Validation of Biomarkers to Predict Immunotherapy Response: A Comprehensive Guide from Discovery to Clinical Application
This article provides a comprehensive roadmap for researchers and drug development professionals on the validation of predictive biomarkers for cancer immunotherapy.
Validation of Biomarkers to Predict Immunotherapy Response: A Comprehensive Guide from Discovery to Clinical Application
Abstract
This article provides a comprehensive roadmap for researchers and drug development professionals on the validation of predictive biomarkers for cancer immunotherapy. It covers the foundational landscape of established and emerging biomarkers, details the stepwise methodological process from analytical to clinical validation, addresses key challenges and optimization strategies, and explores regulatory frameworks and comparative analysis of validation trial designs. By synthesizing current standards and future directions, this guide aims to accelerate the development of robust biomarkers to improve patient selection and outcomes in immuno-oncology.
The Evolving Landscape of Immunotherapy Biomarkers: From Discovery to Clinical Imperative
The Critical Need for Predictive Biomarkers in Immuno-Oncology
Cancer immunotherapy, particularly the use of immune checkpoint inhibitors (ICIs), has fundamentally transformed oncology by enabling durable, long-lasting responses in multiple malignancies including non-small cell lung cancer (NSCLC), melanoma, and triple-negative breast cancer [1]. These treatments work by blocking inhibitory pathways such as programmed cell death protein-1/programmed death-ligand 1 (PD-1/PD-L1) and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), thereby restoring T-cell-mediated antitumor immunity [1]. Despite demonstrated successes across diverse tumor types, only a subset of patients derives clinical benefit from these interventions, while all patients face potential immune-related adverse events (irAEs) and significant financial costs [1] [2].
This variability in treatment response underscores the critical need for robust predictive biomarkers to guide therapy selection, optimize clinical outcomes, and reduce unnecessary toxicity [1]. The ideal biomarker should be specific, reproducible, clinically accessible, and mechanistically informative, though current candidates face challenges including tumor heterogeneity, assay variability, and dynamic biomarker expression across tumor sites and disease stages [1]. This review synthesizes current evidence on predictive biomarkers in immuno-oncology, comparing their performance characteristics, validation methodologies, and clinical applications to inform researchers and drug development professionals.
Established Predictive Biomarkers: Clinical Validation and Performance
PD-L1 Expression
PD-L1, the ligand for PD-1, is frequently expressed on antigen-presenting cells and tumor cells, where its expression is often induced by interferon-gamma within the tumor microenvironment [1]. When PD-L1 binds PD-1, T-cell activation becomes inhibited, resulting in immune tolerance [1]. ICIs targeting this pathway include pembrolizumab and nivolumab (PD-1 inhibitors) and atezolizumab, durvalumab, and avelumab (PD-L1 inhibitors) [1].
PD-L1 has emerged as a key predictive biomarker in NSCLC, with the KEYNOTE-024 trial demonstrating that patients with PD-L1 expression ≥50% experienced significantly improved outcomes with pembrolizumab versus chemotherapy, showing a median overall survival (OS) of 30 months versus 14.2 months (HR: 0.63; 95% CI: 0.47-0.86) [1]. These findings led to pembrolizumab's approval as first-line therapy in advanced NSCLC with high PD-L1 expression [1]. However, the CheckMate-026 trial using nivolumab failed to show similar OS or progression-free survival (PFS) advantages, highlighting the limitations of PD-L1 as a standalone biomarker due to assay variability, different detection antibodies, and tumor heterogeneity [1].
Microsatellite Instability (MSI) and Mismatch Repair Deficiency (dMMR)
MSI and dMMR reflect defects in DNA repair pathways, commonly observed in colorectal cancer, that result in high mutational burden and neoantigen formation [1]. The FDA granted tissue-agnostic approval to pembrolizumab in 2017 based on trials including KEYNOTE-016, KEYNOTE-164, and KEYNOTE-158, which demonstrated a 39.6% overall response rate (ORR) in MSI-high tumors, with durable responses in 78% of cases [1]. MSI-H/dMMR testing is now recommended in guidelines by the American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network (NCCN) as a robust predictor of response to immunotherapy, though its utility remains limited to a subset of patients across various cancer types [1].
Tumor Mutational Burden (TMB)
TMB measures the number of somatic mutations per megabase of DNA, reflecting neoantigen load and tumor immunogenicity [1]. Pembrolizumab received approval for tumors with TMB ≥10 mutations/Mb based on the KEYNOTE-158 trial, which demonstrated a 29% ORR in high-TMB tumors compared to 6% in low-TMB tumors [1]. Additional research by Gandara et al. reported that TMB ≥20 mutations/Mb was associated with improved survival across multiple cancer types (HR: 0.52; 95% CI: 0.47-0.58) [1]. While TMB shows promise as a quantitative predictive marker, challenges remain in standardization across testing platforms and determination of optimal cut-off values across different cancer types.
Table 1: Comparison of Established Predictive Biomarkers in Immuno-Oncology
| Biomarker | Cancer Types | Predictive Value | Limitations | Regulatory Status |
|---|---|---|---|---|
| PD-L1 Expression | NSCLC, Melanoma, TNBC | ORR: 30-50% in PD-L1+ NSCLC; Median OS: 30 vs 14.2 mos in KEYNOTE-024 | Inter-assay variability, tumor heterogeneity, dynamic expression | FDA-approved companion diagnostic for multiple ICIs |
| MSI-H/dMMR | Colorectal, Endometrial, Pan-cancer | ORR: 39.6%; Durable responses in 78% | Limited to small patient subsets (2-4% in most cancers) | FDA-approved tissue-agnostic indication for pembrolizumab |
| Tumor Mutational Burden | Multiple solid tumors | ORR: 29% in TMB-high vs 6% in TMB-low; HR: 0.52 for survival in TMB ≥20 mut/Mb | Lack of standardized cut-offs, platform variability | FDA-approved for pembrolizumab in TMB ≥10 mut/Mb |
Emerging Biomarkers and Novel Approaches
Circulating Biomarkers and Liquid Biopsy
Circulating tumor DNA (ctDNA) comprises tumor-derived DNA fragments in the bloodstream that offer a non-invasive biomarker approach for monitoring treatment response [1]. Research by Al-Showbaki et al. demonstrated that ≥50% ctDNA reduction within 6-16 weeks post-ICI therapy correlated with better PFS and OS across multiple tumor types [1]. Additionally, Tie et al. showed that a ctDNA-guided strategy could reduce adjuvant chemotherapy use in stage II colon cancer without compromising recurrence-free survival [1]. Liquid biopsies are poised to become standard tools in clinical practice by 2025, with advances in ctDNA analysis and exosome profiling expected to increase sensitivity and specificity for early disease detection and monitoring [3].
Other circulating biomarkers showing promise include relative eosinophil count (REC), with one study demonstrating that melanoma patients with REC ≥1.5% had a median OS of 27 months versus 5-7 months for those with lower counts [1]. Flow cytometry analysis of peripheral blood mononuclear cells has also revealed potential predictive value for absolute lymphocyte count and specific immune cell populations in response to CTLA-4 inhibition, though these approaches require further validation [2] [4].
Tumor Microenvironment Biomarkers
The tumor immune microenvironment plays a crucial role in mediating response to immunotherapy. Tumor-infiltrating lymphocytes (TILs), consisting primarily of cytotoxic and helper T cells that infiltrate tumors, reflect host immune response and have demonstrated significant predictive value [1]. High TIL levels in triple-negative and HER2-positive breast cancers are associated with improved immunotherapy response and prognosis, leading to their incorporation into Scandinavian breast cancer guidelines and recognition by the European Society for Medical Oncology (ESMO) for early-stage disease [1]. Despite the absence of universal scoring standards, TIL assessment offers a low-cost and reproducible biomarker approach [1].
Advanced multiplex immunohistochemistry and single-cell analysis technologies are enabling deeper characterization of the tumor microenvironment, identifying specific cell populations and spatial relationships that may predict treatment response more accurately than single-parameter biomarkers [3] [4]. Single-cell analysis technologies are expected to become more sophisticated and widely adopted by 2025, facilitating identification of rare cell populations that may drive disease progression or resistance to therapy [3].
Multi-Omics and Integrated Approaches
Given the complexity of tumor-immune interactions, multiparameter biomarker approaches are increasingly necessary for accurate prediction of clinical benefit [2]. Multi-omics approaches integrate genomic, transcriptomic, proteomic, and metabolomic data to achieve a holistic understanding of disease mechanisms and identify comprehensive biomarker signatures [1] [3]. Research by Bourbonne et al. demonstrated approximately 15% improvement in predictive accuracy using multi-omics with machine learning models, while Li et al. identified specific gene clusters associated with durable response to PD-1 blockade [1].
In the Lung-MAP S1400I trial, investigators found that high CD8⁺GZB⁺ T-cell infiltration predicted better response to nivolumab, while IL-6 and CXCL13 levels were linked to resistance, illustrating the power of immune contexture profiling [1]. The trend toward multi-omics integration is expected to gain momentum through 2025, promoting systems biology approaches and fostering collaborative research efforts across bioinformatics, molecular biology, and clinical research [3].
Table 2: Emerging Biomarkers and Technologies in Immuno-Oncology
| Biomarker Category | Specific Markers | Potential Applications | Current Validation Status |
|---|---|---|---|
| Circulating Biomarkers | ctDNA, REC, MDSCs, Tregs | Response monitoring, early relapse detection, treatment selection | Preliminary clinical evidence; requires prospective validation |
| Tumor Microenvironment | TILs, CD8+GZB+ T cells, Spatial relationships | Predictive of response across multiple tumor types | Clinical validation ongoing; TILs incorporated into some guidelines |
| Multi-Omics Signatures | Genomic, transcriptomic, proteomic profiles | Patient stratification, combination therapy guidance | Research phase; machine learning models in development |
Biomarker Validation: Methodologies and Statistical Considerations
Validation Workflow and Regulatory Framework
The biomarker validation process requires careful attention to both analytical and clinical validation to establish clinical utility [2]. According to regulatory guidelines, biomarker assay validation can be separated into several continuous steps: assessment of basic assay performance (analytical validation); characterization of performance regarding intended use (clinical validation); and validation in independent cohorts to demonstrate clinical utility [2]. For a test to be considered a companion diagnostic, it must be essential for the safe and effective use of a corresponding therapeutic product and undergo rigorous review and approval by the FDA, requiring demonstration of analytical validity, clinical validity, and clinical utility [5].
The Society for Immunotherapy of Cancer (SITC) Immune Biomarkers Task Force has developed recommendations to guide analytical and clinical validation design for specific assays, emphasizing that validation should ultimately qualify assays for use in clinical decision-making [2]. Regulatory agencies are implementing more streamlined approval processes for biomarkers validated through large-scale studies and real-world evidence, with increasing recognition of real-world evidence in evaluating biomarker performance across diverse populations [3].
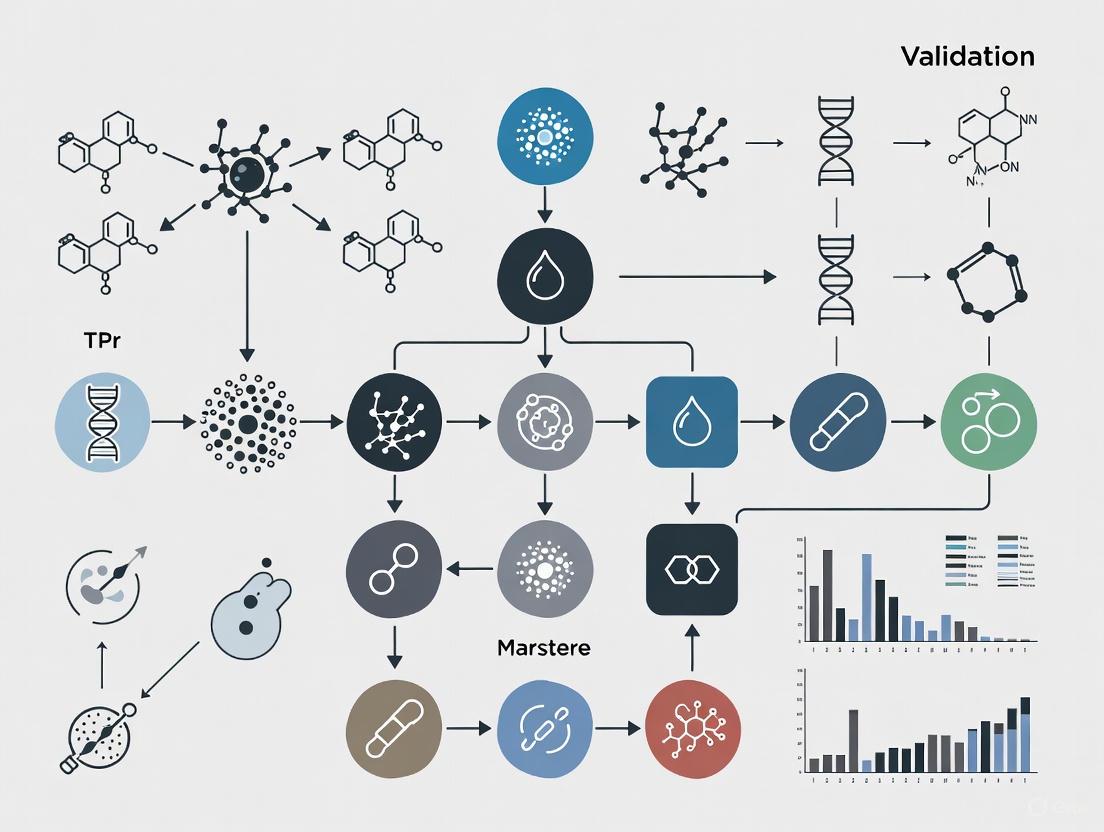
Biomarker Validation Pathway
Statistical Considerations and Methodological Challenges
Biomarker validation must discern associations occurring by chance from those reflecting true biological relationships, requiring careful attention to statistical methodologies [6]. Key considerations include controlling for multiplicity due to investigation of multiple biomarkers or endpoints, addressing within-subject correlation when multiple observations are collected from the same subject, and minimizing selection bias in retrospective studies [6] [7].
Multiplicity presents a particular challenge in biomarker studies because the probability of concluding that there is at least one statistically significant effect across a set of tests when no effect exists increases with each additional test [6]. Methods to control false discovery rate (FDR) are especially useful when using large-scale genomic or other high-dimensional data for biomarker discovery [7]. Additionally, studies with multiple endpoints require multiple testing corrections, prioritization of outcomes, or development of composite endpoints [6].
For predictive biomarker identification, proper statistical analysis requires testing for interaction between treatment and biomarker in a statistical model using data from randomized clinical trials [7]. An example is the IPASS study, which demonstrated a significant interaction between treatment and EGFR mutation status (P<.001) for gefitinib versus chemotherapy in lung cancer [7]. This contrasts with prognostic biomarkers, which can be identified through main effect tests of association between biomarker and outcome without requiring randomization [7].
Artificial Intelligence and Next-Generation Biomarker Discovery
AI-Driven Predictive Models
Artificial intelligence approaches are revolutionizing biomarker discovery by allowing exploitation of high-dimension oncological data in precision immuno-oncology [8]. A systematic review by Prelaj et al. identified 90 studies utilizing AI for predicting ICI efficacy across five data modalities: genomics, radiomics, digital pathology, real-world data, and multimodality data, with 80% published between 2021-2022 [8]. Standard machine learning methods were used in 72% of studies, deep learning methods in 22%, and both in 6%, with NSCLC (36%) and melanoma (16%) being the most frequently studied cancer types [8].
AI technologies enable development of sophisticated predictive models that can forecast disease progression and treatment responses based on complex biomarker profiles, enhancing clinical decision-making and optimizing patient management strategies [3] [9]. Machine learning algorithms also facilitate automated analysis of complex datasets, significantly reducing time required for biomarker discovery and validation [3]. By leveraging AI to analyze individual patient data alongside biomarker information, clinicians can develop tailored treatment plans that maximize efficacy while minimizing adverse effects [3].
Multi-Modal Data Integration
AI approaches have expanded the horizon for biomarker discovery by demonstrating the power of integrating multimodal data from existing datasets to discover new meta-biomarkers [8]. Complex algorithms and novel AI-based markers are emerging through integration of multimodal and multi-omics data, with AI-powered imaging tools improving assessment of tumor microenvironments and immune infiltrates [8] [9]. These approaches offer more precise predictions of therapy responses and aid in better clinical decision-making compared to single-modality biomarkers [9].
Emerging AI models trained on routine laboratory values, imaging data, and spatial "omics" now reportedly outperform PD-L1 in predicting response to immunotherapy, with potential for integration directly into hospital electronic medical records in the near future [10]. However, most studies to date have implemented AI as post hoc analyses rather than prospective designs incorporating AI-based methodologies from the outset, indicating the need for a priori planned prospective trial designs to cover all lifecycle steps of these software biomarkers [8].
AI-Driven Biomarker Discovery
Essential Research Reagents and Technologies
Table 3: Essential Research Reagents and Technologies for Immuno-Oncology Biomarker Research
| Category | Specific Reagents/Technologies | Research Applications | Key Considerations |
|---|---|---|---|
| Immunohistochemistry Assays | PD-L1 IHC 22C3, 28-8, SP142; Multiplex IHC panels | Protein expression analysis, spatial relationship mapping | Antibody validation, platform standardization, scoring protocols |
| Genomic Profiling | Next-generation sequencing panels, FoundationOne CDx, liquid biopsy assays | TMB assessment, MSI status, mutation profiling | Coverage depth, variant calling algorithms, input DNA requirements |
| Immune Monitoring | Multiparametric flow cytometry, ELISpot, single-cell RNA sequencing | Immune cell phenotyping, cytokine profiling, T-cell receptor repertoire | Panel design, sample processing, data normalization |
| Spatial Biology | Multiplex immunofluorescence, digital pathology, CODEX | Tumor microenvironment characterization, cellular interactions | Tissue preservation, image analysis algorithms, multiplexing capacity |
| AI/Computational Tools | Machine learning platforms, deep learning algorithms, data integration software | Predictive model development, biomarker signature identification | Data preprocessing, feature selection, model interpretability |
The field of predictive biomarkers for immuno-oncology is rapidly evolving beyond single-parameter biomarkers toward integrated approaches that capture the complexity of tumor-immune interactions [2]. While established biomarkers like PD-L1, MSI, and TMB provide foundation for treatment selection, emerging technologies including liquid biopsies, AI-driven models, and multi-omics signatures promise enhanced predictive accuracy [1] [8]. The successful clinical integration of these advanced biomarkers will require addressing ongoing challenges in standardization, validation, and equitable access [10].
Looking toward 2025, key trends expected to shape the biomarker landscape include enhanced integration of artificial intelligence and machine learning, rise of multi-omics approaches, advancements in liquid biopsy technologies, and adaptation of regulatory frameworks to accommodate novel biomarker types [3]. Additionally, focus on patient-centric approaches will become more pronounced, with biomarker analysis playing a key role in enhancing patient engagement and outcomes through improved education, incorporation of patient-reported outcomes, and engagement of diverse populations to ensure biomarker relevance across demographics [3]. As these technologies mature, the future of immuno-oncology will increasingly depend on validated predictive biomarkers to guide personalized treatment strategies and maximize therapeutic benefit while minimizing unnecessary toxicity and cost.
Immune checkpoint inhibitors (ICIs) have fundamentally transformed cancer treatment, offering durable responses and prolonged survival for a subset of patients across numerous malignancies [11] [12]. However, clinical benefit remains heterogeneous, with only 20-30% of patients achieving durable responses, underscoring the critical need for robust predictive biomarkers to guide patient selection and optimize therapeutic outcomes [13]. The validation and implementation of biomarkers have become central to precision immuno-oncology, enabling clinicians to identify patients most likely to benefit from specific immunotherapy regimens.
The current clinical landscape is dominated by three established biomarkers: programmed death-ligand 1 (PD-L1) expression, microsatellite instability (MSI) or mismatch repair deficiency (dMMR), and tumor mutational burden (TMB) [12] [14]. These biomarkers provide insights into different aspects of the tumor-immune interaction, from immune checkpoint expression to underlying genomic instability and neoantigen load. This guide provides a comprehensive comparison of these established biomarkers, detailing their clinical validation, technical assessment, and predictive utility within the broader context of immunotherapy biomarker research.
Biomarker Comparison and Clinical Utility
The following table summarizes the key characteristics, clinical applications, and limitations of PD-L1, MSI/dMMR, and TMB in current clinical practice.
Table 1: Comparative Analysis of Established Immunotherapy Biomarkers
| Biomarker | Biological Rationale | Measurement Methods | FDA-Approved Contexts | Key Limitations |
|---|---|---|---|---|
| PD-L1 | Measures adaptive immune resistance; PD-L1 binding to PD-1 on T cells inhibits anti-tumor immunity [14]. | Immunohistochemistry (IHC) with various assays (e.g., 22C3, 28-8, SP142, SP263) and scoring systems (TPS, CPS) [11] [12]. | Companion diagnostic for multiple cancers (NSCLC, HNSCC, gastric, TNBC) [11] [14]. | Significant spatial and temporal heterogeneity; assay and cutoff variability; dynamic expression [11] [12] [15]. |
| MSI/dMMR | Defective DNA repair → frameshift mutations → high neoantigen load → inflamed TME [16]. | IHC (loss of MMR proteins: MLH1, MSH2, MSH6, PMS2) or PCR/NGS for MSI [16] [14]. | Tissue-agnostic indication for pembrolizumab and other ICIs [11] [16]. | Prevalence varies widely across cancer types; biological heterogeneity can modulate response [11] [15]. |
| TMB | High mutation count → increased neoantigen generation → enhanced immune recognition [14]. | Targeted NGS panels, whole exome sequencing (WES); defined as ≥10 mut/Mb for tissue-agnostic approval [11] [12]. | Tissue-agnostic companion diagnostic for pembrolizumab [11] [12]. | Lack of standardization across panels; predictive value inconsistent across tumor types [11] [12]. |
Biomarker Mechanisms and Predictive Value
Biological Pathways and Mechanisms
The predictive power of these biomarkers stems from their roles in distinct biological processes. PD-L1 expression represents a mechanism of adaptive immune resistance, where tumors exploit the PD-1/PD-L1 checkpoint pathway to suppress T-cell-mediated cytotoxicity [15] [14]. In contrast, MSI/dMMR and TMB are both rooted in genomic instability. dMMR leads to a hypermutated phenotype, particularly at microsatellite regions, generating frameshift mutations and a high burden of immunogenic neoantigens that create an inflamed tumor microenvironment rich in tumor-infiltrating lymphocytes [16]. TMB reflects the total number of mutations in the tumor genome, which correlates with the potential for neoantigen formation and subsequent T-cell recognition [14].
