Mechanistic Models vs. AI in Tumor Modeling: A New Paradigm for Computational Oncology
This article provides a comprehensive analysis for researchers and drug development professionals on the distinct yet complementary roles of mechanistic models and artificial intelligence (AI) in computational oncology.
Mechanistic Models vs. AI in Tumor Modeling: A New Paradigm for Computational Oncology
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the distinct yet complementary roles of mechanistic models and artificial intelligence (AI) in computational oncology. We explore the foundational principles of both approaches, from mechanism-driven mathematical theories to data-hungry machine learning algorithms. The scope covers their methodological applications in diagnosis, treatment prediction, and drug discovery, alongside a critical examination of challenges like data scarcity, model interpretability, and clinical validation. By synthesizing current advancements and comparative studies, this review aims to guide the strategic integration of these modeling paradigms to accelerate the development of personalized cancer therapies and improve patient outcomes.
Core Principles: From Biological Mechanisms to Data Patterns
In the field of mathematical oncology, two distinct yet complementary approaches have emerged for modeling tumor biology and treatment response: mechanistic models and AI/machine learning (ML) models [1]. Mechanistic models are knowledge-driven constructs that use mathematical equations to represent our current understanding of biological processes, grounded in the fundamental principles of biology, chemistry, and physics [1]. In contrast, AI/ML models are data-driven approaches that extract hidden patterns and relationships from large datasets without requiring explicit knowledge of the underlying biology [2]. This guide provides an objective comparison of these approaches, focusing on their implementation, performance, and applicability in cancer research and drug development.
Background: Core Principles and Applications
Knowledge-Driven Mechanistic Modeling
Mechanistic mathematical models are abstract, simplified mathematical constructs created to represent parts of biological reality for a particular purpose [1]. In oncology, they describe the behavior of complex cancer systems based on understanding of underlying mechanisms rooted in fundamental biology [1]. These models deliberately approximate reality through equations or rules, with inevitable simplifying assumptions such as reduced dimensionality, dynamic processes approximated as time-invariant, or biological pathways reduced to key components [1].
Common applications in cancer research include investigating somatic cancer evolution and treatment, simulating different radiotherapy fractionation schemes, modeling treatment-induced tumor resistance, and simulating in silico trials for hypothesis generation [1]. The quality of these approximations is validated with data, and their strength lies in generating insights through simulation of unobserved scenarios, even in the absence of experimental data [1].
Data-Driven AI/ML Modeling
AI and machine learning approaches excel at identifying patterns in high-dimensional datasets without requiring specific knowledge about the underlying biology [2]. These models are particularly valuable when only incomplete or limited knowledge is available for a study [2]. In cancer metabolism research, for example, ML techniques have been applied to diverse data sources including RNA-seq data, multi-omics data (transcriptomics, proteomics, phosphoproteomics, and fluxomics), and FDG-PET/CT imaging data [2].
Common applications in oncology include drug response prediction, molecular tumor subtype identification, volumetric tumor segmentation, image-based outcome predictions, and automated intervention planning [1]. The flexibility of highly parameterized models like deep neural networks allows them to approximate complex and mechanistically unknown relationships, functioning as "universal function approximators" [1].
Performance Comparison: Quantitative Analysis
A direct comparison study evaluated the performance of mechanistic modeling versus machine learning approaches for predicting breast cancer cell growth dynamics in response to glucose transporter inhibition [2]. The study tracked growth of MDA-MB-231 breast cancer cells treated with Cytochalasin B (a GLUT1 inhibitor) using time-resolved microscopy and compared predictions across modeling approaches.
Table 1: Model Performance Comparison for Predicting Tumor Cell Growth
| Model Type | Specific Approach | Prediction Accuracy (R²) | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Machine Learning | Random Forest | 0.92 | Highest predictive accuracy | Limited biological interpretability |
| Machine Learning | Decision Tree | 0.89 | Good balance of accuracy/interpretability | Prone to overfitting |
| Machine Learning | K-Nearest Neighbor | 0.84 | Simple implementation | Performance depends on feature selection |
| Mechanistic | ODE Model | 0.77 | Biological interpretability, mechanism elucidation | Lower accuracy than top ML models |
| Machine Learning | Linear Regression | 0.69 | Simple, fast computation | Limited complexity handling |
The quantitative comparison reveals that while the random forest model provided the highest predictive accuracy (R² = 0.92), the mechanism-based model demonstrated respectable predictive capability (R² = 0.77) with the significant added benefit of elucidating biological mechanisms [2]. This trade-off between predictive accuracy and biological interpretability represents a fundamental consideration when selecting modeling approaches for specific research objectives.
Methodologies: Experimental and Computational Workflows
Mechanistic Model Development Process
The development of mechanistic models follows a structured workflow that integrates biological knowledge with mathematical formalization:
Table 2: Mechanistic Model Development Protocol
| Step | Description | Key Considerations |
|---|---|---|
| 1. System Definition | Identify key biological components and interactions | Balance comprehensiveness with simplicity |
| 2. Mathematical Formalization | Translate biological mechanisms into equations (ODEs, PDEs, ABMs) | Select appropriate mathematical framework |
| 3. Parameter Estimation | Calibrate model parameters using experimental data | Address parameter identifiability challenges |
| 4. Model Validation | Test predictions against independent datasets | Ensure biological plausibility beyond fit quality |
| 5. Experimental Testing | Generate and test novel biological predictions | Use model to guide future experiments |
For example, in developing a model for tumor metabolism, researchers create a mechanistic framework incorporating key metabolic pathways active in tumor cells, including glycolysis, TCA cycle, oxidative phosphorylation, and glutaminolysis [3]. The dynamics of metabolite concentrations are modeled using ordinary differential equations with mathematical expressions describing enzyme activities and kinetic parameters obtained from literature [3].
Machine Learning Implementation Workflow
The implementation of machine learning models for cancer research follows a different pathway focused on data processing and algorithm selection:
- Data Collection and Preprocessing: Acquire and clean relevant datasets (e.g., transcriptomics, proteomics, imaging data)
- Feature Selection: Identify the most predictive variables from high-dimensional data
- Model Selection: Choose appropriate ML algorithms based on data characteristics and research questions
- Training and Validation: Implement cross-validation strategies to prevent overfitting
- Performance Evaluation: Assess model accuracy using appropriate metrics (e.g., R², AUC-ROC)
In the breast cancer cell growth prediction study, researchers compared four common ML models: random forest, decision tree, k-nearest-neighbor regression, and linear regression, using time-resolved microscopy data for training and validation [2].
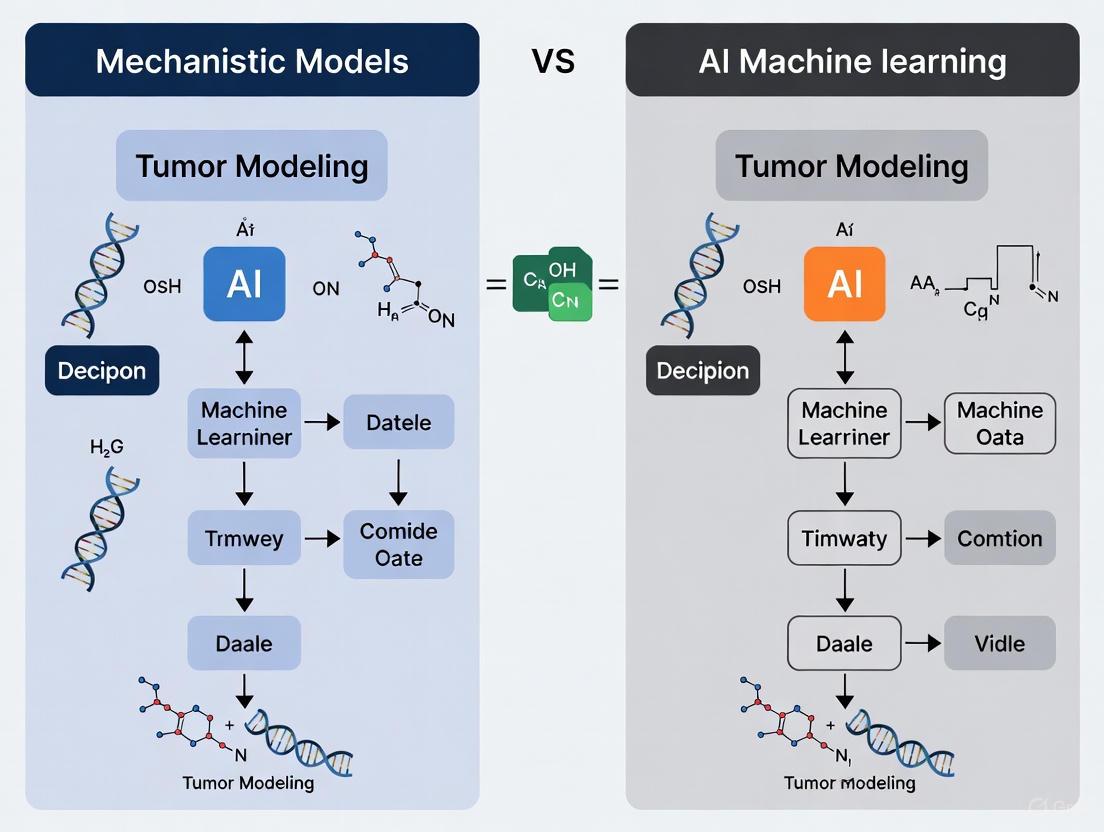
Visualizing Model Integration: The Hybrid Approach
The emerging field of mechanistic learning represents the synergistic combination of mechanistic mathematical modeling and data-driven machine or deep learning [1]. This integration can be visualized through the following workflow:
Research Reagent Solutions for Tumor Modeling
Implementing either modeling approach requires specific experimental resources and computational tools. Below is a compilation of key research reagents and their applications in generating data for model development and validation.
Table 3: Essential Research Reagents and Resources
| Reagent/Resource | Function/Application | Example Use Case |
|---|---|---|
| MDA-MB-231 Cell Line | Triple-negative breast cancer model system | Studying glucose metabolism and inhibitor response [2] |
| Cytochalasin B | Competitive GLUT1 glucose transporter inhibitor | Perturbing glucose uptake to study metabolic adaptations [2] |
| IncuCyte S3 Live-Cell Imaging | Time-resolved microscopy and cell confluence tracking | Longitudinal monitoring of tumor cell growth dynamics [2] |
| Cytotox Red Reagent | Fluorescent dead cell indicator | Quantifying cell death in response to metabolic inhibition [2] |
| GLUT1 Inhibitors | Targeting glucose transport machinery | Investigating metabolic vulnerabilities in cancer cells [2] |
| Multi-omics Datasets | Transcriptomics, proteomics, metabolomics data | Training AI/ML models and validating mechanistic models [4] |
| Immune Checkpoint Reagents | Antibodies targeting PD-1, CTLA-4, LAG3, etc. | Studying tumor-immune interactions in QSP models [4] |
Applications and Future Directions
The integration of mechanistic and AI approaches through mechanistic learning represents the future of computational oncology [1]. This hybrid framework leverages the strengths of both paradigms: the interpretability and biological grounding of mechanistic models, and the pattern recognition capabilities and adaptability of AI/ML [5].
Four categories of mechanistic learning have emerged:
- Sequential: Using model outputs as inputs for another model
- Parallel: Independent modeling with integrated interpretation
- Extrinsic: Using external knowledge to constrain AI models
- Intrinsic: Building biological mechanisms directly into model architectures [1]
These approaches are particularly valuable for addressing complex challenges in oncology research, including longitudinal tumor response predictions and time-to-event modeling [1]. As the field advances, mechanistic learning frameworks show great promise for addressing persistent challenges in oncology such as limited data availability, requirements for model transparency, and integration of complex multi-scale data [1].
The concept of patient-specific digital twins - virtual replicas that simulate disease progression and treatment response - represents one of the most promising clinical applications of these integrated modeling approaches [5]. These computational avatars integrate real-time patient data into mechanistic frameworks enhanced by AI, enabling personalized treatment planning and therapeutic strategy optimization [5].
The field of oncology is witnessing a paradigm shift in how tumors are modeled and understood, characterized by a tension between traditional mechanistic models and emerging artificial intelligence/machine learning (AI/ML) approaches. Mechanistic models are grounded in established biological theory, representing tumor behavior through mathematical equations derived from known physics and biology, such as partial differential equations describing drug diffusion or cell proliferation dynamics. In contrast, AI/ML models are data-driven, learning complex patterns directly from large-scale oncology datasets without requiring pre-specified biological rules [5]. This guide explores how these AI/ML models function as powerful tools for pattern recognition, objectively comparing their performance against traditional methods and mechanistic modeling approaches across key oncology applications.
Core Principles: How AI/ML Models Recognize Patterns in Oncology Data
AI/ML models in oncology excel at identifying multidimensional relationships within complex datasets that often elude human perception or traditional statistical methods. Their operation hinges on several key principles:
Feature Hierarchy Learning: Deep learning models, particularly convolutional neural networks (CNNs), automatically learn hierarchical representations of oncology data. In pathology image analysis, for instance, initial layers might detect simple edges and textures, intermediate layers identify cellular structures, and deeper layers recognize complex tissue architectures indicative of malignancy [6] [7].
Multimodal Data Integration: Advanced AI models fuse heterogeneous data types—including genomic sequences, medical images, clinical records, and protein expressions—to generate more comprehensive predictions. This integration enables the discovery of cross-modal relationships, such as correlating specific genetic mutations with distinctive radiological features visible on CT scans [6] [7].
Nonlinear Pattern Recognition: Unlike traditional statistical methods that often assume linear relationships, ML algorithms capture complex nonlinear interactions between variables. This capability is particularly valuable in tumor ecosystems where biological processes frequently exhibit threshold effects, feedback loops, and complex interdependencies [5] [8].
The following diagram illustrates the fundamental workflow of a data-driven AI/ML model for pattern recognition in oncology, contrasting with hypothesis-driven mechanistic approaches:
Performance Comparison: AI/ML Models Versus Traditional Methods
Diagnostic and Prognostic Performance Across Cancer Types
AI/ML models have demonstrated compelling performance advantages across multiple oncology domains, particularly in diagnostic imaging and survival prediction, as quantified in numerous clinical validation studies.
Table 1: Performance Comparison of AI/ML Models Versus Traditional Methods in Cancer Diagnosis
| Cancer Type | AI/ML Model | Traditional Method | Performance Metrics | Reference |
|---|---|---|---|---|
| Breast Cancer | Deep Learning (Mammography) | Radiologist Interpretation | Superior sensitivity (reduced false negatives by 9.4%) and specificity (reduced false positives by 5.7%) | [9] |
| Lung Cancer | CheXNeXt CNN (Chest X-ray) | Board-certified Radiologists | 52.3% greater sensitivity for masses, 20.4% greater sensitivity for nodules with comparable specificity | [7] |
| Colorectal Cancer | AI-assisted Colonoscopy (CADe) | Standard Colonoscopy | Higher adenoma detection rates; Sensitivity: 97%, Specificity: 95% | [9] [7] |
| Prostate Cancer | Validated AI System (MRI) | Radiologist Assessment | Superior AUC (0.91 vs 0.86); detected more cases of Gleason grade group ≥2 cancers at same specificity | [7] |
| Multiple Cancers | DL in Digital Pathology | Manual Pathology Review | Reduced interpretation variability; Automated tumor-stroma ratio quantification prognostic for survival | [6] [10] |
Table 2: Performance of AI/ML Models in Prognostic Prediction and Therapeutic Guidance
| Clinical Application | AI/ML Model | Comparison Baseline | Performance Outcome | Reference |
|---|---|---|---|---|
| Advanced HCC Survival Prediction | StepCox (forward) + Ridge (101 models tested) | Conventional Staging | C-index: 0.68 (training), 0.65 (validation); 1-2 year AUC: 0.72-0.75 | [11] |
| Bladder Cancer Recurrence | Multi-modal ML (Radiomics + Clinical + Genomic) | Conventional Statistical Models | Superior recurrence prediction accuracy | [8] |
| Prostate Cancer PSA Persistence | Random Forest | Traditional Clinical Nomograms | AUC: 0.861 (training), 0.801 (test set) | [8] |
| Immunotherapy Response | Deep Learning on Pathology Slides | Pathologist Assessment | Identification of histomorphological features correlating with response to immune checkpoint inhibitors | [12] |
Comparison with Mechanistic Modeling Approaches
The performance advantages of AI/ML models must be contextualized within the broader modeling landscape, particularly in relation to traditional mechanistic approaches.
Table 3: AI/ML Models Versus Mechanistic Models in Oncology Research
| Characteristic | AI/ML Models | Mechanistic Models |
|---|---|---|
| Primary Basis | Data-driven pattern recognition | First principles of biology and physics |
| Data Requirements | Large, annotated datasets for training | Detailed mechanistic parameters |
| Interpretability | Often "black box"; limited biological insight | High interpretability with clear biological mechanisms |
| Generalizability | May fail with out-of-distribution data | Better extrapolation to novel conditions |
| Computational Demand | High during training, variable during inference | Often computationally intensive for simulation |
| Key Strength | Superior accuracy with sufficient data | Hypothesis testing and theoretical understanding |
| Regulatory Status | Multiple FDA-approved devices (71 in radiology, pathology) [13] | Mainly research use; limited clinical adoption |
Experimental Protocols: Methodologies for AI/ML Model Validation
Protocol: Development and Validation of Survival Prediction Models
The following methodology, derived from a study on hepatocellular carcinoma (HCC) survival prediction, exemplifies rigorous AI/ML model development [11]:
Cohort Selection and Data Collection:
- Enroll 175 HCC patients with balanced baseline characteristics
- Inclusion criteria: BCLC stage B or C, Child-Pugh class A or B liver function, complete clinical data
- Collect multimodal data: clinical parameters (Child-Pugh score, BCLC stage), tumor characteristics (size, number), treatment variables (radiotherapy, immunotherapy, targeted therapy)
Data Preprocessing and Cohort Division:
- Perform propensity score matching to balance baseline characteristics between treatment groups
- Randomly divide patients into training (60%) and validation (40%) cohorts
- Conduct univariate Cox regression to identify prognostic factors (p < 0.05) for model inclusion
Model Training and Selection:
- Implement 101 different machine learning algorithms on the training cohort
- Include Cox proportional hazards models, regularized Cox models (Ridge, Lasso, Elastic Net), survival trees, and ensemble methods
- Train each model using identified prognostic variables ("Child," "BCLC stage," "Size," "Treatment")
Performance Validation:
- Assess model performance using concordance index (C-index) in both training and validation cohorts
- Perform time-dependent receiver operating characteristic (ROC) analysis at 1-, 2-, and 3-year survival endpoints
- Select best-performing model based on validation cohort performance (StepCox [forward] + Ridge model achieving C-index: 0.65)
Clinical Implementation:
- Generate risk score stratification for patient prognosis
- Enable individualized prognostic assessment to guide treatment decisions
Protocol: AI-Assisted Diagnostic Model Development
For diagnostic applications such as cancer detection in medical images, a different methodological approach is employed [9] [6]:
Dataset Curation:
- Collect large-scale annotated datasets (e.g., 10,000-100,000 images)
- Obtain expert annotations (radiologists/pathologists) for ground truth labels
- Ensure diverse representation across demographics, cancer subtypes, and imaging equipment
Model Architecture Selection:
- Implement convolutional neural networks (CNNs) for image-based tasks
- Utilize transfer learning from pre-trained models when sample size is limited
- Design custom architectures optimized for specific imaging modalities (mammography, CT, pathology whole-slide images)
Training Methodology:
- Apply data augmentation techniques (rotation, flipping, contrast adjustment) to improve generalization
- Utilize progressive training strategies that leverage both strongly and weakly labeled data
- Implement regularization methods (dropout, weight decay) to prevent overfitting
Validation Framework:
- Conduct multi-center external validation on independent datasets
- Compare AI performance against human experts in blinded evaluations
- Assess diagnostic sensitivity, specificity, area under ROC curve, and clinical workflow impact
The following diagram illustrates the integrated approach combining AI/ML pattern recognition with mechanistic modeling principles, representing the future of computational oncology:
Research Reagent Solutions: Essential Tools for AI/ML Oncology Research
The development and validation of AI/ML models in oncology requires specialized data resources and computational tools that function as essential "research reagents" in this domain.
Table 4: Essential Research Reagents and Resources for AI/ML Oncology Research
| Resource Category | Specific Examples | Function in AI/ML Research | Access Considerations |
|---|---|---|---|
| Curated Cancer Databases | The Cancer Genome Atlas (TCGA), Genomic Data Commons | Provides multimodal training data (genomics, images, clinical) for model development | Publicly available with data use agreements |
| AI/ML Software Frameworks | TensorFlow, PyTorch, Scikit-learn | Enables implementation of deep learning and machine learning algorithms | Open-source with community support |
| Medical Imaging Archives | Cancer Imaging Archive (TCIA), LIDC-IDRI | Curated repositories of radiological images with annotations for computer vision applications | De-identified data available for research use |
| Computational Infrastructure | High-performance Computing (HPC) clusters, Cloud GPUs | Provides necessary processing power for training complex models on large datasets | Institutional resources or commercial cloud services |
| Biobanks with Digital Pathology | Institutional biobanks with whole-slide imaging | Digitized histopathology slides for development of computational pathology algorithms | Requires institutional review board approval |
| Clinical Trial Data Repositories | Project Data Sphere, NCTN Navigator | Anonymized clinical trial data for model validation across diverse populations | Controlled access for research purposes |
The comparison between AI/ML models and traditional mechanistic approaches reveals a complementary rather than competitive relationship. AI/ML models demonstrate superior performance in tasks requiring pattern recognition within complex, high-dimensional oncology datasets, consistently matching or exceeding human expert performance and traditional statistical methods across diagnostic and prognostic applications [9] [11] [7]. However, mechanistic models retain crucial advantages in interpretability, hypothesis testing, and extrapolation beyond available data.
