Ensuring Equity in Early Detection: A Comprehensive Guide to Validating Cancer Risk Models Across Diverse Populations
This article addresses the critical challenge of validating cancer risk prediction models across racially, ethnically, and geographically diverse populations—a prerequisite for equitable clinical application.
Ensuring Equity in Early Detection: A Comprehensive Guide to Validating Cancer Risk Models Across Diverse Populations
Abstract
This article addresses the critical challenge of validating cancer risk prediction models across racially, ethnically, and geographically diverse populations—a prerequisite for equitable clinical application. We synthesize current evidence on methodologies for external validation, performance assessment across subgroups, and strategies to enhance generalizability. For researchers and drug development professionals, we provide a structured analysis of validation frameworks, comparative model performance metrics including discrimination and calibration, and emerging approaches incorporating AI and longitudinal data. The review highlights persistent gaps in validation for underrepresented groups and rare cancers, offering practical guidance for developing robust, clinically implementable risk stratification tools that perform reliably across all patient demographics.
The Imperative for Inclusive Validation: Why Population Diversity Matters in Cancer Risk Prediction
The Clinical and Ethical Necessity of Broadly Applicable Risk Models
Clinical risk prediction models are fundamental to the modern vision of personalized oncology, providing individualized risk estimates to aid in diagnosis, prognosis, and treatment selection. [1] Their transition from research tools to clinical assets, however, hinges on a single critical property: broad applicability. A model demonstrating perfect discrimination in its development cohort is clinically worthless—and potentially harmful—if it fails to perform accurately in the diverse patient populations encountered in real-world practice. The clinical necessity stems from the imperative to deliver equitable, high-quality care to all patients, regardless of demographic or geographic background. The ethical necessity is rooted in the fundamental principle of justice, requiring that the benefits of technological advancement in cancer care be distributed fairly across society. This guide examines the performance of cancer risk prediction models when validated across diverse populations, comparing methodological approaches and presenting the experimental data that underpin the journey toward truly generalizable models.
Performance Comparison: Single-Cohort vs. Multi-Cohort Validation
The most telling evidence of a model's generalizability comes from rigorous external validation in populations that are distinct from its development cohort. The tables below synthesize quantitative performance data from recent studies to compare model performance in internal versus external settings and across different demographic groups.
Table 1: Comparison of Model Performance in Internal vs. External Validation Cohorts
| Cancer Type | Model Description | Validation Type | Cohort Size (N) | Performance (AUROC) | Citation |
|---|---|---|---|---|---|
| Breast Cancer | Dynamic AI Model (MRS) with prior mammograms | Development (Initial) | Not Specified | 0.81 | [2] |
| External (Province-wide) | 206,929 | 0.78 (0.77-0.80) | [2] | ||
| Pan-Cancer (15 types) | Algorithm with Symptoms & Blood Tests (Model B) | Derivation (QResearch) | 7.46 Million | Not Specified | [3] |
| External (CPRD - 4 UK nations) | 2.74 Million | Any Cancer (Men): 0.876 (0.874-0.878)Any Cancer (Women): 0.844 (0.842-0.847) | [3] | ||
| Cervical Cancer (CIN3+) | LASSO Cox Model (Estonian e-health data) | Internal (10-fold cross-validation) | 517,884 Women | Harrell's C: 0.74 (0.73-0.74) | [4] |
Table 2: Performance Consistency of a Breast Cancer Risk Model Across Racial/Ethnic Groups in an External Validation Cohort (N=206,929) [2]
| Subgroup | Sample Size (with race data) | Number of Incident Cancers | 5-Year AUROC (95% CI) |
|---|---|---|---|
| East Asian Women | 34,266 | Not Specified | 0.77 (0.75 - 0.79) |
| Indigenous Women | 1,946 | Not Specified | 0.77 (0.71 - 0.83) |
| South Asian Women | 6,116 | Not Specified | 0.75 (0.71 - 0.79) |
| White Women | 66,742 | Not Specified | 0.78 (Overall) |
| All Women (Overall) | 118,093 | 4,168 | 0.78 (0.77 - 0.80) |
The data in Table 1 shows a minor, expected decrease in performance from development to external validation, but the model maintains high discriminatory power, indicating robust generalizability. [3] [2] Table 2 demonstrates that a well-designed model can achieve consistent performance across diverse racial and ethnic groups, a key marker of equitable applicability. [2]
Experimental Protocols for Validation
Protocol 1: Large-Scale External Validation of a Multi-Cancer Prediction Algorithm
This protocol, based on the work by Collins et al. (2025), details the validation of a diagnostic prediction algorithm for 15 cancer types across multiple UK nations. [3]
- Aim: To externally validate the performance of two new prediction algorithms (with and without blood tests) for estimating the probability of an undiagnosed cancer.
- Validation Cohorts:
- QResearch Validation Cohort: 2.64 million patients from England.
- CPRD Validation Cohort: 2.74 million patients from Scotland, Wales, and Northern Ireland. Using a separate cohort from different countries is a robust test of generalizability.
- Model Inputs: Age, sex, deprivation, smoking, alcohol, family history, medical diagnoses, symptoms (both general and cancer-specific), and commonly used blood tests (full blood count, liver function tests).
- Statistical Analysis:
- Discrimination: Calculated the c-statistic (AUROC) for each of the 15 cancer types separately in men and women. Also used the polytomous discrimination index (PDI) to assess the model's ability to discriminate between all cancer types simultaneously.
- Calibration: Compared predicted versus observed risks to ensure the model was accurately estimating the absolute probability of cancer.
- Subgroup Analysis: Assessed performance by ethnic group, age, and geographical area to evaluate consistency.
- Key Outcome: The models showed high discrimination and calibration in both English and non-English validation cohorts, proving their applicability across a diverse national population. [3]
Protocol 2: Dynamic Risk Prediction Model for Breast Cancer
This protocol, from the study by Kerlikowske et al. (2025), focuses on validating a dynamic AI model that uses longitudinal mammogram data. [2]
- Aim: To validate a dynamic mammogram risk score (MRS) model for predicting 5-year breast cancer risk across a racially and ethnically diverse population in a province-wide screening program.
- Study Design & Cohort: A prognostic study of 206,929 women aged 40-74 from the British Columbia Breast Screening Program (2013-2019), with follow-up through a cancer registry until 2023.
- Model Input: The model's sole input was the four standard views of digital mammograms. Its dynamic nature came from incorporating up to 4 years of prior screening images, in addition to the current mammogram, to capture temporal changes.
- Analysis:
- Discrimination: Primary outcome was the 5-year time-dependent AUROC.
- Calibration: Absolute risk was calibrated to US SEER incidence rates. Calibration plots compared predicted vs. observed 5-year risk.
- Stratified Analysis: Performance was rigorously evaluated across subgroups defined by race and ethnicity (East Asian, Indigenous, South Asian, White), age, breast density, and family history.
- Key Outcome: The dynamic model maintained high and consistent discrimination across all racial and ethnic subgroups, demonstrating that AI-based risk tools can be broadly applicable when properly validated. [2]
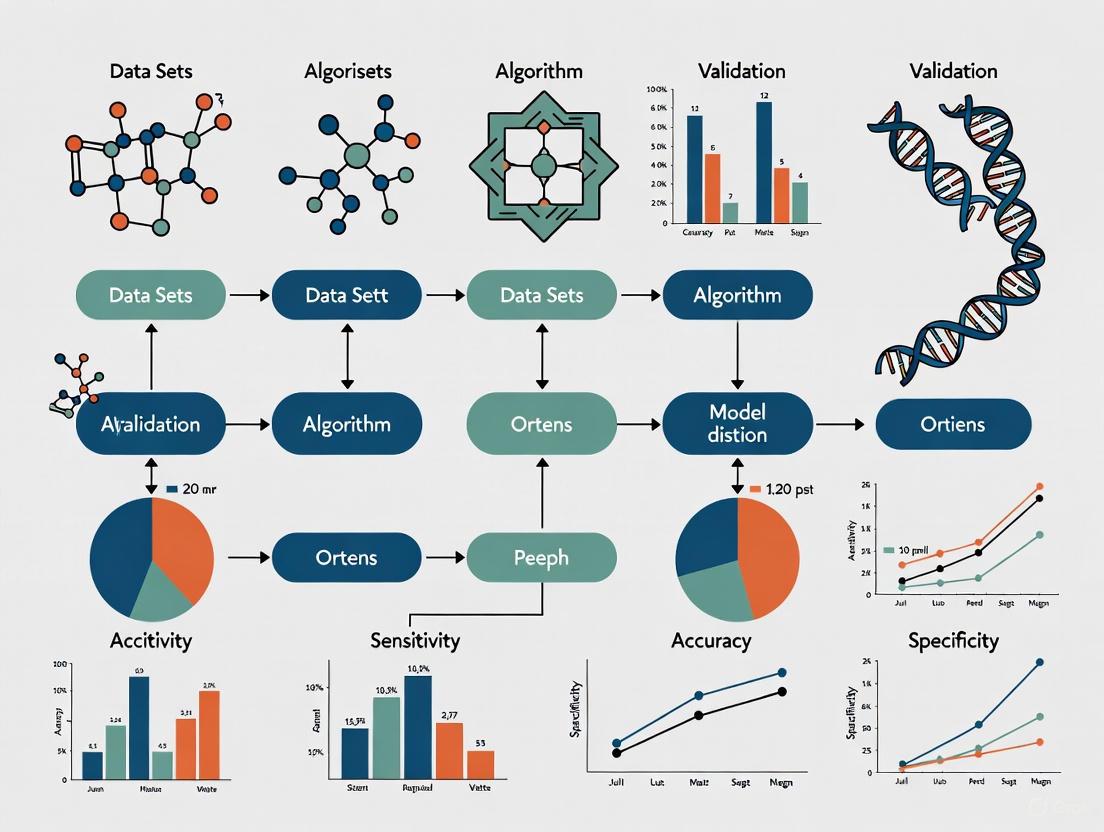
Workflow and Pathway Diagrams
Dynamic Risk Prediction Workflow
The following diagram illustrates the core workflow for developing and validating a dynamic risk prediction model, which leverages longitudinal data to update risk estimates over time. [5] [2]
External Validation Pathway for Broad Applicability
This pathway outlines the critical steps for establishing a model's broad applicability through rigorous external validation, a process essential for clinical implementation. [1] [3] [2]
The Scientist's Toolkit: Essential Reagents for Validation
For researchers developing and validating broadly applicable risk models, the following "toolkit" comprises essential methodological components and resources.
Table 3: Essential Reagents for Robust Risk Model Validation
| Tool Category | Specific Tool/Technique | Function in Validation | Key Reference |
|---|---|---|---|
| Validation Statistics | C-Statistic (AUROC) | Measures model discrimination: ability to distinguish between cases and non-cases. | [4] [3] [2] |
| Calibration Plots/Slope | Assesses accuracy of absolute risk estimates by comparing predicted vs. observed risks. | [4] [3] | |
| Polytomous Discrimination Index (PDI) | Evaluates a model's ability to discriminate between multiple outcome types (e.g., different cancers). | [3] | |
| Data Resampling Methods | 10-Fold Cross-Validation | Robust internal validation technique for model optimization and error estimation. | [4] |
| Bootstrapping | Generates multiple resampled datasets to obtain confidence intervals for performance metrics. | [2] | |
| Variable Selection | LASSO (Least Absolute Shrinkage and Selection Operator) | Regularization technique that performs variable selection to prevent overfitting. | [5] [4] |
| Reporting Guidelines | TRIPOD+AI Checklist | Critical reporting framework to ensure transparent and complete reporting of prediction model studies. | [1] [6] |
| Performance Benchmarking | Net Benefit Analysis (Decision Curve Analysis) | Quantifies the clinical utility of a model by integrating benefits (true positives) and harms (false positives). | [1] |
The journey toward clinically impactful cancer risk prediction models is paved with rigorous, multi-faceted validation. The experimental data and protocols presented herein demonstrate that while performance can generalize well across diverse populations, this outcome is not accidental. It is the product of deliberate methodological choices: the use of large, representative datasets for development; [4] [3] the implementation of dynamic modeling that incorporates longitudinal data; [5] [2] and, most critically, a commitment to comprehensive external validation across geographical, temporal, and demographic domains. [1] [3] [2] The Scientist's Toolkit provides the essential reagents for this task. Ultimately, a model's validity is not proven by its performance on a single, curated cohort, but by its consistent ability to provide accurate, calibrated, and clinically useful risk estimates for every patient it encounters, anywhere. This is the clinical and ethical standard to which the field must aspire.
Cancer risk prediction models are pivotal tools in the era of personalized medicine, enabling the identification of high-risk individuals for targeted screening, early intervention, and tailored preventive strategies [7]. Their development and validation represent an area of "extraordinary opportunity" in cancer research [7]. However, the real-world clinical utility of these models is heavily dependent on two fundamental, and often lacking, properties: their generalizability across diverse populations and their rigorous external validation. This guide provides a comparative analysis of the current performance and development practices of cancer risk prediction models, objectively examining the evidence on their skewed development and the critical gaps in their validation. This analysis is framed for an audience of researchers, scientists, and drug development professionals, with a focus on supporting the broader thesis that advancing cancer care requires a concerted effort to address these shortcomings.
Comparative Performance of Cancer Risk Models
The performance of risk models is primarily quantified by their discrimination (ability to distinguish between those who will and will not develop cancer) and calibration (agreement between predicted and observed risks). The table below summarizes the reported performance of various models, highlighting the diversity in predictive accuracy.
Table 1: Performance Metrics of Selected Cancer Risk Prediction Models
| Cancer Type / Focus | Model Name / Type | Population / Cohort | Key Performance Metrics | Key Variables Included |
|---|---|---|---|---|
| Breast Cancer [8] | 107 Various Models (Systematic Review) | General & High-Risk Populations | AUC Range: 0.51 - 0.96; O/E Ratio Range: 0.84 - 1.10 (n=8 studies) | Demographic, genetic, and/or imaging-derived variables |
| Breast Cancer [9] | iCARE-Lit (Age <50) | UK-based cohort (White non-Hispanic) | AUC: 65.4; E/O: 0.98 (Well-calibrated) | Classical risk factors (questionnaire-based) |
| Breast Cancer [9] | iCARE-BPC3 (Age ≥50) | UK-based cohort (White non-Hispanic) | AUC: Not Specified; E/O: 1.00 (Well-calibrated) | Classical risk factors (questionnaire-based) |
| Multiple Cancers (Diagnostic) [3] | Model B (With blood tests) | English population (7.46M adults) | Any Cancer C-Statistic: Men: 0.876, Women: 0.844; Improved vs. existing models | Symptoms, medical history, full blood count, liver function tests |
| Cancer Prevention [10] | WCRF/AICR Screener | Spanish PREDIMED-Plus subsample | ICC: 0.68 vs. validated methods; Score range 0-7 | 13 questions on body weight, PA, diet (e.g., red meat, plant-based foods) |
The data reveals a wide spectrum of discriminatory accuracy, particularly in breast cancer, where the Area Under the Curve (AUC) can range from near-random (0.51) to excellent (0.96) [8]. Well-calibrated models, like the iCARE versions, show an Expected-to-Observed (E/O) ratio close to 1.0, indicating high accuracy in absolute risk estimation [9]. Furthermore, the integration of diverse data types, such as blood biomarkers, appears to enhance model performance for diagnostic purposes [3].
Skewed Model Development: Geographic and Cancer-Type Disparities
A critical analysis of the development landscape reveals significant biases that limit the global applicability of cancer risk models.
Table 2: Evidence of Skewed Development in Cancer Risk Prediction Models
| Aspect of Skew | Evidence from Literature | Implication |
|---|---|---|
| Geographic Concentration | Of 107 breast cancer models reviewed, 38.3% were developed in the USA and 12% in the UK [8]. Models are often concentrated in the US and UK, with a notable gap for other regions [7]. | Models may not generalize well to populations with different genetic backgrounds, lifestyles, and healthcare environments. |
| Ethnic Homogeneity | Most breast cancer risk models were developed in Caucasian populations [8]. | Predictive performance may degrade in non-Caucasian ethnic groups due to differing risk factor prevalence and effect sizes. |
| Focus on Common Cancers | Significant emphasis on breast and colorectal cancers due to their prevalence [7]. No models were found for several rarer cancers (e.g., brain, Kaposi sarcoma, penile cancer) [7]. | Patients with rarer cancers are deprived of the benefits of risk-stratified prevention and early detection strategies. |
| Variable Integration | Models including both demographic and genetic or imaging data performed better than demographic-only models [8]. | There is a trend towards more complex, multi-factorial models, but these require more data and sophisticated validation. |
This skewed development means that existing models may not perform optimally for populations in Asia, Africa, or South America, or for individuals with rare cancer types, leading to potential misestimation of risk and inequitable healthcare.
Gaps in Model Validation and Proposed Experimental Protocols
A cornerstone of reliable risk prediction is rigorous validation, yet this remains a major gap. External validation—testing a model on data entirely independent from its development set—is infrequently performed.
Detailed Methodology for External Validation
The following workflow, based on established practices from recent high-impact studies [9] [3], outlines a robust protocol for the external validation of a cancer risk prediction model.
The key steps in this validation workflow are:
- Define Validation Objective and Identify Model: Clearly state the purpose (e.g., "to validate the iCARE-BPC3 model for 5-year breast cancer risk in a multi-ethnic European population"). Acquire the complete model specification, including all risk factors, coefficients (log relative risks), and the algorithm for calculating absolute risk [9].
- Secure Independent Validation Cohort(s): Identify one or more cohorts that are entirely separate from the development data. These should represent the target population. For example, the validation of the iCARE models was performed in the UK-based Generations Study, while the development used data from the BPC3 consortium and literature [9]. Sample size must be sufficient, often requiring tens of thousands of participants [8] [3].
- Data Preparation and Harmonization: Extract and harmonize the variables required by the model from the validation cohort. This often requires careful mapping of local data formats and measurements to the model's definitions. Handling missing data (e.g., through statistical imputation) is a critical step [9].
- Calculate Individual Predicted Risks: Apply the model to each individual in the validation cohort to generate a predicted probability of cancer over a specific time horizon (e.g., 5-year risk).
- Assess Model Performance: Evaluate the model using two key metrics:
- Discrimination: Compute the Area Under the Receiver Operating Characteristic Curve (AUC). An AUC of 0.5 indicates no discrimination, while 1.0 indicates perfect discrimination. Models with AUC >0.75 are generally considered clinically useful [8] [9].
- Calibration: Compare the predicted number of cancers to the observed number, often summarized as an Expected-to-Observed (E/O) ratio. A ratio of 1.0 indicates perfect calibration. This is also visualized using calibration plots [9].
- Analyze Subgroup Performance: Crucially, assess model performance across key subgroups, such as different ethnicities, age groups, or geographic regions, to identify specific populations for which the model may be poorly calibrated [3].
The Validation Gap in Context
The scale of the validation gap is stark. In a systematic review of 107 breast cancer risk models, only 18 studies (16.8%) reported any external validation [8]. This lack of independent, prospective validation is the single greatest barrier to the broad clinical application of even the most sophisticated models [9].
The Scientist's Toolkit: Essential Reagents for Risk Model Research
The development and validation of modern cancer risk models rely on a suite of data, software, and methodological tools.
Table 3: Key Research Reagent Solutions for Cancer Risk Prediction
| Tool / Resource | Type | Function / Application |
|---|---|---|
| iCARE Software [9] | Software Tool | A flexible platform for building, validating, and applying absolute risk models using data from multiple sources; enables comparative validation studies. |
| PROBAST Tool [8] | Methodological Tool | The "Prediction model Risk Of Bias Assessment Tool" critically appraises the risk of bias and applicability of prediction model studies. |
| TRIPOD+AI Checklist [6] | Reporting Guideline | A checklist (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis + AI) for ensuring complete reporting of prediction model studies. |
| Large EHR Databases (e.g., QResearch, CPRD) [3] | Data Resource | Electronic Health Record databases provide large, longitudinal, real-world datasets ideal for both model development and population-wide external validation. |
| Polygenic Risk Score (PRS) [9] | Genetic Tool | A single score summarizing the combined effect of many genetic variants; its integration can substantially improve risk stratification for certain cancers. |
| WCRF/AICR Screener [10] | Assessment Tool | A validated, short questionnaire to rapidly assess an individual's adherence to cancer prevention guidelines based on diet and lifestyle in clinical settings. |
The current landscape of cancer risk prediction is a tale of promising sophistication hampered by insufficient validation and population-specific development. While models are becoming more powerful by integrating genetic, clinical, and lifestyle data, their real-world utility is confined to populations that mirror their largely Caucasian, Western development cohorts. The path forward requires a paradigm shift where the funding, prioritization, and publication of research are as focused on rigorous, multi-center, multi-ethnic external validation as they are on initial model development. For researchers and drug developers, this means that selecting a risk model for clinical trial recruitment or public health strategy must involve a critical appraisal of its validation status across diverse groups. The future of equitable and effective cancer prevention depends on closing these validation gaps.
Key Populations Requiring Enhanced Representation
The validation of cancer risk prediction models across diverse populations is a critical scientific endeavor, directly impacting the equity and effectiveness of cancer screening and prevention strategies. The underrepresentation of specific racial and ethnic groups in the research used to develop and validate these models threatens their generalizability and can perpetuate health disparities [11]. For instance, African-Caribbean men face prostate cancer rates up to three times higher than their White counterparts, yet the majority of prostate cancer cell lines in research are derived from White men, potentially missing crucial biological variations [11]. This article objectively compares the performance of a contemporary artificial intelligence (AI)-based risk prediction model across well-represented and underrepresented populations, providing supporting experimental data to highlight validation gaps and the urgent need for enhanced representation.
Comparative Performance Analysis of a Dynamic Risk Prediction Model
A 2025 prognostic study externally validated a dynamic AI-based mammogram risk score (MRS) model across a racially and ethnically diverse population within the British Columbia Breast Screening Program [2]. This model innovatively incorporates up to four years of prior screening mammograms, in addition to the current image, to predict the 5-year future risk of breast cancer. The study's findings offer a clear lens through which to analyze model performance across different populations.
The table below summarizes the model's discriminatory performance, measured by the 5-year Area Under the Receiver Operating Characteristic Curve (AUROC), across various demographic subgroups [2]. An AUROC of 0.5 indicates performance no better than chance, while 1.0 represents perfect prediction.
Table 1: Discriminatory Performance of the Dynamic MRS Model Across Subgroups
| Population Subgroup | 5-Year AUROC | 95% Confidence Interval |
|---|---|---|
| Overall Cohort | 0.78 | 0.77 - 0.80 |
| By Race/Ethnicity | ||
| East Asian Women | 0.77 | 0.75 - 0.79 |
| Indigenous Women | 0.77 | 0.71 - 0.83 |
| South Asian Women | 0.75 | 0.71 - 0.79 |
| White Women | 0.78 | 0.77 - 0.80 |
| By Age | ||
| Women Aged ≤50 years | 0.76 | 0.74 - 0.78 |
| Women Aged >50 years | 0.80 | 0.78 - 0.82 |
The data demonstrates that the model maintained robust and consistent discriminatory performance across the racial and ethnic groups studied, with AUROC values showing considerable overlap in their confidence intervals [2]. This is a significant finding, as previous AI models have shown significant performance drops when validated in racially and ethnically diverse populations [2]. Furthermore, the model showed strong performance in younger women (≤50 years), a key population for early intervention.