Diagram 1: Biomarker interplay in immunotherapy response. The diagram illustrates how dMMR/MSI-H and high TMB contribute to neoantigen formation, leading to T-cell activation and subsequent PD-L1 upregulation, which is targeted by checkpoint inhibitors.
Differential Predictive Value for Treatment Regimens
Emerging evidence suggests that these biomarkers may have differential predictive value depending on the therapeutic regimen. Exploratory analyses from the CheckMate 142 study in MSI-H/dMMR metastatic colorectal cancer revealed that higher expression of inflammation-related gene expression signatures was associated with improved response and survival with nivolumab monotherapy. In contrast, higher TMB, tumor indel burden (TIB), and degree of microsatellite instability were more strongly associated with efficacy with nivolumab plus ipilimumab combination therapy [17]. This suggests that for combination therapy, tumor antigenicity may be a more critical determinant of efficacy than the baseline inflammatory tumor microenvironment [17].
Experimental Protocols and Methodologies
PD-L1 Immunohistochemistry (IHC)
Protocol Overview: PD-L1 expression is quantitatively measured using IHC on formalin-fixed paraffin-embedded (FFPE) tumor tissue sections [12] [18].
Key Steps:
- Tissue Sectioning: Cut FFPE tissue into 4-5 μm sections and mount on slides.
- Deparaffinization and Antigen Retrieval: Use heat-induced epitope retrieval methods to unmask antigens.
- Primary Antibody Incubation: Apply FDA-approved clones (e.g., 22C3 pharmDx, 28-8 pharmDx, SP142, SP263) specific to PD-L1 under standardized conditions [12] [18].
- Detection: Use enzyme-conjugated secondary antibodies and chromogenic substrates for visualization.
- Scoring: Evaluate staining using standardized scoring systems:
MSI/dMMR Testing
Dual-Method Approach: MSI/dMMR status can be determined through two primary methods, often used complementarily.
IHC for MMR Protein Expression:
- Procedure: Perform IHC on FFPE sections for the four MMR proteins (MLH1, MSH2, MSH6, PMS2).
- Interpretation: Loss of nuclear expression in tumor cells for one or more proteins indicates dMMR. Specific patterns guide genetic testing (e.g., MLH1/PMS2 loss suggests sporadic MLH1 promoter hypermethylation) [16].
PCR-Based MSI Analysis:
- DNA Extraction: Isolate DNA from tumor and matched normal tissue.
- PCR Amplification: Amplify a standardized panel of mononucleotide and dinucleotide repeat markers (e.g., BAT-25, BAT-26, NR-21, NR-24, MONO-27).
- Fragment Analysis: Compare fragment sizes between tumor and normal DNA. Instability at ≥2 markers (≥30% for pentaplex panels) defines MSI-H [16].
Next-generation sequencing (NGS) panels now frequently include MSI calling algorithms, providing a high-throughput alternative [16] [19].
Tumor Mutational Burden (TMB) Assessment
NGS-Based Measurement: TMB is calculated from genomic data as the total number of somatic mutations per megabase (mut/Mb) of the genome examined [11] [12].
Standardized Wet Lab Protocol:
- DNA Extraction: Extract high-quality DNA from FFPE tumor tissue and matched normal (when available).
- Library Preparation: Prepare sequencing libraries using comprehensive gene panels (e.g., TruSight Oncology 500, FoundationOne CDx) or whole exome sequencing [18] [19].
- Sequencing: Perform high-coverage sequencing on appropriate platforms (Illumina, Ion Torrent).
- Bioinformatic Analysis:
- Alignment: Map sequencing reads to a reference genome (e.g., GRCh38).
- Variant Calling: Identify somatic single nucleotide variants (SNVs) and small insertions/deletions (indels) using validated pipelines.
- Filtering: Exclude known driver mutations, germline variants (using matched normal or population databases), and synonymous mutations.
- TMB Calculation: Divide the total number of nonsynonymous mutations by the size of the coding region targeted in megabases [18] [19].
Diagram 2: Experimental workflow for biomarker assessment. The flowchart outlines the key steps from sample processing to clinical reporting for PD-L1, MSI/dMMR, and TMB analysis.
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and technologies essential for conducting research on these established biomarkers.
Table 2: Essential Research Reagents for Immunotherapy Biomarker Analysis
| Reagent/Technology | Specific Examples | Research Application | Critical Function |
|---|---|---|---|
| FDA-Approved IHC Assays | 22C3 pharmDx (Agilent), 28-8 pharmDx (Agilent), SP142 (Ventana), SP263 (Ventana) [12] [18]. | Quantifying PD-L1 expression on tumor and immune cells. | Standardized detection and scoring of PD-L1 protein expression; enables cross-study comparisons. |
| MMR IHC Antibodies | Anti-MLH1, Anti-MSH2, Anti-MSH6, Anti-PMS2 [16]. | Identifying loss of MMR protein expression. | Screening for dMMR status; patterns of loss guide further genetic testing. |
| NGS Panels | TruSight Oncology 500 (Illumina), FoundationOne CDx, Oncomine Comprehensive Assay Plus [18] [19]. | Comprehensive genomic profiling. | Simultaneous assessment of TMB, MSI, and specific genomic alterations from limited tissue. |
| MSI PCR Kits | Promega MSI Analysis System, Thermo Fisher MSI Assay [16]. | Standardized fragment analysis for MSI status. | Gold-standard validation of MSI status; often used to confirm NGS-based MSI calls. |
PD-L1, MSI/dMMR, and TMB represent the cornerstone of predictive biomarker testing for immunotherapy, each with distinct strengths and limitations. While these biomarkers have enabled more precise patient selection, their imperfect predictive accuracy highlights the complexity of tumor-immune interactions. Future directions involve developing integrated models that combine these established biomarkers with emerging ones—such as gene expression profiles, gut microbiome signatures, and host factors—to create more comprehensive predictive algorithms [13] [20]. The continued refinement and validation of these biomarkers are essential for advancing precision immuno-oncology and maximizing therapeutic benefit for cancer patients.
The advent of immunotherapy, particularly immune checkpoint inhibitors (ICIs), has fundamentally transformed cancer treatment paradigms. However, a critical challenge remains: only 20–30% of patients achieve durable responses, highlighting an urgent need for reliable predictive biomarkers to guide therapeutic strategies [13] [21]. The field is rapidly evolving beyond single-analyte biomarkers toward integrated, multi-omics approaches. This guide objectively compares the performance of three emerging biomarker classes—Genomic, Proteomic, and Microenvironmental—in predicting immunotherapy response. Framed within the broader thesis of biomarker validation, this review provides researchers and drug development professionals with a comparative analysis of these platforms, supported by experimental data and detailed methodologies.
Comparative Analysis of Emerging Biomarker Classes
The following table summarizes the key characteristics, strengths, and limitations of the three primary emerging biomarker classes.
Table 1: Comparative Overview of Emerging Biomarker Classes for Immunotherapy
| Biomarker Class | Key Examples | Predictive Utility | Clinical Validation Status | Key Strengths | Major Limitations |
|---|---|---|---|---|---|
| Genomic | Tumor Mutational Burden (TMB), Microsatellite Instability (MSI) | Predicts neoantigen load and immunogenicity; tissue-agnostic approval for MSI-H [1]. | FDA approval for pembrolizumab in TMB-high (≥10 mut/Mb) and MSI-H tumors [1]. | Provides a quantifiable measure; foundational for companion diagnostics. | Limited accuracy as a standalone marker; spatial and temporal heterogeneity [1]. |
| Proteomic | Plasma protein signatures (e.g., VASN, PARD3, PTGES3), PD-L1 IHC | PD-L1 is most widely used; novel plasma models predict response in SCLC [22] [23] [21]. | Variable; PD-L1 used clinically but imperfect; novel signatures in validation phases (AUC >0.82) [22] [23]. | Reflects functional protein activity; liquid biopsy enables dynamic monitoring. | PD-L1 expression is dynamic and heterogeneous; assay variability [21]. |
| Microenvironmental | Tumor-Infiltrating Lymphocytes (TILs), Tertiary Lymphoid Structures (TLS) | High CD8+ T cells and mature TLS correlate with improved response and survival [21]. | TILs are recognized in guidelines (e.g., ESMO); TLS is an emerging research biomarker [21]. | Captures the functional immune context; spatial organization is highly informative. | Requires tissue biopsy; complex standardization for scoring and analysis. |
Genomic Biomarkers
Genomic biomarkers analyze the DNA sequence of tumors to identify quantifiable genetic alterations that correlate with response to immunotherapy. The primary candidates include Tumor Mutational Burden (TMB), defined as the number of somatic mutations per megabase of DNA, and Microsatellite Instability (MSI), a condition of hypermutability resulting from defective DNA mismatch repair [1]. These biomarkers function as proxies for the tumor's neoantigen load, which determines its immunogenicity and susceptibility to immune attack.
Table 2: Experimental Data for Key Genomic Biomarkers
| Biomarker | Cancer Type | Therapeutic Context | Reported Performance | Source / Trial |
|---|---|---|---|---|
| TMB (≥10 mut/Mb) | Various solid tumors | Pembrolizumab monotherapy | ORR: 29% in TMB-high vs. 6% in TMB-low | KEYNOTE-158 [1] |
| TMB (≥20 mut/Mb) | Pan-cancer | Immune Checkpoint Inhibitors | Improved survival (HR: 0.52; 95% CI: 0.47-0.58) | Gandara et al. [1] |
| MSI-H/dMMR | Tissue-agnostic | Pembrolizumab | ORR: 39.6%; 78% with durable responses | KEYNOTE-016/164/158 [1] |
Detailed Experimental Protocols
Next-Generation Sequencing (NGS) for TMB and MSI Analysis:
- Sample Acquisition: Obtain tumor tissue via biopsy (or use stored FFPE samples) and a matched normal sample (e.g., blood or saliva).
- DNA Extraction: Use commercial kits (e.g., Qiagen DNeasy) to extract high-quality genomic DNA from both tumor and normal samples. Quantify DNA using fluorometry.
- Library Preparation & Sequencing: Prepare sequencing libraries using comprehensive gene panels (e.g., > 1 Mb) or whole-exome kits. This involves DNA shearing, adapter ligation, and target enrichment. Sequence on an NGS platform (e.g., Illumina NovaSeq).
- Bioinformatic Analysis:
- Alignment: Map sequencing reads to a reference human genome (e.g., GRCh38).
- Variant Calling: Identify somatic mutations (SNVs, indels) by comparing tumor and normal BAM files.
- TMB Calculation: Filter out driver mutations and synonymous variants. TMB is calculated as the total number of non-synonymous mutations divided by the size of the coding region targeted in megabases.
- MSI Status: Analyze the length distribution of microsatellite loci in the tumor sample compared to the normal sample to detect instability.
Research Reagent Solutions
Table 3: Essential Reagents for Genomic Biomarker Research
| Research Reagent | Function | Example Product/Catalog |
|---|---|---|
| DNA Extraction Kit | Iserts high-quality, PCR-amplifiable DNA from FFPE or fresh tissue. | QIAamp DNA FFPE Tissue Kit (Qiagen) |
| NGS Library Prep Kit | Facilitates the preparation of sequencing-ready libraries from input DNA. | Illumina DNA Prep with Enrichment |
| Comprehensive Cancer Panel | A probe-based panel for hybrid capture to prepare libraries for TMB analysis. | SureSelect XT HS Pan-Cancer Panel (Agilent) |
| Bioinformatic Pipeline | Software for the analysis of NGS data, including alignment and variant calling. | Illumina Dragen Bio-IT Platform |
Proteomic Biomarkers
Proteomic biomarkers measure the expression, modification, and interaction of proteins, providing a direct readout of functional biological activity. While PD-L1 immunohistochemistry is the most clinically established proteomic biomarker, its predictive accuracy is limited [1] [21]. Emerging research focuses on plasma proteomic profiling to identify novel, non-invasive predictive signatures. For instance, a recent study in small-cell lung cancer (SCLC) developed a model based on three plasma proteins—VASN, PARD3, and PTGES3 (the VPP model)—which demonstrated robust performance in predicting response to anti-PD-L1 plus chemotherapy [22] [23].
Detailed Experimental Protocols
Mass Spectrometry-Based Plasma Proteomic Profiling:
- Sample Collection and Preparation: Collect peripheral blood into EDTA tubes. Centrifuge to isolate plasma, which is then aliquoted and stored at -80°C. Deplete high-abundance proteins (e.g., albumin, IgG) using immunoaffinity columns to enhance the detection of lower-abundance proteins.
- Protein Digestion: Denature plasma proteins, reduce disulfide bonds, and alkylate cysteine residues. Digest proteins into peptides using trypsin.
- Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS):
- Chromatography: Separate the complex peptide mixture via reverse-phase liquid chromatography.
- Mass Spectrometry: Analyze eluted peptides using a high-resolution mass spectrometer (e.g., Thermo Fisher Orbitrap). The instrument operates in data-dependent acquisition (DDA) mode, cycling between a full MS1 scan (for peptide quantification) and subsequent MS2 scans (for peptide identification via fragmentation).
- Data Analysis and Model Building:
- Protein Identification & Quantification: Process raw data using software (e.g., MaxQuant) to identify proteins and perform label-free quantification (LFQ).
- Statistical Analysis & Machine Learning: Conduct bioinformatic analyses (e.g., pathway enrichment). Use machine learning algorithms like LASSO (Least Absolute Shrinkage and Selection Operator) regression on the proteomic data from a discovery cohort to build a predictive model, which must then be validated in an independent cohort [23].
Research Reagent Solutions
Table 4: Essential Reagents for Proteomic Biomarker Research
| Research Reagent | Function | Example Product/Catalog |
|---|---|---|
| Plasma Prep Tube | Collects and separates plasma from whole blood for biomarker analysis. | BD Vacutainer EDTA Tubes |
| Protein Depletion Column | Removes abundant proteins to enhance detection of low-abundance biomarkers. | ProteoPrep Immunoaffinity Albumin & IgG Depletion Kit (Merck) |
| Trypsin, Sequencing Grade | Enzymatically digests proteins into peptides for LC-MS/MS analysis. | Trypsin Gold, Mass Spectrometry Grade (Promega) |
| LC-MS/MS System | High-resolution system for separating and analyzing complex peptide mixtures. | Orbitrap Fusion Lumos Tribrid Mass Spectrometer (Thermo Fisher) |
Microenvironmental Biomarkers
The tumor microenvironment (TME) is the ecosystem surrounding a tumor, and its composition is a critical determinant of immunotherapy efficacy. Key biomarkers include CD8+ Cytotoxic T Cells, the primary effector cells for killing cancer cells, and Tertiary Lymphoid Structures (TLS), which are organized aggregates of immune cells that form ectopically in tumors and serve as hubs for initiating and sustaining anti-tumor immunity [21]. The density, location, and functional state of these components provide profound insights into the tumor's immune status.
Table 5: Experimental Data for Key Microenvironmental Biomarkers
| Biomarker | Cancer Type | Therapeutic Context | Reported Performance | Source / Study |
|---|---|---|---|---|
| CD8+ T Cells (High Density) | NSCLC | PD-1/PD-L1 Inhibitors | Correlates with improved survival and response. | Frontiers in Immunology [21] |
| Tertiary Lymphoid Structures (TLS) | NSCLC | Immune Checkpoint Inhibitors | Presence correlates with improved patient survival and response to ICIs. | Frontiers in Immunology [21] |
Detailed Experimental Protocols
Multiplex Immunofluorescence (mIF) and Digital Pathology for TME Analysis:
- Tissue Sectioning: Cut formalin-fixed, paraffin-embedded (FFPE) tumor tissue blocks into sequential sections (4-5 μm thick).
- Multiplex Immunofluorescence Staining: Use automated staining platforms and tyramide signal amplification (TSA) based kits to sequentially label multiple antigens on a single tissue section. A typical panel might include antibodies against:
- CD8 (Cytotoxic T cells)
- CD4 (Helper T cells)
- CD20 (B cells)
- Pan-CK (Tumor cells)
- DAPI (Nuclear counterstain)
- Multispectral Imaging: Scan the stained slides using a multispectral microscope (e.g., Akoya Vectra or PhenoImager). This system captures the fluorescence spectrum at each pixel, allowing for the separation of overlapping signals.
- Image and Data Analysis:
- Spectral Unmixing & Cell Segmentation: Use image analysis software (e.g., Akoya inForm, HALO) to unmix the multispectral images, identify individual cell nuclei (DAPI), and classify each cell based on marker expression (phenotyping).
- Spatial Analysis: Calculate cell densities and perform spatial analyses, such as determining the proximity of CD8+ T cells to tumor cells (Pan-CK+). TLS are identified as organized clusters of CD20+ B cells surrounded by CD4+/CD8+ T cells.
Research Reagent Solutions
Table 6: Essential Reagents for Microenvironmental Biomarker Research
| Research Reagent | Function | Example Product/Catalog |
|---|---|---|
| Multiplex IHC/IF Antibody Panel | A pre-optimized panel of antibodies for simultaneous detection of multiple cell types. | Opal Polychromatic IHC Kits (Akoya Biosciences) |
| Automated Staining System | Provides consistent and reproducible staining for multiplexed assays. | BOND RX Research Stainer (Leica Biosystems) |
| Multispectral Imaging System | A slide scanner that captures spectral data for precise fluorescence unmixing. | Vectra POLARIS (Akoya Biosciences) |
| Spatial Biology Analysis Software | Software for cell phenotyping, density quantification, and spatial analysis. | HALO Image Analysis Platform (Indica Labs) |
The Future of Biomarker Discovery: AI and Multi-Omics Integration
The limitations of single-biomarker approaches are driving the field toward multi-omics integration and artificial intelligence (AI). AI and machine learning (ML) are accelerating biomarker discovery by mining complex datasets to identify hidden patterns and improve predictive accuracy [24] [3]. For example, machine learning models like SCORPIO and LORIS have demonstrated superior performance (AUC values up to 0.84-0.85 in select studies) compared to traditional single-biomarker methods like PD-L1 [13]. These models integrate diverse data types—genomic, proteomic, digital pathology images, and clinical features—to generate a holistic "molecular fingerprint" of a patient's disease [20]. This Comprehensive Oncological Biomarker Framework aims to move beyond static snapshots to dynamic, predictive models that can guide truly personalized immunotherapy regimens. The global biomarkers market, projected to grow from $62.39 billion in 2025 to $104.15 billion by 2030, reflects the significant investment and expectation in these advanced technologies [25] [26].
The pursuit of reliable biomarkers to predict response to immunotherapy has represented a central challenge in oncology research. While immune checkpoint inhibitors (ICIs) and adoptive cell therapies like CAR-T have revolutionized cancer treatment, they benefit only a subset of patients, creating an urgent need for predictive biomarkers [27] [28]. Traditional approaches focused on single-parameter biomarkers such as PD-L1 expression and tumor mutational burden (TMB) have demonstrated limited predictive accuracy across diverse patient populations and cancer types [29] [30]. The complexity of tumor-host interactions, encompassing dynamic immune responses, microbial influences, metabolic reprogramming, and mechanical aspects of the tumor microenvironment (TME), necessitates a fundamental shift toward multi-dimensional assessment frameworks [31] [32].
The Society for Immunotherapy of Cancer (SITC) Immune Biomarkers Task Force has emphasized that due to the complexity of immune responses and tumor biology, a single biomarker is unlikely to sufficiently predict clinical outcomes to immune-targeted therapy [28]. Instead, the integration of multiple tumor and host parameters—including protein expression, genomic, transcriptomic, and metabolomic data—may be necessary for accurate prediction of clinical benefit. This paradigm shift recognizes cancer as a systemic disease influenced by host genomic diversity, environmental exposures, and complex host-tumor ecosystems that extend far beyond the tumor cell itself [32].
Limitations of Single-Parameter Biomarker Approaches
Single-parameter biomarkers have served as important initial tools for predicting immunotherapy response but face significant limitations in clinical application. PD-L1 immunohistochemistry suffers from lack of standardization in antibody clones, scoring systems, and expression thresholds across different cancer types [29] [30]. Additionally, PD-L1 expression exhibits dynamic temporal and spatial heterogeneity within tumors, making assessment from limited biopsy material potentially unrepresentative [29].
Tumor mutational burden (TMB), while valuable in certain contexts, shows limited predictive utility in malignancies with low mutation rates such as pediatric acute lymphoblastic leukemia (typically <20 mutations per exome) [33]. The correlation between TMB and neoantigen load is imperfect, and the threshold for "high TMB" varies considerably across cancer types [33]. In direct comparative analyses, TMB demonstrated median time-dependent area under the curve (AUC(t)) values of 0.503-0.543 for predicting overall survival in ICI-treated patients, significantly underperforming compared to integrated models [30].