The most promising future direction lies in hybrid frameworks that leverage the strengths of both approaches [5]. These integrated models use AI/ML for parameter estimation from real-world data while maintaining mechanistic biological constraints, creating "digital twins" that can simulate individual patient disease progression and treatment response [5] [12]. As the field advances, overcoming challenges related to data quality, model interpretability, and regulatory standardization will be essential for translating these powerful pattern recognition tools into routine clinical practice, ultimately enabling more precise, personalized, and effective cancer care.
In the pursuit of overcoming cancer, researchers increasingly rely on computational models to understand tumor dynamics and treatment resistance. Two distinct philosophical approaches have emerged: hypothesis-driven modeling, rooted in mechanistic biological understanding, and correlation-based modeling, which leverages statistical patterns in large datasets. The former builds on established biological principles to explain how and why tumors behave as they do, while the latter identifies predictive relationships from data without necessarily requiring mechanistic insight. Within tumor modeling research, this dichotomy represents a fundamental tension between mechanistic models derived from first principles and artificial intelligence/machine learning approaches that excel at finding patterns in complex data. Both approaches offer distinct advantages and limitations, with the choice depending on research objectives, data availability, and the desired interpretability of results. This guide objectively compares these competing philosophies through their application in oncology, providing researchers with a framework for selecting appropriate methodologies for specific drug development challenges.
Core Philosophical Differences and Mathematical Foundations
The distinction between hypothesis-driven and correlation-based modeling begins with their fundamental philosophical underpinnings and extends to their mathematical implementation.
Hypothesis-driven modeling follows a deductive approach, beginning with a specific biological hypothesis about system mechanisms. These models incorporate established biological knowledge and physical laws, with parameters typically corresponding to measurable biological properties. For example, in tumor growth modeling, parameters might represent proliferation rates, carrying capacity, or drug effect rates [14]. The model structure itself embodies testable hypotheses about underlying mechanisms, such as including separate compartments for proliferative and quiescent cells based on the hypothesis that these populations behave differently under treatment [14].
Correlation-based modeling employs an inductive approach, discovering patterns and relationships directly from data without pre-specified mechanistic assumptions. Parameters in these models often lack direct biological interpretation, instead serving to maximize predictive accuracy. The model structure is typically chosen for flexibility rather than biological plausibility, potentially including complex interaction terms that statistically capture relationships without mechanistic explanation [15].
The table below summarizes the fundamental distinctions between these approaches:
Table 1: Core Philosophical Differences Between Modeling Approaches
| Aspect | Hypothesis-Driven Modeling | Correlation-Based Modeling |
|---|---|---|
| Primary Goal | Explain underlying mechanisms | Predict outcomes accurately |
| Approach | Deductive (theory → model → data) | Inductive (data → model → patterns) |
| Parameter Interpretability | High (parameters map to biology) | Low (parameters often not interpretable) |
| Knowledge Source | Prior biological knowledge | Patterns in datasets |
| Validation Focus | Biological plausibility & predictive accuracy | Predictive accuracy & generalization |
| Causal Claims | Directly testable through model structure | Limited to association without experimentation |
The mathematical foundations further distinguish these approaches. Hypothesis-driven models often employ differential equations that embody biological mechanisms. For instance, ordinary differential equations can characterize tumor burden dynamics:
Table 2: Common Mathematical Frameworks in Tumor Modeling
| Model Type | Mathematical Formulation | Biological Interpretation |
|---|---|---|
| Exponential Growth | dT/dt = kg · T | Unconstrained growth with intrinsic rate kg |
| Logistic Growth | dT/dt = kg · T · (1 - T/Tmax) | Growth with carrying capacity Tmax |
| Gompertz Growth | dT/dt = kg · T · ln(Tmax/T) | Asymmetric growth deceleration |
| Two-Compartment | dP/dt = f(P) - m1 · P + m2 · QdQ/dt = m1 · P - m2 · Q | Distinguishes proliferative (P) and quiescent (Q) cells |
In contrast, correlation-based approaches utilize statistical learning methods. The relationship between model complexity and generalization capability illustrates a key consideration. As complexity increases (e.g., through higher-degree polynomial terms), models fit training data better but may fail to generalize to new data—a phenomenon known as overfitting [15]. Cross-validation techniques help identify the optimal complexity that balances fit and generalizability [15].
Diagram 1: Contrasting Modeling Workflows. This flowchart illustrates the divergent pathways for hypothesis-driven (red) and correlation-based (green) approaches, ultimately converging toward integrated modeling solutions.
Quantitative Comparison in Tumor Modeling Applications
Direct comparison of hypothesis-driven and correlation-based modeling approaches reveals significant differences in their performance characteristics, interpretability, and implementation requirements across various tumor modeling applications.
Table 3: Performance Comparison in Tumor Modeling Applications
| Characteristic | Hypothesis-Driven Models | Correlation-Based Models |
|---|---|---|
| Predictive Accuracy | Moderate to high for mechanisms within model scope | Potentially very high, especially for complex patterns |
| Extrapolation Reliability | High (principled extension of mechanisms) | Low (limited to training data domains) |
| Data Requirements | Lower (parameters can come from separate experiments) | Very high (large datasets needed for training) |
| Computational Demand | Variable (often moderate) | Typically high (especially for training) |
| Interpretability | High (mechanisms explicitly represented) | Low ("black box" problem) |
| Handling Novel Conditions | Strong (based on first principles) | Weak (requires retraining with new data) |
| Implementation Timeline | Longer (model development and validation) | Shorter (using established algorithms) |
The deGeco model for genomic compartments in Hi-C data exemplifies hypothesis-driven advantages, demonstrating high robustness and accurate inference of interaction probability maps from extremely sparse data without parameter training [16]. This approach enabled clear biological insights, including evidence of multiple chromatin states with different self-interaction affinities [16].
Correlation-based approaches face fundamental limitations in establishing causal relationships. The principle that "correlation does not imply causation" is particularly relevant in tumor modeling, where spurious correlations may lead to incorrect conclusions [17] [18]. For example, a correlation between a biomarker and tumor progression might result from a third, unmeasured variable rather than a direct causal relationship [18]. This limitation becomes particularly problematic in high-dimensional datasets where the "curse of dimensionality" increases the risk of finding spurious correlations by chance alone [17].
Experimental Protocols and Methodologies
Rigorous experimental protocols are essential for developing and validating both hypothesis-driven and correlation-based models in tumor research. The methodologies differ significantly between approaches.
Hypothesis-Driven Model Development Protocol
The development of hypothesis-driven models follows a systematic workflow with distinct stages:
Hypothesis Formulation: Precisely define the biological mechanism to be investigated, such as "cohesin-mediated loop extrusion explains TAD formation" or "hypoxia-driven angiogenesis follows a diffusion-limited process" [16].
Model Structural Design: Translate biological hypotheses into mathematical structures using appropriate formalisms. For tumor growth, this might involve selecting between ordinary differential equations (ODEs) for population dynamics, partial differential equations (PDEs) for spatial processes, or hybrid approaches [14]. The Bienenstock-Cooper-Munro (BCM) rule in neuroscience provides an exemplary case where a phenomenological model was later reproduced using mechanistic models with increasing biological detail [19].
Parameter Estimation: Determine parameter values through direct experimental measurement (e.g., proliferation rates from imaging data) or model calibration to experimental observations [20]. The deGeco model utilizes maximum likelihood estimation via optimization algorithms like L-BFGS-B to fit parameters to Hi-C interaction frequency data [16].
Model Validation: Test model predictions against independent datasets not used in parameter estimation. For example, a model predicting tumor response to a novel therapeutic combination should be validated against experimental results in animal models or clinical trial data [20].
Experimental Testing: Design targeted experiments to test specific model predictions and potentially falsify the underlying hypotheses. This iterative process refines both the model and biological understanding [21].
Correlation-Based Model Development Protocol
Correlation-based modeling employs a different methodological approach focused on pattern discovery:
Feature Selection: Identify which variables or features to include in the model. Correlation analysis helps remove redundant features (redundancy) and detect multicollinearity, which can undermine model stability [22]. Techniques like principal component analysis (PCA) may be used to reduce dimensionality while preserving predictive information [16] [22].
Algorithm Selection: Choose appropriate machine learning algorithms based on data characteristics and prediction goals. Options range from regression models for continuous outcomes to classification algorithms for categorical endpoints like treatment response versus resistance [22].
Training-Testing Split: Partition data into training sets for model development and validation sets for performance assessment. Cross-validation techniques, such as leave-one-out cross-validation (LOOCV), provide robust estimates of model generalizability [15].
Performance Metrics: Evaluate models using appropriate metrics including R-squared for variance explained, root mean square error (RMSE) for prediction accuracy, and area under the curve (AUC) for classification tasks [15].
Hyperparameter Tuning: Optimize model parameters that control the learning process rather than representing biological quantities. This typically involves systematic exploration of parameter spaces and validation against held-out data [15].
Diagram 2: Methodological Validation Pathways. The validation approaches differ fundamentally, with hypothesis-driven methods (red) testing mechanistic predictions, while correlation-based methods (green) focus on statistical generalizability.
Successful implementation of both modeling approaches requires specific computational tools, data resources, and methodological frameworks. The table below details essential components of the modern computational oncologist's toolkit.
Table 4: Essential Research Reagents and Computational Tools
| Tool/Resource | Function | Primary Modeling Approach |
|---|---|---|
| Medical Imaging (MRI/PET) | Provides spatial-temporal data on tumor anatomy, cellularity, perfusion, metabolism | Both (mechanistic initialization/feature source) |
| Hi-C Genomic Data | Measures genome-wide chromatin interaction frequencies | Hypothesis-driven (genomic compartment modeling) |
| Single-Cell Sequencing | Resolves intratumor heterogeneity and cell population dynamics | Both (mechanism refinement/feature identification) |
| Ordinary Differential Equations (ODEs) | Models population dynamics and treatment responses | Hypothesis-driven |
| Partial Differential Equations (PDEs) | Captures spatial invasion and microenvironment interactions | Hypothesis-driven |
| Principal Component Analysis (PCA) | Identifies dominant patterns in high-dimensional data | Correlation-based (also used in hypothesis-driven) |
| Cross-Validation Methods | Estimates model generalizability to new data | Correlation-based |
| FAIR Data Principles | Ensures findability, accessibility, interoperability, reusability | Both (enhances reproducibility and integration) |
Medical imaging technologies particularly MRI and PET represent crucial data sources for both approaches, providing non-invasive, spatially-resolved measurements of tumor biology including cellularity (via DW-MRI), vascularity (via DCE-MRI), and metabolism (via FDG-PET) [20]. These imaging modalities can initialize mechanistic models or serve as feature sources for correlation-based approaches.
The FAIR (Findable, Accessible, Interoperable, Reusable) principles have emerged as critical guidelines for both data and model management, supporting integration across modeling philosophies and biological scales [19]. Applying these principles to models and modeling workflows increases transparency, enables validation, and facilitates model reuse and extension [19].
Integrated Approaches and Future Directions
The dichotomy between hypothesis-driven and correlation-based modeling represents a false choice when considering advanced cancer modeling approaches. The most promising future direction lies in integrated methodologies that leverage the strengths of both philosophies while mitigating their respective limitations.
Hybrid approaches are increasingly emerging, where machine learning methods help parameterize mechanistic models or generate hypotheses from complex data, while mechanistic insights constrain and regularize data-driven models to enhance biological plausibility [20] [19]. For example, AI can relate large quantities of 'omic' data to mechanistic model parameters, reducing computational burden or parsing mechanistic model forecasts to select optimal therapies [20]. Similarly, the deGeco model represents a generative probabilistic approach that incorporates both hypothesis-driven mechanistic assumptions and data-driven parameter inference [16].
The FAIR principles provide a framework for this integration by making both models and data findable, accessible, interoperable, and reusable [19]. This enables researchers to combine models representing different biological scales and built using different modeling philosophies, ultimately enhancing our understanding of multiscale cancer phenomena [19]. Integrated workflows might use correlation-based approaches to identify novel patterns in high-dimensional data, then employ hypothesis-driven modeling to explain these patterns through testable biological mechanisms, creating a virtuous cycle of discovery and validation.
For drug development professionals, this integration offers a path toward models that are both predictively accurate and mechanistically interpretable—critical requirements for regulatory acceptance and clinical implementation. As these approaches mature, they promise to accelerate the development of personalized cancer therapies guided by predicted patient response rather than observed outcomes, potentially dramatically improving patient outcomes [20].
The field of computational oncology is increasingly divided between two powerful, yet philosophically distinct, modeling approaches: mechanistic models rooted in biological first principles and data-driven artificial intelligence (AI) models that learn patterns from complex datasets. The selection and initialization of these models are fundamentally guided by the available data types, each with unique strengths and limitations for capturing tumor biology. This guide provides a comparative analysis of three cornerstone data categories—medical imaging, genomics, and clinical records—examining their respective roles in initializing and informing both mechanistic and AI-based modeling paradigms. By objectively evaluating their applications, technical requirements, and performance across experimental settings, we aim to equip researchers with the knowledge to make informed decisions in model selection and development for precision oncology.
Comparative Analysis of Key Data Types
The table below summarizes the core characteristics, applications, and challenges of the three primary data types used in computational oncology.
Table 1: Comparison of Key Data Types for Tumor Model Initialization
| Data Type | Key Subtypes & Sources | Primary Modeling Applications | Technical & Practical Considerations |
|---|---|---|---|
| Medical Imaging [23] [20] | - Anatomic: CT, MRI- Physiologic/Molecular: DWI-MRI, DCE-MRI, FDG-PET- Digital Pathology: Whole-slide images (WSI) | - Tumor growth models [20]- Radiogenomics (linking features to genomics) [23]- AI-based segmentation & diagnosis [1] | - Spatial Resolution: 1-5 mm (clinical); sub-millimeter (microscopy) [20]- Challenges: Standardization of feature extraction; domain shift in digital pathology [23] [20] |
| Genomics [23] [24] [25] | - DNA-level: Somatic mutations, Copy Number Alterations (CNAs), Structural Variants (SVs) from WGS/WES/targeted panels [26] [25]- RNA-level: Gene expression (mRNA-seq) [25]- Epigenomics: DNA methylation [25] | - Molecular subtyping and classification [26] [1]- Predicting variant pathogenicity and drug response [24]- Informing mechanistic pathways | - Panel vs. WGS/WES: Targeted panels (e.g., MSK-IMPACT) are clinically scalable; WGS/WES are more comprehensive but costly [26]- Challenges: Distinguishing driver from passenger mutations; data interpretation [24] |
| Clinical Records [27] [28] [29] | - Demographics: Age, sex [29]- Lifestyle/Behavioral: Smoking status, BMI [29]- Medical History: Comorbidities, family history [29]- Longitudinal EHR Data: Diagnoses, medications, lab results [28] | - Survival and time-to-event analysis [29]- Population health and risk stratification [24]- Augmenting omics analyses via transfer learning [28] | - Data Structure: Often requires mapping and harmonization from heterogeneous EHR systems [27] [29]- Bias: Can reflect hospital-entry bias and lack population representativeness [24] |
Experimental Protocols and Performance Data
Protocol 1: AI for Tumor-Type Classification from Genomic Data
The OncoChat study demonstrates the application of a large language model (LLM) to classify tumor types using genomic alterations [26].
- Objective: To accurately classify 69 different tumor types, including Cancers of Unknown Primary (CUP), based on genomic features.
- Data Initialization:
- Source: American Association for Cancer Research (AACR) Project GENIE consortium.
- Sample Size: 163,585 targeted panel sequencing samples.
- Genomic Features: Single-nucleotide variants (SNVs), copy number alterations (CNAs), and structural variants (SVs) were preprocessed into a dialogue format suitable for LLM instruction-tuning.
- Modeling Approach: The OncoChat model was developed by fine-tuning a foundational LLM on the formatted genomic data from 158,836 samples with known primaries (CKP).
- Performance Metrics [26]:
- On a test set of 19,940 CKP cases, OncoChat achieved an accuracy of 0.774 and an F1 score of 0.756.
- It outperformed existing models like OncoNPC (accuracy: 0.718) and GDD-ENS (accuracy: 0.616).
- For CUP classification, the model correctly identified 22 out of 26 cases (84.6%) with subsequently confirmed tumor types.
Protocol 2: Integrating EHR and Omics via Transfer Learning
The COMET framework leverages large-scale Electronic Health Record (EHR) data to enhance the analysis of smaller omics datasets [28].
- Objective: To improve predictive modeling from high-dimensional omics data (e.g., proteomics) by pretraining on larger, related EHR datasets.
- Data Initialization:
- EHR Pretraining Cohort: 30,843 pregnant patients from Stanford STARR OMOP database.
- Omics Cohort: A subset of 61 patients with targeted proteomics data (1,317 proteins) from serial blood samples.
- Modeling Approach:
- Step 1: A model was pretrained on the large EHR-only cohort to predict "days to labour."
- Step 2: The learned weights were transferred to a multimodal network that integrated both EHR and proteomics data from the smaller omics cohort.
- Performance Metrics [28]:
- COMET achieved a strong Pearson correlation (r = 0.868) between predicted and actual days to labour, significantly outperforming baselines.
- Baseline Comparisons:
- EHR-only baseline: r = 0.768
- Proteomics-only baseline: r = 0.796
- Joint baseline (without pretraining): r = 0.815
Protocol 3: Predicting Time-to-Cancer Diagnosis with Clinical Data
This study used traditional survival analysis and machine learning on clinical and demographic data to predict cancer risk [29].
- Objective: To develop and validate models for predicting the time to first diagnosis for several high-incidence cancers.
- Data Initialization:
- Training Data: 141,979 participants from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial.
- Validation Data: 287,150 participants from the UK Biobank (UKBB).
- Features: 46 sex-agnostic features, including demographics, clinical history, and behavioral data.
- Modeling Approach: Cox proportional hazards model with elastic net regularization was compared against non-parametric methods like survival decision trees and random survival forests.
- Performance Metrics [29]:
- The Cox model achieved a C-index of 0.813 for lung cancer prediction.
- Cancer-specific models consistently outperformed non-specific cancer models.
- The model provided interpretable insights, such as an inverse association between BMI and lung cancer risk.
Workflow Visualization
The following diagram illustrates a synergistic workflow that integrates multiple data types to inform both AI and mechanistic modeling paradigms, leveraging the strengths of each approach.
The table below lists key datasets, platforms, and tools that form the foundation of modern computational oncology research.
Table 2: Key Research Reagents and Resources for Computational Oncology
| Resource Name | Type / Category | Primary Function in Research | Relevant Citation |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) | Comprehensive Database | Provides a vast, multi-platform collection of genomic, epigenomic, transcriptomic, and proteomic data from over 20,000 cancer and normal samples, serving as a benchmark for model development and validation. | [25] |
| AACR Project GENIE | International Registry | An open-source cancer registry of real-world clinical genomic data from multiple institutions, enabling the development of tools like OncoChat on large, clinically heterogeneous datasets. | [26] |
| PyRadiomics | Software Platform | A flexible open-source platform for the extraction of a large set of handcrafted radiomics features from medical images, standardizing quantitative imaging analysis. | [23] |
| UK Biobank (UKBB) | Biobank / Cohort | A large-scale prospective cohort with deep genetic, phenotypic, and health record data, invaluable for longitudinal studies and external model validation. | [28] [29] |
| ClinVar | Clinical Genomics Database | A public archive of reports detailing the relationships between human genetic variations and phenotypic support, used for interpreting variant pathogenicity. | [24] |
| COMET Framework | Computational Method | A machine learning framework that uses transfer learning from large EHR databases to improve the analysis of smaller, high-dimensional omics datasets. | [28] |
| Core Variables (~150) | Data Standardization | A harmonized list of key clinicogenomic data elements defined by experts to ensure fit-for-purpose data collection and interoperability across precision oncology studies. | [27] |
Operational Frameworks and Translational Applications in Oncology
In the evolving landscape of cancer research, computational models have emerged as indispensable tools for understanding tumor dynamics and predicting treatment outcomes. Two predominant paradigms have shaped this field: mechanistic models grounded in biological first principles and data-driven artificial intelligence (AI) approaches that identify patterns from large datasets. Mechanistic models employ mathematical formulations to represent known or hypothesized biological processes, creating dynamic simulations of tumor initiation, growth, invasion, and response to therapeutic interventions [20]. These models are characterized by their foundation in biological mechanisms, dynamic representation of tumor processes over time, and mathematical formalisms that often employ ordinary differential equations (ODEs) or partial differential equations (PDEs) to capture system dynamics [30].
In contrast, AI and machine learning approaches leverage statistical pattern recognition on vast datasets to make predictions without necessarily embodying underlying biological mechanisms [31]. While AI has demonstrated remarkable success in diagnostic imaging and pattern classification, its "black box" nature often limits biological interpretability [32]. The ultimate goal of both approaches is to enable personalized cancer therapy by predicting individual patient responses to specific treatments, potentially avoiding ineffective therapies and their associated toxicities [20]. This review systematically compares these methodological frameworks, examining their respective strengths, limitations, and emerging hybrid approaches that seek to leverage the advantages of both paradigms.
