) [18] | HaeIII drastically improved precision for ddPCR (CVs <5% vs. up to 62.1%) [18]. |
| Multiplexing Efficiency | Custom probe mixes per target, prone to imbalance | Leveled universal probe mix tailored to platform optics [65] | Enabled precise 32-plex detection with high linearity on four different dPCR platforms [65]. |
Experimental Protocols for Key Optimization Strategies
Protocol: Restriction Digestion to Improve Template Quality
The use of restriction enzymes to digest long genomic DNA fragments enhances template accessibility and reduces rain by promoting complete amplification.
- Sample Preparation: Extract DNA using a dedicated kit (e.g., QIAamp DNA FFPE Tissue kit or QIAamp DNA Mini kit) [9] [23].
- Reaction Setup: Incorporate the restriction enzyme directly into the dPCR master mix. For a 40 µL reaction on the QIAcuity, use 0.025 U/µL of a restriction enzyme like Anza 52 PvuII or HaeIII [18] [23].
- Thermal Cycling: The standard cycling protocol typically includes an extended initial hold at 95°C for 2 minutes, which simultaneously activates the hot-start polymerase and the restriction enzyme [23].
- Validation: Compare the coefficient of variation (CV) and the clarity of cluster separation in assays with and without the restriction enzyme.
Protocol: Universal Signal Encoding PCR (USE-PCR) for Probe-Based Assays
USE-PCR decouples the detection chemistry from the specific target, using universal probes to generate consistent, pre-optimized fluorescent signatures, thereby minimizing rain from inefficient probe hydrolysis [65].
- Primer Design: Design allele-specific primers (ASPs) with a 3' end that binds the target and a 5' end that consists of a synthetic "color-coded tag." This tag contains binding sites for universal hydrolysis probes [65].
- Universal Probe Mix: Prepare a single, pre-optimized mixture of universal probes. Each probe is conjugated to a specific fluorophore and is used at a concentration leveled for the specific dPCR platform's optical filters [65].
- Assay Assembly: Combine the template DNA, ASPs with their respective tags, locus-specific primers, and the universal probe mix in the dPCR master mix.
- Partitioning and Amplification: Run the assay on the chosen dPCR platform using a standard endpoint amplification protocol.
- Signal Decoding: Analyze the fluorescence in each partition across available channels. The amplitude and color combination generated by the universal probes correspond to a specific tag, identifying the original target.
The USE-PCR workflow and signal generation mechanism is as follows:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for dPCR Optimization
| Item | Function & Rationale | Example Products & Notes |
|---|---|---|
| High-Efficiency Restriction Enzymes | Cuts long DNA to ensure uniform access to targets, reducing amplification failure and rain. | Anza 52 PvuII [23], HaeIII [18]. Select enzyme based on amplicon sequence. |
| Universal Probe Systems | Decouples detection from target, using pre-optimized probes for consistent signal, reducing rain from probe inefficiency. | USE-PCR probe mixes [65]. Probes must be leveled for the specific dPCR platform. |
| Dedicated Nucleic Acid Kits | Provides high-purity, intact DNA/RNA; critical for complex samples (FFPE, plasma cfDNA). | QIAamp DNA FFPE Tissue kit [9], QIAamp DNA Mini kit [23], KingFisher Flex with MagMax Viral/Pathogen [6]. |
| Platform-Specific Master Mixes | Optimized chemistry and surfactant formulation for stable partitions and efficient amplification. | ddPCR 2X Master Mix [9], QIAcuity Probe PCR Kit [23]. Avoid cross-platform substitution. |
Minimizing rain in dPCR is not achieved by a single solution but through a holistic strategy addressing template, chemistry, and instrumentation. The experimental data demonstrates that template pretreatment with restriction enzymes and the adoption of universal probe systems like USE-PCR significantly enhance precision and cluster resolution. As the field advances, these optimization protocols will be crucial for leveraging the full power of dPCR in detecting rare mutant alleles and other challenging targets, solidifying its advantage over quantitative PCR in sensitivity and absolute quantification.
The accurate detection and quantification of nucleic acids are fundamental to molecular biology, supporting advancements in clinical diagnostics, environmental surveillance, and biomedical research. However, the reliability of these analyses is frequently compromised by the presence of PCR inhibitors in complex sample matrices. These substances can disrupt polymerase activity, leading to reduced amplification efficiency, false-negative results, and significant underestimation of target concentrations [66].
Traditional quantitative PCR (qPCR), while a workhorse technology, is particularly vulnerable because it relies on the efficiency of amplification kinetics, which inhibitors directly impair [67] [16]. Digital PCR (dPCR), the third generation of PCR technology, offers a transformative approach to this problem. By partitioning a sample into thousands of individual reactions, dPCR fundamentally changes how amplification is measured and confers a higher innate tolerance to PCR inhibitors [10] [68]. This guide objectively compares the performance of dPCR and qPCR in the presence of inhibitors, providing supporting experimental data and methodologies relevant to researchers working with challenging samples.
Fundamental Principles: How dPCR Mitigates Inhibition
The core difference between the two technologies lies in their quantification methods and how they handle the amplification process.
qPCR: A Bulk Reaction Vulnerable to Efficiency Loss
- Principle of Operation: In qPCR, the entire reaction mixture is amplified in a single tube, and fluorescence is measured at each cycle during the exponential phase. The cycle threshold (Ct) at which fluorescence crosses a predefined threshold is used to estimate the initial template concentration relative to a standard curve [10] [16].
- Vulnerability to Inhibitors: The presence of inhibitors reduces the effective activity of the DNA polymerase. This leads to a decrease in amplification efficiency, causing a delay in the Ct value. Since quantification is directly inferred from the Ct, this delay results in an underestimation of the true target concentration. Even a 5% difference in reaction efficiency can cause a greater than 2-fold difference in final results [67].
dPCR: Partitioning and Endpoint Counting
- Principle of Operation: dPCR divides the PCR mixture into a large number of parallel nanoreactions—either in droplets or microchambers—so that each partition contains zero, one, or a few target molecules. After endpoint amplification, each partition is read as positive or negative based on its fluorescence. The absolute concentration of the target is then calculated directly from the fraction of negative partitions using Poisson statistics, eliminating the need for a standard curve [22] [10].
- Mechanism of Inhibitor Tolerance: Inhibitors are similarly distributed throughout the partitions. While they may still prevent amplification in some partitions, the majority of partitions remain unaffected. The final quantification is based on the simple binary count of positive partitions, not on the rate or efficiency of amplification. This makes the absolute quantification in dPCR inherently less susceptible to the influence of PCR inhibitors present in complex biological matrices [67] [10] [68].
The following diagram illustrates this core mechanistic difference:
Experimental Evidence: Direct Performance Comparisons
Multiple studies across diverse fields have directly compared the performance of dPCR and qPCR in the presence of inhibitors, consistently demonstrating dPCR's superior robustness.
Case Study 1: Pathogen Detection in Complex Soil Samples
A 2025 study developed a droplet digital PCR (ddPCR) assay for detecting Phytophthora nicotianae, a destructive soil-borne oomycete pathogen. The researchers compared the diagnostic performance of ddPCR and qPCR using 213 field-collected tobacco root and soil samples, which are notoriously challenging due to the presence of humic acids and other PCR inhibitors [69].
Key Findings:
- Higher Detection Rate: ddPCR demonstrated a significantly higher positive detection rate of 96.4% compared to 83.9% for qPCR.
- Superior Diagnostic Accuracy: Receiver operating characteristic (ROC) analysis showed the area under the curve (AUC) for ddPCR was 0.913, compared to 0.885 for qPCR.
- Better Quantification at Low Concentrations: The study concluded that "ddPCR provided better quantification accuracy for low pathogen concentrations in soil, suggesting better tolerance to potential PCR inhibitors in soil" [69].
Case Study 2: Viral Load Measurement in Wastewater
Wastewater is a complex matrix containing various substances that inhibit PCR, including complex polysaccharides, lipids, proteins, and metal ions. A 2024 study evaluated different approaches to reduce PCR inhibition in wastewater samples for SARS-CoV-2 detection [66].
Key Findings:
- The authors noted that "ddPCR has emerged as an alternative approach to overcome the limitations of real time PCR... due to its tolerance to interfering substances that is explained by the partitioning of a single reaction into thousands of individual PCR reactions."
- While dilution is a common strategy to mitigate inhibition in qPCR, it also reduces sensitivity. The study found dPCR to be inherently more robust, stating that "due to the partitioning of PCR reactions into thousands of individual nano-reactions, dPCR is less susceptible than qPCR to the influence of PCR inhibitors that may be present in complex biological matrices" [67] [66].
The table below summarizes key comparative performance metrics from recent studies:
Table 1: Comparative Performance of dPCR vs. qPCR in Complex Samples
| Sample Type / Study | Performance Metric | qPCR | dPCR |
|---|---|---|---|
| Soil Samples [69] | Positive Detection Rate | 83.9% | 96.4% |
| ROC Area Under Curve (AUC) | 0.885 | 0.913 | |
| Sensitivity [10] | Rare Mutation Detection | >1% | ≥ 0.1% |
| Inhibitor Tolerance [67] | Impact on Quantification | Significant | Reduced |
| Quantification [10] | Standard Curve Requirement | Yes | No |
Detailed Experimental Protocol: Assessing dPCR Performance
For researchers seeking to validate dPCR performance in their own inhibitory samples, the following protocol, adapted from the Phytophthora nicotianae study, provides a robust methodological template [69].
Sample Collection and DNA Extraction
- Tobacco Root Tissue: Collect root samples. Grind approximately 50 mg of tissue in liquid nitrogen. Extract total DNA using the DNeasy Plant Mini Kit (Qiagen) according to the manufacturer's protocol.
- Rhizosphere Soil: Collect ~5 grams of soil closely associated with roots. Extract DNA using the DNeasy PowerSoil Kit (Qiagen) as per the manufacturer's instructions.
- Quality Assessment: Assess the quality and concentration of extracted DNA using a NanoDrop spectrophotometer.
ddPCR Assay Setup and Execution
- Reaction Mixture: Prepare a 20 µL reaction containing:
- 10 µL of 2× ddPCR Supermix for Probes (Bio-Rad)
- 1 µL of each forward and reverse primer (final concentration 500 nM each)
- 0.5 µL of probe (final concentration 250 nM), labeled with FAM at the 5' end and BHQ1 at the 3' end
- 2 µL of template DNA
- Nuclease-free water to volume
- Droplet Generation: Generate droplets using the QX200 Droplet Generator (Bio-Rad).
- Thermal Cycling: Transfer droplets to a 96-well PCR plate, seal with pierceable foil, and run on a thermal cycler with the following protocol:
- Initial Denaturation: 95°C for 10 min
- 45 Cycles of:
- Denaturation: 94°C for 30 sec
- Annealing/Extension: 58°C for 1 min
- Final Extension: 98°C for 10 min
- Hold at 4°C
- Droplet Reading and Analysis: Read the droplets using the QX200 Droplet Reader and analyze with QuantaSoft software (Bio-Rad).
Parallel qPCR for Comparison
- Reaction Mixture: Prepare a 20 µL reaction containing:
- 10 µL of 2× Probe qPCR MasterMix
- 1 µL of each primer (500 nM)
- 0.5 µL of probe (250 nM)
- 2 µL of template DNA
- Nuclease-free water to volume
- Thermal Cycling: Use identical cycling conditions to the ddPCR assay on a real-time cycler (e.g., Light Cycler 480 II, Roche).