The following diagram illustrates the experimental workflow for this external validation study, from cohort selection to performance analysis.
Figure 1: Workflow for external validation of the dynamic MRS model.
Detailed Experimental Protocol
The validation of the dynamic MRS model followed a rigorous prognostic study design. The cohort was drawn from the British Columbia Breast Screening Program and included 206,929 women aged 40 to 74 years who underwent screening mammography with full-field digital mammography (FFDM) between January 1, 2013, and December 31, 2019 [2].
- Data Sources and Linkage: Mammogram images were assembled from multiple fixed-site and mobile screening clinics. This data was prospectively linked to the provincial British Columbia Cancer Registry to identify pathology-confirmed incident breast cancers diagnosed through June 2023, with a maximum follow-up of 10 years [2]. This linkage was performed by staff blinded to mammography features to prevent bias.
- Inclusion/Exclusion Criteria: The study included women with one or more screening mammograms. Those diagnosed with breast cancer within the first six months of cohort entry or with a prior history of breast cancer were excluded to ensure the model was predicting new, future cancer events [2].
- Exposure and Outcome Measures: The primary exposure was the AI-generated MRS, which analyzed the four standard views of digital mammograms. The model dynamically incorporated images from the current screening visit and prior mammograms from up to four years preceding the current visit. The primary outcome was the 5-year risk of breast cancer, with performance assessed via discrimination (AUROC), calibration, and risk stratification [2].
- Statistical Analysis: The performance of several model configurations was examined: age only; the current mammogram only (static MRS); prior mammograms only (dynamic MRS); and combinations of these with age. Stratified sub-analyses were pre-specified for race and ethnicity, age, breast density, and family history. Statistical significance and confidence intervals were estimated using 5000 bootstrap samples, and the reporting adhered to the TRIPOD guideline for prediction models [2].
Populations with Inadequate Representation and the Impact on Research
Despite the successful validation in the British Columbia cohort, significant representation gaps persist in oncology research. The following diagram conceptualizes the cycle of underrepresentation and its consequences for model validity and health equity.
Figure 2: The cycle of underrepresentation and pathways to equitable research.
Key populations consistently identified as requiring enhanced representation include:
- Black, Asian, and Minority Ethnic Communities: These groups face a disproportionately higher burden for several cancers but remain inadequately represented in research [11]. For example, the ReIMAGINE Consortium for prostate cancer actively worked to engage diverse communities but found that volunteers from Black, Asian, and minority ethnic backgrounds constituted only 0% to 13% of their meetings, despite the higher risk profile for Black men [11].
- Rare Cancers: A comprehensive analysis of predictive models reveals an uneven distribution of research focus. While breast and colorectal cancers have many models, there are no risk prediction models for several rarer cancers, including brain or nervous system cancer, Kaposi sarcoma, mesothelioma, penile cancer, and anal cancer, among others [7]. This gap is often due to the challenge of gathering sufficient data for model development.
The consequences of these gaps are not merely academic; they directly impact patient care. For instance, a specific gene variation impacting Black men's response to a common prostate cancer drug was missed because the research was conducted predominantly on cell lines from White men [11]. Without comprehensive data from diverse populations, the effectiveness of treatments and the accuracy of risk prediction tools for all populations remain unclear [11].
The Scientist's Toolkit: Research Reagent Solutions
To address the challenge of underrepresentation and conduct equitable cancer risk prediction research, scientists can utilize the following key resources and approaches.
Table 2: Essential Resources for Inclusive Cancer Risk Prediction Research
| Research Reagent or Resource | Function & Application |
|---|---|
| Diverse Biobanks & Cohort Data | Provides genomic, imaging, and clinical data from diverse racial, ethnic, and ancestral populations, essential for model development and external validation. Examples include the "All of Us" Research Program and inclusive cancer screening registries. |
| AI-based Mammogram Risk Score (MRS) | An algorithmic tool that analyzes current and prior mammogram images to predict future breast cancer risk. Its function in capturing longitudinal changes in breast tissue has shown robust performance across diverse populations in external validation [2]. |
| ARUARES (The Apricot) Tool | A framework developed by the "Diverse PPI" group to guide researchers on culturally competent practices for engaging diverse communities. It serves as a mental checklist for inclusive research design and participant recruitment at no additional cost [11]. |
| NIHR INCLUDE Ethnicity Framework | A tool designed to help clinical trialists design more inclusive trials by systematically considering factors that may limit participation for underrepresented groups, ensuring research findings are generalizable [11]. |
| Polygenic Risk Scores (PRS) | A statistical construct that aggregates the effects of many genetic variants to quantify an individual's genetic predisposition to a disease. Its accuracy is highly dependent on the diversity of the underlying genome-wide association studies [12]. |
The external validation of the dynamic MRS model demonstrates that achieving consistent performance across racial and ethnic groups is feasible when diverse validation datasets are employed [2]. However, the broader landscape of cancer risk prediction reveals critical gaps in the representation of key populations, including specific racial and ethnic minorities and individuals predisposed to rarer cancers. Addressing these gaps is not merely a matter of equity but a scientific necessity for generating clinically useful and generalizable models. Future efforts must prioritize the intentional inclusion of these populations in all stages of research, from initial model development to external validation, leveraging available tools and frameworks to build a more equitable future for cancer prevention and early detection.
In the field of cancer risk prediction, model validation transcends a simple performance check—it represents a rigorous assessment of a model's readiness for real-world clinical and public health application. For researchers, scientists, and drug development professionals, understanding the trifecta of validation metrics—calibration, discrimination, and generalizability—is fundamental to translating predictive algorithms into actionable tools. These metrics respectively answer three critical questions: Are the predicted risks accurate and reliable? Can the model separate high-risk from low-risk individuals? Does the model perform consistently across diverse populations and settings? [13] [14] [15].
The validation process typically progresses through defined stages, starting with internal validation to assess reproducibility and overfitting, followed by external validation to evaluate transportability to new populations [14]. As systematic reviews have revealed, many published prediction models, including hundreds developed for COVID-19, demonstrate significant methodological shortcomings in their evaluation, often emphasizing discrimination while neglecting calibration [14]. This imbalance is problematic because poor calibration can make predictions misleading and potentially harmful for clinical decision-making, even when discrimination appears adequate [15]. For instance, in cancer risk prediction, miscalibration can lead to either false reassurance or unnecessary anxiety and interventions, undermining the model's clinical utility.
This guide provides a comprehensive comparison of validation methodologies and metrics, anchoring its analysis in the context of cancer risk prediction models. We synthesize current evidence, highlight performance benchmarks across model types, detail experimental protocols for proper evaluation, and visualize key conceptual relationships to equip researchers with the tools necessary for rigorous model assessment.
Quantitative Performance Comparison of Cancer Risk Models
The performance of cancer risk prediction models varies considerably based on their methodology, predictor types, and target population. The table below synthesizes key validation metrics from recent studies to provide a benchmark for model evaluation.
Table 1: Validation Performance of Selected Cancer Risk Prediction Models
| Cancer Type | Model Name | Discrimination (AUC/C-statistic) | Calibration (O/E Ratio) | Key Predictors Included | Population | Source |
|---|---|---|---|---|---|---|
| Breast Cancer | Machine Learning Pooled | 0.74 | N/R | Genetic, Imaging, Clinical | 27 Countries (Systematic Review) | [16] |
| Breast Cancer | Traditional Model Pooled | 0.67 | N/R | Clinical & Demographic | 27 Countries (Systematic Review) | [16] |
| Breast Cancer | Gail (in Chinese cohort) | 0.543 | N/R | Clinical & Demographic | Chinese | [16] |
| Liver Cancer | Fine-Gray Model | 0.782 (5-year risk) | Fine Agreement | Demographics, Lifestyle, Medical History | UK Biobank | [17] |
| Various Cancers | QCancer (Model B) | N/R | Heuristic Shrinkage >0.99 | Symptoms, Medical History, Blood Tests | UK (QResearch/CPRD) | [18] |
Abbreviations: N/R = Not Reported; O/E = Observed-to-Expected.
A systematic review and meta-analysis of female breast cancer incidence models provides a stark comparison between traditional and machine learning (ML) approaches. ML models demonstrated superior discrimination, with a pooled C-statistic of 0.74 compared to 0.67 for traditional models like Gail and Tyrer-Cuzick [16]. Furthermore, the review highlighted a critical issue of generalizability, noting that traditional models such as the Gail model exhibited notably poor predictive accuracy in non-Western populations, with a C-statistic as low as 0.543 in Chinese cohorts [16]. This underscores the necessity of population-specific validation.
Beyond breast cancer, models for other malignancies show promising performance. A liver cancer risk prediction model developed using the UK Biobank cohort achieved an AUC of 0.782 for 5-year risk, demonstrating good discrimination [17]. Its calibration was also reported to show "fine agreement" between observed and predicted risks [17]. Similarly, recent diagnostic cancer prediction algorithms (e.g., QCancer), which include common blood tests, showed excellent internal consistency with heuristic shrinkage factors very close to one (>0.99), indicating no evidence of overfitting—a common threat to model validity [18].
Experimental Protocols for Model Validation
A robust validation framework requires a structured methodological approach. The following protocols detail the key experiments needed to assess calibration, discrimination, and generalizability.
Protocol for Assessing Model Calibration
Calibration evaluation should be a multi-tiered process, moving from the general to the specific [15].
- Data Preparation: Execute the model to obtain predicted probabilities for each patient in the validation cohort. Ensure the cohort is independent of the development data (external validation) or use appropriate resampling techniques (internal validation) [14].
- Assess Mean Calibration (Calibration-in-the-large):
- Calculate the average predicted risk across all patients in the validation cohort.
- Calculate the overall observed event rate (e.g., cancer incidence).
- Compare the two values. The ratio should be close to 1, indicating that the model does not systematically over- or underestimate risk on average [15].
- Assess Weak Calibration:
- Fit a logistic regression model with the linear predictor from the target model as the only independent variable and the actual outcome as the dependent variable.
- Calibration Intercept (α): A target value of 0 indicates no overall over- or underestimation. A negative value suggests overestimation, a positive value suggests underestimation.
- Calibration Slope (β): A target value of 1 indicates an ideal spread of predictions. A slope < 1 suggests predictions are too extreme (high risks overestimated, low risks underestimated), a slope > 1 suggests predictions are too modest [13] [15].
- Assess Moderate Calibration via Calibration Curves:
- Group patients by their predicted risk (e.g., into deciles or using flexible smoothing).
- For each group, plot the mean predicted risk against the observed event probability.
- A precise calibration curve requires a sufficiently large sample size; a minimum of 200 patients with and 200 without the event has been suggested [15].
- Avoid the Hosmer-Lemeshow Test: This test is not recommended due to its reliance on arbitrary grouping, low statistical power, and uninformative P-value [15].
Protocol for Assessing Model Discrimination
Discrimination evaluates a model's ability to differentiate between patients who do and do not experience the event.
- Calculate the C-statistic (AUC):
- For a binary outcome, this is equivalent to the area under the Receiver Operating Characteristic (ROC) curve.
- It represents the probability that a randomly selected patient with the event (e.g., cancer) has a higher predicted risk than a randomly selected patient without the event [13] [19].
- Values range from 0.5 (no discrimination) to 1.0 (perfect discrimination).
- Calculate the Discrimination Slope:
- Compute the mean predicted risk in patients who experienced the event.
- Compute the mean predicted risk in patients who did not experience the event.
- The discrimination slope is the difference between these two means. A larger difference indicates better separation between the two groups [13].
Protocol for Assessing Model Generalizability
Generalizability, or transportability, is assessed through external validation.
- Cohort Selection: Validate the model in one or more entirely independent datasets. These should be from different but plausibly related settings (e.g., different geographic regions, healthcare systems, or time periods) [14].
- Performance Comparison: Calculate all relevant calibration and discrimination metrics (as described above) within the external cohort.
- Subgroup Analysis: Stratify the analysis by key demographic or clinical factors (e.g., race/ethnicity, sex, socioeconomic status) to identify performance variations across subpopulations [16] [20].
- Performance Benchmarking: Compare the model's performance in the new setting against existing, alternative models to determine if it offers a tangible improvement [18].
Visualizing the Validation Framework
The following diagram illustrates the logical relationships and workflow between the core concepts of model validation, highlighting their role in determining clinical utility.
The Scientist's Toolkit: Essential Reagents for Validation
Successful execution of the validation protocols requires specific statistical tools and methodologies. The table below lists key "research reagents" for a validation scientist.
Table 2: Essential Methodological Reagents for Prediction Model Validation
| Tool/Reagent | Category | Primary Function in Validation | Key Consideration |
|---|---|---|---|
| C-statistic (AUC) | Discrimination Metric | Quantifies model's ability to rank order risks. | Insensitive to calibration; does not reflect clinical utility [13] [19]. |
| Calibration Slope & Intercept | Calibration Metric | Assesses weak calibration and overfitting. | Slope < 1 indicates overfitting; intercept ≠ 0 indicates overall miscalibration [15]. |
| Calibration Plot | Calibration Visual | Graphical representation of predicted vs. observed risks. | Requires sufficient sample size (>200 events & non-events suggested) [15]. |
| Brier Score | Overall Performance | Measures average squared difference between predicted and actual outcomes. | Incorporates both discrimination and calibration aspects [13]. |
| Decision Curve Analysis (DCA) | Clinical Utility | Evaluates net benefit of using the model for clinical decisions across thresholds. | Superior to classification accuracy as it incorporates clinical consequences [17] [14]. |
| Net Reclassification Improvement (NRI) | Incremental Value | Quantifies improvement in risk reclassification with a new model/marker. | Use is debated; can be misleading without clinical context [13] [14]. |
| Internal Validation (Bootstrapping) | Generalizability Method | Assesses model optimism and overfitting in the derivation data. | Preferred over data splitting as it uses the full dataset [14]. |
The successful validation of a cancer risk prediction model is a multi-faceted endeavor that demands rigorous assessment of calibration, discrimination, and generalizability. As evidenced by comparative studies, models that integrate diverse data types—such as genetic, clinical, and imaging data—often achieve superior performance, yet their applicability can be limited by population-specific factors [16] [21]. The field is moving beyond a narrow focus on discrimination, recognizing that calibration is the Achilles' heel of predictive analytics and that the ultimate test of a model's worth is its clinical utility, often best evaluated through decision-analytic measures like Net Benefit [14] [15]. For researchers and drug developers, adhering to structured experimental protocols and utilizing the appropriate methodological toolkit is paramount for developing predictive models that are not only statistically sound but also clinically meaningful and equitable across diverse populations. Future efforts must focus on robust external validation, model updating, and transparent reporting to bridge the gap between model development and genuine clinical impact.
Validation Frameworks in Action: Statistical Methods and Performance Metrics for Diverse Cohorts
Accurately predicting an individual's risk of developing cancer is a cornerstone of personalized prevention and early detection strategies. For these risk prediction models to be trusted and implemented in clinical practice, they must undergo rigorous validation to ensure their predictions are both accurate and reliable. Validation assesses how well a model performs in new populations, separate from the one in which it was developed, guarding against over-optimistic results. Within this process, three core metrics form the essential toolkit for evaluating predictive performance: the Area Under the Receiver Operating Characteristic Curve (AUROC), Calibration Plots, and the Expected-to-Observed (E/O) Ratio.
These metrics serve distinct but complementary purposes. Discrimination, measured by AUROC, evaluates a model's ability to separate individuals who develop cancer from those who do not. Calibration, assessed through E/O ratios and calibration plots, determines the accuracy of the absolute risk estimates, checking whether the predicted number of cases matches what is actually observed. Together, they provide a comprehensive picture of model performance that informs researchers and clinicians about a model's strengths, limitations, and suitability for a given population [22] [23]. This guide objectively compares these metrics and illustrates their application through experimental data from recent cancer risk model studies.
The table below defines the three core validation metrics and their roles in model assessment.
Table 1: Core Metrics for Validating Cancer Risk Prediction Models
| Metric | Full Name | Core Question Answered | Interpretation of Ideal Value | Primary Evaluation Context |
|---|---|---|---|---|
| AUROC | Area Under the Receiver Operating Characteristic Curve | How well does the model rank individuals by risk? | 1.0 (Perfect separation) | Model Discrimination |
| Calibration Plot | --- | How well do the predicted probabilities match the observed probabilities? | Points lie on the 45-degree line | Model Calibration |
| E/O Ratio | Expected-to-Observed Ratio | Does the model, on average, over- or under-predict the total number of cases? | 1.0 (Perfect agreement) | Model Calibration |
Experimental Data from Comparative Model Studies
Performance in Breast Cancer Risk Prediction
Independent, comparative studies in large cohorts provide the best evidence for how risk models perform. The following table summarizes results from two such studies that evaluated established breast cancer risk models.
Table 2: Comparative Performance of Breast Cancer Risk Prediction Models in Validation Studies
| Study & Population | Model Name | AUROC (95% CI) | E/O Ratio (95% CI) | Key Findings |
|---|---|---|---|---|
| Generations Study [9](Women <50 years) | iCARE-Lit | 65.4 (62.1 to 68.7) | 0.98 (0.87 to 1.11) | Best calibration in younger women. |
| BCRAT (Gail) | 64.0 (60.6 to 67.4) | 0.85 (0.75 to 0.95) | Tendency to underestimate risk. | |
| IBIS (Tyrer-Cuzick) | 64.6 (61.3 to 67.9) | 1.14 (1.01 to 1.29) | Tendency to overestimate risk. | |
| Generations Study [9](Women ≥50 years) | iCARE-BPC3 | Not Reported | 1.00 (0.93 to 1.09) | Best calibration in older women. |
| Mammography Screening Cohort [24](Women 40-84 years) | Gail | 0.64 (0.61 to 0.65) | 0.98 (0.91 to 1.06) | Good calibration and moderate discrimination. |
| Tyrer-Cuzick (v8) | 0.62 (0.60 to 0.64) | 0.84 (0.79 to 0.91) | Underestimation of risk in this cohort. | |
| BCSC | 0.64 (0.62 to 0.66) | 0.97 (0.89 to 1.05) | Good calibration; highest AUC among models with density. |
Performance in Lung Cancer Risk Prediction
Calibration can vary dramatically across different populations, as shown by a large-scale evaluation of lung cancer risk models.
Table 3: Variability in E/O Ratios for Lung Cancer Risk Models Across Cohorts [23]
| Risk Model | Range of E/O Ratios Across 10 European Cohorts | Median E/O Ratio | Notes on Cohort Dependence |
|---|---|---|---|
| Bach | 0.41 - 2.51 | >1 | E/O highly dependent on cohort characteristics. |
| PLCOm2012 | 0.52 - 3.32 | >1 | Consistent over-prediction in healthier cohorts. |
| LCRAT | 0.49 - 2.76 | >1 | Under-prediction in high-risk ATBC cohort (male smokers). |
| LCDRAT | 0.51 - 2.69 | >1 | Over-prediction in health-conscious cohorts (e.g., HUNT, EPIC). |
Detailed Methodological Protocols
Protocol for Calculating the E/O Ratio and Assessing Calibration
The E/O ratio is a fundamental measure of overall calibration.
- Step 1: Calculate the Expected Number of Cases (E). For each individual in the validation cohort, use the risk prediction model to compute their probability of developing the cancer within a specified time period (e.g., 5-year risk). Sum these individual probabilities across the entire cohort to obtain the total number of expected cases, E [9] [25].
- Step 2: Determine the Observed Number of Cases (O). Through follow-up of the validation cohort, count the actual number of individuals who developed the cancer within the same time period. This is the observed number of cases, O [9] [25].
- Step 3: Compute the E/O Ratio. The ratio is calculated as E/O. An E/O = 1 indicates perfect overall calibration. An E/O > 1 indicates that the model overestimates risk (predicted more cases than observed), while an E/O < 1 indicates underestimation [9] [23].
- Step 4: Statistical Evaluation. Calculate a 95% confidence interval around the E/O ratio. A ratio is considered statistically significantly different from 1 if its 95% CI does not include 1 [9] [24].
A more nuanced assessment of calibration uses a model-based framework, which can be implemented with statistical software [22]:
- Fit Calibration Models: Fit a regression model in the validation cohort where the outcome is the actual event (cancer) and the predictor is the linear predictor from the risk model (or its log-odds).
Model 1 (Calibration-in-the-large):E(y) = f(ɣ₀ + p), where p is the offset. The intercept ɣ₀ assesses whether predictions are systematically too high or low.Model 2 (Calibration slope):E(y) = f(ɣ₀ + ɣ₁p). The slope ɣ₁ indicates whether the model's discrimination is transportable; an ideal value is 1.
- Create a Calibration Plot: Group individuals by deciles of their predicted risk. For each group, plot the average predicted risk against the observed risk (the proportion who actually developed cancer). A well-calibrated model will have points lying close to the 45-degree line of identity [22].
Figure 1: Workflow for E/O Ratio Calculation and Interpretation
Protocol for Constructing and Interpreting the ROC Curve and AUROC
The ROC curve visualizes the trade-off between sensitivity and specificity across all possible classification thresholds.
- Step 1: Obtain Predictions. For each individual in the validation cohort, obtain the model's predicted probability of having the event (e.g., developing cancer).
- Step 2: Vary the Threshold. Set a series of different probability thresholds (from 0 to 1) at which an individual is classified as "high risk."
- Step 3: Calculate TPR and FPR. For each threshold, calculate the True Positive Rate (TPR/Sensitivity) and False Positive Rate (FPR/1-Specificity) [26].
- TPR = True Positives / (True Positives + False Negatives)
- FPR = False Positives / (False Positives + True Negatives)
- Step 4: Plot the ROC Curve. Plot the FPR on the x-axis and the TPR on the y-axis for all thresholds. The resulting curve is the ROC curve [26] [27].
- Step 5: Calculate the AUROC. Calculate the area under the plotted ROC curve. The AUROC can be interpreted as the probability that a randomly selected individual who developed cancer has a higher risk score than a randomly selected individual who did not [26]. The AUROC ranges from 0.5 (no discriminative ability, equivalent to random guessing) to 1.0 (perfect discrimination) [26] [24].
Figure 2: ROC Curve and AUROC Interpretation Guide
Table 4: Key Reagents and Software for Model Validation
| Tool / Resource | Type | Primary Function in Validation | Example Use Case |
|---|---|---|---|
| iCARE Software [9] | R Software Package | Flexible tool for risk model development, validation, and comparison. | Used to validate and compare iCARE-BPC3 and iCARE-Lit models against established models. |
| PLCOm2012 Model [23] | Risk Prediction Algorithm | Validated model used as a benchmark in comparative lung cancer risk studies. | Served as a comparator in a 10-model evaluation across European cohorts. |
| BayesMendel R Package [24] | R Software Package | Used to run established models like BRCAPRO and the Gail model for risk estimation. | Enabled calculation of 6-year risk estimates in a cohort of 35,921 women. |
| UK Biobank [23] | Epidemiological Cohort Data | Provides large-scale, independent validation data not used in original model development. | Used as a key cohort for externally validating the calibration of lung cancer risk models. |
| TRIPOD Guidelines [25] | Reporting Framework | A checklist to ensure transparent and complete reporting of prediction model studies. | Used in systematic reviews to assess the quality of model development and validation reporting. |
No single metric is sufficient to validate a cancer risk model. AUROC and calibration provide complementary insights, and both must be considered. A model can have excellent discrimination (high AUROC) but poor calibration (E/O ≠ 1), meaning it reliably ranks risks but provides inaccurate absolute risk estimates, which is problematic for clinical decision-making [23]. Conversely, a model can be perfectly calibrated on average (E/O = 1) but have poor discrimination, limiting its utility to distinguish between high- and low-risk individuals [22].