Comparative Analysis: Mechanistic Models vs. AI in Tumor Modeling
Table 1: Fundamental characteristics of mechanistic versus AI approaches in tumor modeling
| Feature | Mechanistic Models | AI/Machine Learning |
|---|---|---|
| Theoretical Foundation | Biological first principles, mathematical representations of known mechanisms | Statistical pattern recognition, neural networks |
| Data Requirements | Lower volume, but requires specific parameter measurements | Very large datasets for training |
| Interpretability | High - parameters typically have biological meaning | Low - often "black box" predictions |
| Temporal Dynamics | Explicitly modeled through differential equations | Learned from longitudinal data |
| Personalization Approach | Parameter calibration using patient-specific data | Pattern matching to similar cases in training set |
| Extrapolation Capability | Strong - can predict responses outside training conditions | Limited - primarily interpolative within training distribution |
| Clinical Integration Challenges | Parameter identifiability, model complexity | Generalizability, explainability, data hunger |
Performance Comparison in Clinical Prediction Tasks
Table 2: Quantitative performance comparison across modeling approaches
| Application Context | Model Type | Performance Metric | Result | Reference |
|---|---|---|---|---|
| Overall Survival Prediction (HCC) | StepCox (forward) + Ridge (AI) | Concordance Index | 0.68 (training), 0.65 (validation) | [11] |
| Immunotherapy Response (NSCLC) | MUSK (Multimodal AI) | Prediction Accuracy | 77% | [33] |
| Immunotherapy Response (NSCLC) | PD-L1 biomarker (Standard) | Prediction Accuracy | 61% | [33] |
| Brain Tumor Segmentation | CNN-based AI | Diagnostic accuracy | Varies by architecture | [32] |
| Melanoma Recurrence Prediction | MUSK (Multimodal AI) | Prediction Accuracy | 83% | [33] |
| Tumor Growth Prediction | ODE-based mechanistic | Spatial accuracy | Hausdorff Distance metrics | [34] |
Experimental Protocols and Methodologies
ODE-Based Mechanistic Modeling of Tumor Growth
Mechanistic models of tumor growth typically employ ordinary differential equations to capture population dynamics of cancer cells and their interactions with treatments. The fundamental experimental protocol involves:
Model Formulation: Researchers define the biological system using ODEs that represent tumor cell proliferation, death, and interaction with therapies. For instance, the exponential growth model is formulated as:
dA/dt = λA
where A represents tumor size and λ is the net growth rate [30]. More sophisticated models incorporate treatment effects, such as radiotherapy response models that partition tumor cells into surviving (A~l~) and dying (A~d~) fractions post-treatment [34]:
A~l~(t~RTstart~) = S · A(t~RTstart~)
A~d~(t~RTstart~) = (1 - S) · A(t~RTstart~)
Parameter Estimation: Using longitudinal patient data (often from medical imaging), researchers calibrate model parameters to individual patients. This typically involves optimization algorithms to minimize the difference between model predictions and observed tumor measurements [30].
Validation: The calibrated model is used to predict future tumor states, which are compared against actual follow-up measurements to assess predictive accuracy. Performance metrics may include Hausdorff Distance for spatial predictions or concordance indices for survival outcomes [34].
AI Model Training and Validation Protocols
AI approaches follow distinct experimental protocols centered on data preparation and model training:
Data Curation: Large datasets comprising medical images, clinical notes, molecular data, and outcome measures are assembled. For example, the MUSK model was trained on 50 million medical images and over 1 billion pathology-related texts [33].
Model Architecture Selection: Researchers choose appropriate neural network architectures (CNNs for images, transformers for multimodal data, etc.) based on the prediction task [32].
Training and Fine-tuning: Models are trained on labeled data, with careful separation of training, validation, and test sets to prevent overfitting. Foundation models like MUSK employ pretraining on broad datasets followed by task-specific fine-tuning [33].
Performance Assessment: Models are evaluated using metrics appropriate to the clinical question (e.g., AUC-ROC for classification tasks, C-index for survival prediction, accuracy for response prediction) [11] [33].
Hybrid Approaches: Integrating Mechanistic and AI Frameworks
Mechanistic Learning with Guided Diffusion Models
Recent research has explored hybrid frameworks that combine the strengths of both approaches. One promising methodology integrates mechanistic ODE models with guided denoising diffusion implicit models (DDIM) for spatio-temporal prediction of brain tumor growth [34].
In this approach, a mechanistic ODE model first captures temporal tumor dynamics and estimates future tumor burden. These estimates then condition a gradient-guided DDIM, enabling synthetic MRI generation that aligns with both predicted growth and patient anatomy. The experimental workflow proceeds as follows:
- Mechanistic Modeling: A compartmental ODE model simulates tumor growth dynamics, incorporating radiotherapy effects when applicable
- Tumor Burden Prediction: The model generates quantitative estimates of future tumor size
- Image Synthesis: A guided diffusion model generates synthetic follow-up MRIs that reflect the predicted tumor burden while maintaining anatomical realism
This hybrid approach addresses a key limitation of pure mechanistic models—their compression of spatial complexity—while providing the biological grounding that pure AI approaches lack [34]. The framework demonstrates particular utility in data-scarce scenarios, such as modeling rare cancers where large training datasets are unavailable.
Multimodal Data Integration Frameworks
Another hybrid approach leverages AI's strength in processing diverse data types while maintaining mechanistic interpretability. The MUSK model exemplifies this strategy by integrating pathology images, clinical notes, and molecular data to predict cancer prognoses and treatment responses [33].
This model architecture employs transformer networks capable of processing both visual and language-based information, creating a unified representation that captures complementary information across data modalities. The model demonstrated superior performance compared to single-modality approaches across multiple cancer types, highlighting the value of integrated data analysis [33].
Table 3: Essential research reagents and computational tools for tumor modeling
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Mathematical Modeling Frameworks | ODE systems (Exponential, Logistic, Gompertz) [30] | Representing intrinsic tumor growth dynamics |
| Medical Imaging Data | MRI (T1, T2, T1-CE, FLAIR sequences) [32] [34] | Model initialization and validation |
| Specialized Imaging Techniques | DCE-MRI, DW-MRI, PET with various tracers [20] | Measuring cellularity, perfusion, hypoxia, metabolism |
| Computational Tools | STRIKE-GOLDD toolbox [30] | Structural identifiability and observability analysis |
| AI Architectures | CNNs, Transformers, DDIM [32] [34] [33] | Image analysis, multimodal learning, synthetic data generation |
| Fluorescent Protein Tags | GFP, RFP variants [35] | In vivo cell tracking and visualization of metastasis |
| Molecular Data Sources | Genomic, transcriptomic, proteomic data [36] | Model personalization and biomarker discovery |
Critical Methodological Considerations
Structural Identifiability and Observability Analysis
A fundamental challenge in mechanistic modeling is ensuring that model parameters can be reliably estimated from available data. Structural identifiability analysis determines whether it is theoretically possible to uniquely determine parameter values from ideal noise-free data, while observability analysis assesses the ability to infer internal state variables from output measurements [30].
Recent research has systematically analyzed these properties for 20 published tumor growth models, revealing that many models face identifiability issues that can compromise their predictive accuracy [30]. This highlights the importance of conducting such analyses during model development and selecting models with appropriate identifiability properties for specific applications.
Data Requirements and Domain Adaptation
Both mechanistic and AI approaches face data-related challenges. Mechanistic models require specific parameter measurements that may be difficult to obtain in clinical settings, while AI models demand large, diverse datasets that adequately represent the patient population [20].
Domain adaptation presents particular challenges, as models trained on data from one institution may perform poorly on data from another due to differences in imaging protocols, staining techniques, or patient populations [32] [20]. Emerging approaches such as federated learning and domain-adversarial training aim to address these limitations but remain active research areas.
The comparison between mechanistic models and AI approaches in tumor modeling reveals complementary strengths that are increasingly being leveraged through hybrid frameworks. Mechanistic models provide biological interpretability and reliable extrapolation, while AI offers powerful pattern recognition capabilities, especially on complex, high-dimensional data. The integration of these paradigms—through approaches such as mechanistic learning with diffusion models or multimodal foundation models—represents the most promising direction for advancing predictive accuracy in clinical applications.
Future research should focus on enhancing model personalization through improved parameter estimation techniques, developing more sophisticated hybrid architectures, and addressing ethical considerations around clinical implementation. As both modeling paradigms continue to evolve, their thoughtful integration holds significant potential for transforming cancer care through truly personalized treatment optimization.
The field of tumor modeling has long been dominated by mechanistic models, which are based on predefined biological principles and mathematical representations of known cancer pathways. While these models provide valuable interpretability, they struggle to capture the full complexity and heterogeneity of cancer biology. In recent years, artificial intelligence and machine learning (AI/ML) have emerged as powerful alternatives that can learn directly from complex medical data without requiring explicit programming of all underlying biological rules [37] [38]. This paradigm shift is particularly evident in cancer diagnosis, where AI/ML systems are demonstrating remarkable capabilities in detecting malignancies across both radiological and pathological domains.
The fundamental distinction between these approaches lies in their core operating principles. Mechanistic models are hypothesis-driven, built upon established knowledge of tumorigenesis, while AI/ML systems are data-driven, discovering patterns directly from imaging and molecular data [37]. This comparison guide objectively evaluates the performance of contemporary AI/ML technologies against traditional methods and each other, providing researchers and drug development professionals with experimental data to inform their diagnostic and research strategies.
Performance Comparison: AI/ML Technologies in Cancer Diagnosis
Diagnostic Accuracy Across Cancer Types
Table 1: Performance metrics of AI/ML systems across different cancer types
| Cancer Type | AI Technology | Sensitivity | Specificity | AUC | Comparative Performance |
|---|---|---|---|---|---|
| Early Gastric Cancer | Deep Convolutional Neural Network (DCNN) | 0.94 [39] | 0.91 [39] | 0.96-0.98 [39] | Superior to traditional CNN (Sensitivity: 0.89) [39] |
| Colorectal Cancer | CRCNet (DL model) | High (Study-specific values not reported) | High (Study-specific values not reported) | High performance across 3 datasets [10] | Achieves endoscopic detection with approximately 90% accuracy [10] |
| Breast Cancer | AI System (McKinney et al.) | Not specified | Not specified | Outperformed radiologists in clinically relevant task [10] | Generalizes from UK training data to US clinical site testing [10] |
| Lung Cancer | Convolutional Neural Network | Not specified | Not specified | 0.93 [40] | Comparable to thoracic radiologists for nodule malignancy risk assessment [40] |
| Cutaneous Melanoma | Multimodal AI (CNNs + GNNs) | High predictive accuracy | High predictive accuracy | Superior to clinical staging [41] | Particularly strong in early-stage cases where traditional stratification fails [41] |
Comparison of AI Architectures in Radiology and Pathology
Table 2: Technical comparison of major AI approaches in cancer imaging
| Characteristic | Machine Learning with Radiomics | Deep Learning | Large Models |
|---|---|---|---|
| Data Requirement | Moderate [40] | Adequate [40] | Enormous [40] |
| Hardware Requirement | Moderate [40] | High [40] | Very High [40] |
| Feature Extraction | Predefined mathematical features [40] | Learned automatically [40] | Learned automatically [40] |
| Performance | Moderate [40] | High [40] | Very High [40] |
| Explainability | Good (Interpretable features) [40] | Poor ("Black box" characteristics) [40] | Poor (Complex decision process) [40] |
| Annotation Needs | Manual delineation required [40] | Flexible annotation [40] | Flexible annotation [40] |
Experimental Protocols and Methodologies
Protocol for AI-Assisted Early Gastric Cancer Detection
A recent systematic review and meta-analysis evaluated AI model performance for early gastric cancer (EGC) detection through rigorous methodology [39]. The protocol involved:
Data Collection and Inclusion Criteria: Researchers systematically searched PubMed, Embase, Web of Science, Cochrane Library, and China National Knowledge Infrastructure databases through January 2025 [39]. Inclusion required studies to evaluate AI accuracy in EGC diagnosis using endoscopic images/videos as input data with histopathological confirmation as the gold standard [39].
Statistical Analysis: Data extraction followed PRISMA guidelines, with two independent reviewers extracting study characteristics using a pre-designed form [39]. Sensitivity and specificity were pooled using a bivariate random effects model, with subgroup analysis by AI model type [39]. Heterogeneity was assessed using I² statistics, and publication bias was evaluated with funnel plots and Egger's test [39].
Validation Approach: The analysis included 26 studies with 43,088 patients total [39]. Performance was validated through dynamic video verification, where AI models achieved an AUC of 0.98, significantly outperforming clinician levels (AUC 0.85-0.90) [39].
Protocol for Multimodal Melanoma Metastasis Prediction
A groundbreaking 2025 study developed a multimodal AI system for predicting metastasis in cutaneous melanoma through sophisticated computational integration [41]:
Data Integration Framework: The research team employed deep learning techniques to process whole-slide histopathological images, concurrently integrating molecular data that provided gene expression patterns and protein markers [41]. Spatial analyses captured distribution and interaction networks of immune and stromal cell populations within the tumor niche [41].
Architecture Design: The system utilized convolutional neural networks (CNNs) tailored for histopathological image analysis combined with graph neural networks (GNNs) that model cellular interactions within tissue architecture [41]. CNNs identified subtle architectural cues associated with aggressive behavior, while GNNs mapped spatial proximity and communication pathways among cells [41].
Validation Methodology: Researchers assembled an extensive dataset comprising digital pathology slides and corresponding molecular data from hundreds of melanoma patients with long-term follow-up on metastatic outcomes [41]. The model underwent cross-validation and testing on independent cohorts, with particular attention to early-stage cases where traditional risk stratification is challenging [41].
Protocol for Radiomics-Based Treatment Response Prediction
Multiple studies have established standardized methodologies for developing radiomics-based predictive models:
Feature Extraction and Selection: The radiomics workflow begins with extracting predefined features from radiological images through data characterization algorithms [40]. These features capture various aspects of tumoral patterns, including intensity-based metrics, texture, shape, peritumoral characteristics, and tumor heterogeneity [40]. Feature selection refines a broad array of features to a task-specific subset to enhance predictive accuracy and minimize redundancy [40].
Model Development and Validation: Selected features are fed into machine learning models such as logistic regression or random forest for outcome prediction [40]. For example, Colen et al. created an XGBoost model with radiomics to predict pembrolizumab response in patients with advanced rare cancers, applying least absolute shrinkage and selection operator for feature selection on pretreatment CT scans [40]. The model achieved 94.7% accuracy when assessed according to RECIST criteria [40].
Multimodal Integration: Advanced approaches integrate radiomic features with complementary data types. Vanguri et al. built a multimodal deep learning model assessing immunotherapy response by integrating CT imaging, histopathologic, and genomic features from patients with advanced non-small cell lung cancer [40]. This integrated approach achieved an AUC of 0.80 and outperformed unimodal models [40].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key research reagents and computational tools for AI/ML cancer diagnosis research
| Tool/Reagent | Function | Application Example |
|---|---|---|
| Deep Convolutional Neural Networks (DCNN) | Advanced image analysis with hierarchical feature extraction [39] | Early gastric cancer detection in endoscopic images [39] |
| Graph Neural Networks (GNNs) | Modeling cellular interactions and spatial relationships within tissue [41] | Mapping immune and tumor cell communication in melanoma [41] |
| Radiomics Feature Extraction Platforms | Quantifying tumor characteristics from medical images [40] | Predicting treatment response in rare cancers [40] |
| Whole-Slide Imaging Systems | Digitizing pathology slides for computational analysis [41] | Creating digital pathology datasets for melanoma metastasis prediction [41] |
| Multimodal Data Fusion Frameworks | Integrating diverse data types (imaging, molecular, spatial) [41] | Combining histopathology with molecular profiling for metastatic risk assessment [41] |
| Interpretability Tools (Grad-CAM, SHAP) | Visualizing and explaining AI decision-making [40] | Highlighting image regions significant for thyroid nodule classification [40] |
Critical Analysis: Performance Limitations and Implementation Challenges
Despite promising performance metrics, AI/ML technologies face significant implementation challenges that must be addressed for widespread clinical adoption.
Technical and Clinical Limitations
The "black box" nature of many AI systems remains a fundamental barrier. Unlike mechanistic models with transparent reasoning processes, deep learning and large models provide limited explanation for their decision-making [42] [40]. This opacity complicates clinical trust and validation, particularly for high-stakes diagnostic decisions [42]. Techniques such as Grad-CAM and SHAP provide some interpretability by highlighting regions contributing to predictions, but full transparency remains elusive [40].
Data quality and diversity present another substantial challenge. AI models require large, high-quality datasets for training, but real-world clinical data often suffers from variability in imaging parameters, population characteristics, and annotation consistency [43] [40]. This frequently leads to performance degradation when models are applied to external datasets from diverse sources [40]. For example, while CADe systems for colorectal polyp detection demonstrate increased adenoma detection in randomized trials, they have not consistently improved identification of advanced colorectal neoplasias in screening programs [10].
Integration and Workflow Considerations
Successful implementation requires seamless integration into existing clinical workflows, which poses both technical and human-factor challenges [44] [41]. The "Third Wheel Effect" describes patient perception of AI as an unnecessary intrusion rather than a valuable addition, potentially undermining doctor-patient relationships [44]. Furthermore, inadequate communication about AI's benefits may exacerbate patient mistrust of AI-aided diagnoses [44].
Resource requirements also vary significantly between approaches. While radiomics-based machine learning has moderate data and hardware needs, deep learning requires adequate resources, and large models demand enormous computational infrastructure [40]. These practical considerations directly impact accessibility and implementation across healthcare settings with varying resources.
Future Directions and Clinical Translation
The evolving landscape of AI/ML in cancer diagnosis points toward several critical developments that will shape future research and clinical implementation.
Explainable AI and Multimodal Integration
Enhancing model interpretability remains a priority for clinical translation. Explainable AI (XAI) approaches are attracting increasing interest as mechanisms to provide patient-friendly explanations of biomedical decisions based on machine learning [44]. This transparency is particularly crucial in oncology, where diagnostic decisions carry significant psychological and emotional implications for patients [44].
Multimodal approaches that integrate diverse data types represent another promising direction. The success of systems combining histopathological images with molecular profiling and spatial data demonstrates the potential of synthesizing complementary information sources [41]. This methodology can reveal previously underappreciated tumor microenvironment components that drive cancer progression while improving predictive accuracy [41].
Validation Frameworks and Clinical Workflow Integration
Future progress requires robust validation frameworks assessing AI performance across diverse populations and clinical settings [39] [41]. Multicenter prospective validation will be essential to establish generalizability and address performance variability across different patient demographics and healthcare systems [39]. Additionally, research should focus on developing standardized protocols for data acquisition, computational infrastructure, and clinician training to bridge the gap between technological innovation and practical healthcare impact [41].
The most successful implementations will likely adopt a hybrid approach that leverages the strengths of both AI/ML and human expertise. Rather than positioning AI as a replacement for clinicians, the optimal framework integrates AI assistance within clinical decision-making processes, enhancing diagnostic accuracy while maintaining physician oversight and patient-centered care [44] [40].
The challenge of predicting patient-specific responses to cancer therapy represents a central frontier in precision oncology. In addressing this challenge, the research community has diverged into two complementary computational philosophies: mechanistic modeling and artificial intelligence/machine learning (AI/ML) approaches. Mechanistic models are grounded in established biological principles, constructing mathematical representations of known tumor dynamics, such as cell cycle progression, drug pharmacokinetics, and tumor-immune interactions. Conversely, AI/ML models are data-driven, discovering complex patterns directly from clinical, genomic, and imaging datasets without pre-specified biological rules. This guide objectively compares the performance of representative tools from both paradigms, examining their experimental validation, methodological frameworks, and applicability to chemotherapy and immunotherapy response prediction.
AI/Machine Learning Tools for Response Prediction
AI/ML tools have demonstrated remarkable progress in predicting therapy response by leveraging large-scale multimodal patient data. The table below compares several leading AI approaches.
Table 1: Comparison of AI/ML Tools for Predicting Therapy Response
| Tool Name | Model Type | Input Data | Cancer Types Validated | Reported Performance | Key Advantage |
|---|---|---|---|---|---|
| SCORPIO [45] | AI (Machine Learning) | Routine blood tests, clinical data (age, sex, BMI) | 21 types (inc. melanoma, lung, bladder, liver, kidney) | 72-76% accuracy for survival prediction over 2.5 years; outperformed TMB | Uses low-cost, routine data; avoids expensive genomic tests |
| Compass [46] | AI (Foundation Model with Concept Bottleneck) | Pan-cancer transcriptomic data | 33 cancer types, validated across 7 cancers and 6 ICIs | Increased precision by 8.5%, MCC by 12.3%, AUPRC by 15.7% vs. baselines | High generalizability to unseen cancers/treatments; provides mechanistic insights |
| Lunit SCOPE IO [47] | AI (Deep Learning on Pathology Images) | Pre-treatment histology slides (H&E stains) | Colorectal cancer (pMMR mCRC), kidney cancer (ccRCC), NSCLC | Identified "inflamed" phenotypes with significantly longer PFS & OS (e.g., response rate 60.5% vs 23.2% in ccRCC) | Leverages standard pathology slides; identifies immune phenotypes |
| AI-Assisted PET Imaging [48] | AI (Radiomics/Deep Learning) | PET imaging data | Breast Cancer (NAC response) | Pooled AUC of 0.80 (95% CI: 0.77-0.84) in meta-analysis | Non-invasive; uses standard-of-care imaging |
Experimental Protocols and Workflows
The performance data in Table 1 is derived from rigorous experimental designs. Below are the core methodologies for the key tools.
SCORPIO Experimental Protocol [45]:
- Objective: To predict survival and tumor response following immune checkpoint inhibitor (ICI) treatment using only routine clinical and blood test data.
- Training Cohort: Data from ~2,000 patients treated at Memorial Sloan Kettering Cancer Center.
- Input Features: Age, sex, body mass index, and measurements from standard blood panels.
- Validation: Tested on several independent validation sets, including real-world cohorts and 10 clinical trials, totaling nearly 10,000 patients.
- Output: A prediction of likelihood of survival and tumor shrinkage.
Compass Experimental Protocol [46]:
- Objective: To build a generalizable foundation model for predicting immunotherapy response from tumor transcriptomic data.
- Training Data: 10,184 tumors across 33 cancer types.
- Model Architecture: A concept bottleneck model that encodes tumor gene expression through 44 biologically grounded immune concepts (e.g., immune cell states, signaling pathways).