- Quantification: Determine quantities based on a standard curve.
Analytical Performance Assessment
- Limit of Blank (LoB): Perform 60 measurements on blank samples (nuclease-free water) to establish background.
- Limit of Detection (LoD): Determine the lowest concentration detectable with 95% confidence using probit regression on 70 measurements across low-concentration series.
- Limit of Quantification (LoQ): Determine the lowest concentration quantifiable with acceptable precision (CV < 25%) using 20 measurements across serial dilutions.
The Scientist's Toolkit: Essential Reagent Solutions
The table below details key reagents and their critical functions in setting up robust dPCR assays, particularly for challenging samples.
Table 2: Essential Research Reagent Solutions for dPCR
| Reagent / Kit | Function & Importance | Example Use Case |
|---|---|---|
| DNeasy PowerSoil Kit (Qiagen) | Efficiently extracts inhibitor-free DNA from complex matrices like soil. Critical for removing humic acids. | DNA extraction from rhizosphere soil for pathogen detection [69]. |
| ddPCR Supermix for Probes (Bio-Rad) | Optimized master mix for droplet-based dPCR. Provides stable emulsion and robust amplification. | Detection of Phytophthora nicotianae in root tissue [69]. |
| NanoDrop Spectrophotometer | Rapidly assesses DNA concentration and purity (A260/280 ratio). Initial quality control check. | Quality assessment of nucleic acids extracted from wastewater [66]. |
| TaqMan Probe-Based Assays | Sequence-specific probes provide high specificity and enable multiplexing in dPCR applications. | Multiplex detection of respiratory viruses (Influenza A/B, RSV, SARS-CoV-2) [6]. |
| PCR Enhancers (e.g., BSA, gp32) | Proteins that bind inhibitors (e.g., humic acids), preventing them from interfering with polymerase. | Added to qPCR reactions to mitigate inhibition in wastewater samples [66]. |
Platform Considerations and Experimental Design
When incorporating dPCR into your research, the choice of platform and careful experimental design are crucial for success.
Comparison of dPCR Platforms
Different dPCR systems employ distinct partitioning technologies, which can influence performance and workflow.
Table 3: Comparison of Common dPCR Partitioning Technologies
| Characteristic | Droplet dPCR (ddPCR) | Nanoplate dPCR (ndPCR) |
|---|---|---|
| Partitioning Method | Water-in-oil emulsion droplets [22] | Solid-state microchambers/ nanowells [22] |
| Typical Partition Count | Thousands to millions of droplets | Tens of thousands of chambers (e.g., ~26,000) [6] |
| Throughput & Workflow | Sequential droplet reading can be slower | Simultaneous imaging of all partitions for faster readout [10] [18] |
| Representative Systems | QX200 (Bio-Rad) [69] [18] | QIAcuity (Qiagen) [18] [6] |
| Key Advantage | High scalability, cost-effective for partitions | Higher reproducibility, ease of automation [22] |
A 2025 cross-platform evaluation study using the ciliate Paramecium tetraurelia found that both the QX200 (ddPCR) and QIAcuity One (ndPCR) platforms "demonstrated similar detection and quantification limits and yielded high precision across most analyses," though precision could be influenced by factors like restriction enzyme choice [18].
Guidance for Experimental Design
- Assay Optimization: Optimize primer and probe concentrations as well as annealing temperature to minimize "rain" (droplets with intermediate fluorescence) and ensure clear separation between positive and negative partitions [69].
- Inhibition Testing: Spike a known quantity of target into your sample and compare the measured concentration to a control in a clean matrix. A significant recovery in the sample matrix with dPCR, but not with qPCR, indicates successful overcoming of inhibition.
- Multiplexing Potential: dPCR simplifies the relative quantification in multiplex assays by providing absolute counts for each target, which is advantageous for allele frequency calculations or pathogen co-detection [68] [6].
The following workflow summarizes the key steps in a dPCR experiment and its advantage in handling inhibitors:
The evidence from multiple independent studies consistently demonstrates that digital PCR offers a significant advantage over quantitative PCR when analyzing complex samples containing PCR inhibitors. The fundamental principle of sample partitioning underpins dPCR's superior robustness, enabling more accurate detection and quantification in challenging matrices like soil, wastewater, and clinical specimens rich in contaminants.
For research applications where sample integrity is paramount and inhibitors are a known challenge—such as environmental monitoring, agricultural pathogen detection, and liquid biopsy—dPCR provides a reliable tool that reduces the need for extensive sample clean-up and mitigates the risk of false negatives. While factors like cost and throughput remain considerations, the enhanced tolerance of dPCR makes it an increasingly indispensable technology in the molecular scientist's toolkit.
The accurate detection of mutant alleles is a cornerstone of modern molecular diagnostics and therapeutic drug development. While both quantitative PCR (qPCR) and digital PCR (dPCR) are established technologies for this purpose, the integrity and accessibility of the genomic DNA (gDNA) template are critical yet often overlooked factors influencing assay performance. This guide explores the strategic use of restriction enzymes to fragment complex gDNA, thereby enhancing target accessibility and improving the precision and sensitivity of nucleic acid quantification. We present experimental data comparing the performance of qPCR and dPCR platforms when analyzing enzyme-digested samples, providing researchers with validated protocols to optimize their detection assays for challenging genomic targets.
In the field of molecular biology, the detection of mutant alleles is essential for applications ranging from cancer biomarker discovery to monitoring drug resistance. The packaging of eukaryotic DNA into chromatin creates a significant structural barrier to molecular processes, including PCR amplification [70]. This compact architecture can obscure target sequences, leading to underestimated copy numbers and reduced assay sensitivity. While much attention is given to selecting between qPCR and dPCR, sample preparation—particularly DNA fragmentation—is a critical parameter for success. Restriction enzymes, with their sequence-specific cleavage activity, provide a controlled means of dissecting complex genomic DNA. This process increases the number of accessible DNA ends and reduces steric hindrance, which is particularly beneficial for targets embedded in repetitive or tightly packed genomic regions [18] [70]. By integrating this simple step into sample preparation workflows, researchers can significantly enhance the performance of downstream PCR applications.
Restriction Enzymes as a Tool for DNA Fragmentation
Fundamental Mechanisms
Restriction enzymes, also known as restriction endonucleases, are enzymes that recognize and cut double-stranded DNA at specific palindromic sequences, typically between 4 and 8 base pairs in length [71] [72]. They are a native defense mechanism in bacteria and have been harnessed as powerful tools in biotechnology. Their function in improving target accessibility is twofold:
- Generation of Accessible Ends: They create double-strand breaks, producing new DNA ends that are more readily accessible to PCR primers and probes.
- Reduction of Steric Hindrance: By cutting long, entangled gDNA into smaller, more manageable fragments, they minimize the effects of DNA folding and coiling that can physically impede polymerase binding and function.
Enzyme Selection Criteria
Choosing the appropriate restriction enzyme is vital. The selection is primarily based on whether its recognition site is present proximal to the target region of interest, without cutting within the target sequence itself [70]. Furthermore, the type of ends produced—sticky (overhanging) or blunt—can influence downstream ligation efficiency but is generally less critical for PCR-based detection. Experimental evidence suggests that the choice of enzyme can directly impact data quality, with different enzymes showing varying levels of effectiveness in improving quantification precision [18].
Experimental Protocol: Employing Restriction Enzymes for Enhanced dPCR
The following methodology details the use of restriction enzymes to prepare genomic DNA for digital PCR analysis, adapted from a study investigating gene copy number variations [18].
Materials and Reagents
- Genomic DNA Sample: Purified from cell lines or tissues of interest.
- Restriction Endonuclease: Selected based on the target genomic region (e.g., HaeIII, EcoRI).
- Appropriate Restriction Enzyme Buffer: Typically supplied with the enzyme.
- Nuclease-Free Water.
- Thermal Cycler or Incubator.
Step-by-Step Procedure
- Digestion Reaction Setup: In a sterile microcentrifuge tube, assemble the following reaction mixture:
- Genomic DNA (100-200 ng): X µL
- 10X Restriction Enzyme Buffer: 2.0 µL
- Restriction Enzyme (e.g., HaeIII, 10 U/µL): 1.0 µL
- Nuclease-Free Water: to 20 µL final volume
- Incubation: Mix the reaction thoroughly by pipetting and centrifuge briefly. Incubate at the enzyme's optimal temperature (commonly 37°C) for 30-60 minutes.
- Enzyme Inactivation: Heat-inactivate the enzyme according to the manufacturer's recommendations (e.g., 20 minutes at 65°C). Alternatively, the digested DNA can be purified using standard ethanol precipitation or spin-column kits.
- Quantification and Dilution: Quantify the digested DNA using a fluorometer and dilute to the desired working concentration for dPCR analysis.
- dPCR Analysis: Proceed with the standard dPCR workflow, including partition generation, end-point PCR amplification, and droplet or well reading.
Comparative Performance Data: qPCR vs. dPCR with Restriction Enzyme Digestion
The integration of a restriction enzyme digestion step prior to PCR analysis provides measurable benefits, particularly for dPCR. The following tables summarize key experimental findings.
Table 1: Impact of Restriction Enzyme Digestion on Precision in dPCR [18]
| Platform | Restriction Enzyme | Sample Type | Coefficient of Variation (CV) Range | Key Finding |
|---|---|---|---|---|
| QX200 ddPCR (Bio-Rad) | EcoRI | Paramecium DNA | 2.5% - 62.1% | High variability, especially at low cell counts |
| QX200 ddPCR (Bio-Rad) | HaeIII | Paramecium DNA | < 5% (all cell counts) | Significantly improved precision |
| QIAcuity One ndPCR (QIAGEN) | EcoRI | Paramecium DNA | 0.6% - 27.7% | Moderate variability |
| QIAcuity One ndPCR (QIAGEN) | HaeIII | Paramecium DNA | 1.6% - 14.6% | Improved precision |
Table 2: General Performance Comparison of qPCR and dPCR for Target Detection [9] [10] [73]
| Parameter | Quantitative PCR (qPCR) | Digital PCR (dPCR) |
|---|---|---|
| Quantification Method | Relative (requires standard curve) | Absolute (no standard curve) |
| Sensitivity / Detection Limit | ~1% mutant allele frequency [9] | ~0.1% mutant allele frequency [9] [10] |
| Tolerance to PCR Inhibitors | Moderate; efficiency impacts Cq values significantly | High; partitioning reduces inhibitor effect [67] [11] |
| Precision | Broader dynamic range, but higher CV at low concentrations [11] | Superior precision, especially for low-abundance targets [18] [11] |
| Impact of Restriction Digestion | Can improve efficiency but does not overcome fundamental sensitivity limits | Markedly improves precision and reliability of copy number estimation [18] |
The Scientist's Toolkit: Essential Reagents for Restriction Enzyme-Based Assays
Table 3: Key Research Reagent Solutions
| Reagent / Tool | Function in Workflow | Application Note |
|---|---|---|
| Restriction Endonucleases | Sequence-specific fragmentation of gDNA to enhance target accessibility. | Selection is critical; HaeIII demonstrated superior precision over EcoRI in a comparative dPCR study [18]. |
| dPCR Master Mix | Proprietary buffer and enzyme formulation optimized for partitioning and amplification. | Formulations are often platform-specific (e.g., Bio-Rad, QIAGEN) due to precise partitioning requirements [67]. |
| Fluorophore-Labeled Probes | Target-specific detection (e.g., TaqMan, FRET probes). | Provides high specificity for allele discrimination in complex backgrounds [71] [11]. |
| Nucleic Acid Purification Kits | Isolation of high-quality, inhibitor-free gDNA from various sample matrices (e.g., FFPE, cells). | Essential for removing contaminants that could interfere with the restriction digestion or PCR steps [9] [73]. |
Workflow and Logical Pathway
The following diagram illustrates the logical workflow for utilizing restriction enzymes to improve target accessibility, from sample preparation to data analysis, and the consequent advantages for qPCR and dPCR.
