Flow Cytometry for Immunophenotyping Hematological Malignancies: From Standardized Protocols to Clinical Applications
This article provides a comprehensive resource for researchers, scientists, and drug development professionals on the application of flow cytometry in the immunophenotyping of hematological malignancies.
Flow Cytometry for Immunophenotyping Hematological Malignancies: From Standardized Protocols to Clinical Applications
Abstract
This article provides a comprehensive resource for researchers, scientists, and drug development professionals on the application of flow cytometry in the immunophenotyping of hematological malignancies. It covers the foundational principles and clinical utility of immunophenotyping for diagnosis, classification, and prognostic stratification. The content delves into standardized methodological protocols, including 8-color flow cytometry and stepwise gating strategies, before addressing common troubleshooting and optimization techniques to ensure high-quality data. Finally, it explores rigorous method validation protocols and comparative analyses essential for reproducible results in both research and clinical settings, synthesizing current standards and future directions in the field.
Principles and Clinical Impact of Immunophenotyping in Hematologic Cancers
The Critical Role of Immunophenotyping in Diagnosis and Classification of Leukemias and Lymphomas
Immunophenotyping by flow cytometry is a cornerstone technology in modern hematopathology, providing an essential tool for establishing diagnoses, prognostic classification, and evaluating treatment effectiveness in leukemias and lymphomas [1]. This powerful technique enables the simultaneous analysis of multiple physical and chemical characteristics of individual cells as they flow in a fluid stream through a laser beam [2]. The fundamental parameters measured include cell size (forward scatter), granularity (side scatter), and the expression of specific cell surface and intracellular markers through fluorescently labeled antibodies [3] [2]. The technology's capacity for high-speed, multiparametric analysis at the single-cell level makes it uniquely suited for identifying malignant populations within heterogeneous samples such as blood, bone marrow, and lymph node suspensions [1] [3].
The clinical utility of immunophenotyping stems from its ability to detect aberrant antigen expression patterns that distinguish malignant cells from their normal counterparts. This is particularly valuable in hematological malignancies, where tumor cells frequently display abnormal antigen expression profiles, including overexpression, loss, or asynchronous expression of lineage-associated markers [2]. The EuroFlow Consortium, formed in 2006, has significantly advanced the field through systematic development and standardization of flow cytometric immunophenotyping, addressing previous limitations in reproducibility across multicenter studies [1]. Their work has culminated in carefully validated 8-color antibody panels and standardized protocols that have improved diagnostic accuracy and consistency in the identification and classification of hematological malignancies [1].
Standardized Approaches for Immunophenotyping
Evolution of Standardization Frameworks
The need for standardized immunophenotyping protocols became increasingly evident as flow cytometry technology evolved from single-color analyses to complex multicolor panels. Early flow cytometric approaches suffered from significant inter-laboratory variability due to differences in antibody panels, instrument settings, and data analysis methods [1]. This limited reproducibility prompted the formation of collaborative working groups, most notably the EuroFlow Consortium, which established standardized procedures for instrument setup, sample preparation, antibody panel design, and data analysis [1] [2]. The development of these standardized protocols represented a paradigm shift in diagnostic flow cytometry, moving from laboratory-specific "home-brew" methods to harmonized approaches that facilitate comparable results across institutions [1].
The EuroFlow Consortium addressed several critical aspects of standardization, including the selection of optimal antibody clones and fluorochrome conjugates, standardization of instrument settings, and implementation of quality control measures [1]. This systematic approach ensured that the resulting data would be reproducible regardless of the testing location. The consortium's work highlighted that effective standardization requires careful attention to every step of the workflow, from sample collection and processing to final data interpretation [1] [4]. These efforts have been particularly important for multicenter clinical trials and studies where consistent data quality is essential for valid comparisons.
Disease-Specific Marker Panels
Standardized immunophenotyping panels have been developed for all major categories of leukemias and lymphomas, with marker selection guided by the World Health Organization (WHO) classification of haematolymphoid tumors and established diagnostic guidelines [2]. The table below summarizes key immunophenotypic markers used in the diagnosis and classification of major hematological malignancies:
Table 1: Essential Immunophenotypic Markers for Leukemia and Lymphoma Classification
| AML | B-Cell ALL | T-Cell ALL | CLL | CML | B-Cell Lymphoma | T-Cell Lymphoma |
|---|---|---|---|---|---|---|
| CD13 | CD10 | CD1a | CD5 | CD11b | CD19 | CD2 |
| CD14 | CD19 | CD2 | CD19 | CD13 | CD20 | CD3 |
| CD33 | CD20 | CD3 | CD20 | CD14 | CD22 | CD4 |
| CD34 | CD22 | CD5 | CD23 | CD33 | CD79a | CD5 |
| CD45 | CD34 | CD7 | CD38 | CD34 | CD5* | CD7 |
| CD64 | CD45 | CD45 | CD43 | CD45 | CD10 | CD8 |
| CD117 | TdT | TdT | CD79b | CD23* | CD30** | CD30** |
| HLA-DR | CD200 | FMC7 | BCL2 | |||
| MPO | Cyclin D1* |
Notes: * mantle cell lymphoma; * follicular lymphoma; * CLL/SLL; anaplastic large cell lymphoma; TdT: terminal deoxynucleotidyl transferase; MPO: myeloperoxidase [2].*
The strategic combination of markers in these panels allows for comprehensive immunophenotypic characterization of hematological malignancies. For example, in B-cell acute lymphoblastic leukemia (B-ALL), the combination of CD10, CD19, CD34, and TdT helps establish both lineage and maturation stage [2] [5]. Similarly, in acute myeloid leukemia (AML), markers such as CD13, CD33, CD117, and MPO identify myeloid lineage, while CD34 and HLA-DR provide information about immaturity [2]. The detection of light chain restriction (kappa or lambda) is fundamental for establishing B-cell clonality in mature B-cell neoplasms, while T-cell clonality can be assessed through evaluation of the T-cell receptor (TCR) Vβ repertoire or TRBC1 and TRBC2 expression [2].
Experimental Protocols for Comprehensive Immunophenotyping
Sample Preparation and Staining Protocols
Proper sample preparation is critical for reliable immunophenotyping results. The protocol begins with obtaining a single-cell suspension from the specimen, which may involve mechanical dissociation or enzymatic digestion for tissue samples [4]. Red blood cell lysis is typically performed using ammonium chloride-based lysing solutions, followed by washing steps to remove cellular debris [2]. Cell viability should exceed 95% to ensure accurate results, as dead cells can nonspecifically bind antibodies and produce misleading data [4]. For intracellular antigen detection, such as TdT or cyclin D1, cells must be fixed and permeabilized using appropriate reagents prior to antibody staining [5].
The staining protocol follows a systematic approach:
- Aliquot cells into test tubes (typically 1-2 × 10^6 cells per tube)
- Add fluorochrome-conjugated antibodies according to predetermined panel configurations
- Incubate for 15-20 minutes at room temperature in the dark
- Wash cells with phosphate-buffered saline (PBS) containing 1% bovine serum albumin (BSA)
- Fix cells with 1% paraformaldehyde if not analyzing immediately
- Acquire data on a flow cytometer within 24-48 hours [4]
For high-throughput applications, such as drug discovery screening, plate-based protocols using 96- or 384-well plates can be implemented with automated liquid handling systems [6]. These approaches significantly increase processing capacity while maintaining staining consistency across samples.
Instrument Setup and Data Acquisition
Standardized instrument configuration is essential for reproducible multicolor flow cytometry. The following protocol outlines key steps for proper instrument setup:
- Daily quality control: Run calibration beads to verify laser alignment, fluidics, and optical detection systems
- Voltage optimization: Adjust photomultiplier tube (PMT) voltages to ensure optimal signal detection while minimizing noise
- Compensation setup: Prepare single-color controls for each fluorochrome in the panel to calculate compensation matrices
- Threshold setting: Establish acquisition thresholds based on forward scatter (FSC) and/or a ubiquitous parameter to exclude debris and noise [4]
Data acquisition should be performed using standardized instrument settings across all samples within a study. For rare population analysis, such as minimal residual disease (MRD) detection, a minimum of 500,000 to 1,000,000 events should be acquired to ensure adequate statistical precision [4] [2]. The sample flow rate should be optimized based on the application—higher flow rates for immunophenotyping analysis and lower flow rates for DNA analysis or when evaluating complex samples with rare populations [3].
Table 2: Flow Cytometry Data Acquisition Parameters
| Parameter | Clinical Immunophenotyping | MRD Detection | DNA Analysis |
|---|---|---|---|
| Minimum Events | 50,000-100,000 | 500,000-1,000,000 | 20,000-50,000 |
| Flow Rate | High | Medium | Low |
| Core Size | Standard | Reduced | Standard |
| Laser Power | Optimized for brightness | Increased for sensitivity | Standard |
| Threshold | FSC and/or SSC | FSC and fluorescence | FSC and DNA dye |
Data Analysis and Interpretation
Data analysis represents a critical phase in the immunophenotyping workflow. The process typically involves sequential gating strategies to identify populations of interest:
- Doublet exclusion: Use FSC-height versus FSC-area to exclude cell aggregates
- Live cell selection: Include viability dye-negative populations
- Lineage identification: Use scatter properties and lineage markers to identify major cell populations
- Abnormal population detection: Identify aberrant immunophenotypes based on established diagnostic criteria [4]
The interpretation of immunophenotypic data requires comparison with normal patterns of antigen expression. Malignant populations typically demonstrate aberrancies such as antigen overexpression, underexpression, asynchronous expression, or lineage infidelity [2]. For example, in B-cell chronic lymphocytic leukemia (CLL), the co-expression of CD5 and CD19 with weak CD20 and surface immunoglobulin is characteristic, while mantle cell lymphoma typically shows brighter CD20 and co-expression of cyclin D1 [2]. The analysis of T-cell neoplasms focuses on aberrancies such as loss of pan-T-cell antigens (CD2, CD3, CD5, CD7), abnormal antigen density, or restricted Vβ repertoire [2].
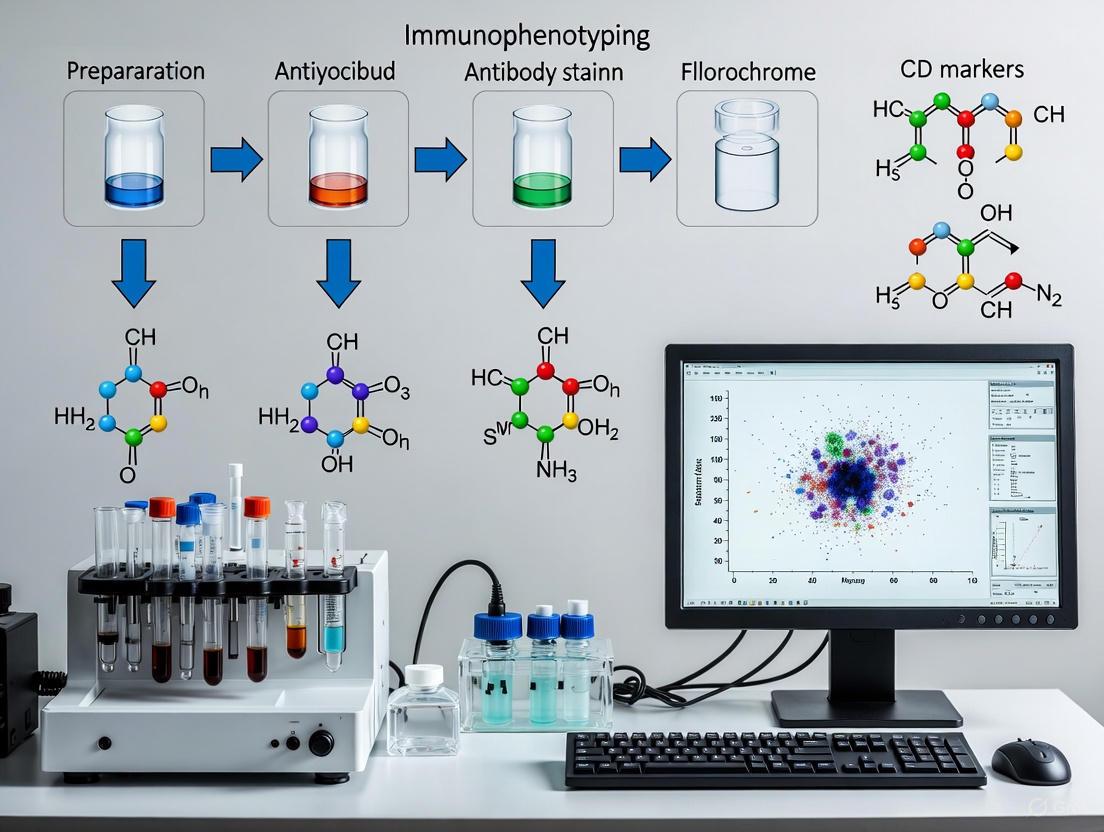
Figure 1: Immunophenotyping Workflow for Hematological Malignancies. This diagram illustrates the sequential steps from sample preparation to final diagnosis, highlighting key stages in the standardized immunophenotyping protocol.
Research Reagent Solutions for Immunophenotyping
Fluorochrome Selection and Panel Design
The selection of appropriate fluorochromes is a critical determinant of successful multicolor immunophenotyping panels. Several factors guide fluorochrome selection, including fluorescence profiles (excitation and emission spectra), relative brightness, fluorescence overlap (spillover), fluorochrome stability, and consistent conjugation to antibodies [7]. The EuroFlow Consortium has systematically evaluated fluorochrome characteristics to identify optimal combinations for multicolor panels [1] [7]. Their research has identified particularly favorable profiles for brilliant violet (BV)421 and BV510 in the violet laser and allophycocyanin (APC) hilite 7 (H7) or APC C750 in the red laser, based on higher fluorescence intensity and resolution with limited spillover into neighboring channels [7].
When designing multicolor panels, the following principles should be applied:
- Bright fluorochromes for low-abundance antigens: Pair bright fluorochromes (e.g., PE, APC) with markers expressed at low density
- Dim fluorochromes for highly expressed antigens: Use dimmer fluorochromes (e.g., FITC, PerCP) for brightly expressed markers
- Minimize spillover: Arrange fluorochromes to minimize spectral overlap between channels
- Validate combinations: Test proposed fluorochrome-antibody combinations to ensure optimal resolution [7]
The continued expansion of available fluorochromes has enabled increasingly complex panels, with modern configurations supporting simultaneous assessment of 20+ parameters [4]. This expanded capability has been particularly valuable for comprehensive immunophenotyping of heterogeneous samples and for detecting rare cell populations, such as minimal residual disease in leukemia patients [2].
Table 3: Essential Fluorochromes for Multicolor Immunophenotyping
| Fluorochrome | Excitation Laser | Emission Maximum | Relative Brightness | Recommended Application |
|---|---|---|---|---|
| FITC | 488 nm | 530 nm | Medium | Highly expressed antigens |
| PE | 488 nm | 576 nm | High | Low density antigens |
| PerCP | 488 nm | 680 nm | Low | Bright markers in complex panels |
| APC | 633/640 nm | 660 nm | High | Critical low-expression markers |
| BV421 | 405 nm | 421 nm | High | Violet laser applications |
| BV510 | 405 nm | 510 nm | Medium | Violet laser with minimal spillover |
| PE-Cy7 | 488 nm | 785 nm | Medium | Tandem fluorophore applications |
| APC-Cy7 | 633/640 nm | 785 nm | Medium | Red laser tandem applications |
Validated Antibody Panels and Controls
The use of validated antibody panels and appropriate controls is fundamental to reliable immunophenotyping. The EuroFlow Consortium has developed standardized 8-color antibody panels for the diagnosis and classification of hematological malignancies, accompanied by detailed standard operating procedures (SOPs) [1]. These panels consist of strategically combined screening tubes adapted to specific clinical questions, followed by multi-tube panels for comprehensive classification within disease categories [1].
Essential controls for immunophenotyping experiments include:
- Unstained controls: Cells processed without antibody staining to assess autofluorescence
- Fluorescence minus one (FMO) controls: Samples containing all antibodies except one to establish gating boundaries
- Isotype controls: Antibodies with irrelevant specificity to assess nonspecific binding
- Compensation controls: Single-stained samples for each fluorochrome to calculate spillover compensation
- Biological controls: Normal samples to establish reference expression patterns [4]
The implementation of standardized panels and controls has significantly improved the consistency and reproducibility of immunophenotyping across laboratories, facilitating more reliable diagnosis and classification of hematological malignancies [1] [2].
Clinical Applications in Leukemia and Lymphoma
Diagnostic and Classification Applications
Immunophenotyping plays an indispensable role in the diagnosis and classification of leukemias and lymphomas according to World Health Organization (WHO) criteria. In acute leukemias, flow cytometry rapidly distinguishes between acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL), with further subclassification into B-ALL and T-ALL [2] [5]. For B-ALL, immunophenotyping identifies differentiation stages (pro-B-ALL, common B-ALL, pre-B-ALL) and can trigger specific molecular testing based on phenotypic patterns [5]. Similarly, T-ALL can be subclassified into pro-T-ALL, pre-T-ALL, cortical T-ALL, and medullary T-ALL based on characteristic antigen expression profiles [5].
In mature lymphoid neoplasms, immunophenotyping provides critical information for diagnosis and classification. For B-cell lymphomas, the demonstration of light chain restriction (kappa or lambda) establishes clonality, while specific antigen patterns help distinguish between different entities such as CLL, mantle cell lymphoma, and follicular lymphoma [2]. T-cell clonality can be assessed through evaluation of the TCR Vβ repertoire or analysis of TRBC1 and TRBC2 expression, providing valuable evidence of malignancy in T-cell lymphoproliferative disorders [2].
Figure 2: Classification of Hematological Malignancies by Immunophenotyping. This diagram illustrates how immunophenotyping guides the classification of major hematological malignancies, with key discriminatory markers shown for each category.
Minimal Residual Disease (MRD) Detection
The detection of minimal residual disease has emerged as a critical application of immunophenotyping in the management of hematological malignancies. MRD refers to the small number of malignant cells that persist after treatment and are undetectable by conventional morphology [2]. Flow cytometric MRD detection relies on the identification of leukemia-associated immunophenotypes (LAIPs) that differ from normal hematopoietic cells [2]. The high sensitivity of modern flow cytometry (typically 0.01% or 10^-4) allows for early detection of residual disease, providing powerful prognostic information and guiding treatment decisions [2].
The EuroFlow Consortium has developed standardized approaches for MRD detection, including comprehensive antibody panels and data analysis protocols [1]. These standardized methods have improved the reproducibility of MRD assessment across institutions, facilitating its integration into clinical trial protocols and routine patient management [1] [2]. In B-ALL, for example, MRD monitoring by flow cytometry provides comparable prognostic information to molecular methods, with the advantage of rapid turnaround time and applicability to a broader range of patients [2] [5].
Emerging Applications in Targeted Therapy
Immunophenotyping is increasingly important in the era of targeted therapy for hematological malignancies. The technology provides a platform for assessing target expression on malignant cells, potentially identifying patients who may benefit from specific targeted agents [6] [5]. For example, the detection of CD20 expression in B-cell lymphomas identifies candidates for rituximab therapy, while CD38 expression in multiple myeloma may guide daratumumab treatment [2].
Emerging applications include "phospho-flow" analysis, which enables assessment of signaling pathway activation in malignant cells through detection of phosphorylated signaling proteins [5]. This approach could potentially monitor response to kinase inhibitors, such as in BCR-ABL-positive leukemias treated with tyrosine kinase inhibitors [5]. Additionally, flow cytometric assays have been developed for detection of fusion proteins, such as BCR-ABL, using immunobead technology [1] [5]. These assays provide rapid turnaround time and may be particularly valuable in settings where molecular diagnostics are not readily available [5].
Immunophenotyping by flow cytometry remains an indispensable tool in the diagnosis, classification, and monitoring of hematological malignancies. The standardization efforts led by groups such as the EuroFlow Consortium have significantly improved the reproducibility and reliability of flow cytometric analysis, addressing previous limitations in multicenter consistency [1] [2]. The development of validated multicolor antibody panels, standardized protocols, and sophisticated data analysis approaches has enhanced our ability to detect even minor abnormal populations, facilitating early diagnosis and sensitive MRD detection [1] [2].
The continuing evolution of flow cytometry technology, including the expansion of measurable parameters and improvements in fluorochrome chemistry, promises to further enhance the resolution and sensitivity of immunophenotyping [7]. These advancements, coupled with growing understanding of disease-specific immunophenotypic profiles, will continue to refine diagnostic accuracy and provide increasingly sophisticated insights into the biology of hematological malignancies. As targeted therapies continue to emerge, immunophenotyping will play an increasingly important role in patient selection and response assessment, solidifying its position as a critical technology in both clinical management and research of leukemias and lymphomas [6] [5].
Establishing Lineage and Maturation Stage of Pathologic Hematopoietic Cells
Flow cytometric immunophenotyping serves as a cornerstone in the diagnosis and classification of hematological malignancies, providing critical information for lineage assignment and maturational analysis of pathologic hematopoietic cells [8]. The fundamental principle underlying this application is that leukemic and lymphomatous cells often reflect the immunophenotypic characteristics of normal precursors blocked at specific differentiation stages, while also displaying aberrant phenotypic patterns that reflect underlying genetic abnormalities [9]. The complexity of multiparameter analysis techniques and the multitude of available monoclonal antibodies demand standardized protocols to achieve interlaboratory reproducibility, forming the basis for quality assurance in both clinical and research settings [8]. This protocol details comprehensive methodologies for establishing lineage and maturation stages of pathologic hematopoietic cells, with particular emphasis on discrimination between normal/reactive bone marrow and myelodysplastic syndromes, acute leukemias, and other hematological malignancies.
Theoretical Framework and Principles
Basis of Lineage Assignment and Maturation Analysis
Hematopoietic cells undergo precisely regulated differentiation processes characterized by sequential gain and loss of specific surface and intracellular antigens. Neoplastic cells derived from these precursors typically maintain immunophenotypic profiles reflective of their lineage commitment and maturation stage, albeit with frequent aberrancies [9]. Multiparametric flow cytometry allows the detection of these antigen expression patterns through simultaneous assessment of multiple parameters, enabling both lineage assignment and identification of pathologic features including aberrant antigen coexpression, maturation asynchrony, and antigen overexpression or underexpression [8] [10].
The consensus protocol established by the Working Group on Flow Cytometry and Image Analysis emphasizes that proper immunophenotyping requires careful selection of reagent panels based on the clinical question, appropriate assay procedures with rigorous quality control, and standardized data interpretation methods [8]. The identification of aberrant phenotypes is particularly crucial, as these patterns reflect genetic abnormalities present in pathologic cells and facilitate discrimination between normal regenerative and malignant processes [9].
Key Antigenic Patterns in Hematopoietic Differentiation
The normal maturation sequences of erythroid, granulocytic, monocytic, and lymphoid lineages are characterized by predictable antigen expression patterns. Deviation from these established patterns signifies potential malignancy. In myelodysplastic syndromes (MDS), for example, hematopoietic maturation abnormalities manifest as asynchronous antigen expression, particularly in CD16/CD13 and CD16/CD11b combinations during granulocytic differentiation [10]. Similarly, in B-cell development, the ordered progression of antigen expression provides a framework for identifying maturation blocks in B-lymphoblastic leukemia [9].
Table 1: Normal Sequence of Erythroid Antigen Expression During Maturation
| Maturation Stage | Early Progenitor | Intermediate Stage | Late Stage |
|---|---|---|---|
| Key Antigens | CD34, CD117 | CD36, Glycophorin A (dim) | Glycophorin A (bright), Band 3 |
| Additional Markers | HLA-DR | Kell glycoprotein, Rh gp | Lutheran gp, Duffy gp |
| Appearance Order | First | Second | Third |
The temporal order of erythroid-specific marker expression follows: Kell glycoprotein, Rh glycoprotein, Landsteiner Wiener (LW) glycoprotein, glycophorin A (GPA), Band 3, Lutheran (Lu) glycoprotein, and Duffy (Fy) glycoprotein [11]. The early appearance of Kell glycoprotein suggests its potential role in early hematopoiesis or cell lineage determination, making it a useful marker for diagnosing erythroleukemia [11].
Experimental Protocols
Sample Preparation and Staining
Materials and Reagents:
- EDTA-anticoagulated bone marrow samples (or peripheral blood)
- Monoclonal antibody combinations (see Table 2 for specific panels)
- Red blood cell lysis reagent (e.g., ammonium chloride solution)
- Phosphate-buffered saline (PBS) with protein stabilizer
- Fixation reagent (e.g., 1-4% paraformaldehyde)
- Permeabilization reagent (for intracellular antigens)
Procedure:
- Sample Collection: Collect 2-5 mL of bone marrow or 10 mL of peripheral blood in EDTA anticoagulant tubes. Process samples within 24 hours of collection, maintaining at room temperature.
Cell Suspension Preparation: Aliquot 2 × 10^6 cells in 100 μL per test tube. For intracellular staining, prepare additional aliquots for fixation and permeabilization.
Staining Protocol (Surface Antigens):
- Add predetermined concentrations of monoclonal antibody cocktails to each tube.
- Incubate for 15-20 minutes at room temperature in the dark.
- Lyse red blood cells using ammonium chloride-based lysing reagent for 10 minutes.
- Centrifuge at 500 × g for 5 minutes and decant supernatant.
- Wash cells with 2-3 mL of PBS/protein stabilizer.
- Repeat centrifugation and resuspend in 0.5 mL of PBS/protein stabilizer.
Staining Protocol (Intracellular/Nuclear Antigens):
- After surface staining, fix cells using commercial fixation reagent for 15 minutes.
- Permeabilize using permeabilization reagent for 10 minutes.
- Add antibodies against intracellular (e.g., CyMPO) or nuclear (e.g., TdT) antigens.
- Incubate for 30 minutes at room temperature in the dark.
- Wash cells with 2-3 mL of permeabilization buffer.
- Centrifuge and resuspend in 0.5 mL of PBS/protein stabilizer for acquisition.
Instrument Setup and Data Acquisition
Quality Control Measures:
- Perform daily instrument calibration using fluorescent beads
- Verify laser delays and photomultiplier tube (PMT) voltages
- Establish compensation settings using single-stained controls or beads
- Validate instrument performance using standardized control cells
Data Acquisition Parameters:
- Acquire a minimum of 30,000 events per tube for initial screening
- For rare population analysis (e.g., minimal residual disease), acquire ≥100,000 events
- For CD34+ progenitor analysis, specifically acquire ≥3 × 10^3 CD34+ cells through electronic gating [12]
- Use logarithmic amplification for fluorescence parameters
- Set appropriate threshold on forward scatter to exclude debris and platelets
Data Analysis and Interpretation
Gating Strategies for Hematopoietic Cells
The initial gating strategy should focus on identifying populations of interest while excluding artifacts and dead cells. The following hierarchical approach is recommended:
- Doublet Discrimination: Plot forward scatter height (FSC-H) versus forward scatter area (FSC-A) to exclude cell aggregates.
- Viability Gating: Exclude dead cells using viability dyes (e.g., propidium iodide) or light scatter properties.
- Blast Identification: Use CD45 versus side scatter (SSC) gating to identify blast populations (typically CD45dim/low and low SSC) [9].
- Progenitor Cell Analysis: For CD34+ hematopoietic progenitor cells (HPC), further subset based on CD45 expression and light scatter characteristics [12].
Diagram 1: Sequential gating strategy for hematopoietic cell analysis
Identification of Major CD34+ Hematopoietic Progenitor Subsets
Bone marrow CD34+ hematopoietic progenitor cells (HPC) constitute a heterogeneous population that can be subdivided into three major subsets based on light scatter characteristics and CD45 expression [12]:
- Immature CD34+ HPC: CD34hi/CD45int/HLA-DRhi/CyMPO-/nTdT-/CD117hi with intermediate light scatter.
- CD34+ B-cell Precursors (BCP): CD34int/CD45int/dim/HLA-DRhi/CyMPO-/nTdTint/CD117- with lower forward and side scatter.
- CD34+ Neutrophil Precursors: CD34hi/CD45int/dim/HLA-DRhi/CyMPOint/hi/nTdT-/CD117hi with highest forward and side scatter.
Additional lineage-committed CD34+ precursors can be identified at smaller percentages:
- Plasmacytoid DC precursors: CD34+/CD123int/hi/HLA-DRhi
- Monocytic precursors: CD34+/HLA-DRhi/CD64hi/CD45hi/CD117-
- Basophil precursors: CD34+/CD123int/hi/HLA-DR-/+
- Mast cell precursors: CD34+/CD117hi/HLA-DR-/int
- Erythroid precursors: CD34+/CD36+/CD64-/CD45lo
Recognition of Aberrant Immunophenotypes
Malignant hematopoietic cells frequently display immunophenotypic aberrancies that facilitate their discrimination from normal counterparts. These include:
- Asynchronous Antigen Expression: Coexpression of typically early and late differentiation antigens
- Antigen Overexpression/Underexpression: Abnormal fluorescence intensity compared to normal cells
- Lineage Infidelity: Expression of antigens typically restricted to other lineages
- Abnormally Homogeneous Antigen Expression: Loss of normal heterogeneity in maturing populations
In MDS, common abnormalities include increased CD34+ cells, aberrant CD117 and CD13 expression, decreased CyMPO, CD64 and CD65 on CD34+ immature and neutrophil precursors, and altered patterns of CD16/CD13 and CD16/CD11b expression during granulocytic maturation [10] [12]. A scoring system based on the number and severity of phenotypic abnormalities efficiently discriminates between normal/reactive and MDS CD34+ HPC [12].