- Validation: Performance was evaluated against 22 baseline methods in 16 independent clinical cohorts spanning seven cancers and six ICIs.
- Output: A response prediction, along with a "personalized response map" that links gene expression to immune concepts to explain the prediction.
Lunit SCOPE IO Experimental Protocol [47]:
- Objective: To use AI for analyzing digitized histology slides to predict response to immunotherapy.
- Input: Pre-treatment H&E-stained tissue slides are digitized into whole-slide images.
- AI Analysis: A deep learning algorithm analyzes the tumor microenvironment, quantifying and spatially characterizing tumor-infiltrating lymphocytes (TILs).
- Output Classification: Tumors are classified as "inflamed" (TILs present within the tumor) or "non-inflamed" (TILs excluded). The "inflamed" phenotype is associated with a higher probability of response to ICIs.
- Validation: Demonstrated in multiple studies, including the AtezoTRIBE trial in metastatic colorectal cancer, where "biomarker-high" patients showed significantly improved progression-free and overall survival.
AI Pathology Analysis Workflow
Mechanistic Modeling Approaches
In contrast to data-driven AI, mechanistic models simulate tumor biology based on predefined mathematical representations of underlying physiological processes. These models are particularly valuable for optimizing treatment scheduling and understanding resistance mechanisms.
Table 2: Comparison of Mechanistic Modeling Approaches
| Model Category | Core Principle | Typical Input Data | Key Outputs | Application in Therapy Prediction |
|---|---|---|---|---|
| Cell Cycle-Based Pharmacodynamic Models [49] | Models drug effects on specific cell cycle phases (G1, S, G2, M) | Cell cycle parameters, drug mechanism of action | Prediction of optimal scheduling for cell cycle-specific chemotherapies | Mitigates resistance by targeting heterogeneous cell populations |
| Tumor Growth & Treatment Response Models [20] | Physics-informed equations describing tumor volume change under therapy | Longitudinal medical imaging (MRI, PET), patient-specific pathophysiology | Simulated tumor response to different drug doses/combinations; in-silico treatment optimization | Personalizes dosing regimens; forecasts long-term response |
| Tumor-Immune Interaction Models [20] | Systems of equations modeling interactions between tumor cells, immune cells, and drugs | Immune cell densities, cytokine concentrations, tumor doubling time | Predicts synergy for immunotherapy combinations; simulates irAEs | Identifies patients likely to benefit from ICIs; optimizes combo therapies |
Experimental Protocols in Mechanistic Modeling
Mechanistic models are built and validated through a distinct process that heavily relies on patient-specific data for calibration.
Protocol for Imaging-Informed Tumor Growth Models [20]:
- Step 1: Data Acquisition. Acquire longitudinal, quantitative medical imaging (e.g., DW-MRI for cellularity, DCE-MRI for perfusion) before and during treatment.
- Step 2: Model Selection. Choose a mathematical framework (e.g., reaction-diffusion equations) that incorporates key biological processes like proliferation, invasion, and cell death.
- Step 3: Parameter Calibration. Initialize the model with patient-specific anatomical data from baseline scans. Use early follow-up scans to calibrate the model's biophysical parameters (e.g., proliferation rate, diffusion coefficient) for that specific patient.
- Step 4: Prediction and Validation. The calibrated model is run forward in time to predict future tumor response to a continued or alternative therapy. Predictions are then compared against actual future scans to validate the model's accuracy.
Protocol for Cell Cycle-Targeted Therapy Optimization [49]:
- Step 1: Model the Network. Construct a system of ordinary differential equations (ODEs) representing the core regulatory network of the cell cycle (CDKs, cyclins, checkpoints).
- Step 2: Incorporate Drug Mechanism. Introduce terms that represent the inhibitory action of a specific chemotherapeutic drug (e.g., a CDK4/6 inhibitor) on its target within the network.
- Step 3: Simulate Treatment Schedules. Run simulations using different dosing schedules (e.g., continuous vs. pulsatile).
- Step 4: Identify Optimal Strategy. Analyze simulation outputs to identify schedules that maximize tumor cell kill while minimizing the emergence of resistant subpopulations or toxicity to normal tissues.
Mechanistic Model Personalization Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
The development and application of these predictive models rely on a suite of key reagents, computational platforms, and data resources.
Table 3: Key Reagents and Platforms for Predictive Oncology Research
| Category | Item | Specific Examples & Functions |
|---|---|---|
| Biological Models | Patient-Derived Organoids [50] | 3D in-vitro models that mimic the patient's tumor heterogeneity and drug response; used for ex-vivo drug screening and resistance studies. |
| Data Resources | Public Genomic/Clinical Repositories | The Cancer Genome Atlas (TCGA), used by Compass for training. Clinical trial data (e.g., IMvigor210) and real-world EHR data used for validation. |
| Computational Platforms | Cloud AI & Modeling Software | Cloud-based platforms for SCORPIO/LORIS; AI software like Lunit SCOPE IO; mathematical modeling environments (MATLAB, Python with SciPy). |
| Imaging & Analysis | Digital Pathology Scanners [47] | High-throughput scanners to create whole-slide images from H&E stains for AI-based image analysis. |
| Biomarker Assays | Genomic & Transcriptomic Profiling | RNA sequencing to generate transcriptomic data for models like Compass; PD-L1 IHC staining and TMB testing as baseline biomarkers. |
The choice between AI/ML and mechanistic models is not a matter of superiority but of strategic fit for the specific research or clinical question.
Use AI/ML models like SCORPIO, Compass, or Lunit SCOPE IO when the primary goal is to achieve high predictive accuracy from complex, high-dimensional data (e.g., transcriptomics, images, EHR) and when the underlying biological mechanisms are too complex to fully encode. Their strength lies in pattern recognition and generalizability across large, diverse patient populations, as evidenced by Compass's performance across 33 cancers [46] and SCORPIO's validation in nearly 10,000 patients [45].
Employ mechanistic models when the research objective is to understand the underlying biological dynamics of treatment response, optimize drug scheduling (e.g., for cell cycle-specific chemotherapies [49]), or generate testable biological hypotheses. These models are indispensable for in-silico experimentation where clinical trials are infeasible, such as testing dozens of combination therapy schedules.
The most promising future direction lies in the integration of both paradigms. AI can be used to infer patient-specific parameters for mechanistic models from clinical data, thereby creating digital twins that are both biologically grounded and individually calibrated. This synergistic approach has the potential to finally realize the promise of truly personalized, predictive oncology.
The pursuit of new therapeutics is undergoing a profound transformation, driven by the integration of advanced computational methodologies. Traditional drug discovery, often a time-consuming and costly process, is being reshaped by two powerful, complementary approaches: mechanistic modeling and artificial intelligence (AI) and machine learning (ML). Within tumor modeling research, these paradigms offer distinct advantages; mechanistic models provide interpretable, biology-grounded simulations, while AI/ML excels at finding complex patterns within high-dimensional data. This guide objectively compares the performance of these approaches, focusing on their application in target identification and compound screening. We frame this comparison within a broader thesis that the future of drug discovery lies not in choosing one over the other, but in strategically integrating mechanistic understanding with data-driven AI power to accelerate the development of safe and effective drugs.
Comparative Analysis: Mechanistic Models vs. AI/ML in Tumor Modeling
The table below summarizes the core characteristics, performance, and applications of mechanistic and AI/ML models based on recent research findings.
Table 1: Performance and Characteristic Comparison of Mechanistic vs. AI/ML Models in Drug Discovery
| Aspect | Mechanistic Models | AI/ML Models |
|---|---|---|
| Core Philosophy | Built on established biological, physiological, and pharmacological principles [51] [2]. | Learn patterns and relationships directly from data without pre-defined biological rules [2] [52]. |
| Interpretability | High; model components and parameters have direct biological meaning (e.g., cell growth rate, inhibition constant) [2]. | Often a "black box"; model decisions can be difficult to trace and explain [53] [54]. |
| Data Requirements | Can be calibrated with smaller, targeted datasets [2]. | Require large, high-quality datasets for training; performance is tightly linked to data volume and quality [55] [52]. |
| Predictive Performance (Example) | R² = 0.77 for predicting breast cancer cell growth dynamics [2]. | Random Forest achieved R² = 0.92 on the same breast cancer cell growth task [2]. |
| Key Strength | Provides causal insights and elucidates biological mechanisms; useful for hypothesis generation [2]. | High predictive accuracy and efficiency in screening large compound libraries or complex datasets [2] [56]. |
| Primary Limitation | May oversimplify complex biology, potentially limiting predictive accuracy [51] [2]. | Lack of inherent explainability can hinder trust and clinical translation; requires extensive data [53] [54]. |
| Typical Application in Tumor Modeling | Modeling the effect of a glucose transporter (GLUT1) inhibitor on tumor cell growth by limiting glucose access [2]. | Predicting drug-target interactions (DTI) and classifying novel target-disease associations from genomic data [57] [52]. |
Experimental Protocols and Methodologies
Protocol for a Mechanistic Tumor Modeling Study
The following protocol is derived from a study modeling the response of breast cancer cells to a glucose uptake inhibitor [2].
- 1. Cell Culture and Treatment: The triple-negative breast cancer cell line MDA-MB-231 is cultured in a glucose-free medium. Before the experiment, the medium is replaced with one containing designated glucose concentrations (e.g., 0.5 mM to 10 mM) and a glucose uptake inhibitor (Cytochalasin B at 0 μM, 2 μM, or 10 μM). A fluorescent dye (Cytotox Red) is added to the medium to mark dead cells.
- 2. Data Acquisition: Cell growth is monitored in real-time using a live cell imaging system (e.g., IncuCyte S3). Phase-contrast and fluorescent images of the entire well are automatically captured every 3 hours for 4 days.
- 3. Image Processing and Data Extraction: Custom software (e.g., in Matlab) is used to segment the images. The total area covered by cells (confluence) and the area covered by dead cells (fluorescent signal) are quantified for each time point, generating time-resolved growth and death curves.
- 4. Model Calibration: A system of ordinary differential equations (ODEs) is developed to describe the dynamics of live and dead cell counts. This mechanism-based model includes parameters for cell proliferation rate, death rate, and a dose-dependent inhibition constant for Cytochalasin B. The model is calibrated by fitting its parameters to the experimental growth curve data.
- 5. Model Validation and Prediction: The calibrated model is used to simulate and predict tumor cell growth under conditions not used in the training set, thereby validating its predictive capability.
Protocol for an AI/ML-Based Drug-Target Interaction Study
This protocol outlines a common workflow for predicting novel drug-target interactions using AI [52].
- 1. Data Curation and Preprocessing: Publicly available data on drugs, targets (proteins), and known interactions are gathered from databases like BindingDB, UniProt, and PubChem. Drug molecules are typically represented as SMILES strings or molecular graphs, while proteins are represented by their amino acid sequences or 3D structures.
- 2. Feature Engineering: Meaningful features are extracted from the raw data. For drugs, this could include molecular fingerprints and physicochemical descriptors. For proteins, features might include amino acid composition, sequence embeddings, or structural descriptors.
- 3. Model Selection and Training: A suitable ML algorithm is selected (e.g., Random Forest, Graph Neural Networks, Transformer-based models). The dataset is split into training, validation, and test sets. The model is trained on the training set to learn the complex relationships between the input features and the known drug-target interactions.
- 4. Model Evaluation: The trained model's performance is evaluated on the held-out test set using metrics such as area under the curve (AUC), accuracy, and precision-recall. This step assesses how well the model generalizes to unseen data.
- 5. Prediction and Experimental Validation: The validated model is used to screen large libraries of drug-like compounds or potential protein targets to predict novel interactions. The highest-ranking predictions are then prioritized for validation in wet-lab experiments.
Visualizing the Workflows
The diagrams below illustrate the core workflows for the mechanistic and AI/ML approaches discussed.
Mechanistic Tumor Model Workflow
AI-Driven Drug-Target Interaction Prediction
The following table details key reagents, tools, and datasets essential for conducting research in this field.
Table 2: Key Research Reagent Solutions for Computational Drug Discovery
| Item Name | Type | Function and Application |
|---|---|---|
| MDA-MB-231 Cell Line | Biological Reagent | A triple-negative breast cancer cell line commonly used in in vitro tumor modeling studies to investigate cancer metabolism and drug response [2]. |
| Cytochalasin B | Small Molecule Inhibitor | A well-characterized glucose transporter (GLUT1) inhibitor used in mechanistic studies to perturb nutrient uptake and model its effects on tumor growth dynamics [2]. |
| IncuCyte S3 Live-Cell Analysis System | Instrumentation | An automated live-cell imaging system that enables non-invasive, quantitative tracking of cell proliferation and death over time, generating crucial data for model calibration [2]. |
| BindingDB | Database | A public, web-accessible database of measured binding affinities for drug-like molecules and proteins, serving as a key data source for training AI-based Drug-Target Interaction (DTI) models [52]. |
| RDKit | Software Tool | An open-source cheminformatics toolkit used for manipulating chemical structures, calculating molecular descriptors, and generating fingerprints from SMILES strings for AI/ML input [52]. |
| EZSpecificity Model | AI Software Tool | An AI model that uses a cross-attention algorithm to predict enzyme-substrate binding specificity, useful for identifying pathways in drug development or synthetic biology [58]. |
| PMLB (Penn Machine Learning Benchmark) | Dataset Suite | A large, curated suite of benchmark datasets used to evaluate and compare the performance of different machine learning algorithms in a standardized manner [55]. |
The comparison reveals that mechanistic and AI/ML models are not simply competitors but powerful allies. The future of accelerated drug discovery lies in hybrid modeling, which integrates the two approaches [51] [54]. For example, AI can be used to rapidly parameterize mechanistic models or to identify novel patterns that inform new mechanistic hypotheses. Conversely, mechanistic models can provide a structured, interpretable framework that guides AI and validates its outputs, thereby addressing the "black box" concern [53] [54]. As the industry moves toward democratizing AI, enforcing guardrails, and demanding transparency [53], this synergistic integration will be crucial for unlocking more efficient, reliable, and interpretable predictive modeling. This will ultimately accelerate the journey from target identification to a clinically successful compound.
Navigating Challenges and Enhancing Model Performance
Addressing Data Scarcity and Quality for Robust Model Training
In the field of tumor modeling research, a fundamental division exists between mechanistic models, which are based on established biological principles, and artificial intelligence (AI) approaches, which learn patterns directly from data. Both paradigms face a significant common challenge: the scarcity and variable quality of robust clinical and experimental data for model training and validation [20]. Mechanistic models require precise, biologically-relevant parameters that are often difficult to measure directly in patients, while data-driven AI models demand large, diverse, and accurately labeled datasets to avoid overfitting and ensure generalization [59] [60]. This data limitation problem is particularly acute in oncology, where tumor heterogeneity, ethical constraints on data collection, and the complexity of integrating multimodal data create substantial barriers to developing reliable predictive models [61]. The critical importance of addressing these data challenges is underscored by the fact that more than 90% of cancer-related deaths are linked to drug resistance [62], a complex phenomenon that requires sophisticated models to predict and overcome. This review systematically compares the strategies employed by both modeling approaches to overcome data limitations, with a particular focus on their applications in tumor growth prediction and therapeutic response modeling.
AI-Driven Solutions for Data Augmentation and Enhancement
Generative AI for Synthetic Data Creation
Artificial intelligence approaches, particularly deep learning, have pioneered innovative methods to combat data scarcity through synthetic data generation. These techniques effectively expand limited datasets by creating artificial but realistic medical images that preserve the statistical properties of original data while introducing diversity crucial for robust model training.
Table 1: Performance Comparison of AI-Based Data Augmentation Methods in Brain Tumor MRI
| Method | Base Architecture | Application | Key Innovation | Reported Performance Improvement |
|---|---|---|---|---|
| MCFDiffusion [63] | Denoising Diffusion Probabilistic Models | Brain tumor MRI classification & segmentation | Converts healthy brain MRIs to tumor-containing images; multi-channel fusion | Classification accuracy: +3%; Dice coefficient: +1.5-2.5% |
| 3D Multi-Contrast Synthesis [64] | Latent Diffusion Model | 3D multi-contrast brain tumor MRI generation | Tumor mask conditioning; adapts 2D latent diffusion to 3D MRI | High-quality generation validated via Fréchet Inception Distance (FID) |
| GAN-Based Augmentation [63] | Generative Adversarial Networks | Binary/multi-class brain tumor classification | Traditional adversarial training | Dice score: 81% (binary); Accuracy: 93.1% (3-class) |
The Multi-Channel Fusion Diffusion Model (MCFDiffusion) represents a significant advancement in this domain [63]. This method addresses class imbalance by systematically converting healthy brain MRI images into images containing tumors through a sophisticated diffusion-based process. Unlike earlier generative adversarial networks (GANs) that often suffer from mode collapse and limited diversity, diffusion models progressively add and remove noise to generate high-quality, varied samples that effectively expand the training dataset. The model's multi-channel approach allows it to handle complex medical imaging data more effectively than single-channel alternatives, resulting in demonstrated improvements of approximately 3% in classification accuracy and 1.5-2.5% in Dice coefficient for segmentation tasks [63].
A more specialized approach employs 3D latent diffusion models with tumor mask conditioning to generate multi-contrast brain tumor MRI samples [64]. This framework utilizes two key components: a 3D autoencoder for perceptual compression and a conditional 3D Diffusion Probabilistic Model (DPM) that generates samples guided by an input tumor mask. This conditioning approach ensures that generated tumors align with anatomically plausible locations and characteristics, addressing both data scarcity and the need for precise tumor localization in training data. The method has been validated on datasets from The Cancer Genome Atlas (TCGA) and the University of Texas Southwestern Medical Center (UTSW), demonstrating its ability to produce high-quality, diverse MRI samples that can supplement real patient data [64].
Multimodal Data Integration Frameworks
Beyond synthetic data generation, AI approaches address data quality challenges through sophisticated multimodal integration techniques that combine diverse data types to create a more comprehensive representation of tumor biology.
Diagram: Multimodal AI Workflow for Oncology Data Integration
Advanced neural architectures including Graph Neural Networks (GNNs) and Transformers have demonstrated remarkable success in integrating diverse oncology data types [61]. These architectures enable the fusion of radiological images, digitized pathology slides, molecular data, and electronic health records, capturing complex relationships that would be missed when analyzing each modality in isolation. For instance, the RadGenNets model exemplifies this approach by integrating clinical and genomics data with PET scans and gene mutation information using a combination of Convolutional Neural Networks and Dense Neural Networks to predict gene mutations in Non-small cell lung cancer patients [61].
The experimental protocol for developing such multimodal AI systems typically involves several critical stages [62]. The process begins with comprehensive data collection spanning demographic, clinical, genomic, transcriptomic, imaging, and pathological data. This is followed by rigorous preprocessing including data cleaning, standardization, normalization, and feature selection to handle the inherent heterogeneity of medical data. Model selection and training employ appropriate algorithms (e.g., SVM, random forest, deep learning) tailored to the specific resistance prediction task. The models then undergo validation using techniques like k-fold cross-validation and testing on independent cohorts to ensure robustness. Finally, model interpretation using methods like SHAP (SHapley Additive exPlanations) analysis provides biological insights and clinical actionable intelligence [62].
Mechanistic Modeling Approaches to Data Limitations
Hybrid Modeling Frameworks
While AI approaches focus primarily on data-driven pattern recognition, mechanistic models incorporate established biological principles to simulate tumor dynamics. To address data scarcity, these models have evolved toward hybrid frameworks that integrate machine learning components to enhance their predictive capabilities with limited data.
The Bayesian combination of Mechanistic Modeling and Machine Learning (BaM3) represents a pioneering approach that leverages the strengths of both paradigms [59]. This method employs mechanistic models as informative Bayesian priors, which are then updated using machine learning-derived insights from patient data. The mathematical formulation demonstrates how the posterior distribution of clinical outputs combines predictions from both approaches:
Where Y represents the clinical outputs, Xm denotes the modelable variables, and Xu represents the unmodelable variables [59]. This integration allows the model to maintain biological plausibility through the mechanistic component while adapting to individual patient characteristics through the machine learning component.
In validation studies, this hybrid approach demonstrated significant improvements over standalone mechanistic models, particularly for patients with late clinical presentation (>95% of simulated patients showed improvements) [59]. When applied to chronic lymphocytic leukemia and ovarian cancer cohorts, the method achieved approximately 60% reduction in mean squared error compared to conventional mechanistic approaches, highlighting its potential for personalized prediction even with sparse clinical data [59].
Leveraging Multi-Scale Data Integration
Mechanistic models address data quality challenges by strategically integrating multi-scale data, using readily available clinical measurements to constrain parameters that cannot be directly measured.
Table 2: Data Types for Informing Mechanistic Tumor Growth Models
| Data Modality | Specific Measurements | Role in Mechanistic Modeling | Clinical Availability |
|---|---|---|---|
| Anatomical MRI [20] | Tumor structure and extent | Define computational domain; assign boundary conditions; identify disease extent | High (routine clinical use) |
| Diffusion-Wweighted MRI (DW-MRI) [20] | Cellularity | Parameterize cell density models; estimate proliferation rates | Moderate (specialized protocols) |
| Dynamic Contrast-Enhanced MRI (DCE-MRI) [20] | Vascularity and perfusion | Inform vascular modeling; estimate nutrient/oxygen delivery | Moderate (specialized protocols) |
| PET Imaging [20] | Glucose metabolism (¹⁸F-FDG); Hypoxia (¹⁸F-FMISO) | Parameterize metabolic models; estimate hypoxia-related treatment resistance | Variable (depends on tracer) |
| Digital Pathology [20] | Whole-slide images; cellular features | Initialize cellular-scale models; validate spatial predictions | Growing availability |
| Molecular Data [60] | Genomic, transcriptomic profiles | Inform inter-patient heterogeneity; parameterize subtype-specific models | Increasing (precision oncology) |
Medical imaging plays a particularly crucial role in informing mechanistic models, with MRI and PET emerging as primary modalities for parameterizing patient-specific models of tumor growth and treatment response [20]. The spatial and temporal resolution of these imaging techniques enables measurement of key biological parameters including cellularity (via diffusion-weighted MRI), vascularity and perfusion (via dynamic contrast-enhanced MRI), hypoxia (via ¹⁸F-fluoromisonidazole PET), and glucose metabolism (via ¹⁸F-flourodeoxyglucose PET) [20]. These measurements directly inform the biological mechanisms incorporated into mathematical models of tumor progression.