The integration of restriction enzyme digestion into sample preparation protocols is a highly effective strategy for mitigating the challenges posed by complex genomic DNA. Experimental data confirms that this step significantly enhances the performance of PCR-based detection, with a more pronounced impact on the absolute quantification capabilities of dPCR. While qPCR remains a powerful tool with a broad dynamic range, dPCR's inherent advantages in sensitivity, precision, and tolerance to inhibitors are further amplified through optimized DNA fragmentation [18] [67] [11]. For researchers and drug development professionals focused on detecting low-abundance mutant alleles—where accuracy is paramount for diagnostic and therapeutic decision-making—the combination of restriction enzyme-based sample preparation and dPCR technology represents a superior and robust solution.
In molecular biology, the reliability of quantitative PCR (qPCR) and digital PCR (dPCR) data is paramount, especially in sensitive applications like detecting low-abundance mutant alleles in cancer research. To address this, the Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines were established in 2009 to standardize the design, execution, and reporting of qPCR experiments [74]. As dPCR technology emerged, the digital MIQE (dMIQE) guidelines were introduced in 2013 to provide a similar framework for this powerful quantification technology [75]. These guidelines aim to ensure experimental reproducibility, reliability, and transparency, allowing other scientists to critically evaluate and independently verify reported results. For researchers comparing dPCR and qPCR for detecting mutant alleles, adherence to these guidelines is not merely a publication formality but a fundamental component of robust scientific practice, ensuring that performance comparisons between the technologies are valid and meaningful.
The MIQE and dMIQE Frameworks
Core Principles and Recent Updates
The MIQE and dMIQE guidelines are built on the principle that transparent, clear, and comprehensive reporting of all experimental details is necessary to ensure the repeatability and reproducibility of PCR results [74]. They provide a checklist of essential information that must accompany any publication of qPCR or dPCR data.
A significant recent development is the release of the MIQE 2.0 guidelines in 2025 [74]. This revision reflects the substantial advances in qPCR technology and its expansion into new domains. The updated guidelines offer clarified recommendations for sample handling, assay design, and validation, along with streamlined reporting requirements designed to help researchers provide all necessary information without undue burden. A key emphasis is on data analysis: MIQE 2.0 states that quantification cycle (Cq) values from qPCR should be converted into efficiency-corrected target quantities and reported with prediction intervals [74]. Furthermore, the guidelines encourage instrument manufacturers to enable the export of raw data to facilitate thorough re-evaluation by reviewers and other researchers.
The Digital PCR Supplement: dMIQE
The dMIQE guidelines, published in 2013, address the unique requirements of dPCR [75]. dPCR works by partitioning a PCR sample into thousands of individual reactions, such that a subset contains the target molecule(s). After end-point amplification, the fraction of positive reactions is counted, and the absolute concentration of the target is calculated using Poisson statistics [76] [9]. This process allows for absolute quantification without the need for standard curves and enables the detection of rare variants with high precision. The dMIQE guidelines provide a framework for reporting the critical parameters specific to this technology, such as partition count, occupancy and rejection rates, and the statistical methods used for concentration determination [75].
The workflow differences between the two techniques are fundamental and are illustrated below.
Comparative Analysis of dPCR and qPCR
Technical and Performance Differences
The choice between dPCR and qPCR is application-dependent, as each technology has distinct strengths and limitations [10] [76]. The core difference lies in quantification method: qPCR is a relative method, requiring a standard curve or reference samples, while dPCR provides absolute quantification without the need for external standards [10]. This makes dPCR particularly advantageous for detecting rare genetic events, such as mutant alleles in a background of wild-type DNA, due to its superior sensitivity and precision [9].
The following table summarizes the key characteristics of each technology.
Table 1: A Comparative Overview of qPCR and dPCR Characteristics
| Feature | Quantitative PCR (qPCR) | Digital PCR (dPCR) |
|---|---|---|
| Quantification Type | Relative (requires standard curve) [10] | Absolute (no standard curve needed) [10] |
| Reaction Format | Bulk reaction [10] | Partitioned into thousands of nanoliter reactions [10] [9] |
| Data Collection | Measures amplification in real-time, cycle-by-cycle [10] | End-point measurement of positive/negative partitions [10] |
| Tolerance to PCR Inhibitors | Lower sensitivity; prone to inhibitors [10] | Higher tolerance / increased robustness [10] |
| Impact of Amplification Efficiency | Data collected at exponential phase is impacted by efficiency changes [10] | Unaffected by changes in amplification efficiency [10] |
| Detection of Rare Mutations | Detects mutation rates typically >1% [10] | Detects mutation rates as low as ≥ 0.1% [10] [9] |
| Key Applications | Gene expression analysis, pathogen detection, microbiome analysis [10] | Copy number variation, rare allele detection, liquid biopsy [10] [76] |
Application in Mutant Allele Detection: An Experimental Case Study
A direct comparison of dPCR and qPCR for detecting the epidermal growth factor receptor (EGFR) T790M mutation in non-small cell lung cancer (NSCLC) highlights dPCR's superior sensitivity for rare alleles [9]. This mutation is a critical biomarker for tyrosine kinase inhibitor (TKI) resistance, and its early detection is clinically significant.
1. Experimental Protocol and Sample Preparation:
- Plasmid Model: Researchers created plasmid samples with defined EGFR T790M mutation rates of 5%, 1%, 0.5%, and 0.1% in a background of wild-type sequences [9].
- Clinical Samples: Genomic DNA was extracted from 10 formalin-fixed paraffin-embedded (FFPE) NSCLC tumor samples using the QIAamp DNA FFPE Tissue kit. DNA concentration and purity (OD260/OD280 ratio between 1.92-1.97) were confirmed spectrophotometrically [9].
- qPCR Method: The ARMS-qPCR (Amplification Refractory Mutation System) was performed using a commercial EGFR mutations detection kit on a 7500 Real-Time PCR system. Thermocycling conditions were: 95°C for 5 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min [9].
- dPCR Method: Droplet digital PCR (ddPCR) was performed using a QX200 system. The 25 µL reaction mix included ddPCR master mix, primer-probe mix, and template. The sample was partitioned into ~20,000 droplets via a droplet generator. Thermocycling conditions were: 95°C for 10 min, followed by 40 cycles of 94°C for 30 sec and 58°C for 1 min, followed by a 98°C enzyme deactivation step [9].
2. Key Findings and Data Comparison: The results from the plasmid model and clinical samples are summarized in the table below.
Table 2: Experimental Results Comparing ARMS-qPCR and ddPCR for EGFR T790M Detection
| Sample Type | Mutation Rate | ARMS-qPCR Result | Droplet Digital PCR Result |
|---|---|---|---|
| Plasmid Model | 5% | Detected reliably [9] | Detected reliably (398 mutant copies) [9] |
| Plasmid Model | 1% | Detected reliably [9] | Detected reliably (57 mutant copies) [9] |
| Plasmid Model | 0.5% | Not reliably detected [9] | Detected reliably (24 mutant copies) [9] |
| Plasmid Model | 0.1% | Not detected [9] | Detected reliably (~6 mutant copies) [9] |
| Clinical Sample N006 | Wild-type by ARMS-qPCR | Not Detected (Wild-type call) [9] | Detected (7 mutant copies in 6,000 wild-type) [9] |
This study demonstrates that ddPCR can reliably detect mutation rates as low as 0.1%, a threshold below the typical capability of ARMS-qPCR [9]. Furthermore, its ability to identify a T790M mutation in a clinical sample that was classified as wild-type by ARMS-qPCR underscores its potential for early diagnosis of TKI resistance before it becomes clinically evident [9].
Essential Research Reagent Solutions
The following table details key materials and reagents required for performing MIQE- and dMIQE-compliant experiments, as exemplified in the cited studies.
Table 3: Key Research Reagents and Their Functions in PCR Experiments
| Reagent / Material | Function | Example from Literature |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolates high-quality DNA or RNA from complex biological samples. | QIAamp DNA FFPE Tissue Kit for genomic DNA from tissue samples [9]. |
| PCR Master Mix | Provides the core components for amplification: DNA polymerase, dNTPs, buffers, and MgCl₂. | ddPCR 2X Master Mix for digital PCR [9]. |
| Sequence-Specific Primers & Probes | Binds complementary target sequences to enable specific amplification and detection. | TaqMan Assays; primers and probes for EGFR T790M detection [9]. |
| Reference Dyes | Acts as an internal positive PCR control for reaction integrity. | VIC-labeled reference system in EGFR ARMS-qPCR kit [9]. |
| Digital PCR Partitioning Oil/Consumables | Creates the nanoliter-sized partitions required for absolute quantification in dPCR. | Droplet Generation Oil for the QX200 ddPCR system [9]. |
The MIQE and dMIQE guidelines are indispensable tools for ensuring the validity and reproducibility of PCR-based research, particularly in the demanding field of mutant allele detection. While qPCR remains a powerful, high-throughput, and cost-effective tool for many applications like gene expression and pathogen detection, dPCR offers distinct advantages for applications requiring absolute quantification, superior sensitivity, and the ability to detect rare genetic variants [10] [76]. The experimental evidence clearly shows that dPCR can detect mutant alleles at abundances as low as 0.1%, outperforming traditional qPCR methods and enabling earlier detection of resistance mutations in cancer [9]. As the field advances, adherence to these reporting guidelines will be crucial for generating reliable data, facilitating accurate comparisons between these complementary technologies, and ultimately driving scientific and clinical progress.
Data-Driven Decisions: Comparing Platform Precision and Clinical Validity
The accurate detection and quantification of low-frequency mutant alleles is a cornerstone of modern molecular diagnostics, with critical applications in cancer research, liquid biopsies, and monitoring treatment-resistant disease subclones. The central challenge lies in reliably distinguishing a minute number of mutant molecules against a vast background of wild-type DNA. This capability directly influences how scientists and drug development professionals detect residual disease, identify emerging resistance mutations, and assess treatment efficacy. Two primary technologies dominate this landscape: quantitative PCR (qPCR) and digital PCR (dPCR). While qPCR has long been the established workhorse for nucleic acid quantification, dPCR offers a fundamentally different approach to absolute quantification without the need for standard curves. This guide provides an objective, data-driven comparison of their performance characteristics—focusing on Limits of Detection (LOD) and Quantification (LOQ)—to inform method selection for detecting low-frequency mutants in research and clinical development.
Quantitative PCR (qPCR)
In qPCR, the entire reaction is run as a single, bulk mixture. The quantification cycle (Cq) at which the amplification curve crosses a fluorescence threshold is used to estimate the starting quantity of the target nucleic acid, relative to a standard curve run in parallel. Its performance for rare allele detection is ultimately constrained by the statistical noise of the wild-type background and the efficiency of the amplification reaction [16].