Table 1: Limitations of Conventional Single-Parameter Biomarkers
| Biomarker | Key Limitations | Predictive Performance | Technical Challenges |
|---|---|---|---|
| PD-L1 IHC | Spatial heterogeneity, dynamic expression | AUC ~0.65 for response prediction [29] | Lack of standardized antibodies/scoring systems |
| TMB | Limited utility in low-mutation cancers | Median AUC(t) 0.503-0.543 for survival [30] | Requires sufficient tissue, complex NGS platforms |
| MSI/dMMR | Applicable to limited cancer subtypes | High predictive value but in <5% of solid tumors | Specialized testing requirements |
| Single cytokine assays | Reflect momentary immune state only | Limited predictive value alone [27] | Dynamic fluctuations, lack of standardized thresholds |
The limitations of these single-parameter approaches become particularly evident when considering the multi-dimensional nature of antitumor immunity. Effective immune responses require a coordinated sequence of events including tumor antigen presentation, T cell activation, trafficking to tumor sites, and infiltration into the immunosuppressive TME—a process that cannot be captured by measuring any single parameter [27] [31].
Multi-Dimensional Biomarker Platforms: Technologies and Methodologies
Multiplex Immunohistochemistry/Immunofluorescence (mIHC/IF)
Multiplex IHC/IF technologies enable simultaneous detection of multiple biomarkers on a single tissue section, preserving spatial context and enabling characterization of immune cell communities within the TME [29]. The MICSSS (Multiplexed Immunohistochemical Consecutive Staining on Single Slide) technique employs repeated cycles of immunoperoxidase labeling, imaging, and dye elution followed by image alignment and integration [29]. Alternatively, Opal multiplex immunofluorescence uses tyramine signal amplification (TSA) with fluorescent signals covalently bound to antigens, allowing antibody stripping via microwave heating while preserving fluorescence signals, enabling 7-9 color staining [29].
These platforms permit comprehensive immune profiling within the tumor immune microenvironment (TIME), including assessment of immune cell density, cellular composition, functional states, and cell-cell interactions [29]. When compared to traditional IHC, mIHC/IF demonstrated superior predictive accuracy for ICI response (AUC 0.79 vs 0.65 for PD-L1 IHC alone) and higher positive predictive value with lower false-positive rates [29].
Multi-Omics Integration Strategies
Integrated multi-omics approaches combine genomic, transcriptomic, proteomic, metabolomic, and microbiomic datasets to capture the complexity of tumor-host interactions. Genomic analyses now extend beyond TMB to include neoantigen quality, HLA evolutionary divergence (HED), and non-SNV sources of neoantigens (frameshifts, splice variants, gene fusions) that may generate more immunogenic epitopes [33].
Single-cell RNA sequencing (scRNA-seq) enables deconvolution of immune cell populations within the TME and identification of T cell exhaustion signatures (e.g., LAG3, TIM3, TOX, NR4A) that predict CAR-T failure [33]. Metabolomic profiling reveals immunosuppressive metabolites like lactate in AML microenvironments and succinate accumulation in CLL that drives T cell dysfunction through epigenetic silencing of effector genes [33].
Microbiome analysis through 16S rRNA sequencing and metagenomics identifies microbial signatures predictive of immunotherapy response. Enrichment of Faecalibacterium correlates with superior CAR-T expansion, while Enterococcus dominance associates with increased CRS severity [33]. Microbial metabolites like butyrate enhance CAR-T stemness through HDAC inhibition [33].
Table 2: Multi-Omics Technologies for Biomarker Discovery
| Technology Platform | Key Parameters Measured | Methodological Considerations | Clinical Applications |
|---|---|---|---|
| scRNA-seq | Immune cell heterogeneity, T cell exhaustion signatures | Requires fresh tissue, high cost, computational complexity | Identifying resistance mechanisms to CAR-T therapy [33] |
| Spatial transcriptomics | Gene expression within tissue architecture, immune cell localization | Preserves spatial context, lower resolution than scRNA-seq | Mapping immune cell niches in classical Hodgkin Lymphoma [33] |
| Metabolomic profiling | Lactate, succinate, arginine levels in TME | Rapid metabolite turnover, requires immediate sample processing | Predicting CAR-T persistence via plasma arginine levels [33] |
| Microbiome sequencing | Gut microbiome composition, functional potential | Confounded by medications, diet, sample collection variables | Modulating ICI response via fecal microbiota transplantation [34] |
Machine Learning-Based Integrative Models
Machine learning algorithms can integrate diverse data types to generate predictive models of immunotherapy response. The SCORPIO system utilizes routine blood tests (complete blood count, comprehensive metabolic panel) and clinical characteristics to predict ICI efficacy across diverse cancer types [30]. Developed on data from 9,745 ICI-treated patients across 21 cancer types, SCORPIO achieved median time-dependent AUC values of 0.763-0.759 for predicting overall survival at 6-30 months, significantly outperforming TMB [30].
These models employ ensemble algorithms with soft voting and five-fold cross-validation for hyperparameter optimization, trained to predict either overall survival or clinical benefit (defined as complete response, partial response, or stable disease ≥6 months) [30]. The incorporation of routinely available clinical and laboratory data provides a practical advantage over more complex genomic assays, with potential for broader implementation across diverse healthcare settings.
The Tumor Microenvironment as a Multi-Dimensional Ecosystem
Mechanical Properties of the TME
The mechanical aspects of the TME represent an underappreciated dimension influencing immunotherapy response. Tumor stiffness creates physical barriers that impede drug penetration and immune cell infiltration through compressed vasculature and dense extracellular matrix [31]. Mechanical forces activate mechanosensitive signaling pathways (YAP/TAZ, integrin signaling) that promote drug efflux and confer therapy resistance [31]. Additionally, stiff matrices recruit immunosuppressive cells including M2 macrophages and regulatory T cells, further inhibiting antitumor immunity [31].
The mechanical TME interacts bidirectionally with classic TME features—hypoxia and acidity drive matrix remodeling through HIF-1α and TGF-β signaling, increasing stromal stiffness that in turn exacerbates hypoxic conditions through vascular compression [31]. This creates a feed-forward loop that reinforces the immunosuppressive TME.
Figure 1: Multidimensional Interactions Within the Tumor Microenvironment (TME). The TME represents a complex ecosystem where mechanical, immune, metabolic, and microbial factors interact bidirectionally to influence therapy response.
Microbial Influences on Antitumor Immunity
The human microbiome constitutes a crucial component of the tumor-host interface, with particular importance for immunotherapy outcomes. Approximately 20% of malignancies are associated with dysbiosis of human microbiomes, mediated through chronic inflammation, immune modulation, and metabolic reprogramming [34]. Specific pathogens like Helicobacter pylori and Fusobacterium nucleatum are established carcinogens, while commensal microbes significantly influence therapy responses [34] [35].
In preclinical models, selective菌群移植 (FMT) from ICI responders to non-responders can restore therapeutic efficacy, with III期临床试验 demonstrating that standardized fecal microbiota capsules achieve disease control rates of 41.2% in previous non-responders [34]. Microbial metabolites including short-chain fatty acids (SCFAs) like butyrate enhance CAR-T cell stemness through epigenetic mechanisms and improve oxidative phosphorylation capacity [33] [35]. Engineering of microbial communities represents a promising therapeutic strategy, with synthetic microbial consortia successfully reversing tumor-associated immune dysregulation in animal models [34].
Experimental Workflows for Biomarker Validation
Analytical Validation Frameworks
The validation of biomarker assays requires rigorous assessment of pre-analytical and analytical variables according to established regulatory guidelines. The SITC Immune Biomarkers Task Force Working Group 1 (WG1) has developed comprehensive frameworks addressing pre-analytical factors (sample collection, processing, storage), analytical performance (specificity, sensitivity, reproducibility), and clinical validation requirements [28]. For multiplex immunofluorescence assays, this includes standardization of antibody validation, tissue processing, signal quantification, and image analysis algorithms to ensure inter-laboratory reproducibility [29].
Fit-for-purpose validation approaches tailor stringency requirements to the intended application, with more rigorous standards required for predictive biomarkers guiding treatment decisions compared to exploratory research assays [28]. For complex assays like mIHC/IF, key validation parameters include antibody cross-reactivity assessment, signal-to-noise optimization, autofluorescence correction, and validation of automated analysis pipelines [29].
Figure 2: Multiplex Immunohistochemistry/Immunofluorescence (mIHC/IF) Experimental Workflow. The process involves standardized pre-analytical sample processing, sequential staining with antibody elution, multispectral imaging, computational analysis, and clinical validation.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Multidimensional Biomarker Analysis
| Research Tool Category | Specific Examples | Primary Applications | Technical Considerations |
|---|---|---|---|
| Multiplex Imaging Platforms | OPAL Polaris, CODEX, Imaging Mass Cytometry | Spatial immune profiling, cell-cell interaction analysis | Antibody validation, spectral overlap compensation [29] |
| Single-Cell Analysis Platforms | 10X Genomics Chromium, BD Rhapsody, Smart-seq2 | Immune cell heterogeneity, T cell receptor repertoire | Cell viability critical, index hopping controls [33] |
| Metabolomic Profiling | LC-MS/MS, NMR spectroscopy | Assessment of oncometabolites, nutrient availability | Rapid sample processing required, stable isotope tracing [36] |
| Microbiome Analysis | 16S rRNA sequencing, shotgun metagenomics | FMT donor screening, microbial source tracking | Contamination controls, biomass assessment [34] |
| Computational Tools | CIBERSORT, xCell, Digital Twins | Microenvironment deconvolution, therapy response modeling | Reference signature optimization, batch effect correction [33] |
Future Directions and Clinical Translation
The field of biomarker development is rapidly evolving toward increasingly integrated assessment frameworks. Digital twin technologies—personalized computational models that integrate genomic, transcriptomic, and immunologic data—are emerging as dynamic platforms for simulating treatment responses and optimizing therapeutic strategies [33]. Longitudinal monitoring approaches using liquid biopsies (ctDNA, CTCs, exosomes) enable real-time assessment of tumor dynamics and immune responses, supporting adaptive treatment personalization [33].
Clinical trial designs are similarly evolving, with basket trials incorporating multi-omics stratification and adaptive trial designs incorporating real-time omics feedback [33]. The successful clinical translation of these approaches will require addressing significant challenges in data heterogeneity across platforms, computational complexity, standardization of analytical pipelines, and establishment of ethical frameworks for data privacy and regulatory approval [33] [32].
The vision for the future involves moving beyond static, single-parameter biomarkers toward dynamic, multi-dimensional assessment frameworks that capture the complex interplay between tumors and their hosts. This approach acknowledges that effective antitumor immunity requires the successful coordination of multiple biological processes, and that therapeutic response is ultimately emergent from this complex system rather than determinable by any single molecular parameter. As these integrated models mature and undergo clinical validation, they hold the promise of transforming immunotherapy from a one-size-fits-all approach to a truly personalized precision medicine paradigm.
Biomarker Enrichment Strategies in Early-Phase Trial Design
In the era of precision medicine, biomarker enrichment strategies have become pivotal in early-phase clinical trial design, particularly in immuno-oncology. These strategies aim to identify patient subgroups most likely to respond to treatment, thereby accelerating drug development and increasing the probability of trial success. The validation of biomarkers to predict response to immunotherapy represents a critical focus in modern oncology research, addressing the challenge that only a subset of patients derives clinical benefit from immune checkpoint inhibitors and other immunotherapeutic approaches. This guide compares the predominant biomarker enrichment strategies, providing researchers with a framework for selecting and implementing these designs in early-phase trials.
Core Biomarker Enrichment Trial Designs
Biomarker enrichment strategies in early-phase trials can be broadly categorized into several distinct designs, each with specific applications, advantages, and limitations. The choice of design depends on the strength of preliminary evidence for the biomarker, its prevalence, and the underlying scientific rationale.
Table 1: Comparison of Core Biomarker Enrichment Trial Designs
| Design Type | Key Principle | When to Use | Advantages | Limitations |
|---|---|---|---|---|
| Enrichment Design | Enroll only biomarker-positive patients [37] | Strong preliminary evidence that benefit is restricted to biomarker-positive subgroup [38] | Efficient signal detection; reduced sample size; increased probability of success in targeted population [39] [11] | Narrower regulatory label; requires validated assay; no information on biomarker-negative patients [37] |
| All-Comers Design | Enroll both biomarker-positive and negative patients without restriction [37] | Preliminary evidence regarding treatment effects in marker subgroups is unclear [38] | Allows retrospective biomarker analysis; avoids missing efficacy in unselected populations [37] | May dilute overall treatment effect if benefit is restricted to a subgroup; larger sample size required [37] |
| Adaptive Enrichment Design | Starts with all-comers population, then restricts enrollment based on interim analysis [39] [40] | Uncertainty about biomarker cut-off or which subgroups benefit; learning and confirming approach needed [39] | Flexibility to refine population during trial; avoids premature termination for full population [39] [40] | Statistical complexity; potential for false enrichment; requires careful planning of interim analyses [39] |
| Stratified Randomization | Enroll all-comers but randomize within biomarker subgroups [37] | Biomarker is prognostic; both low and high biomarker patients may benefit [37] | Removes confounding bias; ensures balanced arms for subgroup comparisons [37] | Requires larger sample size; complex trial logistics [37] |
Advanced Adaptive Designs for Biomarker Integration
Recent methodological advances have focused on adaptive designs that allow for biomarker threshold estimation and population refinement during the trial. These approaches are particularly valuable for continuous biomarkers where no validated cut-off exists at trial initiation.
Biomarker Enrichment and Adaptive Threshold (BEAT) Design
The BEAT design updates the estimated optimal biomarker threshold in blocks by maximizing a utility that balances the size of the biomarker-positive population and the treatment effect in that population [40]. This design allows flexible patient enrichment where biomarker-positive patients are enrolled in the next block, while biomarker-negative patients may be enrolled or excluded based on estimation precision and predictive probability of failure [40].
Key Methodological Components:
- Interim Analyses: Pre-specified interim analyses assess accumulating data to inform adaptations
- Decision Rules: Based on predictive probability of success at final analysis [39]
- Stopping Rules: Early termination for futility based on predictive probability for biomarker-positive patients [40]
- Bayesian Methods: Used for calculating posterior distributions and predictive probabilities [39]
Table 2: Quantitative Performance Comparison of Adaptive Designs
| Design Feature | Classical Single-Stage Design | Two-Stage Adaptive Enrichment Design | BEAT Design |
|---|---|---|---|
| Probability of Correct Decision | Lower (benchmark) | Higher [39] | Highest [40] |
| Sample Size Efficiency | Less efficient | More efficient [39] | Most efficient [40] |
| False Enrichment Rate | Not applicable | Controlled [39] | Minimized [40] |
| Threshold Estimation Accuracy | Not applicable | Moderate | High with precision estimates [40] |
| Flexibility for Futility Stopping | Limited | Available for full population [39] | Available for both full population and subgroups [40] |
Experimental Protocols for Implementation
Protocol 1: Two-Stage Adaptive Biomarker-Guided Design
This protocol is adapted from the design proposed in the context of an oncology Proof of Concept (PoC) trial [39]:
- Stage 1 Enrollment: Recruit an initial cohort of patients (e.g., n=14) from the full population without biomarker restriction
- Interim Analysis (IA): Conduct when pre-specified number of patients have evaluable data
- Calculate predictive probability of success for full population
- If predictive probability < ηfutility, stop trial for futility
- If predictive probability > ηsuccess, continue to Stage 2 with full population
- If promising but inconclusive, identify biomarker subgroup using predefined criteria and continue with enriched population [39]
- Biomarker Threshold Identification: For continuous biomarkers, determine cutoff that divides patients into subgroups based on estimated probability of response to treatment [39]
- Stage 2 Enrollment: Recruit additional patients based on decision from IA
- Final Analysis: Evaluate treatment effect in final population using Bayesian methods with pre-specified decision criteria [39]
Protocol 2: BEAT Design Implementation
This protocol implements the Biomarker Enrichment and Adaptive Threshold detection method [40]:
- Blockwise Enrollment: Divide trial into multiple blocks (typically 3-5)
- Biomarker Response Modeling: Fit model (e.g., logistic regression) to relate biomarker to treatment response after each block [40]
- Utility Optimization: Calculate optimal biomarker threshold that maximizes utility function balancing subgroup size and treatment effect [40]
- Adaptive Enrollment: For next block:
- Enroll all patients above updated threshold
- Optionally enroll some patients below threshold based on estimation precision
- Futility Assessment: After each block, calculate predictive probability of success for biomarker-positive patients; stop if below threshold [40]
- Final Analysis: Classify all enrolled patients as biomarker-positive or negative based on final estimated threshold; test treatment effects accordingly [40]
Visualization of Adaptive Biomarker Trial Design
The following diagram illustrates the decision pathway for a two-stage adaptive biomarker-guided trial design:
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of biomarker enrichment strategies requires specialized reagents and platforms for biomarker assessment and data analysis.
Table 3: Essential Research Reagent Solutions for Biomarker-Driven Trials
| Reagent/Platform | Primary Function | Application in Immunotherapy Trials |
|---|---|---|
| PD-L1 IHC Assays (22C3, 28-8, SP142, SP263 clones) [11] | Detect PD-L1 protein expression in tumor tissue | Patient selection for PD-1/PD-L1 inhibitors; cutoff determination [11] [21] |
| NGS Panels | Assess tumor mutational burden (TMB), microsatellite instability (MSI), specific mutations [11] | Identify patients with TMB-H (≥10 mut/Mb) or MSI-H tumors for immunotherapy [11] |
| ctDNA/Liquid Biopsy Assays | Detect tumor-derived DNA in blood [1] [21] | Dynamic biomarker monitoring; assessment of tumor heterogeneity [1] |
| Multiplex Immunofluorescence | Simultaneous detection of multiple immune cell markers (CD8, CD4, CD68, etc.) [21] | Quantify tumor-infiltrating lymphocytes (TILs) and spatial organization in tumor microenvironment [21] |
| Variance Stabilizing Normalization (VSN) | Data normalization to minimize cohort discrepancies [41] | Improve reproducibility of biomarker measurements across batches and cohorts [41] |
| Bayesian Analysis Software (e.g., Stan, JAGS) | Calculate posterior distributions and predictive probabilities [39] [40] | Interim decision-making for adaptive designs; futility analysis [39] |
Biomarker enrichment strategies in early-phase trial design represent a paradigm shift in immuno-oncology drug development. The comparative analysis presented in this guide demonstrates that adaptive enrichment designs offer significant advantages over traditional fixed designs when biomarker uncertainty exists. These designs increase trial efficiency by focusing resources on patient populations most likely to benefit, while maintaining flexibility through pre-planned interim analyses.
The successful implementation of these strategies requires careful consideration of multiple factors: the strength of preliminary biomarker evidence, assay validation status, statistical operating characteristics, and operational feasibility. As immunotherapy research evolves, emerging approaches such as multi-omics biomarker integration, machine learning-based predictive models, and dynamic biomarker monitoring are likely to further enhance the precision of patient enrichment strategies.
Researchers should select enrichment designs based on their specific developmental context, recognizing that well-executed biomarker strategies can accelerate the delivery of effective immunotherapies to appropriate patient populations while reducing exposure to ineffective treatments in others.
The Biomarker Validation Pipeline: A Stepwise Framework from Analytical to Clinical Validation
The pre-analytical phase, encompassing all processes from sample collection to analysis, represents the most vulnerable stage in the total testing process and stands among the greatest challenges for laboratory professionals [42]. In the context of biomarker validation for predicting immunotherapy response, this phase takes on heightened importance. The accuracy and reliability of predictive biomarkers such as PD-L1 expression, tumor mutation burden (TMB), and gene expression profiles directly depend on rigorous pre-analytical controls [43] [21]. Unfortunately, pre-analytical activities, management of unsuitable specimens, and reporting policies lack full standardization and harmonization worldwide [42]. This variability introduces significant challenges for multi-center clinical trials and biomarker validation studies, where consistent sample handling across different sites is paramount for generating comparable, high-quality data.
The complexity of the pre-analytical phase is particularly evident in immunotherapy research, where biomarkers are derived from diverse sources including tissue, blood, and other bodily fluids [20] [21]. The integrity of these samples directly impacts the performance of downstream analytical techniques such as immunohistochemistry (IHC), ELISA, genomic sequencing, and emerging technologies like surface-enhanced Raman spectroscopy (SERS) [44] [20]. Even with advanced detection platforms, pre-analytical inconsistencies can compromise the predictive accuracy of biomarkers intended to guide immunotherapy treatment decisions [43]. As research moves toward multi-modal biomarker panels and liquid biopsy technologies, standardized pre-analytical protocols become increasingly critical for successful clinical implementation of immunotherapy response prediction tools [43] [20] [21].
Pre-Analytical Variables and Their Impact on Biomarker Integrity
Key Pre-Analytical Factors
The pre-analytical phase encompasses numerous variables that can alter biomarker stability and detection. Understanding and controlling these factors is essential for maintaining sample quality in immunotherapy research:
- Sample Collection Variables: The method of blood draw, including tourniquet application time, can alter the concentration of numerous analytes [42]. For tissue biopsies, sampling location (primary vs. metastatic sites) and collection methods introduce variability, particularly for biomarkers like PD-L1 that show spatial heterogeneity [21].
- Sample Timing: The diurnal variation in certain biomarkers and the collection point during disease progression or treatment can significantly impact results. Emerging research suggests that molecular progression detectable through liquid biopsy might precede anatomical progression, requiring precise timing for optimal predictive value [45].
- Sample Handling and Processing: Centrifugation conditions, temperature during transport and storage, and processing delays represent critical control points. Studies demonstrate that hemolysis affects lactate dehydrogenase (LDH) and aspartate aminotransferase (AST) measurements, both potential biomarkers for immunotherapy response [42].