The experimental protocol for developing patient-specific mechanistic models begins with identifying the key biological processes governing the tumor system of interest [20] [60]. Researchers formulate mathematical equations representing these processes, typically employing partial differential equations for spatial dynamics or ordinary differential equations for temporal dynamics. The model parameters are then initialized using patient-derived imaging and clinical data, with machine learning techniques sometimes employed to estimate parameters that cannot be directly measured. The model is calibrated against longitudinal patient data to refine parameter estimates, and finally validated by comparing predictions with subsequent clinical observations [59]. This approach enables the creation of models that maintain biological fidelity while adapting to individual patient characteristics, even with limited data points.
Comparative Analysis and Research Reagents
Performance Comparison Across Modeling Paradigms
Table 3: Comparative Performance of Modeling Approaches in Addressing Data Scarcity
| Application Domain | Model Type | Data Requirements | Performance Metrics | Key Limitations |
|---|---|---|---|---|
| Advanced HCC Survival Prediction [11] | StepCox (forward) + Ridge ML model | 175 patients (115 RT + 60 non-RT) | C-index: 0.68 (training), 0.65 (validation); AUC: 0.72-0.75 | Requires structured clinical data; limited by sample size |
| Glioma Growth Prediction [59] | BaM3 (Hybrid mechanistic-ML) | Sparse temporal data; ensemble of 500 virtual patients | >95% patients show improvement vs mechanistic model; ~60% MSE reduction in real cohorts | Complex implementation; requires mechanistic understanding |
| Brain Tumor MRI Generation [64] [63] | Diffusion Models (MCFDiffusion) | Paired healthy-diseased images for training | Classification: +3%; Segmentation: +1.5-2.5% Dice | Computational intensity; specialized expertise required |
| Tumor Drug Resistance Prediction [62] | Multimodal Deep Learning | Multi-omics, imaging, clinical data | MGMTpms prediction: 81-87% accuracy across cohorts | Data heterogeneity; interpretability challenges |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Reagents and Computational Tools for Tumor Modeling
| Resource Category | Specific Tools/Solutions | Function in Addressing Data Challenges | Representative Applications |
|---|---|---|---|
| Generative AI Frameworks [64] [63] | Denoising Diffusion Probabilistic Models (DDPM); Latent Diffusion Models | Synthetic data generation; data augmentation for rare tumor types | Brain tumor MRI synthesis; multi-contrast MRI generation |
| Multimodal Data Integration Platforms [61] | Graph Neural Networks (GNNs); Transformers | Fusing disparate data types (imaging, molecular, clinical) | RadGenNets for NSCLC mutation prediction |
| Mechanistic Modeling Environments [59] [60] | Partial Differential Equation Solvers; Bayesian Inference Tools | Implementing biological principles; combining mechanisms with data | BaM3 for tumor growth prediction |
| Public Data Repositories [65] | The Cancer Genome Atlas (TCGA); PCAWG; GENIE | Providing standardized, multi-platform cancer datasets | Model training; validation across cancer types |
| Model Validation Suites [62] [65] | Cross-validation frameworks; AUROC/AUPRC analysis | Assessing model performance; ensuring generalizability | Drug resistance prediction validation |
The challenge of data scarcity and quality in tumor modeling research has spurred innovative solutions across both AI-driven and mechanistic approaches. AI methodologies, particularly generative models and multimodal integration frameworks, excel at expanding limited datasets and discovering complex patterns from heterogeneous data sources. Mechanistic models, enhanced through Bayesian hybrid approaches and strategic multi-scale data integration, maintain biological plausibility while adapting to sparse clinical observations. The emerging consensus indicates that neither approach alone optimally addresses the data challenges in oncology; rather, the most promising path forward lies in strategic integration of both paradigms [59] [60]. Such integration leverages the pattern recognition capabilities of AI with the biological fidelity of mechanistic models, creating a more robust foundation for predictive oncology that can transform cancer care through personalized therapeutic strategies. As these computational approaches continue to evolve and mature, their ability to overcome data limitations will play a pivotal role in accelerating the development of more effective, individualized cancer treatments.
In the field of tumor modeling research, a fundamental tension exists between the predictive power of artificial intelligence (AI) and the need for transparent, interpretable models that researchers and clinicians can trust. Mechanistic models, which are grounded in established biological and physical principles, have long been the gold standard for interpretability in oncology research. These models explicitly incorporate known relationships, such as drug pharmacokinetics and tumor growth dynamics, making their reasoning process transparent [66]. In contrast, AI and machine learning models, particularly deep learning networks, often function as "black boxes," delivering high accuracy but obscuring the rationale behind their predictions [67] [20].
This black-box problem presents significant barriers to clinical adoption in oncology, where understanding why a model suggests a particular treatment or diagnosis can be as crucial as the prediction itself. Regulatory frameworks like the EU's AI Act are increasingly mandating transparency for high-risk AI systems, including those used in medical diagnostics [67]. Furthermore, clinician skepticism toward opaque models and the potential for AI to amplify biases in training data underscore the urgent need for robust interpretability strategies [5] [68].
The convergence of these two modeling paradigms—mechanistic and AI—offers a promising path forward. This guide compares current interpretability strategies, providing tumor modeling researchers with experimental data, methodologies, and practical tools to implement explainable AI (XAI) in their work, thereby bridging the gap between performance and transparency.
Comparative Analysis of Interpretability Techniques
The table below summarizes the core XAI techniques relevant to tumor modeling, comparing their fundamental approaches, key advantages, and primary limitations.
Table 1: Comparison of AI Model Interpretability Techniques
| Technique | Type | Core Functionality | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| SHAP (SHapley Additive exPlanations) [67] [69] | Post-hoc, Model-agnostic | Uses cooperative game theory to assign each feature an importance value for a specific prediction. | Provides consistent, theoretically sound feature attribution; applicable to most AI models. | Computationally intensive; can be slow for large models or datasets. |
| LIME (Local Interpretable Model-agnostic Explanations) [67] [69] | Post-hoc, Model-agnostic | Perturbs input data and approximates the complex model locally with an interpretable one (e.g., linear model). | Intuitive to understand; works with any black-box model. | Explanations can be unstable; sensitive to the perturbation setting. |
| Counterfactual Explanations [67] | Post-hoc, Model-agnostic | Finds the minimal changes to the input required to alter the model's prediction. | Highly actionable for users (e.g., "What should change for a different outcome?"). | Generating plausible and feasible explanations in complex domains like biology is challenging. |
| Attention Mechanisms [67] | Intrinsic | Integrated into model architecture (e.g., Transformers) to highlight which parts of the input the model "focuses on." | Provides explanations as a native part of the model's function; no separate tool needed. | The faithfulness of attention weights as explanations is sometimes debated. |
| Chain-of-Thought (CoT) Prompting [67] | Intrinsic (for LLMs) | Prompts a Large Language Model (LLM) to output its reasoning steps before giving a final answer. | Makes the model's internal "reasoning" process explicit and human-readable. | Risk of "unfaithful explanations" where the generated reasoning does not match the model's actual decision path. |
Experimental Protocols for Evaluating Interpretability
Rigorous evaluation is essential to ensure that explanations provided by XAI techniques are accurate and meaningful. The following section outlines standard protocols for benchmarking these methods.
Benchmarking XAI Techniques in a Radiomics Study
A 2025 study comparing deep learning and radiomics models for predicting hepatocellular carcinoma (HCC) differentiation via ultrasound provides a template for evaluating interpretability in a clinical context [70].
1. Experimental Objective: To develop and compare predictive models for HCC differentiation using ultrasound-based radiomics and deep learning, and to evaluate the clinical utility of a combined model.
2. Data Acquisition and Preprocessing:
- Patient Cohort: Retrospective analysis of 224 patients with pathologically confirmed HCC who underwent surgery. Patients were divided into well-differentiated and moderately-to-poorly differentiated groups based on postoperative pathology [70].
- Ultrasound Imaging: Standardized grayscale ultrasound examinations were conducted. The DICOM images were stored and processed [70].
- Region of Interest (ROI) Delineation: Two experienced ultrasound radiologists independently delineated ROIs on the images using ITK-SNAP software. Inter- and intra-observer reproducibility was assessed via intraclass correlation coefficients (ICCs) to ensure segmentation reliability [70].
3. Model Training and Interpretation:
- Radiomics Model: A large number of features (shape, first-order statistics, texture) were extracted from the ROIs using PyRadiomics. Model-agnostic techniques like SHAP can be applied to the resulting model to identify which image features most strongly predict poor differentiation [70] [67].
- Deep Learning Model: A pre-trained ResNet-101 architecture was fine-tuned on the ultrasound image patches. Intrinsic methods, such as Grad-CAM (a variant of Layer-Wise Relevance Propagation), can be used to generate heatmaps highlighting the image regions most influential in the network's classification [70] [67].
- Performance Validation: Model performance was assessed using receiver operating characteristic (ROC) curves, calibration curves, and decision curve analysis (DCA) [70].
4. Key Findings: The study demonstrated that a combined model integrating both radiomics and deep learning features achieved superior performance (AUC of 0.918) compared to either approach alone. This suggests that hybrid models can capture complementary information, and interpreting them requires a combination of feature-attribution and visualization techniques [70].
Evaluating Model Identifiability in Tumor Growth Modeling
A different approach to interpretability involves assessing the practical identifiability of model parameters, which is a cornerstone of mechanistic modeling and can be applied to evaluate AI models.
1. Experimental Objective: To determine whether the choice of cancer growth model affects estimates of chemotherapy efficacy parameters (IC50 and εmax), which is crucial for understanding if a model's parameters are reliable and interpretable [71].
2. Data Simulation:
- Synthetic Data Generation: Seven common ordinary differential equation (ODE) models of tumor growth (e.g., Exponential, Logistic, Gompertz) were used to generate synthetic tumor growth time courses. This included a control group and groups treated with different drug concentrations [71].
- Modeling Treatment: Chemotherapy was modeled as reducing the growth rate parameter using an Emax model, with known ground-truth values for εmax and IC50 [71].
- Noise Introduction: Gaussian noise (5%, 10%, 20%) was added to the synthetic data to mimic real-world experimental variability [71].
3. Model Fitting and Identifiability Assessment:
- Cross-Fitting Procedure: Each synthetic dataset was fit using all seven growth models, including the "wrong" ones. This tests the robustness of parameter estimation to model misspecification [71].
- Parameter Estimation: Parameters, including εmax and IC50, were estimated by minimizing the sum of squared residuals between the synthetic data and model predictions [71].
- Identifiability Analysis: The practical identifiability of parameters was judged by comparing the accuracy and precision of the estimated parameters against their known true values across the different model fits. For instance, the study found that IC50 was generally identifiable, but εmax was sensitive to the choice of growth model, particularly when the Bertalanffy model was used [71].
This protocol highlights that a model's predictions are only as trustworthy as the identifiability of its parameters. When using AI to estimate parameters for mechanistic models, similar identifiability analyses are necessary to ensure the results are biologically plausible and not an artifact of the model structure.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing interpretable AI and mechanistic modeling requires a suite of computational tools and data resources. The following table details key solutions for researchers in computational oncology.
Table 2: Essential Research Reagent Solutions for Interpretable Tumor Modeling
| Tool/Solution | Type | Primary Function | Application in Interpretability |
|---|---|---|---|
| PyRadiomics [70] | Software Library | Extracts a large number of quantitative features from medical images. | Provides the input features for radiomics models, which are inherently more interpretable than raw pixels. SHAP can then be applied to rank these features by importance. |
| ITK-SNAP [70] | Segmentation Software | Enables manual, semi-automatic, and automatic segmentation of medical images in 2D and 3D. | Critical for defining accurate Regions of Interest (ROIs) on medical images, which is the foundational step for any subsequent image-based analysis and interpretation. |
| SHAP Library [67] [69] | Explainability Library | Implements SHAP values for explaining the output of any machine learning model. | A versatile, model-agnostic tool to explain individual predictions or the overall model behavior by quantifying feature contributions. |
| ResNet Architectures [70] | Deep Learning Model | A class of powerful convolutional neural networks (CNNs) for image analysis. | Often used as a benchmark or feature extractor. Its deep but structured architecture allows for the use of visualization techniques like Grad-CAM to see what the network "looks at." |
| LIME [67] [69] | Explainability Library | Explains individual predictions of any classifier by perturbing the input. | Useful for creating local, intuitive explanations for specific cases (e.g., "Why was this specific tumor classified as high-risk?"). |
| Physiologically Based Pharmacokinetic (PBPK) Platforms [66] | Mechanistic Modeling Framework | Models drug absorption, distribution, metabolism, and excretion (ADME) in a physiologically realistic manner. | Offers a highly interpretable, mechanism-based framework to simulate drug delivery to tumors, providing a baseline against which AI predictions can be compared and validated. |
The journey to overcome the black box in AI is not about choosing between powerful machine learning and interpretable mechanistic models, but rather about strategically integrating them. As the experimental data and comparisons in this guide have shown, techniques like SHAP and LIME can illuminate the decision-making processes of complex AI models, while robustness checks like parameter identifiability analysis ensure their reliability.
The future of interpretable tumor modeling lies in hybrid frameworks. In such systems, AI can handle pattern recognition in high-dimensional data (e.g., medical images or omics) and estimate parameters for mechanistic models, which in turn provide a biologically plausible structure and generate simulations that are inherently understandable to researchers and clinicians [20] [5] [66]. This synergy paves the way for creating patient-specific "digital twins," virtual models that can simulate treatment outcomes and optimize therapeutic strategies in a transparent and trustworthy manner [5]. By adopting these strategies, researchers can build AI systems that are not only predictive but also principled and interpretable, ultimately accelerating the translation of computational insights into clinical breakthroughs.
Computational and Scalability Hurdles in Complex Model Deployment
The pursuit of precision oncology has given rise to two distinct computational paradigms: mechanistic models grounded in biological first principles, and data-driven artificial intelligence (AI) approaches that discover patterns directly from complex datasets. While mechanistic models, such as agent-based models (ABMs) and partial differential equations, provide interpretable simulations of tumor biology and treatment response, they face significant computational burdens when scaling to patient-specific applications [5]. Conversely, AI and machine learning (ML) models can efficiently analyze high-dimensional data but often function as "black boxes" with limited biological insight and substantial infrastructure requirements for deployment [20] [6].
This guide objectively compares the performance and scalability of both approaches, with a specific focus on the computational hurdles researchers encounter when translating models from research environments to clinical applications. By examining experimental data across multiple studies and deployment platforms, we provide a comprehensive framework for selecting appropriate modeling strategies based on specific research objectives and infrastructure constraints.
Performance Benchmarking: Mechanistic Models vs. AI Approaches
Theoretical Foundations and Computational Characteristics
Table 1: Fundamental Characteristics of Tumor Modeling Approaches
| Characteristic | Mechanistic Models | AI/ML Models |
|---|---|---|
| Theoretical Basis | Biological first principles, known pathophysiology | Pattern recognition from data, statistical learning |
| Data Requirements | Lower volume, but requires specific parameter measurements | High-volume training datasets, often thousands of samples |
| Interpretability | High - explicitly represents biological mechanisms | Low to moderate - "black box" nature challenges interpretation |
| Computational Demand | High for complex, spatially-resolved simulations | Variable: high during training, typically lower during inference |
| Scalability Constraints | Computational cost increases exponentially with model complexity | Hardware-intensive training, dependency on quality data |
| Clinical Translation Barriers | Parameter estimation from limited patient data, validation challenges | Generalizability, regulatory approval, integration into clinical workflows |
Mechanistic models are fundamentally based on established biological principles and attempt to simulate the underlying processes governing tumor growth and treatment response. Agent-based models (ABMs), for instance, simulate individual cells and their interactions, capturing emergent behaviors through rules derived from experimental data [5]. These models provide high interpretability because variables and parameters directly correspond to biological entities and processes. However, this biological fidelity comes at a substantial computational cost, particularly when modeling spatially heterogeneous tissues with multiple cell types and molecular species.
In contrast, AI/ML approaches excel at identifying complex, non-linear patterns in high-dimensional datasets without requiring explicit programming of biological rules. Deep learning (DL), a subset of ML utilizing multi-layered neural networks, can automatically discover relevant features from raw data, eliminating manual feature extraction [6]. While this capability enables powerful pattern recognition, it also creates interpretability challenges—a significant concern for clinical deployment where understanding model reasoning is often essential for physician adoption and regulatory approval.
Experimental Performance Data
Table 2: Experimental Performance Metrics from Recent Studies
| Study & Model Type | Dataset Size | Key Performance Metrics | Computational Requirements |
|---|---|---|---|
| HCC ML Prediction [11] | 175 patients | C-index: 0.68 (training), 0.65 (validation); AUC: 0.72-0.75 (1-3 year OS) | 101 algorithms tested; StepCox (forward) + Ridge optimal |
| MRI Brain Tumor DL [32] | 155 studies | Accuracy improvements of 15-30% over traditional methods; specific metrics variable | High GPU utilization; 3D convolutional neural networks |
| Mechanistic ABM [5] | N/A (theoretical) | Captures emergent tumor-immune interactions; qualitative predictive power | Computationally intensive; limited by spatial resolution and cell count |
| Digital Pathology AI [6] | Whole-slide images | Reduces diagnostic time by 50-70%; maintains or improves accuracy | Significant storage and processing needs for whole-slide images |
Recent experimental data highlights the performance characteristics of both approaches. A 2025 study on hepatocellular carcinoma (HCC) demonstrated that ML models could successfully predict overall survival in patients receiving immunoradiotherapy, with the StepCox (forward) + Ridge model achieving concordance indices of 0.68 in training and 0.65 in validation cohorts [11]. The study evaluated 101 different ML algorithms, highlighting the need for extensive computational resources during the model selection and training phases.
For mechanistic models, the primary performance metric is often qualitative accuracy in capturing known biological behaviors rather than quantitative prediction metrics. Agent-based models have successfully reproduced emergent phenomena in the tumor microenvironment, including heterogeneous immune infiltration and metabolic competition [5]. However, these models typically require parameter calibration against experimental data, and their computational demands increase exponentially with spatial resolution and the number of simulated entities.
AI applications in medical imaging have demonstrated particularly strong performance gains. In MRI-based brain tumor diagnosis, deep learning approaches have achieved accuracy improvements of 15-30% over traditional methods, though specific metrics vary considerably across studies [32]. These approaches leverage convolutional neural networks (CNNs) and, increasingly, vision transformers to analyze complex imaging data, but require substantial GPU resources during training and inference.
Deployment Architectures and Scalability Solutions
Model Deployment Platforms
Table 3: AI Model Deployment Platform Comparison (2025)
| Platform | Best For | Scalability Features | Framework Support | Pricing Model |
|---|---|---|---|---|
| Amazon SageMaker [72] [73] | Enterprise AWS users | Auto-scaling, built-in algorithms | TensorFlow, PyTorch, Scikit-learn | Starts at $0.12/hr |
| Google Vertex AI [72] [73] | Scalable cloud AI | AutoML, custom containers | TensorFlow, PyTorch, XGBoost | Custom pricing |
| Microsoft Azure ML [73] | Hybrid deployments | Drag-and-drop designer, automated ML | Multi-framework support | Starts at $0.20/hr |
| BentoML [72] [73] | Self-hosted solutions | Model packaging, Kubernetes-native | Framework-agnostic | Open source |
| Hugging Face Endpoints [73] | LLM deployments | Hosted APIs, model sharing | Transformers, diffusers | Starts at $0.60/hr |
The selection of deployment platforms significantly impacts the scalability and maintenance requirements of computational oncology models. Cloud-based platforms like Amazon SageMaker and Google Vertex AI provide managed services that handle infrastructure scaling, allowing researchers to deploy models without extensive DevOps expertise [73]. These platforms offer auto-scaling capabilities that dynamically adjust computational resources based on inference demand, making them suitable for clinical applications with variable workload patterns.
For organizations with data governance requirements or specialized infrastructure needs, self-hosted solutions like BentoML provide framework-agnostic model packaging and deployment capabilities [72]. This approach offers greater control over the deployment environment but requires in-house expertise for infrastructure management and scaling.
Hybrid and multi-cloud strategies are increasingly common in healthcare organizations, allowing workload distribution across environments based on cost, performance, and data residency requirements [74]. Azure Machine Learning specifically targets these use cases with support for hybrid and multi-cloud deployments, though this flexibility introduces additional complexity in management and monitoring [73].
Computational Workflows
AI Model Deployment Pipeline
The deployment pipeline for computational oncology models involves multiple stages, each with distinct computational requirements. The data acquisition and preprocessing stages often require significant storage and memory resources, particularly for high-resolution medical images or genomic data [6]. Model training represents the most computationally intensive phase, especially for deep learning approaches that may require days or weeks of GPU acceleration [32].
Deployment and monitoring phases focus on serving predictions efficiently, requiring optimized inference engines and continuous performance validation. Performance monitoring is particularly critical for clinical applications, as model accuracy can degrade over time due to dataset shifts or changes in clinical practice [73].
Methodologies: Experimental Protocols and Validation
ML Model Development Protocol
The experimental protocol for developing ML models in oncology follows a structured approach to ensure robustness and generalizability. A recent study on HCC survival prediction exemplifies this process [11]:
Data Curation and Cohort Definition: The study included 175 HCC patients, with 115 receiving immunoradiotherapy and 60 receiving immunotherapy and targeted therapy alone. Inclusion criteria required confirmed HCC diagnosis, Barcelona Clinic Liver Cancer (BCLC) stage B or C disease, Child-Pugh A or B liver function, and complete clinical data.