Digital PCR (dPCR)
Digital PCR takes a different approach by partitioning a single PCR reaction into thousands to millions of individual nanoreactions. After endpoint PCR amplification, each partition is analyzed as positive or negative for the target. The absolute number of target molecules in the original sample is then calculated using Poisson statistics based on the ratio of positive to negative partitions. This partitioning is the source of its power for rare allele detection, as it effectively dilutes the wild-type background and allows for the specific identification of rare mutant-positive partitions [35] [16].
The workflow and logical relationship for method selection is summarized in the diagram below.
Performance Comparison: LOD and LOQ in Focus
Defining LOD and LOQ
The Limit of Detection (LOD) is the lowest concentration of an analyte that can be reliably distinguished from a blank sample, but not necessarily quantified as an exact value. The Limit of Quantification (LOQ) is the lowest concentration that can be measured with acceptable precision and accuracy [77] [78]. For qPCR and dPCR, these limits define the lowest mutant allele frequency an assay can detect and precisely measure, which is paramount for applications like early cancer detection.
Comparative Performance Data
Direct comparisons in the literature demonstrate the superior sensitivity of dPCR for low-abundance targets. A study on EGFR mutations reported that dPCR could achieve an LOD of one mutant molecule in 180,000 wild-type molecules (0.00056%) when analyzing 3.3 μg of genomic DNA. By processing even larger amounts of DNA, the technology demonstrated the potential to detect down to one mutant in over 4 million wild-type molecules, a feat supported by an exceptionally low false-positive rate of one in 14 million [35]. In contrast, the same study noted that the LoD for a separate EGFR assay (T790M) was limited to approximately one mutant in 13,000 wild-type molecules (0.0077%) with a standard DNA input, highlighting that optimal sensitivity is both assay- and system-dependent [35].
A 2025 comparative study of dPCR platforms further quantified these metrics, reporting an LOD of approximately 0.17 copies/μL and an LOQ of 4.26 copies/μL for one ddPCR system, while a nanoplate-based dPCR system showed an LOD of 0.39 copies/μL and an LOQ of 1.35 copies/μL [18]. These findings underscore that while dPCR platforms generally offer high sensitivity, their specific performance can vary.
The table below summarizes key comparative data from the literature.
Table 1: Experimental LOD and LOQ Performance for Mutation Detection
| Target / Application | Technology | Reported LOD | Reported LOQ | Key Experimental Finding |
|---|---|---|---|---|
| EGFR L858R Mutation [35] | Droplet dPCR | 1 in 180,000 (0.00056%) | N/R | Potential for 1 in 4 million detection with high DNA input; False-positive rate: 1 in 14 million. |
| EGFR T790M Mutation [35] | Droplet dPCR | 1 in 13,000 (0.0077%) | N/R | LoD limited by assay performance and DNA input. |
| Synthetic Oligos [18] | Nanoplate dPCR | 0.39 copies/μL | 54 copies/reaction | Platform comparison shows variable LOD/LOQ. |
| Synthetic Oligos [18] | Droplet dPCR (QX200) | 0.17 copies/μL | 85.2 copies/reaction | Different platform showed different optimal LOQ. |
| Cyanobacteria Detection [58] | ddPCR | N/R | N/R | Lower variability and more precise/accurate for environmental samples vs qPCR. |
| Cyanobacteria Detection [58] | qPCR | N/R | N/R | Higher sensitivity and wider dynamic range vs ddPCR, but susceptible to inhibition. |
N/R = Not explicitly Reported in the source material
Detailed Experimental Protocols from Cited Studies
This protocol outlines the comprehensive process used to characterize the LOD for EGFR L858R and T790M assays.
- Assay Design: TaqMan MGB probes and primers were designed for the L858R mutation. For the T790M mutation, PrimeTime LNA-ZEN probes were used to enhance specificity. The amplicon lengths were 78 bp and 51 bp, respectively.
- Sample Preparation: Wild-type human genomic DNA was fragmented to ~3 kb. Synthetic, linearized plasmid DNA served as the mutant template. A titration series was created by spiking mutant plasmid into wild-type genomic DNA at ratios ranging from 0.5% down to 0.0005%. Each sample contained ~20,000 copies/μL of total DNA.
- dPCR Setup: The 50 μL PCR reactions included 1x TaqMan Genotyping Master Mix, 0.2 μM probes, 0.9 μM primers, 1x Droplet Stabilizer, and the prepared DNA sample. Reactions were performed on the RainDance RainDrop system.
- Data Analysis: The number of mutant-positive, wild-type-positive, and double-positive partitions was counted. The LOD was statistically determined with 95% confidence, incorporating data from wild-type-only replicates to establish the false-positive rate, which is critical for defining the ultimate sensitivity limit.
This study provides a model for a head-to-head methodology comparison, focusing on precision and inhibition resistance.
- Assay Design: Primers and hydrolysis probes were designed for genus-specific genes (rpoC1 for Cylindrospermopsis and cpcB for Microcystis). Specificity was verified in silico (BLASTN) and empirically against a panel of non-target cyanobacteria.
- Standard Preparation: Target genes were amplified from genomic DNA, cloned into plasmids, and linearized. Plasmid DNA was quantified via spectrophotometry to create standard curves with known gene copy numbers.
- Duplex PCR Setup: Identical primer-probe mixes were used for both qPCR and ddPCR. qPCR was run on a standard real-time cycler, while ddPCR was performed on a Bio-Rad QX200 droplet system.
- Data Analysis: For qPCR, quantification was based on standard curves. For ddPCR, absolute copy numbers were calculated from the fraction of positive droplets using Poisson statistics. The two techniques were compared based on linearity, quantitative correlation with standards, sensitivity, and performance with inhibited environmental samples.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials referenced in the featured experiments, which are essential for developing and running sensitive assays for low-frequency mutants.
Table 2: Key Research Reagent Solutions for Low-Frequency Mutation Detection
| Item | Function / Application | Specific Example from Literature |
|---|---|---|
| Hydrolysis Probes (TaqMan) | Sequence-specific detection of target alleles during amplification. | TaqMan MGB probes for EGFR L858R [35]. |
| Specialized Probes (LNA/ZEN) | Enhance allele discrimination and binding affinity for difficult targets or to lower background. | PrimeTime LNA-ZEN probes for EGFR T790M [35]. |
| Synthetic DNA Templates | Serve as well-characterized positive controls and for creating standard dilution series for LOD/LOQ studies. | Linearized GeneArt plasmid templates for EGFR mutations [35]. |
| Digital PCR Master Mix | Optimized polymerase and buffer system for efficient amplification in partitioned reactions. | TaqMan Genotyping Master Mix used in RainDrop dPCR system [35]. |
| Restriction Enzymes | Digest genomic DNA to improve accessibility to target sequences, which can enhance assay precision. | HaeIII and EcoRI tested for gene copy number quantification in protists [18]. |
The body of evidence consistently demonstrates that digital PCR holds a significant advantage for applications requiring the utmost sensitivity in detecting low-frequency mutants, often outperforming qPCR by one to two orders of magnitude. dPCR's partitioning principle provides superior resilience to PCR inhibitors and enables absolute quantification without standard curves, making it particularly suited for analyzing challenging sample types like cell-free DNA in liquid biopsies.
However, qPCR remains a powerful and fit-for-purpose technology. It offers a wider dynamic range, higher throughput, faster turnaround times, and lower per-test costs [16]. The choice between them is not a simple declaration of a "winner" but a strategic decision based on the specific requirements of the research or diagnostic question. For initial screening where extreme sensitivity is not critical, qPCR is often optimal. For the detection and precise quantification of very rare mutations (e.g., below 0.1%), particularly in complex matrices, dPCR is currently the undisputed technology of choice. As both technologies continue to evolve, trends point toward increased multiplexing, advanced data analysis, and a push toward practical point-of-care applications, further solidifying their role in advancing genomics and molecular medicine [16].
In molecular biology research, particularly in sensitive applications like detecting mutant alleles, the precision of quantification methods is paramount. Coefficient of Variation (CV), defined as the standard deviation divided by the mean and expressed as a percentage, serves as a key metric for evaluating this precision [40]. This guide provides an objective comparison of precision between quantitative PCR (qPCR) and digital PCR (dPCR), focusing on their performance in quantifying nucleic acids across different experimental scenarios. While qPCR measures amplification in real-time during the exponential phase, dPCR utilizes sample partitioning and end-point detection to enable absolute quantification without standard curves [10]. The partitioning-based nature of dPCR fundamentally enhances its precision, especially for detecting low-abundance targets [23].
Fundamental Principles of CV in PCR Replicates
Understanding Coefficient of Variation (CV)
In PCR data analysis, the Coefficient of Variation (CV) provides a standardized measure of precision that enables meaningful comparison between datasets with different means [40]. It is calculated as:
- CV (%) = (Standard Deviation / Mean) × 100
A lower CV value indicates higher precision and less variability among replicate measurements [40]. For both qPCR and dPCR, monitoring CV is essential for assessing data quality, as excessive variability can compromise the ability to detect true biological differences, potentially leading to false negatives or false positives [40].
Types of Replicates and Their Impact on Precision
Both qPCR and dPCR workflows utilize replicates to estimate and improve precision, but these replicates serve distinct purposes:
Technical Replicates: Multiple measurements of the same biological sample to account for instrumentation and pipetting variability [40]. These help estimate system precision and identify potential outliers.
Biological Replicates: Measurements from different samples within the same experimental group to capture natural biological variability [40].
The strategic use of replicates balances cost against the need for precision, with triplicate technical replicates being common in basic research [40].
Comparative Analysis of Precision Between qPCR and dPCR
Quantitative Comparison of Precision Metrics
Table 1: Direct comparison of precision and performance metrics between qPCR and dPCR
| Parameter | qPCR | dPCR |
|---|---|---|
| Typical CV Range | Higher intra-assay variability [23] | Lower intra-assay variability (e.g., median 4.5% CV) [23] |
| Detection Limit for Mutant Alleles | >1% mutation rate [10] | ≥0.1% mutation rate [10] |
| Quantification Method | Relative (requires standard curve) or absolute with standards [40] [10] | Absolute (no standard curve needed) [10] |
| Impact of PCR Inhibitors | More susceptible [10] | Higher tolerance [10] |
| Effect of Amplification Efficiency | Sensitive to efficiency variations [10] | Less affected by efficiency changes [10] |
| Statistical Foundation | Based on Cq values and standard curves [40] | Poisson statistics applied to partitioned samples [23] |
Experimental Evidence from Comparative Studies
Recent research directly comparing both technologies demonstrates dPCR's superior precision for detecting low-abundance targets. A 2025 study comparing multiplex dPCR and qPCR for detecting periodontal pathobionts found dPCR exhibited significantly lower intra-assay variability (median CV: 4.5%) compared to qPCR [23]. Additionally, dPCR demonstrated superior sensitivity for detecting low bacterial loads, particularly for P. gingivalis and A. actinomycetemcomitans [23].
Bland-Altman analysis in this study revealed good agreement between the technologies at medium to high target concentrations but notable discrepancies at low concentrations (<3 log₁₀ Geq/mL), where qPCR produced false negatives [23]. This enhanced detection capability at low concentrations is particularly relevant for mutant allele detection, where dPCR's ability to detect mutation rates as low as 0.1% provides a significant advantage over qPCR's approximate 1% detection limit [10].