- Sample Identification and Labeling: Patient misidentification or improper specimen labeling can lead to erroneous clinical decisions. Standardized protocols for patient verification and sample labeling are fundamental pre-analytical requirements [46].
Impact on Downstream Analytical Performance
Pre-analytical inconsistencies directly impact the performance of analytical techniques used in biomarker detection. Research on ELISA assays demonstrates how matrix effects and sample handling influence results. One study evaluating ELISA performance for urinary biomarkers found that only 3 of 11 commercially available tests passed accuracy thresholds, with the majority exhibiting coefficients of variation >20% [47]. This disappointing performance was attributed to the urine matrix itself and/or presence of markers in various isoforms, highlighting how sample-specific factors degrade assay performance.
Similarly, pre-analytical factors affect advanced detection technologies. Surface-enhanced Raman spectroscopy (SERS), while offering approximately 1.5-2 orders of magnitude lower detection limits compared to fluorescence-based immunoassays, remains susceptible to pre-analytical variations [44]. The median limit of detection (LOD) for SERS-based immunoassays is 4.3 × 10−13 M compared to 1.5 × 10−11 M for fluorescence immunoassays, but both techniques suffer from challenges including non-specific protein binding and insufficient reproducibility that can be exacerbated by poor pre-analytical practices [44].
Table 1: Impact of Pre-Analytical Errors on Biomarker Detection Technologies
| Analytical Technique | Common Pre-Analytical Challenges | Impact on Biomarker Detection |
|---|---|---|
| Immunohistochemistry (IHC) | Delayed fixation, improper fixative type and volume, fixation time | Altered antigen detection, particularly for PD-L1 expression [21] |
| ELISA | Sample matrix effects, hemolysis, improper storage | Reduced accuracy and precision; high coefficients of variation [47] |
| Genomic Sequencing | Delay in processing, improper storage conditions | Nucleic acid degradation affecting TMB and mutation detection [43] |
| Liquid Biopsy | Cellular lysis during collection, improper stabilizers | False positives in circulating tumor DNA analysis [21] |
| SERS | Non-specific binding, sample contamination | Reduced sensitivity and reproducibility despite low LOD [44] |
Standardization Strategies for Pre-Analytical Workflows
Implementing Quality Control Measures
Establishing robust quality control systems is fundamental for standardizing the pre-analytical phase in immunotherapy biomarker research. Several key strategies have demonstrated effectiveness:
- Automated Identification Systems: Implementing barcode ID systems prevents specimen misidentification and inaccurate labeling, reducing errors at the point of collection [46]. Automated systems for identifying, storing, and tracking samples can eliminate errors at the front end while reducing labor intensity compared to manual implementation.
- Standardized Procedures: Development and adherence to standardized protocols for patient preparation, sample collection, transport, handling, storage, and preparation for testing should represent a major focus [42]. This includes specific guidelines for blood collection tubes, centrifugation parameters, and aliquot preparation.
- Comprehensive Documentation: Specific software developed for recording pre-analytical errors enables harmonization of incident reporting practices within the same laboratory and across national and international laboratories [42]. Systematic recording of pre-analytical errors is highly favorable for identifying recurring issues and implementing corrective actions.
- Rejection Criteria Establishment: Clear, standardized criteria for sample rejection based on defined quality parameters help maintain consistency across studies and clinical sites [42]. This includes specifications for hemolysis indices, lipemia, icterus, and clot formation.
Addressing Sample-Specific Challenges
Different sample types present unique pre-analytical considerations that must be addressed in standardized protocols:
- Tissue Samples: For solid tumor biopsies intended for PD-L1 staining or genomic analysis, standardized fixation protocols are critical. Cold ischemia time (time between tissue collection and fixation) should be minimized, with fixation typically in 10% neutral buffered formalin for defined durations based on tissue size [21].
- Liquid Biopsies: Blood samples for circulating tumor DNA (ctDNA) analysis require specific collection tubes with stabilizers to prevent white blood cell lysis and genomic DNA contamination. Consistent centrifugation protocols are essential for plasma preparation without cellular contamination [21].
- Urine Samples: Studies evaluating ELISA performance in urine highlight the particular challenges of this matrix, including variable pH, protein concentration, and the presence of proteases that can degrade protein biomarkers [47]. Standardized collection with protease inhibitors and pH stabilization is recommended.
Experimental Approaches for Evaluating Pre-Analytical Variables
Methodologies for Assessing Pre-Analytical Factors
Rigorous experimental approaches are necessary to quantify the impact of pre-analytical variables on biomarker stability and detection. Key methodological considerations include:
- Stability Studies: Systematic evaluation of biomarker stability under various storage conditions (temperature, duration) and processing delays. The study by Cuhadar et al. assessed the stability of common biochemical parameters in serum separator tubes with or without gel barrier subjected to various storage conditions, providing evidence-based guidelines for sample handling [42].
- Interference Testing: Controlled studies evaluating the impact of common interferents like hemolysis, lipemia, and icterus on biomarker detection. Koseoglu et al. investigated effects of different hemolysis degrees on common biochemical parameters, finding clinically significant differences for LDH, AST, potassium, and total bilirubin even with visually undetectable hemolysis [42].
- Matrix Comparison Studies: Parallel testing of biomarkers across different sample matrices (serum vs. plasma; tissue vs. liquid biopsy) to establish equivalence or differences. Such studies are particularly relevant for liquid biopsy development where plasma-based biomarkers may replace tissue-based ones [21].
- Method Comparison Studies: Evaluation of the same biomarker across different analytical platforms to assess consistency. This approach is exemplified by studies comparing predictive accuracy of PD-L1 immunohistochemistry, tumor mutation burden, gene expression profiling, and combined biomarkers for immunotherapy response [43].
Table 2: Experimental Protocols for Evaluating Pre-Analytical Variables
| Experimental Approach | Key Protocol Steps | Data Output |
|---|---|---|
| Biomarker Stability Testing | 1. Aliquot samples from single source2. Expose to different time/temperature conditions3. Analyze all samples in same run4. Compare results to baseline | Stability specifications (allowable time delays, storage conditions) |
| Interference Studies | 1. Prepare sample pools without interferent2. Spike with known concentrations of interferent3. Measure biomarker concentration4. Compare to unspiked samples | Threshold values for acceptable interference; correction algorithms |
| Sample Collection Device Comparison | 1. Collect parallel samples using different devices2. Process identically3. Analyze for multiple biomarkers4. Perform statistical comparison | Validation of collection devices for specific biomarkers |
| Pre-analytical Error Tracking | 1. Implement standardized error classification2. Record all pre-analytical incidents3. Analyze trends and root causes4. Implement corrective actions | Quality indicators; error rates; improvement measures |
Case Study: Evaluating Sample Collection Systems
A comprehensive validation study of different serum vacuum tubes for routine clinical chemistry testing exemplifies rigorous pre-analytical evaluation [42]. Such studies are crucial because blood collection tube components including various additives, clot activators, anticoagulants, surfactants, lubricants, stoppers, and separator gels may interact with blood and cause variable biases in laboratory test results. The experimental protocol should include:
- Parallel Sample Collection: Blood samples from the same venipuncture are distributed into different collection devices to minimize biological variation.
- Multiple Biomarker Analysis: Testing a panel of biomarkers relevant to the research context, including those with known susceptibility to pre-analytical variations.
- Statistical Comparison: Using appropriate statistical methods (Bland-Altman analysis, correlation coefficients) to assess agreement between collection systems.
- Clinical Relevance Assessment: Determining if observed differences would impact clinical interpretation or research conclusions.
Similar methodologies can be applied to evaluate sample types relevant to immunotherapy research, including tissue preservation methods, liquid biopsy collection systems, and stabilizers for molecular analysis.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Pre-Analytical Standardization
| Reagent/Kit | Primary Function | Application in Immunotherapy Biomarker Research |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Stabilizes nucleated blood cells prevents genomic DNA contamination | Maintains integrity of circulating tumor DNA for liquid biopsy-based TMB assessment [21] |
| Rapid Tissue Fixation Systems | Standardized fixation that preserves antigenicity and nucleic acids | Consistent PD-L1 IHC staining and molecular analysis from limited tissue samples [21] |
| Proteinase Inhibitor Cocktails | Prevents proteolytic degradation of protein biomarkers | Stabilizes protein targets in urine and blood samples for ELISA-based detection [47] |
| Temperature-Responsive Liposomes | Signal amplification probes for ultrasensitive detection | Enables detection of low-abundance biomarkers in pre-analytically challenged samples [48] |
| Streptavidin-Biotin Complex Reagents | Enhances sensitivity and specificity in immunoassays | Improves detection limits for biomarker quantification in complex matrices [20] |
| Specialized Urine Preservation Kits | Stabilizes urine protein composition and prevents degradation | Standardizes urine biomarker measurements for immunotherapy toxicity monitoring [47] |
Visualizing Pre-Analytical Workflows and Relationships
Pre-Analytical Phase Pathway
Error Impact on Immunotherapy Biomarkers
The validation of biomarkers to predict response to immunotherapy is fundamentally dependent on rigorous standardization of the pre-analytical phase. As research advances toward multi-modal biomarker panels and liquid biopsy technologies, consistent sample handling across multiple collection sites becomes increasingly critical [20] [21]. The promising field of immunotherapy biomarkers, including PD-L1 expression, tumor mutation burden, gene expression profiles, and circulating tumor DNA, requires meticulous attention to pre-analytical variables to ensure reliable predictive accuracy [43] [21].
Future directions should focus on developing evidence-based guidelines specifically tailored to immunotherapy biomarker samples, implementing automated tracking systems for pre-analytical variables, and establishing quality metrics that can be monitored across research networks. As new detection technologies with exceptional sensitivity emerge, such as temperature-responsive liposome-linked immunosorbent assays capable of detecting prostate specific antigen at concentrations as low as 27.6 ag/mL [48], the importance of pre-analytical standardization becomes even more pronounced. Only through comprehensive control of the pre-analytical phase can the promise of precision immunotherapy be fully realized, ensuring that biomarkers accurately stratify patients who will benefit from these powerful but potentially toxic treatments.
In the field of cancer immunotherapy research, the reliable measurement of biomarkers such as PD-L1, tumor mutational burden (TMB), and microsatellite instability (MSI) is fundamental to identifying patients who will respond to treatment. Analytical validation provides the critical foundation that ensures these measurements are trustworthy and meaningful. It confirms through objective evidence that an analytical test consistently meets predefined specifications for accuracy, precision, and reproducibility for its intended purpose [49]. Without rigorous analytical validation, even the most promising biomarker can yield unreliable data, leading to incorrect conclusions in research and potentially compromising patient selection in clinical trials.
The context of immunotherapy presents unique challenges for assay validation. Biomarkers like PD-L1 exhibit significant biological heterogeneity and can be influenced by prior treatments, while complex biomarkers like blood-based TMB (bTMB) require careful consideration of pre-analytical variables and specialized methods to differentiate tumor-specific signals from background noise [50] [12]. This guide objectively compares key methodologies and technology platforms used for analytical validation, providing researchers with the experimental frameworks and data needed to select appropriate strategies for their immunotherapy biomarker development programs.
Core Principles of Analytical Validation
Analytical validation systematically evaluates a method's performance characteristics to ensure it is fit for its intended use. The key parameters, along with their definitions and typical experimental approaches, are summarized in Table 1 below.
Table 1: Core Parameters of Analytical Validation and Their Assessment
| Parameter | Definition | Experimental Approach |
|---|---|---|
| Accuracy (Trueness) | Closeness of agreement between the average value from a large series of test results and an accepted reference value [49]. | Comparison of measured values to a certified reference material (CRM) or results from a reference method. |
| Precision | Closeness of agreement between independent test results obtained under stipulated conditions [49]. | Repeated measurements of the same sample under different conditions (within-run, between-day, between-operator). |
| Reproducibility | A form of precision evaluated under conditions where different factors (e.g., laboratory, technician, day) are varied [49]. | Testing identical samples across multiple laboratories, instruments, or operators. |
| Robustness | Ability of a method to remain unaffected by small, deliberate variations in method parameters [49]. | Systematic alteration of critical steps (e.g., incubation times ±5%, temperatures ±2°C). |
| Limits of Quantification (LOQ) | The highest and lowest concentrations of an analyte that can be reliably measured with acceptable precision and accuracy [49]. | Repeated measurement of serially diluted samples to determine the range where precision and accuracy fall within acceptable limits (e.g., ±20%). |
| Selectivity/Specificity | Ability of the method to measure and differentiate the analyte in the presence of other components that may be expected to be present [49] [50]. | Testing samples spiked with potential interferents (e.g., hemoglobin, lipids) or samples with structurally similar compounds. |
These parameters are interdependent. For instance, a robust assay is more likely to demonstrate good precision across different runs and locations. In the context of immunotherapy, parameters like selectivity are paramount. For example, when validating a circulating tumor DNA (ctDNA) assay for TMB measurement, the method must effectively differentiate true tumor-derived mutations from germline polymorphisms or alterations arising from clonal hematopoiesis [50].
Experimental Protocols for Key Validation Parameters
Protocol for Precision Measurement (Following a SOP framework [49])
- Sample Preparation: Select at least three quality control (QC) samples with analyte concentrations spanning the assay's dynamic range (low, medium, high). Prepare a sufficient volume to conduct all planned runs.
- Experimental Design: Run each QC sample in a minimum of five replicates per run. Conduct runs over at least three separate days, using different reagent lots if possible, and involving different operators to capture intermediate precision.
- Data Analysis: Calculate the mean, standard deviation (SD), and coefficient of variation (CV) for the replicates at each concentration level, both within a single run (repeatability) and between different runs (intermediate precision).
- Acceptance Criteria: The CV for repeatability and intermediate precision should typically be within 20% (or stricter thresholds based on assay requirements). High precision is often prioritized in biotech for faster data turnaround and cost-efficiency [51].
Protocol for Robustness Testing (Following a SOP framework [49])
- Identify Critical Parameters: Determine the steps in the assay procedure most likely to impact the result (e.g., incubation time, temperature, reagent volumes, operator).
- Systematic Variation: Perform the assay using the same set of samples while intentionally varying one parameter at a time. For example, test incubation times of 25, 30, and 35 minutes for a nominal 30-minute step.
- Analysis: Compare the measured analyte concentrations obtained under the varied conditions to those from the standard protocol.
- Incorporate Findings: If results are unaffected, define acceptable tolerances in the final protocol (e.g., "30 ± 3 minutes"). If a parameter is highly sensitive, refine the protocol to control it more stringently.
Diagram 1: Experimental workflow for assessing assay robustness.
Comparison of Technology Platforms for Biomarker Validation
The choice of technology platform significantly impacts the efficiency, scalability, and reliability of biomarker validation. Different classes of biomarkers require specialized approaches, as detailed in Table 2.
Table 2: Comparison of Technology Platforms for Biomarker Analysis
| Platform Category | Example Platforms | Key Advantages | Key Limitations | Automatability & Suitability for Validation |
|---|---|---|---|---|
| Protein Analysis | ELISA, MSD, Luminex, GyroLab | High sensitivity (MSD, GyroLab), quantitative, multiplexing capability (Luminex, MSD) [51]. | Limited multiplexing (ELISA), expensive reagents (MSD, Luminex) [51]. | High. Fully automated systems available; ideal for high-precision, quantitative validation [51]. |
| DNA/RNA Analysis | qPCR, dPCR, NGS | High sensitivity (qPCR/dPCR), comprehensive profiling (NGS) [52] [51]. | Limited multiplexing (qPCR), complex data analysis (NGS), expensive (NGS) [51]. | Moderate to High. Automated systems available for qPCR and NGS library prep; excellent for ctDNA and TMB analysis [51]. |
| Cellular Analysis | Traditional and Spectral Flow Cytometry | High-throughput, multiparameter single-cell analysis, established technology [51]. | Compensation requirements (traditional), complex data analysis (spectral) [51]. | High. Fully automated cell sorting and analysis; best for cellular biomarkers like TILs [51]. |
| Spatial Biology | CODEX, Imaging Mass Cytometry | Spatially resolved analysis, high-plex protein or gene expression in tissue context [51]. | Expensive, significant tissue preparation, complex data analysis [51]. | High. Fully automated image acquisition and analysis; key for understanding tumor microenvironment [51]. |
Platforms like ELISA and qPCR remain widely used due to their established protocols and cost-effectiveness. However, for complex biomarker profiles, multiplexing platforms like Luminex or MSD are preferable. When the biomarker is cellular or requires analysis of specific cell populations, flow cytometry is the leading choice [51]. Automation is a key consideration, as it improves consistency, reliability, throughput, and standardization, which are crucial for efficient validation [51].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful analytical validation relies on a suite of high-quality, well-characterized reagents and materials. The following table lists essential components for setting up and running validated immunoassays, a common method for measuring immunotherapy biomarkers like soluble proteins.
Table 3: Key Research Reagents and Materials for Immunoassay Validation
| Reagent / Material | Function and Importance in Validation |
|---|---|
| Certified Reference Material (CRM) | Provides an accepted reference value to establish method accuracy and trueness. Critical for calibrating assays and demonstrating traceability [49]. |
| Quality Control (QC) Samples | Used to monitor precision and stability of the assay over time. Should be matrix-matched and stored in small, single-use aliquots to avoid freeze-thaw cycles [49]. |
| Matrix-Matched Calibrators | Calibrators prepared in the same biological matrix as the sample (e.g., plasma, serum) account for matrix effects and are essential for achieving accurate recovery and parallelism [49]. |
| High-Specificity Antibodies | The selectivity of the assay depends heavily on the specificity of the capture and detection antibodies. Validating these reagents is a prerequisite for the entire process [49]. |
| Blocking Buffers | Minimize non-specific binding, which is vital for achieving a high signal-to-noise ratio and improving the sensitivity and specificity of the assay. |
Diagram 2: Relationship between key research reagents and the analytical parameters they support.
Analytical validation is a non-negotiable step in the development of robust biomarkers for immunotherapy. The journey from a promising biological signal to a clinically useful test demands rigorous demonstration of accuracy, precision, and reproducibility across well-defined experimental parameters. As the field evolves, the validation of complex, novel biomarkers like blood-based TMB or multi-omics signatures will require even more sophisticated approaches, including the integration of AI and machine learning for data analysis and the use of advanced humanized models to better bridge the gap between preclinical discovery and clinical application [50] [53].
A precision-driven approach, where consistency and reproducibility are prioritized, often provides the most efficient path to generating reliable, actionable data for decision-making in drug development [51]. By adhering to structured experimental protocols, carefully selecting appropriate technology platforms, and utilizing high-quality reagents, researchers can successfully navigate the complexities of analytical validation, thereby accelerating the delivery of effective immunotherapies to patients.
The success of cancer immunotherapy, particularly immune checkpoint blockade (ICB), has revolutionized oncology treatment. However, a significant challenge persists: response rates vary dramatically, and only a minority of patients across most cancer types experience durable benefits [2]. This clinical reality has created an urgent need for robust biomarkers that can accurately predict which patients will respond to treatment, thereby personalizing therapy and improving outcomes. In this pursuit, three high-throughput technologies have emerged as fundamental tools: Next-Generation Sequencing (NGS), Single-Cell RNA Sequencing (scRNA-seq), and Mass Spectrometry (MS). Each technology illuminates a different facet of the complex biology underlying the tumor-immune interaction. The validation of biomarkers to predict response to immunotherapy now increasingly relies on the integration of these technologies, moving beyond single-parameter assays to multi-dimensional profiles of the tumor and its microenvironment [2] [54]. This guide provides an objective comparison of these platforms, detailing their performance, methodologies, and applications in biomarker discovery for immunotherapy.
The following table provides a systematic comparison of the three core technologies, highlighting their primary applications in immunotherapy biomarker discovery.
Table 1: Comparative Analysis of High-Throughput Biomarker Discovery Technologies
| Feature | Next-Generation Sequencing (NGS) | Single-Cell RNA Sequencing (scRNA-seq) | Mass Spectrometry (MS) |
|---|---|---|---|
| Primary Biomarker Class | Genomic & Transcriptomic | Transcriptomic (at single-cell resolution) | Proteomic & Metabolomic |
| Key Applications in Immunotherapy | Tumor Mutational Burden (TMB), Microsatellite Instability (MSI), Somatic mutations, Neoantigen prediction [2] | Deconvoluting immune cell heterogeneity, T-cell clonality, Cellular states in the Tumor Microenvironment (TME) [55] [54] | Protein/phosphoprotein abundance, Post-translational modifications, Metabolic dysregulation [56] [57] |
| Typical Sample Input | Bulk tissue | Single cells (suspensions) | Bulk tissue, single cells, biofluids [57] |
| Level of Information | Bulk analysis of cell populations | Single-cell resolution | Bulk (common) or emerging single-cell resolution [57] |
| Clinical Adoption (Examples) | FDA-approved PD-L1 IHC, TMB (KEYNOTE-158), MSI-H [58] [2] | Primarily in research and clinical trials (e.g., >75 trials listed on ClinicalTrials.gov) [55] | Emerging in clinics; used in research for biomarker panels (e.g., CPTAC) [59] [60] |
| Key Strengths | Comprehensive, hypothesis-free genome-wide analysis; well-established workflows | Unmasks cellular heterogeneity and rare cell populations; defines cell lineages and trajectories [61] | Direct measurement of functional effector molecules (proteins); can detect post-translational modifications [59] |
| Key Limitations | Does not capture cellular heterogeneity or functional protein data | Cannot directly measure protein levels or activity; destructive to sample [61] | Limited depth of coverage in single-cell mode; complex data analysis [57] |
To further quantify their performance, the table below summarizes key experimental metrics from representative studies.