Preprocessing and Feature Selection: Baseline characteristics including sex, age, Child-Pugh class, AFP level, BCLC stage, tumor number, tumor size, portal vein tumor thrombosis, lymph node involvement, and extrahepatic metastasis were analyzed. Propensity score matching (PSM) was performed using 1:1 nearest-neighbor matching without replacement to minimize selection bias.
Model Training and Validation: Patients were randomly divided into training and validation cohorts at a 6:4 ratio. Univariate Cox regression identified prognostic factors associated with overall survival, with variables showing p < 0.05 selected for ML modeling. The study evaluated 101 different ML algorithms, assessing performance using the concordance index (C-index), receiver operating characteristic (ROC) curves, and risk score stratification.
Performance Metrics: The StepCox (forward) + Ridge model demonstrated superior performance with a C-index of 0.68 in training and 0.65 in validation cohorts. Time-dependent ROC analysis showed area under the curve (AUC) values of 0.72, 0.75, and 0.74 at 1, 2, and 3 years in the training cohort, and 0.72, 0.75, and 0.73 in the validation cohort, respectively.
Research Reagent Solutions
Table 4: Essential Research Reagents and Computational Resources
| Resource Category | Specific Tools/Platforms | Function in Research |
|---|---|---|
| Medical Imaging Data | MRI (T1, T2, T1-CE, FLAIR), CT, PET [32] [6] | Provides non-invasive tumor characterization and monitoring |
| Genomic Data | Whole-slide images, RNA/DNA sequencing, liquid biopsies [6] | Enables molecular profiling and biomarker discovery |
| Computational Infrastructure | GPUs (A100, H100), High-performance computing clusters [73] | Accelerates model training and complex simulations |
| ML Frameworks | TensorFlow, PyTorch, Scikit-learn [72] [73] | Provides algorithms and utilities for model development |
| Deployment Platforms | AWS SageMaker, Google Vertex AI, Azure ML, BentoML [72] [73] | Enables model serving, scaling, and monitoring in production |
| Validation Tools | SHAP, Grad-CAM, LIME [32] | Provides model interpretability and validation |
The computational resources required for tumor modeling span from data acquisition tools to deployment platforms. Medical imaging modalities including MRI, CT, and PET provide essential data for both model development and validation [6]. ML frameworks such as TensorFlow and PyTorch offer the algorithmic foundation for developing predictive models, while deployment platforms like AWS SageMaker and Google Vertex AI provide the infrastructure for scaling these models to clinical applications [73].
Validation tools have become increasingly important for building trust in AI systems. Techniques such as SHAP (SHapley Additive exPlanations), Grad-CAM (Gradient-weighted Class Activation Mapping), and LIME (Local Interpretable Model-agnostic Explanations) help researchers and clinicians understand model predictions, addressing the "black box" criticism often leveled against AI approaches [32].
Integration Strategies and Future Directions
Hybrid Modeling Approaches
Model Integration Strategies
The convergence of mechanistic and AI approaches represents the most promising direction for overcoming current computational hurdles. Hybrid modeling frameworks leverage the strengths of both paradigms while mitigating their respective limitations [5].
AI can complement mechanistic models by estimating unknown parameters, initializing models with multi-omics or imaging data, and reducing computational demands through surrogate modeling [5]. For example, AI-generated efficient approximations of computationally intensive agent-based models can enable real-time predictions and rapid sensitivity analyses that would be infeasible with the full mechanistic model.
Conversely, biological constraints from mechanistic models can inform AI architectures, improving model interpretability and consistency with known biology [5]. This approach ensures that AI predictions respect fundamental biological principles, increasing clinician confidence in model outputs.
Emerging Solutions to Scalability Challenges
Several emerging technologies show promise for addressing the scalability challenges in complex model deployment:
Federated Learning: This approach enables model training across multiple institutions without sharing sensitive patient data, addressing both privacy concerns and data scarcity limitations [32]. By training models locally and aggregating parameter updates centrally, federated learning maintains data sovereignty while leveraging diverse datasets for improved model generalizability.
Quantum-Enhanced Computing: While still in early stages, quantum computing approaches may eventually solve optimization problems in mechanistic modeling and ML training that are currently intractable with classical computers [6].
Edge Computing: For real-time applications in clinical settings, edge computing deploys optimized models directly to medical devices or local servers, reducing latency and bandwidth requirements [74]. This approach is particularly valuable for time-sensitive applications such as surgical guidance or radiotherapy planning.
AI-Optimized Hardware: Specialized processors designed specifically for ML workloads continue to improve the computational efficiency of training and inference. Platforms like RunPod offer access to high-end GPUs (A100s, H100s) with spot pricing options that can significantly reduce computational costs for research organizations [73].
The deployment of complex computational models in oncology research presents significant challenges in both computational scalability and clinical translation. Mechanistic models provide biological interpretability but face steep computational demands when scaling to patient-specific applications. AI/ML approaches offer powerful pattern recognition capabilities but require extensive infrastructure for training and deployment, while struggling with interpretability concerns.
The experimental data presented in this guide demonstrates that both approaches can provide value in different contexts, with ML models achieving C-index values of 0.65-0.68 for survival prediction [11], while mechanistic models offer unique insights into tumor biology through simulation of emergent behaviors [5]. The choice between approaches depends on specific research objectives, available data resources, and computational infrastructure.
The most promising path forward lies in hybrid approaches that leverage the strengths of both paradigms. By integrating AI-driven pattern recognition with mechanistic biological constraints, researchers can develop models that are both predictive and interpretable. As deployment platforms continue to evolve, addressing challenges in scalability, interpretability, and clinical integration, computational models are poised to play an increasingly important role in personalized cancer care.
In the quest to overcome the profound challenges of tumor heterogeneity and therapeutic resistance, two distinct computational paradigms have emerged: mechanistic modeling and artificial intelligence (AI). Mechanistic models are built on established principles of biology and physics, using mathematical equations to formalize our understanding of drug transport, tumor growth, and treatment response dynamics. In contrast, AI models are data-driven, employing pattern recognition on large datasets to discover complex relationships without requiring pre-specified biological rules [75]. Historically, these approaches developed along parallel tracks, each with complementary strengths and limitations. The hybrid modeling paradigm represents a frontier in computational oncology, synergistically combining mechanistic knowledge with AI's pattern recognition power to achieve predictive accuracy that exceeds the capabilities of either approach alone. This integration is particularly valuable for addressing the multiscale complexity of cancer, from molecular interactions to tissue-level phenomena, enabling more reliable predictions of treatment efficacy and patient-specific outcomes [76] [75].
Performance Comparison: Hybrid Models Versus Single-Approach Alternatives
Quantitative comparisons across recent studies demonstrate the superior performance of hybrid mechanistic-AI approaches against standalone models across multiple cancer types and prediction tasks.
Table 1: Performance Comparison of Modeling Approaches in Cancer Prediction
| Cancer Type | Prediction Task | Model Type | Performance Metric | Result | Reference |
|---|---|---|---|---|---|
| Pediatric Diffuse Midline Glioma | Spatio-temporal tumor growth | Hybrid Mechanistic-AI (Guided DDIM + ODE) | Spatial similarity metrics | Superior anatomical feasibility & growth directionality | [76] |
| Multiple Cancer Types | Prognosis prediction | Multimodal AI (MUSK) | Accuracy | 75% vs 64% for traditional methods | [33] |
| Advanced HCC | Overall survival | AI-only (StepCox + Ridge) | C-index | 0.65 (validation) | [11] |
| Lung & Gastroesophageal | Immunotherapy response | Multimodal AI (MUSK) | Accuracy | 77% vs 61% for PD-L1 testing | [33] |
| Melanoma | 5-year relapse | Multimodal AI (MUSK) | Accuracy | ~83% (12% better than other models) | [33] |
The performance advantages of hybrid approaches stem from their ability to leverage the respective strengths of each modeling paradigm while mitigating their weaknesses. Mechanistic models provide biologically interpretable frameworks that maintain plausibility even with limited data, while AI components extract subtle patterns from complex datasets that might elude manual specification [75]. For spatio-temporal prediction tasks specifically, hybrid models have demonstrated remarkable capability in generating anatomically feasible future medical images that align with both predicted tumor growth and patient-specific anatomy [76].
Experimental Protocols: Implementing Hybrid Models
Protocol 1: Mechanistic Learning with Guided Diffusion for Brain Tumor Growth Prediction
This protocol from Buehler et al. (2025) integrates ordinary differential equation (ODE) models with denoising diffusion implicit models (DDIM) to predict spatio-temporal progression of pediatric diffuse midline glioma [76].
Sample Preparation and Data Requirements:
- Imaging Data: Multi-parametric MRI scans (T1, T2, T1+Gd, FLAIR) from standardized protocols
- Patient Population: Pediatric diffuse midline glioma cases with longitudinal imaging
- Training Datasets: BraTS adult and pediatric glioma datasets for model training
- Validation: Internal validation on 60 axial slices of in-house longitudinal pediatric DMG cases
Experimental Workflow:
- Mechanistic Modeling Phase: Fit patient-specific ODE model to historical tumor measurements
- Model partitions tumor into surviving (A~l~) and dying (A~d~) fractions post-radiotherapy
- Parameters estimated: net growth rate (λ), surviving fraction (S), decay rate (λ~decay~)
- Temporal extrapolation provides expected tumor size at follow-up time
Diffusion Model Training:
- Train denoising diffusion probabilistic model (DDPM) on brain MRI dataset
- Implement U-Net architecture for reverse diffusion process approximation
- Train separate regressor (R) to predict tumor size relative to brain area
Guided Generation Process:
- Use DDIM variant for deterministic generation during inference
- Apply gradient guidance from trained regressor scaled by parameter s~R~
- Generate follow-up scans reflecting mechanistically predicted tumor burden
Validation Metrics:
- Spatial similarity metrics between generated and actual follow-up scans
- Percentile Hausdorff Distance for tumor growth directionality and extent
- Anatomical feasibility assessment by clinical experts
Protocol 2: Hybrid PK/PD and AI Modeling for Chemotherapy Optimization
This approach integrates physiologically-based pharmacokinetic/pharmacodynamic (PK/PD) modeling with machine learning for optimizing metronomic chemotherapy scheduling [75].
Sample Preparation and Data Requirements:
- In Vitro Data: Drug concentration measurements across vascular, interstitial, and cellular compartments
- Cell Lines: Triple-negative breast cancer cells (MDA-MB-468, SUM-149PT)
- In Vivo Models: Walker 256 and hepatoma 5123 cells in rat models
- Clinical Data: Pharmacokinetic parameters from phase I trials
Experimental Workflow:
- Mechanistic PK/PD Framework:
- Develop multi-compartment model (vascular, interstitial, cellular)
- Incorporate drug-specific physicochemical properties
- Model tumor growth dynamics and emergence of therapeutic resistance
AI-Enhanced Parameter Estimation:
- Train machine learning models on high-dimensional parameter space
- Identify crucial biological programs influencing drug response
- Optimize dosage protocols across wide parameter ranges
Hybrid Prediction and Validation:
- Generate in silico predictions of optimal metronomic dosing
- Experimental validation in chemo-resistant neuroblastoma-bearing mice
- Compare hybrid model predictions against standard maximum tolerated dose protocols
Validation Metrics:
- Tumor mass reduction percentage compared to control
- Drug concentration equilibration time in tumor interstitial fluid
- Cell population dynamics in response to treatment
Visualization: Workflows and Signaling Pathways
Diagram 1: Hybrid model integration workflow showing how mechanistic and AI components combine.
Diagram 2: Modeling biological barriers and therapeutic challenges in cancer.
Research Reagent Solutions: Essential Tools for Hybrid Modeling
Successful implementation of hybrid mechanistic-AI approaches requires specialized computational tools and frameworks. The table below details essential research reagents and their functions in developing and validating these integrated models.
Table 2: Essential Research Reagent Solutions for Hybrid Modeling
| Reagent/Framework | Type | Primary Function | Application Example | Key Features |
|---|---|---|---|---|
| Denoising Diffusion Probabilistic Models (DDPM) | AI Framework | High-fidelity image synthesis with conditional guidance | Spatio-temporal brain tumor growth prediction [76] | Conditional generation, gradient guidance, reverse diffusion process |
| Physiologically-Based Pharmacokinetic (PBPK) Modeling | Mechanistic Framework | Multi-compartment drug distribution modeling | Interspecies scaling of paclitaxel pharmacokinetics [75] | Vascular, interstitial, cellular subcompartments, whole-body disposition |
| MONAI (Medical Open Network for AI) | AI Framework | Open-source PyTorch-based medical AI tools | Precise breast area delineation in mammograms [77] | Pre-trained models, standardized workflows, domain-specific optimizations |
| Ordinary/Partial Differential Equation Solvers | Mathematical Tools | Implement continuous mechanistic models | Tumor growth ODEs, drug transport PDEs [76] [75] | Temporal/spatial discretization, parameter estimation, numerical stability |
| Multimodal Transformers (e.g., MUSK) | AI Architecture | Integrate imaging and textual data for prediction | Cancer prognosis and immunotherapy response [33] | Unified mask modeling, unpaired multimodal data incorporation |
| PathExplore IOP | Digital Pathology Tool | Quantitative analysis of tumor-infiltrating lymphocytes | Immune phenotype characterization in H&E samples [78] | Spatial distribution analysis, immune microenvironment classification |
The integration of mechanistic and AI models represents a paradigm shift in computational oncology, moving beyond the limitations of either approach in isolation. By combining first principles of biology and physics with data-driven pattern discovery, hybrid models achieve superior predictive accuracy while maintaining biological plausibility. Experimental validation across multiple cancer types demonstrates that this approach consistently outperforms traditional methods, particularly for complex prediction tasks such as spatio-temporal tumor progression, therapy response forecasting, and optimal treatment scheduling [33] [76] [75]. As multimodal data availability continues to expand and computational methods mature, the hybrid modeling paradigm is poised to become an indispensable tool in precision oncology, ultimately enabling more personalized and effective cancer therapies.
Benchmarking Performance and Clinical Readiness
The pursuit of personalized cancer therapy relies on computational models that can accurately forecast tumor growth and treatment response. The field is primarily dominated by two complementary paradigms: mechanistic models and artificial intelligence (AI) or machine learning (ML) approaches [20]. Mechanistic models are grounded in biological principles, using mathematical equations to represent known or hypothesized underlying tumor dynamics. In contrast, AI/ML models are data-driven, identifying complex patterns from large historical datasets to make predictions without requiring pre-specified biological rules [79]. Evaluating the success of these models requires a dual focus: rigorous assessment of their predictive accuracy through quantitative metrics and a clear-eyed appraisal of their clinical utility in improving patient management and outcomes. This guide provides a structured comparison of these approaches, detailing performance metrics, experimental protocols, and essential research tools.
Comparative Performance of Modeling Paradigms
Predictive Accuracy Metrics
The table below summarizes quantitative performance data reported for various modeling approaches across different clinical applications.
Table 1: Reported Predictive Accuracy of Tumor Models
| Model Type | Specific Application | Reported Performance | Clinical Context | Source |
|---|---|---|---|---|
| AI/ML (SVM) | Predicting patient response to Gemcitabine & 5-FU | >80% accuracy; PPV 77.8-83.3% [80] | Pan-cancer (TCGA) | [80] |
| AI/ML (DL - CNN) | Lung cancer detection (CheXNeXt) | 52.3% greater sensitivity for masses vs. radiologists [7] | Chest X-ray analysis | [7] |
| AI/ML (DL) | Breast cancer detection | Accuracy exceeding 96% [7] | Medical imaging | [7] |
| Hybrid (Mechanistic + DL) | Predicting survival post-immune checkpoint inhibitor therapy | Higher accuracy vs. single-modality models [81] | Multiple cancer types | [81] |
| Hybrid (BaM3) | Predicting tumor growth (synthetic glioma) | Improved predictions for >95% of patients [79] | Chronic lymphocytic leukemia, Ovarian cancer | [79] |
| Mechanistic (ODE) | Tumor growth and chemotherapy response | Quantified via model calibration/validation metrics [82] | Preclinical and clinical scenarios | [82] |
PPV: Positive Predictive Value; SVM: Support Vector Machine; DL: Deep Learning; CNN: Convolutional Neural Network; ODE: Ordinary Differential Equation.
Clinical Utility and Implementation
Beyond raw predictive accuracy, the real-world value of a model is determined by its clinical utility.
Table 2: Comparison of Clinical Utility and Limitations
| Feature | Mechanistic Models | AI/ML Models | Hybrid Models |
|---|---|---|---|
| Interpretability | High; based on causal biological mechanisms [83] | Low to medium; "black box" nature [62] | Medium; seeks to balance both [79] |
| Data Requirements | Can be initialized with sparse, patient-specific data [79] | Requires large, curated datasets for training [20] | Requires both large datasets and mechanistic understanding [81] |
| Generalizability | Can extrapolate to new conditions via mechanisms [20] | Limited to domains within training data; prone to domain shift [20] | Aims for high generalizability by combining strengths [81] [79] |
| Key Clinical Strength | Optimizing intervention strategies in silico [20] [83] | Diagnostic accuracy and efficiency [7] [84] | Improved personalized survival predictions [81] [79] |
| Primary Limitation | Incomplete knowledge of all biological mechanisms [79] | Need for extensive clinical validation and addressing biases [7] [62] | Computational and methodological complexity [81] [79] |
Experimental Protocols for Model Validation
Protocol for AI/ML Model Development and Validation
The following workflow is adapted from studies that successfully predicted tumor drug resistance and patient responses using AI [62] [80].
- Data Collection and Curation: Assemble a multimodal dataset. This includes genomic data (e.g., from RNA-seq), transcriptomic, proteomic, and metabolomic data; medical images (CT, MRI, PET); and electronic health records (EHR) containing patient demographics, treatment history, and outcomes [62].
- Data Preprocessing: Clean the data to handle missing values and outliers. Standardize and normalize features across different data types. For genomic data, this may involve coding medical concepts and performing recursive feature elimination (RFE) to identify the most informative genes for prediction [62] [80].
- Model Training: Partition the data into a training set (typically 70-80%) and a validation set (20-30%). Train a chosen ML algorithm (e.g., Support Vector Machine (SVM), Random Forest, or Deep Learning framework) on the training set to learn the relationship between input features and the outcome (e.g., responder vs. non-responder) [62] [80].
- Model Validation: Use k-fold cross-validation or leave-one-out cross-validation (LOOCV) on the validation set to assess model performance and mitigate overfitting. Evaluate using metrics such as accuracy, sensitivity, specificity, positive predictive value (PPV), and area under the curve (AUC) [62] [80].
- Interpretation and External Validation: Apply interpretability methods (e.g., SHAP analysis) to understand the model's decisions. For robust generalizability, externally validate the model on a completely independent patient cohort from a different institution [62].
AI/ML Model Workflow
Protocol for Mechanistic and Hybrid Model Calibration
This protocol outlines the process for initializing and validating mechanism-based models, including hybrid approaches that integrate them with AI [79] [82] [83].
- Model Selection and Initialization: Choose a mathematical framework (e.g., Ordinary Differential Equations for tumor burden, or PDEs for spatial growth) based on the biological question. Initialize the model with patient-specific initial conditions (e.g., initial tumor volume, cell density, spatial location) derived from baseline medical imaging (MRI, CT) [82] [83].
- Data Integration for Calibration: Use quantitative, multiparametric imaging data to inform and calibrate the model parameters. Key imaging types include:
- Model Calibration and Selection: Solve an inverse problem to find the set of model parameters that minimizes the difference between the model's output and the observed patient data. Use information criteria (e.g., Akaike Information Criterion) to select the best model from multiple candidates [82] [83].
- Prediction and Validation: Run the calibrated model forward in time to generate a forecast (e.g., of tumor growth or treatment response). Validate the prediction by comparing it to a subsequent, unseen clinical measurement (e.g., a follow-up imaging scan). Metrics like the Brier score and concordance index are used for time-to-event predictions [81] [82].
- Hybridization (Bayesian Coupling): In a hybrid framework, the mechanistic model's prediction is used as an informative prior in a Bayesian statistical model. This prior is then updated with other "unmodelable" patient-specific data (e.g., from omics or EHR) to produce a posterior distribution that represents the final, refined prediction [79].
Mechanistic & Hybrid Model Workflow
The Scientist's Toolkit: Key Research Reagents and Solutions
The following table details essential resources and their functions in developing and validating tumor models.
Table 3: Essential Research Reagents and Resources for Tumor Modeling
| Reagent / Resource | Function in Modeling | Specific Examples / Notes |
|---|---|---|
| The Cancer Genome Atlas (TCGA) | Provides large-scale genomic and clinical data for training and benchmarking AI/ML models [7] [80]. | Contains molecular profiles of over 11,000 tumors across 33 cancer types [7]. |
| Multiparametric Medical Imaging | Used to initialize and calibrate mechanistic models with patient-specific tissue properties [20] [83]. | DW-MRI (cellularity), DCE-MRI (perfusion), FDG-PET (metabolism), FMISO-PET (hypoxia) [83]. |
| Electronic Health Records (EHR) | Source of structured and unstructured clinical data for multimodal AI models and outcome validation [7] [62]. | Includes clinical notes, lab results, treatment schedules, and patient outcomes [62]. |
| Support Vector Machine (SVM) | A machine learning algorithm used for classification tasks, such as predicting patient drug response [80]. | Often combined with Recursive Feature Elimination (SVM-RFE) to identify predictive gene sets [80]. |
| Convolutional Neural Network (CNN) | A class of deep learning model ideal for analyzing image-based data, such as histopathology slides or radiology scans [7] [85]. | Used for automated IHC scoring and detection of abnormalities in medical images [7] [85]. |
| Bayesian Inference Frameworks | The mathematical foundation for hybrid models that couple mechanistic predictions with other data sources [79]. | Enables the creation of a posterior prediction that integrates a mechanistic prior with clinical data [79]. |
The field of oncology is undergoing a paradigm shift in how patient outcomes are modeled and predicted. Traditional mechanistic models are built on established biological and physical principles, utilizing mathematical equations to describe explicit processes like drug pharmacokinetics and tumor growth dynamics [75]. These models, including physiologically based pharmacokinetic (PBPK) models, rely on a priori knowledge of the underlying system [75]. In contrast, artificial intelligence (AI) and machine learning (ML) approaches are data-driven, discovering complex patterns and relationships directly from large-scale clinical, pathological, and imaging datasets without requiring pre-specified mechanistic rules [75] [7]. This case study delves into a direct comparison of these competing paradigms by examining their application to a critical clinical challenge: predicting overall survival in patients with hepatocellular carcinoma (HCC). We will analyze the performance of various AI models, detail their experimental protocols, and situate their emergence within the broader context of tumor modeling research.