Experimental Protocols for Precision Assessment
qPCR Protocol for Precision Measurement
Table 2: Key research reagents for qPCR-based library quantification
| Reagent/Tool | Function | Example Product |
|---|---|---|
| SYBR Green Master Mix | Fluorescent detection of amplified DNA | KAPA SYBR FAST qPCR Master Mix [79] |
| Platform-Specific Primers | Target-specific amplification | KAPA Library Quantification Primer Premix [79] |
| DNA Standards | Generation of standard curve for quantification | Pre-diluted DNA Standards [79] |
| Passive Reference Dye | Normalization of fluorescent signals | ROX dye [40] [79] |
Standard Protocol:
- Reaction Setup: Prepare triplicate reactions containing 2X SYBR FAST Master Mix, 10X primer premix, and template DNA in a total volume of 20 µL [79].
- Thermocycling Conditions: Initial denaturation at 95°C for 10 minutes, followed by 40 cycles of 95°C for 10 seconds and 60°C for 45 seconds [79].
- Data Collection: Monitor fluorescence during the annealing/extension step of each cycle [79].
- Analysis: Determine Cq values, generate standard curve by plotting average Cq against known standard concentrations, and calculate target concentrations from the curve [79].
- Precision Calculation: Compute CV% from technical replicates to assess precision [40].
Critical Considerations: Maintain consistent pipetting technique, avoid optical mixing by keeping sample volume below 20% of total reaction volume, and ensure proper plate sealing and centrifugation [40].
dPCR Protocol for Precision Measurement
Standard Protocol (Adapted from nanoplate-based dPCR):
- Reaction Setup: Prepare 40 µL reaction mixtures containing 4X Probe PCR Master Mix, 0.4 µM of each primer, 0.2 µM of each probe, restriction enzyme, and template DNA [23].
- Partitioning: Load mixture into nanoplate wells for automated partitioning into approximately 26,000 partitions [23].
- Thermocycling: Initial denaturation/enzyme activation at 95°C for 2 minutes, followed by 45 cycles of 95°C for 15 seconds and 58°C for 1 minute [23].
- Endpoint Detection: Image partitions on appropriate fluorescence channels to identify positive and negative reactions [23].
- Poisson Analysis: Apply Poisson statistics to calculate absolute target concentration, using Volume Precision Factor for improved accuracy [23].
Critical Considerations: Optimize primer and probe concentrations during assay development, optimize imaging thresholds and exposure times for each fluorescence channel, and test sample dilutions to avoid positive fluorescence signal saturation [23].
Factors Influencing Precision in qPCR and dPCR
Understanding the factors affecting precision is crucial for optimizing experiments. The precision of both qPCR and dPCR is influenced by three main variation types [40]:
System Variation: Inherent to the measurement system, including pipetting variation and instrument-derived variability [40]. dPCR typically demonstrates lower system variation due to its partitioning approach, which minimizes the impact of pipetting errors through massive parallelization [10].
Biological Variation: Represents true variation in target quantity among samples within the same group [40]. This affects both technologies similarly, though dPCR's sensitivity may reveal biological variation that qPCR cannot detect.
Experimental Variation: The measured variation for samples belonging to the same group, used to estimate biological variation [40]. System variation impacts experimental variation more significantly in qPCR than in dPCR.
Strategies for Improving Precision
For qPCR:
- Implement regular instrument maintenance and performance verification [40]
- Employ good pipetting technique with calibrated equipment [40]
- Use multiplexing with passive reference dyes for normalization [40]
- Apply the twenty-percent rule to prevent optical mixing [40]
- Ensure proper plate sealing and centrifugation [40]
For dPCR:
- Optimize partition number based on target concentration [23]
- Validate imaging parameters for each fluorescence channel [23]
- Utilize Volume Precision Factor for improved concentration calculations [23]
- Apply appropriate dilution factors to avoid saturation [23]
Advanced Applications in Mutant Allele Detection
Special Considerations for Ratiometric Assays
In ratiometric assays such as mutant allele detection, precision measurement requires specialized approaches. For dPCR, the MOVER approximated CV (CVMA) provides a method for assessing ratio precision without technical replicates [80]. The CVMA is calculated as:
- CVMA = [(Upper 95% CI - Lower 95% CI) / (2 × 1.96 × ratio)]
This method leverages the confidence interval around the ratio estimate generated by dPCR software, converting it to a CV equivalent that correlates well with traditional CV calculated from replicates [80]. A CVMA threshold of ≤30% is generally considered acceptable for ratiometric assays [80].
Application-Specific Performance
dPCR demonstrates particular advantages for mutant allele detection due to:
- Enhanced Sensitivity: Ability to detect rare mutants present at frequencies as low as 0.1% [10]
- Superior Precision at Low Concentrations: Lower CV values enable more reliable detection of minimal residual disease [23]
- Tolerance to Inhibitors: Reduced susceptibility to PCR inhibitors in complex clinical samples [10]
- Absolute Quantification: No need for standard curves, improving reproducibility across laboratories [10]
The comparative analysis of CV in qPCR and dPCR replicates demonstrates that dPCR generally offers superior precision, particularly for applications requiring detection of low-abundance targets such as mutant alleles. While qPCR remains a robust and well-established technology suitable for many applications, dPCR's partitioning approach, reduced susceptibility to amplification efficiency variations, and absolute quantification capability provide distinct advantages for precision-critical applications. The choice between technologies should be guided by specific application requirements, with dPCR being particularly valuable for detecting rare mutations, analyzing copy number variations, and applications demanding the highest level of quantification precision.
Digital PCR (dPCR) represents a significant advancement in nucleic acid quantification, enabling absolute quantification of target molecules without requiring standard curves. This technology partitions a PCR reaction into thousands of individual reactions, allowing precise counting of target molecules using Poisson statistics [22]. Two primary partitioning methodologies have emerged: droplet-based dPCR (ddPCR), which encapsulates reactions in water-in-oil emulsions, and nanoplate-based dPCR (ndPCR), which distributes reactions across nanoscale chambers on a solid chip [22]. While both approaches share the same fundamental principle, their technical differences may impact performance in critical applications such as detecting rare mutant alleles in cancer research [22] [29].
Understanding the consistency between these platforms is essential for molecular diagnostics, particularly as dPCR gains prominence in clinical applications like liquid biopsy, minimal residual disease monitoring, and infectious disease quantification [22]. This comparison guide objectively evaluates the performance characteristics of droplet-based and nanoplate-based dPCR systems through published experimental data, providing researchers with evidence-based insights for platform selection.
Fundamental Technological Differences
The core distinction between droplet-based and nanoplate-based systems lies in their partitioning mechanisms and fluidic handling. In droplet-based systems (e.g., Bio-Rad QX200), microfluidic circuits generate monodisperse water-in-oil droplets, typically producing 20,000 droplets per sample at picoliter volumes [81]. These droplets function as independent PCR microreactors, requiring careful stabilization with surfactants to prevent coalescence during thermal cycling [22]. Fluorescence detection occurs via in-line reading as droplets flow single-file past a detector.
In contrast, nanoplate-based systems (e.g., QIAGEN QIAcuity) use microfabricated chips with fixed nanoscale wells, typically generating 8,500-10,000 partitions per sample [18] [81]. These systems employ closed-channel microfluidics for automated partition generation and endpoint imaging for fluorescence detection [82]. The solid-state nature of nanoplates eliminates concerns about droplet stability but offers less flexibility in partition count.
Table 1: Core Technological Specifications of dPCR Platforms
| Parameter | Droplet-based dPCR (ddPCR) | Nanoplate-based dPCR (ndPCR) |
|---|---|---|
| Partition Type | Water-in-oil droplets | Nanoscale wells/chambers |
| Typical Partition Count | ~20,000 droplets [81] | ~8,500 partitions [81] |
| Partition Volume | Picoliter range [22] | Nanoliter range |
| Readout Method | In-line droplet streaming [22] | Endpoint planar imaging [22] |
| Automation Level | Manual droplet generation | Integrated fluidic handling [82] |
| Sample Dead Volume | Higher [83] | Lower [83] |
Performance Comparison: Sensitivity, Precision, and Agreement
Limits of Detection and Quantification
Multiple studies have systematically compared the sensitivity of ddPCR and ndPCR platforms. In a comprehensive evaluation using synthetic oligonucleotides, the limit of detection (LOD) for ndPCR was approximately 0.39 copies/µL input, compared to 0.17 copies/µL input for ddPCR [18]. However, the limit of quantification (LOQ) showed an inverse pattern, with ndPCR demonstrating better quantification at lower concentrations (1.35 copies/µL input versus 4.26 copies/µL input for ddPCR) [18]. This suggests that while ddPCR might have slightly better detection capabilities, ndPCR provides more reliable quantification near the detection limit.
In environmental testing applications for water quality assessment, both platforms demonstrated comparable 95% LODs ranging between 4.5-10 target copies per reaction across three different bacterial assays (HF183/BacR287, Entero1a, and EC23S857) [83]. The consistency in LOD values across platforms indicates that both technologies can deliver similar sensitivity for well-optimized assays.
Precision and Accuracy
Precision, measured by coefficient of variation (CV), is a critical parameter for applications requiring detection of small fold-changes. Both platforms demonstrate high precision across most concentration ranges, with CVs typically below 15% for concentrations above the LOQ [18]. However, the choice of restriction enzymes significantly impacts precision, particularly for ddPCR. One study found that using HaeIII instead of EcoRI dramatically improved ddPCR precision, reducing CVs from >60% to <5% for certain sample types [18]. ndPCR showed less variability between restriction enzymes, suggesting potentially more robust performance across different assay conditions [18].
In DNA methylation analysis comparing the two platforms, both demonstrated excellent precision with specificity ≥99.62% and sensitivity ≥98.03% for detecting methylated CDH13 genes in breast cancer tissue [81]. The quantitative methylation levels showed strong correlation between platforms (r = 0.954), indicating high inter-platform reproducibility for methylation-specific assays [81].
Table 2: Quantitative Performance Metrics from Comparative Studies
| Performance Metric | Droplet-based dPCR (ddPCR) | Nanoplate-based dPCR (ndPCR) | Study Context |
|---|---|---|---|
| Limit of Detection | 0.17 copies/µL [18] | 0.39 copies/µL [18] | Synthetic oligonucleotides |
| Limit of Quantification | 4.26 copies/µL [18] | 1.35 copies/μL [18] | Synthetic oligonucleotides |
| Typical CV Range | 6-13% [18] | 7-11% [18] | Above LOQ concentrations |
| Restriction Enzyme Impact | Significant (CV up to 62% with EcoRI) [18] | Moderate (CV up to 28% with EcoRI) [18] | Paramecium tetraurelia DNA |
| Quantitative Correlation | r = 0.954 with ndPCR [81] | r = 0.954 with ddPCR [81] | DNA methylation analysis |
Comparative Analysis of Experimental Protocols
The methodological approaches from key comparative studies reveal standardized procedures for cross-platform evaluation:
Nucleic Acid Extraction and Preparation: In DNA methylation studies comparing dPCR platforms, researchers isolated genomic DNA from formalin-fixed paraffin-embedded (FFPE) breast cancer tissues using the DNeasy Blood and Tissue Kit (Qiagen) [81]. DNA concentrations were quantified using fluorometric methods (Qubit 3.0 with dsDNA BR Assay), followed by bisulfite conversion using the EpiTect Bisulfite Kit (Qiagen) to distinguish methylated from unmethylated cytosine residues [81].