Table 2: Flow Cytometric Scoring System for MDS Diagnosis
| Parameter | Normal (0 points) | Moderately Abnormal (1 point) | Markedly Abnormal (2 points) |
|---|---|---|---|
| CD34+ HPC Percentage | <0.05% | 0.05-0.10% | >0.10% |
| Myeloblast Phenotype | No aberrancies | 1-2 aberrancies | ≥3 aberrancies |
| Maturing Myeloid Cells | Normal maturation pattern | Mildly abnormal patterns | Severely abnormal/blocked maturation |
| Lymphoid Precursors | Normal B-cell precursors | Reduced B-cell precursors | Absent B-cell precursors |
| Erythroid Precursors | Normal antigen expression | Mild antigen asynchrony | Severe antigen deficiency |
Application in Specific Hematologic Malignancies
Myelodysplastic Syndromes (MDS)
Flow cytometry provides critical diagnostic information in MDS, particularly when morphology is equivocal and cytogenetics is normal [10]. Key applications include:
- Detection of Myeloblast Abnormalities: Identification of aberrant phenotypes on CD34+ cells including overexpression of CD117, CD13, and CD33, decreased CD45, CD38, and HLA-DR, and aberrant expression of CD4, CD7, CD11b, and CD56 [12].
- Analysis of Maturing Compartments: Recognition of dysgranulopoiesis through abnormal CD16/CD13 and CD16/CD11b patterns, altered CD64 and CD65 expression on monocytes, and aberrant erythroid antigen expression [10].
- Progenitor Distribution Analysis: Documentation of expansion of erythroid- and neutrophil-lineage CD34+ cells in low-grade MDS at the expense of CD34+ plasmacytoid dendritic cell and B-cell precursors, while high-grade MDS shows expansion of immature CD34+ precursors [12].
The percentage of MDS patients displaying two or more phenotypic abnormalities ranges from 62-78%, with disease progression associated with increasing numbers of aberrancies [10].
Acute Leukemias
In acute leukemias, flow cytometry is essential for lineage assignment, subclassification, and detection of minimal residual disease (MRD). The EuroFlow consortium has developed standardized 8-color antibody panels for comprehensive immunophenotypic analysis [13]. Key principles include:
- Lineage Assignment: Use of combination markers to establish lymphoid (CD19, CD22, cyCD79a, CD3, cyCD3, CD2, CD7) versus myeloid (MPO, CD13, CD33, CD65, CD117, CD64, CD14, CD41, CD61, Glycophorin A) lineage [9].
- Maturation Stage Determination: Identification of stages of maturation arrest within B- (pro-B, common-B, pre-B) and T-lymphoid (pro-T, pre-T, cortical-T, medullary-T) lineages.
- Aberrant Phenotype Detection: Recognition of leukemia-associated immunophenotypes (LAIPs) including asynchronous antigen expression, antigen overexpression/underexpression, and lineage infidelity [9].
For MRD detection, flow cytometry offers sensitivity of 0.01% (1 leukemic cell in 10,000 normal cells), requiring acquisition of approximately 1,000,000 events to achieve this sensitivity level [13].
Research Reagent Solutions
Table 3: Essential Monoclonal Antibody Panels for Hematopoietic Cell Characterization
| Target Cell Population | Essential Antibody Specificities | Clinical/Research Utility |
|---|---|---|
| Myeloid Progenitors | CD34, CD45, CD117, CD13, CD33, HLA-DR, CD38, CD90, CD123 | Stem cell enumeration, AML characterization |
| Granulocytic Maturation | CD16, CD11b, CD13, CD15, CD65, CD10, CD64 | MDS diagnosis, maturation studies |
| Monocytic Lineage | CD14, CD64, CD36, CD163, CD4, CD11c, HLA-DR | CMML diagnosis, monocyte subset analysis |
| Erythroid Maturation | CD36, CD71, CD235a (Glycophorin A), CD105, CD49d | Erythroleukemia, MDS with erythroid dysplasia |
| B-cell Maturation | CD19, CD10, CD20, CD34, CD45, TdT, CD22, CD79a, IgM | B-ALL classification, B-cell maturation blocks |
| T-cell Maturation | CD3, CD5, CD7, CD1a, CD4, CD8, CD34, TdT, CD45 | T-ALL classification, T-cell maturation analysis |
Troubleshooting and Quality Assurance
Common Technical Issues and Solutions
- High Background Fluorescence: Ensure proper antibody titration; verify Fc receptor blocking when needed; check for cellular autofluorescence.
- Poor Population Resolution: Verify instrument calibration; check compensation matrices; confirm antibody cocktail compatibility.
- Low Cell Recovery: Optimize washing steps; avoid excessive centrifugation; verify cell concentration before staining.
- Inconsistent Results Between Experiments: Standardize sample processing time; use consistent antibody lots; implement daily quality control.
Data Interpretation Pitfalls
- Overlapping Populations: Use additional discriminating markers; employ multidimensional analysis techniques.
- Non-Specific Binding: Include appropriate isotype controls; use Fc receptor blocking.
- Antigenic Modulation: Minimize time between staining and analysis; standardize staining protocols.
- Maturation Continuums: Establish reference ranges for normal maturation patterns; use quantitative fluorescence analysis.
Advanced Applications and Future Directions
The field of flow cytometric immunophenotyping continues to evolve with technological advancements. Emerging applications include:
- High-Parameter Flow Cytometry: Simultaneous assessment of 20-30 parameters using spectral flow cytometry or mass cytometry (CyTOF).
- Automated Analysis Algorithms: Implementation of cluster analysis, principal component analysis, and other bioinformatic approaches to identify complex immunophenotypic patterns [14].
- Functional Assessment: Integration of phospho-specific antibodies to evaluate signaling pathway activation in conjunction with immunophenotyping.
- Rare Event Detection: Enhanced sensitivity for minimal residual disease detection through increased event acquisition and improved gating strategies.
The consistent application of standardized protocols, comprehensive antibody panels, and rigorous quality control measures will ensure that flow cytometric immunophenotyping remains an indispensable tool for establishing lineage and maturation stage of pathologic hematopoietic cells in both research and clinical settings.
Prognostic Stratification and Detection of Minimal Residual Disease (MRD)
Minimal Residual Disease (MRD) refers to the small number of cancer cells that persist in patients after treatment, at levels below the detection capability of conventional microscopy. In hematological malignancies, the presence of MRD is a powerful independent prognostic factor, strongly associated with higher relapse risk and shorter survival [15] [16]. The clinical utility of immunophenotyping for diagnosing, classifying, and prognostically stratifying hematological malignancies is well-established [17] [18]. Flow cytometric immunophenotyping represents one of the most relevant clinical applications in this field, enabling specific identification of neoplastic cells and their accurate enumeration and phenotypic characterization [17]. With the development of novel therapeutic agents that induce deeper responses, the need for highly sensitive MRD assessment techniques has become paramount for risk stratification and treatment guidance [19] [20]. This document outlines standardized protocols and application notes for MRD detection within the broader context of flow cytometry for immunophenotyping hematological malignancies research.
MRD Detection Methods: Technical Comparison
The evolution of MRD detection technologies has significantly improved sensitivity and applicability, enabling researchers and clinicians to assess treatment response with unprecedented depth. The primary methods currently employed include multiparametric flow cytometry (MFC), next-generation flow cytometry (NGF), and next-generation sequencing (NGS). Each technique offers distinct advantages and limitations, which are summarized in the table below.
Table 1: Comparison of Major MRD Detection Technologies
| Method | Sensitivity | Applicability | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Multiparametric Flow Cytometry (MFC) | 10-4 to 10-5 [21] | High (>90% for AML; >95% for MM) [15] [21] | Fast turnaround (<6 hours); broad availability; assesses cellular heterogeneity [15] [21] | Requires fresh sample; limited standardization; operator-dependent [15] [22] |
| Next-Generation Flow (NGF) | 10-5 to 10-6 [19] [21] | Very High (>95%) [21] | High sensitivity and standardization (e.g., EuroFlow); high reproducibility [21] [22] | Sample processing requires protocol adaptation to acquire millions of cells [21] |
| Next-Generation Sequencing (NGS) | 10-5 to 10-6 [19] [23] | Lower than MFC (requires baseline sample) [16] | Ultra-sensitive; tracks clonal evolution; provides molecular fingerprint [23] [16] | High cost; complex bioinformatics; longer turnaround time [23] |
The choice of method depends on the clinical or research question, required sensitivity, available infrastructure, and the specific hematologic malignancy. In multiple myeloma, for instance, both NGF and NGS show a strong correlation in MRD level assessment (r=0.9722), and sustained MRD negativity detected by either method is a significant predictor of superior progression-free survival (PFS) [19] [20]. In Acute Lymphoblastic Leukemia (ALL), NGS has demonstrated superior sensitivity in identifying MRD-positive cases compared to MFC, and its results correlate strongly with clinical outcomes [23].
Prognostic Value of MRD Status
MRD status has emerged as a critical biomarker for prognostic stratification across various hematological malignancies. Achieving MRD negativity is consistently associated with significantly improved clinical outcomes, transcending traditional risk stratifications.
Table 2: Prognostic Impact of MRD Status in Hematologic Malignancies
| Malignancy | MRD Negativity Definition | Prognostic Impact | Key Supporting Evidence |
|---|---|---|---|
| Multiple Myeloma (MM) | <1 clonal plasma cell per 105 nucleated cells [16] | Superior PFS and OS; overcomes high-risk genetics [19] [16] | 3-year PFS: 100% (sustained MRD-) vs 67.6% (non-sustained) by NGF [19] |
| Acute Myeloid Leukemia (AML) | <1 aberrant blast per 103–104 cells (0.01–0.1%) [15] | Higher relapse risk; shorter survival [15] | MRD+ associated with reduced OS (HR: 5.153; p < 0.0001) [15] |
| Acute Lymphoblastic Leukemia (ALL) | <1 leukemic cell per 104–106 cells [23] | Superior Event-Free Survival (EFS) and OS [23] | NGS-based MRD stratification highly predictive of relapse post-transplant/CAR-T [23] |
The timing and persistence of MRD negativity are also crucial. In multiple myeloma, sustained MRD negativity, defined as two consecutive negative assessments at least 6 months apart, is associated with exceptionally favorable outcomes, including 100% 3-year PFS in one study [19]. This suggests that sustained MRD negativity may be a more robust endpoint than a single time point assessment.
Detailed Experimental Protocols
EuroFlow Next-Generation Flow (NGF) for Multiple Myeloma MRD
The EuroFlow NGF protocol is a standardized, high-sensitivity method for MRD detection in multiple myeloma, achieving sensitivities of up to 10-6 [19] [21].
Key Research Reagent Solutions:
- Bone Marrow Aspirate: Collected in EDTA or heparin; EDTA samples should be processed within 24 hours at room temperature [21].
- Backbone Antibody Panel: Fluorochrome-conjugated antibodies against CD45, CD38, CD138, CD19, CD56, CD27, CD81, and CD117, plus cytoplasmic kappa and lambda light chains [21].
- Viability Stain: LIVE/DEAD Fixable Aqua Dead Cell Stain Kit to exclude non-viable cells [21].
- Lysing Solution: For erythrocyte lysis.
Procedure: Bulk-Lysis Staining Method [21]
- Sample Preparation: Obtain a first-pull bone marrow aspirate to minimize peripheral blood contamination.
- Cell Counting: Determine total nucleated cell count. The protocol is designed to process a sufficient volume of bone marrow to acquire millions of events.
- Bulk Lysis: Lyse a calculated volume of bone marrow sample upfront to remove red blood cells.
- Antibody Staining: Resuspend the cell pellet and stain with the pre-mixed 8-color or 10-color antibody panel. Incubate in the dark for 20 minutes.
- Secondary Lysis: Lyse the sample a second time to remove any residual erythrocytes.
- Data Acquisition: Acquire data on a flow cytometer capable of high-speed multiparametric analysis. Current consensus guidelines require a minimum of 2 million and recommend 5 million events per tube to achieve a sensitivity of 10-5 [21].
- Data Analysis: The gating strategy involves:
- Identification of viable, single-cell events.
- Selection of CD38++CD138+ plasma cells.
- Discrimination between normal (polytypic) and aberrant (monotypic) plasma cells based on the expression of CD19, CD56, CD27, CD81, CD45, and cytoplasmic light chains.
The entire workflow for the EuroFlow NGF protocol is visualized below.
Multiparametric Flow Cytometry for AML MRD
This protocol details a validated 10-color flow cytometry assay for MRD detection in Acute Myeloid Leukemia (AML), based on consensus recommendations [15].
Key Research Reagent Solutions:
- Bone Marrow Specimen: Collected in EDTA, ACD, or heparin.
- AML MRD Antibody Panel: A 3-tube, 10-color panel incorporating a robust 5-marker backbone (CD34, CD117, CD13, CD45, HLA-DR) and additional lineage differentiation markers.
- Lysing Solution.
Procedure [15]
- Sample Processing: Use a lyse-wash-stain procedure. Start with a target cell count of 20 million cells, adding 2 million cells per tube for staining.
- Antibody Staining: Stain cells in three separate tubes with the pre-defined antibody combinations.
- Data Acquisition: Acquire data on a high-performance flow cytometer (e.g., BD FACSLyric). Target event collection is 1.2 million events per tube, aiming for a total of 3 million analyzed events to achieve a lower limit of quantification of 0.01% [15].
- Data Analysis: Use a combination of "Leukemia-Associated Immunophenotype" (LAIP) and "Difference from Normal" (DfN) approaches to identify aberrant myeloid blasts. The analysis must carefully distinguish these from regenerating normal hematopoietic precursors.
Integrated MRD Assessment Strategy
A modern MRD assessment strategy often involves integrating multiple technologies to overcome the limitations of any single method. For intramedullary disease, the combination of NGF and NGS provides highly sensitive and complementary data, with NGF offering a broad phenotypic profile and NGS enabling clonal tracking [19] [16]. For a comprehensive assessment, intramedullary MRD testing should be complemented with extramedullary imaging techniques such as FDG-PET/CT or whole-body diffusion-weighted MRI to detect residual disease in bones or other organs not sampled by bone marrow aspiration [16]. The logic for an integrated MRD assessment strategy in a clinical trial or research setting is outlined below.
The standardization and implementation of high-sensitivity MRD detection methods, particularly advanced flow cytometry protocols like EuroFlow NGF, have fundamentally transformed the prognostic stratification of hematological malignancies. The strong, independent prognostic power of MRD status underscores its potential as a surrogate endpoint in clinical trials and a guide for treatment personalization. Future efforts must focus on the global harmonization of technical protocols, data interpretation, and reporting to ensure reproducibility and comparability across laboratories [17] [22]. Furthermore, research into the biological characteristics of MRD cells and their interplay with the immune microenvironment will be crucial for developing novel therapies aimed at eradicating residual disease and achieving cures.
Identifying Phenotypic Aberrations Linked to Specific Genetic Abnormalities
Flow cytometric immunophenotyping has become the preferred method for the lineage assignment and maturational analysis of malignant cells in acute leukemias and lymphomas [8]. The complexity of multiparameter analysis techniques and the multitude of available monoclonal antibodies demand a standardization of protocols for the use of flow cytometry in clinical laboratories to achieve interlaboratory reproducibility [8]. Multi-parameter flow cytometry has increased our ability to screen large numbers of cellular events, and aids in diagnosis, prognostic stratification and identification of potential therapeutic targets for hematologic neoplasms [24]. Beyond its diagnostic utility, identifying correlations between immunophenotype and genetic abnormalities can reveal possible immunophenotypic patterns that may serve as surrogate markers predicting specific genetic abnormalities [24]. This application note provides detailed methodologies for detecting these critical phenotypic-genotypic relationships in hematological malignancies.
Key Phenotypic-Genetic Correlations in Hematologic Malignancies
Multiple Myeloma (MM) Phenotypic-Genetic Associations
Research has demonstrated significant correlations between aberrant antigen expression patterns and cytogenetic abnormalities in multiple myeloma. Distinction between clonal neoplastic plasma cells (PCs) and non-neoplastic PCs is determined by the differential expression pattern of a constellation of markers, including CD138, CD38, CD45, CD56 and CD117 along with cytoplasmic/surface light chains, instead of a single marker [24].
Table 1: Correlation Between Antigen Expression and Genetic Abnormalities in Multiple Myeloma
| Antigen | Genetic Association | Biological/Clinical Correlation |
|---|---|---|
| CD56 (NCAM) | Hyperdiploidy [24] | Higher expression associated with hyperdiploidy [24] |
| FGFR3 translocation [24] | Higher expression noted in association with FGFR3 [24] | |
| c-MAF translocation [24] | Lacked NCAM mRNA expression [24] | |
| CD117 (Kit) | Hyperdiploidy [24] | Higher expression associated with hyperdiploidy [24] |
| FGFR3 translocation [24] | Lower Kit expression noted [24] | |
| c-MAF translocation [24] | High Kit expression observed [24] | |
| CD52 | c-MAF and FGFR3 subgroups [24] | High CD52 mRNA expression was associated with c-MAF and FGFR3 subgroups [24] |
| CKS1B amplification [24] | Positive correlation with CD52 expression (p=0.02) [24] | |
| CD20 | t(11;14) translocation [24] | Established association between CD20, CCND1 and t(11;14) translocation [24] |
| CKS1B amplification [24] | Negative correlation with CD20 expression (p=0.0108) [24] |
These phenotypic differences in multiple myeloma are associated with distinct genetic subgroups, which potentially has important diagnostic and prognostic value [24]. The association between CD20 and t(11;14) is particularly well-established, while other correlations provide new insights into disease biology.
Acute Myeloid Leukemia (AML) Immunophenotypic Patterns
Acute myeloid leukemias with recurrent genetic abnormalities demonstrate distinctive immunophenotypic profiles that can guide diagnostic testing. Database-guided analysis approaches have been developed to rapidly identify these patterns and direct appropriate genetic testing.
Table 2: AML with Recurrent Genetic Abnormalities - Database Analysis Performance
| AML Genetic Subtype | Cases in Database | Sensitivity (%) | Negative Predictive Value (%) |
|---|---|---|---|
| t(8;21) | 8 [25] | 92 [25] | 98.5 [25] |
| t(15;17) | 19 [25] | 92 [25] | 98.5 [25] |
| inv(16)/t(16;16) | 12 [25] | 92 [25] | 98.5 [25] |
| MLL-r (KMT2A) | 11 [25] | 92 [25] | 98.5 [25] |
This Compass database-guided analysis method excluded AML associated with t(8;21), t(15;17), inv(16), and KMT2A translocation with 92% sensitivity and a 98.5% negative predictive value in a prospective validation study of 125 suspected AML patients [25]. Such approaches allow for rapid orientation of genetic and molecular biology testing to achieve a rapid, accurate diagnosis [25].
Myelodysplastic Syndromes (MDS) and CMML Aberrations
In myelodysplastic syndromes, a simplified flow cytometry approach has identified major phenotypic abnormalities with clinical significance. Using a basic percentage-based analysis method, researchers found that 90% of MDS patients had at least one phenotypic abnormality when compared to normal bone marrow samples [26].
The three main phenotypic abnormalities in MDS are:
CD56 expression on monocytes was specifically associated with chronic myelomonocytic leukemia (CMML), providing a simple diagnostic tool for this disease entity [26]. This association was statistically significant both in bone marrow (p=0.03) and blood circulating monocytes (p=0.01 against normal subjects and patients with monocytosis) [26].
Experimental Protocols
Multiparametric Flow Cytometry for Plasma Cell Neoplasms
Sample Preparation and Antibody Panel
- Sample Requirements: Bone marrow specimens are collected in appropriate anticoagulants (heparin or EDTA). A minimum of 167 specimens provides statistical power for correlative studies [24].
- Antibody Panel Design: The five-color panel should include:
- Primary gating markers: CD38, CD45, CD138
- Aberrancy markers: CD56, CD117, CD19, CD20, CD52
- Clonality assessment: Kappa/Lambda light chains
- Staining Protocol:
- Aliquot 100μL of bone marrow suspension into tubes
- Add predetermined optimal concentrations of antibodies
- Incubate for 15-20 minutes in the dark at room temperature
- Lyse red blood cells using ammonium chloride solution
- Wash twice with phosphate-buffered saline
- Resuspend in 0.5mL of PBS for acquisition
Instrument Setup and Data Acquisition
- Flow Cytometer: Utilize a calibrated five-color flow cytometer (e.g., FC500, Beckman Coulter) [24]
- Quality Control: Perform daily calibration using standardized beads
- Acquisition Parameters: Collect a minimum of 100,000 events per tube, with particular attention to the plasma cell gate identified by CD38 bright and CD138 expression
- Gating Strategy:
- Initial gate on viable cells using forward and side scatter
- Sequential gating on CD38 bright/CD138+ plasma cells
- Confirm CD45 expression patterns
- Analyze aberrant marker expression on identified plasma cell population
Database-Guided Analysis for AML
Reference Database Construction
- Case Selection: Collect well-classified AML cases according to WHO recommendations:
- t(8;21) AML (n=8)
- t(15;17) AML (n=19)
- inv(16)/t(16;16) AML (n=12)
- MLL-rearranged AML (n=11)
- Normal myeloid-committed hematopoietic precursors (n=20) [25]
- Data Processing: Export fcs files and build Compass databases using specialized software (e.g., Infinicyt 2.0)
- Population Definition: Normal my-HPCs should include:
- Neutrophil lineage: CD45+low/int CD117+ CD34+/- HLA-DR+int CD13+ CD14- IREM2- CD33+ CD36-
- Monocyte lineage: CD45+low/int CD117+ CD34+/- HLA-DR+hi CD64+ CD14- CD300e[IREM-2]- CD13+ CD33+
- Erythroid lineage: CD45-/+low CD117+ CD34+/- HLA-DR+low/int CD36+ CD105+ CD33- CD35+low [25]
Prospective Case Analysis
- Sample Testing: Process new AML cases through standardized antibody panels (e.g., EuroFlow AML/MDS panel)
- Database Comparison: Compare blast events from new cases against reference databases using balanced APS plots
- Similarity Scoring: Score similarity based on the position of the median from the new case relative to the 1 and 2 standard deviation curves for defined AML groups
- Genetic Testing Guidance: Use immunophenotypic patterns to prioritize specific genetic tests:
- t(8;21) pattern: RUNX1-RUNX1T1 FISH
- APL-like pattern: PML-RARA FISH
- inv(16) pattern: CBFB-MYH11 FISH
Simplified MDS Phenotypic Analysis
Basic Percentage-Based Protocol
- Panel Design: Five-color combination: CD36FITC-CD117PE-CD45ECD-CD34Cy5-CD56Cy7 [26]
- Gating Strategy:
- Identify granulocytes using CD45 and side scatter
- Gate monocytes based on CD45 and forward scatter characteristics
- Set thresholds for abnormal expression based on normal controls
- Abnormality Criteria:
- CD36 on granulocytes: >10% positive cells in bone marrow
- CD117 on granulocytes: >10% positive cells in bone marrow
- CD56 on monocytes: >20% positive cells in bone marrow [26]
- Interpretation: Consider a case positive for MDS-associated phenotype if at least one abnormality is present (90% sensitivity) [26]
Data Analysis and Interpretation
Flow Cytometry Data Analysis Fundamentals
Flow cytometry data is typically represented using graphical representations such as histograms, scatter plots, and density plots to visualize multiple parameters and facilitate the identification of different cell populations [27].
- Histograms: Display a single parameter, with the x-axis showing signal intensity and the y-axis representing the number of events. Best used when most cells express a marker of interest and the staining is bright [28].
- Dot Plots/Scatter Plots: Present multiparameter data, where each event is mapped onto the graph based on expression of specific parameters. Essential for identifying population subsets and aberrant co-expression patterns [28].
- Gating Strategies: Use quadrant, rectangular, elliptical, and polygon gates to quantify populations. For percentage calculations, remember that gates represent subsets of your total population, and drilling down requires back-calculation to determine total population percentages [27].
Database-Guided Analysis Workflow
The Compass database-guided analysis represents an advanced approach for identifying phenotypic aberrations linked to genetic abnormalities:
Quality Assurance and Standardization
- Control Samples: Include normal bone marrow controls with normal blood counts to establish baseline expression percentages [26]
- Instrument Calibration: Perform daily quality control using standardized beads to ensure consistent performance [22]
- Standardized Protocols: Adopt consensus protocols for reagent panels, sample preparation, and data analysis to achieve interlaboratory reproducibility [8]
- Validation: Correlate flow cytometric findings with genetic results (FISH, molecular studies) to validate immunophenotypic-genetic correlations
Research Reagent Solutions
Table 3: Essential Research Reagents for Phenotypic-Genetic Correlation Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Lineage Assignment Antibodies | CD38, CD45, CD138 [24] | Primary gating and identification of cell populations of interest |
| Aberrancy Marker Antibodies | CD56, CD117, CD19, CD20, CD52 [24] | Detection of immunophenotypic abnormalities associated with genetic subtypes |
| Clonality Assessment Reagents | Kappa/Lambda light chains [24] | Determination of clonality in B-cell and plasma cell neoplasms |
| Viability/Vital Dyes | Propidium iodide, 7-AAD | Exclusion of dead cells from analysis to improve data quality |
| Standardized Antibody Panels | EuroFlow AML/MDS panel [25] | Consistent multiparameter analysis across laboratories and studies |
| Data Analysis Software | Infinicyt Compass, CXP software [25] [24] | Database-guided analysis and objective pattern recognition |
Applications in Drug Development and Clinical Research
The identification of phenotypic aberrations linked to specific genetic abnormalities has significant implications for drug development and clinical research:
- Therapeutic Target Identification: Aberrant antigens or cytogenetic abnormalities hold potential for being targeted in therapy tailored to the individual patient [24]. For example, CD52 expression patterns in specific genetic subgroups may inform anti-CD52 therapy applications.
- Clinical Trial Stratification: Immunophenotypic patterns can serve as inclusion criteria or stratification factors in clinical trials, particularly for targeted therapies.
- Minimal Residual Disease Monitoring: Database-guided different-from-normal (DfN) analysis provides a nonsubjective method for MRD assessment, potentially detecting residual disease below morphological assessment thresholds [25].
- Treatment Response Assessment: Serial immunophenotypic analysis can track clonal evolution and emergence of new aberrant populations during treatment, providing insights into resistance mechanisms.
The standardization of flow-cytometric immunophenotyping represents an urgent and important task for the accurate and standardized diagnosis and monitoring of hematologic malignancies [22]. International efforts such as the EuroFlow Consortium have proposed standardized approaches encompassing instrument settings, antibody panels, sample preparation protocols, and data analysis protocols to improve reproducibility and reliability of these analyses [22].
Current Status and Clinical Utility in Modern Hematopathology
Flow cytometry has revolutionized the field of hematopathology, establishing itself as an indispensable tool for the diagnosis, classification, and monitoring of hematological malignancies [2]. This technology enables the rapid, multiparametric analysis of single cells, providing high-throughput information critical for identifying aberrant immunophenotypes in leukemias and lymphomas [2]. However, the inherent complexity of multicolor panels and the multitude of manual steps in the workflow introduce significant variability, necessitating rigorous standardization to ensure diagnostic accuracy and inter-laboratory reproducibility [2] [29]. The clinical community now stands to benefit substantially from concerted efforts to harmonize protocols, reagent panels, and data analysis strategies, thereby increasing the comparability of findings across different institutions and research studies [2] [30]. This application note details the current status of these standardization initiatives and provides actionable protocols for implementation in clinical and research settings.
Current Status: Achieving Reproducibility Through Standardization
Key Standardization Initiatives and Their Impact
International consortia have made significant strides in standardizing flow cytometric immunophenotyping. The EuroFlow Consortium, for instance, has developed fully standardized 8-color flow cytometry procedures, including standardized instrument settings, laboratory protocols, and antibody panels, specifically designed for the diagnosis and classification of hematological malignancies [29]. Similarly, the Human ImmunoPhenotyping Consortium (HIPC) has developed standardized, eight-color panels for identifying major immune cell subsets in peripheral blood, produced as pre-configured, lyophilized reagents in 96-well plates to minimize variability [30]. These efforts build upon earlier consensus protocols established by working groups aimed at achieving inter-laboratory reproducibility [8].
The implementation of such standardized protocols has demonstrated a remarkable reduction in cross-site variability. Studies show that while within-site variability is consistently low, cross-site variability is significantly reduced when centralized analysis is performed compared to site-specific analysis [30]. Furthermore, automated gating algorithms have now matured to a point where they can match the performance of central manual analysis for many panels, exhibiting little to no bias and comparable variability, thereby streamlining and standardizing the analysis pipeline [30].
Clinically Relevant Marker Panels for Hematological Malignancies
Standardized panels have been developed and agreed upon by several working groups, aligned with the World Health Organization (WHO) classification of haematolymphoid tumors and the Bethesda guidelines [2] [31]. The table below summarizes the essential markers for immunophenotyping major hematological malignancies.
Table 1: Standardized Immunophenotyping Markers for Hematological Malignancies
| AML | B-Cell ALL | T-Cell ALL | CLL | CML | B-Cell Lymphoma | T-Cell Lymphoma |
|---|---|---|---|---|---|---|
| CD13 | CD10 | CD1a | CD5 | CD11b | CD19 | CD2 |
| CD14 | CD19 | CD2 | CD19 | CD13 | CD20 | CD3 |
| CD33 | CD20 | CD3 | CD20 | CD14 | CD22 | CD4 |
| CD34 | CD22 | CD5 | CD23 | CD33 | CD79a | CD5 |
| CD45 | CD34 | CD7 | CD38 | CD34 | CD5^$,&^ | CD7 |
| CD64 | CD45 | CD45 | CD43 | CD45 | CD10^*^ | CD8 |
| CD117 | TdT | TdT | CD79b | CD30^§^ | CD30^§^ | |
| HLA-DR | CD200 | BCL2^*^ | ||||
| MPO | FMC7 | Cyclin D1^$^ |
Footnotes: CML diagnosis is definitively confirmed by proving the t(9;22) Philadelphia chromosome translocation (by FISH) or BCR-ABL1 fusion gene (by qRT-PCR). B-Cell Lymphoma markers vary by subtype: * Follicular lymphoma, $ Mantle cell lymphoma, & CLL/SLL, § Anaplastic large cell lymphoma. TdT: terminal deoxynucleotidyl transferase; MPO: myeloperoxidase. [2]
Experimental Protocols: Standardized Workflows for Reliable Results
EuroFlow Standard Operating Procedure (SOP) for Instrument Setup
Proper instrument configuration is the foundation of reproducible flow cytometry data. The EuroFlow SOP ensures consistent instrument performance across different laboratories and time points [29].