The experimental data reveal critical lessons for researchers. First, even the best models currently show only moderate discrimination, with AUROCs typically in the 0.60-0.65 range for breast cancer [9] [24]. Second, calibration is not an inherent property of the model but a reflection of its match to a specific population. As Table 3 demonstrates, the same lung cancer model can severely overestimate risk in one cohort and underestimate it in another, often due to the "healthy volunteer effect" in epidemiological cohorts [23]. Therefore, external validation in a population representative of the intended clinical use case is mandatory.
Future efforts to improve models involve integrating novel risk factors like polygenic risk scores (PRS) and mammographic density, which are expected to significantly enhance risk stratification [9]. However, these advanced models will require independent prospective validation before broad clinical application. For now, researchers should prioritize model discrimination and careful cutoff selection for screening decisions, while treating calibration metrics as a crucial check on the applicability of a model to their specific target population.
Stratified Analysis Techniques for Racial, Ethnic and Age Subgroups
Validation of cancer risk prediction models across diverse populations is a critical scientific imperative in the quest to achieve health equity in cancer prevention and control. Risk prediction models have the potential to revolutionize precision medicine by identifying individuals most likely to develop cancer, benefit from interventions, or survive their diagnosis [28]. However, their utility depends fundamentally on ensuring validity and reliability across diverse socio-demographic groups [28]. Stratified analysis—the practice of evaluating model performance within specific racial, ethnic, and age subgroups—represents a fundamental methodology for assessing and improving the generalizability of these tools. This comparative guide examines the techniques, findings, and methodological frameworks for conducting stratified analyses of cancer risk prediction models, providing researchers with evidence-based approaches for validating model performance across population subgroups.
The Imperative for Subgroup Analysis in Model Validation
Limitations of Race-Agnostic and Age-Agnostic Models
Cancer risk prediction models developed without consideration of subgroup differences face significant limitations. Models that either erroneously treat race as a biological factor (racial essentialism) or exclude relevant socio-contextual factors risk producing inaccurate estimates for marginalized populations [28]. The origins of these limitations stem from historical precedents, such as the incorporation of "race corrections" that adjust risk estimates based on race without biological justification [28]. These corrections can harm patients by affecting eligibility for services; for instance, race-based adjustments in breast cancer risk models may lower risk estimates for Black women solely based on race, potentially making them ineligible for high-risk screening options [28].
Additionally, the exclusion of socio-contextual factors known to shape health outcomes threatens model validity and perpetuates harm by attributing health disparities to biology rather than structural inequities [28]. Residential segregation, economic disinvestment, environmental toxin exposure, and limited access to health-promoting resources disproportionately affect Black communities and correlate with cancer risk, yet these factors are rarely incorporated into risk models [28].
Dataset Limitations and Representation Gaps
Significant gaps exist in datasets used for model development and validation. Most established cohorts, such as the Nurses' Health Study (approximately 97% White), predominantly represent White populations [28]. While dedicated cohorts like the Black Women's Health Study (N=55,879) and Jackson Heart Study (N=5,301) represent important advances, they remain relatively new and smaller in scale [28]. A 2025 systematic review of breast cancer risk prediction models confirmed that most were developed in Caucasian populations, highlighting ongoing representation issues [8].
Techniques for Stratified Analysis
Statistical Methods for Subgroup Validation
Stratified analysis requires specific statistical techniques to evaluate model performance across subgroups. The following methodologies represent standard approaches for assessing discrimination, calibration, and clinical utility:
Discrimination Analysis: Area under the receiver operating characteristic curve (AUC) or C-statistic calculated separately for each subgroup measures the model's ability to distinguish between cases and non-cases within that group [29] [8]. AUC values range from 0.5 (no discrimination) to 1.0 (perfect discrimination), with values ≥0.7 generally considered acceptable.
Calibration Assessment: Observed-to-expected (O/E) or expected-to-observed (E/O) ratios evaluate how closely predicted probabilities match observed event rates within subgroups [9] [29]. Well-calibrated models have O/E ratios接近 1.0, with significant deviations indicating poor calibration.
Reclassification Analysis: Examines how risk stratification changes when using new models versus established ones within specific subgroups, assessing potential clinical impact [30].
Net Benefit Evaluation: Quantifies the clinical utility of models using decision curve analysis, balancing true positives against false positives across different risk thresholds [9].
Table 1: Key Metrics for Stratified Model Validation
| Metric | Calculation Method | Interpretation | Application in Subgroup Analysis |
|---|---|---|---|
| AUC (Discrimination) | Area under ROC curve | ≥0.7: Acceptable; ≥0.8: Excellent | Calculate separately for each racial, ethnic, age subgroup |
| O/E Ratio (Calibration) | Observed events ÷ Expected events | 1.0: Perfect calibration; <1.0: Overestimation; >1.0: Underestimation | Compare across subgroups to identify miscalibration patterns |
| Calibration Slope | Slope of observed vs. predicted risks | 1.0: Ideal; <1.0: Overfitting; >1.0: Underfitting | Assess whether risk factors have consistent effects across groups |
| Sensitivity/Specificity | Proportion correctly identified at specific threshold | Threshold-dependent performance | Evaluate clinical utility for screening decisions in each subgroup |
Subgroup-Specific Model Development
When existing models demonstrate poor performance in specific subgroups, researchers may develop subgroup-specific models. The iCARE (Individualized Coherent Absolute Risk Estimation) software provides a flexible framework for building absolute risk models for specific populations by combining information on relative risks, age-specific incidence, and mortality rates from multiple data sources [9]. This approach enables the creation of models that incorporate subgroup-specific incidence rates and risk factor distributions.
Comparative Performance Across Subgroups: Evidence from Multiple Cancers
Breast Cancer Risk Models
A 2021 validation study compared four breast cancer risk prediction models (BCRAT, BCSC, BRCAPRO, and BRCAPRO+BCRAT) across racial subgroups in a diverse cohort of women undergoing screening mammography [29]. The study utilized data from 122,556 women across three large health systems, following participants for five years to assess model performance.
Table 2: Breast Cancer Risk Model Performance by Racial Subgroup
| Model | Overall AUC (95% CI) | White Women AUC | Black Women AUC | Calibration (O/E) Black Women | Key Findings |
|---|---|---|---|---|---|
| BCRAT (Gail) | 0.63 (0.61-0.65) | Comparable to overall | Comparable to overall | Well-calibrated | No significant difference in performance between Black and White women |
| BCSC | 0.64 (0.62-0.66) | Comparable to overall | Comparable to overall | Well-calibrated | Incorporation of breast density did not create racial disparities |
| BRCAPRO | 0.63 (0.61-0.65) | Comparable to overall | Comparable to overall | Well-calibrated | Detailed family history performed similarly across groups |
| BRCAPRO+BCRAT | 0.64 (0.62-0.66) | Comparable to overall | Comparable to overall | Well-calibrated | Combined model showed improved calibration in women with family history |
The study found no statistically significant differences in model performance between Black and White women, suggesting that these established models function similarly across racial groups in terms of discrimination and calibration [29]. However, the authors noted limitations in assessing other racial and ethnic groups due to smaller sample sizes.
Beyond racial subgroups, the study also evaluated model performance by age and other characteristics, finding that discrimination was poorer for HER2+ and triple-negative breast cancer subtypes (more common in Black women) and better for women with high BMI [29]. This highlights the importance of considering multiple intersecting characteristics in stratified analysis.
Lung Cancer Risk Models
Research on lung cancer risk prediction models demonstrates how alternative approaches can address screening disparities. The current United States Preventive Services Task Force (USPSTF) criteria based solely on age and smoking history have been shown to exacerbate racial disparities [30]. A study of 883 ever-smokers (56.3% African American) evaluated the PLCOm2012 risk prediction model against USPSTF criteria [30].
The PLCOm2012 model significantly increased sensitivity for African American patients compared to USPSTF criteria (71.3% vs. 50.3% at the 1.70% risk threshold, p<0.0001), while showing no significant difference for White patients (66.0% vs. 62.4%, p=0.203) [30]. This demonstrates how risk prediction models can potentially reduce, rather than exacerbate, disparities in cancer screening when properly validated across subgroups.
A 2024 systematic review and meta-analysis of lung cancer risk prediction models reinforced these findings, showing that models like LCRAT, Bach, and PLCOm2012 consistently outperformed alternatives, with AUC differences up to 0.050 between models [31]. The review included 15 studies comprising 4,134,648 individuals, providing substantial evidence for model performance across diverse populations.
Age-Based Stratification
Age represents another critical dimension for stratified analysis. Validation of the iCARE breast cancer risk prediction models demonstrated important age-related patterns in performance [9]. In women younger than 50 years, the iCARE-Lit model showed optimal calibration (E/O=0.98, 95% CI=0.87-1.11), while BCRAT tended to underestimate risk (E/O=0.85) and IBIS to overestimate risk (E/O=1.14) in this age group [9]. For women 50 years and older, iCARE-BPC3 demonstrated excellent calibration (E/O=1.00, 95% CI=0.93-1.09) [9].
These findings highlight the necessity of age-stratified validation, as models may perform differently across age groups due to varying risk factor prevalence and incidence rates.
Experimental Protocols for Stratified Validation
Cohort Assembly and Inclusion Criteria
Robust stratified validation requires careful cohort assembly. The breast cancer model validation study by [29] established a protocol that can be adapted for various cancer types:
Multi-site Recruitment: Assemble cohorts from multiple healthcare systems serving diverse populations. The breast cancer study included Massachusetts General Hospital, Newton-Wellesley Hospital, and University of Pennsylvania Health System [29].
Standardized Data Collection: Collect risk factor data through structured questionnaires at the time of screening, including: age, race/ethnicity, age at menarche, age at first birth, BMI, history of breast biopsy, history of atypical hyperplasia, and family history of breast cancer [29].
Electronic Health Record Supplementation: Extract additional data from EHRs, including breast density measurements from radiology reports, pathologic diagnoses, and genetic testing results [29].
Cancer Outcome Ascertainment: Determine cancer cases through linkage with state cancer registries rather than relying solely on institutional data [29].
Follow-up Protocol: Ensure minimum five-year follow-up for all participants to assess near-term risk predictions [29].
Validation Workflow for Stratified Analysis
Statistical Analysis Plan
A comprehensive statistical analysis plan for stratified validation should include:
Pre-specified Subgroups: Define racial, ethnic, and age subgroups prior to analysis, with particular attention to ensuring adequate sample sizes for each group [29].
Handling of Missing Data: Implement standardized approaches for missing risk factor data, such as assuming no atypical hyperplasia for missing values or using multiple imputation where appropriate [29].
Competing Risk Analysis: Account for competing mortality risks using appropriate statistical methods, as implemented in the iCARE framework [9].
Multiple Comparison Adjustment: Apply corrections for multiple testing when evaluating model performance across numerous subgroups.
Sensitivity Analyses: Conduct analyses to test the robustness of findings to different assumptions and missing data approaches.
Table 3: Essential Resources for Stratified Analysis of Cancer Risk Models
| Resource Category | Specific Tools | Function in Stratified Analysis | Key Features |
|---|---|---|---|
| Statistical Software | R Statistical Environment with BCRA, BayesMendel, and iCARE packages | Model implementation and validation | Open-source, specialized packages for specific cancer models [29] |
| Risk Model Packages | BCRA R package (v2.1), BayesMendel R package (v2.1-7), BCSC SAS program (v2.0) | Calculation of model-specific risk estimates | Validated algorithms for established models [29] |
| Data Integration Platforms | iCARE (Individualized Coherent Absolute Risk Estimation) Software | Flexible risk model development and validation | Integrates multiple data sources; handles missing risk factors [9] |
| Validation Metrics | PROBAST (Prediction model Risk Of Bias Assessment Tool) | Standardized quality assessment of prediction model studies | Structured evaluation of bias across multiple domains [8] |
| Cohort Resources | Black Women's Health Study, Jackson Heart Study, Multiethnic Cohort Study | Development and validation in underrepresented populations | Focused recruitment of underrepresented groups [28] |
Stratified analysis of cancer risk prediction models across racial, ethnic, and age subgroups represents both an ethical imperative and methodological necessity in advancing precision medicine. The evidence demonstrates that while significant challenges remain in representation and model development, methodologically rigorous subgroup validation can identify performance disparities and guide improvements. The consistent finding that properly validated models can perform similarly across racial groups offers promise for equitable cancer risk assessment.
Future directions should include: (1) development of larger diverse cohorts specifically for model validation; (2) incorporation of social determinants of health as explicit model factors rather than using race as a proxy; (3) standardized reporting of stratified performance in all model validation studies; and (4) investment in resources comparable to genomic initiatives to address social and environmental determinants of cancer risk [28]. Through committed application of stratified analysis techniques, researchers can ensure that advances in cancer risk prediction benefit all populations equally, moving the field toward its goal of eliminating cancer disparities and achieving genuine health equity.
The TRIPOD Guideline for Transparent Reporting of Prediction Models
Transparent and complete reporting is fundamental to the development and validation of clinical prediction models, a process crucial for advancing personalized medicine. The TRIPOD (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis) guideline provides a foundational checklist to ensure that studies of diagnostic or prognostic prediction models are reported with sufficient detail to be understood, appraised for risk of bias, and replicated [32]. With the increasing use of artificial intelligence (AI) and machine learning in prediction modeling, the original TRIPOD statement has been updated to TRIPOD+AI, which supersedes the 2015 version and provides harmonized guidance for 27 essential reporting items, irrespective of the modeling technique used [33]. This guide compares these reporting frameworks within the critical context of validating cancer risk prediction models across diverse populations.
The following table summarizes the core characteristics of the original TRIPOD statement and its contemporary update, TRIPOD+AI.
| Feature | TRIPOD (2015) | TRIPOD+AI (2024) |
|---|---|---|
| Primary Focus | Reporting of prediction models developed using traditional regression methods [32]. | Reporting of prediction models using regression or machine learning/AI methods; supersedes TRIPOD 2015 [33]. |
| Number of Items | 22 items [32]. | 27 items [33]. |
| Key Additions in TRIPOD+AI | Not applicable. | New items addressing machine learning-specific aspects, such as model description, code availability, and hyperparameter tuning strategies [33]. |
| Scope of Models Covered | Diagnostic and prognostic prediction models [32]. | Explicitly includes AI-based prediction models, ensuring broad applicability across modern modeling techniques [33]. |
| External Validation Emphasis | Highlights the importance of external validation and its reporting requirements [32]. | Maintains and reinforces the need for transparent reporting of external validation studies, crucial for assessing model generalizability [33]. |
Experimental Validation in Cancer Risk Prediction: A TRIPOD-Compliant Case Study
A 2025 prognostic study validating a dynamic, AI-based breast cancer risk prediction model exemplifies the application of rigorous, transparent research practices in line with TRIPOD principles [2].
Experimental Protocol and Methodology
- Objective: To examine whether a dynamic risk prediction model incorporating prior mammograms could accurately predict future breast cancer risk across a racially and ethnically diverse population in a population-based screening program [2].
- Study Design & Cohort: This prognostic study used data from 206,929 women aged 40–74 years in the British Columbia Breast Screening Program. Participants were screened with full-field digital mammography (FFDM) between 2013 and 2019, with follow-up for incident breast cancers through June 2023 [2].
- Prediction Model & Exposure: The core exposure was an AI-generated mammogram risk score (MRS). The model was "dynamic," meaning it incorporated not just the most current mammogram but also up to four years of prior screening images to capture temporal changes in breast tissue [2].
- Outcomes & Analysis: The primary outcome was the 5-year risk of breast cancer, assessed using the area under the receiver operating characteristic curve (AUROC). Performance was evaluated overall and across subgroups defined by race, ethnicity, and age. Calibration (the agreement between predicted and observed risks) was also assessed [2].
Key Experimental Findings and Performance Data
The study yielded quantitative results that demonstrate the model's performance in a diverse, real-world setting. The data in the table below summarizes the key outcomes.
| Performance Metric | Overall Performance | Performance in Racial/Ethnic Subgroups | Performance by Age |
|---|---|---|---|
| 5-Year AUROC (95% CI) | 0.78 (0.77–0.80) [2] | East Asian: 0.77 (0.75–0.79)Indigenous: 0.77 (0.71–0.83)South Asian: 0.75 (0.71–0.79)White: Consistent performance [2] | ≤50 years: 0.76 (0.74–0.78)>50 years: 0.80 (0.78–0.82) [2] |
| Comparative Performance | Incorporating prior images (dynamic MRS) improved prediction compared to using a single mammogram time point (static MRS) [2]. | Performance was consistent across racial and ethnic groups, demonstrating generalizability [2]. | The model showed robust performance across different age groups [2]. |
| Risk Stratification | 9.0% of participants had a 5-year risk >3%; positive predictive value was 4.9% with an incidence of 11.8 per 1000 person-years [2]. | Not specified for individual subgroups. | Not specified for individual age categories. |
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key resources and methodologies used in the featured breast cancer risk prediction study and the broader field.
| Research Reagent / Material | Function in Prediction Model Research |
|---|---|
| Full-Field Digital Mammography (FFDM) Images | Served as the primary input data for the AI algorithm. The use of current and prior images enabled the dynamic assessment of breast tissue changes over time [2]. |
| Provincial Cancer Registry (e.g., British Columbia Cancer Registry) | Provided the definitive outcome data (pathology-confirmed incident breast cancers) for model training and validation through record linkage, ensuring accurate endpoint ascertainment [2]. |
| AI-Based Mammogram Risk Score (MRS) Algorithm | The core analytical tool that extracts features from mammograms and computes an individual risk score. The dynamic model leverages longitudinal data for improved accuracy [2]. |
| TRIPOD+AI Checklist | Provides the essential reporting framework to ensure the model's development, validation, and performance are described transparently and completely, facilitating critical appraisal and replication [33]. |
| Color-Blind Friendly Palette (e.g., Wong's palette) | A resource for creating accessible data visualizations, ensuring that charts and graphs conveying model performance are interpretable by all researchers, including those with color vision deficiencies [34]. |
Workflow Diagram for Validating a Cancer Risk Prediction Model
The following diagram, generated with Graphviz, illustrates the logical workflow for the external validation of a cancer risk prediction model across diverse populations, as demonstrated in the case study.
Diagram 1: Validation workflow for a cancer risk prediction model.
The evolution from TRIPOD to TRIPOD+AI represents a critical adaptation to the methodological advances in prediction modeling. For researchers validating cancer risk models across diverse populations, adhering to these reporting guidelines is not merely a matter of publication compliance but a cornerstone of scientific integrity. Transparent reporting, as exemplified by the breast cancer risk study, allows the scientific community to properly assess a model's performance, understand its limitations across different sub-groups, and determine its potential for clinical implementation to achieve equitable healthcare outcomes.
The clinical implementation of artificial intelligence (AI)-based cancer risk prediction models hinges on their generalizability across diverse populations and healthcare settings. A critical step in this process is external validation, where a model's performance is evaluated in a distinct population not used for its development [1]. This case study examines the successful external validation of a dynamic breast cancer risk prediction model within the province-wide, organized British Columbia Breast Screening Program [2]. This validation provides a robust template for assessing model performance across racially and ethnically diverse groups, a known challenge in the field where models developed on homogeneous populations often see performance drops when applied more broadly [2] [7].
The validated model is a dynamic risk prediction tool that leverages AI to analyze serial screening mammograms. Its core innovation lies in incorporating not just a single, current mammogram, but up to four years of prior screening images to forecast a woman's five-year future risk of breast cancer. This approach captures temporal changes in breast parenchyma, such as textural patterns and density, which are significant long-term risk indicators [2].
The primary objective of this external validation study was to determine if the model's performance, previously validated in Black and White women in an opportunistic U.S. screening service, could be generalized to a racially and ethnically diverse population within a Canadian government-organized screening program that operates with biennial digital mammography starting at age 40 [2].
Methodology
Study Population and Data Source
The prognostic study utilized data from the British Columbia Breast Screening Program, drawing from a cohort of 206,929 women aged 40 to 74 who underwent screening mammography between January 1, 2013, and December 31, 2019 [2].
- Cohort Characteristics: The cohort had a mean age of 56.1 years and was racially diverse. Among the 118,093 women with self-reported race data, there were 34,266 East Asian, 1,946 Indigenous, 6,116 South Asian, and 66,742 White women [2].
- Outcome Ascertainment: Incident, pathology-confirmed breast cancer diagnoses were identified through linkage to the provincial British Columbia Cancer Registry, with follow-up through June 2023. The mean follow-up time was 5.3 years, during which 4,168 cancers were diagnosed [2].
Experimental Protocol and Workflow
The model validation followed a rigorous protocol for external validation of a prognostic prediction model. Table 1 summarizes the key components of the experimental methodology.
Table 1: Summary of Experimental Protocol for External Validation
| Component | Description |
|---|---|
| Model Input | The four standard views of full-field digital mammograms (FFDM) from the current screening visit and prior visits within a 4-year window [2]. |
| Index Prediction | A dynamic mammogram risk score (MRS) generated by an AI algorithm analyzing changes in mammographic texture over time [2]. |
| Primary Outcome | The 5-year risk of breast cancer, assessed using the Area Under the Receiver Operating Characteristic Curve (AUROC) [2]. |
| Performance Metrics | Discrimination (5-year AUROC), calibration (predicted vs. observed risk), and clinical risk stratification (absolute risk) [2]. |
| Comparative Models | The dynamic model was compared against simpler models: age only; a static model using only the current mammogram; and prior mammograms only [2]. |
| Stratified Analyses | Performance was evaluated across subgroups defined by race and ethnicity, age (≤50 vs. >50 years), and breast density [2]. |
The following diagram illustrates the sequential workflow of the external validation process.
The Scientist's Toolkit: Research Reagent Solutions
The successful execution of this large-scale validation study relied on several key resources and methodologies, which can be considered essential "research reagents" for similar endeavors in the field. Table 2 details these critical components.
Table 2: Key Research Reagent Solutions for External Validation Studies
| Tool / Resource | Function in the Validation Study |
|---|---|
| Provincial Tumor Registry | Served as the definitive, independent data source for verifying the primary outcome (incident breast cancer) via data linkage, ensuring objective endpoint ascertainment [2]. |
| Full-Field Digital Mammograms (FFDM) | The raw imaging data used as direct input for the AI model. Standardized imaging protocols across the screening program were essential for consistent feature extraction [2]. |
| Dynamic Prediction Methodology | A statistical framework that uses repeated measurements (longitudinal mammograms) to estimate coefficients linking these time-series predictors to the outcome of interest [2]. |
| TRIPOD Reporting Guideline | The Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis guideline was followed, ensuring comprehensive and standardized reporting of the study methods and findings [2]. |
| Bootstrapping (5000 samples) | A resampling technique used to calculate robust 95% confidence intervals and p-values for performance metrics, accounting for uncertainty in the estimates [2]. |
Results and Performance Data
Primary Validation Outcomes
The external validation demonstrated that the dynamic model maintained high discriminatory performance in the new population. The primary results are summarized in Table 3.