Assay Design and Optimization: For the CDH13 methylation assay, researchers designed primers and probes to target three specific CpG sites in the promoter region using MethPrimer and Primer3Plus software [81]. The assay simultaneously detected methylated (FAM-labeled) and unmethylated (HEX-labeled) sequences in a single reaction, with identical primer sequences for both targets and differential probes to distinguish methylation status [81].
Reaction Setup and Thermal Cycling: Typical 12μL ndPCR reactions contained 3μL of 4× Probe PCR Master Mix, 0.96μL of each primer, 0.48μL of each probe, and 2.5μL DNA template [81]. The cycling protocol included heat activation (95°C for 2min), followed by 40 cycles of denaturation (95°C for 15s) and combined annealing/extension (57°C for 1min) [81]. For ddPCR, 20μL reactions used 10μL of Supermix for Probes, 0.45μL of each primer and probe, and 2.5μL DNA template, with droplet generation followed by thermal cycling with initial denaturation (95°C for 10min) and 40 cycles (94°C for 30s, 57°C for 1min) [81].
Data Analysis and Threshold Setting: For ndPCR, the QIAcuity Software Suite automatically analyzed partitions, with thresholds manually set based on positive controls and binding specificity [81]. Acceptance criteria included >7,000 valid partitions and ≥100 positive partitions [81]. Methylation levels were calculated as the ratio of FAM-positive partitions to all positive partitions. For ddPCR, data were analyzed using Quantasoft software with similar quality metrics.
Practical Implementation Considerations
Workflow Efficiency and Operational Factors
Workflow differences significantly impact practical implementation in research and clinical settings. Nanoplate-based systems generally offer more streamlined workflows with integrated fluidic handling that automates partition generation, reducing manual steps and potential operator error [82]. The closed-system design also minimizes contamination risk. However, these systems typically have fixed partition counts, limiting flexibility for different application needs.
Droplet-based systems require separate droplet generation instruments, adding manual steps to the workflow [81]. However, they offer greater flexibility in partition numbers and the ability to generate droplets from larger sample volumes, which can be beneficial for rare target detection [84]. The requirement for careful droplet handling and potential stability concerns during thermal cycling represent operational considerations [22].
In environmental testing applications, the lower dead volume of ndPCR systems may provide better analytical sensitivity when template is limiting, as more loaded template is actually analyzed [83]. One study found that ndPCR detected HF183/BacR287 (a human fecal contamination marker) more frequently than ddPCR when target abundance was below 100 copies/100mL [83].
Application-Specific Performance
The optimal platform choice often depends on the specific application:
For DNA methylation analysis, both platforms perform excellently with strong correlation, suggesting that workflow considerations rather than performance differences should guide selection [81].
In environmental water testing, platform choice may impact results at very low target concentrations, with ndPCR potentially offering slight advantages for detection frequency near the LOD [83].
For gene copy number variation studies, restriction enzyme selection significantly impacts precision, particularly for ddPCR, suggesting more extensive optimization may be required for droplet-based systems [18].
In rare mutation detection (e.g., JAK2V617F in myeloproliferative neoplasms), ddPCR has demonstrated exceptional sensitivity with limit of quantification of 0.01% variant allele frequency, though direct cross-platform comparisons for this specific application are limited [29].
Table 3: Essential Research Reagent Solutions for dPCR Experiments
| Reagent Category | Specific Examples | Function in dPCR Workflow |
|---|---|---|
| Nucleic Acid Extraction Kits | DNeasy Blood & Tissue Kit (Qiagen) [81] | Isolation of high-quality DNA from various sample types including FFPE tissues |
| Bisulfite Conversion Kits | EpiTect Bisulfite Kit (Qiagen) [81] | Chemical conversion of unmethylated cytosines to uracils for methylation analysis |
| dPCR Master Mixes | QIAcuity 4× Probe PCR Master Mix [81]; Supermix for Probes (Bio-Rad) [81] | Optimized reaction components including polymerase, dNTPs, and buffers for partition amplification |
| Reference Materials | NIST SRM 2917 [83] | Certified plasmid DNA with known target copies for assay validation and quality control |
| Restriction Enzymes | HaeIII, EcoRI [18] | Enhance access to target sequences in complex genomes, improving precision and accuracy |
Based on comprehensive cross-platform evaluations, both droplet-based and nanoplate-based dPCR systems deliver highly comparable and reproducible results for most applications. The strong quantitative agreement (r = 0.954) observed in methylation studies [81] and similar precision metrics across platforms [18] suggest that both technologies can provide reliable data for research and clinical applications.
Platform selection should consider specific application requirements:
Choose nanoplate-based systems when workflow integration, ease of use, and consistent partition quality are priorities, particularly for clinical environments [82]. The automated fluidic handling and lower dead volume may also provide benefits when working with limited samples [83].
Choose droplet-based systems when maximum partition numbers, protocol flexibility, or established laboratory protocols are key considerations. The ability to generate more partitions can be beneficial for rare mutation detection [29] and applications requiring high dynamic range.
For detecting mutant alleles in cancer research, both platforms demonstrate sufficient sensitivity and precision, though assay optimization—particularly restriction enzyme selection for ddPCR—is crucial for optimal performance [18]. The consistency between platforms supports the growing implementation of dPCR in molecular diagnostics and provides confidence in comparing results across different laboratory settings.
Digital PCR (dPCR) represents a transformative advancement in molecular diagnostics for bloodstream infections (BSIs). Clinical studies consistently demonstrate that dPCR exhibits significantly higher sensitivity and a drastically shorter turnaround time compared to conventional blood culture, while also providing absolute quantification of pathogen load. This capability is crucial for rapid diagnosis and early intervention in life-threatening conditions such as sepsis.
Quantitative Comparison: dPCR vs. Blood Culture
The following table summarizes key performance metrics from recent clinical studies directly comparing dPCR and blood culture methodologies.
Table 1: Performance Metrics of dPCR versus Blood Culture in Clinical Studies
| Study Population | Sample Size | dPCR Positivity Rate | Blood Culture Positivity Rate | dPCR Sensitivity | dPCR Specificity | Turnaround Time (dPCR vs. BC) |
|---|---|---|---|---|---|---|
| Suspected infections [85] [86] | 149 patients | 28.2% (42/149) | 4.0% (6/149) | 83.3%* | 74.0%* | ~4.8 hours vs. ~94.7 hours |
| Critically ill patients with suspected BSIs [87] | 60 episodes | 83.3% (50/60) | 16.7% (10/60) | 90.0% | N/R | ~4 hours vs. ~48-72 hours |
| ICU patients with suspected BSIs [88] | 438 episodes | 41.1% (180/438) | 9.1% (40/438) | 72.5%* | 63.1%* | ~2.5 hours vs. ~24-120 hours |
| ICU patients suspected of sepsis [89] | 69 patients | 73.9% (51/69) | 27.5% (19/69) | 63.2% | N/R | N/R |
Against blood culture as reference standard. *9 out of 10 culture-positive episodes were identified by dPCR [87]. N/R = Not Reported.
Detailed Experimental Data and Protocols
Key Study on Broad Pathogen Detection
A 2025 retrospective study of 149 patients with suspected infections provides compelling evidence for dPCR's superior sensitivity [85] [86].
Table 2: Pathogen Detection Profile from a 149-Patient Study [85] [86]
| Detection Metric | Digital PCR (dPCR) | Blood Culture (BC) |
|---|---|---|
| Positive Specimens | 42 | 6 |
| Total Pathogen Strains Detected | 63 | 6 |
| Species Diversity | 13 species (8 bacteria, 2 fungi, 3 viruses) | 5 species |
| Polymicrobial Infections | 14 cases | Not reported |
| Pathogen Concentration Range | 25.5 - 439,900 copies/mL | N/A |
Experimental Protocol [85] [86]:
- Sample Collection: Venous blood samples were collected in EDTA tubes using standard aseptic procedures.
- Plasma Separation: Plasma was immediately separated via centrifugation at 1,600 × g for 10 minutes.
- DNA Extraction: Plasma DNA was extracted using commercial nucleic acid purification kits and an automated purification system.
- dPCR Assay: 15 μL of extracted DNA was added to a pre-mixed reaction dry powder containing fluorescent probes and primers. The mixture was partitioned into droplets using a droplet digital PCR system.
- Amplification & Analysis: PCR amplification was performed, followed by droplet analysis using a chip scanner across six fluorescence channels. Data were analyzed using dedicated software.
Detection of Antimicrobial Resistance (AMR) Genes
dPCR's capability extends beyond pathogen identification to the detection of critical resistance genes, enabling precision treatment. A study on Acinetobacter baumannii developed a dual ddPCR assay targeting the species-specific gene gltA and the carbapenem resistance gene OXA-23 [90].
- Performance: The assay demonstrated a limit of detection (LOD) of 3 × 10⁻⁴ ng/μL, tenfold more sensitive than quantitative PCR (qPCR). It showed 100% concordance with blood culture and drug sensitivity tests when applied to 35 clinical BSI patients [90].
- Broader AMR Detection: Another prospective ICU study identified 40
blaKPC, 3blaNDM, and 38mecAgenes using a multiplex dPCR panel, providing rapid resistance profiling within hours [88].
The Scientist's Toolkit: Essential Research Reagents
The table below details key reagents and their functions for implementing dPCR in pathogen detection research.
Table 3: Key Research Reagent Solutions for dPCR-Based Pathogen Detection
| Reagent / Material | Function / Application | Examples / Specifications |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of microbial DNA from whole blood or plasma | Magnetic serum/plasma DNA kits; Column-based methods [85] [87] |
| dPCR Supermix | Provides optimized buffer, enzymes, and nucleotides for partition-based PCR | ddPCR Supermix for Probes (No dUTP) [90] |
| Primer/Probe Sets | Target-specific amplification and detection | TaqMan probes labeled with FAM, HEX, etc., for multi-channel detection [85] [90] |
| Droplet Generation Oil | Creates stable water-in-oil emulsion for partitioning samples | Commercial droplet generation oil [90] |
| Positive Control Materials | Validates assay performance and limits of detection | Synthesized DNA fragments; DNA from reference microbial strains [90] [88] |
dPCR Workflow for Bloodstream Pathogen Detection
The following diagram illustrates the streamlined workflow from sample collection to result analysis in dPCR-based pathogen detection.
Impact of Prior Antibiotic Therapy
A significant advantage of dPCR is its resilience to pre-sampling antibiotic use, which often inhibits microbial growth in culture. In a study of 144 patients, prior antibiotic treatment significantly reduced blood culture positivity from 42.9% to 27.2%, whereas the positivity rate of a PCR-based method (Sepsis@Quick) was unaffected (57.1% vs. 69.1%) [91]. This confirms that molecular detection of pathogen DNA remains effective even after antibiotic administration, making it a more reliable tool for patients who have already received empirical treatment.
Robust clinical validation data firmly establishes digital PCR as a superior methodological alternative to blood culture for the rapid and sensitive detection of bloodstream pathogens. Its significantly higher detection rates, quantitative results, rapid turnaround time, and capacity to identify antimicrobial resistance markers directly from blood samples make dPCR an indispensable tool for modern clinical microbiology and sepsis research. The integration of dPCR into diagnostic workflows can facilitate earlier targeted therapy, improve antibiotic stewardship, and potentially enhance patient outcomes in life-threatening infections.