Table 2: Experimental Performance Metrics from Key Studies
| Technology | Specific Application | Reported Performance / Output | Context / Study |
|---|---|---|---|
| NGS | Tumor Mutational Burden (TMB) as a biomarker for anti-PD-1 (pembrolizumab) | FDA-approved as a predictive biomarker across solid tumors based on KEYNOTE-158 trial [58] | Validated in a pan-cancer context |
| scRNA-seq | High-resolution definition of myeloid cell subtypes and tumor-associated T cells in NSCLC | Identification of cell subtypes and their functional characteristics linked to therapy response [55] | Applied in clinical trial NCT04789252 |
| Label-free MS Proteomics | Single-cell proteomic analysis of HeLa cells | Identification of ~843 proteins per single cell on average [57] | Demonstrates depth of coverage achievable at single-cell level |
| TMT-assisted MS Proteomics | Multiplexed single-cell proteomics | Identification of >1,000 proteins per cell, enabling analysis of cellular biological processes [57] | Allows multiplexing of 10-18 samples in a single run |
| Spatial Transcriptomics | Analysis of immune cell infiltration and spatial organization in the TME | Elucidation of spatial patterns predictive of therapeutic response [54] | Integrated with single-cell data for context |
Detailed Experimental Protocols
Understanding the standardized workflows for each technology is crucial for evaluating the experimental data they generate.
Next-Generation Sequencing (NGS) for Genomic Biomarkers
Protocol Objective: To identify genomic alterations (e.g., mutations, TMB, MSI) from tumor tissue.
- Sample Preparation & DNA Extraction: DNA is extracted from tumor tissue (typically FFPE) and matched normal sample (e.g., blood or saliva). Quality control (QC) is performed to assess DNA quantity and integrity.
- Library Preparation: Fragmented DNA undergoes end-repair, adapter ligation, and PCR amplification to create a sequencing library. Target enrichment is often performed using hybrid capture-based panels (e.g., MSK-IMPACT) for specific genes or whole exome/genome sequencing.
- Sequencing: Libraries are loaded onto NGS platforms (e.g., Illumina) for high-throughput parallel sequencing.
- Bioinformatic Analysis:
- Alignment: Sequencing reads are aligned to a reference human genome.
- Variant Calling: Somatic variants (SNVs, indels) are identified by comparing tumor and normal sequences.
- Biomarker Calculation: TMB is calculated as the number of non-synonymous mutations per megabase of the sequenced genome. MSI status is determined by assessing the length instability of microsatellite loci compared to normal tissue.
- Clinical Correlation: The identified genomic biomarkers are correlated with clinical response to immunotherapy from trial data (e.g., high TMB associated with improved response to pembrolizumab) [58] [2].
Single-Cell RNA Sequencing (scRNA-seq) for Cellular Heterogeneity
Protocol Objective: To profile the transcriptome of individual cells within the tumor microenvironment (TME).
- Single-Cell Isolation: A single-cell suspension is prepared from fresh tumor tissue. Cells are isolated using:
- Microfluidic Technology (e.g., Fluidigm C1, 10x Genomics Chromium): This is the most common high-throughput method, capturing cells in nanoliter-sized droplets [61].
- Fluorescence-Activated Cell Sorting (FACS): Used to sort specific cell populations based on surface markers prior to sequencing.
- Library Preparation: Within droplets or wells, cells are lysed, and mRNA is barcoded with Unique Molecular Identifiers (UMIs) during reverse transcription. This allows each transcript to be uniquely counted, mitigating PCR amplification bias [61]. The barcoded cDNA is then amplified and prepared for sequencing.
- Sequencing: Libraries are sequenced on NGS platforms, typically generating tens of thousands of reads per cell.
- Bioinformatic Analysis:
- Quality Control & Demultiplexing: Reads are assigned to individual cells based on their barcodes.
- Clustering & Cell Type Identification: Dimensionality reduction algorithms (e.g., t-SNE, UMAP) and clustering (e.g., Louvain) group cells based on similar gene expression patterns, identifying distinct cell types (e.g., T cells, macrophages, cancer cells).
- Differential Expression & Trajectory Inference: Analysis identifies genes differentially expressed between conditions or cell states and reconstructs developmental lineages [55] [61].
Diagram 1: scRNA-seq Workflow for Biomarker Discovery.
Mass Spectrometry-Based Proteogenomic Integration
Protocol Objective: To directly identify and quantify proteins and variant peptides resulting from genomic alterations, bridging the gap between genotype and phenotype.
- Sample Preparation: Proteins are extracted from tumor tissue or biofluids. They are digested into peptides (typically using trypsin). For multiplexed quantification, peptides can be labeled with isobaric tags (e.g., Tandem Mass Tags - TMT).
- Liquid Chromatography (LC): Peptides are separated by hydrophobicity using nano-flow liquid chromatography.
- Mass Spectrometry Analysis:
- Ionization: Peptides are ionized via Electrospray Ionization (ESI).
- Mass Analysis: The mass-to-charge ratio (m/z) of intact peptides is measured in the mass analyzer (e.g., Orbitrap, timsTOF).
- Fragmentation: Selected peptides are fragmented, and the m/z of the resulting fragments is measured, generating a spectrum that reveals the peptide's sequence.
- Proteogenomic Integration:
- Custom Database Search: A patient-specific protein database is created using genomic and transcriptomic (RNA-seq) data from the same sample. This database includes non-synonymous mutations, fusion genes, and novel splice junctions [59].
- Peptide Identification: MS/MS spectra are searched against this custom database to identify variant peptides and novel protein sequences that would be absent in generic reference databases.
- Validation: Identified biomarker candidates (e.g., S100A9 and GRN for HCC) are often validated using targeted MS (e.g., MRM/SRM) in larger patient cohorts [59] [60].
Diagram 2: Proteogenomic Workflow for Biomarker Discovery.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of these technologies relies on a suite of specialized reagents and platforms.
Table 3: Key Research Reagent Solutions for High-Throughput Biomarker Discovery
| Category | Item | Function |
|---|---|---|
| NGS | Hybrid-capture probes (e.g., MSK-IMPACT) | Enriches sequencing libraries for genes of interest, enabling focused and cost-effective analysis. |
| scRNA-seq | 10x Genomics Chromium System | A high-throughput microfluidic platform for simultaneous barcoding of thousands of single cells. |
| scRNA-seq | Unique Molecular Identifiers (UMIs) | Short random barcodes attached to each transcript during reverse transcription, enabling accurate digital counting and removal of PCR amplification bias [61]. |
| Mass Spectrometry | Tandem Mass Tags (TMT) | Isobaric chemical tags that allow multiplexed (up to 18-plex) relative quantification of peptides from different samples in a single LC-MS/MS run, reducing technical variability [57]. |
| Mass Spectrometry | nanoPOTS (Nanodroplet Processing in One Pot for Trace Samples) | An automated sample preparation platform that minimizes surface adsorptive losses, enabling proteomic analysis of single cells and very small samples [57]. |
| Data Analysis | Cell Ranger (10x Genomics) | A standardized software suite for processing raw sequencing data from the Chromium system into a gene expression matrix for downstream analysis. |
| Data Analysis | Seurat / Scanpy | Popular open-source R/Python packages for comprehensive analysis of scRNA-seq data, including clustering, visualization, and differential expression. |
The quest to validate biomarkers for immunotherapy response is increasingly moving beyond reliance on any single technology. While NGS provides the foundational genetic blueprint, scRNA-seq reveals the cellular composition and interactions within the TME, and mass spectrometry delivers functional data on the proteins and metabolites that execute cellular programs. The most powerful insights are emerging from the integration of these multi-omics datasets [58] [54]. For instance, proteogenomic analyses by the Clinical Proteomic Tumor Analysis Consortium (CPTAC) have identified functional subtypes and druggable vulnerabilities in cancers like lung adenocarcinoma that were missed by genomics alone [58] [59]. Similarly, spatial omics technologies are now adding a crucial layer of topological context, showing where these molecular events occur within the tissue architecture [54]. The future of biomarker discovery lies in harnessing these complementary technologies in concert, using advanced computational and artificial intelligence approaches to integrate their data, thereby generating a holistic and predictive view of the tumor-immune interface to guide personalized immunotherapy.
The advent of cancer immunotherapy has revolutionized oncology treatment, establishing itself as a crucial pillar for managing numerous tumor types [62]. However, not all patients respond equally to these treatments, creating an urgent need for reliable biomarkers that can predict treatment response and toxicity. Biomarkers now hold a central position in decision-making for clinical medicine, drug development, and treatment guidance [49]. In the specific context of immunotherapy, validated biomarkers are essential for selecting patients who are most likely to benefit from treatment, thereby optimizing outcomes and minimizing unnecessary exposure to potential side effects.
The clinical validation of a biomarker represents a critical stage in establishing its utility for patient care. This process focuses on assessing a biomarker's ability to accurately reflect the clinical state of interest—in this case, likely response to immunotherapy. Two statistical measures form the cornerstone of clinical validation: clinical sensitivity and clinical specificity [63] [64]. Sensitivity measures the test's ability to correctly identify patients who will respond to treatment (true positive rate), while specificity measures its ability to correctly identify those who will not respond (true negative rate) [65]. These metrics are intrinsically linked to the determination of an optimal cutoff value, which represents the threshold for classifying a test as positive or negative [63] [65].
This guide provides a comprehensive comparison of methodologies and technologies for establishing the clinical sensitivity, specificity, and optimal cutoff values for biomarkers predicting response to immunotherapy.
Core Concepts: Sensitivity, Specificity, and Cutoff Determination
Fundamental Definitions and Calculations
For a biomarker test used to predict response to immunotherapy, its performance is evaluated against a reference standard (e.g., confirmed tumor response per RECIST criteria) using a confusion matrix, as outlined below [63] [65].
Table 1: Components for Calculating Sensitivity and Specificity
| Metric | Definition | Calculation Formula |
|---|---|---|
| True Positive (TP) | Patients predicted to respond who do respond | - |
| False Negative (FN) | Patients predicted not to respond who actually would respond | - |
| True Negative (TN) | Patients predicted not to respond who do not respond | - |
| False Positive (FP) | Patients predicted to respond who do not respond | - |
| Sensitivity | Proportion of responders correctly identified | TP / (TP + FN) [63] [65] |
| Specificity | Proportion of non-responders correctly identified | TN / (TN + FP) [63] [65] |
From these core components, other key performance indicators can be derived.
Table 2: Derived Performance Metrics for Biomarker Tests
| Metric | Calculation Formula | Interpretation |
|---|---|---|
| Positive Predictive Value (PPV) | TP / (TP + FP) [63] |
Probability that a patient predicted to respond will actually respond |
| Negative Predictive Value (NPV) | TN / (TN + FN) [63] |
Probability that a patient predicted not to respond will actually not respond |
| Accuracy | (TP + TN) / (TP + FP + TN + FN) [63] |
Overall proportion of correct classifications |
It is critical to distinguish between analytical sensitivity and clinical sensitivity. Analytical sensitivity, often called the lower limit of detection (LLOD), refers to the lowest concentration of an analyte that an assay can reliably detect [64]. In contrast, clinical sensitivity is a measure of how well the test result correlates with the patient's clinical outcome [64].
The Receiver Operating Characteristic (ROC) Curve and Cutoff Determination
Most biomarker tests yield a continuous numerical value. To convert this into a clinically actionable "positive" or "negative" result, a cutoff value (or threshold) must be established. The choice of this threshold directly creates a trade-off between sensitivity and specificity [63]. Setting a low cutoff may increase sensitivity (minimizing false negatives, or漏诊), but at the expense of specificity (increasing false positives, or误诊). Conversely, a high cutoff improves specificity but reduces sensitivity [63] [65].
The Receiver Operating Characteristic (ROC) curve is the primary tool for visualizing this trade-off and determining the optimal cutoff. An ROC curve plots the true positive rate (sensitivity) against the false positive rate (1 - specificity) across all possible cutoff values [65].
The point on the ROC curve that is closest to the top-left corner of the graph (0,1) is generally considered the optimal cutoff, as it simultaneously maximizes both sensitivity and specificity [65]. The area under the ROC curve (AUC) is a single metric that summarizes the overall performance of the biomarker; an AUC of 1 represents a perfect test, while an AUC of 0.5 indicates no discriminative power, equivalent to a random guess [65].
Comparative Analysis of Immunoassay Technologies
The accurate measurement of biomarker levels hinges on the choice of analytical technology. While the enzyme-linked immunosorbent assay (ELISA) has long been the gold standard, advanced multiplex platforms now offer significant advantages for biomarker validation [66] [67].
Table 3: Comparative Analysis of Key Immunoassay Platforms
| Platform | Mechanism | Multiplexing Capacity | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Traditional ELISA [67] | Antibody-based colorimetric detection in a 96-well plate. | Single-plex only. | High specificity and sensitivity for its target; well-established and trusted; reproducible results [67]. | Measures only one analyte per sample; relatively large sample volume required [67]. |
| Electrochemiluminescence (ECL) / MSD [66] [67] | Uses electrochemical and chemiluminescent principles for detection. | Low-to-mid plex (typically up to 10-plex per well). | Up to 100x greater sensitivity than ELISA; broader dynamic range; reduced sample volume [66]. | Lower multiplexing capacity compared to bead-based or PEA assays. |
| Bead-Based (Luminex) [67] | Uses color-coded magnetic beads coated with capture antibodies. | Mid-to-high plex (typically up to 80 proteins) [67]. | Good for measuring groups of related proteins (e.g., cytokines); high-throughput; conserves sample [67]. | Potential for biological interference in high-plex panels; requires specialized instrumentation [67]. |
| Proximity Extension Assay (PEA) / Olink [67] [68] | Uses antibody pairs with DNA tags; binding event creates a quantifiable DNA barcode. | High-plex (up to 5,000+ proteins) [67]. | Ultra-high sensitivity and specificity; very low sample volume (1 µL); minimal cross-reactivity [67] [68]. | DNA-based readout may not directly correlate with functional protein activity. |
Quantitative Performance and Cost Data
The choice of platform significantly impacts not only data quality but also operational efficiency and cost.
Table 4: Quantitative Performance and Operational Comparison
| Parameter | Traditional ELISA | Multiplex Bead-Based (e.g., Luminex) | Multiplex ECL (e.g., MSD) |
|---|---|---|---|
| Sample Volume per Analyte | ~50-100 µL [67] | ~25-50 µL for a full panel [67] | Lower volume per analyte than ELISA [66] |
| Dynamic Range | Relatively narrow [66] | Broad [67] | Very broad (up to 5+ logs) [66] |
| Analytical Sensitivity | Good (varies by analyte) | Good to very good [67] | Excellent (up to 100x more sensitive than ELISA) [66] |
| Cost per Sample (Example) | ~$61.53 for 4 analytes [66] | ~$19.20 for a 4-plex panel [66] | Higher per-plex cost than bead-based, but cost-effective for low-plex panels |
| Hands-on Time | High for multiple analytes | Lower per data point [67] | Lower per data point |
The data shows that for a panel of four inflammatory biomarkers (IL-1β, IL-6, TNF-α, IFN-γ), using a multiplex assay can yield substantial cost savings of over $42 per sample compared to running four individual ELISAs [66]. Furthermore, multiplex platforms like MSD and LC-MS/MS are increasingly favored by regulators due to their superior precision, sensitivity, and freedom from matrix effects, which can facilitate a smoother regulatory review process [66].
Experimental Protocols for Clinical Validation
A robust clinical validation study requires a meticulously planned and executed protocol. The following workflow outlines the key stages.
Detailed Methodologies for Key Experiments
1. Cohort Definition and Sample Collection:
- Patient Selection: Define a prospective and well-characterized cohort of patients scheduled to receive immunotherapy. The cohort should reflect the intended use population. As per the 2025 SITC consensus, all immunotherapy clinical protocols should incorporate a defined set of essential biomarkers [62] [69].
- Sample Collection: Adhere to standardized pre-analytical procedures. Collect biofluids (e.g., serum, plasma) at baseline (prior to treatment initiation). Consistent handling, processing, and storage conditions (e.g., freeze-thaw cycles) are critical, as they directly impact analyte stability and subsequent measurement validity [49].
2. Biomarker Measurement and Clinical Outcome Assessment:
- Analytical Measurement: Run the collected samples on the chosen, previously analytically validated platform (e.g., multiplex immunoassay, LC-MS/MS) [49]. The assay should be performed with appropriate quality controls (blanks, calibrators, quality control samples) to ensure data reliability.
- Clinical Endpoint Assessment: The clinical outcome (response vs. non-response) must be determined independently of the biomarker test result, using a validated "gold standard." In oncology, this is typically radiographic tumor assessment per RECIST v1.1 criteria, performed by clinicians blinded to the biomarker data.
3. Data Analysis and Cutoff Determination:
- ROC Curve Construction: For the biomarker's continuous measurement, calculate sensitivity and specificity at every possible cutoff value. Use these data pairs to plot the ROC curve.
- Optimal Cutoff Selection: Identify the cutoff value that maximizes the Youden's Index (J = Sensitivity + Specificity - 1) or the point closest to the top-left corner of the ROC plot [65].
- Performance Calculation: At the chosen cutoff, calculate the final clinical sensitivity, specificity, PPV, NPV, and overall accuracy.
4. Independent Validation:
- The cutoff value and performance metrics established in the initial ("training") cohort must be validated in a separate, independent ("validation") cohort. This step is non-negotiable to confirm the generalizability of the biomarker and avoid overfitting.
Method Validation Parameters
According to best practices, any method used for biomarker quantification, whether ELISA or a multiplex platform, must undergo rigorous method validation to ensure the reliability of the data it generates. Key parameters to validate include [49]:
- Precision: The closeness of agreement between independent test results. This includes repeatability (within-run) and intermediate precision (between-run, between-days, between-analysts) [49].
- Trueness/Recovery: The closeness of agreement between the average value obtained from a large series of measurements and an accepted reference value. This is often assessed by spiking a known amount of analyte into the sample matrix [49].
- Selectivity/Specificity: The ability of the method to measure the analyte accurately in the presence of other components that may be expected to be present (e.g., cross-reactivity with similar molecules) [49].
- Limits of Quantification (LOQ): The highest and lowest concentrations of an analyte that can be quantitatively determined with acceptable precision and trueness [49].
- Parallelism/Dilution Linearity: Demonstrates that a sample can be diluted and still provide a reliable result, confirming that the matrix of the sample does not interfere with the assay [49].
- Sample Stability: Evaluates the stability of the analyte under specific conditions (e.g., freeze-thaw, benchtop storage) [49].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Key Reagents and Materials for Biomarker Validation Studies
| Item | Function/Description | Key Considerations |
|---|---|---|
| Validated Immunoassay Kits | Pre-designed panels (e.g., cytokine, immune checkpoint) for specific pathways. | Choose panels relevant to immunotherapy (e.g., PD-L1, cytokine profiles). Verify species reactivity and validate performance for your sample type [67]. |
| Matched Antibody Pairs | For developing in-house (Luminex, MSD) or custom assays. | Requires rigorous validation for specificity, sensitivity, and lack of cross-reactivity [67]. |
| Quality Controls (QC) | Calibrators and control samples for monitoring assay performance. | Essential for both intra- and inter-assay precision monitoring. Should be run in every batch [49]. |
| Biological Sample Collection Kits | Standardized tubes for blood, serum, or plasma collection. | Critical for pre-analytical consistency. Use tubes with appropriate additives (e.g., EDTA, Heparin) and ensure consistent processing protocols [49]. |
| Multiplex Analyzer | Instrument for running and reading multiplex assays (e.g., Luminex, MSD instruments). | Selection depends on chosen technology. Requires proper calibration and maintenance [67]. |
| Data Analysis Software | Software for instrument operation, data acquisition, and statistical analysis (ROC analysis). | Should include tools for calculating standard curves, concentrations, and advanced statistical modules for ROC and cutoff analysis. |
The development of reliable biomarkers is a critical component in advancing cancer immunotherapy, as it enables the identification of patients most likely to benefit from immune checkpoint inhibitors (ICIs) and other immunotherapeutic approaches. Despite the transformative success of immunotherapy in oncology, clinical benefits remain confined to a subset of patients, underscoring the necessity for robust predictive biomarkers to guide treatment selection [1] [12]. The validation of these biomarkers follows a highly regulated developmental process, progressing from analytical validation to clinical validation and, ultimately, to the demonstration of clinical utility [70].
Statistical validation forms the foundation of this process, ensuring that biomarkers can reliably distinguish between patient populations with divergent expected outcomes to a specific treatment. Key methodologies in this statistical framework include the proper partitioning of data into training sets and validation sets, and the application of Receiver Operating Characteristic (ROC) analysis to evaluate biomarker performance [70]. These approaches are essential for mitigating overfitting, assessing generalizability, and providing a quantitative measure of a biomarker's discriminatory power. The rigorous application of these statistical principles is paramount for translating promising biomarker candidates into clinically actionable tools that can personalize immunotherapy and improve patient outcomes.
Core Statistical Methodologies
Training and Validation Sets
The use of training and validation sets is a fundamental practice in statistical learning to ensure that a predictive model or biomarker signature generalizes well to new, unseen data. This process involves splitting the available study population into distinct groups.
- Training Set: This set of samples is used for the initial discovery and model building. In this phase, researchers identify and characterize a single biomarker or, more commonly, build a mathematical model or algorithm from a subset of measured variables [70]. For complex, multi-analyte assays, the computational algorithm must be fully defined and locked before moving to the validation phase [70].
- Validation Set: This independent sample group is used to test the external validity of the biomarker or model developed in the training set. The performance of the model on this set provides an unbiased evaluation of its predictive power [70].