Performance Comparison of AI Models in HCC
Recent studies have systematically evaluated a wide array of AI models for HCC survival prediction, demonstrating their potential to augment clinical decision-making. The table below summarizes the performance of key models from recent clinical studies.
Table 1: Performance of AI Models in HCC Survival Prediction from Clinical Studies
| Study Focus | Best Performing Model(s) | Key Performance Metrics | Dataset & Cohort Size |
|---|---|---|---|
| OS in Advanced HCC receiving Immunoradiotherapy [11] | StepCox (forward) + Ridge | C-index: 0.68 (training), 0.65 (validation);1-year AUC: 0.72; 2-year AUC: 0.75; 3-year AUC: 0.74 [11] | 175 patients (115 RT, 60 non-RT) |
| OS across all HCC stages [86] | Medium Gaussian SVM (with feature selection) | Accuracy for predicting mortality: 87.8% [86] | 393 patients (stages 1-4) |
| Post-surgical Recurrence from Histopathology [87] | HCC-SurvNet (Deep CNN) | C-index: 0.724 (internal test), 0.683 (external test) [87] | 299 (development), 53 (internal test), 198 (external test) patients |
| Disease-Specific Survival across 16 Cancers [33] | MUSK (Multimodal Foundation Model) | Accuracy for prognosis: 75% (vs. 64% for clinical standards) [33] | Training on The Cancer Genome Atlas |
Beyond these specific implementations, the fundamental advantage of AI models lies in their ability to integrate and find complex, non-linear patterns within multimodal data. This includes clinical variables, pathology reports, and medical images, often leading to more accurate predictions than traditional staging systems or single-biomarker tests [33] [7]. For instance, the MUSK model, which leverages both images and text, demonstrated a significant improvement (about 12%) in predicting melanoma recurrence compared to other models and more accurately identified patients who would benefit from immunotherapy compared to the standard PD-L1 biomarker test [33].
Experimental Protocols and Model Methodologies
The development and validation of robust AI models follow a rigorous pipeline, from data curation to final validation. The workflow for a typical histopathology-based deep learning model is illustrated below.
Diagram 1: AI Model Development Workflow for HCC Prognosis
Data Acquisition and Preprocessing
The foundation of any AI model is high-quality, well-annotated data. Key data types and their sources include:
- Digital Histopathology Images: Formalin-fixed, paraffin-embedded (FFPE) liver resection samples are stained with hematoxylin and eosin (H&E) and digitized into Whole Slide Images (WSIs) [87]. A critical preprocessing step involves using a convolutional neural network (CNN) to automatically detect and select tiles containing tumor tissue from the vast WSI, a process trained on tens to hundreds of thousands of manually annotated tiles [87].
- Structured Clinical Data: Demographic, laboratory, and treatment data are routinely collected from electronic health records. In a large nomogram study, this included variables such as age, HCC screening status, alcoholic liver disease, Child-Pugh grade, tumor size, and treatment method [88].
- Multimodal Data: Advanced models like MUSK are trained on "unpaired multimodal data," which expands the available training pool by using images and text that are related but not necessarily from the exact same case [33].
Feature Selection and Model Training
Identifying the most predictive variables is a crucial step. Common techniques include:
- Clinical Variable Selection: Studies often use univariate Cox regression to identify prognostic factors (e.g., Child-Pugh class, BCLC stage, tumor size) with a significance level of p < 0.05, which are then used for multivariate analysis and model building [11] [88]. Other feature selection methods like Minimum Redundancy Maximum Relevance (MRMR), Chi-square, ANOVA, and Kruskal-Wallis tests are also employed to select the most informative features from a larger set [86].
- Model Training and Comparison: Researchers typically evaluate a wide array of ML algorithms. One study compared 101 different ML algorithms, finding the StepCox (forward) + Ridge model to be superior [11]. Another common approach is to use binary classification (e.g., predicting 6-month, 1-year, 2-year, and 3-year survival) with models like Weighted KNN, Medium Gaussian Support Vector Machines (SVM), and neural networks [86].
Validation and Performance Assessment
Rigorous validation is essential to ensure model generalizability. Standard practices include:
- Data Splitting: Patients are randomly divided into a training cohort (e.g., 60-78%) and a validation/internal test cohort (e.g., 22-40%) with no patient overlap between sets [11] [87].
- External Validation: The highest level of validation involves testing the model on a completely independent dataset from a different institution [87].
- Performance Metrics: Key metrics include the Concordance Index (C-index) to assess the model's overall ranking ability, time-dependent Area Under the Receiver Operating Characteristic Curve (AUC) to measure classification accuracy at specific timepoints, and Kaplan-Meier analysis with log-rank tests to evaluate the model's ability to stratify patients into distinct risk groups [11] [87].
The Scientist's Toolkit: Key Research Reagents and Solutions
Successfully developing an AI model for HCC prognosis requires a suite of computational and data resources.
Table 2: Essential Research Tools for AI-Driven HCC Survival Analysis
| Tool / Solution | Function in Research | Specific Examples / Notes |
|---|---|---|
| Digital Whole Slide Scanner | Converts glass pathology slides into high-resolution digital images for computational analysis. | Essential for creating the dataset used by deep learning models like HCC-SurvNet [87]. |
| Tumor-Annotated Datasets | Provides ground-truth data for training and validating tile classification CNNs. | e.g., Stanford-HCCDET with 128,222 tiles from 36 WSIs [87]. |
| Public Cancer Genomics Databases | Sources of large-scale, multimodal data for model training and external validation. | The Cancer Genome Atlas (TCGA) is widely used (e.g., TCGA-LIHC) [87] [7]. |
| Feature Selection Algorithms | Identifies the most relevant prognostic variables from a large pool of clinical data. | MRMR, Chi-square, ANOVA, and Kruskal-Wallis tests are commonly used [86]. |
| Multimodal Fusion Architectures | AI frameworks capable of integrating diverse data types (images, text, genomics). | Foundation models like MUSK leverage unpaired images and text for more robust predictions [33]. |
This case study demonstrates that AI and ML models are achieving robust performance in predicting HCC survival, often surpassing traditional clinical prognostic tools. The comparison reveals that while mechanistic models provide interpretability based on biological first principles, AI models excel at harnessing complex, high-dimensional data to generate highly accurate, personalized predictions. The future of tumor modeling lies not in choosing one paradigm over the other, but in their strategic integration. As suggested in Nature Reviews Cancer, mechanistic models can generate in-silico data to train AI systems, while AI can help refine the parameters of mechanistic models, creating a powerful synergistic loop to further improve patient stratification and treatment planning in oncology [75].
In modern oncology, computational models are becoming indispensable tools for personalizing radiotherapy, aiming to maximize tumor control while minimizing damage to healthy tissues. The field is largely defined by two complementary approaches: mechanistic models and AI-driven machine learning. Mechanistic models are physics-based and seek to simulate the underlying biological processes of tumor growth and treatment response using mathematical equations. In contrast, AI and machine learning are data-driven, identifying complex patterns from clinical datasets to make predictions without explicit programming of the underlying biology. This case study objectively compares these paradigms, focusing on their application in optimizing radiotherapy, supported by experimental data and detailed methodologies.
Comparative Performance Analysis of Modeling Approaches
The table below summarizes the core characteristics, performance, and validation of key studies representing both modeling paradigms.
Table 1: Performance and Characteristics of Radiotherapy Optimization Models
| Model Name / Type | Cancer Type | Key Performance Metrics | Comparative Outcome | Validation Method |
|---|---|---|---|---|
| Mechanistic (GliODIL) [89] | Glioblastoma | Recurrence coverage (compared to standard margin) | Consistently outperformed standard uniform margin plan | 152 patients with post-treatment follow-up for recurrence |
| AI/ML (StepCox + Ridge) [11] | Hepatocellular Carcinoma (HCC) | C-index: 0.68 (training), 0.65 (validation); 1-yr OS AUC: 0.72 | Superior among 101 tested ML algorithms for survival prediction | Internal validation on 40% hold-out cohort |
| AI/ML (Reinforcement Learning) [90] | Mesothelioma (Mouse Model) | Tumor Control Probability (TCP) | Exceeded TCP of 1-2 RT fractions; outperformed by baseline 2Gy/fraction schedule | Comparison with experimental results in a murine model |
| AI (iSeg Deep Learning) [91] [92] | Lung | Dice Score (DSC): 0.73 (Internal), 0.70-0.71 (External) | Matched human inter-observer variability; flagged regions linked to local failure | Multi-center validation across 9 clinics |
Experimental Protocols and Workflows
The Mechanistic Workflow: GliODIL for Glioma
The GliODIL framework exemplifies a modern, hybrid mechanistic approach for personalizing glioma radiotherapy. Its methodology integrates physics-based modeling with clinical data [89].
1. Data Acquisition and Preprocessing:
- Input Data: Pre-treatment multi-modal imaging, specifically Magnetic Resonance Imaging (MRI) and Fluoroethyl-L-Tyrosine Positron Emission Tomography (FET-PET).
- Processing: Tissue extraction via atlas registration and automatic tumor segmentation to delineate boundaries (edema, enhancing core, necrotic core).
2. Model Inference and Optimization:
- Core Physics Model: The framework uses a Fisher-Kolmogorov-type Reaction-Diffusion Partial Differential Equation (PDE) to describe tumor cell diffusion and proliferation.
- Inverse Problem Solving: GliODIL infers the full, patient-specific spatial distribution of tumor cell concentration by solving an inverse problem. It optimizes a discrete loss function that softly assimilates three key constraints:
- Physics Constraint (LPDE): Adherence to the Fisher-Kolmogorov growth model.
- Imaging Data Constraint (LDATA): Alignment with the observed patient MRI and FET-PET data.
- Initial Condition Constraint (L_IC): Assumptions about the initial focal origin of the tumor.
- Numerical Method: The ODIL technique employs a multi-resolution grid and automatic differentiation, enhancing computational speed over traditional methods.
3. Radiotherapy Planning:
- The output is a personalized map of tumor cell concentration.
- This map is used to define a non-uniform radiotherapy target volume, aiming to cover high-risk regions beyond the visible tumor, potentially replacing the standard uniform 1.5-2.0 cm margin.
The AI/ML Workflow: Survival Prediction in Liver Cancer
A study on advanced Hepatocellular Carcinoma (HCC) demonstrates a pure data-driven AI/ML workflow for predicting Overall Survival (OS) in patients receiving immunoradiotherapy [11].
1. Cohort Definition and Data Preparation:
- Patients: 175 advanced HCC patients were divided into a training cohort (60%) and a validation cohort (40%).
- Variables: Clinical features including "Child" (liver function), "BCLC stage," tumor "Size," and "Treatment" (with or without radiotherapy) were identified as key prognostic factors.
2. Model Training and Selection:
- Algorithm Screening: 101 different machine learning algorithms were trained on the training cohort to predict overall survival.
- Performance Evaluation: Models were assessed using the Concordance Index (C-index) and time-dependent Receiver Operating Characteristic (ROC) curves.
- Model Selection: The "StepCox (forward) + Ridge" model was selected as the best performer based on its validation metrics.
3. Clinical Validation and Application:
- The model's predictive power was confirmed on the independent validation cohort.
- The resulting risk score can stratify patients into high- or low-risk groups, potentially informing personalized treatment decisions.
Visualizing the Modeling Pathways
The following diagrams, generated with Graphviz DOT language, illustrate the logical workflows and signaling pathways central to these modeling approaches.
Signaling Pathways in Tumor Response
This diagram visualizes the core biological and physical signaling pathways that mechanistic models often seek to represent, connecting radiotherapy to tumor control and toxicity.
Model Integration Workflow
This diagram outlines the integrated workflow of the GliODIL framework, showing how data and physics are combined to inform radiotherapy planning.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The table below details key computational tools, models, and data types that form the essential "reagent solutions" for research in this field.
Table 2: Key Research Reagent Solutions for Radiotherapy Modeling
| Tool/Reagent | Type | Primary Function | Example Use Case |
|---|---|---|---|
| Fisher-Kolmogorov PDE | Mechanistic Model | Describes tumor cell diffusion and proliferation to simulate spatiotemporal growth. | Predicting invisible tumor infiltration in glioblastoma [89]. |
| Reinforcement Learning (e.g., Deep Q-Network) | AI/ML Model | Learns optimal treatment scheduling policies through interaction with a simulated environment. | Optimizing combination therapy schedules in preclinical models [90]. |
| 3D UNet (iSeg) | AI/ML Model (Deep Learning) | Automates 3D segmentation of tumors on medical images, accounting for motion. | Delineating lung tumors across respiratory motion in 4D CT scans [91] [92]. |
| Multi-modal Imaging (MRI/FET-PET) | Data Source | Provides complementary structural (MRI) and metabolic (FET-PET) information on tumors. | Informing mechanistic models to infer tumor cell density [89]. |
| Genomically Adjusted Radiation Dose (GARD) | Biomarker / Metric | A genomics-based metric that predicts tumor radiosensitivity and personalizes dose prescription. | Connecting tumor gene expression patterns to radiation dose-response [93]. |
| Radiomics Feature Extractors (e.g., PyRadiomics) | Software Tool | Extracts quantitative, sub-visual features from medical images for model building. | Developing predictive models for tumor differentiation or treatment toxicity [70] [94]. |
Discussion and Future Directions
The comparative analysis reveals that mechanistic models and AI/ML are not mutually exclusive but are increasingly synergistic. Mechanistic models like GliODIL offer high interpretability by grounding predictions in established physics and biology, which is crucial for clinical trust and generating hypotheses about tumor growth [89]. Their ability to perform well even with limited data points (e.g., a single time point) is a significant strength. In contrast, AI/ML models excel at identifying complex, non-linear patterns from large, multimodal datasets, achieving state-of-the-art performance in specific tasks like image segmentation and survival prediction [11] [91].
A key limitation of pure AI models is their "black box" nature and the challenge of robust error control, which hinders clinical adoption for high-stakes decisions [89]. Furthermore, they require large, well-annotated datasets, which are often scarce in radiation oncology [93]. Mechanistic models, while interpretable, can be computationally intensive and may rely on simplifications of complex biology.
The most promising future direction lies in hybrid frameworks that integrate both paradigms. The GliODIL framework itself is a prime example, blending a physics-based PDE with data-driven optimization to constrain its solutions [89]. Similarly, the concept of "digital twins" – patient-specific computer simulations that can be updated with real-time data – represents the ultimate expression of this synergy, promising a future where radiotherapy is continuously adapted to the individual patient's evolving disease [93].
The field of computational oncology stands at a pivotal crossroads, marked by the convergence of two powerful modeling paradigms: mechanistic models rooted in biological first principles and data-driven artificial intelligence (AI) approaches. While mechanistic models encode known physics and biology of tumor growth and treatment response, AI/machine learning (ML) excels at identifying complex patterns from large-scale multimodal datasets. Digital twin technology represents the synthesis of these approaches, creating dynamic virtual representations of individual patients' tumors that can be updated with real-time clinical data to predict disease progression and optimize therapeutic interventions [95] [96]. The clinical adoption of this technology, however, hinges on addressing significant challenges in validation, regulatory approval, and seamless integration into clinical workflows.
The potential impact of digital twins is magnified by the profound heterogeneity of cancer, which manifests as genetic, molecular, and spatial variations between tumors and even within a single tumor. This heterogeneity contributes significantly to treatment resistance and therapeutic failure [95]. Digital twins aim to overcome these challenges by enabling truly personalized therapy selection through in silico testing of various treatment strategies against a virtual replica of the patient's tumor, thereby potentially improving outcomes while reducing exposure to ineffective treatments and their associated toxicities [20] [96].
The Modeling Spectrum: Mechanistic Models vs. AI/ML Approaches
Fundamental Philosophies and Technical Implementations
Mechanistic models and AI/ML approaches differ fundamentally in their underlying philosophy, data requirements, and interpretability. The table below summarizes the core characteristics of each approach and their emerging hybridizations.
Table 1: Comparison of Modeling Approaches in Computational Oncology
| Feature | Mechanistic Models | AI/ML Approaches | Hybrid Models |
|---|---|---|---|
| Foundation | Biological first principles, physics | Statistical patterns in data | Integration of both paradigms |
| Interpretability | High (transparent causality) | Low ("black box") | Variable (context-dependent) |
| Data Requirements | Lower (but requires domain knowledge) | Very high (large datasets) | Moderate to high |
| Strength | Prediction outside training data; hypothesis testing | Pattern recognition in complex datasets | Improved prediction with biological plausibility |
| Limitation | May oversimplify biology | Limited generalizability beyond training data | Implementation complexity |
| Clinical Translation | Emerging (e.g., digital twins) | Rapid for diagnostic imaging | Pioneering (e.g., clinical trial optimization) |
Mechanistic models attempt to mathematically represent known biological processes governing tumor behavior. These include agent-based models (ABMs) that simulate individual cells and their interactions, and reaction-diffusion equations that describe the spatial and temporal dynamics of nutrients, growth factors, and therapeutic agents within the tumor microenvironment [5]. For example, mechanistic models have been developed to simulate key pathways such as the ErbB receptor-mediated Ras-MAPK and PI3K-AKT signaling pathways, and the p53-mediated DNA damage response pathway, which are crucial in understanding cancer cell proliferation and apoptosis [95].
In contrast, AI/ML models are predominantly data-driven, learning statistical relationships from large datasets without requiring explicit programming of biological rules. These include deep learning architectures that can process high-dimensional data such as medical images and genomic sequences [20]. However, their "black box" nature often limits clinical trust and interpretability, as they may produce accurate predictions without revealing the underlying biological mechanisms [95].
The Emergence of Hybrid Frameworks
Hybrid frameworks are emerging as the most promising path forward, leveraging the strengths of both approaches. In these frameworks, mechanistic models provide the biological scaffolding, while AI/ML techniques enhance computational efficiency and enable parameter estimation from complex data [5]. For instance, AI can create efficient "surrogate models" of computationally intensive mechanistic models, enabling rapid parameter exploration and uncertainty quantification that would be infeasible with the original models [95] [5]. Alternatively, biological constraints derived from mechanistic knowledge can inform AI architectures, improving their interpretability and ensuring consistency with established cancer biology [5].
Table 2: Digital Twin Applications Across Cancer Types and Clinical Use Cases
| Cancer Type | Modeling Approach | Clinical Application | Reported Outcome/Goal |
|---|---|---|---|
| High-Grade Glioma | Mechanism-based (TumorTwin) [97] | Radiation therapy optimization | Personalized treatment planning based on quantitative MRI |
| Triple-Negative Breast Cancer (TNBC) | Integrated MRI-biomath models [96] | Neoadjuvant chemotherapy response prediction | Superior prediction of pathological complete response (pCR) vs. traditional volume metrics |
| Pediatric Cancers | Spatial-temporal sensing computer model [96] | Identify efficient, low-toxicity treatments | First model sensing development of normal and malignant tumors (in development) |
| Uterine Cancer | Black-box digital twin model [96] | Personalized care planning | Exploration of personalized treatment strategies |
| Various Cancers | ABM with cellular systems biology [95] | Therapy optimization across tumor types | Understanding how tumor microenvironment influences therapeutic efficacy |
Digital Twins: From Virtual to Clinical Reality
Conceptual Framework and Workflow
A cancer digital twin is defined by the National Academies of Sciences, Engineering, and Medicine as "a set of virtual information constructs that mimics the structure, context, and behavior of a natural or engineered system, dynamically updated with data from its physical counterpart, with predictive capabilities to inform decision-making" [95]. In clinical oncology, this translates to a dynamic computational model of an individual patient's tumor that is continually updated with clinical data and can simulate response to various therapeutic interventions.
The following diagram illustrates the core conceptual framework and iterative workflow of a cancer digital twin:
Diagram Title: Conceptual Framework of a Cancer Digital Twin
This framework highlights the bidirectional data flow essential to digital twins: clinical data initializes and updates the model, while simulation outputs inform clinical decisions, creating a continuous feedback loop that refines both the virtual model and physical-world treatment.
Current Research Landscape and Clinical Applications
Research into digital twins for oncology has surged since 2020, with significant contributions from the United States, Germany, Switzerland, and China [96]. Funding primarily comes from government agencies, notably the U.S. National Institutes of Health and National Cancer Institute, which have initiated collaborative projects with the Department of Energy to advance patient-specific cancer digital twins [96].
Digital twins are being explored across diverse clinical applications in oncology:
- Treatment Response Prediction: For triple-negative breast cancer (TNBC), models integrating MRI data with biologically-based mathematical models have outperformed traditional tumor volume measurements in predicting pathological complete response to neoadjuvant chemotherapy [96].
- Radiation Therapy Optimization: Frameworks like TumorTwin leverage quantitative MRI data to create patient-specific models of high-grade glioma growth and response to radiation therapy, enabling personalized treatment planning [97].
- Surgical Planning: Digital twins can simulate procedures using real-time hemodynamic data, allowing clinicians to evaluate multiple surgical options and reduce operative risks [98].