The evolution of polymerase chain reaction (PCR) technology from conventional to quantitative real-time PCR (qPCR) and now to digital PCR (dPCR) has provided researchers with increasingly powerful tools for nucleic acid quantification. This advancement is particularly crucial in fields like oncology and infectious disease diagnostics, where detecting minute genetic variations—such as mutant alleles in a vast background of wild-type DNA—can determine treatment success [22]. While qPCR has served as the workhorse for molecular diagnostics for decades, dPCR's emergence offers a paradigm shift through its absolute quantification capability without the need for standard curves [10]. This guide provides an objective comparison of these technologies, focusing on the practical considerations of instrumentation, reagent costs, and workflow efficiency that inform platform selection for research and clinical applications, particularly in mutant allele detection.
The global market dynamics reflect this technological transition, with the dPCR and qPCR market valued at approximately $10.87 billion in 2024 and projected to reach $24.58 billion by 2035, growing at a compound annual growth rate (CAGR) of 7.70% [92]. dPCR is concentrated in applications requiring absolute quantification, such as liquid biopsy and rare mutation detection, with a market size of approximately $500 million, while qPCR maintains a broader presence across diverse applications with a market size of approximately $1.5 billion [93].
Technology Comparison: dPCR vs. qPCR
Fundamental Principles and Workflows
The core distinction between dPCR and qPCR lies in their quantification methods. qPCR relies on relative quantification by measuring amplification fluorescence during exponential phase and comparing to standards, while dPCR utilizes partitioning to enable absolute target counting through Poisson statistics [10].
Table 1: Fundamental Characteristics of qPCR versus dPCR
| Feature | Quantitative PCR (qPCR) | Digital PCR (dPCR) |
|---|---|---|
| Quantification Method | Relative, requires standard curve | Absolute, no standards needed |
| Data Collection | Real-time during exponential phase | End-point analysis |
| Reaction Format | Bulk reaction in single tube | Partitioned into thousands of reactions |
| Impact of PCR Efficiency | Significantly affected | Minimal impact |
| Tolerance to Inhibitors | Moderate | High |
| Mutation Detection Sensitivity | ~1% mutant allele frequency [9] | ~0.1% mutant allele frequency [9] [10] |
| Dynamic Range | Broad | Broad but may saturate at high concentrations [18] |
Diagram 1: qPCR vs. dPCR Workflows
Performance Comparison in Mutant Allele Detection
The superior sensitivity of dPCR for detecting low-abundance mutations has been demonstrated in multiple studies. A 2015 study comparing amplification refractory mutation system-based qPCR (ARMS-qPCR) and droplet digital PCR (ddPCR) for detecting EGFR T790M mutations in non-small cell lung cancer found that ddPCR reliably detected mutation rates as low as 0.1% (approximately 6 mutant copies in 6,000 wild-type copies), while ARMS-qPCR detection was limited to 1-5% mutation rates [9]. Critically, in clinical samples, one sample identified as wild-type by ARMS-qPCR showed a clear T790M mutation with ddPCR, demonstrating dPCR's enhanced sensitivity for detecting resistance mutations before clinical manifestation [9].
A 2025 study comparing dPCR and Real-Time RT-PCR for respiratory virus quantification found dPCR demonstrated superior accuracy, particularly for high viral loads of influenza A, influenza B, and SARS-CoV-2, and for medium loads of RSV, showing greater consistency and precision [6]. This precision advantage extends to copy number variation analysis, where dPCR's lower measurement variability provides significant benefits.
Table 2: Quantitative Performance Comparison
| Performance Metric | qPCR | dPCR | Experimental Context |
|---|---|---|---|
| Measurement Variability (%CV) | 5.0% [4] | 2.3% [4] | Human genomic DNA (175 cp/μL) |
| Precision with Pooled Replicates | 4.4% CV [4] | 1.5% CV [4] | Two replicates pooled/averaged |
| Limit of Detection (LOD) | Varies by assay (~1%) [9] | 0.17-0.39 copies/μL [18] | Synthetic oligonucleotides |
| Limit of Quantification (LOQ) | Dependent on standard curve | 54-85.2 copies/reaction [18] | Synthetic oligonucleotides |
| Detection Concordance | Reference standard | 91.7% with dPCR [12] | EGFR T790M in plasma cfDNA |
Experimental Protocols for Performance Validation
EGFR Mutation Detection Protocol
The following detailed methodology from the 2015 study comparing ARMS-qPCR and ddPCR for EGFR T790M mutation detection illustrates a direct performance comparison approach [9]:
Sample Preparation:
- Plasmid samples: Created by mixing T790M mutant plasmids with wild-type EGFR plasmid to yield 6, 30, 60, and 300 copies of mutant molecules in 6,000 wild-type molecules (0.1%, 0.5%, 1%, and 5% mutation rates)
- Clinical samples: Formalin-fixed paraffin-embedded (FFPE) tumor samples from NSCLC patients with tumor content ≥50% verified by hematoxylin and eosin staining
- DNA extraction: QIAamp DNA FFPE Tissue kit with concentration determination by Nanodrop 2000 spectrophotometer (OD260/OD280 ratio: 1.92-1.97)
ARMS-qPCR Protocol:
- Kit: Human EGFR Gene Mutations Detection kit (detecting 29 common EGFR mutations)
- Platform: 7500 Real Time PCR System (Applied Biosystems)
- Reaction volume: Not specified, templates adjusted to 10 ng/μL concentration
- Thermocycling conditions: 95°C for 5 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min
- Detection: Mutation assays labeled with FAM, positive PCR control labeled with VIC
Droplet Digital PCR Protocol:
- Platform: QX200 Droplet Digital PCR System (Bio-Rad)
- Reaction volume: 25 μL (12.5 μL ddPCR 2X Master mix, 1.25 μL 20X primer/TaqMan Probe mix, 8.75 μL nuclease-free water, 2.5 μL template)
- Droplet generation: 20 μL sample + 70 μL droplet generation oil via droplet generator
- Thermocycling: 95°C for 10 min, 40 cycles of 94°C for 30 sec and 58°C for 1 min, 98°C for 10 min, then hold at 4°C
- Analysis: Droplet reading and Poisson statistical analysis for absolute quantification
Precision Performance Comparison Protocol
A technical note from Stilla Technologies compared the precision performance of Crystal Digital PCR (cdPCR) using the Naica System to qPCR [4]:
Experimental Design:
- Sample type: Single unique PCR master mix spiked with 175 cp/μL human genomic DNA
- Target gene: Albumin (ALB)
- Replication: 23 technical replicates for each technology
- Volume: 25 μL for both techniques
- Operator: Same experimenter to reduce variability
qPCR Methodology:
- Standard curves: Generated from same DNA matrix as experimental samples
- Efficiency validation: R² ≥ 0.990, efficiency of 98.1% (R² = 0.991) obtained
- Analysis: Comparative Cq method with standard curve quantification
Crystal Digital PCR Methodology:
- Partitioning: Droplet generation with average of 26,299 droplets per sample
- Quantification: Direct absolute quantification without standard curve
- Analysis: Crystal Miner software for positive/negative cluster determination
Cost-Benefit Analysis: Instrumentation and Reagents
Instrumentation and Workflow Considerations
The selection between dPCR and qPCR involves balancing performance requirements with economic practicalities. dPCR systems generally require higher initial investment than qPCR platforms, potentially limiting accessibility for some laboratories [92]. However, this cost differential is narrowing with newer systems, and the value proposition must consider the total workflow efficiency and required performance specifications.
Table 3: Workflow and Throughput Comparison
| Characteristic | qPCR | dPCR |
|---|---|---|
| Setup Time | Minimal, established protocols | Moderate, partitioning step adds time |
| Automation Potential | High, well-established | Varies by platform (nanoplate systems offer higher automation) |
| Data Analysis Complexity | Moderate, standard curve dependent | Moderate, Poisson statistics and threshold setting |
| Sample Throughput | High, 96-well or 384-well standard | Moderate to high (nanoplate systems: 96-well equivalent) |
| Hands-on Time | Low | Moderate, though decreasing with automation |
| Multiplexing Capability | Established | Improving with newer systems |
Diagram 2: Cost-Benefit Decision Factors
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Essential Research Reagents and Materials
| Item | Function | Application Notes |
|---|---|---|
| DNA Extraction Kits (QIAamp, MagMax) | Isolation of high-quality nucleic acids from various sample types | Critical for both technologies; sample purity affects qPCR more significantly [9] [6] |
| Probe-Based Master Mixes | Fluorescent detection of specific targets | Essential for both technologies; dPCR requires specialized partitioning-compatible mixes [9] [4] |
| Reference Standard Materials | Calibration curve generation for qPCR | Required for qPCR relative quantification; not needed for dPCR absolute quantification [10] |
| Partitioning Oil/Reagents | Generation of nanoliter droplets or chambers | dPCR-specific consumable; quality critical for partition integrity [9] |
| Restriction Enzymes (EcoRI, HaeIII) | DNA digestion to improve target accessibility | Particularly important for dPCR analysis of complex genomes; enzyme choice affects precision [18] |
| Positive/Negative Controls | Assay validation and quality control | Essential for both technologies; dPCR often uses synthetic oligonucleotides as standards [18] |
Application-Specific Considerations and Future Directions
Selecting the Appropriate Technology
The choice between dPCR and qPCR should be guided by specific application requirements:
Choose dPCR when:
- Detecting rare mutations (<1% allele frequency) in oncology (e.g., T790M resistance mutation) [9] [12]
- Absolute quantification without standards is required [10]
- Working with challenging samples containing PCR inhibitors [10]
- High precision is needed for copy number variation or low-fold change detection [4]
- Liquid biopsy applications requiring sensitive detection of circulating tumor DNA [93]
Choose qPCR when:
- Budget constraints limit instrument acquisition [92]
- High-throughput routine testing with established targets is performed
- Broad dynamic range is more critical than detection limit
- Well-established protocols and assays exist for the target
- Point-of-care or decentralized testing is needed (with emerging portable systems)
Emerging Trends and Future Outlook
The dPCR and qPCR market continues to evolve with several key trends shaping future development. Automation and miniaturization of platforms are increasing throughput and reducing human error [92]. The integration of AI-driven analytics and machine learning in PCR workflows is optimizing data interpretation and efficiency [92]. There is also growing adoption of multiplex PCR assays allowing simultaneous detection of multiple targets, saving time and cost per analysis [93] [92].
For dPCR specifically, expansion into liquid biopsy and cancer mutation detection is enhancing its value proposition due to superior accuracy and sensitivity [92]. The development of lyophilized reagents and room-temperature-stable kits is facilitating point-of-care and decentralized testing applications [92]. As these trends continue, the cost-benefit calculus between dPCR and qPCR will likely shift further toward dPCR for an expanding range of applications, particularly in precision medicine and rare allele detection.