Table 3: Primary Performance Results of the Dynamic Risk Model in External Validation
| Performance Measure | Result | Context/Comparison |
|---|---|---|
| Overall 5-year AUROC | 0.78 (95% CI: 0.77-0.80) | Analysis based on mammogram images alone. |
| Performance vs. Static Model | Improved prediction vs. single time-point mammogram. | Consistent with prior findings that serial images enhance accuracy [2]. |
| Positive Predictive Value (PPV) | 4.9% | For the 9.0% of participants with a 5-year risk >3%. |
| Incidence in High-Risk Group | 11.8 per 1000 person-years | - |
Performance Across Racial, Ethnic, and Age Subgroups
A critical finding was the consistency of the model's performance across diverse demographic groups, as detailed in Table 4.
Table 4: Model Performance (5-year AUROC) Across Racial, Ethnic, and Age Subgroups
| Subgroup | AUROC | 95% Confidence Interval |
|---|---|---|
| East Asian Women | 0.77 | 0.75 - 0.79 |
| Indigenous Women | 0.77 | 0.71 - 0.83 |
| South Asian Women | 0.75 | 0.71 - 0.79 |
| White Women | Consistent with overall performance | (Reported as consistent) |
| Women Aged ≤50 years | 0.76 | 0.74 - 0.78 |
| Women Aged >50 years | 0.80 | 0.78 - 0.82 |
Discussion
Interpretation of Findings
The successful external validation of this dynamic AI model within the British Columbia screening program provides a compelling case study in achieving generalizability. The model demonstrated robust and consistent discriminatory performance across all racial and ethnic subgroups analyzed, a notable achievement given that many AI models exhibit degraded performance when applied to populations underrepresented in their training data [2] [7]. This underscores the model's potential for equitable application in multi-ethnic screening programs.
Furthermore, the improved performance over static, single-time-point models highlights the prognostic value of tracking mammographic change over time. By capturing the evolution of breast tissue texture, the dynamic model accesses a richer set of predictive information, moving beyond a snapshot assessment to a longitudinal risk trajectory [2].
Research Implications
This case study offers a blueprint for the rigorous external validation required before clinical implementation of AI tools. It emphasizes that validation must:
- Be conducted in a setting that mirrors the intended use environment (e.g., an organized screening program).
- Involve a population that is both large and demographically diverse to thoroughly assess generalizability.
- Adhere to rigorous methodological and reporting standards, such as the TRIPOD guideline [2] [1].
Future research should focus on the long-term clinical utility of such models for personalizing screening intervals and prevention strategies, and on continued post-deployment monitoring to ensure sustained performance across populations [1].
Incorporating Genetic and Biomarker Data into Validation Protocols
The landscape of cancer risk prediction has fundamentally transformed, moving from models based solely on demographic and lifestyle factors to sophisticated integrative frameworks that incorporate genetic and biomarker data. This evolution is critical for enhancing early detection, enabling personalized prevention strategies, and improving the allocation of healthcare resources. The validation of these advanced models, particularly across diverse populations, represents a central challenge and opportunity in modern oncology research. This guide objectively compares contemporary approaches for integrating multi-scale data into robust validation protocols, providing researchers and drug development professionals with a comparative analysis of methodologies, performance metrics, and practical implementation frameworks.
Comparative Analysis of Contemporary Validation Studies
Recent landmark studies demonstrate the field's progression toward integrating multiple data types and employing advanced machine learning for validation. The table below summarizes the design and scope of three distinct approaches.
Table 1: Comparison of Recent Cancer Risk Prediction Model Studies
| Study / Model | Primary Data Types Integrated | Study Design & Population | Key Validation Approach | Cancer Types Targeted |
|---|---|---|---|---|
| FuSion Model [35] [36] | 54 blood biomarkers & 26 epidemiological exposures | Prospective cohort; 42,666 individuals in China | Discovery/validation cohort split; prospective clinical follow-up | Multi-cancer (Lung, Esophageal, Gastric, Liver, Colorectal) |
| Bladder Cancer DM Model [37] | Clinical risk factors & transcriptomic data (ADH1B) | Retrospective; SEER database & external validation cohort | Internal/external validation; machine learning biomarker discovery | Bladder Cancer (Distant Metastasis) |
| Colombian BCa PRS Model [38] | Polygenic Risk Score (PRS), clinical & imaging data | Case-control; 1,997 Colombian women | Ancestry-specific PRS validation in an admixed population | Sporadic Breast Cancer |
Each model reflects a different strategy for data integration and validation. The FuSion Model emphasizes a high volume of routine clinical biomarkers validated in a large, prospective population-based setting [35] [36]. In contrast, the Bladder Cancer DM Model leverages a public national registry and couples it with a focused, machine-learning-driven discovery of a single, potent biomarker (ADH1B) [37]. The Colombian BCa PRS Model addresses a critical gap in the field by focusing on the performance of genetic tools in an under-represented, admixed population, highlighting that polygenic risk scores (PRS) must be adapted and validated for specific ancestral backgrounds to be clinically useful [38].
Quantitative Performance Metrics Across Models
The predictive accuracy and clinical utility of a model are ultimately quantified using standardized metrics. The following table compares the performance outcomes of the featured studies.
Table 2: Comparative Model Performance and Clinical Yield
| Study / Model | Key Predictive Performance (AUC) | Clinical Utility / Risk Stratification | Reported Calibration |
|---|---|---|---|
| FuSion Model [35] [36] | 0.767 (95% CI: 0.723-0.814) for 5-year risk | High-risk group (17.19% of cohort) accounted for 50.42% of cancers; 15.19x increased risk vs low-risk. | Not explicitly reported |
| Bladder Cancer DM Model [37] | Training: 0.732; Internal Val.: 0.750; External Val.: 0.968 | Nomogram identifies risk factors (tumor size ≥3 cm, N1-N3, lack of surgery). | Calibration curves showed good predictive accuracy |
| Colombian BCa PRS Model [38] | PRS alone: 0.72; PRS + Clinical/Imaging: 0.79 | Combined model significantly enhanced risk stratification in Admixed American women. | Not explicitly reported |
The performance data reveals several key insights. The FuSion Model demonstrates strong performance in a multi-cancer context, with a high Area Under the Curve (AUC) and impressive real-world clinical yield, where following high-risk individuals led to a cancer or precancerous lesion detection rate of 9.64% [35] [36]. The Bladder Cancer DM Model showcases an exceptionally high AUC in external validation (0.968), though this may be influenced by the specific, smaller cohort used [37]. The step-wise improvement in the Colombian BCa PRS Model, where adding PRS to clinical data boosted the AUC from 0.66 to 0.79, provides quantitative evidence for the power of integrated data types over single-modality assessments [38].
Detailed Experimental Protocols for Validation
A robust validation protocol is foundational to generating credible and generalizable models. This section details the core methodologies employed in the cited studies.
Protocol 1: Prospective Population-Based Cohort Validation
The FuSion study provides a template for large-scale validation of a biomarker-centric model [35] [36].
- Cohort Recruitment and Splitting: The protocol initialized with 42,666 participants, divided into a discovery cohort (n=16,340) and an independent validation cohort (n=26,308). This pre-specified split ensures that the model's performance is tested on data not used in its development.
- Data Preprocessing: Rigorous handling of missing data was employed, excluding variables with >20% missingness and using the K-nearest neighbors (KNN) algorithm for imputation. Extreme values were winsorized (values below 0.1st and above 99.9th percentiles excluded), and continuous biomarkers were Z-score standardized.
- Model Training and Feature Selection: Five supervised machine learning approaches were used. A LASSO-based feature selection strategy identified the most informative predictors, ultimately yielding a parsimonious model containing four key biomarkers, age, sex, and smoking intensity.
- Outcome Assessment and Follow-up: Cancer outcomes were rigorously defined using ICD-10 codes and confirmed via pathology reports and imaging. A prospective clinical follow-up of 2,863 high-risk subjects was conducted using advanced screening methods (e.g., LDCT, endoscopy) to assess the model's yield rate in detecting new cancers or precancerous lesions.
Protocol 2: Retrospective Registry Data with Biomarker Discovery
This protocol, used in the bladder cancer study, leverages existing datasets for discovery and initial validation [37].
- Data Sourcing and Harmonization: Clinical data for patients with muscle-invasive bladder cancer were retrieved from the SEER database (training/internal validation) and an external hospital cohort (external validation). Variables were harmonized between databases using standardized coding.
- Nomogram Construction and Validation: Independent risk factors for distant metastasis were identified via univariate and multivariate logistic regression. These factors were incorporated into a nomogram. The model's discriminative ability was compared to traditional staging systems using AUC, and calibration was assessed with calibration curves.
- Machine Learning Biomarker Discovery: A separate transcriptomic analysis pipeline was executed. Four bladder cancer datasets (GSE13507, GSE37817, GSE166716, GSE256292) were obtained from GEO, underwent batch effect removal and normalization. LASSO regression and Random Forest algorithms were applied to this training cohort to identify potential biomarker genes like ADH1B, which was then validated using TCGA-BLCA data.
Protocol 3: Ancestry-Specific Polygenic Risk Score Validation
This protocol is essential for ensuring the equity and generalizability of genetic tools [38].
- Ancestry Estimation and Cohort Stratification: Genetic ancestry of participants is estimated using reference datasets (e.g., 1000 Genomes Project) and tools like iAdmix. Participants are classified into genetic ancestry groups (e.g., Admixed American, African, European).
- PRS Development and Training: Ancestry-specific PRS are developed using genome-wide association study (GWAS) summary statistics from corresponding populations. The scores are trained and tested on multi-ancestry cohorts (e.g., UK Biobank, MESA) to optimize their parameters.
- Integrated Model Evaluation: The predictive ability of the PRS is assessed alone and in combination with clinical risk factors (e.g., breast density, family history). The AUC is calculated for each model to quantify the improvement gained by data integration. This validation is performed within the specific target population (e.g., Colombian women).
The following workflow diagram synthesizes these protocols into a generalized validation pipeline for genetic and biomarker data.
Generalized Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
The successful execution of these validation protocols relies on a suite of specialized research reagents and technological platforms. The table below catalogs key solutions used in the featured studies.
Table 3: Key Research Reagent Solutions for Validation Studies
| Category / Item | Specific Examples / Platforms | Primary Function in Validation |
|---|---|---|
| Biomarker Analysis Platforms | ELISA, Meso Scale Discovery (MSD), Luminex, GyroLab [39] | Multiplexed, quantitative measurement of protein biomarkers from blood samples. |
| Genomic Analysis Platforms | RT-PCR, qPCR, Next-Generation Sequencing (NGS), RNA-Seq [39] | Targeted and comprehensive analysis of genetic variants and gene expression. |
| Cohort & Data Resources | SEER Database, UK Biobank, GEO, TCGA [37] [38] | Provide large-scale, well-characterized clinical, genomic, and outcome data for model development and validation. |
| Computational & ML Tools | LASSO Regression, Random Forest, CatBoost, R software, glmnet package [35] [37] [40] | Perform feature selection, model training, and statistical validation. |
| Ancestry Determination Tools | iAdmix, Principal Component Analysis (PCA), 1000 Genomes Project [38] | Estimate genetic ancestry to ensure population-specific model calibration. |
The selection of platforms involves critical trade-offs. For biomarker analysis, ELISA and qPCR offer established, cost-effective protocols, while MSD and Luminex provide superior multiplexing capabilities for profiling complex analyte signatures [39]. In genomic analysis, NGS and RNA-Seq are indispensable for comprehensive discovery, but qPCR remains a gold standard for validating specific targets. The use of large public databases like SEER and UK Biobank is crucial for powering retrospective studies, but must be supplemented with targeted, prospective cohorts from diverse backgrounds to overcome generalizability limitations [37] [38].
The integration of genetic and biomarker data into validation protocols is no longer a speculative endeavor but an established paradigm for advancing cancer risk prediction. The comparative analysis presented in this guide demonstrates that while methodologies may differ—ranging from massive prospective biomarker collections to focused ancestry-specific PRS validation—the core principles of rigorous cohort splitting, transparent data preprocessing, and comprehensive performance evaluation are universal. The future of the field, as highlighted by these studies, points toward even greater integration of multi-omics data, the mandatory inclusion of diverse populations in validation workflows, and the continued refinement of machine learning techniques to unravel the complex interplay between genetics, biomarkers, and cancer risk. This will ensure that predictive models are not only statistically powerful but also equitable and impactful in real-world clinical and public health settings.
Overcoming Validation Challenges: Strategies to Enhance Model Robustness and Generalizability
Addressing Spectrum Bias and Over-Optimism in Model Performance
Cancer risk prediction models are pivotal for identifying high-risk individuals, enabling targeted screening and early intervention strategies. However, their real-world clinical impact is often limited by two pervasive methodological issues: spectrum bias and performance over-optimism. Spectrum bias occurs when a model is developed in a population that does not adequately represent the spectrum of individuals in whom it will be applied, particularly concerning demographic, genetic, and clinical characteristics [41]. Over-optimism arises when model performance is estimated from the same data used for development, without proper validation techniques, leading to inflated performance metrics [42] [43]. These challenges are particularly acute in oncology, where risk prediction influences critical decisions from prevention to treatment selection [1]. This guide objectively compares validation methodologies and performance metrics across cancer types, providing researchers with experimental frameworks for robust model evaluation.
Quantitative Performance Comparison Across Cancer Types
Extensive reviews reveal consistent patterns in the performance and validation status of risk prediction models across major cancer types. The table below synthesizes quantitative performance data and validation maturity from recent systematic reviews and meta-analyses.
Table 1: Comparative Performance of Cancer Risk Prediction Models
| Cancer Type | Number of Models Identified | Typical AUC Range | Models with External Validation | Key Limitations Documented |
|---|---|---|---|---|
| Lung [44] | 54 | 0.698 - 0.748 | Multiple (PLCOM2012, Bach, Spitz) | Limited validation in Asian populations; few models for never-smokers |
| Breast [21] | 107 | 0.51 - 0.96 | 18 | Majority developed in Caucasian populations; variable quality |
| Endometrial [41] | 9 | 0.64 - 0.77 | 5 | Homogeneous development populations; limited generalizability |
| Gastric [1] | >100 | Not consistently reported | Limited | Proliferation without clinical implementation; most not validated |
The performance metrics demonstrate that while some models achieve good discrimination (AUC > 0.8), many exhibit only moderate performance (AUC 0.7-0.8). The proportion of models undergoing external validation remains concerningly low across cancer types, particularly for breast cancer where only 17% (18/107) of developed models have been externally validated [21]. The highest performing validated model is PLCOM2012 for lung cancer (AUC = 0.748), though its performance is specific to Western populations and may not generalize to Asian contexts [44].
Table 2: Impact of Predictor Types on Model Performance
| Predictor Category | Example Cancer Types | Performance Impact | Implementation Considerations |
|---|---|---|---|
| Demographic & Clinical | All cancer types | Baseline performance (AUC ~0.6-0.75) | Widely available but limited discrimination |
| Genetic (PRS/SNPs) [41] [21] | Breast, Endometrial | Moderate improvement (+0.02-0.05 AUC) | Cost, accessibility, ethnic variability in PRS |
| Imaging/Biopsy Data [21] | Breast | Substantial improvement (AUC up to 0.96) | Resource-intensive, requires specialist interpretation |
| Blood Biomarkers [3] | Multiple (Pan-cancer) | Significant improvement (e.g., +0.032 AUC for any cancer) | Routine collection, standardized assays |
Incorporating multiple predictor types generally enhances performance, though with diminishing returns. For breast cancer, models combining demographic and genetic or imaging data outperformed those using demographic variables alone, though adding multiple complex data types did not substantially further improve performance [21]. For endometrial cancer, only 4 of 9 models incorporated polygenic risk scores, and just one utilized blood biomarkers [41].
Experimental Protocols for Model Validation
Internal Validation Techniques
Robust internal validation is essential before proceeding to external validation. The following experimental protocols have been systematically evaluated for high-dimensional cancer prediction models:
Cross-Validation Procedures:
- k-Fold Cross-Validation: Recommended for Cox penalized regression models in high-dimensional settings (e.g., transcriptomic data with 15,000 features). The dataset is randomly partitioned into k subsets (typically k=5 or 10). The model is trained on k-1 folds and validated on the remaining fold, rotating until all folds have served as validation [43].
- Nested Cross-Validation: Employed when both model selection and hyperparameter tuning are required. Consists of an inner loop for parameter optimization and an outer loop for error estimation. Particularly valuable for small sample sizes (n < 500) but exhibits performance fluctuations depending on the regularization method [43].
Alternative Internal Validation Methods:
- Bootstrap Validation: Conventional bootstrap tends to be over-optimistic, while the 0.632+ bootstrap correction is often overly pessimistic, particularly with small samples (n = 50 to n = 100) [43].
- Train-Test Split: Simple random splitting (e.g., 70% training, 30% testing) shows unstable performance, especially with limited samples, and is not recommended for high-dimensional cancer data [43].
Table 3: Internal Validation Method Performance with High-Dimensional Data
| Validation Method | Recommended Sample Size | Stability | Risk of Optimism | Computational Intensity |
|---|---|---|---|---|
| Train-Test Split | >1000 | Low | High | Low |
| Bootstrap (conventional) | >500 | Moderate | High (over-optimistic) | Moderate |
| Bootstrap (0.632+) | >500 | Moderate | High (over-pessimistic) | Moderate |
| k-Fold Cross-Validation | >100 | High | Low | Moderate |
| Nested Cross-Validation | 50-500 | Moderate | Low | High |
Experimental evidence from simulation studies using transcriptomic data from the SCANDARE head and neck cohort (NCT03017573) demonstrates that k-fold cross-validation provides the optimal balance between bias and stability for internal validation of Cox penalized models with time-to-event endpoints [43].
External Validation Protocols
External validation assesses model generalizability to entirely independent populations and settings. The recommended protocol includes:
Cohort Selection Criteria:
- Temporal Validation: Using data from the same institutions but different time periods
- Geographical Validation: Application to populations from different regions or countries
- Domain Validation: Testing in populations with different clinical characteristics or risk profiles
Performance Assessment Metrics:
- Discrimination: C-statistic or AUC with 95% confidence intervals
- Calibration: Observed-to-expected (O/E) ratio or calibration plots
- Clinical Utility: Decision curve analysis to evaluate net benefit across risk thresholds
For lung cancer models, external validation of PLCOM2012 (AUC = 0.748; 95% CI: 0.719-0.777) demonstrated superior performance compared to Bach (AUC = 0.710; 95% CI: 0.674-0.745) and Spitz models (AUC = 0.698; 95% CI: 0.640-0.755) [44]. A recent pan-cancer algorithm development study validated models in two separate cohorts totaling over 5 million people, demonstrating consistent performance across subgroups defined by ethnicity, age, and geographical area [3].
Visualizing Bias and Validation Relationships
The diagram below illustrates the interconnected relationship between bias sources, their consequences for model performance, and recommended validation strategies to mitigate these issues.
This framework visualizes how methodological limitations in development lead to specific performance issues, each requiring targeted validation approaches. The reverse arrows indicate how proper validation can retrospectively identify and help correct these biases.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagents and Methodological Solutions for Robust Model Validation
| Tool Category | Specific Solution | Function | Implementation Example |
|---|---|---|---|
| Statistical Software | R (version 4.4.0+) | Model development and validation | Simulation studies for internal validation methods [43] |
| Validation Frameworks | PROBAST Tool | Risk of bias assessment | Quality appraisal of prediction model studies [44] [21] |
| Reporting Guidelines | TRIPOD+AI Checklist | Transparent reporting of model development | Ensuring complete reporting of discrimination and calibration [41] [1] |
| Data Resources | Large Electronic Health Records (e.g., QResearch) | Model derivation and validation | Development of algorithms for 15 cancer types using 7.46 million patients [3] |
| Performance Assessment | Time-dependent AUC | Discrimination assessment with time-to-event data | Evaluation of Cox penalized regression models [43] |
| Calibration Metrics | Observed/Expected (O/E) Ratio | Absolute risk prediction accuracy | Assessment of model calibration in breast cancer prediction [21] |
Addressing spectrum bias and over-optimism requires methodologically rigorous approaches throughout the model development lifecycle. Key strategies include prospective design with diverse participant recruitment, robust internal validation using k-fold cross-validation, and comprehensive external validation across geographically and demographically distinct populations. The integration of novel data types, particularly genomic information and routinely collected blood biomarkers, shows promise for enhancing predictive performance while introducing new generalizability challenges. Future efforts should focus on the implementation of validated models in diverse clinical settings, with ongoing monitoring to ensure maintained performance across population subgroups. By adhering to these methodological standards, researchers can develop cancer risk prediction tools that genuinely translate into improved early detection and prevention outcomes across diverse populations.
Technical Solutions for Models with Weak Discriminatory Accuracy (AUC < 0.65)
The validation of cancer risk prediction models across diverse populations is a critical endeavor in modern oncology research. Accurate risk stratification is foundational for implementing effective screening programs, enabling personalized prevention strategies, and ultimately improving patient outcomes. Despite advances in predictive analytics, many models, particularly those relying on traditional statistical methods or limited feature sets, demonstrate weak discriminatory accuracy, often evidenced by an Area Under the Curve (AUC) of less than 0.65. Such performance is generally considered insufficient for reliable clinical application. This guide objectively compares technical solutions that have been empirically demonstrated to enhance model performance, providing researchers and drug development professionals with validated methodologies to overcome this significant challenge. The focus is on scalable, data-driven approaches that improve accuracy while maintaining generalizability across diverse patient demographics.
Comparative Performance of Technical Solutions
The following table summarizes quantitative data from recent studies that implemented specific technical solutions to improve model performance, providing a clear comparison of their effectiveness.
Table 1: Performance Improvement of Technical Solutions for Cancer Risk Prediction
| Technical Solution | Cancer Type | Base Model/Feature Set Performance (AUC) | Enhanced Model Performance (AUC) | Key Technologies/Methods Employed |
|---|---|---|---|---|
| Stacking Ensemble Models [45] | Lung | 0.858 (Logistic Regression) | 0.887 (Stacking Model) | LightGBM, XGBoost, Random Forest, Multi-layer Perceptron (MLP) |
| Multi-modal Data Fusion [46] [47] | Colorectal | 0.615 (Direct Prediction from Images) | 0.672 (WSI + Clinical Data) | Transformer-based Image Analysis, Multi-modal Fusion Strategies |
| AI-Based Mammogram Analysis [48] | Breast | ~0.57 (Traditional Clinical Models, e.g., IBIS, BCRAT) | 0.68 (Deep Learning on Mammograms) | Deep Learning, Prior Mammogram Integration (Mammogram Risk Score - MRS) |
| Advanced Data Preprocessing [49] | Breast | Not Explicitly Stated (Lower performance with raw data) | F1-Score: 0.947 (After Box-Cox Transformation) | Box-Cox Transformation, Synthetic Minority Over-sampling Technique (SMOTE) |
| Machine Learning (vs. Classical Models) [45] | Lung | ~0.70 (Classical LLP/PLCO Models) | 0.858 (Logistic Regression with expanded features) | Epidemiological Questionnaires, Logistic Regression |
Detailed Experimental Protocols and Methodologies
Implementation of Stacking Ensemble Models
Objective: To significantly improve lung cancer risk prediction by leveraging a stacking ensemble of machine learning models to capture complex, non-linear relationships in epidemiological data [45].