Protocol: Daily Instrument Setup and Quality Control
- Laser Optimization: Turn on lasers and allow them to stabilize for a minimum of 30 minutes. Using standardized calibration beads, adjust the photomultiplier tube (PMT) voltages for each detector to achieve the same target fluorescence values daily.
- Fluorescence Compensation: Prepare single-stain controls for each fluorochrome used in the panel. Use either compensation beads or cells stained with the respective antibody.
- Acquire data for each single-stain control.
- In the acquisition software, calculate the compensation matrix based on the spillover of each fluorochrome into other detectors.
- Apply this matrix to all experimental samples acquired during that session.
- Quality Control Check: Run a standardized control sample (e.g., lyophilized control PBMCs) to verify that the instrument is performing within established parameters and that the mean fluorescence intensity (MFI) for key markers falls within the expected range.
Standardized Staining Protocol for PBMC Immunophenotyping
The following protocol, adapted from HIPC and EuroFlow methodologies, ensures minimal variability in sample preparation and staining [30] [32].
Protocol: Staining of Peripheral Blood Mononuclear Cells (PBMCs)
Research Reagent Solutions: Table 2: Essential Reagents for Standardized Staining
| Reagent / Material | Function | Example |
|---|---|---|
| Lymphocyte Panel | Pre-configured, lyophilized antibody cocktail for specific cell subsets. | BD Lyoplate, EuroFlow panels [30] [29] |
| Viability Dye | Distinguishes live from dead cells to exclude compromised cells from analysis. | Ghost Dye, ViaDye Red, Fixable Viability Dye [32] |
| Brilliant Stain Buffer | Mitigates fluorescence resonance energy transfer (FRET) between certain dyes, preserving signal integrity. | BD Biosciences [32] |
| FACS Wash Buffer | Isotonic buffer for washing and resuspending cells without affecting antigenicity. | PBS with 2-5% FCS and 0.1% sodium azide [32] |
| Compensation Beads | Used to generate single-color controls for accurate fluorescence compensation. | CompBead Plus [32] |
Procedure:
Sample Preparation:
- Isolate PBMCs from fresh blood using Ficoll-Paque density gradient centrifugation.
- Wash cells twice in FACS Wash Buffer and resuspend to a concentration of 1 x 10^7 cells/mL.
- Note: For consistent results, use fresh, viable cells. If cryopreservation is necessary, standardize the freezing and thawing process meticulously.
Staining Process:
- Aliquot 2 x 10^6 cells (200 µL) into a 96-well U-bottom plate. Centrifuge at 400g for 5 minutes and decant the supernatant.
- (Optional Sequential Staining): For complex panels involving chemokine receptors, a two-layer staining may be optimal.
- First Layer: Resuspend the cell pellet in 15 µL of a pre-titrated antibody cocktail containing a few critical antibodies (e.g., CCR6, TCRγδ, CXCR5). Incubate for 30 minutes at room temperature (RT), protected from light [32].
- Second Layer: Add 35 µL of the remaining antibody cocktail directly to the well (without washing). Incubate for another 30 minutes at RT, protected from light.
- (Standard Staining): For most panels, resuspend the cell pellet in the complete, pre-mixed antibody cocktail. Incubate for 30 minutes at RT, protected from light.
Viability Staining and Fixation:
- Wash cells once with 120 µL FACS Wash Buffer.
- Resuspend cells in 50 µL of diluted viability dye (e.g., ViaDye Red, 1:5000 in PBS) and incubate for 20 minutes at RT.
- Wash cells once and fix with 100-200 µL of 1% paraformaldehyde (PFA) in PBS. Fixed samples are stable for up to 24-48 hours at 4°C before acquisition.
Data Analysis: Bridging Manual and Automated Gating
The analysis phase is a major source of variability. A hybrid approach leveraging both manual and automated methods enhances reproducibility [30].
Protocol: Standardized Data Analysis Workflow
Data Pre-processing:
- Apply the compensation matrix calculated during instrument setup to all sample files.
- Create a primary gate on cells, excluding debris, using FSC-A vs. SSC-A.
- Exclude doublets by gating single cells using FSC-H vs. FSC-A.
Centralized Manual Gating:
- For multi-center studies, transfer FCS files to a central site for analysis using a unified gating strategy.
- Identify major cell populations using a sequential, hierarchical gating strategy.
- Use fluorescence-minus-one (FMO) controls to guide accurate gate placement for dimly expressed markers.
Automated Gating:
- Utilize automated algorithms (e.g., those validated by the FlowCAP consortium) to identify predefined cell subsets.
- Tools like the
OpenCytoframework within the R environment can be used to implement and combine the best-performing algorithms [30]. - Validate the output of automated gates against manual analysis by an expert until the algorithm's performance is confirmed.
The following diagram illustrates the core workflow for standardized flow cytometry analysis.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of standardized flow cytometry relies on a core set of high-quality reagents and materials. The following table details the essential components of the toolkit.
Table 3: Key Research Reagent Solutions for Standardized Immunophenotyping
| Category | Specific Product/Type | Critical Function & Rationale |
|---|---|---|
| Standardized Antibody Panels | EuroFlow 8-color tubes; BD Lyoplate (HIPC panels) | Pre-configured, lyophilized panels eliminate reagent titration errors and ensure lot-to-lot consistency across sites [30] [29]. |
| Viability Dyes | Fixable viability dyes (e.g., ViaDye Red, Ghost Dye) | Critical for excluding dead cells which cause non-specific antibody binding, thereby improving data quality and accuracy [32]. |
| Quality Control Materials | Lyophilized control cells (e.g., CytoTrol); Compensation beads | Used for daily instrument performance tracking (QC) and creating single-stain controls for compensation, ensuring data integrity [30] [32]. |
| Staining Buffers | Brilliant Stain Buffer; FACS Wash (PBS + FCS + Azide) | Reduces fluorochrome interaction (FRET) in complex panels and provides an optimal medium for antibody staining and washing steps [32]. |
| Data Analysis Software | OpenCyto (R/Bioconductor); FlowJo with unified templates | Enforces consistent, reproducible gating strategies, either through automated algorithms or standardized manual gating templates [30]. |
The clinical utility of flow cytometry in modern hematopathology is inextricably linked to the implementation of standardized methodologies. From sample preparation and instrument setup to data analysis, the protocols and tools detailed in this application note provide a clear roadmap for achieving the high levels of accuracy, reproducibility, and inter-laboratory comparability required for both clinical diagnostics and translational research. The ongoing development of sophisticated automated analysis platforms and commercially available standardized reagent panels promises to further streamline workflows, making robust and reproducible immunophenotyping an achievable standard in laboratories worldwide.
Standardized Protocols and Gating Strategies for Robust Cell Analysis
Flow cytometric immunophenotyping serves as a fundamental pillar for the diagnosis, classification, and monitoring of hematological malignancies. The evolution from 3-4 color flow cytometry to 8-color multiparameter panels has enabled more precise identification and characterization of malignant cell populations. However, this increased complexity introduced significant inter-laboratory variability due to differences in reagent selection, instrument setup, and sample preparation protocols [33]. The EuroFlow Consortium (EU-FP6, LSHB-CT-2006-018708) established a comprehensive standardized framework encompassing instrument settings, laboratory protocols, and antibody panels to maximize reproducibility and comparability of data across different flow cytometers and clinical laboratories [34] [33]. This Application Note details the core methodologies and protocols of the EuroFlow standardization, providing researchers and drug development professionals with a validated system for immunophenotyping of hematological malignancies.
EuroFlow Standardized Instrument Settings
Fluorochrome Configuration and Instrument Selection
The EuroFlow consortium selected an 8-color approach as the minimum requirement for cost-effective immunophenotyping, allowing simultaneous use of backbone markers for cell population identification and characterization markers for detailed phenotypic analysis [33]. The standardized fluorochrome combinations were designed for three-laser flow cytometer instruments available at the project's inception, primarily the BD FACSCanto II and Beckman Coulter Navios [35].
Table 1: EuroFlow Standardized 8-Color Fluorochrome Configuration
| Laser Line | Fluorochrome 1 | Fluorochrome 2 | Fluorochrome 3 | Fluorochrome 4 |
|---|---|---|---|---|
| Blue (488 nm) | FITC (Pre-selected) | PE (Pre-selected) | PerCP / PerCP-Cy5.5 | PE-Cy7 |
| Red (633/635 nm) | APC (Pre-selected) | APC-Cy7 / Alexa Fluor 700 | - | - |
| Violet (405/407 nm) | Pacific Blue / Horizon V450 | Pacific Orange / Horizon V500 | - | - |
Key selection criteria included spectral compatibility, relative brightness, and availability of high-quality antibody conjugates [33]. The selection process involved both predefined fluorochromes based on extensive previous experience (FITC, PE, APC) and systematic evaluation of newer fluorochromes for the violet laser line [33].
Standard Operating Procedures for Instrument Setup
The EuroFlow standardization provides detailed Standard Operating Procedures for instrument setup and compensation to ensure consistent daily performance:
- Instrument Setup SOPs: Define specific target fluorescence values for rainbow calibration particles to standardize photomultiplier tube (PMT) voltages across instruments, ensuring comparable fluorescence measurements between laboratories [36].
- Compensation SOPs: Provide protocols for establishing fluorescence compensation matrices using specific antibody capture beads and stained cells to properly account for spectral overlap between the eight fluorochromes [33].
- Platform-Specific Protocols: The EuroFlow website hosts continuously updated SOPs for various flow cytometer models including BD FACSCanto II, BD LSRFortessa, BD Lyric, and Beckman Coulter Navios [36].
The feasibility of this cross-platform standardization was demonstrated in a Swiss multicenter study where both BD FACSCanto II and Beckman Coulter Navios instruments produced highly comparable data when following EuroFlow SOPs [37].
Standardized Antibody Panels for Hematological Malignancies
Panel Design Strategy and Validation
EuroFlow antibody panels were constructed through 2-7 sequential design-evaluation-redesign rounds using specialized software tools for multivariate data analysis [38]. This rigorous validation process against reference databases of normal and WHO-classified malignant cells distinguished EuroFlow from previous consensus panels based primarily on expert opinion [38].
The panel architecture follows a strategic combination of:
- Backbone Markers: Positioned at identical fluorochrome positions across tubes to provide consistent multidimensional localization of target cell populations [38].
- Characterization Markers: Optimally placed based on diagnostic utility for detecting aberrant phenotypes and differentiation patterns [38].
This design strategy enables both screening of unknown samples and comprehensive classification of identified malignancies through a structured diagnostic algorithm [38].
Comprehensive Antibody Panels
The EuroFlow consortium has developed and validated multiple specialized antibody panels for different diagnostic applications in hematological malignancies.
Table 2: EuroFlow Standardized Antibody Panels for Hematological Malignancies
| Panel Name | Primary Application | Key Backbone Markers | Characterization Markers | Clinical Utility |
|---|---|---|---|---|
| Acute Leukemia Orientation Tube (ALOT) | Initial screening of acute leukemias | CD45, CD34, CD117 | Myeloid: MPO, CD13, CD33Lymphoid: CD19, CD7, CD2 | Lineage assignment and blast identification [38] |
| Lymphoid Screening Tube (LST) | Screening of lymphoproliferative disorders | CD45, CD19, CD3, CD4, CD8 | CD20, CD10, CD5, CD38, CD56, kappa, lambda | B-cell and T-cell clonality assessment [37] |
| Multiple Myeloma MRD Panel | Minimal residual disease in myeloma | CD45, CD38, CD138 | CD19, CD27, CD56, CD28, CD117, cykappa, cylambda | High-sensitivity MRD detection (1x10⁻⁶) [36] |
| Chronic Lymphocytic Leukemia Panel | MRD assessment in CLL | CD45, CD19, CD5, CD3 | CD20, CD79b, CD43, ROR1, CD81, CD22 | Standardized MRD monitoring [39] |
The panels are continuously updated, with current compositions and technical information available through the official EuroFlow website [36].
Experimental Protocols and Workflows
Sample Preparation and Staining Protocol
The EuroFlow SOP for sample preparation ensures consistent processing across different laboratory settings:
- Sample Requirements: Defines optimal anticoagulants, storage conditions, and processing timelines for peripheral blood, bone marrow, and cerebrospinal fluid [36].
- Bulk Lysis Procedure: Uses ammonium chloride-based lysing solution for red blood cell removal while preserving leukocyte morphology and antigen expression [36].
- Staining Protocol: Standardizes antibody volumes, incubation times (typically 15-30 minutes at room temperature, protected from light), and washing steps to minimize technical variability [33].
The protocol includes specific modifications for different sample types, such as low cellularity specimens (cerebrospinal fluid) or solid tissue samples that require mechanical dissociation [36].
Data Acquisition and Analysis Framework
Standardized data acquisition and analysis complete the integrated EuroFlow workflow:
- Acquisition Standards: Defines minimum event counts for adequate sensitivity, particularly crucial for minimal residual disease detection [40].
- Software Tools: Employs Infinicyt software (Cytognos SL) for multivariate data analysis, including data merge and calculation functions for multi-tube analysis [38].
- Reference Databases: Uses accumulated data from normal and malignant samples for pattern recognition and automated population classification [38].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for EuroFlow Protocols
| Reagent/Material | Function | Specification/Alternative |
|---|---|---|
| 8-Antibody Panels | Simultaneous multiparameter analysis | Pre-defined combinations for specific malignancies [38] |
| Rainbow Calibration Beads | Instrument standardization | Target MFI values established for PMT calibration [36] |
| Ammonium Chloride Lysing Solution | Erythrocyte removal | Bulk lysis protocol for cell preservation [36] |
| Compensation Beads | Fluorescence compensation | Antibody capture beads for single-color controls [33] |
| Infinicyt Software | Data analysis | Multivariate analysis, data merge, and reference comparison [38] |
| Viability Markers | Exclusion of dead cells | 7-AAD or similar viability dyes [36] |
The EuroFlow standardization represents a comprehensive system for 8-color flow cytometric immunophenotyping of hematological malignancies. Through rigorously validated instrument settings, standardized antibody panels, and detailed laboratory protocols, the framework enables highly reproducible and comparable data across different laboratories and instrument platforms [34] [33]. The availability of continuously updated protocols through the EuroFlow website ensures that researchers and clinical laboratories can implement these standardized approaches for improved diagnostic accuracy and reliable monitoring of treatment response, particularly for minimal residual disease detection [36] [40]. For drug development professionals, these standardized protocols provide a robust platform for consistent immunophenotypic evaluation across multicenter clinical trials.
Immunophenotyping by flow cytometry is a fundamental technique for identifying and classifying immune cells based on the specific markers they express, providing a powerful tool for mapping immune system composition at the single-cell level [41]. In hematological malignancies research, this technique enables the detailed characterization of aberrant cell populations, contributing to accurate diagnosis, disease classification, and minimal residual disease (MRD) monitoring [42] [2]. The reliability of these analyses depends heavily on a systematic, stepwise gating strategy that progressively refines heterogeneous cell samples into specific, well-defined immune subsets [41]. This sequential approach ensures the accurate identification of target populations while effectively excluding artifacts such as dead cells and cell aggregates that could compromise data interpretation [27]. The implementation of standardized gating protocols is particularly crucial in clinical laboratories, where consistency and reproducibility directly impact diagnostic accuracy and therapeutic decision-making [2].
Foundational Principles of Flow Cytometry Gating
Gating involves the sequential application of digital boundaries to flow cytometry data to isolate specific cell populations based on their physical and fluorescent characteristics [27]. This process relies on two primary data types: light scatter measurements indicating physical properties, and fluorescence emissions revealing marker expression [2]. Forward scatter (FSC) correlates with cell size, while side scatter (SSC) indicates internal complexity or granularity [2]. Fluorescence parameters detect the presence of fluorochrome-conjugated antibodies bound to specific cellular markers, enabling immunophenotyping [41].
Data visualization employs histogram and scatter plot formats, each serving distinct analytical purposes. Histograms display single-parameter distributions, ideal for assessing marker expression levels across a population [28]. In contrast, scatter plots present dual-parameter data, enabling the simultaneous analysis of two characteristics and facilitating population discrimination through quadrant analysis [28] [43]. Dot plots, density plots, and contour plots represent variations of scatter plots that aid in visualizing population densities and identifying rare cell subsets [27] [28].
Table: Essential Flow Cytometry Data Visualizations
| Plot Type | Parameters Displayed | Primary Utility | Example Application |
|---|---|---|---|
| Histogram | Single parameter (fluorescence intensity or light scatter) | Display distribution of one characteristic across entire population | Assessing CD4 expression levels across lymphocytes [28] |
| Dot Plot | Two parameters (FSC/SSC or two fluorescence markers) | Identify population clusters based on two simultaneous characteristics | Distinguishing CD4+ vs. CD8+ T cells [28] |
| Density Plot | Two parameters with color-coding for event density | Visualize population densities in high-resolution | Identifying rare cell populations that form low-density clusters [28] |
| Contour Plot | Two parameters with contour lines for density | Highlight areas with high event concentration | Defining central population characteristics while de-emphasizing outliers [28] |
Stepwise Gating Strategy for Immunophenotyping
A robust gating strategy follows a hierarchical approach that progressively refines the population of interest. The sequential application of gates ensures that subsequent analyses focus on well-defined, viable single cells, minimizing technical artifacts and improving data quality [41].
Initial Gating Steps: Viability and Singlets
The initial gating steps focus on eliminating technical artifacts that could compromise downstream analysis. First, dead cells are excluded using viability dyes such as 7-AAD or propidium iodide, as dead cells nonspecifically bind antibodies and generate inaccurate fluorescence data [41]. Following viability gating, single cells are isolated using FSC-H (height) versus FSC-A (area) plotting to exclude doublets and cell aggregates [27]. Doublets appear with disproportionate FSC-A relative to FSC-H and can distort marker expression analysis by representing multiple cells measured as a single event [41].
Identification of Leukocyte Populations
After establishing the live, single-cell population, the next critical step involves identifying leukocytes using CD45 gating combined with light scatter properties [9]. CD45, a pan-leukocyte marker expressed on all white blood cells, effectively distinguishes leukocytes from other bone marrow or peripheral blood elements [9]. When combined with SSC parameters, CD45 gating enables the discrimination of major leukocyte lineages: lymphocytes (CD45 high, SSC low), monocytes (CD45 high, SSC intermediate), and granulocytes (CD45 moderate, SSC high) [9]. This step is particularly crucial in hematological malignancy diagnostics, where it facilitates the initial identification of abnormal blast populations that often exhibit characteristic CD45/SSC patterns [9].
Lineage-Specific Gating and Subset Identification
Following leukocyte identification, lineage-specific markers are applied to isolate target populations. For T-cell analysis, CD3 gating identifies the total T-cell population, which can be further subdivided into helper T cells (CD3+CD4+) and cytotoxic T cells (CD3+CD8+) [41]. B-cells are typically identified through CD19 expression, while myeloid lineages utilize markers such as CD14, CD16, CD13, and CD33 [2]. In hematological malignancies research, this lineage-specific gating often reveals aberrant immunophenotypes, including expression of markers not typically present on certain cell lineages (e.g., myeloid markers on lymphoblasts) or abnormal levels of expected markers [42] [2].
Advanced Subset Discrimination
The final gating steps focus on identifying specialized subsets within the broader lineage categories. For example, within the CD4+ T-cell population, regulatory T cells (Tregs) can be identified through co-expression of CD25 and FoxP3, often with low CD127 expression [41]. Similarly, memory and naive T-cell subsets can be discriminated using CD45RA/RO and CCR7 markers [41]. In B-cell malignancies, light chain restriction (kappa or lambda) assessment provides critical evidence of clonality, a hallmark of lymphoproliferative disorders [2]. For plasma cell disorders such as multiple myeloma, identification of abnormal plasma cells relies on CD138 and CD38 expression combined with aberrant features including CD56 expression, CD19 absence, and cytoplasmic light chain restriction [44].
Sequential Gating for Immune Cell Identification
Standardized Marker Panels for Hematological Malignancies
In clinical flow cytometry, standardized marker panels are essential for consistent diagnosis and classification of hematological malignancies. International consortia such as EuroFlow have developed comprehensive recommendations to ensure harmonized approaches across laboratories [42] [2]. These panels utilize carefully selected antibody combinations to identify lineage commitment, maturation stages, and aberrant expression patterns characteristic of specific hematological neoplasms.
Table: Standardized Immunophenotyping Panels for Hematological Malignancies
| Malignancy | Core Diagnostic Markers | Aberrant Patterns | MRD Markers |
|---|---|---|---|
| AML | CD34, CD117, CD13, CD33, CD15, CD64, CD14, HLA-DR, MPO [2] | Asynchronous antigen expression, lineage infidelity (e.g., CD7 on myeloid blasts) [42] | LAIPs (Leukemia-Associated Immunophenotypes), Different-from-Normal approach [42] |
| B-ALL | CD19, CD10, CD34, CD20, CD22, CD79a, TdT [2] | Aberrant myeloid marker expression (CD13, CD33), overexpression of CD10 [42] | CD19, CD10, CD34, CD20, CD38 with sensitivity 10⁻⁴–10⁻⁵ [42] |
| T-ALL | CD2, CD3, CD5, CD7, CD4, CD8, CD34, CD1a, TdT [2] | Aberrant loss of pan-T-cell markers, abnormal intensity of CD3 expression [42] | CD2, CD5, CD7, CD34, CD99 with sensitivity 10⁻⁴–10⁻⁵ [42] |
| CLL | CD19, CD5, CD20, CD23, CD43, CD79b, CD200 [2] | CD5+ B-cells with weak CD20, CD79b, and surface immunoglobulin [42] | CD19, CD5, CD20, CD81 with sensitivity 10⁻⁴–10⁻⁵ [42] |
| Multiple Myeloma | CD138, CD38, CD45, CD56, CD19, CD27, CD28, CD117 [42] | CD19⁻, CD56⁺, CD45⁻/low, CD27⁻, CD81⁻, cytoplasmic κ/λ restriction [44] | CD138, CD38, CD45, CD56, CD19, CD27 with sensitivity 10⁻⁵–10⁻⁶ [42] |
Experimental Protocol for Comprehensive Immunophenotyping
Sample Preparation and Staining
Proper sample handling is fundamental to successful immunophenotyping. Bone marrow or peripheral blood samples should be processed within 24-48 hours of collection, maintaining viability through appropriate anticoagulants and storage conditions [2]. For surface staining, cells are first resuspended in staining buffer containing phosphate-buffered saline with 1% bovine serum albumin. Antibody titration experiments should precede panel implementation to determine optimal reagent concentrations that maximize signal-to-noise ratios [41]. The staining protocol involves incubating 1×10⁶ cells per test with predetermined antibody cocktails for 20-30 minutes in the dark at 4°C [45]. Following incubation, cells are washed twice with staining buffer to remove unbound antibody before resuspension in fixation buffer or acquisition buffer [41]. For intracellular markers like FoxP3 or cytoplasmic immunoglobulins, cells require fixation and permeabilization using commercial kits according to manufacturer protocols [41].
Instrument Setup and Quality Control
Consistent instrument performance is critical for reproducible immunophenotyping. Daily quality control procedures should include calibration with standardized beads to ensure laser alignment and fluidic stability [2]. Voltage settings for photomultiplier tubes should be optimized to place negative populations appropriately on scale while maintaining positive signals within dynamic range [27]. Compensation controls, consisting of single-stained beads or cells for each fluorochrome in the panel, are essential to correct for spectral overlap between detection channels [41]. For multicolor panels exceeding 6-8 parameters, automated compensation calculation software improves accuracy and efficiency [46]. Fluorescence-minus-one (FMO) controls, which contain all antibodies except the one of interest, provide crucial references for establishing positive/negative boundaries, particularly for dimly expressed markers or continuous expression patterns [41].
Data Acquisition and Analysis
Data acquisition should target sufficient cellular events to ensure statistical significance, particularly for rare cell populations. For minimal residual disease detection, acquiring at least 3-5×10⁶ cells is recommended to achieve sensitivities of 10⁻⁴ to 10⁻⁶ [42]. During analysis, apply the stepwise gating strategy systematically across all samples, maintaining consistent gate positions based on biological and technical controls [28]. Utilize both "leukemia-associated immunophenotype" (LAIP) and "different-from-normal" approaches for MRD detection, with the former tracking patient-specific aberrant phenotypes identified at diagnosis and the latter identifying any abnormal differentiation patterns during follow-up [42]. For complex data sets, unsupervised clustering algorithms can complement conventional gating by identifying significant subpopulations that might be overlooked by sequential gating strategies [46].
The Scientist's Toolkit: Essential Research Reagents
Table: Key Research Reagent Solutions for Flow Cytometry Immunophenotyping
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Viability Dyes | 7-AAD, Propidium Iodide, Fixable Viability Dyes e780 [45] | Distinguish live from dead cells to exclude artifacts from analysis [41] |
| Lineage Marker Antibodies | CD45, CD3, CD19, CD14, CD33 [2] | Identify major leukocyte lineages and establish initial population gates [41] |
| Subset Discrimination Antibodies | CD4, CD8, CD56, CD16, CD123 [2] | Further refine populations into functional subsets (T-cells, NK cells, dendritic cells) [41] |
| Activation/Functional Marker Antibodies | CD25, CD69, HLA-DR, PD-1, CD38 [41] | Assess cellular activation status and functional capacity in immune monitoring [46] |
| Intracellular Staining Reagents | FoxP3, Ki-67, Cytokine antibodies [41] | Detect intracellular targets requiring cell permeabilization after surface staining [41] |
| Compensation Controls | UltraComp eBeads, ArC Beads, single-stained cells [41] | Correct for spectral overlap between fluorochromes in multicolor panels [46] |
| Cell Preparation Reagents | RBC Lysis Buffer, Ficoll for PBMC isolation [45] | Prepare single-cell suspensions from whole blood or bone marrow [2] |
Applications in Hematological Malignancies Research
The stepwise gating strategy finds critical applications across the spectrum of hematological malignancies research and clinical management. In acute leukemias, multiparametric flow cytometry enables comprehensive immunophenotypic characterization that complements genetic classification and provides independent prognostic information [42] [9]. The identification of aberrant antigen expression patterns facilitates the detection of minimal residual disease (MRD) at sensitivities of 10⁻³ to 10⁻⁶, far exceeding morphological assessment capabilities [42]. In mature lymphoid neoplasms, flow cytometry rapidly establishes clonality through light chain restriction in B-cell malignancies or abnormal T-cell receptor Vβ repertoire expression in T-cell disorders [2]. For multiple myeloma and other plasma cell dyscrasias, immunophenotyping distinguishes normal from malignant plasma cells based on characteristic antigen expression patterns including CD56 overexpression, CD19 downregulation, and CD45 underexpression [44].
The technological evolution from conventional flow cytometry to next-generation approaches continues to expand applications in hematological malignancies. Mass cytometry (CyTOF) increases parameter capacity by utilizing metal-conjugated antibodies and time-of-flight detection, enabling more detailed immunophenotypic profiling of complex malignancies [44]. Spectral flow cytometry simplifies panel design and improves data quality through full-spectrum fluorescence detection, while advanced computational analysis tools facilitate the identification of previously unrecognized cell populations through automated clustering algorithms [46]. These technological advances, combined with standardized gating strategies, promise to further enhance the precision and reproducibility of immunophenotyping in both research and clinical diagnostics.
In the research of hematological malignancies, multicolor flow cytometry has become an indispensable tool for detailed immunophenotyping. This technology enables the simultaneous detection of multiple cell surface and intracellular markers, providing powerful insights into disease classification, minimal residual disease detection, and therapeutic response monitoring. The fundamental principle involves using fluorochrome-conjugated antibodies that bind to specific cellular antigens, allowing researchers to characterize complex cell populations in heterogeneous samples such as peripheral blood and bone marrow [47].
The evolution from conventional to spectral flow cytometry represents a significant advancement in the field. While conventional flow cytometry identifies fluorophores primarily by their peak emissions, spectral flow cytometry captures the entire emission spectrum of each fluorophore, enabling more precise discrimination between signals [48]. This technological progression has facilitated the development of high-dimensional panels capable of assessing 30-40 parameters simultaneously, dramatically enhancing our ability to decipher the complex immunology of hematological cancers [49] [50]. For researchers focusing on leukemias and lymphomas, where identifying aberrant antigen expression patterns is crucial for diagnosis and classification, mastering multicolor panel design is essential [47].
Core Principles of Fluorophore Selection
Strategic Fluorophore-Antigen Pairing
The cornerstone of effective panel design lies in the strategic pairing of fluorochromes with antibodies based on antigen expression levels. The guiding principle is to pair the brightest fluorochromes with the weakest expressing antigens [51] [52]. This approach ensures adequate signal resolution for detecting dim markers, which is particularly important when characterizing rare cell populations or weakly expressed antigens in hematological malignancies.
When expression levels are unknown, erring on the side of using brighter fluorophores is recommended [51]. The relative brightness of common fluorophores used in flow cytometry follows a general hierarchy, with Phycoerythrin (PE) and Allophycocyanin (APC) among the brightest, while Fluorescein Isothiocyanate (FITC) and Peridinin-Chlorophyll-Protein (PerCP) are typically dimmer [52]. Understanding this brightness spectrum is crucial for making informed decisions during panel design.
Table 1: Fluorophore Brightness Guide for Common Flow Cytometry Dyes
| Fluorophore | Relative Brightness | Recommended Application |
|---|---|---|
| PE, APC | High | Low-expression antigens, rare cell populations |
| FITC, PerCP | Medium | Medium to high-expression antigens |
| Tandem Dyes | Variable (often high) | Dependent on stability and proper conjugation |
Managing Spectral Overlap
Spectral overlap occurs when the emission spectrum of one fluorophore spills into the detection channel of another, potentially causing false positive signals and compromising data accuracy [52]. In conventional flow cytometry, this issue is managed through compensation, a mathematical correction process that requires single-stained controls for each fluorophore in the panel [52] [47].