Conclusion
The choice between dPCR and qPCR for mutant allele detection is not one of superiority but of strategic application. qPCR remains a powerful, high-throughput, and cost-effective tool for screening and quantifying targets of moderate abundance. In contrast, dPCR excels in scenarios demanding the utmost sensitivity and absolute precision, such as detecting rare mutations, analyzing copy number variations with high resolution, and working with inhibitor-rich samples. Future directions point toward the increased integration of dPCR in clinical diagnostics for liquid biopsies, the standardization of assays across platforms, and its growing role in validating cell and gene therapies. For researchers and drug developers, understanding the distinct advantages of each technology is paramount for advancing precision medicine and achieving robust, reproducible results in genomic analysis.
References
- 1. Allele-Specific Quantitative PCR for Accurate, Rapid, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4931339/]
- 2. Absolute vs. Relative Quantification for qPCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/absolute-vs-relative-quantification-real-time-pcr.html]
- 3. Relative versus absolute RNA quantification [https://pmc.ncbi.nlm.nih.gov/articles/PMC7883443/]
- 4. Precision performance of Crystal Digital PCR vs. ... [https://www.stillatechnologies.com/digital-pcr/naica-system-analysis/precision-performance-of-crystal-digital-pcr-vs-quantitative-pcr/]
- 5. Real-time digital polymerase chain reaction (PCR) as a novel ... [https://tlcr.amegroups.org/article/view/59179/html]
- 6. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 7. A standard curve based method for relative real time PCR data processing | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-6-62]
- 8. A simple, accurate and universal method for quantification of PCR - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4784296/]
- 9. Comparison of droplet digital PCR and conventional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4353752/]
- 10. dPCR vs qPCR [https://www.qiagen.com/us/applications/digital-pcr/beginners/dpcr-vs-qpcr]
- 11. Comparison of Droplet Digital PCR and Quantitative PCR ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0159004]
- 12. Comparative analysis of QS3D versus droplet digital PCR ... [https://www.sciencedirect.com/science/article/pii/S2405844022026275]
- 13. Pairwise efficiency: a new mathematical approach to qPCR data analysis increases the precision of the calibration curve assay | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-019-2911-5]
- 14. Simple Absolute Quantification Method Correcting for Quantitative PCR Efficiency Variations for Microbial Community Samples - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370567/]
- 15. Digital Assays Part I: Partitioning Statistics and Digital PCR [https://www.sciencedirect.com/science/article/pii/S2472630322013334]
- 16. Quantitative or digital PCR? A comparative analysis for ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993624001584]
- 17. Digital PCR (dPCR) vs Real-Time PCR (qPCR) [https://firalismolecularprecision.com/2025/04/09/dpcr-qpcr-differences/]
- 18. Comparing the precision of two digital PCR applications for ... [https://www.nature.com/articles/s41598-025-13143-8]
- 19. Digital PCR for Rare Mutation Detection [https://www.thermofisher.com/us/en/home/life-science/pcr/digital-pcr/mutation-detection.html]
- 20. Digital PCR for Single-Cell Analysis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10886679/]
- 21. PCR-Based Methods for the Enrichment of Minority Alleles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2811432/]
- 22. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 23. Digital PCR outperforms quantitative real-time PCR for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288185/]
- 24. Methods for comparing multiple digital PCR experiments [https://pmc.ncbi.nlm.nih.gov/articles/PMC4983647/]
- 25. Digital PCR Market Size, Forecast Report [https://www.mordorintelligence.com/industry-reports/digital-pcr-market]
- 26. Understanding Ct Values in Real-Time PCR [https://www.thermofisher.com/blog/behindthebench/understanding-ct-values/]
- 27. What is a Ct Value and does it differ from qPCR Cq Values? [https://bitesizebio.com/24581/what-is-a-ct-value/]
- 28. The mathematics of qRT-PCR in virology [https://virologyresearchservices.com/2025/01/13/the-mathematics-of-qrt-pcr-in-virology/]
- 29. Laboratory-developed Droplet Digital PCR Assay for ... [https://www.sciencedirect.com/science/article/pii/S2699940425000190]
- 30. When to Choose Digital PCR vs. Real-Time PCR? [https://www.thermofisher.com/blog/behindthebench/when-to-choose-digital-pcr-vs-real-time-pcr/]
- 31. Performance Comparison of Droplet Digital PCR and Next- ... [https://pubmed.ncbi.nlm.nih.gov/40346007/]
- 32. What is Polymerase Chain Reaction (PCR) [https://www.addgene.org/protocols/pcr/]
- 33. PCR Cycling Parameters—Six Key Considerations for ... [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-cycling-considerations.html]
- 34. Dual-molecular barcode sequencing detects rare variants ... [https://www.nature.com/articles/s41598-020-60361-3]
- 35. Determining lower limits of detection of digital PCR assays ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5129438/]
- 36. qPCR vs. dPCR: Which Technology is Right for Your Lab? [https://avam.com/avam-articles/qpcr-vs-dpcr-which-technology-is-right-for-your-lab/]
- 37. Enhanced Ratio of Signals Enables Digital Mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4411249/]
- 38. Development and validation of a methylation-specific ... [https://www.nature.com/articles/s41598-025-15228-w]
- 39. A comparative analysis of high - throughput platforms for validation of... [https://www.nature.com/articles/srep10375?error=cookies_not_supported&code=d4ec44e8-f876-41a3-816c-3b7ba945968d]
- 40. Quantitative PCR (qPCR) Data Analysis [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/precision-qpcr.html]
- 41. Combination of fluorescence color and melting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3627564/]
- 42. Recommended dye combinations for multiplex qPCR [https://eu.idtdna.com/page/support-and-education/decoded-plus/recommended-dye-combinations-for-multiplex-qpcr/]
- 43. HEX (Hexachlorofluorescein) in Fluorophores [https://www.lumiprobe.com/t/fluorophores/hex]
- 44. What are the differences between PCR, RT-PCR, qPCR ... [https://www.enzo.com/note/what-are-the-differences-between-pcr-rt-pcr-qpcr-and-rt-qpcr/]
- 45. PCR vs qPCR vs RT-PCR vs RT-qPCR: What's the Difference [https://www.molsentech.com/post/pcr-vs-qpcr]
- 46. Evaluating the sensitivity of droplet digital PCR for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10903512/]
- 47. Comparative analysis of hybrid-SNP microarray and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288236/]
- 48. Digital droplet PCR is an accurate and precise method to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546813/]
- 49. dPCR vs. ddPCR: Why Precision Matters in Cell and Gene ... [https://www.roslinct.com/insights/dpcr-vs-ddpcr/]
- 50. Comparative study of tools for copy number variation ... [https://www.nature.com/articles/s41598-025-06527-3]
- 51. Next-Generation Sequencing CNV Detection & Analysis [https://bionano.com/blogs/next-generation-sequencing-cnv-detection-analysis/]
- 52. A Comparative Study of Medium-Coverage Genome ... [https://www.sciencedirect.com/science/article/pii/S1525157825001199]
- 53. Benchmarking scRNA-seq copy number variation callers [https://www.nature.com/articles/s41467-025-62359-9]
- 54. A Multiplex SNaPshot Assay as a Rapid Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3157611/]
- 55. Multiplex Detection of Hotspot Mutations by Rolling Circle- ... [https://www.sciencedirect.com/science/article/pii/S0023683722031889]
- 56. Single-Color Digital PCR Provides High-Performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6593258/]
- 57. Chip-based digital Polymerase Chain Reaction as ... [https://www.sciencedirect.com/science/article/pii/S2405844022026846]
- 58. of Comparison and Droplet Quantitative ... PCR Digital PCR Multiplex [https://pmc.ncbi.nlm.nih.gov/articles/PMC4495218/]
- 59. Rapid and Simultaneous Genotyping of Multiple Alleles in ... [https://www.nature.com/articles/s41598-020-59986-1]
- 60. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 61. MIQE Guidelines | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-assays/why-choose-taqman-assays/publish-real-time-pcr-results.html]
- 62. Validating Real-Time Polymerase Chain Reaction (PCR) Assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC7834634/]
- 63. An Internal Control for Routine Diagnostic PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC124832/]
- 64. Consensus guidelines for the validation of qRT-PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8792405/]
- 65. Multiplexed, universal probe-based rare variant detection ... [https://www.nature.com/articles/s41598-025-08814-5]
- 66. Evaluation of PCR-enhancing approaches to reduce ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969724069250]
- 67. When to Choose Quantitative PCR vs Digital PCR [https://kcasbio.com/blogs/quantitative-pcr-vs-digital-pcr-choosing-the-right-platform-for-bioanalysis/]
- 68. Digital PCR Applications | Thermo Fisher Scientific - ES [https://www.thermofisher.com/us/en/home/life-science/pcr/digital-pcr/applications.html]
- 69. Development and validation of a droplet digital PCR assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12061998/]
- 70. Assaying chromatin structure and remodeling by restriction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3607496/]
- 71. Restriction Enzymes as a Target for DNA-Based Sensing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6641459/]
- 72. Restriction Endonucleases in Genome Mapping and Analysis [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/molecular-cloning/restriction-enzymes/restriction-enzymes-genome-mapping.html]
- 73. Comparison of Digital PCR and Quantitative PCR with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9705847/]
- 74. MIQE 2.0: Revision of the Minimum Information for ... [https://pubmed.ncbi.nlm.nih.gov/40272429/]
- 75. The digital MIQE guidelines: Minimum Information for ... [https://pubmed.ncbi.nlm.nih.gov/23570709/]
- 76. Quantitative or digital PCR? A comparative analysis for ... [https://www.sciencedirect.com/science/article/pii/S0165993624001584]
- 77. Method Validation Essentials, Limit of Blank ... [https://www.biopharminternational.com/view/method-validation-essentials-limit-blank-limit-detection-and-limit-quantitation]
- 78. A tutorial for computing limits of detection and ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267021011685]
- 79. KAPA Library Quantification Kits [https://sequencing.roche.com/us/en/products/group/kapa-library-quantification-kits.html]
- 80. a tool for quantifying precision in ratiometric droplet digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8923918/]
- 81. Comparative Analysis of Two Digital PCR Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361875/]
- 82. Nucleic acid amplification tests in digital microfluidics [https://www.nature.com/articles/s41378-025-00977-5]
- 83. A Head-to-Head Comparison of Two Microfluidic Digital ... [https://www.preprints.org/manuscript/202509.2212]
- 84. dPCR vs qPCR vs end-point PCR [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/digital-pcr/digital-pcr-vs-quantitative-pcr-vs-end-point-pcr]
- 85. Comparative analysis between digital PCR and blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515817/]
- 86. Comparative analysis between digital PCR and blood ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1615409/full]
- 87. A Comparison of Blood Pathogen Detection Among ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.641202/full]
- 88. Clinical validation of a multiplex droplet digital PCR for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9358819/]
- 89. A retrospective study of the detection of sepsis pathogens ... [https://www.sciencedirect.com/science/article/pii/S2405844024035540;]
- 90. Development and clinical validation of a dual ddPCR ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1338395/full]
- 91. PCR-based Sepsis@Quick test is superior in comparison ... [https://www.nature.com/articles/s41598-019-50150-y]
- 92. Digital PCR (dPCR) and Real-Time PCR (qPCR) Market ... [https://www.pharmiweb.com/press-release/2025-07-08/digital-pcr-dpcr-and-real-time-pcr-qpcr-market-share-growth-demand-statistics-2025-2035]
- 93. Digital PCR (DPCR) and QPCR Strategic Insights [https://www.archivemarketresearch.com/reports/digital-pcr-dpcr-and-qpcr-183926]