- Clinical Trial Optimization: In clinical trials, digital twins can serve as virtual control arms or simulate patient responses to treatments, potentially reducing the need for extensive human trials and accelerating therapeutic development [99] [98].
The Validation Imperative: Protocols and Reproducibility
Verification, Validation, and Uncertainty Quantification (VVUQ)
For digital twins to achieve clinical adoption, they must undergo rigorous verification, validation, and uncertainty quantification (VVUQ). Verification ensures the computational model is solved correctly, while validation determines how accurately the model represents the real-world biological system. Uncertainty quantification characterizes the limitations and confidence intervals of model predictions [95].
The complexity and multiscale nature of cancer biology presents significant challenges for VVUQ. A model may be well-validated at the tissue scale (e.g., predicting tumor volume on imaging) but poorly validated at the cellular or molecular scale (e.g., predicting immune cell infiltration). Furthermore, the dynamic recalibration of digital twins with new patient data introduces additional validation complexities not present in static models [95] [5].
Experimental Protocols for Model Validation
Robust validation requires standardized experimental protocols that systematically compare model predictions with clinical outcomes. The following workflow illustrates a comprehensive validation approach for a therapeutic response model:
Diagram Title: Digital Twin Model Validation Workflow
Key components of digital twin validation include:
- Multi-fidelity Validation: Comparing predictions against data at multiple biological scales (molecular, cellular, tissue) and temporal resolutions (short-term vs. long-term outcomes) [95] [5].
- Prospective Validation: Testing model predictions against future clinical outcomes in a controlled trial setting, which provides stronger evidence than retrospective validation alone [96].
- Uncertainty Propagation: Quantifying how measurement errors in input data (e.g., imaging noise, assay variability) affect the confidence in model predictions [95].
- Sensitivity Analysis: Identifying which model parameters most significantly influence outcomes, helping prioritize which biological processes require most accurate measurement [95].
Large-sample studies (e.g., those utilizing comprehensive data resources like Flatiron Health's Panoramic datasets with 1.5 billion data points) provide greater statistical power for validation, while small-sample studies often focus on validating the technological approach in specific patient subgroups [100] [96].
Navigating the Regulatory and Clinical Implementation Landscape
Regulatory Hurdles and Adoption Barriers
The regulatory pathway for digital twins as clinical decision support tools remains uncertain and complex. Key challenges include:
- Algorithmic Transparency: Regulatory agencies like the FDA must evaluate "black box" AI algorithms where the decision-making process may not be fully interpretable [5].
- Dynamic Model Evolution: Unlike traditional medical devices, digital twins continuously learn and adapt from new patient data, creating challenges for regulatory frameworks designed for static devices [98] [5].
- Clinical Validation Burden: Demonstrating improved patient outcomes requires extensive clinical validation, which is resource-intensive and time-consuming [5] [96].
- Reimbursement Mechanisms: Current medical billing models are designed to reimburse for services rendered after diagnosis, not for predictive care interventions based on digital twin simulations [98]. As of 2025, with only 23 AI-specific CPT codes available compared to over 950 FDA-approved AI devices, the majority of AI-enhanced tools, including digital twins, lack standardized billing mechanisms [101].
Additional adoption barriers identified in the 2025 landscape include immature tools (77% of health systems), financial concerns (47% of providers), lack of reimbursement pathways (40%), healthcare integration complexity, and trust/regulatory uncertainty [101].
Implementation Strategies and Ecosystem Readiness
Successful implementation of digital twins requires addressing both technical and ecosystem challenges:
- Phased Implementation: Starting with pilot projects in specific clinical domains (e.g., radiation oncology) before expanding to broader applications [98].
- Workflow Integration: Seamlessly embedding digital twin technologies into existing clinical workflows and electronic health record systems to minimize disruption [101] [98].
- Interdisciplinary Collaboration: Establishing teams that include clinicians, data scientists, engineers, and administrators to bridge expertise gaps [5] [96].
- Data Infrastructure: Building robust data pipelines capable of handling multimodal data from EHRs, medical imaging, genomics, and wearable devices while ensuring interoperability [97] [96].
The broader ecosystem is evolving to support digital twin implementation through initiatives like the American Medical Association's development of new CPT codes for AI-augmentative services and the FDA's work on adaptive frameworks for AI/ML-based software as a medical device [101].
Essential Research Toolkit for Digital Twin Development
The development and validation of cancer digital twins requires a sophisticated toolkit spanning data acquisition, computational modeling, and validation infrastructure. The table below details key research reagents and resources essential for the field.
Table 3: Essential Research Reagent Solutions for Digital Twin Development
| Category | Specific Tools/Resources | Function/Role | Implementation Example |
|---|---|---|---|
| Computational Frameworks | TumorTwin [97], PhysiCell [5], HAL [97] | Provide modular environments for building, calibrating, and testing digital twin models | TumorTwin enables composition of different data, model, and solver objects for rapid prototyping |
| Data Resources | The Cancer Genome Atlas (TCGA) [95], Flatiron Panoramic [100], CPTAC [95] | Supply multimodal, longitudinal data for model training and validation | Flatiron's 1.5B+ data points enable validation with long patient follow-up |
| Imaging Data | Quantitative MRI (ADC maps) [97], DW-MRI, DCE-MRI [20], PET [20] | Provide spatial, physiological, and metabolic data for model personalization | Apparent Diffusion Coefficient (ADC) from DW-MRI informs cellularity in glioma models |
| Molecular Data | Single-cell sequencing [95], multi-omics [95], ATR-FTIR spectroscopy [20] | Enable characterization of intratumoral heterogeneity at cellular resolution | Single-cell sequencing profiles genetically distinct tumor sub-populations |
| Validation Benchmarks | Expert-curated datasets [100], synthetic patient datasets [97] | Serve as gold standards for validating AI/ML and mechanistic models | Flatiron's decade of expert-curated data validates AI-enabled data elements |
The clinical adoption of digital twins in oncology represents a paradigm shift from reactive to predictive, personalized medicine. While significant challenges remain in validation, regulatory approval, and clinical implementation, the convergence of mechanistic modeling and AI/ML approaches offers a promising path forward. Success will require continued interdisciplinary collaboration, development of standardized validation frameworks, and adaptive regulatory pathways that can accommodate the dynamic nature of digital twin technologies.
The most immediate applications are likely in treatment optimization for specific cancers like high-grade glioma and triple-negative breast cancer, where modeling approaches have already demonstrated clinical utility. As the technology matures and overcomes validation and regulatory hurdles, digital twins have the potential to become integral tools in clinical oncology, enabling truly personalized therapy selection and optimizing outcomes for cancer patients.
Conclusion
The future of computational oncology lies not in choosing between mechanistic and AI models, but in strategically leveraging their complementary strengths. Mechanistic models provide a foundational, interpretable understanding of tumor biology, while AI excels at identifying complex patterns within large, multimodal datasets. The most promising path forward involves the development of hybrid frameworks, where AI can estimate parameters for mechanistic models or act as efficient surrogates, and mechanistic principles can inform and constrain AI architectures. Overcoming challenges related to data quality, model interpretability, and rigorous clinical validation is paramount. Ultimately, this synergistic approach is poised to power the next generation of predictive tools, including patient-specific 'digital twins,' ushering in a new era of truly personalized and optimized cancer therapy.
References
- 1. Frontiers | A review of mechanistic learning in mathematical oncology [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1363144/full]
- 2. -based and machine learning Comparing for... mechanism models [https://pmc.ncbi.nlm.nih.gov/articles/PMC10300192/]
- 3. A mechanistic reveals the key principles... modeling framework [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1009841]
- 4. Frontiers | A mechanistic quantitative systems pharmacology model ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1571844/full]
- 5. Challenges and opportunities for the next generation of... | PLOS Biology [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003269]
- 6. Current AI technologies in cancer diagnostics and treatment | Molecular Cancer | Full Text [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 7. Artificial Intelligence Advancements in Oncology: A Review of Current Trends and Future Directions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025054/]
- 8. Frontiers | The Role of AI in GU Oncology : From Data Complexity to... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1588967/abstract]
- 9. How Artificial Intelligence Is Transforming Cancer Care in ... [https://oncodaily.com/oncolibrary/artificial-intelligence-ai]
- 10. Artificial intelligence in cancer: applications, challenges, and future perspectives | Molecular Cancer | Full Text [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02450-3]
- 11. Frontiers | Performance of AI -based machine learning models for... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1719479/full]
- 12. Artificial Intelligence in Cancer Drug Discovery in 2025 - OncoDaily [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 13. Artificial intelligence in oncology: current applications and future perspectives | British Journal of Cancer [https://www.nature.com/articles/s41416-021-01633-1]
- 14. A Review of Mathematical Models for Tumor Dynamics and Treatment Resistance Evolution of Solid Tumors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6813171/]
- 15. 6 Comparing | Statistical models modelling [https://bookdown.org/btmarti25/FD2E/comparing-models.html]
- 16. - Hypothesis probabilistic driven enables a principled... modelling [https://pmc.ncbi.nlm.nih.gov/articles/PMC9943678/]
- 17. of Limitations in Predictive Correlation Models [https://www.linkedin.com/advice/1/what-limitations-using-correlation-coefficients-xrdue]
- 18. . Causation | Difference, Designs & Examples Correlation vs [https://www.scribbr.com/methodology/correlation-vs-causation/]
- 19. Combining hypothesis - and data- driven neuroscience modeling in... [https://elifesciences.org/articles/69013]
- 20. Patient-specific, mechanistic models of tumor growth incorporating artificial intelligence and big data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10491321/]
- 21. Adopting a Hypothesis - Driven Workflow | Medium Modeling [https://medium.com/data-science/adopting-a-hypothesis-driven-modeling-workflow-9edc8b80a8ed]
- 22. in machine learning — All you need to know | Medium Correlation [https://medium.com/@abdallahashraf90x/all-you-need-to-know-about-correlation-for-machine-learning-e249fec292e9]
- 23. Imaging genomics of cancer: a bibliometric analysis and review [https://pmc.ncbi.nlm.nih.gov/articles/PMC11877899/]
- 24. Biomedical informatics and machine learning for clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5946905/]
- 25. TCGA - Data Types Collected - NCI [https://www.cancer.gov/ccg/research/genome-sequencing/tcga/using-tcga-data/types]
- 26. Large language models enable tumor-type classification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490231/]
- 27. Core variables for real-world clinicogenomic data ... [https://www.sciencedirect.com/science/article/pii/S2949820125000062]
- 28. A machine learning approach to leveraging electronic ... [https://www.nature.com/articles/s42256-024-00974-9]
- 29. Predicting time-to-first cancer diagnosis across multiple ... [https://www.nature.com/articles/s41598-025-08790-w]
- 30. Analysing the Structural Identifiability and Observability of Mechanistic ... [https://www.mdpi.com/2306-5354/12/10/1048]
- 31. Frontiers | Exploring the role of artificial intelligence in chemotherapy development, cancer diagnosis, and treatment: present achievements and future outlook [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1475893/full]
- 32. AI in MRI brain tumor diagnosis: A systematic review of machine learning and deep learning advances (2010–2025) - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0169743925000991]
- 33. Unique Stanford Medicine-designed AI predicts cancer prognoses, responses to treatment [https://med.stanford.edu/news/all-news/2025/01/ai-cancer-prognosis.html]
- 34. Mechanistic Learning with Guided Diffusion Models to Predict Spatio-Temporal Brain Tumor Growth [https://arxiv.org/html/2509.09610]
- 35. Application of GFP imaging in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4383682/]
- 36. The clinical application of artificial intelligence in cancer precision... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06139-5]
- 37. Clinical applications of artificial intelligence and machine learning in cancer diagnosis: looking into the future | Cancer Cell International | Full Text [https://cancerci.biomedcentral.com/articles/10.1186/s12935-021-01981-1]
- 38. Machine Learning and AI in Cancer Prognosis, Prediction, and Treatment Selection: A Critical Approach - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10312208/]
- 39. Frontiers | Comparative accuracy of different artificial... diagnostic [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1670843/full]
- 40. Integrating artificial intelligence into radiological cancer imaging: from diagnosis and treatment response to prognosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11795265/]
- 41. Multimodal AI Predicts Melanoma Metastasis Using Microenvironment [https://bioengineer.org/multimodal-ai-predicts-melanoma-metastasis-using-microenvironment/]
- 42. Interpretable artificial intelligence in radiology and radiation oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10546466/]
- 43. Top Oncology Innovations That Shaped the First Half of 2025 | Cancer ... [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 44. The Use of Artificial Intelligence (AI) in the Radiology Field: What Is the State of Doctor–Patient Communication in Cancer Diagnosis? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856827/]
- 45. Tool May Help Guide Use of Cancer AI - NCI Immunotherapy [https://www.cancer.gov/news-events/cancer-currents-blog/2025/ai-predicts-cancer-immunotherapy-response-survival]
- 46. Generalizable AI predicts immunotherapy outcomes across cancers and treatments | medRxiv [https://www.medrxiv.org/content/10.1101/2025.05.01.25326820v1]
- 47. ESMO 2025 : Lunit’s AI tool predicts ... immunotherapy response [https://www.medicaldevice-network.com/news/esmo-2025-lunit-ai-tool-predicts-immunotherapy-response-across-cancer-types/]
- 48. Artificial intelligence-assisted PET imaging for predicting neoadjuvant... [https://pubmed.ncbi.nlm.nih.gov/40960690/]
- 49. A comprehensive review of computational cell cycle models in guiding cancer treatment strategies | npj Systems Biology and Applications [https://www.nature.com/articles/s41540-024-00397-7]
- 50. Modeling methods of different tumor organoids and their application in tumor drug resistance research [https://www.oaepublish.com/articles/cdr.2025.34]
- 51. A hybrid modeling approach for assessing mechanistic of... models [https://www.nature.com/articles/s41598-021-90637-1?error=cookies_not_supported&code=a36f4ddc-e98f-436c-84f6-fdab6c1eb5e9]
- 52. Application of Artificial Intelligence In Drug-target Interactions Prediction: A Review | npj Biomedical Innovations [https://www.nature.com/articles/s44385-024-00003-9]
- 53. The State of Adopting AI in Drug in Discovery 2025 [https://chemaxon.com/blog/ai-in-drug-discovery]
- 54. Revolutionizing drug discovery: Integrating artificial intelligence with quantitative systems pharmacology - PubMed [https://pubmed.ncbi.nlm.nih.gov/40774584/]
- 55. PMLB: a large benchmark suite for machine learning evaluation and comparison | BioData Mining | Full Text [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-017-0154-4]
- 56. Artificial Intelligence in Drug Market to Hit USD 13.6 Bn Discovery [https://media.market.us/artificial-intelligence-in-drug-discovery-market-news-2025/]
- 57. How Open Targets is using Artificial Intelligence and Machine Learning to identify and prioritise drug targets [https://blog.opentargets.org/machine-learning-for-drug-target-identification-and-prioritisation-at-open-targets/]
- 58. UI researchers create AI-powered drug development tool - The Daily Illini [https://dailyillini.com/news-stories/science-technology/2025/11/15/ui-researchers-create-ai-powered-drug-development-tool/]
- 59. Improving personalized tumor growth predictions using a Bayesian combination of mechanistic modeling and machine learning | Communications Medicine [https://www.nature.com/articles/s43856-021-00020-4]
- 60. [2308.14925] Patient-specific, mechanistic models of tumor growth incorporating artificial intelligence and big data [https://arxiv.org/abs/2308.14925]
- 61. Frontiers | Multimodal data integration for oncology in the era of deep neural networks: a review [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2024.1408843/full]
- 62. Emerging artificial intelligence-driven precision therapies in tumor drug resistance: recent advances, opportunities, and challenges | Molecular Cancer | Full Text [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02321-x]
- 63. Multi channel fusion diffusion models for brain tumor MRI data ... [https://www.nature.com/articles/s41598-025-06529-1?error=cookies_not_supported&code=126640b9-f6ff-4958-a65e-ffc906c90aac]
- 64. Synthesizing 3D Multi-Contrast Brain Tumor MRIs Using Tumor Mask... [https://pubmed.ncbi.nlm.nih.gov/38715792/]
- 65. Artificial Intelligence in Cancer Research and Precision Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8034385/]
- 66. Using mathematical modelling and AI to improve delivery and efficacy of therapies in cancer | Nature Reviews Cancer [https://www.nature.com/articles/s41568-025-00796-w]
- 67. Explainability AI : LLM Transparency & CoT Techniques 2025 [https://futureagi.com/blogs/ai-explainability-tools-techniques-2025]
- 68. Evaluating AI in Models : More Than Just Numbers 2025 [https://www.linkedin.com/pulse/evaluating-ai-models-2025-more-than-just-numbers-joe-abraham-pmp--vjaec]
- 69. How Explainable AI Drives Enterprise Trust, Compliance & Competitive... [https://www.firstaimovers.com/p/ai-interpretability-enterprise-transparency]
- 70. Frontiers | Comparative analysis of deep learning and radiomics models in predicting hepatocellular carcinoma differentiation via ultrasound [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1685725/full]
- 71. Frontiers | Assessing the role of model choice in parameter identifiability of cancer treatment efficacy [https://www.frontiersin.org/journals/applied-mathematics-and-statistics/articles/10.3389/fams.2025.1542617/full]
- 72. Top 8 Machine Learning Model Tools in Deployment 2025 [https://www.truefoundry.com/blog/model-deployment-tools]
- 73. Top 10 AI Model Platforms Tools in Deployment : Features, Pros... 2025 [https://www.devopsschool.com/blog/top-10-ai-model-deployment-platforms-tools-in-2025-features-pros-cons-comparison/]
- 74. Cloud Deployment in Models : The Smart Way... - Wikitechy 2025 [https://www.wikitechy.com/cloud-deployment-models-cloud-service-models/]
- 75. Using mathematical modelling and AI to... | Nature Reviews Cancer [https://www.nature.com/articles/s41568-025-00796-w?error=cookies_not_supported&code=cb98d75a-6341-4fb7-9b92-23acd2237b33]
- 76. Learning with Guided Diffusion Mechanistic to Predict... Models [https://arxiv.org/html/2509.09610v1]
- 77. The AI revolution: how multimodal intelligence will reshape the oncology ecosystem | npj Artificial Intelligence [https://www.nature.com/articles/s44387-025-00044-4]
- 78. Frontiers | Application progress of artificial intelligence in tumor diagnosis and treatment [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2024.1487207/full]
- 79. Improving personalized tumor growth predictions using a Bayesian... [https://www.nature.com/articles/s43856-021-00020-4?error=cookies_not_supported]
- 80. Machine learning predicts individual cancer patient responses to therapeutic drugs with high accuracy | Scientific Reports [https://www.nature.com/articles/s41598-018-34753-5]
- 81. Hybridizing mechanistic mathematical modeling with deep learning... [https://pubmed.ncbi.nlm.nih.gov/38586046/]
- 82. Validating the predictions of mathematical models describing tumor growth and treatment response - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11888553/]
- 83. Mechanism-Based Modeling of Tumor Growth and Treatment Response Constrained by Multiparametric Imaging Data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6535803/]
- 84. Evolving and Novel Applications of Artificial Intelligence in Cancer Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070983/]
- 85. Convergence of evolving artificial intelligence and machine learning techniques in precision oncology | npj Digital Medicine [https://www.nature.com/articles/s41746-025-01471-y]
- 86. hepatocellular carcinoma Predicting with artificial intelligence survival [https://www.nature.com/articles/s41598-025-90884-6?error=cookies_not_supported&code=12dd61fc-e293-4425-bbfe-58859fdb96ff]
- 87. Deep learning predicts postsurgical recurrence of hepatocellular carcinoma from digital histopathologic images | Scientific Reports [https://www.nature.com/articles/s41598-021-81506-y]
- 88. Construction of a survival prediction model for patients with hepatocellular carcinoma (HCC) based on real clinical data: a single-center retrospective study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078820/]
- 89. Individualizing glioma radiotherapy planning by optimization of a data and physics-informed discrete loss | Nature Communications [https://www.nature.com/articles/s41467-025-60366-4]
- 90. Reinforcement learning with mechanistic to models ... optimise [https://research-repository.uwa.edu.au/en/publications/reinforcement-learning-with-mechanistic-models-to-optimise-radiot]
- 91. This AI tracks lung tumors as you breathe — and it... | ScienceDaily [https://www.sciencedaily.com/releases/2025/06/250630073440.htm]
- 92. Deep learning for automated, motion-resolved tumor segmentation in... [https://pubmed.ncbi.nlm.nih.gov/40588532/]
- 93. Data Science Opportunities To Improve Radiotherapy Planning and Clinical Decision Making - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11698470/]
- 94. Machine Learning-Based Models for Prediction of Toxicity Outcomes in Radiotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7289968/]
- 95. Towards verifiable cancer digital twins: tissue level modeling protocol for precision medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11537925/]
- 96. From virtual to reality: innovative practices of digital twins in tumor therapy | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06371-z]
- 97. TumorTwin: A python framework for patient-specific digital twins in oncology [https://arxiv.org/html/2505.00670v1]
- 98. Diagnostics & Billing: Reimbursing Predictive Care When... Digital Twin [https://www.linkedin.com/pulse/digital-twin-diagnostics-billing-reimbursing-care-when-daniel-cham-md-vsxwc]
- 99. for clinical trials: early days, rapid... - Clinical Trials Arena Digital twins [https://www.clinicaltrialsarena.com/news/oct-dach-2025-digital-twins-clinical-trials/]
- 100. What experts at Flatiron, PicnicHealth, MMIT expect for [https://www.drugdiscoverytrends.com/clinical-care-convergence-2025/]
- 101. AI Clinical in U.S. Healthcare: A Adoption Update 2025 [https://www.linkedin.com/pulse/clinical-ai-adoption-us-healthcare-2025-update-jonathan-govette-3ignc]