Materials & Workflow:
- Data Source: A case-control dataset comprising 5,421 lung cancer cases and 10,831 matched controls.
- Data Preprocessing:
- Features with >25% missing values were excluded.
- Remaining missing values were imputed using the
missForestR package, which handles mixed-data types and non-linear relationships. - Categorical variables were one-hot encoded.
- Continuous variables were normalized using Z-score standardization.
- Base Learners: A diverse set of eight machine learning models was trained and optimized via 5-fold cross-validation:
- Regularized Logistic Regression (LogiR)
- Random Forest (RF)
- Light Gradient-Boosting Machine (LightGBM)
- Extreme Gradient Boosting (XGBoost)
- Extra Trees (ET)
- Adaptive Boosting (AdaBoost)
- Gradient Boosting Decision Tree (GBDT)
- Support Vector Machine (SVM)
- Meta-Learner: The predictions from the base learners were used as input features to train a final logistic regression model (the meta-learner) to generate the ultimate prediction.
- Evaluation: Model performance was assessed on a held-out test set (10% of the data) using AUC, accuracy, and recall.
Figure 1: Workflow for Building a Stacking Ensemble Model
Multi-modal Fusion of Histopathology and Clinical Data
Objective: To enhance the prediction of 5-year colorectal cancer progression risk by integrating features from whole-slide images (WSI) with structured clinical data [46] [47].
Materials & Workflow:
- Data Source: The New Hampshire Colonoscopy Registry, including longitudinal follow-up data.
- Image Feature Extraction:
- A transformer-based deep learning model was adapted for histopathology image analysis.
- The model was trained to predict intermediate clinical variables, a strategy that improved final risk prediction compared to direct end-to-end training.
- Non-Imaging Features: Clinical variables from medical records were extracted and processed.
- Fusion Strategy: Deep learning-derived image features were combined with the non-imaging clinical features using multi-modal fusion strategies. This integrated feature set was used to train the final risk prediction model.
- Evaluation: Performance was measured by the AUC for predicting 5-year progression risk and compared against models using only images or only clinical data.
Deep Learning for Mammogram-Based Risk Assessment
Objective: To create a more accurate and equitable 5-year breast cancer risk prediction model using deep learning applied to mammography images [48] [50].
Materials & Workflow:
- Data Source: 206,929 women from the British Columbia Breast Screening Program, a diverse population including East Asian, Indigenous, South Asian, and White women.
- AI Model Training:
- A deep learning model was trained to analyze mammogram images.
- A key innovation was the incorporation of up to four years of prior mammograms, creating a dynamic Mammogram Risk Score (MRS) that leverages temporal changes.
- Validation: The model was validated on a large, independent, multi-ethnic cohort. Its performance was compared to traditional risk models like Tyrer-Cuzick (IBIS) and the Breast Cancer Risk Assessment Tool (BCRAT).
- Evaluation: The primary metric was the 5-year AUC. The model was also assessed for consistency across different racial and ethnic subgroups.
The Scientist's Toolkit: Key Research Reagents and Solutions
The following table details essential materials, computational tools, and data sources critical for implementing the described technical solutions.
Table 2: Essential Research Reagents and Solutions for Model Improvement
| Item Name/Type | Function/Purpose | Example Implementation |
|---|---|---|
| Epidemiological Questionnaires | Collects comprehensive demographic, behavioral, and clinical risk factor data for model feature space expansion [45]. | Used to gather data on smoking, diet, occupational exposure, and medical history for lung cancer risk prediction [45]. |
| missForest R Package | Accurately imputes missing data in mixed-type (continuous & categorical) datasets, preserving complex variable interactions [45]. | Employed for data preprocessing before model training to handle missing values without introducing significant bias [45]. |
| Transformer-Based Image Models | Analyzes high-resolution whole-slide images (WSI) to extract rich, prognostically relevant feature sets [46] [47]. | Adapted for histopathology image analysis in colorectal cancer to predict progression risk from polyp images [46]. |
| Box-Cox Transformation | A power transformation technique that stabilizes variance and normalizes skewed data distributions, improving model performance [49]. | Applied to preprocess the SEER breast cancer dataset, enhancing the accuracy of ensemble models like stacking [49]. |
| LightGBM / XGBoost | High-performance, gradient-boosting frameworks effective for tabular data, capable of capturing complex non-linear patterns [45]. | Served as powerful base learners in a stacking ensemble for lung cancer prediction [45]. |
| Multi-modal Fusion Architectures | Combines feature vectors from disparate data types (e.g., images, clinical records) into a unified, more predictive model [46] [47]. | Used to fuse WSI-derived features with clinical variables for improved colorectal cancer risk stratification [46]. |
Figure 2: Core Components of an Improved Risk Prediction Framework
The empirical data clearly demonstrates that overcoming weak discriminatory accuracy in cancer risk models requires moving beyond traditional approaches. Solutions such as stacking ensemble models, multi-modal data fusion, and deep learning on medical images have proven capable of boosting AUC values from marginal levels (e.g., <0.65) to more clinically actionable ranges (≥0.68 to 0.89). The consistent theme across successful methodologies is the integration of diverse, high-dimensional data and the application of sophisticated algorithms capable of identifying complex, non-linear patterns. For researchers focused on validating models across diverse populations, these technical solutions offer a validated pathway to developing robust, equitable, and accurate prediction tools that can reliably inform screening protocols and personalized intervention strategies.
Dynamic risk prediction represents a paradigm shift in oncology, moving beyond static assessments by incorporating longitudinal data to update an individual's probability of developing cancer as new information becomes available. Unlike traditional models that provide a single risk estimate based on a snapshot in time, dynamic models leverage temporal patterns in biomarkers, imaging features, and clinical measurements to offer updated forecasts throughout a patient's clinical journey. This approach more closely mimics clinical reasoning, where physicians continuously revise prognoses based on changes in patient status [51]. The validation of these models across diverse populations is crucial for ensuring equitable cancer prevention and early detection strategies, particularly as healthcare systems worldwide increasingly adopt personalized, risk-adapted screening protocols [2] [52].
Comparative Performance of Dynamic Risk Prediction Models
Quantitative Performance Metrics Across Model Architectures
Table 1: Performance comparison of dynamic risk prediction models for breast cancer
| Model Name | Architecture/Approach | Data Input | Prediction Window | AUC/AUROC | Study Population |
|---|---|---|---|---|---|
| Dynamic MRS Model [2] | AI-based mammogram risk score | Current + prior mammograms (up to 4 years) | 5-year risk | 0.78 (95% CI: 0.77-0.80) | 206,929 women (diverse racial/ethnic groups) |
| MTP-BCR Model [53] | Deep learning with multi-time point transformer | Longitudinal mammograms + risk factors | 10-year risk | 0.80 (95% CI: 0.78-0.82) | 9133 women (in-house dataset) |
| LongiMam [54] | CNN + RNN (GRU) | Up to 4 prior mammograms + current | Short-term risk | Improved prediction vs single-visit | Population-based screening dataset |
| Machine Learning Models (Pooled) [55] | Various ML algorithms (mostly neural networks) | Mixed (imaging + risk factors) | Variable (≤5 years to lifetime) | 0.73 (95% CI: 0.66-0.80) | 218,100 patients across 8 studies |
Performance Across Diverse Populations
A critical requirement for clinically useful risk prediction is generalizability across diverse populations. Recent studies have specifically addressed this challenge by validating models in multi-ethnic cohorts:
Table 2: Performance of dynamic MRS model across racial and ethnic groups [2]
| Population Group | Sample Size | 5-year AUROC | 95% Confidence Interval |
|---|---|---|---|
| Overall Cohort | 206,929 | 0.78 | 0.77-0.80 |
| East Asian Women | 34,266 | 0.77 | 0.75-0.79 |
| Indigenous Women | 1,946 | 0.77 | 0.71-0.83 |
| South Asian Women | 6,116 | 0.75 | 0.71-0.79 |
| White Women | 66,742 | 0.78 | 0.76-0.80 |
| Women ≤50 years | - | 0.76 | 0.74-0.78 |
| Women >50 years | - | 0.80 | 0.78-0.82 |
The consistent performance across racial and ethnic groups demonstrates the potential for broad clinical applicability of these models [2]. This is particularly significant given that previous models largely developed and validated on White populations have shown decreased performance when applied to other groups [55].
Experimental Protocols and Methodologies
Protocol for Dynamic Mammogram Risk Assessment
The dynamic Mammogram Risk Score (MRS) model exemplifies a rigorously validated approach for breast cancer risk prediction [2]:
Data Collection and Preprocessing:
- Collected full-field digital mammograms (FFDM) from population-based screening programs
- Standardized image acquisition across multiple sites (95% Hologic machines, 5% General Electric)
- Established minimum quality controls and exclusion criteria (e.g., no breast cancer diagnosis within first 6 months of cohort entry)
Model Architecture and Training:
- Input: Four standard views of digital mammograms (current and prior examinations)
- Incorporated up to 4 years of prior screening mammograms to forecast 5-year future risk
- Generated dynamic MRS based on changes in mammographic texture over time
- Used statistical methodology linking longitudinal predictors to outcomes through dynamic prediction algorithms
Validation Framework:
- External validation in province-wide screening program in British Columbia, Canada
- Assessment of discrimination (time-dependent AUROC), calibration, and risk stratification
- Bootstrapping with 5000 replicates to estimate 95% CIs
- Stratified analyses by race/ethnicity, age, breast density, and family history
Protocol for Multi-Time-Point Breast Cancer Risk Model
The MTP-BCR model employs an end-to-end deep learning approach specifically designed to capture temporal changes in breast tissue [53]:
Dataset Curation:
- Retrospective collection of longitudinal screening mammograms with at least one year of follow-up
- Inclusion of both cancer-free women and those diagnosed with breast cancer within 10 years
- Structured data as retrospective trajectories for each woman
Model Architecture:
- Multi-time point transformer to combine static and dynamic risk features
- Multi-level learning for breast-specific and patient-level risk assessment
- Multi-task learning incorporating clinical prior knowledge including radiologic features and risk factors
- Capability to handle 0-5 prior reference mammograms before target mammogram
Output and Interpretation:
- 10-year breast cancer risk prediction at both patient and unilateral breast level
- Generation of heatmaps to highlight suspicious areas and enhance clinical interpretability
- Simultaneous assessment of primary and recurring breast cancer risks
Dynamic Risk Prediction Workflow: This diagram illustrates the integration of longitudinal data with temporal analysis for dynamic risk assessment.
Statistical Frameworks for Longitudinal Analysis
Joint Modeling of Longitudinal and Survival Data
The jmBIG package provides a specialized statistical framework for dynamic risk prediction that addresses the unique challenges of longitudinal healthcare data [51]:
Theoretical Foundation:
- Joint longitudinal-survival models account for dependence between repeated measures and time-to-event outcomes
- Bivariate proportional hazards model: ( hi(t) = h0(t) \exp(xi' \beta + ui(t)) )
- Where ( h0(t) ) is baseline hazard, ( xi ) are covariates, and ( u_i(t) ) is a function of longitudinal data
Computational Innovations:
- Efficient, scalable implementations of joint modeling algorithms for large-scale healthcare datasets
- Bayesian estimation methods with parallel computing capabilities
- Handling of high-dimensionality and complex relationships between multiple outcomes
Clinical Implementation:
- Dynamic predictions updated as new longitudinal measurements become available
- Accounting for irregular observation times common in clinical practice
- Integration with electronic health records for real-time risk assessment
Comparison of Temporal Data Processing Methods
Table 3: Approaches for analyzing longitudinal data in cancer prediction [52]
| Method Category | Key Characteristics | Common Algorithms | Applications in Cancer Prediction |
|---|---|---|---|
| Feature Engineering | Manual creation of temporal features | Trend analysis, summary statistics | 16/33 studies in recent review |
| Deep Learning (Sequential) | Direct processing of time-series data | RNN, LSTM, GRU, Transformers | 18/33 studies in recent review |
| Joint Modeling | Simultaneous analysis of longitudinal and time-to-event data | Bayesian joint models, proportional hazards | Time-to-cancer prediction |
Computational Frameworks and Software
Table 4: Essential computational resources for dynamic risk prediction research
| Resource Name | Type | Primary Function | Application Context |
|---|---|---|---|
| jmBIG [51] | R Package | Joint modeling of longitudinal and survival data | Large-scale healthcare dataset analysis |
| LongiMam [54] | Deep Learning Framework | CNN + RNN for longitudinal mammogram analysis | Breast cancer risk prediction |
| MTP-BCR [53] | Deep Learning Model | Multi-time point risk prediction | Short-to-long-term breast cancer risk |
| PROBAST [55] [52] | Assessment Tool | Risk of bias evaluation for prediction models | Model validation and quality assessment |
Data Requirements and Specifications
Imaging Data Standards:
- Full-field digital mammograms (FFDM) in standard views (CC and MLO)
- Minimum resolution requirements for feature extraction
- Standardized preprocessing protocols (VOI LUT transformation, background removal)
- Temporal consistency in image acquisition parameters [54]
Longitudinal Data Structure:
- Regular follow-up intervals (typically annual screening)
- Minimum of 3-5 time points for meaningful trajectory analysis
- Consistent data elements across time points
- Handling of missing visits and irregular intervals [53] [54]
Clinical and Demographic Covariates:
- Age, race/ethnicity, family history
- Breast density measurements
- Prior biopsy history and results
- Menopausal status and reproductive factors [2] [53]
Data Requirements Framework: Essential components for developing dynamic risk prediction models.
Dynamic risk prediction models represent a significant advancement over traditional static approaches by leveraging longitudinal data to provide updated risk assessments that reflect the evolving nature of cancer development. The experimental evidence demonstrates that incorporating temporal information, particularly from sequential mammograms, substantially improves predictive performance across diverse populations. Models that integrate multiple time points through sophisticated deep learning architectures or joint modeling frameworks consistently outperform single-time-point assessments, achieving AUC values of 0.75-0.80 across racial and ethnic groups [2] [53].
The validation of these models in large, diverse populations is essential for their successful implementation in personalized screening programs. Future development should focus on enhancing model interpretability, standardizing evaluation metrics across studies, and addressing computational challenges associated with large-scale longitudinal data. As these dynamic approaches mature, they hold significant promise for transforming cancer screening from population-based to individually tailored protocols, ultimately improving early detection while reducing the harms of overscreening.
The integration of artificial intelligence (AI) with multi-modal data represents a transformative shift in cancer risk prediction. AI is revolutionizing oncology by systematically decoding complex patterns within vast datasets that are often imperceptible to conventional analysis [56]. This guide provides an objective comparison of how AI models leverage novel data types—particularly medical imaging and blood-based biomarkers—to enhance the accuracy, robustness, and clinical applicability of cancer risk assessment. A critical theme explored herein is the performance of these models across diverse populations, a key factor for equitable and effective clinical deployment. The convergence of advanced imaging analysis and AI-driven biomarker discovery is paving the way for a new era in precision oncology, enabling more personalized and proactive healthcare strategies [57].
Comparative Performance of AI Models in Cancer Detection and Risk Prediction
The performance of AI models varies significantly based on the data modality used, the specific cancer type, and the clinical task (e.g., screening vs. risk prediction). The tables below summarize key quantitative findings from recent studies, allowing for a direct comparison of model efficacy.
Table 1: Performance of AI Models in Cancer Detection from Medical Imaging
| Cancer Type | Imaging Modality | AI Task | Model/System Name | Sensitivity (%) | Specificity (%) | AUC | External Validation | Ref |
|---|---|---|---|---|---|---|---|---|
| Colorectal Cancer | Colonoscopy | Malignancy detection | CRCNet | 82.9 - 96.5 | 85.3 - 99.2 | 0.867 - 0.882 | Yes, multiple cohorts | [56] |
| Colorectal Cancer | Colonoscopy/Histopathology | Polyp classification (neoplastic vs. nonneoplastic) | Real-time image recognition system (SVM) | 95.9 | 93.3 | NR | No (single-center) | [56] |
| Breast Cancer | 2D Mammography | Screening detection | Ensemble of three DL models | +2.7% to +9.4% (vs. radiologists) | +1.2% to +5.7% (vs. radiologists) | 0.810 - 0.889 | Yes, UK model tested on US data | [56] |
| Breast Cancer | 2D/3D Mammography | Early cancer detection | Progressively trained RetinaNet | +14.2% to +17.5% (at avg. reader specificity) | +16.2% to +24.0% (at avg. reader sensitivity) | 0.927 - 0.971 | Yes, multiple international sites | [56] |
Table 2: Performance of AI Models in Cancer Risk Prediction Using Multimodal Data
| Study Focus | Data Modalities | Best Performing Model(s) | Reported Accuracy/Performance | Key Predictive Features Identified | Ref |
|---|---|---|---|---|---|
| General Cancer Risk Prediction | Lifestyle & Genetic Data | Categorical Boosting (CatBoost) | Test Accuracy: 98.75%, F1-score: 0.9820 | Personal history of cancer, Genetic risk level, Smoking status | [40] |
| Breast Cancer Risk Prediction (Systematic Review) | Demographic, Genetic, Imaging/Biopsy | Various (107 developed models) | AUC range: 0.51 - 0.96 | Models combining demographic & genetic or imaging data performed best | [8] |
| Pan-Cancer Risk Prediction Review | Lifestyle, Epidemiologic, EHR, Genetic | Ensemble Techniques (e.g., XGBoost, Random Forest) | Encouraging results, but many studies underpowered | Varied greatly; highlights need for large, diverse datasets | [58] |
| Acute Care Utilization in Cancer Patients | Electronic Health Records (EHR) | LASSO, Random Forest, XGBoost | Performance fluctuated over time due to data drift | Demographic info, lab results, diagnosis codes, medications | [59] |
Experimental Protocols and Methodologies
AI-Driven Analysis of Medical Imaging
Workflow Overview: The standard pipeline for developing AI-based imaging analysis tools involves data curation, model training, and rigorous validation [56] [59].
- Data Acquisition and Curation: Large, retrospective datasets of medical images (e.g., mammograms, colonoscopies, histopathology slides) are collected. Each image is de-identified and annotated by clinical experts to establish a gold-standard label (e.g., "cancerous," "benign," "neoplastic polyp"). The dataset is typically partitioned into training, validation, and test sets [56].
- Model Training and Architecture: Deep learning architectures, particularly Convolutional Neural Networks (CNNs), are the cornerstone of image-based AI. For cancer detection in 2D and 3D mammography, models like RetinaNet and ensembles of multiple CNNs have been successfully employed [56]. These models are trained to extract spatial hierarchies of features directly from the pixel data, learning to distinguish subtle patterns associated with malignancy.
- Performance Benchmarking: Model performance is quantified using standard metrics such as Sensitivity, Specificity, and the Area Under the Receiver Operating Characteristic Curve (AUC). Crucially, leading studies benchmark AI performance against human radiologists or pathologists in reader studies [56]. External validation on completely independent datasets from different hospitals or countries is considered the highest level of evidence to prove generalizability [56] [8].
- Analysis of "Missed" Cancers: To test the limits of AI systems, some experiments involve analyzing "pre-index" exams—images acquired 12-24 months before a cancer diagnosis that were originally deemed negative. AI models have demonstrated the ability to identify subtle signs of cancer in these prior exams, showing a potential for earlier detection than standard clinical practice [56].
AI Medical Imaging Analysis Workflow
AI-Driven Blood Biomarker Discovery and Integration
Workflow Overview: AI is revolutionizing biomarker discovery by finding complex, non-intuitive patterns in high-dimensional biological data that traditional statistical methods miss [57].
- Multi-Omic Data Integration: AI models, including deep learning and explainable AI (XAI) frameworks, are applied to vast and diverse datasets. These include genomics, transcriptomics, proteomics, and metabolomics derived from sources like tumor biopsies and liquid biopsies (e.g., blood tests) [57]. Platforms like PandaOmics use AI to analyze this multimodal omics data for biomarker and therapeutic target identification.
- Identifying Biomarker Signatures: Unlike hypothesis-driven traditional approaches, AI uses a data-driven approach to uncover novel biomarker signatures. It can integrate various 'omics' data to understand multi-omics biomarkers that provide a more comprehensive view of tumor biology [57]. For example, AI can analyze levels of circulating tumor DNA (ctDNA) to detect disease recurrence or treatment resistance before it becomes clinically apparent [57].
- Linking Biomarkers to Clinical Outcomes: The core task is to correlate the identified biomarker patterns with specific clinical outcomes, such as patient survival, response to therapy (predictive biomarkers), or disease aggressiveness (prognostic biomarkers). The Predictive Biomarker Modeling Framework (PBMF), which uses contrastive learning, is an advanced method for systematically extracting predictive biomarkers from rich clinical data [57].
- Validation and Explainability: Retrospective studies are used to validate the prognostic and predictive value of AI-discovered biomarkers [57]. Explainable AI (XAI) is critical here, as it helps clinicians understand the connection between specific biomarkers and patient outcomes, thereby building trust in the AI's recommendations [57] [60].
AI Biomarker Discovery Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
This section details key computational tools, frameworks, and data types essential for research in AI-based cancer risk prediction.
Table 3: Key Research Reagents and Computational Tools
| Tool/Reagent Name | Type | Primary Function in Research | Application Context |
|---|---|---|---|
| Convolutional Neural Networks (CNNs) | Deep Learning Architecture | Extracts spatial features from medical images for classification, detection, and segmentation. | Analyzing 2D/3D mammography, histopathology slides, and colonoscopy videos [56]. |
| Categorical Boosting (CatBoost) | Machine Learning Algorithm | Handles categorical data efficiently; high-performance gradient boosting for tabular data. | Predicting cancer risk from structured data combining lifestyle, genetic, and clinical factors [40]. |
| PandaOmics | AI-Driven Software Platform | Analyzes multimodal omics data to identify therapeutic targets and biomarkers. | Discovering novel biomarker signatures from integrated genomic, transcriptomic, and proteomic datasets [57]. |
| SHapley Additive exPlanations (SHAP) | Explainable AI (XAI) Framework | Interprets model predictions by quantifying the contribution of each input feature. | Providing clarity on which factors (e.g., genetic, lifestyle) most influenced a risk prediction [58]. |
| FUTURE-AI Guideline Framework | Governance & Validation Framework | Provides structured principles (Fairness, Robustness, etc.) for developing trustworthy AI. | Ensuring AI models are clinically deployable, ethical, and validated across diverse populations [60]. |
| Diagnostic Framework for Temporal Validation | Validation Methodology | Systematically vets ML models for future applicability and consistency over time. | Monitoring and addressing performance decay in predictive models due to clinical data drift [59]. |
Validation Across Diverse Populations: A Critical Imperative
The performance of any cancer risk prediction model is not universal. Validation across diverse populations is a fundamental challenge and a prerequisite for clinical translation [58] [8] [60].
- The Problem of Homogeneous Data: Many AI models are developed and validated on datasets from specific geographic or ethnic backgrounds (e.g., predominantly Caucasian populations), raising concerns about their accuracy and fairness when applied to other groups [58] [8]. Models trained on such data may fail to generalize, potentially exacerbating existing health disparities.