For optimal panel design, fluorophores should be spread as much as possible across the spectrum to minimize overlap [51]. Additionally, avoiding fluorochromes that can be excited by more than one laser (such as APC-Cy7) reduces complexity [51]. With the advent of spectral flow cytometry, researchers can now utilize fluorophores with similar emission maxima but distinct spectral signatures, providing greater flexibility in panel design [48].
Table 2: Spectral Overlap Management Strategies by Cytometry Type
| Strategy | Conventional Flow Cytometry | Spectral Flow Cytometry |
|---|---|---|
| Primary Method | Compensation | Spectral unmixing |
| Fluorophore Selection | Choose dyes with minimal emission spectrum overlap | Can use dyes with similar peaks but distinct full spectra |
| Key Metrics | Spillover spreading matrix | Similarity index, complexity index |
| Control Requirement | Single-stained controls for each fluorophore | Full spectrum controls |
Figure 1: Spectral Overlap and Detection Workflow. This diagram illustrates how fluorophore emission spectra can overlap, requiring compensation in conventional flow cytometry or spectral unmixing in full spectrum systems.
Panel Design Workflow and Optimization Strategies
Instrument-Specific Configuration
The first critical step in panel design involves understanding the technical specifications of the available flow cytometer. Researchers must determine the number and type of lasers, the number of detectors, and the specific optical filters available on their instrument [52] [47]. Each fluorophore must be excited by a corresponding laser wavelength, and its emission spectrum must align with the instrument's detection filters. Consulting with core facility managers or reviewing instrument manuals ensures proper alignment between panel design and instrument capabilities [52].
Modern spectral cytometers, such as the Cytek Aurora, utilize multiple lasers (typically 405nm, 488nm, 561nm, and 640nm) and capture full emission spectra across numerous detectors [49]. This configuration enables the use of advanced metrics like the similarity index (which quantifies spectral signature overlap between fluorophores) and the complexity index (which predicts interference among fluorophore combinations) [49]. These quantitative tools guide researchers in selecting fluorophore combinations that minimize spread and maintain resolution in high-parameter panels.
Systematic Panel Building Process
Designing an effective multicolor panel requires a methodical approach. The process begins with careful selection of antigen targets based on the biological question and cell populations of interest [53]. For hematological malignancies, this typically includes lineage markers, activation markers, and disease-specific antigens [47]. Following target selection, researchers should:
- Tier markers by biological importance and expression level, categorizing them as primary, secondary, or tertiary [54].
- Assign fluorophores following the brightness principle: brightest fluorophores to the least abundant markers [51] [54].
- Check reagent availability and consider custom conjugation for rare or novel targets [54].
- Review theoretical panel design using online panel design tools and spectral viewers to predict potential issues [54].
- Empirically test the panel using appropriate cell samples and controls to validate performance [53] [54].
Figure 2: Panel Design and Optimization Workflow. This workflow outlines the systematic process for developing effective multicolor flow cytometry panels, from initial planning to final validation.
Advanced Considerations for High-Dimensional Panels
As panel complexity increases, additional factors require consideration. For panels exceeding 20 parameters, careful attention must be paid to co-expressed markers (antigens expressed on the same cell population) [54]. When markers are co-expressed, they should be paired with fluorophores having minimal spectral overlap to maintain resolution [54]. Additionally, the use of tandem dyes (such as PE-Cy7 and APC-Cy7) requires caution as they can be susceptible to degradation, leading to altered fluorescence properties and increased compensation challenges [53].
In spectral flow cytometry, the traditional "dump channel" approach (combining multiple exclusion markers in one detector) is not recommended as it can cause issues with spectral unmixing [54]. Instead, assigning individual detectors to these markers enables deeper interrogation of cellular heterogeneity. For high-dimensional immunophenotyping assays, researchers have successfully developed panels containing up to 48 markers for comprehensive analysis of human peripheral blood and bone marrow samples [49].
Experimental Protocols for Panel Validation
Antibody Titration and Staining Protocol
Proper antibody titration is essential for achieving optimal signal-to-noise ratio in flow cytometry experiments. The following protocol ensures appropriate antibody concentrations:
- Prepare cell sample: Use cells known to express the target antigen(s) of interest. For hematological malignancies, cell lines or primary patient samples with known phenotype are ideal [47].
- Create antibody dilutions: Prepare a series of antibody dilutions, typically spanning a 10-fold concentration range (e.g., 0.1μg/mL to 10μg/mL).
- Stain cells: Aliquot cells into tubes and add titrated antibodies. Include unstained and single-color controls for compensation.
- Incubate and wash: Follow standard staining protocols for your cell type and antigen targets.
- Acquire data: Run samples on the flow cytometer, ensuring adequate event collection for statistical analysis.
- Analyze results: Determine the optimal concentration as the point where the Stain Index (separation between positive and negative populations) is maximized, typically before the plateau phase of binding [51].
Compensation Setup and Controls
Accurate compensation is critical for multicolor flow cytometry data integrity. The following protocol ensures proper compensation:
- Prepare compensation controls: For each fluorophore in the panel, prepare a sample stained singly with that fluorophore [52]. Compensation beads can be used as an alternative to cells [52].
- Match experimental conditions: Use the same antibody clone, fluorophore, and staining protocol as the experimental panels.
- Ensure adequate signal: The positive population should be at least 10% of the total sample and as bright or brighter than any experimental sample [52].
- Acquire compensation controls: Run each single-stained control, collecting sufficient events for accurate compensation calculations.
- Apply compensation: Use instrument software to calculate and apply compensation matrices to experimental samples.
- Verify compensation accuracy: Check that the median fluorescence of negative and positive populations is equal in spillover channels [52].
Fluorescence-Minus-One (FMO) Controls
FMO controls are essential for establishing accurate gating boundaries, particularly for dimly expressed markers or densely populated regions of scatter plots [41]. To implement FMO controls:
- Design FMO panels: For each marker of interest, prepare a control containing all antibodies except that specific marker.
- Use the same cell type: FMO controls should use the same cell type as experimental samples to account for autofluorescence.
- Set gating boundaries: Use FMO controls to establish the upper limit of background fluorescence for the omitted marker.
- Apply to experimental data: Use the FMO-defined gates when analyzing fully stained samples, particularly for population discrimination.
Essential Controls and Troubleshooting in Hematological Malignancies
Critical Controls for Diagnostic Accuracy
In the context of hematological malignancies, where accurate immunophenotyping directly impacts diagnosis and treatment decisions, implementing comprehensive controls is non-negotiable. Beyond standard compensation and FMO controls, several specific controls enhance data reliability:
- Viability dye inclusion: Dead cells nonspecifically bind antibodies, potentially leading to false positive results [41]. Amine-reactive viability dyes (e.g., LIVE/DEAD Fixable stains) effectively identify and exclude dead cells from analysis [54].
- Internal negative controls: Utilize populations within the sample that are known to lack expression of specific markers as internal negative controls [47].
- Reference samples: When available, include samples with known immunophenotypes (e.g., normal peripheral blood or bone marrow) as reference standards for instrument performance and staining quality.
- Longitudinal consistency controls: For studies monitoring disease progression or treatment response, implement strategies to maintain consistency across time points, such as using frozen aliquots of control samples [50].
Troubleshooting Common Issues
Even carefully designed panels can encounter issues during implementation. The following table addresses common challenges in multicolor flow cytometry for hematological malignancies:
Table 3: Troubleshooting Guide for Multicolor Flow Cytometry
| Problem | Potential Causes | Solutions |
|---|---|---|
| High Background | Dead cells, antibody concentration too high, insufficient washing | Titrate antibodies, include viability dye, increase wash steps |
| Poor Population Resolution | Spectral overlap, insufficient brightness for target antigen | Reassign fluorophores, use brighter fluorophore for low-expression targets |
| Unexpected Negative Populations | Antigen loss due to processing, antibody degradation | Verify sample integrity, check antibody performance |
| Increased Spread in Spectral Cytometry | High panel complexity, similar fluorophores | Check complexity index, select fluorophores with lower similarity |
| Inconsistent Results Between Runs | Instrument drift, reagent lot variation, operator error | Implement standardization protocols, use reference controls |
The Scientist's Toolkit: Research Reagent Solutions
Successful multicolor panel implementation requires careful selection of reagents and tools. The following essential materials form the foundation of robust immunophenotyping assays:
Table 4: Essential Research Reagents and Tools for Multicolor Flow Cytometry
| Reagent/Tool Category | Specific Examples | Function and Application |
|---|---|---|
| Viability Dyes | LIVE/DEAD Fixable Stains, Propidium Iodide, 7-AAD | Distinguish live from dead cells to reduce nonspecific binding |
| Bright Fluorophores | PE, APC, Brilliant Violet 421 | Detect low-abundance antigens and characterize rare cell populations |
| Tandem Dyes | PE-Cy7, APC-Cy7, Brilliant Violet 785 | Expand panel size by creating new spectral signatures |
| Lineage Markers | CD45, CD3, CD19, CD33 | Identify major cell populations in heterogeneous samples |
| Online Panel Design Tools | Thermo Fisher Panel Builder, Cytek SpectroFlo | Assist in theoretical panel design and fluorophore selection |
| Compensation Beads | Anti-Mouse/Rat Ig κ Compensation Beads | Provide consistent positive and negative populations for compensation controls |
| Reference Controls | Normal peripheral blood mononuclear cells, Cell lines | Standardize instrument performance and staining protocols across experiments |
Designing effective multicolor flow cytometry panels for immunophenotyping hematological malignancies requires a systematic approach that balances fluorophore brightness, antigen expression levels, and spectral characteristics. The advent of spectral flow cytometry has expanded possibilities for high-dimensional analysis, but has also increased the importance of careful panel design and validation. By following the principles and protocols outlined in this document—including strategic fluorophore-antigen pairing, comprehensive control strategies, and methodical troubleshooting—researchers can develop robust panels that generate reliable, reproducible data. As the complexity of immunophenotyping panels continues to grow, these foundational practices will remain essential for advancing our understanding of hematological malignancies and improving patient outcomes through more precise diagnostic and therapeutic approaches.
The accurate diagnosis and classification of hematological malignancies rely heavily on high-resolution flow cytometric immunophenotyping. This process fundamentally requires that cell samples are in the form of a high-quality single-cell suspension [55] [2]. The quality of this initial preparation step is paramount; even the most advanced flow cytometer cannot compensate for a poorly prepared sample, and suboptimal suspensions can lead to inaccurate data, instrument blockages, and compromised diagnostic results [56]. The core challenge lies in effectively dissociating cells from each other and from the extracellular matrix—particularly from solid tissues or adherent cultures—while preserving cell viability, surface antigens, and intrinsic biological states [57] [58]. Within the context of hematological malignancies, where identifying rare aberrant populations or minimal residual disease (MRD) is critical, standardized and effective sample preparation is not merely a technical step, but a foundational component of diagnostic accuracy and reproducibility across laboratories [59] [2].
The Critical Importance of a Single-Cell Suspension for Flow Cytometry
In flow cytometry, the fluidics system is designed to guide cells in a single file through a laser-based interrogation point [55]. When two or more cells are stuck together, forming a doublet or clump, they are registered as a single, large event. This can severely complicate data analysis by obscuring the true immunophenotype of individual cells and must be gated out during analysis [55]. The negative impacts of inadequate single-cell suspensions are multifaceted.
First, cell clumps can cause physical blockages in the flow cytometer's fluidic system, leading to instrument downtime and inaccurate scatter and fluorescence measurements [57] [56]. Second, clumping can result in non-uniform staining and fixation, as reagents may not adequately penetrate the clump, leading to uneven staining of the cells within and potentially masking antigen expression [57]. Third, for the analysis of rare cell populations—such as residual blast cells in post-treatment monitoring—clumping can lead to a preferential loss of specific cell types, skewing the quantitative analysis and compromising the sensitivity of MRD detection [57] [2]. Therefore, the goal of sample preparation is to create a monodispersed, viable cell suspension that ensures each cell is individually and accurately analyzed for all parameters of interest [56].
Best Practices and General Principles for Sample Preparation
Regardless of the starting material, several universal principles underpin the successful creation of a high-quality single-cell suspension. Adherence to these best practices minimizes artifacts and ensures data integrity.
Maintaining High Cell Viability
Dead and dying cells are detrimental to flow cytometry data. Their compromised membranes allow antibodies and fluorescent dyes to bind non-specifically, creating high background fluorescence and potentially leading to false-positive results [56]. To maintain high viability:
- Add Protein: Supplement buffers and media with protein (e.g., 2% Fetal Bovine Serum or 1% Bovine Serum Albumin) at all stages of cell processing to protect cell integrity. An exception is when staining with fixable viability dyes, where protein should be added immediately after the staining step to avoid dye absorption by the protein itself [57].
- Practice Gentle Resuspension: Fragile cells, such as those from hematological samples, require gentle but thorough mixing. Avoid vortexing at maximum speed, and instead use careful pipetting or gentle vortexing of the cell pellet before adding buffer [57].
Preventing and Removing Cell Clumps
The formation of cell clumps is a major obstacle that must be actively managed.
- Use DNase: DNA released from damaged cells acts as a glue, causing cell aggregation. Adding DNase I (e.g., at 25 mg/mL) to isolation and resuspension buffers digests free DNA, effectively reducing clumping [57].
- Use EDTA: For cell types whose adhesion is cation-dependent, adding a cation chelator like EDTA (e.g., 2 mM) to buffers can prevent clumping by chelating calcium and magnesium ions [57].
- Filter the Suspension: Filtering the cell suspension through a fine mesh cell strainer (typically 40-70 µm) before analysis is a critical step to remove any remaining clumps and debris, thereby preventing instrument blockages [57] [56].
- Mix Before Acquisition: Cells can settle and form clumps while waiting to be acquired. Always vortex, flick, or pipette the sample immediately before loading it onto the flow cytometer [57].
Quality Control and Monitoring
Consistently check the quality of the cell suspension throughout the preparation process.
- Visual Inspection: Large clumps can often be seen with the naked eye. A simple visual check of the suspension in the tube can provide an initial assessment of quality [57].
- Microscopy: Using a low-power light microscope to examine the sample is a straightforward method to confirm that a monodispersed suspension has been achieved and to assess cell health [57].
- Viability Staining: Incorporate a viability dye, such as propidium iodide or 7-AAD, to quantitatively assess the proportion of live cells and to permit their selective gating during data analysis [56].
Protocols for Different Sample Types
The specific methodology for creating a single-cell suspension varies significantly depending on the sample origin. The following protocols are adapted from standardized procedures.
Protocol for Adherent Cell Cultures
Adherent cell lines require detachment from the culture vessel. The choice of detachment method is critical to preserve surface epitopes [60].
- Detach Cells: Remove culture medium and wash cells with a buffer free of Ca²⁺/Mg²⁺. Detach cells using a gentle enzyme-based solution like Accutase or TrypLE. These are generally preferred over trypsin, which can cleave peptide sequences and degrade cell surface proteins [57] [60]. Alternatively, a non-enzymatic cell dissociation buffer containing EDTA can be used.
- Transfer and Dissociate: Transfer the cell suspension to a conical centrifuge tube. Use a pipette to gently dissociate any remaining clumps.
- Wash and Count: Centrifuge the cells (300-400 x g for 4-5 minutes), discard the supernatant, and resuspend the pellet in flow cytometry staining buffer. Perform a cell count and viability analysis.
- Resuspend: Centrifuge again and resuspend the cell pellet at a final concentration of 1 x 10⁷ cells/mL (or as required for the specific experiment) [60].
Protocol for Lymphoid Tissues (Spleen, Lymph Nodes)
Lymphoid tissues are typically easy to dissociate, often requiring only mechanical disruption [60].
- Harvest Tissue: Place the freshly harvested tissue (e.g., spleen, thymus, lymph node) into a culture dish containing 10 mL of ice-cold flow cytometry staining buffer.
- Mechanical Disruption: Tease the tissue apart by pressing it with the plunger of a 3-mL syringe. Alternatively, mash the tissue between the frosted ends of two glass microscope slides.
- Filter: Pass the resulting cell suspension through a nylon mesh cell strainer placed on top of a conical tube to remove clumps and debris.
- Wash and Count: Centrifuge the suspension (300-400 x g for 4-5 minutes) and resuspend in buffer. Perform a cell count and viability analysis.
- Final Resuspension: Centrifuge again and resuspend the cells at the desired concentration for staining and acquisition [60].
Protocol for Solid Tissues and Tumors
Solid tissues and tumors require a combination of mechanical and enzymatic dissociation to break down the extracellular matrix [58] [60].
- Mince Tissue: Harvest the tissue and mince it into 2-4 mm pieces using sterile scissors or a scalpel blade.
- Enzymatic Digestion: Incubate the tissue pieces with an appropriate enzyme cocktail (e.g., collagenase, trypsin) diluted in PBS at the optimal temperature and time according to the enzyme manufacturer's instructions.
- Disperse and Filter: After digestion, disperse the cells by gentle pipetting and filter the suspension through a cell strainer into a conical tube.
- Wash: Centrifuge the cells (300-400 x g for 4-5 minutes) and wash the pellet twice with PBS to remove enzyme residues.
- Final Preparation: Resuspend the final cell pellet in flow cytometry staining buffer, perform a cell count and viability analysis, and adjust to the desired concentration [60].
Table 1: Quantitative Comparison of Cell Dissociation Methods for Adherent Cells
| Method | Single Cell Yield | Impact on Viability | Impact on Surface Antigens | Key Applications |
|---|---|---|---|---|
| Trypsin Alone | 31.9% [61] | Can be harsh, reducing viability [55] | Can cleave and destroy epitopes [57] | General cell culture, not recommended for sensitive immunophenotyping |
| Collagenase-Trypsin Mix | 62.1% - 85.5% [61] | Higher viability maintained [61] | Better preservation of protein expression [61] | High-throughput flow cytometry, sensitive immunophenotyping |
| Accutase/ TrypLE | High [57] | High viability maintained [57] | Gentle; minimal epitope damage [57] | Ideal for delicate primary cells and stem cells |
| Non-Enzymatic (EDTA) | Variable [57] | High viability maintained [57] | No enzymatic damage to proteins [57] | When preserving sensitive surface receptors is critical |
Protocol for Whole Blood and Bone Marrow
These samples are naturally in suspension but require processing to isolate the mononuclear cells or to lyse red blood cells.
- Dilution: Dilute the blood or bone marrow sample at least 1:1 with PBS.
- Density Gradient Centrifugation: Carefully layer the diluted sample over an equal volume of Ficoll-Paque density gradient medium. Centrifuge at 400 x g for 20 minutes at room temperature with the brake OFF.
- Harvest PBMCs: Collect the peripheral blood mononuclear cell (PBMC) layer (a cloudy ring) at the interface between the PBS and Ficoll layers, and transfer it to a new tube.
- Wash and Count: Fill the tube with PBS to wash the cells, then centrifuge (300-400 x g for 4-5 minutes). Discard the supernatant, resuspend the cell pellet in buffer, and perform a cell count and viability analysis.
- Final Resuspension: Centrifuge once more and resuspend the PBMCs at the desired concentration [60]. For some applications, particularly in clinical hematology, whole blood is used with a red blood cell lysis step after immunostaining [55].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Single-Cell Suspension Preparation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Accutase/TrypLE | Gentle enzyme blends for cell detachment. | Preferred over trypsin for preserving surface antigens in adherent cells and primary cultures [57]. |
| Collagenase | Enzyme that degrades collagen in the extracellular matrix. | Essential for dissociating solid tissues and tumors; often used in combination with other enzymes [61] [58]. |
| DNase I | Degrades free DNA released from dead cells. | Reduces cell clumping and aggregation caused by DNA "glue"; add to dissociation and wash buffers [57]. |
| EDTA | Chelates calcium and magnesium ions (cation chelator). | Weakly dissociates adherent cells; prevents cell adhesion and clumping in suspension by inhibiting cation-dependent adhesion [57] [60]. |
| Cell Strainers | Nylon mesh filters with defined pore size (e.g., 70 µm). | Removes cell clumps and tissue debris prior to staining and flow cytometry analysis to prevent instrument blockages [57] [60]. |
| Viability Dyes (PI, 7-AAD) | Stain dead cells with compromised membranes. | Allows for the identification and subsequent gating exclusion of dead cells during data analysis to reduce background noise [56]. |
| Fc Receptor Blocking Solution | Blocks non-specific binding of antibodies to Fc receptors. | Crucial for reducing background staining on immune cells, such as monocytes and macrophages, improving signal-to-noise ratio [56]. |
Standardization in the Context of Hematological Malignancies
In clinical diagnostics, the need for reproducible and comparable results across laboratories has driven major efforts toward standardization. Initiatives like the EuroFlow Consortium have developed fully standardized laboratory procedures, including sample preparation, for 8-color flow cytometric immunophenotyping [59]. The implementation of such Standard Operating Procedures (SOPs) is key to minimizing inter-laboratory variability, which can be introduced through manual steps and operator bias [59] [2]. Standardization covers all aspects, from the specific clones of antibody reagents and their fluorochrome conjugates to the precise protocols for tissue dissociation and staining [59] [8]. This is particularly critical for the detection of minimal residual disease (MRD), where the accurate identification of very small aberrant cell populations requires exceptionally high-quality sample preparation and standardized panels to ensure consistency and sensitivity across different testing sites and over time [2].
Workflow and Troubleshooting
The following diagram summarizes the key decision points and steps in the journey to create a high-quality single-cell suspension, incorporating critical checks and troubleshooting actions.
Diagram 1: Workflow for Preparing Single-Cell Suspensions
The generation of a high-quality single-cell suspension is a critical, non-negotiable first step in any flow cytometry experiment for hematological malignancies research and diagnosis. The protocols and best practices outlined here—from the judicious selection of detachment reagents for adherent cells to the combined mechanical and enzymatic digestion of solid tissues—provide a roadmap for achieving this goal. By prioritizing cell viability, actively preventing aggregation, and implementing rigorous quality control checks, researchers and clinicians can ensure that the data generated is accurate, reproducible, and clinically meaningful. In an era of increasingly complex multiparameter flow cytometry and heightened requirements for standardized diagnostics, mastery of these fundamental sample preparation techniques is more important than ever.
Flow cytometry is an indispensable tool for the diagnosis, classification, and monitoring of hematological malignancies, enabling multiparametric single-cell analysis of complex biological samples [2] [62]. The technique relies on the detection of specific protein markers, which can reside on the cell surface or within the cell's interior. Accurately detecting these targets requires fundamentally different staining approaches: extracellular staining for surface proteins and intracellular staining for internal components [63]. The distinction between these methods is particularly crucial in immunophenotyping of leukemias and lymphomas, where markers may include cell surface clusters of differentiation (CD markers), intracellular enzymes like myeloperoxidase (MPO), or nuclear proteins such as terminal deoxynucleotidyl transferase (TdT) [2] [64]. Proper sample preparation, including fixation and permeabilization for intracellular targets, is essential for preserving cell morphology and obtaining reliable, reproducible data, which are critical for accurate disease classification and minimal residual disease (MRD) detection [2]. This application note provides detailed protocols and key considerations for implementing both extracellular and intracellular staining methods within the context of hematological malignancy research.
Key Differences Between Intracellular and Extracellular Staining
The fundamental difference between intracellular and extracellular staining lies in the cellular barriers that antibodies must cross to reach their targets. Extracellular staining detects antigens present on the outer surface of the cell membrane, which are readily accessible to antibodies in their native state. This method uses live, unfixed cells and does not require membrane disruption [63]. In contrast, intracellular staining targets antigens located within the cell's interior—in the cytoplasm, organelles, or nucleus. Accessing these targets requires a two-step process: fixation to stabilize and "freeze" the cellular structure, followed by permeabilization to create pores in the lipid membrane, allowing antibodies to enter the cell [65] [66].
The choice between these methods is dictated by the target antigen's localization and the research objectives. For comprehensive immunophenotyping of hematological malignancies, a combination of both is often necessary. For instance, classifying acute leukemias requires surface markers (e.g., CD19, CD33) alongside intracellular markers (e.g., MPO, TdT) to determine lineage commitment and maturation stage [2]. When combining these techniques, the standard practice is to stain surface markers first on live cells, then fix and permeabilize the cells before proceeding with intracellular antibody incubation [63] [67] [66]. This sequential approach preserves the structural integrity of surface epitopes, which can be altered or destroyed by fixatives and detergents.
Table 1: Core Differences Between Intracellular and Extracellular Staining
| Parameter | Extracellular Staining | Intracellular Staining |
|---|---|---|
| Target Location | Cell surface membrane [63] | Cytoplasm, organelles, nucleus [63] |
| Cell Status | Live, unfixed cells [63] | Fixed and permeabilized cells [63] |
| Key Steps | Antibody incubation, washing [63] | Fixation, permeabilization, then antibody incubation [63] |
| Primary Application | Immunophenotyping (e.g., CD markers) [2] | Detecting internal proteins (e.g., cytokines, TdT, MPO) [2] [64] |
| Compatibility with Tandem Dyes | High | Variable; methanol damages PE and APC [67] |
Fixation and Permeabilization Methods
Fixation Agents
Fixation stabilizes the cellular structure by cross-linking or precipitating macromolecules, preventing antigen diffusion and preserving the cell's state at the time of fixation.
Aldehydes (e.g., Paraformaldehyde-PFA): PFA (1-4%) is the most common cross-linking fixative. It preserves cellular structure by creating covalent bonds between proteins and nucleic acids [63] [66]. Standard protocol involves incubating cells in ice-cold 1-4% PFA for 15-20 minutes on ice [63] [65]. Cross-linking fixatives are often preferable for studying post-translational modifications like phosphorylation [65]. A potential drawback is increased cellular autofluorescence due to protein cross-linking [65].
Organic Solvents (e.g., Methanol, Ethanol, Acetone): These agents act by precipitating proteins and dissolving lipids. Methanol (90%) is a common choice, often used as a standalone fixative and permeabilization agent. Cells are typically resuspended in ice-cold 90% methanol and incubated for 10-15 minutes at -20°C or on ice [63] [68]. Alcohol-based fixation is suitable for many intracellular antigens, including some phospho-proteins, and fixed cells can be stored at -20°C for extended periods [65] [67]. However, these solvents denature protein-based fluorophores like PE and APC and significantly alter light scatter properties, complicating population gating [68] [67].
Permeabilization Agents
Permeabilization disrupts the cell membrane to allow antibody entry. The choice of agent depends on the strength required to access the target antigen.
Mild Detergents (e.g., Saponin): Saponin creates small, reversible pores in the membrane by complexing with cholesterol [63] [65]. It is typically used at concentrations of 0.1-0.5% and requires its presence in all subsequent wash and antibody buffers to maintain permeability [65]. Saponin is ideal for detecting secreted cytokines or cytoplasmic antigens near the plasma membrane and is less likely to alter surface antigen epitopes [63] [67].
Strong Detergents (e.g., Triton X-100, Tween-20): These non-ionic detergents (e.g., 0.1-0.3% Triton X-100) solubilize lipid membranes, creating larger, permanent pores [63] [65]. They are suitable for most intracellular targets, including nuclear antigens [63]. Tween-20 has been shown to provide high mean fluorescence intensity for intracellular nucleic acid detection [69]. However, harsh detergents can lyse cells with prolonged incubation and may damage some surface epitopes [67].
Organic Solvents (e.g., Methanol): As mentioned, methanol simultaneously fixes and permeabilizes by precipitating proteins and dissolving lipids. It is highly effective for nuclear and cytoskeletal antigens but is the most damaging to cell structure and light scatter profiles [63] [65].
Table 2: Comparison of Fixation and Permeabilization Methods
| Method | Mechanism | Recommended Concentration | Incubation | Best For | Considerations |
|---|---|---|---|---|---|
| Paraformaldehyde (PFA) | Cross-links proteins [66] | 1-4% [63] | 15-20 min, on ice or RT [63] [65] | Surface staining prior to perm; phospho-protein detection [65] | Can increase autofluorescence; requires subsequent permeabilization [65] |
| Methanol | Precipitates proteins, dissolves lipids [65] | 90% in PBS [68] | ≥10 min, on ice [68] | Nuclear antigens; long-term storage; some phospho-proteins [63] [65] | Denatures PE/APC; alters light scatter; not for surface epitopes [68] [67] |
| Saponin | Creates cholesterol pores (reversible) [65] | 0.1-0.5% [63] [65] | 10-30 min, RT [65] [69] | Cytoplasmic antigens, cytokines [63] [67] | Pores are reversible; must be included in all buffers [65] |
| Triton X-100 | Solubilizes membranes (irreversible) [63] | 0.1-1% [63] | 10-15 min, RT [63] [65] | Most intracellular targets, including nuclear [63] | Harsh; can lyse cells over time [67] |
| Tween-20 | Solubilizes membranes (irreversible) [69] | 0.2% [69] | 30 min, RT [69] | Intracellular nucleic acids (e.g., rRNA) [69] | Provides high fluorescence intensity for RNA detection [69] |
The following diagram illustrates the decision-making workflow for selecting the appropriate staining method and corresponding fixation/permeabilization agents based on the target antigen's location.
Detailed Protocols
Protocol for Extracellular Staining
This protocol is designed for detecting cell surface antigens, such as CD markers used in immunophenotyping [63] [70].
- Sample Preparation: Harvest cells and prepare a single-cell suspension in ice-cold phosphate-buffered saline (PBS) or washing buffer (PBS with 0.5-1% BSA or 5-10% FCS) [63]. For blood samples, use red blood cell (RBC) lysis buffer. Determine cell count and viability, which should ideally be 90-95% [63]. Centrifuge at 200-300 x g for 5 minutes at 4°C and resuspend to a concentration of 0.5–1 x 10^6 cells/mL [63].
- Viability Staining (Optional but Recommended): Incubate cells with a viability dye (e.g., 7-AAD, DAPI) according to the manufacturer's instructions in the dark at 4°C [63]. Wash cells twice with wash buffer. Note: DNA-binding viability dyes cannot be used with fixed cells.
- Fc Receptor Blocking: To prevent non-specific antibody binding, resuspend the cell pellet in a blocking buffer (e.g., 2-10% goat serum, human IgG, or mouse anti-CD16/CD32) and incubate for 30-60 minutes in the dark at 4°C [63].