- Cross-Validation: Techniques like 5-fold cross-validation are often employed to compensate for overfitting, especially when sample sizes are limited. However, it is crucial to recognize that internal validation or cross-validation alone is not sufficient for clinical application. External validation on an independent dataset, or multiple independent datasets, is required for regulatory approval and clinical implementation [70].
ROC Analysis and the Area Under the Curve (AUC)
The Receiver Operating Characteristic (ROC) curve is a fundamental tool for evaluating the diagnostic performance of a biomarker.
- Definition and Purpose: The ROC curve is a plot that illustrates the diagnostic ability of a binary classifier system by mapping the True Positive Rate (TPR or Sensitivity) against the False Positive Rate (FPR or 1-Specificity) across a series of cutoff thresholds [70] [71]. It provides a comprehensive visual representation of the trade-off between sensitivity and specificity.
- Area Under the Curve (AUC): The AUC is a single scalar value that summarizes the overall performance of the biomarker. An AUC of 0.5 indicates no discriminatory power (equivalent to random guessing), while an AUC of 1.0 denotes a perfect biomarker [72] [71]. In practice, an AUC value above 0.7 or 0.8 is often considered indicative of good predictive power.
- Cutoff Selection: The ROC curve enables researchers to determine the optimal cutoff point that best discriminates between responders and non-responders. This point is selected based on the clinical context, balancing the desired sensitivity and specificity [70] [72].
Advanced and Emerging Methodologies
Beyond these core methods, the field is advancing with more sophisticated statistical approaches.
- Covariate-Adjusted ROC (AROC): Traditional ROC analysis captures only marginal associations. Covariate-adjusted ROC methods incorporate individual-level factors (e.g., age, sex, comorbidities) to provide a refined, personalized evaluation of diagnostic precision. This is particularly important in heterogeneous clinical populations [71].
- Machine Learning (ML) Integration: ML models, including feedforward neural networks (FNNs), are being applied to AROC analysis. These models can capture complex, non-linear relationships between covariates and biomarker performance, offering a more flexible and powerful approach compared to traditional parametric methods [71].
- Multi-Omics and Biology-Guided Deep Learning: Integrating genomic, transcriptomic, and proteomic data through machine learning can improve biomarker precision. One approach is biology-guided deep learning (BgDL), where models are trained to simultaneously predict tumor microenvironment status and treatment outcomes from medical images, enhancing interpretability and biological relevance [73] [74].
Experimental Protocols for Biomarker Validation
The validation of predictive biomarkers in immunotherapy requires carefully designed experimental protocols. The following workflow outlines a standard approach for developing and validating a biomarker signature from high-dimensional data, such as gene expression profiles.
Detailed Experimental Workflow
Data Collection and Cohort Definition: Begin with a well-defined patient cohort treated uniformly with the immunotherapy of interest. Pre-treatment samples (e.g., tumor tissue for RNA sequencing) are collected. The cohort should be of sufficient size to allow for statistically powerful partitioning into training and validation sets [70].
Data Pre-processing: Normalize the raw data (e.g., gene expression counts) to remove technical artifacts. For multi-dataset integration, apply batch effect correction algorithms like the
Combatfunction from theSVApackage in R [73].Data Partitioning: Randomly split the cohort into a training set (typically ~70-80% of samples) and a validation set (the remaining ~20-30%). The training set is used for all model development, while the validation set is held back and used only once for final model assessment [70].
Feature Selection and Model Training (on Training Set):
- Apply feature selection methods (e.g., univariate selection, causal-based metrics, LASSO regression) to identify the most predictive biomarkers from thousands of candidates [75] [73].
- Train a classification model (e.g., logistic regression, random forest, support vector machine) using the selected features to predict the clinical endpoint (e.g., response to immunotherapy) [76] [75].
- Lock the Algorithm: Fully specify the computational algorithm, including all selected features and their weights. No further changes should be made before validation [70].
Internal Validation (on Training Set): Use cross-validation (e.g., 5-fold or Leave-One-Out Cross-Validation - LOOCV) on the training set to obtain an initial, unbiased estimate of model performance and to fine-tune hyperparameters [76] [75].
Blinded Prediction and ROC Analysis (on Validation Set): Apply the locked model to the held-out validation set to generate predictions. Construct an ROC curve by plotting the TPR against the FPR at various decision thresholds. Calculate the AUC to summarize performance [70] [71].
External Validation: The ultimate step for clinical validation is to test the model's performance on one or more completely independent cohorts from different institutions or studies. This is a regulatory requirement for approval [70].
Comparative Performance of Statistical Approaches
The choice of statistical and machine learning methods significantly impacts the performance of biomarker signatures. The table below summarizes a comparative analysis of different feature selection and classification methods evaluated on a gastric cancer dataset, where the number of biomarkers (K) was restricted.
Table 1: Performance Comparison of Feature Selection and ML Classifiers in Gastric Cancer Biomarker Discovery
| Feature Selection Method | Machine Learning Classifier | Number of Biomarkers (K) | Sensitivity (at Specificity=0.9) | Key Findings and Context |
|---|---|---|---|---|
| Causal-based Metric [75] | Various (GBT, RF, MLP) | 3 | 0.240 | Outperformed logistic regression (LR), which achieved 0.000 sensitivity. |
| Causal-based Metric [75] | Various (GBT, RF, MLP) | 10 | 0.520 | Outperformed logistic regression (LR), which achieved 0.040 sensitivity. |
| Univariate Feature Selection [75] | Various (GBT, RF, MLP) | 10 | 0.520 | Most performant when a greater number of biomarkers were permitted. |
| Logistic Regression (Benchmark) [75] | Logistic Regression | 3 | 0.000 | Served as a baseline for comparison with contemporary ML methods. |
| Logistic Regression (Benchmark) [75] | Logistic Regression | 10 | 0.040 | Performance was significantly lower than modern ML classifiers. |
| Immuno-oncology Gene Panel [76] | Logistic Regression | 32-gene signature | AUC: 0.83 | Outperformed traditional clinical biomarkers (AUC=0.8) in predicting immunotherapy response in GI cancers. |
Further comparative data comes from a systematic review of machine learning applied to gastrointestinal cancers. In one study, an immuno-oncology gene signature achieved an AUC of 0.83 for predicting immunotherapy response, outperforming traditional clinical biomarkers (AUC = 0.8) and principal component analysis of the whole dataset (AUC = 0.81) [76]. Another study validated published RNA signatures using logistic regression on an independent gastric cancer cohort (n=45), in some cases outperforming the originally reported results (AUC: reported/LR comparison - 0.74/0.831 and 0.67/0.735) [76].
To implement the statistical validation workflows described, researchers rely on a suite of software tools, databases, and experimental reagents.
Table 2: Key Resources for Biomarker Validation Research
| Resource Name | Type | Primary Function | Relevance to Validation |
|---|---|---|---|
| R Programming Language [73] | Software | Statistical computing and graphics. | Primary platform for data normalization, statistical analysis, model building, and generating ROC curves (using packages like pROC, ROCR, AROC). |
limma & sva R Packages [73] |
Software | Data normalization and batch effect correction. | Critical for pre-processing genomic data; limma normalizes arrays, sva removes batch effects from multi-dataset studies. |
glmnet R Package [73] |
Software | Regularized regression modeling. | Implements LASSO regression for feature selection while building predictive models. |
| STRING Database [73] | Online Database | Protein-Protein Interaction (PPI) network construction. | Used to explore functional interactions between candidate biomarker genes, adding biological context. |
| ROC Plotter [72] | Online Tool | Online transcriptome-level validation of predictive biomarkers. | Allows researchers to validate the association between gene expression and therapy response (e.g., immunotherapy) using public transcriptomic data. |
| Gene Expression Omnibus (GEO) [73] | Public Database | Repository of functional genomics datasets. | Source of independent validation cohorts for external validation of biomarker models. |
| CellAge Database [73] | Curated Gene Set | Database of genes associated with cellular senescence. | Example of a source for biologically relevant gene sets that can be used to inform feature selection. |
Navigating Challenges in Biomarker Development: Technical, Biological, and Standardization Hurdles
Addressing Tumor Heterogeneity and Dynamic Biomarker Expression
Cancer remains one of the most formidable challenges in modern medicine, with its complexity and heterogeneity representing significant obstacles to effective treatment, particularly in immunotherapy [77]. Tumor heterogeneity manifests at multiple levels – within individual tumors (intratumoral), between different lesions in the same patient (intertumoral), and temporally as cancers evolve under therapeutic pressure [77]. This biological diversity drives dynamic changes in biomarker expression, often resulting in acquired resistance to treatments that initially showed promise [77] [78].
The validation of biomarkers to predict response to immunotherapy requires navigating this intricate landscape. Emerging research highlights that traditional, static biomarker assessment is insufficient for capturing the evolving nature of the tumor ecosystem [77] [78]. The field is consequently shifting toward multidimensional models that integrate spatial and temporal biomarker monitoring to address these dynamics [77]. This guide compares current methodologies and technological approaches that enable researchers to better understand and overcome the challenges posed by tumor heterogeneity in immuno-oncology research.
Comparative Analysis of Methodological Approaches
The following table summarizes key methodological approaches for addressing tumor heterogeneity and dynamic biomarker expression in immunotherapy research.
Table 1: Comparison of Methodological Approaches for Addressing Tumor Heterogeneity
| Approach | Key Features | Applications in Immunotherapy | Limitations |
|---|---|---|---|
| Multi-region Sequencing | Profiles multiple regions of a single tumor; identifies subclonal architecture. | Maps heterogeneous distribution of predictive biomarkers (e.g., PD-L1, TMB). | Invasive; may miss micrometastases; does not capture temporal changes [77]. |
| Longitudinal Liquid Biopsy | Serial sampling of blood to analyze circulating tumor DNA (ctDNA); tracks evolution non-invasively [79]. | Monitors dynamic changes in resistance mutations and minimal residual disease (MRD) [80] [78]. | May not reflect heterogeneity in lesions with low shedding; requires high sensitivity assays [78]. |
| Single-Cell Multi-omics | Resolves cellular diversity by analyzing genomic, transcriptomic, and proteomic data at single-cell resolution [77]. | Identifies rare immune cell populations and their functional states within the tumor microenvironment (TME). | Technically complex; expensive; computational challenges in data integration [77]. |
| Spatial Transcriptomics/Proteomics | Preserves tissue architecture while quantifying gene or protein expression in situ [77]. | Characterizes the spatial context of immune cell infiltration and tertiary lymphoid structures (TLS) [81]. | Lower throughput than dissociative methods; resolution limits for single-cell analysis in dense tissues. |
| Digital Pathology with AI | Uses machine learning to extract quantitative features from whole-slide images (H&E/IHC) [77]. | Discovers and validates morphological biomarkers of immune response; predicts TLS presence and maturity [81]. | "Black box" models require careful validation; dependent on high-quality, annotated datasets [77]. |
Tracking Dynamic Biomarkers: Minimal Residual Disease (MRD) as a Paradigm
Minimal Residual Disease (MRD) monitoring exemplifies the critical importance of tracking dynamic biomarkers to predict clinical outcomes and guide treatment decisions. This approach is particularly advanced in hematological malignancies but holds growing promise for solid tumors.
Experimental Protocols for MRD Detection
The following table outlines the core methodologies for MRD detection, each with distinct advantages and implementation requirements.
Table 2: Core Methodologies for Minimal Residual Disease (MRD) Detection
| Methodology | Target | Sensitivity | Key Workflow Steps | Primary Clinical Application |
|---|---|---|---|---|
| Multiparameter Flow Cytometry (MFC) | Abnormal immunophenotypes on cell surface | 10-4 to 10-5 [78] | 1. Sample preparation (bone marrow/blood)2. Antibody staining with fluorescent panels3. Data acquisition on flow cytometer4. Analysis to identify aberrant cell populations | Rapid assessment of treatment response; risk stratification in ALL and AML [78]. |
| Next-Generation Sequencing (NGS) | Clonal immunoglobulin/T-cell receptor gene rearrangements or somatic mutations | Up to 10-6 [78] | 1. DNA extraction from sample2. PCR amplification and library preparation (targeted or whole-genome)3. High-throughput sequencing4. Bioinformatic analysis for variant allele frequency | Highly sensitive tracking of clonal evolution; used in Ph+ ALL and clinical trials like BOVen for MCL [80] [78]. |
| Quantitative PCR (qPCR) | Tumor-specific genetic aberrations (e.g., BCR::ABL1 fusion) [78] | 10-4 to 10-5 [78] | 1. RNA extraction and reverse transcription to cDNA2. Real-time PCR with fusion-specific probes3. Quantification against a standard curve | Monitoring disease burden in CML and Ph+ ALL; standardized international reporting [78]. |
| dPCR (Digital PCR) | Single nucleotide variants (SNVs), fusions | 10-5 and beyond | 1. Sample partitioning into thousands of nanoreactions2. End-point PCR amplification3. Absolute quantification by counting positive/negative partitions | Absolute quantification without standard curves; detecting very low-frequency mutations. |
The Workflow of MRD Monitoring in Ph+ ALL
The complex process of MRD monitoring in Ph-positive Acute Lymphoblastic Leukemia (Ph+ ALL) reveals the challenges of dynamic biomarkers and clonal evolution, which can be visualized in the following workflow.
Research demonstrates that in Ph+ ALL, a significant challenge arises from multilineage involvement, where the BCR::ABL1 fusion gene is found not only in lymphoblasts but also in myeloid cells and other hematopoietic lineages [78]. This biological phenomenon directly impacts MRD monitoring, as it can cause discordance between different detection methods—for instance, MRD negativity by flow cytometry or immunoglobulin gene sequencing may coincide with persistent BCR::ABL1 positivity by PCR [78]. Such discordance, observed in 27-43% of Ph+ ALL patients, complicates clinical decision-making regarding treatment intensity and the need for allogeneic stem cell transplantation [78]. This underscores the necessity of employing integrated, multimodal biomarker strategies rather than relying on a single assay.
Spatial Heterogeneity and the Tumor Microenvironment
The spatial organization of cells within the tumor ecosystem is a critical determinant of immunotherapy response. The presence and quality of tertiary lymphoid structures (TLS)—organized aggregates of immune cells that form in non-lymphoid tissues near tumors—have emerged as a powerful spatial biomarker [81].
Tertiary Lymphoid Structures: A Spatial Biomarker for Immunotherapy
TLS are inducible structures that facilitate the local activation and expansion of tumor-specific T and B cells. Their assessment requires methodologies that preserve spatial information.
Table 3: Classification and Assessment of Tertiary Lymphoid Structures (TLS)
| TLS Category | Defining Histological Features | Associated Immune Cells | Predictive Value for Immunotherapy |
|---|---|---|---|
| Early TLS (E-TLS) | Dense lymphocyte aggregates without clear organization; lack follicular dendritic cells (FDC) network and germinal centers (GC) [81]. | T cells, naive B cells, scattered CD4+ T cells [81]. | Limited immune activation; weaker correlation with positive outcome [81]. |
| Primary Follicle-like TLS (PFL-TLS) | Presence of immature FDCs, but no visible germinal center reaction; identified by CD21+ but CD23- staining [81]. | FDC networks, naive B cells, T cells. | Intermediate prognostic value. |
| Secondary Follicle-like TLS (SFL-TLS) - Mature TLS | Organized structures with distinct T cell and B cell zones; active germinal centers with CD21+ and CD23+ FDCs [81]. | FDCs, GC B cells, T follicular helper cells, antibody-producing plasma cells. | Strongly associated with improved survival and response to immune checkpoint inhibitors across multiple cancer types, including NSCLC [81]. |
Maturation and Function of Tertiary Lymphoid Structures
The development and immune function of TLS represent a coordinated process that can be effectively visualized. The following diagram illustrates the maturation stages of TLS and their functional impact on anti-tumor immunity.
Consensus findings indicate that the density and maturity of TLS are strongly associated with favorable prognosis and improved responses to immune checkpoint inhibitors in NSCLC and other solid tumors [81]. Specifically, the presence of mature TLS (SFL-TLS) correlates with prolonged survival and enhanced treatment efficacy, independent of PD-L1 expression status [81]. This positions TLS assessment as a crucial complementary spatial biomarker for refining patient stratification in immunotherapy.
The Scientist's Toolkit: Essential Research Reagent Solutions
Advancing research on tumor heterogeneity requires a sophisticated toolkit of reagents and technologies. The following table catalogs essential solutions for designing robust experiments in this field.
Table 4: Essential Research Reagent Solutions for Tumor Heterogeneity Studies
| Research Tool Category | Specific Examples & Targets | Key Function in Research | Application Context |
|---|---|---|---|
| Multiplex Immunofluorescence (mIF) Panels | CD3, CD8, CD20, CD21/CD23, PD-1, PD-L1, Pan-CK | Enables simultaneous visualization of multiple cell lineages and functional markers on a single tissue section, preserving spatial context. | Validation of TLS presence, maturity, and immune cell composition; analysis of spatial relationships between immune and tumor cells [81]. |
| Single-Cell RNA Sequencing Kits | 10x Genomics Chromium, BD Rhapsody | Facilitates high-throughput transcriptomic profiling of individual cells to deconvolute cellular heterogeneity and identify rare subpopulations. | Characterization of the tumor microenvironment (TME); tracking clonal evolution; identifying resistance mechanisms [77]. |
| Liquid Biopsy Assay Kits | ctDNA extraction kits; NGS panels for common driver mutations (e.g., EGFR, KRAS, TP53) | Allows for non-invasive, serial monitoring of tumor burden and genomic evolution via analysis of circulating tumor DNA (ctDNA). | Tracking dynamic biomarker changes (e.g., MRD); assessing tumor heterogeneity and emergence of resistance mutations during therapy [79] [78]. |
| Digital PCR Assays | Droplet Digital PCR (ddPCR) for BCR::ABL1, EGFR T790M | Provides absolute quantification of target sequences with ultra-high sensitivity, ideal for detecting low-frequency mutations in complex samples. | Validation of NGS findings; highly sensitive MRD monitoring; analysis of liquid biopsy samples [78]. |
| Flow Cytometry Panels for Immune Profiling | T cell exhaustion markers (PD-1, LAG-3, TIM-3); myeloid-derived suppressor cell (MDSC) markers | Enables high-dimensional immunophenotyping of dissociated tumor samples or peripheral blood to assess functional immune states. | Profiling the systemic and local immune response; correlating immune phenotypes with therapy outcomes. |
Addressing tumor heterogeneity and dynamic biomarker expression requires a fundamental shift from static, single-modal assessment to integrated, longitudinal monitoring. No single technology suffices to capture the full complexity of the evolving tumor ecosystem. The most promising path forward lies in combining spatial biomarkers like TLS, longitudinal liquid biopsy for MRD and clonal tracking, and high-resolution single-cell and spatial omics [77] [78] [81].
This multi-dimensional approach, powered by computational integration and artificial intelligence, is paving the way for more predictive biomarker models. Ultimately, overcoming heterogeneity is not about finding a single universal biomarker, but about building a dynamic, multi-faceted understanding of each patient's disease over time, enabling truly personalized immunotherapy strategies.
The successful application of biomarkers to predict response to immunotherapy hinges on the accuracy, reproducibility, and reliability of the assays used to measure them. A significant challenge in both translational research and clinical practice is inter-laboratory variability—the inconsistency of results when the same sample is analyzed across different laboratories, platforms, or assay kits. This variability can obscure true biological signals, impede the validation of predictive biomarkers, and ultimately hinder the development of personalized cancer treatments. This guide objectively compares various assay platforms and experimental approaches, providing a framework for researchers and drug development professionals to navigate and mitigate these critical standardization challenges.
The Standardization Challenge: Causes and Consequences
Inter-laboratory variability arises from multiple sources throughout the experimental workflow. Key contributors include:
- Assay Platform and Reagents: Different immunoassay formats (e.g., ELISA, CLIA, LFA) exhibit varying performance characteristics. Furthermore, even for the same biomarker, different commercial kits may use unique antibody clones, calibrants, and detection systems, leading to discrepant results [82].
- Sample Handling: Pre-analytical variables such as sample collection methods, storage conditions, and freeze-thaw cycles can significantly impact analyte stability and measured concentrations [83].
- Data Interpretation and Scoring: Subjectivity in interpreting results, particularly for assays like immunohistochemistry (IHC) for PD-L1, introduces another layer of variability. Differences in scoring algorithms (e.g., Tumor Proportion Score vs. Combined Positive Score) further complicate direct comparisons [21] [82].
The consequences are profound. For immunotherapy biomarkers, a lack of standardization can lead to the misclassification of patients, potentially excluding someone from a beneficial treatment or subjecting them to unnecessary toxicity. It also complicates multi-center clinical trials, as data from different sites may not be directly comparable, thereby weakening the evidence needed for regulatory approval of new biomarkers or drugs [83].
Comparative Performance of Assay Platforms
Objective comparison of platform performance is a foundational step in understanding and selecting methodologies. The following tables summarize experimental data from studies that directly compared different assay types.
Table 1: Comparative Diagnostic Performance of Serological Immunoassays for SARS-CoV-2 Antibody Detection
| Assay Platform | Specificity (%) | Overall Sensitivity (%) | Sensitivity >14 Days Post-Symptom Onset (%) | Key Characteristics |
|---|---|---|---|---|
| LFA (One Step) | 100.0 | 73.8 | 97.6 | Rapid, point-of-care; detects IgG/IgM against nucleocapsid and spike [84]. |
| LFA (Alltest) | 100.0 | 61.3 | ~85* | Rapid, point-of-care; detects IgG/IgM against nucleocapsid [84]. |
| ELISA (Dia.Pro) | 100.0 | 85.9 | >97 | Higher throughput than LFA; detects IgG/IgM against nucleocapsid and spike [84]. |
| CLIA (COV2T) | 100.0 | 92.0 | 100.0 | High sensitivity and precise quantification; detects total antibodies against spike [84]. |
| CLIA (Elecsys) | 100.0 | 88.0 | >97 | High sensitivity and precise quantification; detects total antibodies against nucleocapsid [84]. |
Note: *Value estimated from graphical data in source material [84].