- Frameworks for Fairness and Robustness: The FUTURE-AI guidelines establish Fairness and Universality as core principles, stating that "AI tools should work equally well for everyone, no matter their age, gender, or background" and should be "adaptable to different healthcare systems and settings around the world" [60]. This necessitates the proactive inclusion of diverse demographic, genetic, and socioeconomic factors during model development and the use of independent, multi-center validation cohorts [56] [8].
- Addressing Temporal Data Drift: Real-world medical environments are dynamic. Changes in medical technology, treatments, and disease patterns can cause "data shift," degrading model performance over time [59]. Robust validation requires frameworks that assess model longevity and performance on prospective, time-stamped data, not just retrospective splits [59]. This ensures models remain relevant and accurate in evolving clinical settings.
The integration of AI-based imaging analysis and blood biomarker trends holds immense promise for creating a new generation of accurate, personalized cancer risk prediction models. As the comparative data shows, these tools can match or even surpass human expert performance in specific tasks like image-based cancer detection. However, their ultimate success and clinical utility are contingent upon rigorous validation that explicitly addresses two critical areas: performance across diverse populations and robustness to real-world data shifts. Future progress will depend on the widespread adoption of structured development guidelines, such as the FUTURE-AI principles, and a committed focus on generating prospective evidence from varied clinical settings to ensure these powerful technologies benefit all patient populations equitably.
Practical Approaches for Validating Models in Rare Cancers and Small Subgroups
Validating cancer risk prediction and diagnostic models for rare cancers and small patient subgroups presents unique methodological challenges that distinguish them from models for common cancers. Rare cancers, collectively defined as those with an incidence of fewer than 6 per 100,000 individuals, nonetheless account for approximately 22% of all cancer diagnoses and are characterized by significantly worse five-year survival rates (47% versus 65% for common cancers) [61]. This survival disparity is partially attributable to difficulties in achieving timely and accurate diagnosis, a challenge exacerbated by the scarcity of data that hinders the development and robust validation of predictive models [61] [7]. Conventional validation approaches, which often rely on large, single-dataset splits, are frequently inadequate for rare cancers due to insufficient sample sizes, leading to models that may fail to generalize across diverse clinical settings and populations. This guide synthesizes current methodologies and provides a structured framework for the rigorous validation of predictive models in these data-scarce environments, a critical endeavor for improving patient outcomes in rare oncology.
Comparative Analysis of Model Performance and Validation Strategies
The table below summarizes quantitative performance data and key validation approaches from recent studies focused on rare cancers or complex prediction tasks, illustrating the relationship between model architecture, data constraints, and validation rigor.
Table 1: Performance and Validation Strategies of Selected Oncology Models
| Model Name | Cancer Focus | Key Architecture/Technique | Performance (AUROC) | Primary Validation Method |
|---|---|---|---|---|
| RareNet [61] | Multiple Rare Cancers (e.g., Wilms tumor, CCSK) | Transfer Learning from CancerNet (VAE) | 0.96 (F1-score) | 10-fold cross-validation on 777 samples from TARGET database |
| Multi-cancer Risk Model [3] | 15 Cancer Types (General) | Multinomial Logistic Regression (with/without blood tests) | 0.876 (Men), 0.844 (Women) for any cancer | External validation on 2.64M (England) and 2.74M (Scotland, Wales, NI) patients |
| XGBoost for CGP [62] | Pan-cancer (Predicting genome-matched therapy) | eXtreme Gradient Boosting (XGBoost) | 0.819 (Overall) | Holdout test (80/20 split) on 60,655 patients from national database |
| Integrative Biomarker Model [63] | 5 Cancers (Lung, Esophageal, Liver, Gastric, Colorectal) | LASSO feature selection with multiple ML algorithms | 0.767 (5-year risk) | Prospective validation in 26,308 individuals from FuSion study |
Analysis of Comparative Data
The data reveals a clear trend: models tackling multiple common cancers achieve strong performance (AUROC >0.76) by leveraging enormous sample sizes, with the highest-performing models utilizing external validation across millions of patients [3] [63]. For rare cancers, where such datasets are nonexistent, the RareNet model demonstrates that advanced techniques like transfer learning can achieve high accuracy (~96% F1-score) even on a small dataset (n=777) [61]. Its reliance on cross-validation, rather than a single holdout set, provides a more robust estimate of performance in a low-data regime. Furthermore, the Japanese CGP study [62] highlights that complex prediction tasks (e.g., identifying genome-matched therapy) can be addressed with sophisticated machine learning models like XGBoost, but they still require large, centralized datasets (n=60,655) to succeed.
Foundational Principles for Rigorous Validation
The validation of models for small subgroups must adhere to a stringent set of principles to ensure clinical reliability and translational potential.
Demonstrated Generalizability: A model's performance must be evaluated on data that is entirely separate from its training data, ideally from different geographic regions or healthcare systems. The high-performing multinomial logistic regression model for cancer diagnosis was not just developed on 7.46 million patients but was externally validated on two separate cohorts totaling over 5.3 million patients from across the UK, proving its robustness across populations [3]. For rare cancers where external datasets are scarce, internal validation techniques like repeated k-fold cross-validation become paramount.
Mechanistic Interpretability: Understanding the biological rationale behind a model's predictions is critical for building clinical trust, especially when validating on small subgroups where overfitting is a risk. Employing Explainable AI (XAI) techniques, such as SHapley Additive exPlanations (SHAP), allows researchers to identify which features most strongly drive predictions. This approach was successfully used in a nationwide Japanese study to elucidate clinical features—such as cancer type, age, and presence of liver metastasis—that predict the identification of genome-matched therapies from Comprehensive Genomic Profiling (CGP) [62].
Data Relevance and Actionability: The data used for both training and validation must be clinically relevant and actionable. This means using data sources that reflect the intended clinical use case. For instance, the RareNet model utilized DNA methylation data, which provides distinct epigenetic signatures for different cancers and can be obtained from tumor biopsies [61]. Similarly, a dynamic breast cancer risk model was validated using prior mammogram images, a readily available data source in screening programs, ensuring the model's inputs are actionable in a real-world clinical context [48].
Experimental Protocols for Validation in Small Subgroups
Protocol: Transfer Learning for Rare Cancer Diagnosis
Transfer learning leverages knowledge from a model trained on a large, related task to improve performance on a data-scarce target task. The following workflow, based on the RareNet study [61], details the protocol for applying this technique to rare cancer diagnosis using DNA methylation data.
Diagram 1: Transfer Learning Workflow for Rare Cancers
Detailed Methodology:
- Step 1: Base Model Pre-training. Begin with a deep learning model pre-trained on a large, diverse dataset of common cancers. For example, CancerNet is a variational autoencoder (VAE) trained on DNA methylation data from 13,325 samples across 33 cancer types from The Cancer Genome Atlas (TCGA). The input features are 24,565 clusters of CpG (beta) values [61].
- Step 2: Model Adaptation. To adapt this model for rare cancers (e.g., Wilms Tumor, Clear Cell Sarcoma of the Kidney), remove the original classifier output layer (with 34 nodes for common cancers and normal) and replace it with a new, randomly initialized layer matching the number of rare cancer classes plus normal (e.g., 6 output nodes). Crucially, freeze the weights of the pre-trained encoder and decoder components. This preserves the general knowledge of cancer methylation patterns learned from the large dataset [61].
- Step 3: Classifier Training. Train only the new classifier head using the small rare cancer dataset (e.g., 777 samples from the TARGET database). This allows the model to learn to map the general, high-level features extracted by the frozen encoder to the specific rare cancer classes [61].
- Step 4: Robust Validation. Perform 10-fold cross-validation to evaluate model performance reliably. In each fold, 80% of the rare cancer data is used for training, 10% for validation (to adjust hyperparameters), and 10% for testing. The final performance metric is the average across all 10 test folds, providing a stable estimate of accuracy despite the limited data [61].
Protocol: Multi-Cohort External Validation
For models where some data is available, external validation across multiple, independent cohorts is the gold standard for assessing generalizability.
Diagram 2: Multi-Cohort External Validation
Detailed Methodology:
- Step 1: Model Derivation. Develop the initial prediction model using a large, representative dataset. The UK study developed two models (with and without blood tests) using multinomial logistic regression on a cohort of 7.46 million individuals from England, incorporating predictors like age, symptoms, medical history, and blood test results [3].
- Step 2: Independent Validation. Validate the finalized model on at least two completely separate, geographically distinct cohorts. The UK study used one validation cohort of 2.64 million patients from England and a second of 2.74 million patients from Scotland, Wales, and Northern Ireland, ensuring the model was tested against different population characteristics and healthcare practices [3].
- Step 3: Performance Assessment. Quantify model performance on the validation cohorts using discrimination, calibration, and clinical utility. Key metrics include:
- Discrimination: Report the c-statistic (Area Under the Receiver Operating Characteristic Curve, AUROC) for each cancer type and for any cancer overall. For example, the model with blood tests achieved a c-statistic of 0.876 for men and 0.844 for women for any cancer [3].
- Calibration: Compare predicted probabilities against observed outcomes to ensure the model is not systematically over- or under-estimating risk.
- Step 4: Subgroup Analysis. Actively evaluate and report model performance across key demographic and clinical subgroups, such as different age groups, racial and ethnic populations, and stages of cancer (early vs. late) [3] [48]. This is essential for identifying and addressing performance disparities in small subgroups within the larger population.
Table 2: Essential Resources for Model Development and Validation
| Resource Category | Specific Examples | Function in Validation |
|---|---|---|
| Data & Biobanks | TCGA, TARGET, C-CAT (Japan), CPRD (UK), QResearch | Provides large-scale, clinically annotated datasets for model training and external testing. |
| Machine Learning Frameworks | Scikit-learn, XGBoost, PyTorch, TensorFlow | Enables implementation of algorithms, from logistic regression to deep neural networks. |
| Explainable AI (XAI) Libraries | SHAP (SHapley Additive exPlanations) | Interprets complex model predictions, identifying driving features for validation [62]. |
| Biomarker Assays | DNA Methylation Profiling (e.g., WGBS), Blood Biomarkers (e.g., CEA, CA-125) | Provides actionable, molecular input data for model development and verification [61] [63]. |
| Validation Specimens | Patient-Derived Organoids (PDOs), Patient-Derived Xenografts (PDXs) | Offers clinically relevant pre-clinical models for initial experimental validation of predictions [64]. |
The validation of predictive models in rare cancers and small subgroups demands a deliberate and multifaceted approach that moves beyond conventional methodologies. As evidenced by the comparative data and protocols presented, success in this domain is achievable through the strategic application of techniques such as transfer learning to overcome data scarcity, rigorous multi-cohort external validation to prove generalizability, and the incorporation of explainable AI to build clinical trust and uncover biological insights. Adhering to the foundational principles of data actionability, expressive architecture, and fairness is paramount. By systematically implementing these advanced validation strategies, researchers and drug development professionals can accelerate the translation of robust, reliable models into clinical practice, ultimately helping to close the survival gap for patients with rare cancers.
Evidence-Based Model Assessment: Comparative Performance Across Populations and Settings
The validation of cancer risk prediction models across diverse populations represents a critical frontier in oncology research, bridging the gap between algorithmic innovation and clinical utility. While established statistical models have provided foundational frameworks for risk stratification, next-generation artificial intelligence (AI) approaches are demonstrating remarkable potential to enhance predictive accuracy and generalizability. This comparison guide objectively examines the performance characteristics, methodological approaches, and validation status of these competing paradigms within the specific context of cancer risk prediction, providing researchers and drug development professionals with evidence-based insights for model selection and translational application.
The evolution of cancer risk prediction has progressed from early statistical models incorporating limited clinical parameters to contemporary AI-driven architectures capable of processing complex multimodal data streams. This technological transition necessitates rigorous head-to-head performance evaluation across diverse patient demographics to ensure equitable application across global populations. The following analysis synthesizes current evidence regarding the comparative performance of established versus next-generation approaches, with particular emphasis on validation metrics including discrimination, calibration, and generalizability across racial and ethnic groups.
Performance Comparison: Quantitative Metrics
Discrimination Performance Across Cancer Types
Table 1: Model Discrimination Performance by Cancer Type and Methodology
| Cancer Type | Model Category | Specific Model/Approach | AUC (95% CI) | Study Population | Citation |
|---|---|---|---|---|---|
| Lung Cancer | AI Models (Imaging) | AI with LDCT | 0.85 (0.82-0.88) | Multiple populations | [65] |
| Lung Cancer | AI Models (Overall) | Various AI approaches | 0.82 (0.80-0.85) | Multiple populations | [65] |
| Lung Cancer | Traditional Models | Various regression approaches | 0.73 (0.72-0.74) | Multiple populations | [65] |
| Breast Cancer | AI (Dynamic MRS) | Prior + current mammograms | 0.78 (0.77-0.80) | 206,929 women (multi-ethnic) | [2] |
| Breast Cancer | AI (Static MRS) | Single mammogram | 0.67-0.72* | Multiple populations | [2] |
| Breast Cancer | Traditional (Clinical + AI) | Clinical factors + single mammogram | 0.63-0.67 | Kaiser Permanente population | [2] |
| Colorectal Cancer | Traditional (Trend-based) | ColonFlag (FBC trends) | 0.81 (0.77-0.85) | Multiple validations | [66] |
| Breast Cancer (Various) | Multiple Approaches | 107 developed models | 0.51-0.96 | Broad systematic review | [21] |
*Estimated from context describing performance improvement with prior mammograms
Performance Across Demographic Subgroups
Table 2: Next-Generation Model Performance Across Racial/Ethnic Subgroups
| Population Subgroup | Model Type | Cancer Type | AUC (95% CI) | Validation Cohort | Citation |
|---|---|---|---|---|---|
| East Asian Women | Dynamic MRS | Breast Cancer | 0.77 (0.75-0.79) | 34,266 women | [2] |
| Indigenous Women | Dynamic MRS | Breast Cancer | 0.77 (0.71-0.83) | 1,946 women | [2] |
| South Asian Women | Dynamic MRS | Breast Cancer | 0.75 (0.71-0.79) | 6,116 women | [2] |
| White Women | Dynamic MRS | Breast Cancer | 0.78 (0.77-0.80) | 66,742 women | [2] |
| Women ≤50 years | Dynamic MRS | Breast Cancer | 0.76 (0.74-0.78) | British Columbia cohort | [2] |
| Women >50 years | Dynamic MRS | Breast Cancer | 0.80 (0.78-0.82) | British Columbia cohort | [2] |
Methodological Approaches: Experimental Protocols
Established Statistical Models
Traditional cancer risk prediction models primarily employ regression-based methodologies that incorporate static risk factors at discrete timepoints. The foundational approach includes:
- Cox Proportional Hazards Models: Time-to-event analyses that incorporate fixed covariates with assumption of proportional hazards over time [7]
- Logistic Regression Models: Binary outcome prediction using combinations of demographic, clinical, and genetic factors [7] [21]
- Risk Score Algorithms: Points-based systems assigning weights to individual risk factors based on regression coefficients [7]
These established approaches typically incorporate limited longitudinal data and process risk factors as independent variables without capturing complex interactions or temporal patterns confined within normal ranges [66].
Next-Generation AI Approaches
Next-generation models leverage advanced computational architectures to process complex data patterns and temporal trends:
- Dynamic Risk Prediction: Incorporates longitudinal data (e.g., prior mammograms, serial blood tests) using statistical methodologies that link repeated measurements to outcomes through trajectory analysis [2] [66]
- Deep Learning Architectures: Neural network-based analysis of imaging data, capturing subtle parenchymal patterns not discernible through human visual assessment [2] [65]
- Ensemble Methods: Integration of multiple AI approaches (XGBoost, random forests) with traditional statistical models to enhance predictive performance [66] [65]
- Joint Modeling: Simultaneous modeling of longitudinal biomarker data and time-to-event outcomes, accounting for measurement error and correlation structures [66]
Figure 1: Methodological comparison of established versus next-generation modeling approaches and their validation pathways.
Validation Protocols for Diverse Populations
Robust validation methodologies are essential for establishing model generalizability:
- Internal Validation: Bootstrapping techniques (e.g., 5000 resamples) to estimate confidence intervals and correct for overoptimism [2]
- External Validation: Application to completely independent datasets from different geographic regions and healthcare systems [2] [21]
- Subgroup Performance Analysis: Stratified evaluation across racial, ethnic, and age subgroups to identify performance disparities [2]
- Calibration Assessment: Comparison of predicted versus observed event rates across risk deciles using observed/expected ratios [2] [21]
Research Reagent Solutions: Technical Toolkit
Table 3: Essential Research Materials and Analytical Tools for Cancer Risk Model Development
| Research Component | Function/Purpose | Example Specifications | Citation |
|---|---|---|---|
| Full-Field Digital Mammography | Image acquisition for breast cancer risk assessment | Hologic and General Electric machines (95% Hologic in BC program) | [2] |
| Longitudinal Blood Test Data | Trend analysis for cancer risk prediction | Full blood count, liver function tests, inflammatory markers | [66] |
| Population Cancer Registries | Outcome ascertainment and incidence rate calibration | British Columbia Cancer Registry, SEER program linkage | [2] |
| PROBAST Tool | Methodological quality assessment for prediction models | Standardized risk of bias evaluation across four domains | [66] [21] |
| Digital Biobanks | Multimodal data integration and model training | Linked screening images, clinical data, and tumor registry outcomes | [2] |
| High-Performance Computing | AI model training and validation | NVIDIA Blackwell architecture (25x throughput increase) | [67] |
Discussion and Research Implications
The comparative analysis reveals a consistent pattern of superior discrimination performance for next-generation AI approaches, particularly those incorporating longitudinal data and imaging information. The pooled AUC advantage of 0.09 for AI models versus traditional approaches in lung cancer prediction [65] and the significant improvement in 5-year risk prediction with dynamic mammogram analysis (AUC 0.78 vs 0.63-0.67 for traditional clinical+AI models) [2] demonstrate the tangible benefits of advanced methodologies.
Perhaps most notably, next-generation approaches show promising performance consistency across racial and ethnic subgroups, addressing a critical limitation of earlier models primarily developed and validated in Caucasian populations [2] [21]. The maintained AUC performance across East Asian (0.77), Indigenous (0.77), South Asian (0.75), and White (0.78) populations for the dynamic mammogram risk score suggests enhanced generalizability potential [2].
Limitations and Research Gaps
Despite promising results, significant challenges remain:
- Validation Deficits: Most models lack extensive external validation, with only 18 of 107 breast cancer models undergoing external validation [21]
- Calibration Reporting: Inadequate assessment and reporting of calibration metrics, with only 8 of 107 breast cancer studies reporting observed/expected ratios [21]
- Rare Cancers: Notable absence of predictive models for rare cancers (brain, mesothelioma, bone sarcoma) [7]
- Methodological Bias: High risk of bias in analysis domains for most studies, primarily due to incomplete handling of missing data and overfitting [66] [65]
Future Directions
Priority research initiatives should include:
- Prospective Validation Studies: Rigorous external validation of promising AI models across diverse healthcare settings [2] [65]
- Standardized Reporting: Adoption of TRIPOD guidelines for transparent reporting of prediction model studies [2]
- Integration of Multi-Omics Data: Incorporation of genomic, proteomic, and metabolomic biomarkers to enhance predictive accuracy [7]
- Dynamic Model Refinement: Continuous learning systems that incorporate newly acquired patient data for real-time risk updating [2] [66]
The transition from established statistical models to next-generation AI approaches represents a paradigm shift in cancer risk prediction, offering enhanced accuracy and potential for population-wide implementation. However, realizing this potential requires meticulous attention to validation methodologies, particularly across diverse demographic groups, to ensure equitable application of these advanced technologies in clinical and public health settings.
Breast cancer risk prediction models are critical tools for stratifying populations, guiding screening protocols, and enabling personalized preventive care. Models such as the Individualized Coherent Absolute Risk Estimation (iCARE), the Breast Cancer Risk Assessment Tool (BCRAT or Gail model), and the International Breast Cancer Intervention Study (IBIS or Tyrer-Cuzick) model are widely used in clinical and research settings. However, their development has primarily relied on data from populations of European ancestry, raising significant concerns about generalizability and performance across racially and ethnically diverse groups [68]. As global populations become increasingly heterogeneous, understanding the calibration, discrimination, and clinical utility of these models in non-White women is a scientific and public health imperative. This case study synthesizes current evidence on the comparative performance of iCARE, BCRAT, and IBIS models across different ethnicities, highlighting advances, persistent gaps, and methodological considerations for robust validation in diverse populations.
The iCARE, BCRAT, and IBIS models integrate different sets of risk factors and are built on varying statistical frameworks, leading to distinct strengths and limitations.
Table 1: Core Components of Major Breast Cancer Risk Prediction Models
| Model | Key Risk Factors Included | Genetic Components | Primary Development Population |
|---|---|---|---|
| iCARE | Classical risk factors (varies by version), mammographic density | Polygenic risk score (PRS) optional | Synthetic model from multiple data sources; flexible for calibration [9] |
| BCRAT (Gail) | Age, race/ethnicity, family history, biopsy history, reproductive factors | None | Primarily White women, with adaptations for Black women [29] |
| IBIS (Tyrer-Cuzick) | Extensive family history, hormonal/reproductive factors, BMI | BRCA1/2 pathogenic variants; optional PRS in later versions | Primarily non-Hispanic White women [69] |
The iCARE model represents a flexible approach that allows for the integration of relative risks from various sources (e.g., cohort consortia or literature) and calibration to specific population incidences and mortality rates [9]. The BCRAT model is a parsimonious tool that uses a relatively limited set of questionnaire-based risk factors and has been extensively validated, though often showing low to moderate discrimination [29]. The IBIS model incorporates a more comprehensive set of risk factors, including extensive family history to estimate the probability of carrying BRCA1/2 mutations, making it particularly suited for settings where hereditary cancer is a concern [69].
Comparative Model Performance Metrics
Quantitative Performance Across Ethnicities
External validation studies provide critical insights into how these models perform in real-world, diverse populations. Key metrics include calibration (the agreement between expected and observed number of cases, measured by E/O ratio) and discrimination (the ability to separate cases from non-cases, measured by the Area Under the Curve, AUC).
Table 2: Model Performance Metrics Across Racial and Ethnic Groups
| Population / Study | Model | Calibration (E/O ratio) | Discrimination (AUC) |
|---|---|---|---|
| Women <50 years (White, non-Hispanic) [9] | iCARE-Lit | 0.98 (95% CI: 0.87-1.11) | 65.4 (95% CI: 62.1-68.7) |
| BCRAT | 0.85 (95% CI: 0.75-0.95) | 64.0 (95% CI: 60.6-67.4) | |
| IBIS | 1.14 (95% CI: 1.01-1.29) | 64.6 (95% CI: 61.3-67.9) | |
| Women ≥50 years (White, non-Hispanic) [9] | iCARE-BPC3 | 1.00 (95% CI: 0.93-1.09) | Not specified |
| BCRAT | 0.90 (95% CI: 0.83-0.97) | Not specified | |
| IBIS | 1.06 (95% CI: 0.99-1.14) | Not specified | |
| Hispanic Women (WHI) [69] | IBIS | 0.75 (95% CI: 0.62-0.90)* | No significant difference by race/ethnicity |
| Multi-Ethnic Screening Cohorts (Black & White) [29] | BCRAT, BCSC, BRCAPRO, BRCAPRO+BCRAT | Comparable calibration overall (O/E ~1) | Comparable, moderate discrimination (AUCs similar across models); no significant difference between Black and White women |
*An E/O <1 indicates the model overestimated risk in this population.