- Antibody Staining: Resuspend cells in 100 µL of FACS buffer containing the pre-titrated fluorescently-labeled antibody (typically 0.5-1 µg). Vortex gently and incubate on ice for 30 minutes in the dark [70].
- Washing: Wash cells with 2 mL of FACS buffer. Centrifuge at 200-300 x g for 5 minutes at 4°C and carefully aspirate the supernatant.
- Analysis: Resuspend cells in 0.5-2 mL of FACS buffer and analyze immediately on a flow cytometer. Alternatively, fix cells with 1-2% PFA and store at 4°C in the dark for up to one week [70].
Protocol for Simultaneous Intracellular and Extracellular Staining
This sequential protocol is critical for immunophenotyping, where both surface markers (e.g., CD3, CD19) and intracellular markers (e.g., TdT, MPO, cytokines) need to be analyzed on the same cell [63] [65] [66].
- Surface Staining: Perform steps 1-5 of the extracellular staining protocol. Crucial Note: If using protein-based fluorophores like PE or APC, ensure you will NOT be using methanol for permeabilization later, as it denatures these fluorophores [67].
- Fixation: After the final wash from surface staining, resuspend the cell pellet in 100 µL of ice-cold 4% PFA per 1 million cells. Gently vortex and incubate for 15-20 minutes at room temperature in the dark [65].
- Washing: Add 1 mL of PBS and pellet cells by centrifugation. Aspirate the supernatant into a PFA waste container. Repeat once [63] [65].
- Permeabilization: Choose one method based on your target antigen (refer to Table 2).
- For Saponin (Mild): Resuspend cells in 100 µL of permeabilization buffer (0.1% saponin, 0.5% BSA in PBS). Incubate for 10 minutes at room temperature. Note: Saponin is reversible; all subsequent wash and antibody buffers must contain 0.1% saponin to maintain permeability [65].
- For Triton X-100 (Strong): Resuspend cells in 100 µL of permeabilization buffer (0.1-0.3% Triton X-100 in 0.5% BSA/PBS). Incubate for 10-15 minutes at room temperature [65].
- For Methanol (Strong): Ensure cells are pre-chilled. Resuspend pellet in 100 µL of ice-cold 90% methanol while gently vortexing. Incubate for a minimum of 10 minutes on ice [68] [65]. Cells can be stored in methanol at -20°C at this point.
- Intracellular Antibody Staining: Wash cells twice with the appropriate permeabilization wash buffer (e.g., containing saponin if that method was used). Resuspend the cell pellet in 100 µL of permeabilization buffer containing the pre-titrated intracellular antibody. Incubate for 1 hour at room temperature or as per antibody manufacturer's instructions [68] [65].
- Final Washes and Analysis: Wash cells twice with permeabilization buffer. Perform a final wash with PBS alone to remove detergents. Resuspend cells in 200-500 µL of PBS and analyze on a flow cytometer [68].
The Scientist's Toolkit: Key Reagent Solutions
Successful flow cytometry experiments rely on a set of essential reagents, each serving a specific function in sample preparation and staining.
Table 3: Essential Reagents for Flow Cytometry Staining
| Reagent | Function/Purpose | Example Formulations |
|---|---|---|
| FACS/Wash Buffer | Provides an isotonic medium for washing and staining; proteins like BSA or serum reduce non-specific binding. | PBS with 0.5-1% BSA or 5-10% Fetal Calf Serum (FCS); often includes 0.1% sodium azide to prevent capping [63] [70]. |
| Viability Dyes | Distinguishes live from dead cells for exclusion during analysis, as dead cells bind antibodies non-specifically [63]. | DNA-binding dyes: 7-AAD, DAPI, TOPRO3 (for live cells). Amine-reactive fixable dyes (for use with fixed cells) [63]. |
| Fc Blocking Reagent | Blocks Fc receptors on cells to prevent non-specific antibody binding, reducing background signal. | 2-10% species-specific serum (e.g., goat serum), human IgG, or monoclonal antibodies against Fc receptors (e.g., anti-CD16/CD32) [63]. |
| Fixatives | Stabilizes cellular structure and immobilizes intracellular antigens. | 1-4% Paraformaldehyde (PFA) [63] [65], 90% Methanol [63] [68], 100% Acetone [63]. |
| Permeabilization Agents | Disrupts the cell membrane to allow antibody access to intracellular targets. | Mild: Saponin (0.1-0.5%) [65]. Strong: Triton X-100 (0.1-1%), Tween-20 (0.2%) [63] [69]. |
| Antibody Dilution Buffer | Provides an optimal environment for antibody binding while maintaining cell stability. | 0.5% BSA in PBS; for saponin protocols, use 0.1% saponin in 0.5% BSA/PBS [68] [65]. |
Critical Considerations for Hematological Malignancy Research
Standardization of flow cytometry protocols is paramount in clinical hematology to ensure accuracy, reproducibility, and comparability of results across laboratories [2]. The workflow involves many manual steps susceptible to operator bias, making consistent protocol adherence essential for reliable diagnosis and MRD monitoring [2]. The fixation and permeabilization steps are critical variables that can significantly impact staining quality and data interpretation.
Fluorochrome compatibility is a major consideration in panel design. Methanol permeabilization, while effective for many intracellular targets, denatures common protein-based fluorophores like PE and APC, as well as some tandem dyes [67]. Researchers should consult compatibility tables and manufacturer data when designing multiparametric panels. Conversely, many small molecule dyes (e.g., Alexa Fluor dyes, PerCP) and certain cyanine dyes are methanol-resistant [67].
The choice of permeabilization method can also "unmask" or destroy specific epitopes. For example, while aldehyde fixation is generally preferred for phospho-protein detection, some targets like phospho-STAT proteins are best detected following ice-cold methanol treatment, which can uncover these epitopes [65]. Therefore, researchers must validate their fixation and permeabilization conditions for each new intracellular target, referring to antibody manufacturer guidelines whenever possible [65]. Finally, it is crucial to include proper experimental controls, such as an unstained sample, a viability dye control, and a fluorescence-minus-one (FMO) control for each channel, all treated with the same fixation and permeabilization reagents to account for their effects on scatter properties and autofluorescence [67].
Solving Common Challenges and Enhancing Data Quality
Flow cytometric immunophenotyping serves as an indispensable tool for the diagnosis, classification, and monitoring of hematological neoplasms [62] [2]. The technique's power lies in its ability to perform multiparametric single-cell analysis, rapidly identifying phenotypically abnormal populations in diseases including leukemia, lymphoma, plasma cell neoplasms, and myelodysplastic syndromes [62] [2]. However, the reliability of this data is fundamentally dependent on the implementation of proper experimental controls. Controls account for variability and background noise, enabling researchers to distinguish specific signals from non-specific background and ensuring that the generated data is both valid and reproducible [71].
In the context of hematological malignancy research, where accurate detection of aberrant immunophenotypes can directly impact diagnosis and treatment decisions, the role of controls becomes even more critical [2]. This application note details three essential controls—unstained, fluorescence minus one (FMO), and isotype controls—framing their use within the rigorous requirements of immunophenotyping for hematological cancers. We provide detailed protocols and data presentation guidelines to standardize assay setup and enhance the quality of diagnostic and research findings.
Theoretical Foundation and Applications of Core Controls
Comparative Functions of Essential Controls
The following table summarizes the primary role, key applications, and limitations of each control type in the context of immunophenotyping hematological malignancies.
Table 1: Essential Controls for Flow Cytometry in Hematological Malignancy Research
| Control Type | Primary Role & Purpose | Key Applications in Hematological Malignancies | Key Limitations |
|---|---|---|---|
| Unstained Control | Determines the inherent autofluorescence of cells and sets baseline for instrument voltages [72] [71] [73]. | Establishing negative population boundaries; identifying autofluorescence in blast populations or myeloid cells [72] [73]. | Does not account for any antibody-related staining or spectral overlap [74]. |
| FMO Control | Serves as a gating control to define the upper boundary of background fluorescence, accounting for fluorescence spread from other fluorochromes in the panel [74] [71] [75]. | Critical for accurately gating dim or variable expression markers (e.g., CD34, CD117, CD5 in some contexts) and identifying weakly positive blast populations [74] [75]. | Does not control for nonspecific antibody binding; requires more sample and reagents [74] [76]. |
| Isotype Control | Qualitatively assesses the level of non-specific antibody binding caused by Fc receptor binding or other non-epitope-driven interactions [76] [77]. | Assessing background "stickiness" in cultured primary cells or cell lines; verifying Fc blocking efficiency for myeloid lineage cells [72] [76]. | Should not be used to set positive/negative gates; matched perfection is impractical [76]. |
Visualizing the Control Selection Workflow
The following diagram illustrates the decision-making process for selecting the appropriate control based on the experimental objective.
Detailed Experimental Protocols
Protocol 1: Unstained Control Setup
Purpose: To determine the inherent autofluorescence of the cell sample and establish baseline settings for photomultiplier tubes (PMTs) [73].
Materials:
- Single-cell suspension from patient peripheral blood, bone marrow, or lymph node biopsy.
- Appropriate buffer (e.g., PBS + 0.5% BSA).
- Flow cytometer.
Method:
- Sample Preparation: Prepare a single-cell suspension of your experimental cells using standard protocols for lysing red blood cells if necessary [2].
- Aliquot: Transfer an aliquot of cells (e.g., 100 µL containing 1x10^5 to 1x10^6 cells) into a FACS tube.
- Washing: Wash cells with 2 mL of buffer. Centrifuge at 300-500 x g for 5 minutes. Carefully decant the supernatant.
- Resuspension: Resuspend the cell pellet in an appropriate volume of buffer (e.g., 200-500 µL) for acquisition.
- Data Acquisition: Analyze the unstained control sample on the flow cytometer first. Adjust the forward scatter (FSC), side scatter (SSC), and fluorescence detector voltages (PMTs) so that the negative cell population is positioned within the first decade of the logarithmic plot [73].
Protocol 2: Fluorescence Minus One (FMO) Control Setup
Purpose: To accurately determine the boundary between negative and positive staining for a specific marker in a multicolor panel, accounting for fluorescence spread from all other fluorochromes [74] [75].
Materials:
- Single-cell suspension.
- Full antibody panel including all fluorescently-conjugated antibodies.
- Buffer.
Method:
- Panel Design: For a multicolor panel with 'n' antibodies, prepare 'n' FMO control tubes. Each tube contains all antibodies except one [75].
- Staining: For a given FMO control (e.g., the "CD34-FMO" tube), add all antibodies from your panel except the CD34-specific antibody to the cell aliquot.
- Incubation: Follow your standard staining protocol for incubation, washing, and resuspension.
- Gating: During analysis, use the FMO control to set the positive gate for the omitted marker. The FMO control shows the maximum fluorescence signal that the negative population can have in that channel due to background and spillover from other dyes [74]. The gate should be set so that 99% of the cells in the FMO control are considered negative [75].
Table 2: Example FMO Control Matrix for a 4-Color Panel
| Tube Name | Anti-CD3 (FITC) | Anti-CD4 (PE) | Anti-CD8 (PE-Cy5) | Anti-CD45 (PE-Cy7) |
|---|---|---|---|---|
| Full Stain | + | + | + | + |
| FMO-FITC | - | + | + | + |
| FMO-PE | + | - | + | + |
| FMO-PE-Cy5 | + | + | - | + |
| FMO-PE-Cy7 | + | + | + | - |
Protocol 3: Isotype Control Setup
Purpose: To qualitatively assess the level of non-specific antibody binding in the experiment [76] [77].
Materials:
- Single-cell suspension.
- Specific, fluorescently-conjugated antibody of interest.
- Fluorescently-conjugated isotype control antibody, matched to the specific antibody in host species, isotype (IgG1, IgG2a, etc.), light chain, fluorophore, and F:P (fluorophore-to-protein) ratio [76] [77].
- Buffer, potentially including FcR blocking reagent [72].
Method:
- Sample Preparation: Prepare two aliquots of the same cell sample.
- Staining: Stain one aliquot with the specific antibody. Stain the second aliquot with the matched isotype control antibody. Use the same concentration and staining conditions for both tubes.
- Fc Blocking (Recommended): For samples containing monocytes, macrophages, or B-cells, include an Fc receptor blocking step prior to antibody staining to reduce false positives [72] [73].
- Acquisition & Analysis: Analyze both samples on the flow cytometer. A well-optimized assay with effective blocking will show minimal staining in the isotype control tube. The isotype control reveals the level of background fluorescence caused by non-specific interactions; it should not be used to define positive versus negative cells or to set gating boundaries [76].
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents required for implementing these critical controls in a research or clinical flow cytometry setting.
Table 3: Essential Research Reagents for Flow Cytometry Controls
| Reagent / Material | Function & Purpose | Application Notes |
|---|---|---|
| Viability Dye (e.g., 7-AAD, Propidium Iodide, DRAQ7) [72] [73] | Distinguishes live from dead cells; dead cells exhibit high autofluorescence and nonspecific binding, which can lead to inaccurate results. | Use with unfixed cells. Essential for removing dead cell artifacts, particularly in samples from tissue biopsies or cell cultures [72]. |
| Compensation Beads [72] | Used to create single-stained controls for accurate fluorescence compensation, correcting for spectral spillover between channels. | Provide a consistent and abundant particle for setting compensation, superior to using rare cell populations [72]. |
| Fc Receptor (FcR) Blocking Reagent [72] [73] | Blocks non-specific binding of antibodies to Fc receptors on immune cells (e.g., monocytes, macrophages, dendritic cells). | Critical when staining myeloid cells or certain cell lines (e.g., THP-1, Daudi). Reduces false positives and is verified by isotype control [72] [73]. |
| Matched Isotype Control [76] [77] | A negative control antibody that matches the specific antibody's species, isotype, light chain, fluorophore, and conjugation. | Used to qualitatively evaluate non-specific antibody binding. Must be carefully matched to be meaningful [76]. |
| Biological Controls (e.g., KO cell lines, known positive/negative samples) [74] [73] | Serve as a biological reference to confirm staining specificity and evaluate overall assay performance. | The gold standard for confirming antibody specificity, especially for intracellular staining [73]. |
Integration in Hematological Malignancy Immunophenotyping
In the diagnosis of hematological malignancies, the identification of abnormal populations relies on detecting deviations from the normal immunophenotype of cells [2]. Proper use of controls is fundamental to this process. For example, the detection of dim CD45 expression on blasts in Acute Myeloid Leukemia (AML) or the variable expression of CD5 in certain B-cell lymphomas requires FMO controls for accurate gating, as these populations may not be clearly separated from negatives [74] [2]. Furthermore, the "stickiness" of many malignant cells, particularly in lymphoma, makes the use of isotype controls combined with FcR blocking vital for interpreting the specificity of antibody binding [76].
Standardization, including the use of validated antibody panels and consistent control strategies as highlighted in the Bethesda International Consensus Conference recommendations, is key to improving diagnostic accuracy and comparability across laboratories [62] [2]. The integration of AI into flow cytometry data analysis promises further enhancements in standardization and automated gating, but the fundamental need for well-characterized experimental controls remains unchanged [78].
In immunophenotyping hematological malignancies, the accuracy of data interpretation is paramount for both basic research and clinical decision-making. A significant challenge in achieving this accuracy is non-specific staining, which can obscure true antigen-specific signals and lead to flawed data. Two of the most prevalent sources of this background signal are the non-specific binding of antibodies to Fc receptors (FcRs) on immune cells and the uptake of antibodies by dead cells [79] [72]. Fc receptors can bind the constant region (Fc portion) of antibodies, independent of the antigen-binding site, causing antibodies to attach to cells that do not express the target antigen [79]. Meanwhile, dead cells, with their compromised membrane integrity, exhibit increased autofluorescence and non-specific antibody binding, potentially resulting in false-positive populations [80] [72]. Within the context of heterogeneous samples like peripheral blood mononuclear cells (PBMCs) or primary tumor samples, failing to address these issues can severely impact the reliability of identifying leukemia-associated immunophenotypes (LAIPs) and other critical biomarkers [81]. This application note provides detailed protocols and data-driven strategies to mitigate these key sources of error, thereby ensuring the generation of robust and reproducible flow cytometry data.
Mechanisms and Impacts of Non-Specific Staining
Fc Receptor-Mediated Binding
Fc receptors are constitutively expressed on the surface of various immune cells, including monocytes, macrophages, B cells, and natural killer (NK) cells [79] [72]. During staining, the Fc region of fluorophore-conjugated antibodies can bind to these receptors, leading to false-positive signals that are misinterpreted as antigen expression. This is particularly problematic in hematological malignancies where the tumor microenvironment (TME) is rich in phagocytic cells, and the malignant cells themselves may express FcRs [79] [81]. This non-specific binding increases background noise, reduces the signal-to-noise ratio, and can mask the detection of dimly expressed but biologically significant antigens.
Dead Cell-Induced Artifacts
Dead cells are a major source of interference in flow cytometry for several reasons. Their permeable membranes allow intracellular components like NADPH and flavins to be exposed, causing significant autofluorescence, especially upon excitation with a 488 nm laser [72]. Furthermore, the damaged membranes permit fluorophore-conjugated antibodies to enter the cell and bind non-specifically to intracellular components, a process not related to target epitope recognition [80] [72]. In populations with low viability, such as processed primary samples or stressed cultured cells, these effects can lead to a drastic overestimation of marker positivity and a distorted view of cell population frequencies [80]. The 1999 study by Schmid et al. emphasized that light scatter differences are often insufficient to discriminate dead cells, particularly after permeabilization, underscoring the necessity of fluorescent viability dyes [80].
Table 1: Comparison of Common Viability Dyes for Flow Cytometry
| Viability Dye | Principle of Action | Excitation/Emission | Compatibility with Fixation | Key Considerations |
|---|---|---|---|---|
| Propidium Iodide (PI) | Cell-impermeable, intercalates into DNA of dead cells. | ~535 nm/~617 nm [4] | Not compatible (stains after fixation) | Inexpensive; requires DNAse-free conditions. |
| 7-AAD (7-Aminoactinomycin D) | Cell-impermeable, binds DNA of dead cells. | ~546 nm/~647 nm [80] | Not compatible | Good for DNA content analysis combined with viability [80]. |
| DRAQ7 | Cell-impermeable far-red fluorescent DNA dye. | ~488 nm, ~633 nm/~694 nm, ~780 nm [72] | Compatible | Photostable; suitable for long-term live-cell imaging. |
| Calcein AM | Cell-permeable; converted to green fluorescent calcein by live-cell esterases. | ~494 nm/~517 nm [72] | Compatible (after hydrolysis) | Stains live cells; requires functional intracellular esterases. |
Experimental Protocols
Protocol 1: Blocking Fc Receptors
Objective: To prevent non-specific antibody binding via Fc receptors, thereby reducing background staining and improving signal specificity.
Materials:
- Single-cell suspension (e.g., PBMCs, cultured cell lines)
- Fc Blocking Reagent (e.g., Human Seroblock, Mouse Seroblock [79] or purified anti-CD16/32 for mouse cells)
- Flow Cytometry Staining Buffer (PBS without Ca2+/Mg2+, containing 0.1-1% BSA or 1-10% FBS) [79]
- Refrigerated centrifuge
Procedure:
- Prepare Cells: Harvest and wash cells in cold staining buffer. Pellet cells by centrifugation (e.g., 300-400 x g for 5 minutes) and aspirate the supernatant thoroughly.
- Resuspend and Block: Resuspend the cell pellet in a sufficient volume of staining buffer containing the Fc blocking reagent. A typical recommendation is to incubate with the Fc block for 5-10 minutes at room temperature [79].
- Stain with Antibodies: Without washing, proceed directly to adding your pre-titrated, fluorophore-conjugated antibody cocktail to the same tube. Mix gently.
- Incubate and Wash: Complete the standard staining protocol (incubation for 20-30 minutes on ice protected from light), followed by one or two washes with staining buffer.
- Resuspend and Acquire: Resuspend the stained cell pellet in an appropriate volume of staining buffer for data acquisition on the flow cytometer.
Technical Notes:
- Fc blocking should be performed immediately before the antibody staining step.
- For tissue homogenates or cell lines known to have high FcR expression (e.g., Daudi, THP-1), this step is critical [72].
- The blocking reagent can often be added directly to the primary antibody mixture to streamline the workflow.
Protocol 2: Excluding Dead Cells with 7-AAD
Objective: To accurately identify and exclude dead cells from flow cytometry analysis using the fluorescent DNA dye 7-AAD.
Materials:
- Single-cell suspension
- Flow Cytometry Staining Buffer
- 7-AAD stock solution (e.g., 100-200 µg/mL)
- Non-fluorescent Actinomycin D (AD) - Optional, for intracellular staining protocols [80]
- Refrigerated centrifuge
Procedure for Surface Staining Only:
- Stain Surface Antigens: Complete the surface antibody staining protocol as described, including the Fc blocking step.
- Add 7-AAD: Following the final wash, resuspend the cell pellet in staining buffer. Add 7-AAD to a final concentration of 0.002-2.5 µg/mL and mix thoroughly.
- Incubate: Incubate the cells for 5-20 minutes on ice, protected from light. Do not wash after adding 7-AAD.
- Acquire Data: Analyze the samples on the flow cytometer within 30-60 minutes. The 7-AAD signal is typically detected in the PerCP-Cy5.5 or APC-Cy7 channel (~660 nm).
Procedure for Combined Surface & Intracellular Staining (ICS): The method described by Schmid et al. is particularly suited for low-viability samples and complex staining panels [80].
- Stain Surface Antigens: Perform surface staining and wash.
- Add 7-AAD and Block: Resuspend the cells in staining buffer containing 7-AAD and a high concentration (e.g., 50 µg/mL) of non-fluorescent Actinomycin D (AD). Incubate for 20 minutes on ice.
- Fix and Permeabilize: Without washing, proceed to fixation and permeabilization using a commercial buffer set. The presence of AD during permeabilization prevents the transfer of 7-AAD from dead cells to the DNA of live cells, preserving the viability discrimination [80].
- Stain Intracellular Antigens: Perform intracellular staining in the presence of permeabilization buffer, then wash and resuspend for acquisition.
Technical Notes:
- Titrate the 7-AAD concentration for your specific cell type to achieve clear separation between live (7-AAD negative) and dead (7-AAD positive) populations.
- Since 7-AAD binds DNA, it is incompatible with subsequent cell cycle analysis unless a specialized method like the one above is used.
Workflow and Data Analysis
The following workflow integrates Fc receptor blocking and dead cell exclusion into a comprehensive staining procedure for immunophenotyping.
Gating Strategy for Accurate Analysis
A sequential gating strategy is essential to isolate the population of interest for reliable analysis. The key first step is the exclusion of dead cells and doublets.
- Exclude Doublets: Plot Forward Scatter-Area (FSC-A) vs. Forward Scatter-Height (FSC-H). Gate on the population of single cells that show a linear relationship between height and area [27].
- Exclude Dead Cells: From the singlets gate, create a plot of the viability dye (e.g., 7-AAD) versus FSC-A or SSC-A. Gate tightly on the negative population to select only live cells for downstream analysis [80] [27].
- Identify Lymphocyte Population: On the live, single cells, use FSC-A vs. SSC-A to gate on the lymphocyte population based on size and granularity.
- Immunophenotyping: Apply subsequent fluorescent antibody gates (e.g., CD45 vs. CD3) to the live, single lymphocyte population to identify specific immune cell subsets.
Table 2: Essential Controls for Mitigating Non-Specific Staining
| Control Type | Purpose | Composition | How to Use |
|---|---|---|---|
| Fc Block Control | Verify efficacy of Fc receptor blocking. | Sample + Fc Block, then stained. | Compare with unstained and fully stained samples. Reduced MFI indicates effective blocking. |
| Unstained Control | Measure cellular autofluorescence. | Cells only, no antibodies. | Set baseline fluorescence and detector voltages. |
| Viability Dye Control | Confirm dead cell identification. | Single-stained sample with viability dye. | Set the gate to separate live (dye-negative) from dead (dye-positive) cells. |
| Fluorescence Minus One (FMO) Control | Accurately set positive/negative gates for each marker. | Cells stained with all antibodies in the panel except one. | Determines the upper boundary of negative events, accounting for spillover from other fluorochromes [72]. |
| Isotype Control | Assess non-specific antibody binding (limited utility). | Antibody with same isotype and fluorophore but irrelevant specificity. | Not recommended for setting positivity gates. Can give a general sense of background [72]. |
The Scientist's Toolkit: Key Research Reagent Solutions
The following table lists essential reagents for implementing the protocols described in this note.
Table 3: Essential Reagents for Fc Blocking and Dead Cell Exclusion
| Reagent / Kit | Function | Example Products | Key Features |
|---|---|---|---|
| Fc Blocking Reagents | Blocks non-specific binding to Fcγ receptors on immune cells. | Human Seroblock, Mouse Seroblock [79]; purified anti-CD16/32. | Species-specific; ready-to-use formulations. |
| Cell Staining Buffer | Antibody diluent and wash buffer; reduces non-specific binding. | BioLegend's Cell Staining Buffer [79]; PBS with 0.1-1% BSA or 1-10% FBS. | Protein carrier; often free of biotin, Ca2+, Mg2+. |
| Viability Dyes (Cell-Impermeable) | Distinguishes live from dead cells by staining permeable membranes. | 7-AAD, Propidium Iodide (PI), DRAQ7 [80] [72]. | DNA-binding; excluded from live cells. |
| Viability Dyes (Live Cell Staining) | Labels live cells via enzymatic activity. | Calcein AM [72]. | Requires functional intracellular esterases. |
| Fixation/Permeabilization Buffers | For intracellular (IC) staining; some kits preserve viability dye signal. | Cyto-Fast Fix/Perm Buffer Set, True-Phos Perm Buffer [79]. | Commercial kits ensure reproducibility for IC staining. |
| Compensation Beads | Create single-color controls for accurate spectral compensation. | Anti-mouse/rat/hamster Igκ Compensation Beads. | Bind to antibodies, providing a uniform positive signal without cells. |
Antibody Titration and Fluorophore Optimization for Maximum Signal-to-Noise
In the field of immunophenotyping hematological malignancies, high-parameter flow cytometry has become an indispensable tool for lineage assignment, maturational analysis, and detection of minimal residual disease [8]. The complexity of these analyses demands rigorous optimization of staining protocols to maximize data quality and reproducibility. A cornerstone of this optimization is the implementation of precise antibody titration and strategic fluorophore allocation, which together dramatically improve the signal-to-noise ratio, reduce spillover spreading, and enhance the resolution of dimly expressed antigens—a common challenge in leukemic cell populations [82] [83]. This application note provides detailed protocols and data-driven recommendations to achieve maximum sensitivity and specificity in flow cytometric assays for hematological research.
Core Principles of Signal-to-Noise Optimization
The Role of Antibody Titration
Antibody titration is not merely a reagent-saving exercise; it is a critical step for minimizing nonspecific binding and reducing spillover spreading in multicolor panels. Using a saturating antibody concentration can lead to increased background noise and compromise the detection of dim signals in other detectors. In contrast, a separating concentration provides optimal resolution between positive and negative populations [83].
The Stain Index (SI) is a key metric for quantifying the quality of an antibody-fluorophore conjugate. It is calculated as follows [83]:
SI = (Mean Fluorescence Intensity of Positive Cells – Mean Fluorescence Intensity of Negative Cells) / (2 × Standard Deviation of the Negative Population)
Titration should aim to identify the antibody dilution that yields the highest SI, indicating the best possible separation.
Strategic Fluorophore Selection and Panel Design
The pairing of fluorophores with specific cellular targets is a fundamental decision. Adherence to the following principles is crucial for panel success [83]:
- Pair bright fluorophores with antibodies for low-abundance antigens. For example, in hematological malignancies, markers with dim expression or those that are internalized upon stimulation benefit from the brightest available dyes.
- Pair dim fluorophores with antibodies for highly expressed antigens. This prevents bright signals from overwhelming the detector and spilling over into multiple channels.
- Use spectrally distinct fluorophores for co-expressed markers. This minimizes spillover spreading between channels that must be resolved independently.
- Use spectrally similar fluorophores for markers expressed on mutually exclusive cell populations. When subpopulations are gated separately, the spillover between their respective channels becomes less critical.
Experimental Protocols
Protocol: Antibody Titration for Optimal Signal-to-Noise
Purpose: To determine the optimal working concentration of an antibody-conjugate that provides the best separation between positive and negative cell populations.
Materials:
- Single-cell suspension (e.g., cell line or primary patient sample)
- Titration of the antibody-conjugate of interest (e.g., serial 2-fold dilutions)
- Staining buffer (e.g., PBS with 1-2% FBS)
- Flow cytometer
Method:
- Prepare the antibody dilutions. Begin with the manufacturer's recommended concentration and perform a series of 2-fold dilutions in staining buffer.
- Aliquot the cells. Distribute a consistent number of cells (e.g., 0.5-1 million) into as many tubes as there are antibody dilutions, plus one tube for an unstained/negative control.
- Stain the cells. Add each antibody dilution to its corresponding cell pellet, resuspend, and incubate for the standardized time (e.g., 20-30 minutes on ice in the dark).
- Wash and acquire. Wash the cells twice with staining buffer, resuspend in a fixed volume, and acquire data on the flow cytometer using previously optimized detector voltages.
- Analyze and calculate. For each dilution, gate on the population of interest. Record the Mean Fluorescence Intensity (MFI) of both the positive and negative populations and calculate the Stain Index (SI) for each dilution.
- Plot and determine optimum. Plot the calculated SI against the antibody concentration. The separating concentration is typically at or near the peak of the SI curve, before the curve plateaus [83].
Protocol: Extended Antibody Incubation for Enhanced Sensitivity
Purpose: To improve the detection sensitivity and resolution of low-abundance or difficult-to-stain antigens by leveraging extended incubation times, which allow the antibody-antigen reaction to approach equilibrium.
Materials:
- Single-cell suspension
- Titrated antibody
- Staining buffer
- Flow cytometer
Method:
- Stain with optimized concentration. Use the separating concentration of antibody determined in Protocol 3.1.