Table 2: Inter-Assay Variability in Lipoprotein(a) [Lp(a)] Measurement Across Clinical Laboratories
| Assay | Correlation with Reference Method | Inter-Assay Coefficient of Variation (CV) Range | Factors Contributing to Variability |
|---|---|---|---|
| Multiple Clinical Lp(a) Assays | Good linear correlation | 3.3% to 69.1% | Not concentration-dependent; not correlated with Lp(a) isoform sizes [83]. |
The data in Table 1, while from infectious disease research, clearly illustrates a universal principle: platform choice directly impacts key performance metrics like sensitivity and specificity. CLIAs generally offer superior sensitivity and are amenable to high-throughput, automated quantification, whereas LFAs provide rapid results at the potential cost of lower overall sensitivity [84] [85]. Table 2 highlights that even for established clinical biomarkers, inter-assay variability can be extreme, underscoring the critical need for standardization initiatives, such as the use of common reference materials and harmonized methodologies [83].
Experimental Protocols for Assay Comparison and Validation
To robustly compare assay performance or validate a new test, researchers should employ structured experimental protocols. The following methodology outlines key steps.
Protocol for Cross-Platform Assay Comparison
1. Sample Selection and Panel Creation:
- Assemble a panel of well-characterized samples, including both positive and negative controls. For biomarker studies, this should encompass a range of clinically relevant concentrations [83].
- Include pre-pandemic or disease-negative samples to robustly assess specificity [84] [85].
- For longitudinal response monitoring, include serial samples from the same patient, if possible.
2. Parallel Testing and Data Collection:
- Test all samples in duplicate or triplicate across the platforms or kits being compared within a defined period to minimize drift [84] [83].
- Record raw data and calculated concentrations according to each platform's specific protocol.
- Ensure operators are blinded to results from other platforms to prevent bias.
3. Statistical Analysis and Agreement Assessment:
- Calculate standard performance metrics: sensitivity, specificity, positive percent agreement (PPA), and negative percent agreement (NPA) [85].
- Assess concordance using Cohen's kappa (κ) statistic: κ < 0.20 (slight agreement), 0.21–0.40 (fair), 0.41–0.60 (moderate), 0.61–0.80 (substantial), 0.81–1.00 (almost perfect) [84] [85].
- For quantitative assays, use linear regression and Bland-Altman plots to evaluate correlation and systematic biases between methods.
Visualization of Standardization Strategies
The following diagram illustrates a strategic pathway to overcome inter-laboratory variability, from recognizing the problem to implementing validated solutions.
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting appropriate reagents and materials is critical for robust and reproducible assay development. The table below details essential components for immunoassay-based biomarker studies.
Table 3: Essential Research Reagents for Immunoassay Development and Standardization
| Research Reagent | Critical Function | Considerations for Standardization |
|---|---|---|
| Validated Antibodies | Specific recognition and detection of the target biomarker. | Antibody clone specificity can vary; validate for each application and sample type (e.g., FFPE, serum) [82]. |
| Universal Reference Materials | Calibrate assays to a common standard, enabling cross-platform data comparison. | Using a common calibrant (e.g., USP AAV9 Reference Material) can reduce inter-kit variability [86]. |
| Control Panels | Monitor assay performance, precision, and drift over time. | Should include positive, negative, and borderline controls covering the assay's dynamic range [83]. |
| Calibrators and Standards | Generate a standard curve for quantitative analysis. | Traceability to an international reference standard improves consistency across labs [83] [86]. |
Overcoming inter-laboratory variability is not a one-time task but a continuous process integral to biomarker validation. The path forward requires a concerted effort from the research community:
- Embrace Reference Materials: Widespread adoption of universal, commutable reference standards is paramount for aligning results across different commercial kits and platforms [83] [86].
- Adhere to Guidelines: Following evidence-based guidelines, such as those from the College of American Pathologists for PD-L1 testing, ensures analytical validity and clinical utility [82].
- Leverage Advanced Technologies: Incorporating digital pathology and artificial intelligence for automated scoring of IHC or tissue-based biomarkers can significantly reduce subjective interpretation bias [13] [21] [87].
- Promote Data Sharing: Participating in interlaboratory comparison studies and sharing standardized performance data accelerates the identification and resolution of variability sources [83] [86].
By systematically comparing assay platforms, implementing rigorous validation protocols, and adopting harmonized tools and practices, researchers and drug developers can enhance the reliability of predictive biomarkers, thereby unlocking the full potential of precision immunotherapy.
The remarkable heterogeneity of patient responses to immunotherapy has created an urgent need for robust predictive biomarkers to guide treatment decisions. While conventional single-parameter biomarkers like PD-L1 expression or tumor mutational burden (TMB) have demonstrated utility, their predictive value remains limited, highlighting the complex, multi-factorial nature of treatment response and resistance [88] [89]. Multi-omic integration represents a transformative approach that simultaneously analyzes genomic, proteomic, and immunological data to capture the intricate biological networks underlying immunotherapy efficacy and toxicity.
This integrated paradigm addresses fundamental biological complexity by examining the flow of information from DNA-level alterations to functional protein expression and immune system interactions. The clinical imperative is clear: only 37% of tumors harbor actionable alterations when assessed by genomic methods alone, as demonstrated by the MSK-IMPACT study [58]. In contrast, multi-omics strategies can reveal functional subtypes and druggable vulnerabilities missed by single-omics approaches, as shown by Clinical Proteomic Tumor Analysis Consortium (CPTAC) studies of ovarian and breast cancers [58]. For researchers and drug development professionals, understanding available integration methodologies, their performance characteristics, and implementation requirements is crucial for advancing biomarker discovery and validation.
Multi-Omic Technologies and Data Types for Immunobiology
Core Omics Technologies
Multi-omic integration in immunotherapy research leverages complementary technologies that probe different layers of biological regulation:
Genomics investigates DNA-level alterations using whole exome sequencing (WES) and whole genome sequencing (WGS) to identify somatic mutations, copy number variations (CNVs), and single nucleotide polymorphisms (SNPs). In immunotherapy contexts, genomics enables assessment of tumor mutational burden (TMB) and neoantigen prediction, with TMB validated as a predictive biomarker for pembrolizumab treatment across solid tumors in the KEYNOTE-158 trial [58]. Recent advances also reveal the importance of non-SNV sources of neoantigens, including frameshift mutations and gene fusions, which can produce more immunogenic neoantigens due to greater sequence divergence from wild-type peptides [89].
Transcriptomics explores RNA expression patterns through microarray or RNA sequencing technologies, encompassing mRNA, long noncoding RNAs (lncRNAs), and miRNAs. Gene-expression signatures such as Oncotype DX (21-gene) and MammaPrint (70-gene) have demonstrated clinical utility in tailoring adjuvant chemotherapy decisions in breast cancer [58]. In immunotherapy, transcriptomics identifies T-cell exhaustion signatures predictive of CAR-T failure and enables deconvolution of immune cell infiltration patterns within the tumor microenvironment [89].
Proteomics investigates protein abundance, post-translational modifications, and interactions using high-throughput methods including liquid chromatography-mass spectrometry (LC-MS) and reverse-phase protein arrays. As proteins represent functional effectors in biological systems, proteomic data can reveal druggable vulnerabilities missed by genomics alone. For example, CPTAC studies showed that proteomics identifies functional subtypes in ovarian and breast cancers, directly informing discovery of protein-based biomarkers for predicting therapeutic responses [58].
Emerging Technologies including single-cell multi-omics and spatial multi-omics technologies are expanding the scope of biomarker discovery by enabling unprecedented resolution in characterizing cellular states, activities, and spatial relationships within the tumor microenvironment [58]. These technologies provide critical insights into tumor heterogeneity and tumor-immune interactions essential for personalized therapeutic strategies in cancer.
Immunological Data Types
Specialized immunological profiling techniques capture critical dimensions of anti-tumor immunity:
T-cell receptor (TCR) sequencing profiles the repertoire of antigen-recognizing receptors, with studies integrating HLA and TCR sequencing to predict immune checkpoint inhibitor response in melanoma using multiple-instance learning models [88].
Immune cell phenotyping via flow cytometry or single-cell RNA sequencing characterizes immune cell populations and their activation states, identifying correlates of response such as CD4+ memory T-cell expansion in classical Hodgkin lymphoma responders [89].
Cytokine profiling quantifies soluble immune mediators, with elevations in IL-6 and IFN-γ at 24 hours post-CAR-T infusion forecasting severe cytokine release syndrome (CRS) [89].
Histocytometry combines microscopy with multiplexed antibody staining to visualize immune cell spatial distributions within tissue sections, providing critical context for understanding immune-tumor interactions.
Computational Integration Methods: Strategies and Performance Comparison
Integration Approaches and Methodologies
Multi-omics data integration strategies fall into three primary methodological categories, each with distinct strengths and applications in immunotherapy research:
Statistical and Correlation-based Methods: These approaches identify relationships between omics layers using correlation metrics (Pearson's, Spearman's), network analysis, and regression techniques. Weighted Gene Correlation Network Analysis (WGCNA) identifies clusters of co-expressed, highly correlated genes (modules) whose expression patterns can be linked to clinically relevant traits [90]. The xMWAS platform performs pairwise association analysis combining Partial Least Squares (PLS) components and regression coefficients to generate integrative network graphs [90]. These methods are particularly valuable for hypothesis generation and identifying coordinated multi-omics patterns associated with immunotherapy response.
Multivariate and Dimension Reduction Methods: These techniques project high-dimensional omics data into lower-dimensional spaces to facilitate integration and visualization. Methods include Multi-Omics Factor Analysis (MOFA), Joint Non-negative Matrix Factorization (MultiNMF), and iCluster variants [91] [88]. These approaches effectively capture shared variation across omics layers and have demonstrated utility in identifying molecular subtypes with distinct immunotherapy responses. For example, joint NMF has been employed to decompose gene expression matrices and identify pivotal genes correlated with immunotherapy response [88].
Machine Learning/Artificial Intelligence Methods: ML/AI approaches capture complex, non-linear relationships within and between omics layers. Similarity Network Fusion (SNF) constructs and fuses patient similarity networks from each omics layer [91]. Deep learning models including convolutional neural networks (CNNs) and multiple-instance learning frameworks integrate radiology, pathology, and multi-omics data to predict immunotherapy response [88]. These methods have shown particular promise in handling the heterogeneity and high dimensionality of multi-omics data, with dynamic deep attention-based models demonstrating higher accuracy than unimodal approaches in predicting response of NSCLC patients to anti-PD-1/PD-L1 blockade [88].
Comparative Performance of Integration Methods
Evaluating integration methods for cancer subtyping reveals important performance characteristics with direct implications for immunotherapy biomarker discovery:
Table 1: Performance Comparison of Multi-Omics Integration Methods for Cancer Subtyping
| Method Category | Representative Algorithms | Accuracy (C-index/ARI) | Robustness | Computational Efficiency | Key Applications in Immunotherapy |
|---|---|---|---|---|---|
| Network-Based | SNF [91], NEMO [91], CIMLR [91] | Moderate to High (0.65-0.82) | Moderate | Moderate | Patient similarity network fusion, identification of immune subtypes |
| Statistics-Based | iClusterBayes [91], LRAcluster [91], moCluster [91] | Variable (0.58-0.79) | Moderate to High | Low to Moderate | Molecular subtyping, dimension reduction for biomarker discovery |
| Machine Learning | Subtype-GAN [91], RMTLR [88], LASSO [88] | High (0.75-0.89) | Variable | Variable | Response prediction, feature selection, non-linear pattern recognition |
| Deep Learning | CNN [88], Multiple-instance learning [88] | Highest in multimodal setups | High with sufficient data | Low (requires GPU) | Radiomics integration, TCR sequence analysis, predictive modeling |
Key insights from comparative analyses reveal that:
No single method outperforms others across all cancer types or clinical questions, emphasizing the importance of method selection based on specific research objectives [91].
Integrating more omics data does not always improve performance; in some cases, adding data types with high technical noise or low biological relevance can negatively impact results [91].
Network-based methods generally demonstrate robust performance across multiple cancer types, while statistics-based approaches show more variable performance depending on data characteristics [91].
Machine learning methods excel in predictive accuracy but require careful feature selection and validation to ensure generalizability [88].
Experimental Protocols for Multi-Omic Biomarker Validation
Protocol 1: Multi-Omic Immunotherapy Response Prediction
This protocol outlines a comprehensive approach for developing predictive biomarkers of immunotherapy response integrating genomic, transcriptomic, and proteomic data:
Cohort Selection and Sample Collection: Recruit patients scheduled to receive immunotherapy (e.g., anti-PD-1/PD-L1 inhibitors). Collect matched tumor tissue (fresh frozen or FFPE), blood samples (for plasma proteomics and germline DNA), and clinical annotations at baseline.
Multi-Omic Data Generation:
- DNA Extraction and Sequencing: Perform whole exome sequencing (WES) on tumor and germline DNA to identify somatic mutations, calculate TMB, and predict neoantigens using pipelines like INTEGRATE-neo and NetMHCpan [89].
- RNA Extraction and Sequencing: Conduct total RNA sequencing to quantify gene expression, immune cell deconvolution using CIBERSORT or xCell, and identify transcriptomic signatures of T-cell exhaustion (LAG3, TIM3, TOX) [89].
- Protein Extraction and Quantification: Implement liquid chromatography-mass spectrometry (LC-MS) or Olink proximity extension assays to quantify protein abundance and cytokine levels, focusing on immune checkpoint proteins and serum biomarkers (e.g., IL-6, IFN-γ, ANG2) [58] [89].
Data Preprocessing and Quality Control:
- Process sequencing data through standardized pipelines (e.g., GATK for WES, STAR for RNA-seq) with quality metrics (coverage depth, mapping quality).
- Normalize proteomics data using variance-stabilizing transformation and correct for batch effects using ComBat or similar methods.
- Annotate datasets with clinical variables (tumor stage, prior treatments, irAE history).
Multi-Omic Data Integration and Modeling:
- Apply feature selection methods (LASSO, random forest) to identify predictive variables from each omics layer.
- Implement integration algorithms (SNF, MOFA, or deep learning models) to combine selected features from all omics platforms.
- Train predictive models using machine learning algorithms (random forest, XGBoost, or neural networks) with cross-validation to predict binary response (responder vs. non-responder) or continuous outcomes (progression-free survival).
Model Validation and Clinical Translation:
- Validate models in independent cohorts using the same laboratory and computational workflows.
- Assess clinical utility by calculating sensitivity, specificity, and area under the receiver operating characteristic curve (AUC).
- Develop simplified clinical assays targeting the most informative biomarkers for practical implementation.
Protocol 2: Tumor Microenvironment Characterization Using Single-Cell Multi-Omics
This protocol describes an approach for comprehensive tumor microenvironment characterization to identify mechanisms of immunotherapy resistance:
Sample Processing and Single-Cell Isolation: Process fresh tumor tissues using mechanical dissociation and enzymatic digestion to create single-cell suspensions. Isolate live immune cells and tumor cells using fluorescence-activated cell sorting (FACS) or magnetic bead separation.
Single-Cell Multi-Omic Profiling:
- Perform single-cell RNA sequencing (10X Genomics platform) to profile transcriptomes of individual immune and tumor cells.
- Implement CITE-seq (Cellular Indexing of Transcriptomes and Epitopes by Sequencing) to simultaneously measure surface protein expression alongside transcriptomes.
- Conduct TCR sequencing from the same single cells to link clonality with functional states.
Data Integration and Analysis:
- Process scRNA-seq data using Seurat or Scanpy pipelines, including quality control, normalization, and batch correction.
- Cluster cells based on integrated transcriptome and protein expression to identify distinct immune and tumor subpopulations.
- Reconstruct TCR clonotypes and track expanded clones across cell states.
- Infer cell-cell communication networks using tools like CellPhoneDB or NicheNet.
Spatial Validation:
- Validate single-cell findings using spatial transcriptomics (Visium) or multiplexed immunofluorescence (CODEX) on tissue sections.
- Correlate spatial distributions of identified cell states with clinical response metrics.
The following workflow diagram illustrates the key steps in multi-omic data integration for immunotherapy biomarker discovery:
Figure 1: Workflow for Multi-Omic Data Integration in Immunotherapy Biomarker Discovery
Successful implementation of multi-omic integration strategies requires specialized wet-lab and computational resources:
Table 2: Essential Research Reagent Solutions for Multi-Omic Integration Studies
| Category | Specific Tools/Reagents | Function | Key Considerations |
|---|---|---|---|
| Sequencing Technologies | Illumina NovaSeq (WES, RNA-seq), 10X Genomics (single-cell), Nanopore (long-read) | Comprehensive genomic and transcriptomic profiling | Coverage requirements (≥100x for WES), sample quality inputs, single-cell viability |
| Proteomics Platforms | Liquid chromatography-mass spectrometry (LC-MS), Olink proximity extension assay, reverse-phase protein arrays | Protein quantification and post-translational modification detection | Sample preparation consistency, normalization methods, dynamic range limitations |
| Immunological Assays | Multiplexed flow cytometry, Olink Immune Response panel, TCRβ sequencing kit | Immune cell phenotyping and receptor repertoire analysis | Panel design optimization, sample freshness requirements, controls for activation states |
| Spatial Biology Tools | Visium spatial gene expression, CODEX multiplexed immunofluorescence, NanoString GeoMx | Tissue context preservation for molecular data | Region of interest selection criteria, antibody validation, integration with bulk data |
| Computational Resources | R/Bioconductor packages (MOVICS, mixOmics), Python (Scanpy, Scikit-learn), cloud computing platforms | Data integration, analysis, and visualization | Computational expertise requirements, scalability to large datasets, reproducibility frameworks |
| Data Repositories | The Cancer Genome Atlas (TCGA), Clinical Proteomic Tumor Analysis Consortium (CPTAC), Cancer Cell Line Encyclopedia (CCLE) | Access to reference datasets for method validation and comparison | Data harmonization challenges, consent restrictions, clinical annotation completeness |
Applications and Validation in Immunotherapy Research
Successful Applications in Cancer Immunotherapy
Multi-omic integration has generated significant advances in predicting and understanding immunotherapy outcomes:
Response Prediction in Solid Tumors: A dynamic deep attention-based multiple-instance learning model integrating radiology, pathology, and multi-omics data demonstrated higher accuracy than unimodal approaches in predicting response of NSCLC patients to anti-PD-1/PD-L1 blockade [88]. Similarly, integration of RNA-seq data with somatic mutations, copy number alterations, and protein expression alterations identified distinct subcohorts within the tumor microenvironment with unique responses to immunotherapy [88].
CAR-T Cell Therapy Optimization: In DLBCL patients receiving CD19-CAR-T, pre-infusion upregulation of exhaustion genes (LAG3, TIM3, TOX) in manufactured products associates with poor persistence and disease progression [89]. Single-cell RNA sequencing reveals that sustained responders demonstrate stem-like memory T-cells (TCF7+, LEF1+), providing insights for improving CAR-T product composition [89].
Toxicity Prediction: Cytokine profiling identifies IL-6 and IFN-γ elevations at 24 hours post-CAR-T infusion as predictors of severe cytokine release syndrome (CRS), while ANG2 and sFLT1 associate with neurotoxicity [89]. Germline variants in complement pathway genes (CFH, CFI) increase neurotoxicity risk after CD19-CAR-T therapy, enabling preemptive interventions [89].
Colorectal Cancer Subtyping: Integration of transcriptomics, epigenomics, genomics, and gut microbiome profiles identified two major CRC subtypes (CS1 and CS2) with distinct molecular characteristics and survival outcomes using the MOVICS package [92]. The developed Multi-Omics Integrative Clustering and Machine Learning Score (MCMLS) model demonstrated strong prognostic value and consistently predicted immunotherapy response across six independent datasets [92].
Validation Frameworks and Clinical Translation
Robust validation of multi-omics biomarkers requires rigorous analytical and clinical frameworks:
Analytical Validation: Establish assay precision, accuracy, sensitivity, specificity, and reproducibility following guidelines such as the FDA's Bioanalytical Method Validation. For computational methods, implement cross-validation, bootstrap resampling, and independent cohort testing.
Clinical Validation: Demonstrate association between biomarker signatures and clinically relevant endpoints (overall survival, progression-free survival, objective response rate) in prospective cohorts. Control for confounding factors including cancer type, line of therapy, and performance status.
Regulatory Considerations: For biomarkers intended as companion diagnostics, engage early with regulatory agencies regarding evidentiary standards. Consider novel clinical trial designs (basket trials with omics stratification) to accelerate biomarker validation [89].
Multi-omic integration represents a paradigm shift in immunotherapy biomarker development, moving beyond reductionist single-parameter approaches to capture the complex biological networks underlying treatment response and resistance. The synergistic combination of genomic, proteomic, and immunological data has demonstrated superior predictive performance across multiple cancer types and immunotherapy modalities.
Despite these promising advances, significant challenges remain in standardization, data harmonization, and clinical implementation. Future developments will likely focus on single-cell multi-omics technologies that resolve cellular heterogeneity, longitudinal sampling strategies that capture dynamic biomarker changes during therapy, and AI-driven integration approaches that extract maximal biological insights from complex datasets. Additionally, the emergence of digital twin concepts for in silico clinical trials and CRISPR-based epitope editing further refine precision immunotherapy strategies [89].