The data reveal that model performance is highly dependent on the specific population and setting. For White, non-Hispanic women, the iCARE models demonstrated excellent calibration, while BCRAT tended to underestimate risk and IBIS to overestimate it in younger women [9]. A critical finding from the Women's Health Initiative was that the IBIS model was well-calibrated overall but significantly overestimated risk for Hispanic women (E/O=0.75), indicating a need for population-specific adjustments [69]. Encouragingly, one large study of screening cohorts found that several models, including BCRAT, showed comparable calibration and discrimination between Black and White women, suggesting potential robustness across these groups [29].
Impact of Integrating Polygenic Risk Scores and Mammographic Density
The integration of additional risk factors like polygenic risk scores (PRS) and mammographic density (MD) is a key strategy to improve model performance.
Figure 1: Workflow for Enhancing Risk Models with PRS and MD
Theoretical Improvements: A risk projection analysis using iCARE-BPC3 estimated that while classical risk factors alone could identify approximately 500,000 US White women at moderate-to-high risk (>3% 5-year risk), the addition of MD and a 313-variant PRS was projected to increase this number to approximately 3.5 million women [9]. This highlights the substantial potential of integrated models to refine risk stratification.
Validation in Black Women: The first externally validated PRS for women of African ancestry (AA-PRS) showed an AUC of 0.584. When this AA-PRS was combined with a risk factor-based model (the Black Women's Health Study model), the AUC increased to 0.623, a meaningful improvement toward personalized prevention for this population [70]. This combined model helps address a critical disparity in risk prediction tools.
Experimental Protocols for Model Validation
Core Methodological Framework
Robust validation of risk models requires a standardized approach to assess performance in independent cohorts. The following workflow outlines the key stages in this process.
Figure 2: Standard Workflow for Risk Model Validation
Cohort Definition: Studies typically involve assembling a cohort of asymptomatic women with no prior history of breast cancer who are eligible for screening (e.g., aged 40-84) [29]. Key exclusion criteria include a history of breast cancer, mastectomy, known BRCA1/2 mutations (for some models), and less than 5 years of follow-up data to ensure adequate outcome assessment [29].
Data Collection and Harmonization: Risk factor data (e.g., family history, reproductive history, BMI, biopsy history) are collected via questionnaires and/or electronic health records. Breast density is often obtained from radiology reports. Outcomes—incident invasive breast cancers—are typically ascertained via linkage with state or national cancer registries to ensure nearly complete case capture [29]. Methods for handling missing data (e.g., multiple imputation) and assumptions about unverified family history are clearly defined.
Statistical Analysis:
- Calibration is assessed by calculating the ratio of the total expected (E) to observed (O) number of breast cancer cases over a specific time horizon (e.g., 5-years). An E/O ratio of 1 indicates perfect calibration. This is often assessed within deciles of predicted risk and across demographic subgroups [9] [69].
- Discrimination is evaluated using the Area Under the receiver operating characteristic Curve (AUC), also known as the C-statistic. This metric quantifies the model's ability to distinguish between women who will and will not develop breast cancer [29] [70].
- Subgroup Analysis is crucial. Performance metrics are stratified by self-reported race and ethnicity to identify specific populations for which models may require recalibration or adjustment [29] [69].
Table 3: Key Resources for Risk Model Development and Validation
| Resource / Tool | Type | Function in Research |
|---|---|---|
| iCARE Software [9] | Statistical Tool / R Package | Flexible platform to build, validate, and compare absolute risk models using multiple data sources. |
| BayesMendel R Package [29] | Statistical Tool / R Package | Implements the BRCAPRO and BRCAPRO+BCRAT models for risk assessment incorporating family history. |
| BCRAT (BCRA) R Package [29] | Statistical Tool / R Package | Official software for calculating 5-year and lifetime breast cancer risk using the Gail model. |
| BCSC SAS Program [29] | Statistical Tool / SAS Code | Validated code for calculating 5-year breast cancer risk using the Breast Cancer Surveillance Consortium model. |
| CanRisk Tool [68] | Web Application | Implements the BOADICEA model for breast and ovarian cancer risk, updated for diverse ethnicities. |
| Polygenic Risk Scores (PRS) | Genetic Data | Scores derived from multiple SNPs (e.g., 313-SNP score) to capture common genetic susceptibility [9] [70]. |
| Biobanks & Cohort Studies | Data Resource | Large-scale studies (e.g., Women's Health Initiative, UK Biobank, Black Women's Health Study) provide data for model development and validation in diverse populations [69] [70] [68]. |
Discussion and Future Directions
Synthesis of Evidence and Remaining Challenges
The evidence compiled indicates that no single model consistently outperforms others across all ethnic groups. While tools like iCARE can be well-calibrated in White populations, and models like BCRAT show comparable performance between Black and White women in some settings, significant miscalibration has been observed, particularly for Hispanic women using the IBIS model [69]. This underscores that model performance is not transferable by default and must be rigorously validated in each target population.
A major challenge is that most models, including the core versions of BCRAT and IBIS, were developed primarily with data from White women [68]. This foundational bias can lead to inaccuracies in populations with different distributions of genetic variants, lifestyle risk factors, and baseline incidence rates. Furthermore, the addition of promising biomarkers like PRS has historically been limited by a lack of large-scale genome-wide association studies (GWAS) in diverse populations, though this is beginning to change with efforts like the development of an AA-PRS [70].
Pathways to Equitable Risk Prediction
Future progress hinges on several key strategies:
- Purposeful Development and Validation in Diverse Cohorts: Research must prioritize the inclusion of underrepresented racial and ethnic groups in both model development and validation studies. This requires leveraging diverse biobanks and consortium data [68].
- Model Adaptation and Updating: Existing models can be adapted by incorporating ethnicity-specific risk factor distributions, relative risks, and baseline cancer incidences, as demonstrated by the recent update of the BOADICEA model for the UK's ethnically diverse population [68].
- Transparent Reporting and Assessment: The PROBAST tool provides a framework for assessing the risk of bias in prediction model studies, which is critical for evaluating the quality of validation evidence [71].
- Accounting for Population Differences During Validation: Statistical methods that formally assess and adjust for differences between the development and validation populations are essential for a fair evaluation of a model's transportability and reproducibility [72].
In conclusion, while established models like iCARE, BCRAT, and IBIS provide a foundation for breast cancer risk assessment, their performance varies significantly across ethnicities. The pursuit of health equity in breast cancer prevention depends on the continued development, refinement, and transparent validation of risk prediction tools that perform reliably for all women.
The integration of artificial intelligence (AI) into clinical oncology offers unprecedented potential for improving cancer risk prediction, yet its real-world impact hinges on a critical factor: reliable performance across diverse patient populations and clinical settings. Many AI models demonstrate excellent performance in controlled development environments but suffer significant performance degradation when deployed in new hospitals or with different demographic groups. This challenge stems from data heterogeneity—variations in data sources, generating processes, and latent sub-populations—which, if unaddressed, can lead to unreliable decision-making, unfair outcomes, and poor generalization [73]. The field is now transitioning from model-centric approaches, which focus primarily on algorithmic innovation, to heterogeneity-aware machine learning that systematically integrates considerations of data diversity throughout the entire ML pipeline [73]. This comparative guide examines the current state of AI-enhanced cancer risk prediction models, objectively evaluating their validation performance across diverse clinical environments and providing researchers with methodologies to develop more robust, generalizable tools.
Comparative Performance of AI Models Across Populations
The predictive performance of clinical AI models is primarily assessed through discrimination and calibration. Discrimination, typically measured by the C-statistic or Area Under the Receiver Operating Characteristic Curve (AUC), quantifies a model's ability to distinguish between patients who develop cancer and those who do not [1] [44]. Calibration, evaluated using observed-to-expected (O/E) ratios and Hosmer-Lemeshow tests, measures how well predicted probabilities match observed outcomes across different risk levels [74] [44]. The table below summarizes key performance metrics and their interpretation:
Table 1: Key Metrics for Evaluating Cancer Risk Prediction Models
| Metric | Definition | Interpretation | Optimal Range |
|---|---|---|---|
| C-statistic/AUC | Ability to distinguish between cases and non-cases | Values >0.7 indicate acceptable discrimination; >0.8 indicate good discrimination [44] | 0.7-1.0 |
| O/E Ratio | Ratio of observed to expected events | Measures calibration; values closer to 1.0 indicate better calibration [74] [44] | 0.85-1.20 [74] |
| Hosmer-Lemeshow Test | Goodness-of-fit test for calibration | p-value >0.05 indicates adequate calibration [44] | >0.05 |
| Sensitivity | Proportion of true positives correctly identified | Higher values indicate better detection of actual cancer cases | Context-dependent |
| Specificity | Proportion of true negatives correctly identified | Higher values indicate better avoidance of false alarms | Context-dependent |
Cross-Population Performance of AI Models
Substantial evidence indicates that AI and machine learning models generally outperform traditional statistical approaches in cancer risk prediction, though their performance varies significantly across different populations. The following table synthesizes performance data from multiple validation studies:
Table 2: Comparative Performance of Cancer Risk Prediction Models Across Populations
| Cancer Type | Model | Population | Performance (C-statistic) | Notes |
|---|---|---|---|---|
| Breast Cancer | Machine Learning (pooled) | Multiple populations | 0.74 [74] | Integrated genetic & imaging data |
| Breast Cancer | Traditional Models (pooled) | Multiple populations | 0.67 [74] | Established models like Gail, Tyrer-Cuzick |
| Breast Cancer | Gail Model | Chinese cohorts | 0.543 [74] | Significant performance drop in non-Western populations |
| Lung Cancer | PLCOM2012 (External Validation) | Western populations | 0.748 (95% CI: 0.719-0.777) [44] | Outperformed other established models |
| Lung Cancer | Bach Model | Western populations | 0.710 (95% CI: 0.674-0.745) [44] | Developed from CARET trial |
| Lung Cancer | Spitz Model | Western populations | 0.698 (95% CI: 0.640-0.755) [44] | |
| Lung Cancer | TNSF-SQ Model | Taiwanese never-smoking females | Not quantified | Identified 27.03% as high-risk for LDCT screening [44] |
The performance advantage of ML models is particularly evident in breast cancer risk prediction, where they achieve a pooled C-statistic of 0.74 compared to 0.67 for traditional models [74]. This enhanced performance is most pronounced when models integrate multidimensional data sources, including genetic, clinical, and imaging data [74]. However, a critical finding across cancer types is that models developed primarily on Western populations frequently exhibit reduced predictive accuracy when applied to non-Western populations, as dramatically illustrated by the Gail model's performance drop to 0.543 in Chinese cohorts [74]. This underscores the critical importance of population-specific validation and model refinement.
Experimental Protocols for Robust Validation
Multicohort Training Methodology
Objective: To develop AI models with enhanced generalizability by training on combined datasets from multiple clinical cohorts, thereby diluting site-specific patterns while enhancing disease-specific signal detection [75].
Experimental Workflow:
Diagram 1: Multicohort training and validation workflow. VUMC: VU University Medical Center; ZMC: Zaans Medical Center; BIDMC: Beth Israel Deaconess Medical Center.
Procedure:
- Data Collection: Gather retrospective data from multiple clinical centers with varying geographical locations, patient demographics, and clinical protocols. In the referenced blood culture prediction study, data came from VU University Medical Center (VUMC) in the Netherlands, Zaans Medical Center (ZMC) in the Netherlands, and Beth Israel Deaconess Medical Center (BIDMC) in the United States [75].
- Model Training: Develop two types of models:
- External Validation: Evaluate all models on completely held-out cohorts not used in training (e.g., validate models trained on VUMC+ZMC on BIDMC data) [75].
- Performance Assessment: Compare AUC values and calibration plots between single-cohort and multi-cohort approaches using statistical methods like bootstrap resampling to estimate confidence intervals [75].
Key Findings: This methodology demonstrated that models trained on combined cohorts achieved significantly higher AUC scores (0.756) in external validation compared to traditional single-cohort approaches (AUC=0.739), with a difference of 0.017 (95% CI: 0.011 to 0.024) [75]. This approach specifically improves generalizability by diluting institution-specific patterns while enhancing detection of robust disease-specific predictors.
Comprehensive Validation Protocol
Objective: To establish a rigorous validation framework that assesses model performance, fairness, and stability across diverse demographic groups and clinical settings.
Experimental Workflow:
Diagram 2: Comprehensive model validation protocol
Procedure:
- Internal Validation: Assess model performance on development data using resampling methods:
- Internal-External Validation: When working with large, clustered datasets (e.g., multiple hospitals, geographic regions):
- External Validation: The gold standard for assessing generalizability:
- Comprehensive Performance Assessment:
- Discrimination: Calculate C-statistic/AUC with confidence intervals [1] [44].
- Calibration: Assess using O/E ratios, calibration plots, and Hosmer-Lemeshow tests [1] [74].
- Clinical Utility: Evaluate using decision curve analysis to estimate net benefit across different risk thresholds [1].
- Fairness Assessment: Stratify performance metrics across demographic subgroups (age, sex, ethnicity, socioeconomic status) to identify disparities [1].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful development and validation of generalizable AI models requires specific methodological approaches and resources. The following table details key components of the research toolkit for creating robust, clinically applicable prediction models:
Table 3: Essential Research Reagent Solutions for AI Model Validation
| Tool Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Data Resources | Multi-center consortium data, Publicly available datasets (e.g., MIMIC-IV-ED [75]), Clustered healthcare data | Provides heterogeneous training data essential for developing generalizable models | Ensure representativeness of target population; Address data sharing agreements and privacy concerns |
| Bias Assessment Tools | PROBAST (Prediction model Risk Of Bias Assessment Tool) [74] [44], Subgroup analysis frameworks | Critical appraisal of study quality and risk of bias; Identification of performance disparities across subgroups | Essential for systematic reviews of existing models; Should be applied during model development |
| Model Training Approaches | Multicohort training [75], Ensemble techniques (XGBoost, Random Forest) [58], Invariant learning methods [73] | Enhances generalizability by diluting site-specific patterns; Handles complex, non-linear relationships | Multicohort training significantly improves external performance [75]; Ensemble methods are most applied in cancer risk prediction [58] |
| Validation Methodologies | Internal-external cross-validation [1], Bootstrap resampling, Geographic external validation [44] | Assesses model stability and transportability; Provides realistic performance estimates in new settings | Particularly important when implementing models in diverse healthcare systems |
| Performance Metrics | C-statistic/AUC, O/E ratios, Calibration plots, Net benefit from decision curve analysis [1] | Comprehensive assessment of discrimination, calibration, and clinical utility | Calibration is as important as discrimination for clinical implementation |
| Implementation Frameworks | TRIPOD+AI reporting guideline [1], Post-deployment monitoring protocols [1] | Ensures transparent reporting and ongoing performance assessment after clinical implementation | Critical for maintaining model performance over time as data distributions shift |
The validation of AI-enhanced cancer risk prediction models across diverse clinical settings remains a formidable challenge, yet methodological advances are paving the way for more robust and equitable tools. The evidence consistently demonstrates that models trained on heterogeneous, multi-cohort data significantly outperform single-center models in external validation [75], and that comprehensive validation strategies encompassing internal, internal-external, and geographic external validation are essential for assessing true generalizability [1] [44]. The scientific toolkit for achieving trustworthy AI continues to evolve, with particular emphasis on fairness assessment, model stability checks, and post-deployment monitoring [1] [73].
For researchers and drug development professionals, the path forward requires steadfast commitment to heterogeneity-aware machine learning principles throughout the entire model development pipeline [73]. This includes proactive engagement with diverse data sources, rigorous fairness assessments across demographic subgroups, and transparent reporting following established guidelines. By adopting these approaches, the field can bridge the current gap between model development and clinical practice, ultimately realizing the promise of AI to deliver equitable, high-quality cancer care across all populations.
Cancer risk prediction models represent a transformative approach in oncology, enabling the identification of high-risk individuals who may benefit from targeted screening and preventive interventions. Unlike single-cancer models, multi-cancer risk stratification tools aim to assess susceptibility across multiple cancer types simultaneously, creating a more efficient framework for population health management. The development of these models has accelerated with advances in artificial intelligence (AI) and the availability of large-scale biomedical data, yet their clinical implementation requires rigorous validation across diverse populations [76]. This review systematically compares current multi-cancer risk prediction tools, focusing on their validation outcomes, methodological frameworks, and limitations, to inform researchers and drug development professionals about the state of this rapidly evolving field.
The validation of these models is particularly crucial as healthcare moves toward precision prevention. Current evidence suggests that risk-stratified screening approaches could significantly improve the efficiency of cancer detection programs by targeting resources toward those who stand to benefit most. However, the transition from development to clinical application requires careful assessment of model performance across different demographic groups and healthcare settings [77] [25].
Comparative Analysis of Multi-Cancer Risk Prediction Tools
Table 1: Performance Metrics of Validated Multi-Cancer Risk Prediction Models
| Model/Study | Cancer Types Covered | Key Predictors | Validation Cohort Size | Discrimination (AUC/HR) | Risk Stratification Power |
|---|---|---|---|---|---|
| FuSion Model [36] | Lung, esophageal, liver, gastric, colorectal (5CAs) | 4 biomarkers + age, sex, smoking | 26,308 external validation | 0.767 (95% CI: 0.723-0.814) | 15.19-fold increased risk in high vs. low-risk group |
| Pan-Cancer Risk Score (PCRS) [77] | 11 common cancers | BMI, smoking, family history, polygenic risk scores | 133,830 females, 115,207 males | HR: 1.39-1.43 per 1 SD | 4.6-fold risk difference between top and bottom deciles |
| Carcimun Test [78] | Multiple cancer types | Protein conformational changes | 172 participants | 95.4% accuracy, 90.6% sensitivity, 98.2% specificity | 5.0-fold higher extinction values in cancer patients |
| Young-Onset CRC RF Model [79] | Colorectal cancer (young-onset) | Clinical variables from EMR | 10,874 young individuals | 0.859 (internal), 0.888 (temporal validation) | High recall of 0.840-0.872 |
Table 2: Clinical Validation and Limitations of Multi-Cancer Risk Models
| Model/Study | Study Design | Clinical Validation | Key Strengths | Major Limitations |
|---|---|---|---|---|
| FuSion Model [36] | Population-based prospective | Independent validation cohort; clinical follow-up of 2,863 high-risk subjects | Integrated multi-scale data; real-world clinical utility | Limited to five cancer types; Chinese population only |
| Pan-Cancer Risk Score [77] | Prospective cohort (UK Biobank) | External validation in independent cohorts | Incorporates PRS and modifiable risk factors | Limited to White British ancestry; assumes fixed test performance |
| Carcimun Test [78] | Prospective single-blinded | Included inflammatory conditions as controls | Robust against inflammatory false positives; simple measurement technique | Small sample size; limited cancer types and stages |
| AI/ML Review [76] | Systematic assessment | Variable across studies | Handles complex, non-linear relationships | Lack of external validation in most models; limited diversity |
Methodological Approaches in Model Development and Validation
Biomarker-Based Integrative Models
The FuSion study exemplifies a comprehensive approach to multi-cancer risk model development, integrating diverse data types from a large prospective cohort. The methodology encompassed several sophisticated stages:
Study Population and Data Collection: The researchers recruited 42,666 participants from the Taizhou Longitudinal Study in China, with a discovery cohort (n=16,340) and an independent validation cohort (n=26,308). Participants aged 40-75 years provided epidemiological data through face-to-face interviews, physical examinations, and blood samples [36].
Variable Selection and Processing: The initial set of 80 medical indicators (54 blood-derived biomarkers and 26 epidemiological exposures) underwent rigorous preprocessing. Variables with >20% missing values were excluded, and highly correlated pairs (correlation coefficient >0.8) were reduced. K-nearest neighbors (KNN) imputation addressed remaining missing values in continuous variables, while outliers beyond the 0.1st and 99.9th percentiles were excluded. All biomarkers were standardized using Z-score transformation for model fitting [36].
Machine Learning and Feature Selection: Five supervised machine learning approaches were employed with a LASSO-based feature selection strategy to identify the most informative predictors. The final model incorporated just four key biomarkers alongside age, sex, and smoking intensity, demonstrating the value of parsimonious model design [36].
Outcome Assessment and Validation: Cancer outcomes were ascertained through ICD-10 codes from local registries, with diagnoses confirmed via pathology reports, imaging, or clinical evaluations. The model's performance was assessed through both internal validation and external validation in an independent cohort, with additional prospective clinical follow-up to verify cancer events [36].
Genetic and Epidemiological Integration Models
The Pan-Cancer Risk Score (PCRS) development utilized a different methodological approach, focusing on integrating genetic and conventional risk factors:
Study Population: The model was developed and validated using data from 133,830 female and 115,207 male participants of White British ancestry aged 40-73 from the UK Biobank, with 5,807 and 5,906 incident cancer cases, respectively [77].
Risk Factor Integration: Sex-specific Cox proportional hazards models were employed with the baseline hazard specified as a function of age. The model incorporated two major lifestyle exposures (smoking status and pack-years, BMI), family history of specific cancers, and polygenic risk scores for eleven cancer types [77].
Statistical Analysis: The PCRS was computed as a weighted sum of predictors from the multicancer Cox model. Performance was evaluated using standardized hazard ratios and time-dependent AUC metrics. The researchers used the Bayes theorem to project PPV and NPV for established MCED tests across different risk strata [77].
Protein-Based Detection Technology
The Carcimun test employs a distinctive technological approach based on protein conformational changes:
Analytical Principle: The test detects conformational changes in plasma proteins through optical extinction measurements at 340 nm. The underlying principle suggests that malignancies produce characteristic alterations in plasma protein structures that can be quantified through this method [78].
Experimental Protocol: Plasma samples are prepared by adding 70 µl of 0.9% NaCl solution to the reaction vessel, followed by 26 µl of blood plasma. After adding 40 µl of distilled water, the mixture is incubated at 37°C for 5 minutes. A blank measurement is recorded at 340 nm, followed by adding 80 µl of 0.4% acetic acid solution before the final absorbance measurement [78].
Blinded Analysis: All measurements were performed in a blinded manner, with personnel conducting the extinction value measurements unaware of the clinical or diagnostic status of the samples. A predetermined cut-off value of 120, established in prior research, was used to differentiate between healthy and cancer subjects [78].
Figure 1: Carcimun Test Experimental Workflow
Machine Learning Approaches for Specific Populations
For young-onset colorectal cancer (YOCRC), researchers developed a specialized risk stratification model using electronic medical records:
Data Source and Preprocessing: The study retrospectively extracted data from 10,874 young individuals (18-49 years) who underwent colonoscopy. After excluding features with >65% missing data, a combination of simple imputation and Random Forest algorithm addressed remaining missing values. Outliers were managed by winsorizing at the 1st and 99th percentiles [79].
Feature Selection and Model Development: The Boruta feature selection method was employed to identify key predictors, handling nonlinear relationships and interactions between features. Eight machine learning algorithms were trained, including Logistic Regression, Random Forest, and XGBoost, with random downsampling to address class imbalance [79].