- Extend incubation time. Instead of a standard 30-minute incubation, incubate the antibody with the cells for an extended period (e.g., 16-20 hours/overnight) at 4°C in the dark.
- Wash and acquire. Proceed with washing and data acquisition as in the standard protocol.
Key Considerations:
- Improved Sensitivity: Extended incubation times can lead to a substantial increase in MFI for a given antibody, or allow for a 10-fold reduction in antibody usage to achieve the same MFI as a short incubation [82].
- Reduced Variability: Overnight staining brings the antibody-antigen interaction closer to equilibrium, which significantly reduces inter-experimental variability and facilitates the accurate pooling of data from experiments conducted over extended time courses [82].
- Intracellular Staining: This method is particularly beneficial for intracellular targets (e.g., cytokines, transcription factors) where antigen access is restricted. Fixation and permeabilization followed by overnight staining can vastly improve the resolution of proteins like Foxp3 [82].
The following workflow visualizes the decision process for staining optimization:
Data Presentation and Analysis
Quantitative Comparison of Staining Conditions
Table 1: Impact of Antibody Concentration and Incubation Time on Staining Resolution. Data adapted from Andersson et al. and PMC9827877 [82].
| Antibody | Concentration (μg/mL) | Incubation Time | MFI (Positive) | MFI (Negative) | Stain Index |
|---|---|---|---|---|---|
| CXCR5-P-e610 | 0.5 | 15 min | 1,850 | 210 | 8.5 |
| CXCR5-P-e610 | 0.5 | 30 min | 3,900 | 220 | 18.1 |
| CXCR5-P-e610 | 0.5 | 60 min | 7,200 | 230 | 32.6 |
| CXCR5-P-e610 | 0.05 | 16 hrs | 7,150 | 225 | 32.2 |
| CD25-APC | 0.5 (Sat.) | 30 min | 45,000 | 1,500 | 15.0 |
| CD25-APC | 0.1 (Sep.) | 30 min | 15,000 | 800 | 9.4 |
| CD25-APC | 0.1 (Sep.) | 16 hrs | 16,500 | 750 | 11.0 |
Fluorophore Performance and Spillover
Table 2: Relative Brightness and Spillover Spreading Characteristics of Common Fluorophores. SE = Spillover Error [83].
| Fluorophore | Relative Brightness | High Spillover Channels | Recommended Use |
|---|---|---|---|
| FITC | Moderate | Minimal | Highly expressed antigens |
| APC | Bright | Minimal | Low-abundance antigens |
| PE-Cy7 | Bright | Multiple (e.g., BV711, APC) | Use with caution; pair with bright, abundant antigens |
| Brilliant Violet 711 (BV711) | Bright | PerCP-Cy5.5, APC, PE | Low-abundance antigens; check spillover matrix |
| PerCP-Cy5.5 | Moderate | PE, BV711 | Moderately expressed antigens |
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Flow Cytometry Optimization.
| Item | Function/Application |
|---|---|
| Viability Dye (e.g., LIVE/DEAD Fixable Stain) | Critical for excluding dead cells from analysis, which non-specifically bind antibodies and drastically skew population statistics [83]. |
| Pre-titrated Antibody Panels | Commercially available panels that have been pre-optimized for concentration and spectral overlap, saving time and validation resources. |
| Compensation Beads | Uniform particles used to establish single-color controls for accurate spectral overlap compensation on the flow cytometer. |
| FMO (Fluorescence Minus One) Controls | Controls containing all antibodies in a panel except one, essential for setting accurate positive gates, especially for dim markers and continuous expression patterns [83]. |
| Standardized Staining Buffer | Buffer formulation that ensures consistent pH and protein content to minimize non-specific antibody binding during staining procedures. |
Integrated Workflow for Panel Validation
The following diagram summarizes the comprehensive, iterative process of designing and validating a high-performance flow cytometry panel, integrating the principles of titration, fluorophore selection, and control strategies.
In the field of hematological malignancies research, high-quality flow cytometry data is paramount for accurate immunophenotyping, minimal residual disease (MRD) monitoring, and subsequent therapeutic decision-making [42]. The integrity of this data is directly dependent on the quality of sample acquisition. Issues such as clogs, low signal strength, and high background fluorescence represent significant technical hurdles that can compromise data resolution and lead to misinterpretation of experimental results. This application note details the standardized protocols and troubleshooting methodologies developed by consortia such as EuroFlow and the Human ImmunoPhenotyping Consortium (HIPC) to address these common acquisition challenges, ensuring the generation of reliable and reproducible data in a clinical research setting [30] [84].
Experimental Protocols for Acquisition Quality Control
Standardized Instrument Setup and Quality Control
The EuroFlow consortium has established that a rigorously standardized instrument setup protocol is the foundation for reproducible data acquisition and for mitigating issues related to signal variability and background noise [84].
Procedure:
- Startup and Laser Warm-up: Allow the flow cytometer lasers to warm up for a minimum of 30 minutes to ensure stable output and consistent fluorescence measurements.
- Optical Alignment: Perform daily quality control using standardized fluorescent beads. Assess the coefficient of variation (CV) for peak signals to verify that the fluidics and optics are in optimal alignment.
- Fluorescence Compensation: Create a compensation matrix using single-stain controls. For multi-color panels exceeding 6 colors, the EuroFlow protocol emphasizes the use of antibody-capture beads (e.g., CompBeads) stained with each individual fluorochrome-conjugated antibody used in the panel [84]. This corrects for spectral spillover, which is a major contributor to high background in adjacent channels.
- Threshold Setting: Set the threshold primarily on Forward Scatter (FSC) to eliminate sub-cellular debris and small particles from acquisition, thereby reducing background and the risk of data file contamination. The threshold should be set high enough to exclude noise but low enough to capture all target cells [30].
Pre-Acquisition Sample Preparation to Prevent Clogs
Clogs in the flow cytometer's fluidics system are frequently caused by aggregates or large particulates in the sample. The following protocol, derived from standardized sample preparation guidelines, is designed to minimize this risk [30] [4].
Procedure:
- Filtration: Following staining and final resuspension, pass the single-cell suspension through a sterile 35-70 µm cell strainer or nylon mesh.
- Visual Inspection: Before loading the tube onto the instrument, briefly vortex the sample to ensure a homogeneous suspension.
- Pipetting: Avoid pipetting from the bottom of the tube where aggregates may have settled.
Establishing a Gating Strategy to Identify and Exclude Background
A clear gating strategy is essential to distinguish specific signal from background, a process critical for identifying rare cell populations like those in MRD detection [42] [28].
Procedure:
- Viability Gating: Use a live/dead fluorescent dye (e.g., propidium iodide or a fixable viability dye) to exclude dead cells, which non-specifically bind antibodies and contribute significantly to background fluorescence [4].
- Singlets Gating: Plot FSC-H (height) versus FSC-A (area) to identify and gate on single cells, excluding doublets or multiple cells that can cause aberrant signal readings [30].
- Lymphocyte/Mononuclear Gate: Use FSC-A and Side Scatter (SSC-A) to gate on the target population of interest (e.g., lymphocytes), excluding debris and other cell types [28].
The logical workflow for systematic troubleshooting is summarized in the diagram below.
Data Presentation and Analysis
Quantitative Metrics for Signal and Background Assessment
Systematic assessment of acquisition quality relies on specific quantitative metrics derived from the flow cytometer's output. The table below outlines key parameters and their target values for optimal data quality in immunophenotyping.
Table 1: Key Performance Metrics for Flow Cytometry Acquisition
| Parameter | Description | Target / Acceptable Range | Measurement Tool |
|---|---|---|---|
| Sample Pressure | Stability of core stream pressure | Stable, within instrument specification | Instrument pressure sensor & event rate monitor |
| CV of Standard Beads | Measure of optical alignment and focusing | Typically < 3% for bright beads | Quality control beads (e.g., Spherotech RCP-30-5A) |
| Stain Index (SI) | Ratio of specific signal to background spread [84] | Maximize (Higher is better) | Calculated: (MFIpositive - MFInegative) / (2 × SD_negative) |
| % of Background in FSC/SSC | Proportion of events in debris region | Minimize (Target < 5-10% of total) | FSC vs SSC plot, gating |
| Signal-to-Background Ratio | Brightness of positive population relative to negative | > 10:1 for clear resolution | Calculated: MFIpositive / MFInegative |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists critical reagents and materials, as emphasized by standardized protocols, that are essential for preventing and troubleshooting the acquisition issues discussed.
Table 2: Research Reagent Solutions for Acquisition Troubleshooting
| Item | Function / Purpose | Example & Notes |
|---|---|---|
| Cell Strainer | Removes cell aggregates and large debris to prevent fluidic clogs. | 35-70 µm nylon mesh strainers. |
| Viability Dye | Distinguishes live from dead cells; dead cells are a primary source of non-specific background [4]. | Propidium Iodide, Fixable Viability Dyes (e.g., eFluor 506). |
| Standardized Antibody Panels | Pre-optimized combinations ensure fluorochrome compatibility and minimize spillover, reducing background [84]. | EuroFlow or HIPC lyophilized panels (e.g., BD Lyoplate) [30] [84]. |
| Compensation Beads | Generate a clean, cellular background-free population for calculating accurate compensation matrices. | Anti-mouse/rat Ig κ compensation beads. |
| QC Alignment Beads | Verify laser delay, optical alignment, and instrument performance consistency over time. | Spherotech RCP-30-5A or similar 8-peak rainbow beads. |
| Sheath Fluid & Cleaning Solution | Maintains a clean, particle-free fluidics path. Use cleaning solution for de-clogging and routine shutdown. | Manufacturer-recommended sheath fluid and 10% bleach or Contrad 70 solution. |
Addressing flow cytometry acquisition issues requires a systematic approach rooted in standardized protocols. As demonstrated by international consortia, rigorous instrument setup, meticulous sample preparation, and the use of optimized reagent panels are fundamental to preventing clogs, maximizing signal strength, and minimizing background fluorescence [30] [84]. Adherence to these detailed application notes and protocols ensures the generation of high-fidelity data, which is critical for robust immunophenotyping in hematological malignancies research and reliable clinical decision-making.
Preventing Day-to-Day Variability through Standardized Procedures
In the field of clinical flow cytometry, immunophenotyping serves as a cornerstone for the diagnosis, classification, and monitoring of hematological malignancies. However, the utility of this powerful technology is often compromised by significant day-to-day and inter-laboratory variability, which can affect the reproducibility and reliability of results. This variability stems from multiple sources, including differences in sample handling, reagent selection, instrument setup, and data analysis strategies. Standardized procedures have emerged as an essential solution to this challenge, enabling laboratories to generate highly comparable data sets. The implementation of such standards, as demonstrated by large consortia like EuroFlow and the Human ImmunoPhenotyping Consortium (HIPC), transforms individual laboratories into components of a unified diagnostic network, thereby enhancing the power of multi-center clinical trials and routine patient care [34] [85] [86].
Quantifying Variability in Flow Cytometry
Understanding the sources and magnitude of variability is the first step in its control. In flow cytometry, variability can be broadly categorized as technical or biological.
Technical Variability
Technical variability arises from the experimental process itself. A coordinated study by the HIPC consortium revealed that while within-site variability is often low, cross-site variability can be significant. This is particularly true for cell subsets defined by dimly expressed markers or those that are rare in the sample [85]. Manual gating, a traditional analysis method, has been identified as a major source of subjectivity; even experts can produce inter-laboratory coefficients of variation (CV) ranging from 17% to 44% when analyzing the same samples [85] [87].
Biological Variability
Biological variability refers to natural differences between individuals or within an individual over time. Studies on peripheral blood mononuclear cells (PBMC) have shown that while most major cell populations exhibit low intra-individual variability over time, certain subpopulations, such as CD56+ T cells and terminally differentiated CD4+ T cells, demonstrate high inter-individual variability. Furthermore, factors such as age and ethnicity can significantly influence the frequency of several immune cell populations, necessitating their consideration in study design and data analysis [88].
Table 1: Sources and Impact of Variability in Flow Cytometry Immunophenotyping
| Variability Type | Specific Source | Impact on Results |
|---|---|---|
| Technical | Sample handling & staining | Altered antigen expression & cell viability [88] |
| Instrument setup & calibration | Shifts in fluorescence intensity & population resolution [34] [84] | |
| Manual gating strategies | High inter-observer CVs (17-44%), especially for non-discrete subsets [85] [87] | |
| Fluorochrome-antibody combinations | Spillover and compensation artifacts affecting signal purity [84] | |
| Biological | Donor age & ethnicity | Significantly affects frequencies of naïve T cells and other subsets [88] |
| Rare or dimly expressed populations | Higher CVs in identification and quantification [85] |
Standardized Procedures for Minimizing Variability
The implementation of Standard Operating Procedures (SOPs) covering the entire flow cytometry workflow is critical for reducing variability. The success of the EuroFlow and FranceFlow consortia provides a robust framework for these procedures.
Instrument Setup and Calibration
Standardized instrument setup is foundational for comparing data across different days and instruments. The EuroFlow SOP for instrument settings uses a stepwise approach to ensure optimal and reproducible performance [34] [84]. This process involves using stable calibration beads to adjust photomultiplier tube (PMT) voltages to a target value, thereby standardizing the optical path and detector sensitivity across instruments. The FranceFlow group demonstrated that after implementing this SOP, 23 instruments across 19 laboratories could be considered a single, unified laboratory, with CVs for cell subset percentages below 7% [86].
Fluorochrome and Panel Design
The selection of fluorochromes is a critical decision in panel design. The EuroFlow consortium conducted systematic evaluations to define optimal 8-color combinations based on fluorochrome brightness, spillover, and compatibility with common laser and filter configurations [34] [84]. A key principle is to match bright fluorochromes with dimly expressed antigens and dim fluorochromes with highly expressed antigens. Furthermore, the use of lyophilized, pre-configured antibody panels (e.g., BD Lyoplate) minimizes errors in reagent addition and ensures lot-to-lot consistency, significantly improving cross-site reproducibility [85].
Sample Preparation and Staining
Standardizing sample handling from collection to acquisition is vital. Protocols must be meticulously detailed for blood and bone marrow processing, staining, and fixation. The FACSLyse-Bulk protocol is an example of a standardized bulk lysis and staining method that allows for the processing of millions of cells in under 90 minutes. This protocol minimizes cell loss and maintains antigen integrity, which is essential for high-sensitivity applications like Measurable Residual Disease (MRD) detection, where a limit of detection (LOD) below 0.001% is required [89]. Fixing samples after staining stabilizes the fluorescence signal and allows for delayed acquisition without degradation [89].
Data Acquisition and Analysis
Standardization of data analysis is perhaps the most significant hurdle. Two complementary approaches have proven effective:
- Centralized Manual Gating: Having a single, trained operator analyze all data from a multi-center study reduces gating-associated variability [85].
- Automated Gating: Computational algorithms, benchmarked by the FlowCAP consortium, can match the performance of centralized manual analysis with little to no bias. Automated gating provides a robust, objective, and scalable solution for standardizing data interpretation [85].
The integrated workflow below illustrates how these standardized components connect to form a cohesive strategy for preventing variability.
Experimental Protocols for Reproducibility
Protocol: Standardized Bulk Lysis and Staining for High-Sensitivity MRD Detection
This protocol, adapted from the FACSLyse-Bulk method, is designed for processing large volumes of bone marrow or blood to achieve a low limit of detection (<0.001%) for MRD analysis [89].
Key Materials:
- Flow cytometer with at least 8 color channels
- Pre-titrated antibody cocktails for target populations
- Bulk lysing solution (containing formaldehyde for membrane fixation)
- FACS tubes (5 mL polypropylene)
Methodology:
- Cell Staining: Transfer up to 10 million cells into a tube. Centrifuge and resuspend in PBS with 10% FBS. Add the optimized antibody cocktail and incubate for 30 minutes at 4°C, protected from light.
- Bulk Lysis and Fixation: Add a commercial bulk lysing solution directly to the stained cells without washing. Incubate for 10-15 minutes at room temperature. This step simultaneously lyses erythrocytes and fixes the nucleated cells.
- Wash and Resuspend: Centrifuge the sample to remove lysate. Wash the cell pellet once in PBS and resuspend in a precise volume of FACS buffer (PBS with 0.5% FBS and 2mM EDTA).
- Data Acquisition: Acquire data on the flow cytometer. The fixation step allows samples to be stored at 4°C for several hours before acquisition without significant loss of signal or increase in background.
Quality Control:
- Acquire a minimum of 3-5 million nucleated cells to ensure an LOD < 0.001%.
- Use single-stained compensation beads to create a compensation matrix for each run.
- Record the percentage of debris and doublets; well-processed samples typically show <5% debris and <2% doublets [89].
Protocol: Cross-Laboratory Reproducibility Assessment
This protocol outlines the procedure used by the FranceFlow group to assess inter-laboratory reproducibility, a model for internal quality control [86].
Key Materials:
- Aliquots of a stable control sample (e.g., cryopreserved PBMC or lyophilized control cells)
- Standardized lyophilized antibody plates (e.g., HIPC Lyoplate)
- SOPs for instrument setup and sample processing
Methodology:
- Sample Distribution: Distribute identical aliquots of the control sample to all participating laboratories.
- Standardized Staining and Acquisition: All laboratories process, stain, and acquire data from the control sample on the same day using the same pre-defined SOPs and antibody panels.
- Centralized Data Analysis: Collect all FCS files and perform analysis using both centralized manual gating and automated gating algorithms.
- Statistical Analysis: Calculate the frequency and median fluorescence intensity (MFI) for key cell subsets. Determine the inter-laboratory coefficient of variation (CV) for each parameter.
Expected Outcomes: With successful standardization, CVs for cell subset percentages should be below 10%, and CVs for MFI values should be below 30% for most markers, indicating high inter-laboratory reproducibility [86].
Table 2: Key Reagent Solutions for Standardized Immunophenotyping
| Reagent / Material | Function in Standardization | Example & Notes |
|---|---|---|
| Lyophilized Antibody Panels | Pre-configured cocktails eliminate pipetting errors and ensure reagent consistency. | BD Lyoplate (HIPC Consortium); EuroFlow panels [85] [84] |
| Calibration Beads | Used in standardized instrument setup to adjust PMT voltages to a target baseline. | Beckman Coulter Cyto-Trol; UltraComp eBeads [88] [85] |
| Bulk Lysing/Fixation Solution | Simultaneously lyses red blood cells and fixes stained white blood cells, preventing antigen degradation. | Component of the FACSLyse-Bulk protocol [89] |
| Single-Stain Compensation Beads | Generate a consistent and accurate compensation matrix for each experiment, critical for multicolor panels. | UltraComp eBeads [88] |
| Stable Control Cells | Provide a biological reference for inter-assay and inter-laboratory reproducibility testing. | Cryopreserved PBMC; Lyophilized control cells (CytoTrol) [85] [86] |
The imperative for standardized procedures in clinical flow cytometry is clear and supported by robust evidence. The concerted efforts of international consortia have yielded practical, validated SOPs that encompass instrument setup, reagent selection, sample processing, and data analysis. The implementation of these standards, as demonstrated by the FranceFlow group, allows diverse laboratories to function as a single unit, producing highly reproducible data. This harmonization is crucial for advancing the field, enabling reliable disease classification, accurate MRD detection, and the validation of novel biomarkers in multi-center clinical trials. As flow cytometry continues to evolve with increasing panel sizes and complexity, a commitment to standardization will remain the bedrock of data quality and clinical utility.
Ensuring Reproducibility and Analytical Rigor
Analytical method validation provides a means to ensure that flow cytometry data are credible and reproducible, with the extent of validation tailored to the intended use of the data [90]. The "fit-for-purpose" approach recognizes that validation requirements differ significantly between basic research, regulated non-clinical studies, and clinical diagnostics. For immunophenotyping of hematological malignancies, validation ensures accurate lineage assignment, maturational analysis, and detection of aberrant antigen expression that are critical for diagnosis and classification [8] [7].
The complexity of multiparameter analysis techniques and the multitude of available monoclonal antibodies demand standardized protocols to achieve interlaboratory reproducibility [8]. As flow cytometry evolves from research toward clinical applications, the validation framework must progressively incorporate more rigorous controls, documentation, and performance characteristics to ensure reliable results across different laboratory settings.
Experimental Design and Sample Preparation
Sample Information and Handling
A detailed description of sample collection and processing is fundamental to reproducible flow cytometry. The experimental design should specify the number of independent experiments and replicates per experiment [91]. Sample preparation details must include specific methodologies such as proteases for cell isolation, filtration approaches for single-cell suspensions, red blood cell lysis reagents, permeabilization procedures, and fixatives utilized [91]. For hematological malignancies, bone marrow and peripheral blood samples require standardized anticoagulation and processing timelines to maintain cell viability and antigen integrity.
All fluorescent reagents should be documented with complete information including vendors, catalog numbers, and clone designations [91]. This documentation is particularly critical for antibody panels targeting hematological malignancies, where consistent clone performance directly impacts diagnostic accuracy.
Research Reagent Solutions
Table 1: Essential Research Reagents for Flow Cytometry Validation
| Reagent Type | Specific Examples | Function in Validation |
|---|---|---|
| Fluorochrome-conjugated Antibodies | Brilliant Violet 421, Allophycocyanin (APC) Hilite 7 [7] | Lineage assignment and detection of aberrant antigen expression in hematological malignancies |
| Viability Discriminators | Propidium iodide [91] | Exclusion of dead cells to improve analysis accuracy |
| Sample Preparation Reagents | Red blood cell lysis reagents, proteases, fixatives [91] | Standardized sample processing for reproducible results |
| Compensation Controls | Antibody-capture beads [91] | Correction for spectral overlap in multicolor panels |
| Isotype Controls | Species and isotype-matched immunoglobulins [27] | Assessment of nonspecific antibody binding |
| Reference Standards | Stabilized cellular controls [90] | Monitoring instrument and assay performance over time |
Validation Protocols for Different Applications
Three-Tiered Validation Approach
The fit-for-purpose validation framework encompasses three distinct protocols appropriate for different research and clinical contexts [90]:
Limited Validation for Research Settings applies to basic research laboratories focused on discovery. This protocol establishes fundamental performance characteristics including precision (repeatability), sensitivity, and stability under specific experimental conditions. It typically involves intra-assay and inter-assay precision testing with a minimum of three replicates across three days using quality control materials that mimic study samples.
Comprehensive Validation for Regulated Laboratories represents the minimum requirements for laboratories operating under regulatory oversight. This protocol expands on limited validation to include accuracy, specificity, limits of detection, and robustness in addition to precision and sensitivity. Method robustness should be tested by deliberately varying critical parameters (e.g., incubation time, temperature, reagent lots) to establish operational tolerances.
Transfer Validation for Multi-Site Studies ensures consistency when methods are transferred between laboratories. This protocol verifies that the receiving laboratory can reproduce the method performance established by the developing laboratory through statistical comparison of results obtained by both laboratories testing the same panel of samples.
Table 2: Validation Requirements by Application Context
| Performance Characteristic | Research Setting | Regulated Laboratory | Clinical Diagnostic Use |
|---|---|---|---|
| Precision | Required (limited replicates) | Required (extended replicates) | Required (CLIA/CAP guidelines) |
| Accuracy | Not required | Required | Required (method comparison) |
| Sensitivity | Qualitative assessment | Quantitative (limit of detection) | Quantitative with clinical cutoffs |
| Specificity | Basic characterization | Comprehensive assessment | Clinical specificity validation |
| Robustness | Limited testing | Formal testing | Extensive testing |
| Stability | Sample stability only | Reagent and sample stability | Full stability documentation |
Data Acquisition Standards
Proper data acquisition parameters must be documented and standardized to ensure reproducible results. The flow cytometer instrument should be described including manufacturer, model, and software version [91]. Laser lines and optical emission filters used for corresponding fluorescent reagents must be documented [91]. As the number of fluorochromes increases, proper compensation becomes critical to correct for spectral overlap and ensure that each channel detects only fluorescence from its designated fluorophore [91].
For multicolor panels used in hematological malignancies, the number of events collected must be sufficient for the precision required, with rare cell populations necessitating larger event counts [91]. The compensation approach should be specified, including whether antibodies, cells, or beads were used for compensation controls [91].
Data Acquisition Workflow for Flow Cytometry Validation
Data Analysis and Interpretation Standards
Gating Strategies and Controls
Appropriate gating strategies are essential for accurate data interpretation in hematological malignancy immunophenotyping. The gating scheme should outline all light scatter gates, live-dead gates, doublet gates, and fluorescence-detecting gates [91]. Methods to define gates might include unstained controls, biological controls, isotype controls, fluorescence minus one (FMO) controls, or internal negative populations within the sample [91] [27].
For elimination of dead cells and doublets, side scatter and forward scatter properties are utilized to distinguish these from viable single cells [27]. When identifying rare cell populations in hematological malignancies, such as minimal residual disease, proper gating becomes particularly critical and requires rigorous validation of gating strategies.
Data Presentation Guidelines
Flow cytometry data should be presented to allow accurate interpretation of results. Both axes of plots should be labeled with the antibody and fluorochrome used rather than instrument-specific parameter descriptions [91]. Percentages should be listed in gates, and plots should avoid piling up events on the axis [91]. For bivariate displays, contours or density dot plots are preferred over single dot displays as they better represent population distributions [91].
When calculating percentages from gated populations, researchers must consider whether to report percentages relative to the immediate parent gate or the total population [27]. For clinical applications, this distinction can have significant diagnostic implications.
Flow Cytometry Data Analysis Workflow
Advanced Applications in Hematological Malignancies
Multicolor Panel Design
Fluorochrome selection represents a critical step in designing multicolor antibody panels for hematological malignancies. Several criteria guide fluorochrome selection: fluorescence profiles (excitation and emission), relative brightness, fluorescence overlap, fluorochrome stability, and reproducible conjugation to antibodies [7]. The EuroFlow consortium has demonstrated systematic approaches for evaluating compatible fluorochromes, identifying optimal combinations with higher fluorescence intensity and/or resolution with limited fluorescence overlap into neighbor channels [7].
For clinical applications in hematological malignancies, standardized 8-, 10- and 12-color fluorochrome combinations provide a framework for initial antibody panel design [7]. These standardized panels ensure consistent immunophenotyping across laboratories while allowing sufficient flexibility for disease-specific refinements.
Transition to Clinical Applications
The transition from research flow cytometry to clinical applications requires additional validation considerations. Clinical laboratories must establish rigorous quality control procedures, standardized staining and acquisition protocols, and validated analysis approaches performed by trained technical experts [92]. Board-certified hematopathologists typically review clinical flow cytometry data, integrating immunophenotypic findings with morphological and molecular data for comprehensive diagnostic interpretation [92].
For drug development applications, flow cytometry assays may require validation under Good Laboratory Practice (GLP) regulations or CLIA certification for clinical trial support [92] [90]. The validation extent should reflect the application's criticality, with diagnostic applications requiring the most rigorous validation and exploratory research applications requiring more limited validation.
Fit-for-purpose method validation provides a structured framework for ensuring flow cytometry data quality across the spectrum from basic research to clinical diagnostics. By implementing appropriate validation protocols based on the intended data use, researchers and clinicians can generate reproducible, reliable immunophenotyping data for hematological malignancies. The standardized approaches outlined in this protocol support quality assurance and facilitate the transition of innovative flow cytometry applications from research discoveries to clinical practice, ultimately improving the diagnosis and monitoring of hematological malignancies.
In the diagnosis and monitoring of hematological malignancies, flow cytometric immunophenotyping is an indispensable tool [62] [2]. Its utility hinges on the performance of antibody reagents, making rigorous antibody validation a cornerstone of reproducible and reliable science [93] [94]. The "reproducibility crisis," fueled in part by poorly characterized antibodies, underscores the critical need for thorough validation protocols [93]. For clinical researchers and drug development professionals, establishing robust validation procedures is not merely good practice—it is essential for accurate diagnosis, prognostic stratification, and therapeutic monitoring [17]. This application note details a comprehensive framework for validating antibodies in the context of hematological malignancies, focusing on the core pillars of specificity, sensitivity, and lot-to-lot reproducibility.
The Critical Importance of Antibody Validation
Antibodies are fundamental reagents for characterizing everything from basic cellular subsets to complex aberrant phenotypes in leukemia and lymphoma [2]. However, without proper validation, these reagents can lead science down incorrect paths, costing valuable time and resources, and potentially impacting patient outcomes [93]. Evidence suggests that a significant proportion of commercial antibodies fail validation tests; one study found only half of over 5,000 antibodies passed specificity standards in Western blotting and immunohistochemistry [93]. Another alarming study showed that none of 49 antibodies against G protein-coupled receptor subtypes were specific for a single subtype [93].
Validation is particularly crucial for flow cytometry due to its multiparametric nature and the increasing complexity of data analysis [94]. As the field advances toward higher-parameter instrumentation and automated data analysis, the demand for exceptionally high-quality antibody performance has never been greater [94] [2]. Proper validation ensures that the data generated accurately reflects the biology of the hematological malignancy being studied, enabling confident clinical decision-making and robust research outcomes.
Pillars of Antibody Validation: Specificity, Sensitivity, and Reproducibility
A comprehensive antibody validation strategy must address three fundamental properties: specificity, sensitivity, and reproducibility. These properties form the foundation of reliable immunophenotyping data in hematological malignancies.
Specificity: Ensuring Target Recognition Accuracy
Specificity refers to an antibody's ability to discriminate its target epitope from other epitopes and bind with high affinity [93]. It is the most fundamental characteristic requiring validation.
- Genetic Strategies: Knockout (using CRISPR/Cas9) or knockdown (using siRNA) models provide compelling evidence of specificity by demonstrating the absence of signal in cells lacking the target protein [93] [95]. This is especially useful for ubiquitously expressed proteins where negative control cell types are not readily available [93].
- Orthogonal Methods: Comparing flow cytometry results with data from complementary techniques, such as Western blotting (to confirm target size) or immunohistochemistry/immunofluorescence (to confirm cellular localization), verifies specificity through non-antibody-dependent methods [93] [95].
- Biological Systems: Using cell lines or tissues with well-established positive and negative expression profiles for the target provides a biological context for specificity confirmation [95]. Treatments that modulate protein expression (e.g., cytokines, inhibitors) can also serve this purpose [95].
Sensitivity: Determining Detection Limits
Sensitivity relates to the antibody's capacity for target detection in a given experimental setting, effectively defining the lowest expression level that can be reliably detected [93].
- Titration: A critical step for optimizing sensitivity is antibody titration to determine the optimal signal-to-noise ratio [72] [96]. Using either too much or too little antibody can reduce sensitivity, either through increased background or insufficient signal.
- Expression Range Testing: Validating antibody performance across cell lines or patient samples with known high, medium, low, and negative expression levels ensures the antibody is sensitive enough to detect biologically relevant expression levels [95].
- Comparison to Reference Standards: In clinical settings, sensitivity can be quantified against established diagnostic standards or reference methods, which is particularly important for detecting minimal residual disease (MRD) [2].
Lot-to-Lot Reproducibility: Maintaining Consistency
Reproducibility encompasses consistent antibody performance across different lots and multiple experiment iterations [93]. Lot-to-lot variability is a significant contributor to the reproducibility crisis in biomedical research.
- Recombinant Antibody Technology: A key strategy to ensure lot-to-lot reproducibility is switching from traditional hybridoma-based antibodies to recombinant antibodies [93]. Recombinant antibodies are derived from a defined set of genes and produced through a highly standardized process, resulting in consistent structure and performance [93].
- Standardized Validation Panels: Implementing standardized panels and protocols across laboratories, as demonstrated by the FranceFlow and EuroFlow consortia, significantly improves inter-laboratory reproducibility [86]. The FranceFlow group showed that after standardization, coefficients of variation (CVs) across 19 centers were below 7% for cell subset percentages and under 30% for median fluorescence intensities [86].
- Rigorous Quality Control: Manufacturers must implement stringent quality control measures, including side-by-side testing of new lots against established reference lots across multiple applications and cell types [93].
Table 1: Key Validation Strategies and Their Applications
| Validation Strategy | Methodology | Primary Validation Aspect | Application in Hematologic Malignancies |
|---|---|---|---|
| Genetic Knockout/Knockdown | CRISPR/Cas9 or siRNA to eliminate target protein | Specificity | Essential for validating antibodies against new targets or phosphorylated epitopes |
| Orthogonal Methods | Comparison with Western blot, IHC, mass spectrometry | Specificity | Confirms cellular localization and target size; critical for diagnostic accuracy |
| Titration | Testing serial antibody dilutions | Sensitivity | Optimizes signal-to-noise ratio for both high and low-abundance antigens |
| Recombinant Technology | Use of genetically defined antibody sequences | Reproducibility | Ensures consistent performance across lots and manufacturing scales |
| Standardized Panels | Multi-center consensus panels and protocols | Reproducibility | Enables comparable results across clinical sites and longitudinal studies |
Experimental Protocols for Antibody Validation
Protocol 1: Specificity Confirmation via CRISPR/Cas9 Knockout
This protocol provides a robust method for confirming antibody specificity by demonstrating loss of signal in target-deficient cells.
Materials:
- Wild-type cell line relevant to the hematologic malignancy (e.g., REH for B-ALL, Jurkat for T-ALL)
- Isogenic cell line with CRISPR/Cas9-mediated knockout of the target gene
- Antibody of interest with appropriate fluorochrome conjugate
- Isotype control antibody
- Flow cytometry staining buffer (PBS with 1-5% FBS)
- Fc receptor blocking reagent (for primary cells)
- 12x75mm flow cytometry tubes or 96-well plates
- Flow cytometer with appropriate laser and filter configuration
Procedure:
- Harvest and Count Cells: Harvest logarithmically growing cells and determine viability and cell count. Use only samples with >90% viability.
- Fc Receptor Blocking: For primary samples or cell lines expressing Fc receptors, incubate cells with Fc blocking reagent for 10-15 minutes on ice [72].
- Antibody Staining: Aliquot approximately 1-5x10^5 cells per tube. Add titrated antibody concentration to both wild-type and knockout cell samples. Include isotype control tubes for both cell types. Incubate for 20-30 minutes in the dark on ice.
- Washing: Add 2-3mL of staining buffer to each tube, centrifuge at 300-500xg for 5 minutes, and decant supernatant completely.
- Resuspension: Resuspend cell pellets in 200-500µL of staining buffer for analysis.
- Data Acquisition: Acquire data on flow cytometer using consistent instrument settings between wild-type and knockout samples.
- Analysis: Compare fluorescence intensity between wild-type and knockout cells. A specific antibody will show significantly reduced or absent staining in the knockout cells compared to wild-type controls.
Protocol 2: Antibody Titration for Sensitivity Optimization
This protocol establishes the optimal antibody concentration that provides the best signal-to-noise ratio, maximizing sensitivity while minimizing non-specific binding.
Materials:
- Cell sample with known positive expression of the target antigen
- Cell sample with known negative expression (biological negative)
- Antibody of interest in unconjugated or conjugated form
- Serial dilutions of the antibody (e.g., 0.125µg, 0.25µg, 0.5µg, 1µg, 2µg per test)
- Flow cytometry staining buffer
- Flow cytometer
Procedure:
- Prepare Antibody Dilutions: Create a series of antibody dilutions in staining buffer covering a range above and below the manufacturer's recommended concentration.
- Cell Preparation: Aliquot 1-5x10^5 positive and negative cells per tube for each antibody dilution to be tested.
- Staining: Add each antibody dilution to both positive and negative cell samples. Incubate for 20-30 minutes in the dark on ice.
- Washing and Resuspension: Wash cells once with 2-3mL staining buffer, centrifuge, decant supernatant, and resuspend in fixed volume for analysis.
- Data Acquisition: Acquire all samples using identical flow cytometer settings.
- Analysis: Determine the median fluorescence intensity (MFI) for both positive and negative populations at each concentration. Calculate the signal-to-noise ratio (Staining Index) using the formula: (MFIpositive - MFInegative) / (2 × SD_negative). The optimal concentration provides the highest Staining Index.
Protocol 3: Lot-to-Lot Comparison
This protocol validates consistency between antibody lots to ensure experimental reproducibility over time.
Materials:
- Current validated antibody lot (Reference)
- New antibody lot (Test)
- Multiple cell types with varying expression levels of the target (negative, low, medium, high expressors)
- Flow cytometry staining buffer
- Flow cytometer with standardized settings
Procedure:
- Panel Design: Include both antibody lots in the same experiment to eliminate day-to-day instrument variability.
- Cell Staining: Stain replicates of each cell type with both the reference and test lots at the optimized concentration. Use identical staining conditions for both lots.
- Data Acquisition: Acquire data for all samples in a single session using consistent cytometer settings.
- Analysis: Compare the median fluorescence intensity (MFI) and staining pattern between the reference and test lots across all cell types. Calculate the percentage difference in MFI for each population. Consistent lots should show <20% variation in MFI values [86].
- Documentation: Maintain thorough records of lot comparisons as part of quality assurance protocols.
Research Reagent Solutions for Hematological Malignancies
The appropriate selection of reagents is fundamental to successful immunophenotyping in hematological malignancies. The following table details essential components for antibody-based flow cytometry assays.
Table 2: Essential Research Reagents for Flow Cytometric Analysis of Hematological Malignancies
| Reagent Category | Specific Examples | Function and Importance in Validation |
|---|---|---|
| Validated Antibody Panels | EuroFlow AML/Orientation tubes, B-cell chronic lymphoproliferative disorder panels | Standardized pre-validated panels ensure consistent identification of aberrant populations and improve inter-laboratory reproducibility [2] [86] |
| Recombinant Antibodies | Miltenyi Biotec recombinant portfolio (>1300 clones) | Defined genetic sequence enables consistent production, minimal batch-to-batch variation, and reliable long-term studies [93] |
| Viability Dyes | 7-AAD, Propidium Iodide, DRAQ7 | Distinguish live from dead cells to exclude artifacts from non-specific antibody binding and autofluorescence common in apoptotic malignant cells [72] |
| Fc Receptor Blocking Reagents | Human FcR Blocking Reagent, purified human IgG | Reduce non-specific antibody binding to Fc receptor-expressing cells (e.g., monocytes, macrophages), decreasing background and improving signal clarity [72] |
| Compensation Beads | Anti-antibody coated compensation beads | Create single-color controls for accurate spectral overlap compensation in multicolor panels, essential for data accuracy in high-parameter flow [72] |
| Cell Preparation Reagents | RBC Lysis Buffer, DNAse I | Prepare single-cell suspensions free of debris and clumps from peripheral blood, bone marrow, and tissue samples [2] |
| Standardized Controls | Isotype controls, FMO controls, biological negative/positive controls | Establish background fluorescence, define positive populations, and validate staining specificity in complex multicolor panels [72] |
Standardized Marker Panels for Hematological Malignancies
Standardized antibody panels are crucial for consistent diagnosis and classification of hematological malignancies. The following table summarizes key markers recommended by international consensus groups based on the WHO classification and Bethesda guidelines [2].
Table 3: Essential Markers for Immunophenotyping of Hematological Malignancies
| Disease Category | Key Diagnostic Markers | Additional/Conditional Markers |
|---|---|---|
| Acute Myeloid Leukemia (AML) | CD13, CD14, CD33, CD34, CD45, CD64, CD117, HLA-DR, MPO [2] | CD11b, CD15, CD38, CD123 |
| B-Cell Acute Lymphoblastic Leukemia (B-ALL) | CD10, CD19, CD20, CD22, CD34, CD45, TdT [2] | CD79a, CD13, CD33, CD15, CD81, CD58 |
| T-Cell Acute Lymphoblastic Leukemia (T-ALL) | CD1a, CD2, CD3, CD5, CD7, CD45, TdT [2] | CD4, CD8, CD34, CD99, TCR Vβ repertoire |
| Chronic Lymphocytic Leukemia (CLL/SLL) | CD5, CD19, CD20, CD23, CD38, CD43, CD79b, CD200 [2] | FMC7, ROR1, ZAP-70, surface immunoglobulin light chain restriction |
| B-Cell Lymphoma | CD19, CD20, CD22, CD79a [2] | CD5, CD10, CD30, BCL2, Cyclin D1 (depending on subtype) |
| T-Cell Lymphoma | CD2, CD3, CD4, CD5, CD7, CD8 [2] | CD25, CD26, CD30, CD45RA, CD45RO, TCR Vβ repertoire, TRBC1 |
Visualization of Validation Workflows
Antibody Validation Strategy Diagram
Experimental Controls Workflow
Comprehensive antibody validation is non-negotiable for generating reliable, reproducible data in the flow cytometric analysis of hematological malignancies. By implementing the structured approaches outlined in this application note—rigorously addressing specificity, sensitivity, and lot-to-lot reproducibility—researchers and clinical laboratories can significantly enhance the quality of their immunophenotyping work. The standardization efforts led by consortia like FranceFlow and EuroFlow demonstrate that reproducible multicolor flow cytometry across multiple centers is achievable through standardized instrument settings, reagent panels, and analytical protocols [86]. As the field progresses toward increasingly complex multiparameter assays and advanced applications like minimal residual disease monitoring, commitment to these validation principles will ensure that antibody-based data continues to provide clinically actionable insights for patient diagnosis, classification, and treatment monitoring.
Validation Protocols for Moderate-Risk Laboratory-Developed Tests
A Laboratory Developed Test (LDT) is defined as an in vitro diagnostic (IVD) product intended for clinical use that is designed, manufactured, and used within a single Clinical Laboratory Improvement Amendments (CLIA)-certified laboratory that meets requirements to perform high-complexity testing [97]. The regulatory framework for LDTs is undergoing significant transformation, with the U.S. Food and Drug Administration (FDA) issuing a Final Rule to phase out its general enforcement discretion approach [97]. This evolving landscape necessitates that laboratories developing moderate-risk LDTs for immunophenotyping hematological malignancies establish robust, documented validation protocols that meet emerging regulatory standards.
Moderate-risk LDTs typically include IVDs that require premarket submission via 510(k) clearance [97]. For flow cytometry-based assays in hematological malignancies, this encompasses the majority of quantitative immunophenotyping tests used for diagnosis, classification, and minimal residual disease (MRD) monitoring. The FDA is implementing a four-year, five-stage transition period for LDT enforcement discretion, with Stage 5 (covering moderate and low-risk IVDs) scheduled to take effect on May 6, 2028 [97]. This application note provides detailed validation protocols aligned with these forthcoming requirements, specifically contextualized for flow cytometry assays in hematological malignancy research and clinical applications.
Core Validation Parameters for Moderate-Risk LDTs
Validation of moderate-risk LDTs requires demonstration of both analytical and clinical validity. The "fit-for-purpose" approach to validation ensures that the level of validation is appropriate for the assay's intended use, balancing regulatory requirements with practical considerations [98]. For flow cytometry assays in hematological malignancies, key validation parameters with their corresponding acceptance criteria and industry standards are summarized in Table 1 below.
Table 1: Core Validation Parameters for Moderate-Risk Flow Cytometry LDTs
| Validation Parameter | Acceptance Criteria | Recommended Procedure | Applicable Standards |
|---|---|---|---|
| Accuracy | Demonstrated by method comparison or reference materials | Comparison to FDA-cleared test or clinical samples with known status | CLSI H62 [98] [99] |
| Precision (Intra-assay) | ≤10-25% CV for common populations; ≤30-35% CV for rare populations | Repeated testing of same sample (n≥20) over multiple runs (n≥3) | CLSI H62 [99] |
| Precision (Inter-assay) | ≤15-30% CV for common populations | Testing of same sample over multiple days (n≥5) with different operators | CLSI H62 [98] |
| Sensitivity (Limit of Detection) | Established for rare cell populations (e.g., MRD at 0.01%) | Serial dilutions of positive cells in negative matrix | ICCS Guidelines [99] |
| Specificity | ≤5% interference from expected sources | Testing with potentially interfering substances (e.g., therapeutic antibodies) | CLSI H62 [98] |
| Reportable Range | Verified across clinically relevant concentrations | Linearity studies with samples spanning expected values | CLSI EP06 [99] |
| Reference Intervals | Established for each reported cell population | Testing of 20-40 healthy donor samples appropriate for age | CLSI EP28-A3C [99] |
| Sample Stability | ≤20% difference from baseline values | Testing after defined storage intervals and conditions | ICSH/ICCS Guidelines [99] |
Experimental Protocol: Validation of a B-Cell Depletion Monitoring Assay
Background and Intended Use
This protocol outlines the validation of a moderate-risk LDT for monitoring B-cell depletion therapy in patients with B-cell hematological malignancies or autoimmune conditions. The assay utilizes multiparameter flow cytometry to quantify absolute CD19+ B-cell counts in peripheral blood, providing critical pharmacodynamic data for anti-CD20 therapeutics such as rituximab, obinutuzumab, and ofatumumab [98]. CD19 is selected as the primary biomarker rather than CD20 due to therapeutic antibody interference, as CD19 covers the entire spectrum of B-cell genesis and maturation without being occupied by administered monoclonal antibodies [98].
Required Materials and Reagents
Table 2: Research Reagent Solutions for B-Cell Depletion Assay
| Item | Function | Specification | Example Products |
|---|---|---|---|
| TBNK Reagent | Multiparameter immunophenotyping | 6-7 color antibody panel including CD45, CD3, CD19, CD4, CD8, CD16, CD56 | BD Multitest 6-Color TBNK [98] |
| Trucount Tubes | Absolute cell counting | Lyophilized bead pellet with known count | BD Trucount Tubes [98] |
| Blood Collection Tubes | Sample preservation | K3EDTA with cell preservation reagents | Cell-Stabilizing Tubes (e.g., Streck) [98] |
| Quality Control Material | Process control | Stabilized human leukocytes and erythrocytes | BD Multi-Check Control, CD-Chex Plus [98] |
| Calibration Beads | Instrument standardization | Fluorescent beads for setup and tracking | CS&T Beads [98] |
| Viability Dye | Dead cell exclusion | Membrane impermeant dye | Propidium iodide, LIVE/DEAD Fixable dyes [91] [100] |
Sample Preparation and Staining Procedure
Sample Collection: Collect peripheral blood via venipuncture into cell-stabilizing blood collection tubes containing K3EDTA and cell preservation reagents. Maintain samples at room temperature and process within 48 hours of collection [98].
Staining Protocol:
- Gently mix blood samples by inversion 8-10 times
- Pipette 50 μL of well-mixed whole blood into a Trucount tube
- Add 20 μL of TBNK reagent cocktail directly to the blood in the Trucount tube
- Mix immediately by gentle vortexing (5-10 seconds)
- Incubate for 15 minutes in the dark at room temperature (20-25°C)
- Add 450 μL of 1X BD FACS Lysing Solution
- Mix by gentle vortexing and incubate for 15 minutes in the dark at room temperature
- Store stained samples at 2-8°C and acquire within 6 hours
Instrument Setup and Quality Control:
- Perform daily instrument quality control using CS&T beads
- Verify fluorescence sensitivity and optical alignment
- Create Levey-Jennings charts to monitor instrument performance over time [98]
- Run quality control material (BD Multi-Check Control) with each analytical run
Data Acquisition and Gating Strategy
Data acquisition should be performed using standardized instrument settings with a stopping criterion of 2,500 collected lymphocytes or 10,000 total events [98]. The gating strategy follows a hierarchical approach as illustrated in the workflow diagram below:
Diagram 1: Hierarchical Gating Strategy for B-Cell Enumeration
Validation Experimental Design
The following experiments should be conducted to establish assay performance claims:
Precision Study:
- Test 3 levels of controls (low, normal, high B-cell counts) with 5 replicates each
- Repeat testing over 5 separate days with 2 different operators
- Calculate within-run, between-run, and total precision (%CV)
- Acceptance Criteria: Intra-assay CV ≤15%, Inter-assay CV ≤20%
Accuracy Assessment:
- Perform method comparison with a validated predicate method (if available)
- Test 20 clinical samples spanning the reportable range
- Use Deming regression analysis to evaluate correlation
- Acceptance Criteria: Slope 0.90-1.10, R² ≥0.95
Linearity and Reportable Range:
- Prepare serial dilutions of high B-cell sample in low B-cell matrix
- Test 5 levels across the anticipated measuring range
- Assess linearity using polynomial regression
- Acceptance Criteria: %Deviation from linearity ≤15%
Sample Stability:
- Test fresh samples and samples stored at room temperature and 2-8°C
- Evaluate stability at 0, 24, 48, and 72 hours
- Acceptance Criteria: ≤20% difference from baseline value [99]
Reference Interval Establishment:
- Test samples from at least 20 healthy donors
- Establish non-parametric 95% reference intervals
- Acceptance Criteria: Statistically valid reference range established
Regulatory Considerations and Documentation
Quality Systems and Compliance
Laboratories developing moderate-risk LDTs must implement Quality System (QS) requirements per FDA regulations, including design controls, purchasing controls, acceptance activities, and corrective and preventive actions [97]. Documentation should demonstrate adherence to these requirements through:
- Standard Operating Procedures (SOPs) for all testing processes
- Comprehensive validation reports with raw data and statistical analysis
- Operator training and qualification records
- Instrument maintenance and calibration logs
- Quality control monitoring with defined corrective actions
The validation should follow a "fit-for-purpose" approach, where the extent of validation is determined by the assay's intended use and clinical application [98]. For moderate-risk LDTs, this typically requires more extensive validation than research-use-only assays but may not require the full validation expected for high-risk tests.
Modification of Existing Tests
Laboratories should note that significant modifications to "grandfathered" LDTs or FDA-cleared tests generally require submission of a new premarket application. The FDA considers the following changes as significant modifications [97]:
- Changes to the indications for use
- Alterations to the operating principle of the IVD
- Inclusion of significantly different technology (e.g., addition of AI/ML algorithms)
- Changes that adversely affect performance or safety specifications
For modified FDA-cleared tests, laboratories must follow design controls and quality system requirements. If modifications render the test no longer substantially equivalent to the original, a Premarket Approval (PMA) application may be required [97].
Analytical Framework for Flow Cytometry Data Interpretation
Quantitative Flow Cytometry Applications
Quantitative flow cytometry (QFCM) enables precise measurement of absolute molecule counts on individual cells, providing critical data for hematological malignancy assessment. Key applications in hematological malignancies include:
- CD34+ hematopoietic stem cell enumeration for transplant dosing determination [101]
- Minimal Residual Disease (MRD) detection in acute lymphocytic leukemia through quantification of TdT, CD10, and CD19 molecules per cell [101]
- B-cell chronic lymphoproliferative disorder characterization via quantitative profiling of CD19, CD20, CD22, CD23, CD79b, and CD5 [101]
- T-cell antigen quantification for diagnosis and prognostic evaluation in leukemias [101]
QFCM utilizes fluorescence calibration standards and quantification bead kits to convert fluorescence intensity into standardized units such as Molecules of Equivalent Soluble Fluorochrome (MESF) or Antigen Binding Capacity (ABC) [101]. This standardization enables reproducible measurements across experiments and institutions, which is essential for longitudinal disease monitoring and multicenter clinical trials.
Gating Strategy and Data Visualization
Proper gating strategies are fundamental to accurate flow cytometry data interpretation. The following diagram illustrates a comprehensive gating approach for immunophenotyping in hematological malignancies:
Diagram 2: Comprehensive Gating Strategy for Hematological Malignancies
Data should be presented using appropriate visualization methods, including histogram overlays for marker expression comparisons and bivariate plots for population identification [28]. For publication, include all gating strategies, compensation controls, and population percentages to ensure reproducibility and transparency [91].
Validation of moderate-risk LDTs for flow cytometry-based immunophenotyping of hematological malignancies requires a systematic, documented approach that addresses all relevant analytical performance characteristics. As regulatory oversight of LDTs continues to evolve, laboratories must implement robust validation protocols that demonstrate both analytical and clinical validity. The protocols outlined in this application note provide a framework for developing compliant, fit-for-purpose assays that generate reliable results for clinical decision-making while meeting emerging regulatory expectations.
The reliable transfer of flow cytometric methods for the immunophenotyping of hematological malignancies between facilities is a critical yet complex challenge in both research and clinical diagnostics. The complexity of multiparameter analysis techniques and the multitude of available monoclonal antibodies demand a standardization of protocols to achieve inter-laboratory reproducibility [8]. Consistent results are vital for multi-center clinical trials, diagnostic standardization, and the validation of new therapeutic targets, ensuring that data generated in one laboratory can be confidently compared or combined with data from another. This application note outlines a standardized framework and detailed protocols to ensure the robust transfer of flow cytometry methods, thereby enhancing the reliability of data in hematological malignancy research.
Core Principles of Method Transfer
Successful method transfer rests on three foundational pillars: comprehensive documentation, harmonized instrumentation, and standardized reagent management. Without strict adherence to these principles, technical variations can compromise data integrity and lead to irreproducible findings.
Comprehensive Documentation: A successful transfer begins with a detailed Transfer Protocol that explicitly defines all critical procedures and acceptance criteria for the method's performance. This serves as the primary reference for all participating facilities [91]. Furthermore, a Sample and Data Acquisition Worksheet should be utilized to meticulously record sample preparation details, instrument configuration, and laser and filter specifications for every experiment, ensuring full traceability [91] [102].
Harmonized Instrumentation: Inconsistent instrument settings are a major source of variability. Key optical specifications, including laser lines and optical emission filters, must be documented and matched as closely as possible between facilities [91] [102]. Regular calibration using standardized particles or fluorescent beads is mandatory to ensure instruments are performing optimally and consistently over time [103].
Standardized Reagent Management: Reagent variability must be minimized. All antibodies and fluorescent reagents should be sourced from the same vendors and include catalog numbers and clone designations in the documentation [91]. A critical pre-transfer step is antibody titration to determine the optimal staining concentration for each reagent, which maximizes the signal-to-noise ratio and ensures consistent staining intensity across different laboratories [104].
Pre-Transfer Planning and Documentation
A meticulously planned pre-transfer phase is the most critical determinant of a successful method transfer. This stage involves aligning all stakeholders on the objectives, deliverables, and success metrics of the transfer process.
Defining Transfer Scope and Success Criteria
The transferring facility (the "sending lab") and the receiving facility (the "receiving lab") must jointly establish a Quality Agreement. This document delineates responsibilities, timelines, and the specific performance parameters that will be used to judge the success of the transfer. The success criteria should be based on quantitative, measurable outcomes from the validation experiments.
Table 1: Key Performance Indicators for Method Transfer Validation
| Parameter | Target Acceptance Criterion | Measurement Method |
|---|---|---|
| Cell Population Frequency | Coefficient of Variation (CV) < 15% between labs | Comparison of percentage of target cells (e.g., leukemic blasts) in defined gates |
| Median Fluorescence Intensity (MFI) | CV < 20% for key markers | Comparison of MFI values for consistently expressed antigens |
| Detection Sensitivity | Consistent identification of rare populations down to 0.1% | Analysis of spiked-in or known rare cell subsets |
| Intra-assay Precision | CV < 10% for replicate samples within the same lab | Running multiple replicates of the same sample |
The Method Transfer Package
The sending lab must prepare a comprehensive Method Transfer Package for the receiving lab. This package is the source of truth for the method and should contain, at a minimum, the protocol for sample preparation, panel information, and data analysis specifications [8] [91].
- Sample Preparation Protocol: Detailed procedures for tissue dissociation, red blood cell lysis, viability dye staining, cell counting, and fixation/permeabilization if required.
- Staining Protocol: A step-by-step guide including antibody staining volumes and incubation times, Fc receptor blocking procedures, wash steps, and buffer formulations.
- Instrument Setup SOP: A standardized operating procedure for starting up the cytometer, running quality control beads, and setting up the acquisition template with predefined detector voltages.
- Compensation Setup: Instructions for preparing single-stain controls and setting compensation matrices [104] [103].
- Gating Strategy: A detailed, step-by-step graphical representation of the gating hierarchy, from lymphocytes/debris exclusion through to the final target populations [91] [105].
Experimental Protocols for Transfer Validation
The following core protocols form the basis for experimental validation that the transferred method is performing acceptably in the receiving laboratory.
Protocol: Standardized Sample Preparation and Staining
This protocol is designed for the immunophenotyping of human peripheral blood mononuclear cells (PBMCs) in the context of hematological malignancies.
Materials:
- Biological Sample: Human PBMCs from healthy donors or patients with hematological malignancies.
- Staining Buffer: PBS containing 1-2% fetal bovine serum (FBS) or BSA.
- Fc Receptor Blocking Reagent: Human IgG or commercial Fc block.
- Viability Dye: e.g., Propidium Iodide (PI), 7-AAD.
- Antibody Panel: Titrated, fluorochrome-conjugated antibodies against target antigens (e.g., CD45, CD3, CD19, CD34).
- Compensation Beads: Antibody capture beads for generating single-stain controls.
- Flow Cytometer: Calibrated according to manufacturer's specifications.
Procedure:
- Sample Preparation: Resuspend frozen PBMCs or use fresh cells. Count cells and ensure viability is >90%. Centrifuge at 300-500 x g for 5 minutes and resuspend in staining buffer to a concentration of 1 x 10^7 cells/mL [103].
- Fc Receptor Blocking: Aliquot 100 µL of cell suspension (1 x 10^6 cells) into a FACS tube. Add Fc receptor blocking reagent and incubate for 10-15 minutes on ice.
- Surface Staining: Add the pre-mixed antibody cocktail directly to the tube. Vortex gently and incubate for 30 minutes in the dark at 4°C.
- Washing: Add 2 mL of staining buffer to the tube, centrifuge at 500 x g for 5 minutes, and carefully decant the supernatant.
- Viability Staining: Resuspend the cell pellet in staining buffer containing the viability dye (e.g., PI) and incubate for 5-10 minutes in the dark at 4°C.
- Fixation (Optional): If required, resuspend cells in a suitable fixative (e.g., 1-4% paraformaldehyde).
- Data Acquisition: Resuspend cells in an appropriate volume of buffer (e.g., 300-500 µL) and acquire data on the flow cytometer within a defined timeframe (e.g., 4 hours if unfixed).
Protocol: Establishing and Applying Controls
Appropriate controls are non-negotiable for validating assay performance and correctly interpreting data during method transfer [104] [103].
Table 2: Essential Flow Cytometry Controls for Method Transfer
| Control Type | Purpose | Preparation |
|---|---|---|
| Unstained Cells | Determines cellular autofluorescence [103]. | Cells processed without any fluorescent reagents. |
| Single-Stain Controls | Required for calculating compensation (conventional) or creating a spectral unmixing matrix (spectral) [104] [103]. | Compensation beads or cells stained with a single antibody conjugate. |
| Fluorescence Minus One (FMO) | Determines background fluorescence and guides accurate gate placement for markers with low expression or continuous expression patterns [104] [105] [103]. | Cells stained with all antibodies in the panel except one. |
| Isotype Controls | Assesses non-specific antibody binding (use with caution and in conjunction with FMO) [104] [103]. | Cells stained with an irrelevant antibody matched to the specific antibody's isotype and fluorophore. |
| Biological Control (Positive/Negative) | Validates the entire experimental process. | A sample with a known phenotype (e.g., healthy donor PBMCs) or a reference stabilized cell type. |
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their critical functions in ensuring a robust and transferable flow cytometry assay.
Table 3: Essential Reagents for Flow Cytometry Method Transfer
| Reagent / Material | Function | Criticality for Transfer |
|---|---|---|
| Pre-Titrated Antibody Panels | Ensures optimal signal-to-noise ratio and consistent staining intensity between labs. | High |
| Standardized Buffer Systems | Minimizes non-specific binding and variation caused by differences in buffer composition. | High |
| Antibody Capture Beads | Provides a consistent and homogeneous material for generating high-quality single-stain controls for compensation. | High |
| Viability Dyes (e.g., PI, 7-AAD) | Allows for the exclusion of dead cells, which exhibit increased autofluorescence and non-specific antibody binding. | High |
| Fc Receptor Blocking Reagent | Reduces non-specific staining through interactions with Fc receptors expressed on many immune cells. | Medium |
| Reference Standard Cells (e.g., PBMCs) | Provides a biologically relevant sample to track assay performance and stability over time and between locations. | High |
| Instrument Calibration Beads | Verifies that the flow cytometer's lasers, detectors, and fluidics are performing within specified parameters. | High |
Data Acquisition, Analysis, and Reporting Standards
Consistency in how data is collected and interpreted is the final, crucial step in the transfer process.