Validation Framework: Models underwent both internal validation (50% data split) and temporal validation using data from a different year, demonstrating robustness across time periods. The Random Forest classifier emerged as the optimal approach with AUCs of 0.859 and 0.888 in internal and temporal validation, respectively [79].
Critical Assessment of Validation Outcomes
Discrimination and Calibration Performance
The evaluated models demonstrate varying levels of predictive performance across different validation settings:
The FuSion model achieved an AUROC of 0.767 for five-year risk prediction of five gastrointestinal cancers, with robust performance in both internal and external validation cohorts. The model demonstrated exceptional clinical utility in prospective follow-up, where high-risk individuals (17.19% of the cohort) accounted for 50.42% of incident cancer cases [36].
The PCRS approach showed strong risk stratification capabilities, with hazard ratios of 1.39 and 1.43 per standard deviation increase in risk score for females and males, respectively. The integration of polygenic risk scores provided significant improvement over models based solely on conventional risk factors, increasing the AUC from 0.55-0.57 to 0.60-0.62 [77].
The Carcimun test demonstrated exceptional discrimination in its validation cohort, with 90.6% sensitivity and 98.2% specificity. Importantly, it maintained this performance when including participants with inflammatory conditions, a notable challenge for many cancer detection tests [78].
Clinical Validation and Real-World Performance
Prospective clinical validation remains the gold standard for assessing model utility:
The FuSion study followed 2,863 high-risk subjects clinically, finding that 9.64% were newly diagnosed with cancer or precancerous lesions. Cancer detection in the high-risk group was 5.02 times higher than in the low-risk group and 1.74 times higher than in the intermediate-risk group [36].
For the PCRS model, researchers projected performance implications for existing MCED tests. They demonstrated that risk stratification significantly impacts positive predictive value; for example, 75-year-old females in the 90-95th PCRS percentile had a 2.6-fold increased 1-year risk compared to those in the 5-10th percentile, translating to a 22.1% PPV difference for the Galleri test [77].
Figure 2: Model Validation Framework and Key Metrics
Limitations and Barriers to Clinical Implementation
Methodological and Generalizability Concerns
Current multi-cancer risk stratification tools face several significant limitations that hinder broad clinical adoption:
Population Diversity Deficits: Most models have been developed in homogenous populations, raising concerns about generalizability. The FuSion model was developed exclusively in a Chinese population, while the PCRS utilized data from individuals of White British ancestry [36] [77]. Systematic reviews highlight this as a pervasive issue across cancer prediction models, with limited representation of diverse racial and ethnic groups [25] [8].
Validation Gaps: Despite promising performance in development cohorts, many models lack comprehensive external validation. A systematic review of breast cancer risk prediction models found that only 18 of 107 developed models reported external validation [8]. Similarly, AI-based approaches often suffer from insufficient validation, with many studies being underpowered or using too many variables, increasing noise [76].
Calibration Variability: The accuracy of absolute risk predictions varies substantially across models and populations. In breast cancer risk prediction, models like BCRAT have demonstrated underestimation of risk (E/O=0.85), while others like IBIS have shown overestimation (E/O=1.14) in external validation [9]. Proper calibration is essential for clinical decision-making but remains challenging to achieve consistently.
Technical and Implementation Challenges
Data Quality and Preprocessing: The performance of risk prediction models is highly dependent on data quality and preprocessing methods. As seen in the YOCRC model development, handling missing values, outliers, and imbalanced data requires sophisticated approaches that may not be standardized across institutions [79].
Interpretability and Transparency: Complex machine learning models, particularly deep learning approaches, often function as "black boxes" with limited interpretability. While explainable AI techniques like SHAP values are emerging, the field lacks standardized approaches for model interpretation that would facilitate clinical trust and adoption [76].
Integration with Existing Screening Paradigms: Most multi-cancer risk tools have not been adequately evaluated within established screening workflows. Their impact on patient outcomes, cost-effectiveness, and resource utilization remains uncertain, creating barriers to healthcare system adoption [77] [25].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagents and Methodological Components in Multi-Cancer Risk Prediction
| Category | Specific Components | Function/Application | Examples from Literature |
|---|---|---|---|
| Biomarker Panels | Blood-based biomarkers (ALB, ALP, ALT, AFP, CEA, CA-125) | Quantitative risk assessment; early detection signals | FuSion study incorporated 54 blood-derived biomarkers [36] |
| Genetic Risk Components | Polygenic risk scores (PRS); SNP arrays | Capture inherited susceptibility across multiple cancers | PCRS incorporated PRS for 11 cancer types [77] |
| Data Processing Tools | K-nearest neighbors (KNN) imputation; feature selection algorithms | Handle missing data; identify most predictive features | Boruta feature selection used in YOCRC model [79] |
| Machine Learning Algorithms | Random Forest; LASSO; XGBoost; Neural Networks | Model complex relationships; improve prediction accuracy | Multiple ML approaches compared in FuSion and YOCRC studies [36] [79] |
| Validation Frameworks | Internal/external validation; temporal validation; calibration metrics | Assess model performance and generalizability | FuSion used independent validation cohort; YOCRC used temporal validation [36] [79] |
Multi-cancer risk stratification tools represent a promising approach for enhancing cancer prevention and early detection. Current models demonstrate variable performance, with the most successful implementations integrating multiple data types—including epidemiological factors, blood-based biomarkers, and genetic information—and employing machine learning techniques to capture complex relationships. However, significant limitations persist, particularly regarding population diversity, external validation, and calibration consistency.
Future development should prioritize several key areas: (1) inclusion of diverse populations to ensure equitable application across racial, ethnic, and socioeconomic groups; (2) standardized validation frameworks incorporating external, temporal, and prospective clinical validation; (3) enhanced model interpretability through explainable AI techniques; and (4) systematic evaluation within existing healthcare workflows to demonstrate real-world utility and cost-effectiveness. As these tools evolve, they hold tremendous potential for transforming cancer screening from a one-size-fits-all approach to a precision prevention strategy that optimally allocates resources based on individualized risk assessment.
External validation is a critical step in the evaluation of clinical prediction models, assessing whether a model developed in one population performs reliably in new, independent datasets. For researchers and developers working with cancer risk prediction models, understanding the common pitfalls in external validation studies is essential for producing models that are generalizable and clinically useful. Recent systematic reviews highlight significant challenges in this process, from performance degradation to methodological oversights that can compromise the real-world applicability of otherwise promising models. This guide examines these pitfalls through the lens of recent evidence, providing a structured comparison to inform more robust validation practices.
Quantifying the Performance Degradation in External Validation
Systematic reviews consistently demonstrate that prediction models experience measurable performance degradation when validated externally compared to their internal validation performance. This decline reveals the true generalizability of a model and highlights the risk of overestimating performance when relying solely on internal validation.
Table 1: Performance Metrics in Internal vs. External Validation
| Model Category | Validation Type | Performance Metric | Median Performance | Notes |
|---|---|---|---|---|
| Sepsis Real-Time Prediction Models [80] | Internal Validation | AUROC (6-hr pre-onset) | 0.886 | Partial-window validation |
| External Validation | AUROC (6-hr pre-onset) | 0.860 | Partial-window validation | |
| Internal Validation | Utility Score | 0.381 | Full-window validation | |
| External Validation | Utility Score | -0.164 | Significant decline (p<0.001) | |
| Lung Cancer Risk Models [81] | External Validation | AUC (PLCOm2014+PRS) | 0.832 | General population |
| External Validation | AUC (Korean LC model) | 0.816 | Ever-smokers | |
| External Validation | AUC (TNSF-SQ model) | 0.714 | Non-smoking females | |
| Blood Test Trend Cancer Models [66] | External Validation | C-statistic (ColonFlag) | 0.81 (pooled) | Colorectal cancer risk |
The performance gap between internal and external validation can be substantial. For sepsis prediction models, the median Utility Score dropped dramatically from 0.381 in internal validation to -0.164 in external validation, indicating a significant increase in false positives and missed diagnoses when models were applied to new populations [80]. Similarly, the performance of lung cancer risk prediction models varied considerably across different populations, with area under curve (AUC) values ranging from 0.714 to 0.832 depending on the target population and model type [81].
Methodological Pitfalls in Validation Study Design
Single-Study External Validation Limitations
Single-study external validation, where a model is validated using data from only one external source, creates significant interpretation challenges. A demonstration using the Subarachnoid Hemorrhage International Trialists (SAHIT) repository revealed substantial performance variability across different validation cohorts [82].
Table 2: Performance Variability in Single-Study External Validations
| Performance Metric | Mean Performance (95% CI) | Performance Range | Between-Study Heterogeneity (I²) |
|---|---|---|---|
| C-statistic | 0.74 (0.70-0.78) | 0.52-0.84 | 92% |
| Calibration Intercept | -0.06 (-0.37-0.24) | -1.40-0.75 | 97% |
| Calibration Slope | 0.96 (0.78-1.13) | 0.53-1.31 | 90% |
This variability demonstrates that a model's performance in one validation study may not represent its true generalizability. The high between-study heterogeneity (I² > 90%) indicates that performance is highly dependent on the specific choice of validation data [82]. This pitfall is particularly relevant for cancer risk prediction models intended for diverse populations, as a single validation might provide an overly optimistic or pessimistic assessment of model utility.
Incomplete Validation Frameworks and Metrics
Many validation studies employ incomplete frameworks that limit understanding of real-world performance. In a systematic review of sepsis prediction models, only 54.9% of studies applied the recommended full-window validation with both model-level and outcome-level metrics [80]. Similar issues plague cancer prediction models, where calibration is frequently underassessed despite being crucial for clinical utility [66].
The reliance on a single performance metric, particularly the area under the receiver operating characteristic curve (AUROC), presents another significant pitfall. In sepsis prediction models, the correlation between AUROC and Utility Score was only 0.483, indicating that these metrics provide complementary information about model performance [80]. This discrepancy is critical because a high AUROC may mask important deficiencies in sensitivity or positive predictive value that would limit clinical usefulness.
Domain-Specific Challenges in Cancer Prediction
Limited Validation of AI-Based Pathology Models
In digital pathology-based artificial intelligence models for lung cancer diagnosis, external validation remains exceptionally limited. A systematic scoping review found that only approximately 10% of papers describing development and validation of these tools reported external validation [83]. Those that did often used restricted datasets and retrospective designs, with limited assessment of how these models would perform in real-world clinical settings with their inherent variability.
Inadequate Attention to Calibration
While discrimination (the ability to distinguish between cases and non-cases) is commonly reported, calibration (the agreement between predicted and observed risks) is frequently overlooked. In a review of cancer prediction models incorporating blood test trends, only one external validation study assessed model calibration despite its critical importance for clinical decision-making [66]. Poor calibration can lead to systematic overestimation or underestimation of risk, potentially resulting in inappropriate clinical decisions.
Experimental Protocols and Validation Methodologies
Leave-One-Cluster-Out Cross-Validation Protocol
To address the limitations of single-study external validation, the leave-one-cluster-out cross-validation protocol provides a more robust approach for assessing model generalizability [82].
Experimental Workflow:
- Data Preparation: Assemble multiple datasets from different sources (studies, geographical areas, time periods)
- Cluster Definition: Treat each data source as a separate cluster
- Iterative Validation: For each cluster:
- Use all other clusters for model development/training
- Validate the model on the held-out cluster
- Calculate performance metrics (discrimination and calibration)
- Performance Synthesis: Pool performance estimates using random-effects meta-analysis
- Heterogeneity Assessment: Quantify between-cluster variability using I² statistic
This methodology provides multiple external validation points, offering a more comprehensive assessment of model performance across different populations and settings.
Full-Window Versus Partial-Window Validation Framework
For real-time prediction models, the validation framework significantly impacts performance estimates [80].
Experimental Protocol:
- Full-Window Validation:
- Include all time windows until sepsis onset or patient discharge
- Better represents real-world clinical use with inherent class imbalance
- Calculates both model-level (AUROC) and outcome-level (Utility Score) metrics
- Partial-Window Validation:
- Include only a subset of pre-onset time windows
- Simplifies validation but risks overestimating performance
- Typically focuses only on model-level metrics
The full-window approach provides a more realistic assessment of clinical utility, particularly for models that will operate in continuous monitoring scenarios.
Visualization of External Validation Workflows
Diagram 1: External validation workflows showing critical assessment points where common pitfalls occur, leading to performance variability and incomplete generalizability assessment.
Table 3: Research Reagent Solutions for Prediction Model Validation
| Tool/Resource | Function | Application Notes |
|---|---|---|
| PROBAST [66] | Risk of bias assessment tool for prediction model studies | Critical for systematic evaluation of methodological quality |
| CHARMS Checklist [84] | Data extraction framework for systematic reviews of prediction models | Standardizes information collection across studies |
| Leave-One-Cluster-Out Cross-Validation [82] | Robust validation method for clustered data | Provides multiple external validation points; superior to single-study validation |
| Full-Window Validation Framework [80] | Comprehensive temporal validation approach for real-time prediction models | Assesses performance across all time windows rather than selected subsets |
| Random-Effects Meta-Analysis [82] | Statistical synthesis of performance across multiple validations | Quantifies between-study heterogeneity and provides pooled performance estimates |
| Calibration Assessment Tools [82] [84] | Evaluation of agreement between predicted and observed risks | Includes calibration plots, intercept, and slope; essential for clinical utility |
External validation remains a challenging but indispensable component of prediction model development, particularly for cancer risk stratification. The evidence from recent systematic reviews reveals consistent patterns of performance degradation when models are applied to new populations, highlighting the limitations of single-study validations and incomplete assessment frameworks. Successful implementation requires robust methodological approaches including multiple external validations, comprehensive performance metrics, and careful attention to calibration. By addressing these common pitfalls, researchers can develop more generalizable cancer risk prediction models that maintain their performance across diverse populations and clinical settings, ultimately supporting more effective early detection and prevention strategies.
Conclusion
The validation of cancer risk prediction models across diverse populations remains both a statistical challenge and an ethical imperative. Current evidence demonstrates that while next-generation models incorporating AI, prior mammograms, and polygenic risk scores show improved performance, their generalizability depends on rigorous external validation in representative populations. Successful models achieve consistent calibration and discrimination across racial, ethnic, and age subgroups—as evidenced by recent AI-based breast cancer models maintaining AUROCs of 0.75-0.80 across diverse groups. Future efforts must prioritize inclusive development cohorts, standardized validation protocols, and dynamic models that incorporate longitudinal data. For clinical implementation, researchers should focus on transparent reporting, independent prospective validation, and demonstrating utility in real-world screening and prevention decisions. Only through these collective efforts can we achieve the promise of equitable, precision cancer prevention for all populations.
References
- 1. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 2. Validation of a Dynamic Risk Prediction Model Incorporating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12144620/]
- 3. Development and external validation of prediction ... [https://www.nature.com/articles/s41467-025-57990-5]
- 4. Nationwide study on development and validation of a risk ... [https://www.nature.com/articles/s41598-024-75697-3]
- 5. Developing and Validating Risk Assessment Models of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6908945/]
- 6. Comparing the Performance of Machine Learning Models ... [https://www.jmir.org/2025/1/e76215]
- 7. Comparative Analysis of Predictive Models for Individual ... [https://www.mdpi.com/2673-7523/5/2/29]
- 8. A systematic review of prediction models for risk of breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560532/]
- 9. Comparative Validation of Breast Cancer Risk Prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7073933/]
- 10. Development and validation of a short screener to evaluate ... [https://www.sciencedirect.com/science/article/pii/S026156142500069X]
- 11. Addressing health disparities and equitable representation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12149224/]
- 12. A Review of Cancer Risk Prediction Models with Genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4179686/]
- 13. Assessing the performance of prediction models: a framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575184/]
- 14. Methodological guidance for the evaluation and updating of ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01801-8]
- 15. Calibration: the Achilles heel of predictive analytics [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1466-7]
- 16. Development and performance of female breast cancer incidence risk ... [https://pubmed.ncbi.nlm.nih.gov/40684451/]
- 17. Development and validation of a risk prediction model ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9768800/]
- 18. Development and external validation of prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12059126/]
- 19. : Practical Considerations in Developing and... Predicting Cancer Risk [https://link.springer.com/article/10.1007/s40471-015-0048-2]
- 20. Development and Validation of Cancer Risk Prediction ... [https://cdas.cancer.gov/approved-projects/5941/]
- 21. A systematic review of prediction for models of breast risk cancer [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14990-4]
- 22. Assessing Calibration of Prognostic Risk Scores - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3933449/]
- 23. Pitfalls in interpreting calibration in comparative ... [https://www.nature.com/articles/s41698-024-00785-6]
- 24. Performance of Breast Cancer Risk-Assessment Models in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7225681/]
- 25. Insights and limitations of endometrial cancer risk prediction ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-15200-x]
- 26. What is a ROC Curve and How to Interpret It [https://www.displayr.com/what-is-a-roc-curve-how-to-interpret-it/]
- 27. Drawing Guidelines for Receiver Operating Characteristic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7308134/]
- 28. Essentialism and Exclusion: Racism in Cancer Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8634398/]
- 29. Validation of Breast Cancer Risk Models by Race/Ethnicity, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8750569/]
- 30. Risk Prediction Model Versus United States Preventive ... [https://www.sciencedirect.com/science/article/pii/S1556086420306389]
- 31. Head-to-head comparisons of risk discrimination by ... [https://www.sciencedirect.com/science/article/pii/S2589537025000070]
- 32. Transparent reporting of a multivariable prediction model for ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-014-0241-z]
- 33. TRIPOD+AI statement: updated guidance for reporting ... [https://pubmed.ncbi.nlm.nih.gov/38626948/]
- 34. Colour Blindness & Colour Choices - CamBioc Teaching [https://cambiocteach.com/accessibility/colourchoice/]
- 35. Development and validation of an integrative 54 biomarker ... [https://pubmed.ncbi.nlm.nih.gov/40790537/]
- 36. Development and validation of an integrative 54 biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341305/]
- 37. Development and validation of a risk prediction model for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1607173/full]
- 38. Clinical validation of an integrated risk assessment test ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1556907/full]
- 39. Precision-Driven Biomarker Validation: A Biotech ... [https://www.criver.com/eureka/precision-driven-biomarker-validation-biotech-perspective-part-i]
- 40. Predicting cancer risk using machine learning on lifestyle ... [https://www.nature.com/articles/s41598-025-15656-8]
- 41. Insights and limitations of endometrial cancer risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628995/]
- 42. Risk prediction tools for cancer in primary care [https://www.nature.com/articles/bjc2015409]
- 43. Internal validation strategy for high dimensional prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451366/]
- 44. Predictive performance of risk prediction models for lung ... [https://www.nature.com/articles/s41598-024-83875-6]
- 45. Improving Lung Cancer Risk Prediction Using Machine ... [https://www.mdpi.com/2072-6694/17/10/1651]
- 46. Improving Colorectal Cancer Screening and Risk ... [https://pubmed.ncbi.nlm.nih.gov/41109668/]
- 47. Improving Colorectal Cancer Screening and Risk ... [https://www.sciencedirect.com/science/article/pii/S0002944025003803]
- 48. Validation of a Dynamic Risk Prediction Model ... [https://pubmed.ncbi.nlm.nih.gov/40478575/?utm_source=SimplePie&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1bAXfGTh08tVk-e1kpwuqxoVfiUn_5olMN9ewCML2bdAMGPEOD&fc=20220524054416&ff=20250606171536&v=2.18.0.post9+e462414]
- 49. Machine Learning Techniques Improving the Box–Cox ... [https://www.mdpi.com/2079-9292/14/16/3173]
- 50. Cancer Risk Prediction Paradigm Shift: Using Artificial Intelligence to Improve Performance and Health Equity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9552274/]
- 51. jmBIG: enhancing dynamic risk prediction and personalized ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02289-0]
- 52. Artificial intelligence methods applied to longitudinal data from ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02473-w]
- 53. Predicting short- to long-term breast cancer risk from ... [https://www.nature.com/articles/s41523-025-00831-x]
- 54. The LongiMam model for improved breast cancer risk ... [https://arxiv.org/html/2509.21383v1]
- 55. An Assessment of the Predictive Performance of Current ... [https://publichealth.jmir.org/2022/12/e35750/]
- 56. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 57. AI-driven biomarker discovery: enhancing precision in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906928/]
- 58. Artificial intelligence to predict cancer risk, are we there yet ... [https://www.sciencedirect.com/science/article/pii/S0959804925002217]
- 59. Diagnostic framework to validate clinical machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12219301/]
- 60. International Experts Establish FUTURE-AI Guidelines for ... [https://www.helmholtz-munich.de/en/iml/news-detail/international-experts-establish-future-ai-guidelines-for-trustworthy-healthcare-ai]
- 61. RareNet: a deep learning model for rare cancer diagnosis [https://www.nature.com/articles/s41598-025-08829-y]
- 62. A machine learning-based analysis of nationwide cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11629217/]
- 63. Development and validation of an integrative 54 biomarker ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00812-z]
- 64. The Hallmarks of Predictive Oncology - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11969157/]
- 65. Comparing Artificial Intelligence and Traditional ... [https://www.sciencedirect.com/science/article/pii/S1546144025001474]
- 66. Clinical Prediction Models Incorporating Blood Test Trend for ... [https://cancer.jmir.org/2025/1/e70275]
- 67. Comparing Top Generative AI Models in 2025 [https://browsewiz.com/blog/the-frontier-of-intelligence-comparing-top-generative-ai-models-in-2025]
- 68. Adapting the BOADICEA breast and ovarian cancer risk ... [https://www.nature.com/articles/s41416-025-03117-y]
- 69. Performance of the IBIS/Tyrer-Cuzick model of breast cancer ... [https://pubmed.ncbi.nlm.nih.gov/34228814/]
- 70. Addition of polygenic risk score to a risk calculator for ... [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-023-01748-8]
- 71. Breast Cancer Risk Assessment Tools for Stratifying ... [https://www.mdpi.com/2072-6694/15/4/1124]
- 72. Accommodating Population Differences in Risk Prediction ... [https://statistics.columbian.gwu.edu/accommodating-population-differences-risk-prediction-model-validation]
- 73. Data Heterogeneity Modeling for Trustworthy Machine ... [https://arxiv.org/html/2506.00969v1]
- 74. Development and performance of female breast cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278464/]
- 75. Embracing cohort heterogeneity in clinical machine ... [https://www.nature.com/articles/s41598-023-35557-y]
- 76. Artificial intelligence to predict cancer risk, are we there yet ... [https://www.sciencedirect.com/science/article/abs/pii/S0959804925002217]
- 77. Potential utility of risk stratification for multicancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10122653/]
- 78. Evaluation of an innovative multi-cancer early detection test [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1520869/full]
- 79. Development and validation of machine learning models ... [https://www.nature.com/articles/s41698-024-00719-2]
- 80. A methodological systematic review of validation and ... [https://www.nature.com/articles/s41746-025-01587-1]
- 81. A systematic review and meta-analysis of lung cancer risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12086449/]
- 82. Pitfalls of single-study external validation illustrated with a ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02280-9]
- 83. Systematic scoping review of external validation studies of AI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145442/]
- 84. a systematic literature review and external validation in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6580880/]