Standardized Data Acquisition
The receiving lab must run pre-defined quality control beads to ensure instrument performance (e.g., lasers, fluidics) is within specified limits before acquiring experimental data. The number of events to be collected for the target population should be specified in the transfer protocol to ensure sufficient statistical power, especially for rare cell populations [91]. Detector voltages must be set according to the transfer package SOP and should not be arbitrarily adjusted.
Gating Strategy and Data Interpretation
A clearly documented gating strategy is essential to prevent analyst-induced variability.
- Sequential Gating: The strategy should follow a logical hierarchy: (1) removal of debris based on FSC/SSC, (2) selection of single cells using FSC-A vs. FSC-H, (3) selection of live cells using the viability dye, and finally (4) identification of the target immunophenotype [105].
- Use of FMO Controls: Gate positions, particularly for dimly expressed antigens or when resolving continuous expression, must be set based on FMO controls, not unstained cells or isotype controls [104] [105]. This practice accounts for fluorescence spread from all other fluorochromes in the panel.
- Cross-Lab Verification: Initially, analysts from both sending and receiving labs should analyze the same data files to verify they are applying the gating strategy identically.
Data Presentation for Publication
To ensure clarity and reproducibility, all published data from transferred methods should include specific plot information [91] [102]:
- Axis Labels: Use the antigen and fluorochrome name (e.g., "CD45-APC"), not just detector names (e.g., "FL4").
- Scale Information: Clearly indicate linear or logarithmic scales with tick marks and corresponding values.
- Population Statistics: Display the percentage of cells within each gate.
- Event Count: Indicate the total number of events displayed on the plot in the figure legend.
The following workflow diagram summarizes the key stages of a robust method transfer process between two facilities.
Troubleshooting and Performance Monitoring
Even with meticulous planning, issues can arise. A systematic approach to troubleshooting is essential.
- Addressing Staining Variability: If staining intensity is inconsistent, first verify that both labs are using the same antibody clones, fluorochromes, and lot numbers. Confirm that titration was performed and that the staining protocol (incubation time, temperature, buffer) is followed precisely [104].
- Resolving Population Resolution Issues: If the separation between positive and negative populations is poor, check the instrument's optical alignment and calibration. Re-visit the single-stain controls to ensure compensation or unmixing is correct. Employ FMO controls to confirm gate placement [104] [103].
- Implementing Long-Term Monitoring: Post-transfer, the receiving lab should implement a long-term quality control program. This typically involves periodically running a standardized reference control (e.g., stabilized human PBMCs) and tracking key metrics like MFI and population percentages over time using Levy-Jennings charts to detect assay drift.
The faithful transfer of flow cytometry methods for immunophenotyping hematological malignancies is an active process that demands rigorous standardization, open communication, and thorough validation. By adopting the structured framework and detailed protocols outlined in this document, research and development teams can significantly enhance the reliability and comparability of data generated across different facilities. This, in turn, accelerates drug development, strengthens multi-center clinical studies, and ultimately improves the diagnostic and prognostic accuracy in the management of hematological cancers.
Comparative Analysis of Antibody Performance and Staining Specificity
Flow cytometry is an indispensable tool in the diagnosis and monitoring of hematological malignancies, enabling high-throughput, multiparametric analysis of single cells within heterogeneous populations [2]. The reliability of this technique, however, is fundamentally dependent on the performance and specificity of the antibodies used for immunophenotyping. Inaccurate data stemming from poorly characterized antibodies can directly impact diagnostic accuracy and subsequent therapeutic decisions [106]. This application note provides a comparative analysis of antibody staining methodologies and performance factors, supported by standardized protocols and quantitative data, to guide researchers in generating robust, reproducible flow cytometry data for hematological malignancy research.
The choice between direct and indirect staining methods is a primary consideration in experimental design. Each approach offers distinct advantages and limitations that influence factors such as time, cost, sensitivity, and background signal [107].
Table 1: Comparison of Direct and Indirect Antibody Staining Methods
| Factor | Direct Staining | Indirect Staining | Comments |
|---|---|---|---|
| Time | Low | High | Direct protocols are shorter with only one labeling step [107]. |
| Cost | High | Low | Secondary antibodies are inexpensive; one secondary can detect many primaries [107]. |
| Complexity | Low | High | Indirect methods require secondary antibody selection and additional controls [107]. |
| Sensitivity | Low | High | Multiple secondary antibodies bind per primary, amplifying the signal [107]. |
| Species Cross-reactivity | Minimized | Potential | Secondary antibodies may cross-react; use pre-adsorbed antibodies to prevent this [107]. |
| Background | Reduced | Potential | Samples with endogenous immunoglobulins may exhibit high background [107]. |
The direct method, where a fluorophore-conjugated primary antibody is used, is typically preferred for multicolor flow cytometry due to its simplicity and reduced propensity for non-specific binding. In contrast, the indirect method, which uses a labeled secondary antibody to detect an unlabeled primary, offers significant signal amplification, which can be beneficial for detecting low-abundance antigens [107].
Figure 1: Workflow comparison of direct and indirect immunofluorescence staining protocols.
Quantitative Metrics for Antibody and Fluorophore Performance
Fluorophore Brightness and Stain Index
The success of a flow cytometry experiment, particularly when detecting weakly expressed markers, often depends on the fluorophore's brightness. The Stain Index is a key quantitative metric that normalizes for signal intensity and background, providing a relative measure of fluorophore brightness on a specific cytometer [108]. It is calculated as:
Stain Index = (Mean Fluorescence Intensity of Positive Population - Mean Fluorescence Intensity of Negative Population) / (2 × Standard Deviation of the Negative Population) [108]
A higher stain index indicates a better signal-to-noise ratio. When designing multicolor panels, brighter fluorophores (higher stain index) should be paired with weakly expressed antigens, while dimmer fluorophores can be used for highly abundant targets [108].
Table 2: Properties of Common Fluorophores Used in Flow Cytometry
| Fluorophore | Excitation (nm) | Emission (nm) | Relative Brightness | Notes |
|---|---|---|---|---|
| Phycoerythrin (PE) | 565 | 575 | 5 | Protein-based, very bright [107]. |
| Allophycocyanin (APC) | 645 | 660 | 5 | Protein-based, very bright [107]. |
| Alexa Fluor 647 | 650 | 668 | 5 | Similar to APC but more suitable for intracellular staining [107]. |
| PE-Cyanine 7 (PE-Cy7) | 496, 565 | 774 | 4 | Tandem dye, highly sensitive to light [107]. |
| Alexa Fluor 488 | 495 | 519 | 3 | Similar to FITC but more stable and brighter [107]. |
| FITC | 494 | 520 | 2 | Sensitive to pH changes and photobleaching [107]. |
| Pacific Blue | 410 | 455 | 1 | Useful for labelling highly abundant antigens [107]. |
Antibody Validation and Specificity
A critical challenge in biomedical research is that a significant percentage of commercial antibodies fail to recognize their intended targets specifically. Large-scale validation studies have found that more than 50% of commercial antibodies failed in one or more standard applications [106]. This underscores the necessity of rigorous antibody validation for generating reliable data.
The gold standard for validating antibody specificity is the use of isogenic knockout cell lines, where the signal in wild-type cells is compared to that in genetically modified cells where the target gene has been knocked out [109] [106]. A specific antibody will show a clear signal loss in the knockout cells, confirming its specificity for the target protein.
Standardized Protocols for Cell Staining
Protocol for Cell Surface Antigen Staining
This protocol is optimized for the detection of proteins on the cell membrane, a cornerstone of immunophenotyping in hematological malignancies [110].
- Sample Preparation: Harvest cells and create a single-cell suspension. Wash cells in an isotonic phosphate buffer supplemented with 0.1-0.5% BSA or 5-10% fetal calf serum (FCS) by centrifugation at 350-500 x g for 5 minutes. For peripheral blood, use EDTA or heparin as an anticoagulant and perform red blood cell lysis if necessary [63] [110]. Determine cell count and resuspend at a concentration of 0.5–1 × 10^6 cells/100 µL [63].
- Fc Receptor Blocking: Incubate cells with an FcR blocking reagent (e.g., 2-10% serum, human IgG, or specific anti-FcR antibodies) for 15-60 minutes at 4°C to prevent non-specific antibody binding [63] [72].
- Antibody Incubation: Add fluorophore-conjugated primary antibodies at a titrated concentration (typically 5-10 µL per 10^6 cells). Vortex gently and incubate for 30 minutes in the dark at 4°C [110].
- Washing: Centrifuge at 350-500 x g for 5 minutes, decant the supernatant, and resuspend the cell pellet in 2 mL of staining buffer. Repeat this wash step twice to remove unbound antibody [110].
- Analysis: Resuspend the final cell pellet in 200-400 µL of staining buffer for acquisition on the flow cytometer [110].
Protocol for Intracellular Antigen Staining
Detection of intracellular proteins, such as transcription factors or cytokines, requires additional steps to make the internal cellular components accessible to antibodies [63].
- Cell Surface Staining (Optional): If analyzing both surface and intracellular markers, complete the cell surface staining protocol first (steps 1-4 above), then proceed to fixation [63].
- Fixation: After the final wash, resuspend the cell pellet in a fixative such as 1-4% paraformaldehyde (PFA) and incubate for 15-20 minutes on ice. This step preserves the cellular structure [63].
- Washing: Wash cells twice with suspension buffer to remove excess fixative [63].
- Permeabilization: Resuspend the cell pellet in a permeabilization solution (e.g., 0.1% Triton X-100, NP-40, or saponin) and incubate for 10-15 minutes at room temperature. This step disrupts the cell membrane, allowing antibodies to enter. Note: If acetone is used as a fixative, a separate permeabilization step is not required [63].
- Washing: Wash cells twice with suspension buffer or a permeabilization wash buffer [63].
- Intracellular Antibody Incubation: Resuspend cells in permeabilization buffer containing the fluorophore-conjugated antibody against the intracellular target. Incubate for 30 minutes in the dark at 4°C [63].
- Washing and Analysis: Wash cells twice with permeabilization buffer, then resuspend in staining buffer for flow cytometric analysis [63].
Essential Controls for Reliable Data Interpretation
Incorporating appropriate controls is non-negotiable for accurate data interpretation and is a critical component of standardized practice, especially in clinical diagnostics [2] [72].
- Viability Staining: Use cell-impermeable DNA-binding dyes (e.g., 7-AAD, propidium iodide) to exclude dead cells, which exhibit high autofluorescence and non-specific antibody binding [63] [72].
- Unstained and FMO Controls: Unstained cells are used to measure autofluorescence. Fluorescence Minus One (FMO) controls, which contain all antibodies in a panel except one, are essential for accurate gating in multicolor experiments as they account for fluorescence spillover [72].
- Isotype Controls: These antibodies match the host species, isotype, and conjugation of the primary antibody but lack specific target recognition. They help assess the level of non-specific Fc-mediated binding, though they should not be used to set positivity gates [72].
- Biological Controls: Where possible, use knockout cell lines or cells with known negative/positive expression of the marker as the most robust negative or positive controls [72].
- Compensation Controls: Use cells or compensation beads stained singly with each fluorophore in the panel to correct for spectral overlap into adjacent detectors [72].
Figure 2: A flowchart of essential controls required for rigorous flow cytometry experiments and their specific purposes.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Reagents for Flow Cytometry Experiments
| Reagent / Material | Function / Purpose | Examples |
|---|---|---|
| Flow Cytometry Staining Buffer | Suspension and washing medium; protein (BSA) reduces non-specific binding, sodium azide prevents capping. | PBS with 0.5% BSA or 5-10% FCS [63] [110]. |
| Fc Receptor Blocking Reagent | Blocks non-specific binding of antibodies to Fc receptors on immune cells. | Human IgG, mouse anti-CD16/CD32, goat serum [63] [110]. |
| Viability Dye | Distinguishes live from dead cells during analysis. | 7-AAD, Propidium Iodide, DRAQ7 [63] [72]. |
| Fixative | Preserves cellular structure and cross-links proteins for intracellular staining. | 1-4% Paraformaldehyde (PFA), Methanol, Acetone [63]. |
| Permeabilization Agent | Disrupts the cell membrane to allow antibody access to intracellular targets. | Triton X-100, NP-40, Saponin, Tween 20 [63]. |
| Compensation Beads | Uniform particles used with single-stained antibodies to calculate compensation matrices. | Anti-mouse/rat/rabbit Ig compensation beads [72]. |
| Red Blood Cell (RBC) Lysis Buffer | Lyses red blood cells in peripheral blood samples to isolate nucleated cells for analysis. | Ammonium chloride-based or commercial lyse buffers [63] [110]. |
The reliability of flow cytometry data in hematological malignancy research is inextricably linked to antibody performance and staining specificity. Researchers can significantly enhance the quality and reproducibility of their data by making informed choices between direct and indirect staining methods, selecting fluorophores based on quantitative metrics like the stain index, adhering to standardized staining protocols, and implementing a comprehensive panel of controls. The ongoing efforts toward global standardization of technical procedures, data interpretation, and reporting will further solidify flow cytometry's role as an indispensable tool in both research and clinical diagnostics [2] [17].
Conclusion
Flow cytometric immunophenotyping has become an indispensable tool for the diagnosis, classification, and monitoring of hematological malignancies. The synthesis of foundational knowledge, standardized methodologies, robust troubleshooting practices, and rigorous validation protocols is essential for generating clinically actionable and reproducible data. Future directions emphasize the need for continued global standardization of technical procedures and data interpretation, as championed by initiatives like EuroFlow, to maximize the clinical utility of this powerful technology. The integration of advanced multiparametric analysis and the correlation of phenotypic data with genetic findings promise to further refine disease classification, guide targeted therapies, and ultimately improve patient outcomes in biomedical and clinical research.
References
- 1. EuroFlow: Resetting leukemia and lymphoma . immunophenotyping [https://pmc.ncbi.nlm.nih.gov/articles/PMC3437406/]
- 2. An Update on Flow Cytometry Analysis of Hematological Malignancies: Focus on Standardization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190783/]
- 3. | PPTX Flow cytometry [https://www.slideshare.net/slideshow/flow-cytometry-46618943/46618943]
- 4. Publishing flow cytometry data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2822558/]
- 5. New flow cytometry in hematologic malignancies - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2791934/]
- 6. Newsletter: From Research to Therapy: How Flow Cytometry Supports the Drug Discovery Pipeline - FluoroFinder [https://fluorofinder.com/newsletter-from-research-to-therapy-how-flow-cytometry-supports-the-drug-discovery-pipeline/]
- 7. Fluorochrome choices for multi-color flow cytometry - PubMed [https://pubmed.ncbi.nlm.nih.gov/31181212/]
- 8. Consensus protocol for the flow of... cytometric immunophenotyping [https://pubmed.ncbi.nlm.nih.gov/8656686/]
- 9. (PDF) Multidimensional Flow of... Cytometry Immunophenotyping [https://www.academia.edu/8918652/Multidimensional_Flow_Cytometry_Immunophenotyping_of_Hematologic_Malignancy]
- 10. Detection of hematopoietic maturation abnormalities by flow cytometry in myelodysplastic syndromes and its utility for the differential diagnosis with non-clonal disorders - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0145212606001573]
- 11. The expression of human blood group antigens during erythropoiesis in a cell culture system - PubMed [https://pubmed.ncbi.nlm.nih.gov/10361141/]
- 12. The immunophenotype of different immature, myeloid and B- cell ... [https://www.nature.com/articles/leu200849?error=cookies_not_supported&code=ffc3557a-17ba-4305-88a8-1ef647a350db]
- 13. Advances and issues in flow detection of... cytometric [https://tp.amegroups.org/article/view/3551/html]
- 14. Data Analysis in Flow Cytometry: The Future Just Started - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2909632/]
- 15. Measurable Residual Disease Analysis by Flow Cytometry: Assay Validation and Characterization of 385 Consecutive Cases of Acute Myeloid Leukemia [https://www.mdpi.com/2072-6694/17/7/1155]
- 16. in multiple myeloma: current status Minimal residual disease [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-021-00328-2]
- 17. Clinically useful information provided by the flow ... cytometric [https://pubmed.ncbi.nlm.nih.gov/10508115/]
- 18. (PDF) Clinically useful information provided by the flow ... cytometric [https://www.academia.edu/27820386/Clinically_useful_information_provided_by_the_flow_cytometric_immunophenotyping_of_hematological_malignancies_current_status_and_future_directions]
- 19. value of Prognostic by EuroFlow... minimal residual disease detected [https://pubmed.ncbi.nlm.nih.gov/40241540/]
- 20. value of Prognostic by EuroFlow... minimal residual disease detected [https://haematologica.org/article/view/12033]
- 21. Monitoring of Measurable Residual Disease in Multiple Myeloma by Multiparametric Flow Cytometry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6788635/]
- 22. KoreaMed Synapse [https://synapse.koreamed.org/articles/1516085907]
- 23. Frontiers | The emerging role of next-generation sequencing in minimal ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1570041/full]
- 24. Neoplastic Plasma Cell Aberrant Antigen Expression Patterns and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4408538/]
- 25. Frontiers | Database-Guided Analysis for Immunophenotypic Diagnosis... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.746951/full]
- 26. A simple method for detection of major phenotypic in... abnormalities [https://haematologica.org/article/view/4487]
- 27. Data analysis in flow cytometry | Abcam [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/data-analysis-in-flow-cytometry]
- 28. How to Interpret Flow Cytometry Data | Fortis Life Sciences [https://www.fortislife.com/resources/antibody-resources/how-to-interpret-flow-cytometry-data]
- 29. EuroFlow standardization of flow instrument settings and... cytometer [https://www.nature.com/articles/leu2012122?error=cookies_not_supported]
- 30. Standardizing Flow Cytometry Immunophenotyping Analysis from the Human ImmunoPhenotyping Consortium | Scientific Reports [https://www.nature.com/articles/srep20686]
- 31. An Update on Flow Cytometry Analysis of Hematological Malignancies: Focus on Standardization [https://www.mdpi.com/2072-6694/17/12/2045]
- 32. Advanced immunophenotyping of lymphocyte and monocyte subsets in healthy Australian adults using a novel spectral flow cytometry panel - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322900/]
- 33. EuroFlow standardization of flow instrument settings and... cytometer [https://www.nature.com/articles/leu2012122?error=cookies_not_supported&code=7caf8a48-03c6-471b-be1d-6081cf8d0525]
- 34. of flow cytometer EuroFlow and... standardization instrument settings [https://pubmed.ncbi.nlm.nih.gov/22948490/]
- 35. The EuroFlow ™ SOPs – Cytognos, S.L. [https://www.cytognos.com/academy/cytognos-technology/euroflow/the-euroflow-sops/]
- 36. Protocols Standardized EuroFlow [https://euroflow.org/protocols/]
- 37. Standardization of 8-color flow cytometry across different flow cytometer instruments: A feasibility study in clinical laboratories in Switzerland - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0022175917302053]
- 38. EuroFlow antibody panels for standardized n-dimensional flow cytometric immunophenotyping of normal, reactive and malignant leukocytes | Leukemia [https://www.nature.com/articles/leu2012120]
- 39. Performance of a novel eight-color flow cytometry panel for measurable residual disease assessment of chronic lymphocytic leukemia - PubMed [https://pubmed.ncbi.nlm.nih.gov/38535092/]
- 40. Toward Standardization of Flow-Cytometric Immunophenotyping for the Diagnosis and Monitoring of Hematologic Malignancies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10813827/]
- 41. Immunophenotyping by flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/immunophenotyping-by-flow-cytometry]
- 42. Multiparametric Flow for MRD Monitoring in Hematologic... Cytometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC8470441/]
- 43. Data Analysis: What does a histogram for flow cytometry tell me? | Unsolved Mysteries of Human Health | Oregon State University [https://unsolvedmysteries.oregonstate.edu/data-analysis-what-does-histogram-flow-cytometry-tell-me]
- 44. Frontiers | Dissecting immunophenotypic diversity in multiple myeloma... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1642609/full]
- 45. Tracing Human IgE B Cell Antigen Receptor-Bearing Cells With... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8721004/]
- 46. A user's guide to multicolor flow cytometry panels for comprehensive immune profiling - PubMed [https://pubmed.ncbi.nlm.nih.gov/34033799/]
- 47. Flow Cytometry in the Diagnosis of Leukemias - Leukemia - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK586209/]
- 48. and Optimization for High-Dimensional... Panel Design [https://pubmed.ncbi.nlm.nih.gov/32150355/]
- 49. Spectral Flow Cytometry Methods and Pipelines for Comprehensive Immunoprofiling of Human Peripheral Blood and Bone Marrow - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10962315/]
- 50. Panel Design and Optimization for Full Spectrum Flow Cytometry - PubMed [https://pubmed.ncbi.nlm.nih.gov/38526784/]
- 51. Design for Multicolor ... | Boster Bio Panel Flow Cytometry [https://www.bosterbio.com/protocol-and-troubleshooting/flow-cytometry-optimization/fluorescent-conjugates]
- 52. Designing a multicolour protocol | Abcam flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/designing-a-multicolor-protocol]
- 53. | Tips for Building Multicolor Flow Cytometry Flow Cytometry Panels [https://www.sigmaaldrich.com/PT/en/technical-documents/technical-article/protein-biology/flow-cytometry/multicolor-flow-cytometry-tips]
- 54. Spectral Flow | Thermo Fisher Scientific - US Cytometry Panel Design [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-methods/spectral-flow-cytometry-panel-design.html]
- 55. a Preparing - Single for Cell Suspension Flow Cytometry [https://fluorofinder.com/preparing-a-single-cell-suspension-for-flow-cytometry/]
- 56. Sample Preparation Tips for Accurate Flow Results Cytometry [https://www.labx.com/resources/sample-preparation-tips-for-accurate-flow-cytometry-results/5521]
- 57. How To Prepare a Good Single | Applied Cell Suspension Cytometry [https://www.appliedcytometry.com/articles/good-single-cell-suspension/]
- 58. Best Practices for Preparing a Single from Solid... Cell Suspension [https://pubmed.ncbi.nlm.nih.gov/30523671/]
- 59. EuroFlow standardization of flow cytometer instrument settings and immunophenotyping protocols | Leukemia [https://www.nature.com/articles/leu2012122]
- 60. BestProtocols: Cell for Preparation Protocols Flow Cytometry [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/cell-preparation-flow-cytometery.html]
- 61. A protocol to effectively create single of adherent... cell suspensions [https://pubmed.ncbi.nlm.nih.gov/19997869/]
- 62. Flow cytometric immunophenotyping for hematologic neoplasms - PubMed [https://pubmed.ncbi.nlm.nih.gov/18198345/]
- 63. Protocol | Abcam Flow Cytometry [https://www.abcam.com/en-us/technical-resources/protocols/flow-cytometry-for-intracellular-and-extracellular-targets]
- 64. Flow cytometric detection of intracellular antigens for immunophenotyping of normal and malignant leukocytes - PubMed [https://pubmed.ncbi.nlm.nih.gov/8709649/]
- 65. Protocol | Proteintech Group Intracellular Flow Cytometry Staining [https://www.ptglab.com/news/blog/intracellular-flow-cytometry-staining-protocol/]
- 66. Newsletter: Intracellular Fundamentals - FluoroFinder Flow Cytometry [https://fluorofinder.com/newsletter-intracellular-flow-cytometry-fundamentals-2/]
- 67. Perm Flow : Intracellular... | Boster Bio Cytometry Fixation Method [https://www.bosterbio.com/protocol-and-troubleshooting/flow-cytometry-optimization/perm-fixation-method]
- 68. , Methanol Flow Cytometry Permeabilization Protocol [https://www.cellsignal.com/learn-and-support/protocols/protocol-flow-methanol-permeabilization]
- 69. Assessment of Different Permeabilization of Minimizing... Methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC3895578/]
- 70. (FC) Flow | Rockland Cytometry Protocol [https://www.rockland.com/resources/flow-cytometry-protocol/]
- 71. How to Set Up Proper Controls for Your Flow Experiment Cytometry [https://synapse.patsnap.com/article/how-to-set-up-proper-controls-for-your-flow-cytometry-experiment]
- 72. Recommended controls for flow | Abcam cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/recommended-controls-for-flow-cytometry]
- 73. Tips on Flow - Abacus dx Cytometry Controls [https://www.abacusdx.com/life-science/tips-flow-cytometry-controls/]
- 74. Short article on FMO used in controls . flow cytometry [https://med.uth.edu/imm/flow-cytometry-services/protocols-and-guidelines/fmo-controls/]
- 75. What are Fluorescence Minus One ( FMO ) Controls ? [https://www.news-medical.net/life-sciences/What-are-Fluorescence-Minus-One-(FMO)-Controls.aspx]
- 76. When To Use (And Not Use) Flow Cytometry Isotype Controls - ExpertCytometry [https://expertcytometry.com/when-to-use-and-not-use-flow-cytometry-isotype-controls/]
- 77. Isotype Control Antibodies | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/antibodies/primary-antibodies/control-antibodies/isotype-control-antibodies.html]
- 78. AI in flow cytometry: Current applications and future directions - PubMed [https://pubmed.ncbi.nlm.nih.gov/40985220/]
- 79. 5 Recipes for Flow Buffers - FluoroFinder Cytometry [https://fluorofinder.com/flow-cytometry-buffers/]
- 80. analysis of Flow proliferation and phenotype in... cytometric live cell [https://pubmed.ncbi.nlm.nih.gov/10554182/]
- 81. Frontiers | Editorial: Precision immunotherapy and novel target... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1703886/full]
- 82. Do more with Less: Improving High Parameter Cytometry Through... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9827877/]
- 83. Best Practices for Multiparametric Flow Cytometry [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-79/best-practices-multiparametric-flow-cytometry.html]
- 84. EuroFlow standardization of flow instrument settings and... cytometer [https://www.nature.com/articles/leu2012122?error=cookies_not_supported&code=cd1de26a-93f7-4161-8314-796c499287aa]
- 85. Analysis from... Standardizing Flow Cytometry Immunophenotyping [https://www.nature.com/articles/srep20686?error=cookies_not_supported&code=7eef1379-7b40-4053-aee8-4901e630bd0c]
- 86. Standardization of Flow Cytometric Immunophenotyping for Hematological Malignancies: The FranceFlow Group Experience - PubMed [https://pubmed.ncbi.nlm.nih.gov/31364809/]
- 87. Reducing variability in flow cytometry | Nature Reviews Immunology [https://www.nature.com/articles/nri3158-c2]
- 88. An integrated workflow to assess technical and biological variability of cell population frequencies in human peripheral blood by flow cytometry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5296239/]
- 89. High-Sensitivity Flow for the Reliable Detection of... Cytometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC11727296/]
- 90. Flow Cytometry Method Validation Protocols [https://pubmed.ncbi.nlm.nih.gov/30418706/]
- 91. Publishing flow cytometry data - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2822558/]
- 92. services | NeoGenomics Laboratories Flow cytometry [https://www.neogenomics.com/flow-cytometry-services/]
- 93. of Validation for Antibodies - FluoroFinder Flow Cytometry [https://fluorofinder.com/antibody-validation/]
- 94. Relevance of Antibody for Validation Flow Cytometry [https://pubmed.ncbi.nlm.nih.gov/31577065/]
- 95. Product Performance & Validation | Cell Signaling Technology [https://www.cellsignal.com/about-us/cst-antibody-validation-principles]
- 96. - Basics, Data Interpretation & Flow Choice Cytometry Antibody [https://www.rapidnovor.com/antibody-flow-cytometry/]
- 97. Overview of FDA Final Rule Laboratory Developed Test [https://www.ascp.org/news/news-details/2024/05/14/overview-of-fda-laboratory-developed-test-final-rule]
- 98. B-Cell Depletion Assays via Validating | Mabion Flow Cytometry [https://www.mabion.eu/science-hub/articles/bioanalytical-flow-cytometry-assay-validation-strategy/]
- 99. (PDF) Flow Method Cytometry Protocols Validation [https://www.academia.edu/102913540/Flow_Cytometry_Method_Validation_Protocols]
- 100. Flow Cytometry Panel Design: The Basics | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-71/bioprobes-71-flow-cytometry-panel-design.html]
- 101. Quantitative Flow Cytometry: Applications & Benefits - KCAS Bio [https://kcasbio.com/blogs/understanding-quantitative-flow-cytometry/]
- 102. Spot the Difference: 5 Ways to Improve the Presentation of Your Flow Cytometry Data [https://bitesizebio.com/26007/spot-the-difference-5-ways-to-improve-the-presentation-of-your-flow-cytometry-data/]
- 103. Flow Cytometry | Flow Cytometry Reagents | Bio-Techne [https://www.bio-techne.com/applications/flow-cytometry]
- 104. Spectral Flow Cytometry Panel Controls and Sample Preparation | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-methods/spectral-flow-cytometry-panel-controls-sample-preparation.html]
- 105. Gating for Beginners | Proteintech Group Flow Cytometry [https://www.ptglab.com/news/blog/flow-cytometry-gating-for-beginners/]
- 106. Scaling of an antibody validation procedure enables quantification of... [https://elifesciences.org/reviewed-preprints/91645]
- 107. Types of antibody for antigen detection in staining flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/types-of-antibody-staining-for-flow-cytometry]
- 108. Index for Stain - Explained - FluoroFinder Flow Cytometry [https://fluorofinder.com/stain-index-flow-cytometry/]
- 109. A guide to selecting high- performing for... | F1000Research antibodies [https://f1000research.com/articles/14-1158]
- 110. Flow Cytometry Protocol for Cell Surface Markers (FACS Protocol): R&D Systems [https://www.rndsystems.com/resources/protocols/flow-cytometry-protocol-staining-membrane-associated-proteins-suspended-cells]