For researchers and drug development professionals, successful implementation requires careful selection of integration methodologies matched to specific biological questions, rigorous validation across independent cohorts, and development of clinically practical assays that preserve the predictive power of multi-omic signatures. As these technologies mature and computational methods advance, multi-omic integration promises to transform immunotherapy from empirical medicine to truly personalized precision oncology, ultimately improving outcomes for cancer patients.
Liquid Biopsies and Circulating Biomarkers for Non-Invasive Monitoring
The validation of biomarkers to predict response to immunotherapy represents a critical frontier in oncology research. While tissue biopsy remains the gold standard for initial tumor diagnosis, its invasive nature and inability to capture spatial and temporal tumor heterogeneity limit its utility for serial monitoring of dynamic immunotherapy responses [93] [94]. Liquid biopsy has emerged as a powerful complementary approach that enables non-invasive tracking of circulating biomarkers released by tumors into bodily fluids, primarily blood [95].
This paradigm shift is particularly relevant for immune checkpoint blockade (ICB) therapies, where only a subset of patients experiences durable clinical benefits, and the need for predictive biomarkers is paramount [94] [21]. Liquid biopsy provides a comprehensive view of the entire tumor burden through repeated sampling, allowing researchers and clinicians to monitor evolving molecular landscapes during treatment and identify biomarkers associated with response, resistance, and immune-related adverse events [96].
This guide objectively compares the performance characteristics of major liquid biopsy biomarkers and their detection technologies within the context of immunotherapy biomarker validation, providing experimental data and methodologies relevant to researchers, scientists, and drug development professionals.
Comparative Analysis of Circulating Biomarkers
Liquid biopsy encompasses multiple analyte classes, each with distinct biological origins, technical considerations, and clinical applications. The table below summarizes the key performance characteristics of major circulating biomarkers in the context of immunotherapy monitoring.
Table 1: Performance Comparison of Major Liquid Biopsy Biomarkers for Immunotherapy Monitoring
| Biomarker | Biological Origin | Detection Technologies | Key Advantages | Primary Limitations | Representative Clinical Applications in Immunotherapy |
|---|---|---|---|---|---|
| ctDNA(Circulating Tumor DNA) | Apoptotic/Necrotic tumor cells [93] | ddPCR, NGS (CAPP-Seq, TAm-Seq), BEAMing [96] | Short half-life (16min-2.5h) enables real-time monitoring; Captures tumor heterogeneity; Can assess tumor mutation burden (bTMB) [97] [94] | Low concentration in early-stage disease; Can be confounded by clonal hematopoiesis [96] | Early response assessment; Monitoring resistance mutations; Predicting hyperprogression [94] [96] |
| CTCs(Circulating Tumor Cells) | Cells shed from primary/metastatic tumors [93] | CellSearch (FDA-approved), Immunomagnetic separation, Microfluidic devices [93] [96] | Enables functional studies & culture; Provides intact cellular material for DNA, RNA, and protein analysis; Role in metastasis [93] [96] | Very rare in blood (1 CTC per 10^6 leukocytes); Short half-life (1-2.5h); Technical challenges in isolation [93] | Prognostic assessment; Monitoring PD-L1 expression dynamics on tumor cells [94] |
| Exosomes & EVs(Extracellular Vesicles) | Secreted by cells through endosomal pathway [94] | Ultracentrifugation, Nanomembrane ultrafiltration, Precipitation [95] | Stable in circulation; Contain proteins, nucleic acids; Reflect parent cell composition; Cross blood-brain barrier [95] [94] | Standardization challenges in isolation; Heterogeneous population | Analyzing tumor-derived proteins (e.g., PD-L1) and nucleic acids [94] |
| Soluble Immune Proteins | Secreted by immune and tumor cells [94] | ELISA, Ella automated microfluidic platform [98] | Simple detection; Measure immune activation status; Inexpensive analysis | Limited specificity for tumor immune context | Predicting response to anti-PD-1 therapy (e.g., IFN-γ, CTLA-4) [98] |
Experimental Protocols for Biomarker Analysis
ctDNA Analysis for Immunotherapy Monitoring
Objective: To quantify and characterize ctDNA for early response assessment in patients receiving immune checkpoint inhibitors.
Methodology:
- Sample Collection: Collect peripheral blood (typically 10-20mL) in cell-free DNA collection tubes [98].
- Plasma Separation: Centrifuge at 1600-2000 × g for 10-20 minutes to separate plasma from cellular components.
- cfDNA Extraction: Isolate cell-free DNA using commercial kits (e.g., MagMAX Cell-Free DNA Isolation Kit) [98].
- Quantification: Measure DNA concentration using fluorometric methods (e.g., Qubit dsDNA HS Assay Kit) [98].
- Mutation Analysis:
- Data Interpretation: Monitor variant allele frequency changes over time; decreasing levels indicate response, while increasing levels suggest progression [94] [96].
Key Experimental Consideration: The half-life of ctDNA is short (16 minutes to 2.5 hours), making it ideal for real-time monitoring but requiring rapid sample processing [97].
CTC Isolation and Phenotypic Characterization
Objective: To isolate and quantify CTCs and assess PD-L1 expression dynamics during immunotherapy.
Methodology:
- Sample Collection: Draw blood in specialized preservative tubes (e.g., CellSave tubes for CellSearch system).
- CTC Enrichment:
- Detection & Enumeration: Immunofluorescence staining for epithelial (CK8,18,19), leukocyte (CD45), and nuclear (DAPI) markers [93].
- PD-L1 Staining: Additional immunofluorescence for PD-L1 to assess expression levels on CTCs [94].
- Analysis: Count CTCs and calculate PD-L1 positivity percentage; correlate with clinical outcomes.
Key Experimental Consideration: CTCs are extremely rare, and their fragility requires gentle processing to maintain cell viability for functional studies [93].
Soluble Immune Factor Profiling
Objective: To quantify soluble immune checkpoint proteins and cytokines as biomarkers of immune activation.
Methodology:
- Sample Collection: Collect serum or plasma samples at baseline and serial timepoints during therapy.
- Multiplex Immunoassay: Use automated microfluidic platforms (e.g., Ella, Bio-Techne) with custom cartridges [98].
- Protein Detection: Simultaneously quantify multiple analytes (e.g., PD-L1, LAG-3, TIM-3, CTLA-4, IFN-γ).
- Data Analysis: Normalize concentrations to standard curves; establish cutoff values for response prediction.
Key Experimental Consideration: Sample timing relative to treatment cycles is critical for interpreting soluble biomarker levels [98].
Biomarker Performance Data in Immunotherapy Context
The table below summarizes quantitative performance characteristics of key biomarkers based on recent clinical studies.
Table 2: Experimental Performance Data of Liquid Biopsy Biomarkers in Immunotherapy Studies
| Biomarker | Cancer Type | Detection Technology | Key Performance Metrics | Clinical Correlation |
|---|---|---|---|---|
| ctDNA(Dynamic monitoring) | NSCLC [96] | CAPP-Seq | Early ctDNA reduction predicted radiographic response with 93% accuracy [96] | ctDNA changes preceded radiographic changes by 8.7 weeks (median) |
| ctDNA(bTMB) | NSCLC [21] | NGS panels | High bTMB correlated with improved PFS (HR: 0.39) on ICB [21] | Potential alternative to tissue TMB for patient selection |
| IFN-γ(Soluble protein) | Cutaneous SCC [98] | Ella automated immunoassay | High baseline IFN-γ associated with shorter PFS (p=0.038) [98] | Post-treatment decrease associated with improved response |
| CTCs(PD-L1+ enumeration) | NSCLC [94] | CellSearch/IF | PD-L1+ CTCs detected in 75% of patients pre-treatment [94] | Dynamic changes in PD-L1+ CTCs correlated with treatment response |
| Exosomal PD-L1 | Melanum [94] | Ultracentrifugation/ELISA | Higher levels correlated with immune suppression | Potential mechanism of resistance to ICB |
Workflow Visualization
Liquid Biopsy Workflow for Immunotherapy Monitoring This diagram illustrates the comprehensive workflow from sample collection to clinical application, highlighting the multiple biomarker streams that can be analyzed in parallel for a holistic view of treatment response.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Liquid Biopsy in Immunotherapy Studies
| Reagent/Category | Specific Examples | Primary Function | Considerations for Immunotherapy Applications |
|---|---|---|---|
| Blood Collection Tubes | Cell-free DNA BCT tubes, CellSave tubes | Preserve sample integrity during transport | Different preservatives optimized for ctDNA vs. CTC analysis |
| Nucleic Acid Extraction Kits | MagMAX Cell-Free DNA Isolation Kit, QIAamp Circulating Nucleic Acid Kit | Isolate high-quality ctDNA/cfDNA | Extraction efficiency for short DNA fragments is critical |
| CTC Enrichment Systems | CellSearch CTC Test, Parsortix system, CTC-iChip | Islect and enumerate rare CTCs | Platform choice affects capacity for downstream molecular analysis |
| Immunoassay Platforms | Ella automated immunoassay, MSD multiplex assays | Quantify soluble immune proteins | Multiplex capacity enables comprehensive immune profiling |
| PCR Reagents | ddPCR supermix, QIAseq targeted panels | Detect rare mutations in ctDNA | Sensitivity requirements depend on tumor fraction |
| NGS Library Prep | AVENIO ctDNA kits, QIAseq Targeted DNA Panels | Prepare libraries for mutation profiling | Panels should include immunologically relevant genes |
| Exosome Isolation Kits | ExoQuick, Total Exosome Isolation Kit | Enrich extracellular vesicles | Method affects exosomal RNA/protein yield and purity |
| Cell Culture Reagents | CTC culture media, FBS, supplements | Expand CTCs for functional studies | Enables drug testing and mechanism validation |
Liquid biopsy technologies provide researchers and drug development professionals with a powerful toolkit for validating biomarkers that predict response to immunotherapy. Each biomarker class—ctDNA, CTCs, exosomes, and soluble proteins—offers complementary insights into the dynamic interplay between tumors and the immune system under therapeutic pressure.
The experimental protocols and performance data presented in this guide demonstrate that integrated approaches, leveraging multiple analyte types and detection technologies, offer the most comprehensive strategy for biomarker validation. As the field advances, standardization of methodologies and analytical frameworks will be essential for translating these circulating biomarkers into clinically validated tools that can optimize immunotherapy outcomes through personalized treatment strategies.
Ongoing clinical trials (20 currently recruiting in the U.S. as of 2025) continue to explore the utility of liquid biopsy in immunotherapy contexts, promising to further refine our understanding of how these minimally invasive tools can guide therapeutic decision-making [95] [99].
Collaborative Frameworks and Data-Sharing Initiatives for Biomarker Advancement
The validation of biomarkers to predict response to immunotherapy represents one of the most critical challenges in modern oncology. Despite the revolutionary impact of immune checkpoint inhibitors (ICIs) across multiple malignancies, only 20-30% of patients experience sustained benefit, creating an urgent need for reliable predictive biomarkers [87]. The development and validation of these biomarkers face substantial hurdles, including biological complexity, technical variability, and insufficient sample sizes from individual studies. Collaborative frameworks and data-sharing initiatives have emerged as essential enablers to overcome these limitations by pooling resources, standardizing methodologies, and accelerating the qualification of biomarkers as regulatory-grade tools. This review compares major ongoing initiatives, their operational frameworks, and their collective impact on advancing biomarker science for immunotherapy.
Comparative Analysis of Major Initiatives
Table 1: Overview of Major Biomarker Data-Sharing Initiatives
| Initiative Name | Primary Focus | Key Features | Data Sharing Model | Governance Framework |
|---|---|---|---|---|
| European Platform for Neurodegenerative Diseases (EPND) | Neurodegenerative diseases (Alzheimer's, Parkinson's) | Federated platform connecting existing cohorts; sample and data discovery [100] | Three-tiered: Federated, Distributed, Centralized [100] | Co-created guidance with patient input; GDPR compliance [100] |
| Biomarker Data Repository (BmDR) | Kidney safety biomarkers; potential expansion to other areas [101] | Focus on biomarker qualification as drug development tools; diverse stakeholder committees [101] | Centralized repository of de-identified data [101] | Multi-stakeholder committees (Community Engagement, Legal, Technical) [101] |
| Alzheimer's Disease Data Initiative (ADDI) / AD Workbench | Alzheimer's disease research | Global network of data scientists and datasets; connected to EPND [100] | Cloud-based research environment [100] | Not specified in available sources |
Table 2: Technical Implementation Comparison
| Initiative | Discovery Capabilities | Analysis Environment | Sample Access | Patient Engagement |
|---|---|---|---|---|
| EPND | Connection to existing catalogs (e.g., EMIF-AD: 48 cohorts, 85,000+ patients) via MONTRA; sample catalogs via MOLGENIS/ELIXIR [100] | Secure, cloud-based workspaces; support for federated analysis when direct data access not permitted [100] | Sample catalog discovery; request management integrated with data access [100] | Patient and caregiver input in guidance development; focus on trust and awareness [100] |
| BmDR | Not specifically described | Data available to FDA and stakeholders for research on biological understanding of biomarkers [101] | Not the primary focus | Dedicated Community Engagement Committee with patient representatives; focus on lay language communication [101] |
| ADDI/AD Workbench | Connected to EPND discovery tools | Provides critical infrastructure for EPND platform [100] | Not specified | Not specified |
Experimental Data and Validation Outcomes
Validation Approaches and Outcomes
Table 3: Biomarker Validation Outcomes from Collaborative Efforts
| Biomarker Category | Validation Approach | Key Findings | Limitations Identified |
|---|---|---|---|
| Immunotherapy Response Biomarkers | External validation of 59 reported irAE risk biomarkers in 110 melanoma patients [102] | Poor discriminatory value for most biomarkers; only 4 T-cell subsets showed modest capacity for colitis prediction [103] | Pre-therapy flow cytometry and clinical data insufficient for reliable irAE prediction in most cases [103] |
| Digital Biomarkers | Continuous monitoring via wearables, smartphones in clinical trials [104] | Enabled high-resolution, longitudinal data collection; detection of subtle neurological changes in real time [104] | Data quality variability across devices; algorithmic bias; privacy concerns [104] |
| Multi-omics Integration | Machine learning models integrating genomic, transcriptomic, proteomic data [1] | ~15% improvement in predictive accuracy for immunotherapy response [1] | Requires large, diverse datasets; computational complexity; standardization challenges [1] |
Detailed Experimental Protocols
Protocol 1: External Validation of Predictive Biomarkers for Immune-Related Adverse Events
This protocol derives from the study by Glehr et al. (2022) that externally validated 59 previously reported biomarkers for irAE risk [103].
- Patient Cohort: 110 patients with Stage III/IV melanoma receiving combined Nivolumab (anti-PD-1) and Ipilimumab (anti-CTLA-4) therapy [103]
- Sample Collection: Peripheral blood collected in EDTA-vacutainers before treatment initiation; processed within 4 hours at 4°C [103]
- Flow Cytometry Analysis: Staining with DURAClone reagent panels (T Cell Subsets, TCRs, Treg, B Cell, Dendritic Cell, Granulocytes); data acquisition on Navios flow cytometer using Kaluza software v2.1 [103]
- Clinical Parameter Assessment: Routine hematological, biochemical parameters; irAE grading by dermatological oncologist based on standardized criteria (hepatitis, colitis, thyroiditis) [103]
- Statistical Validation: Univariate analysis using two-sample Wilcoxon test; ROC curves with AUC calculation; penalized logistic regression with elastic-net (alpha=0.9) and random forest models (500 trees) in leave-one-out cross-validation [103]
Protocol 2: Multi-Omics Biomarker Discovery for Immunotherapy Response
This protocol synthesizes approaches from multiple sources in the search results for comprehensive biomarker identification [1] [105].
Data Collection and Integration:
- Transcriptomic data from GEO repository (19 datasets, 1434 tumor samples across esophageal, gastric, HNSCC, lung, urothelial cancers, melanoma) [105]
- Pre-treatment tumor samples with simultaneously available clinical response data (responders: PR/CR or PFS>12 months; non-responders: PD/SD or PFS<12 months) [105]
- Integration with genomic (TMB, MSI), proteomic, and clinical data [1]
Bioinformatic Analysis:
- Quantile normalization and scaling of gene expression data [105]
- ROC analysis and Mann-Whitney test across all genes to identify features linked to therapy response [105]
- Gene Ontology enrichment analysis for biological process identification [105]
- Machine learning model development with cross-validation [1]
Validation Framework:
Technical Implementation and Data Sharing Models
Data Sharing Architecture
The collaborative initiatives employ varied technical architectures to balance data accessibility with security and governance requirements:
Data Sharing Architecture Diagram
Biomarker Validation Workflow
The pathway from biomarker discovery to regulatory qualification involves multiple validation stages across collaborative frameworks:
Biomarker Validation Workflow Diagram
Research Reagent Solutions and Essential Materials
Table 4: Key Research Reagent Solutions for Biomarker Studies
| Reagent/Material | Function | Application Example |
|---|---|---|
| DURAClone Reagent Panels (IM Phenotyping, T Cell Subsets, TCRs, Treg, B Cell, Dendritic Cell) | Multiparametric flow cytometry staining for immune cell profiling [103] | Identification of T cell subsets associated with irAE risk in melanoma patients [103] |
| Digital Biomarker Platforms (Wearables, smartphones, connected medical devices) [104] | Continuous, real-world monitoring of physiological and behavioral parameters [104] | Detection of subtle neurological changes in stroke trials; monitoring of cancer treatment tolerance [104] |
| Liquid Biopsy Technologies (ctDNA analysis, exosome profiling) [3] | Non-invasive sampling for biomarker detection and monitoring [1] | Circulating tumor DNA dynamics integrated with physiologic data in oncology trials [104] |
| Multi-omics Platforms (Genomic, transcriptomic, proteomic, metabolomic) [1] [3] | Comprehensive biomarker signature identification [1] | Integration of genomic, transcriptomic, and proteomic data to improve predictive accuracy for immunotherapy response [1] |
| Digital Spatial Profiling Technologies (Multiplex immunofluorescence, spatial transcriptomics) [87] | Spatial resolution of tumor microenvironment architecture [87] | Analysis of immune cell infiltration patterns and their correlation with treatment response [87] |
Collaborative frameworks and data-sharing initiatives are fundamentally transforming biomarker advancement by addressing critical limitations in sample sizes, data diversity, and validation robustness. The comparative analysis reveals that successful initiatives share common features: flexible data-sharing models that accommodate various governance requirements, strong patient engagement strategies, and integration with existing research infrastructures. As biomarker science evolves toward multi-parametric approaches integrating digital, molecular, and spatial data, these collaborative frameworks will become increasingly essential for generating the evidence required for regulatory qualification and clinical implementation. Future success will depend on continued standardization efforts, interoperability between platforms, and sustainable models that extend beyond initial funding periods to maximize the value of shared data and samples.
Regulatory Pathways and Clinical Trial Designs for Biomarker Qualification and Approval
The successful development of immunotherapies increasingly depends on validated biomarkers that can predict which patients are most likely to respond to treatment. Biomarkers, defined as "a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention," play a crucial role in precision medicine approaches to cancer treatment [106]. For immunotherapy research, biomarkers help identify patient subgroups likely to benefit from specific immunotherapeutic agents, potentially improving outcomes while reducing unnecessary exposure to ineffective treatments and their associated side effects. The validation of these biomarkers ensures they are reliable, reproducible, and clinically meaningful for their intended use in both drug development and clinical practice. Regulatory oversight by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) provides a critical framework for this validation process, though their approaches exhibit distinct characteristics and requirements.
Regulatory Framework Comparison: FDA vs. EMA
FDA Biomarker Qualification Process
The FDA's approach to biomarker validation is facilitated through its Drug Development Tool (DDT) Qualification Program [107]. This program describes the process for qualifying drug development tools, including biomarkers, for potential use across multiple drug development programs. While the FDA notes that the specific guidance is currently being rewritten in accordance with the 21st Century Cures Act, the agency remains actively engaged in biomarker development through various workshops and stakeholder engagements [107]. Recent FDA-sponsored events have focused on topics such as "Biomarker-driven Drug Development for Allergic Diseases and Asthma" (February 2024) and "Identification of Concepts and Terminology for Multi-Component Biomarkers" (March 2022), indicating ongoing evolution in the regulatory science of biomarkers.
The FDA's practical application of biomarker validation is evident in recent oncology approvals. In July-September 2025, the FDA demonstrated its focus on precision medicine by approving several therapies with companion diagnostics to identify specific patient populations [108]. These include:
- Zongertinib for non-small cell lung cancer (NSCLC) with HER2 mutations, paired with the Oncomine Dx Express Test
- Sunvozertinib for NSCLC with EGFR exon 20 insertion mutations, also paired with the Oncomine Dx Express Test
- Imlunestrant for ER-positive, HER2-negative, ESR1-mutated advanced breast cancer, paired with the Guardant360 CDx assay [108]
EMA Biomarker Qualification Process
The EMA formalized its "Qualification of Novel Methodologies for Medicine Development" procedure in 2008 [109] [106]. This process is overseen by the EMA's Committee for Medicinal Products for Human Use (CHMP), which provides opinions based on recommendations from the Scientific Advice Working Party (SAWP). The EMA procedure can result in different outcomes: a confidential Qualification Advice (QA) for early-stage discussions on evidence generation strategy, or a Qualification Opinion (QO) issued when evidence is deemed adequate to support the biomarker's intended use [106]. A draft QO is published for public consultation before final adoption to confirm validity with the scientific community.
Between 2008 and 2020, the EMA received 86 biomarker qualification procedures, of which only 13 resulted in qualified biomarkers [106]. This highlights the stringent evidentiary requirements of the process. Most biomarkers were proposed (45 of 86) and qualified (9 of 13) for use in patient selection, stratification, and/or enrichment, followed by efficacy biomarkers (37 proposed, 4 qualified) [106]. The data reveal a shift from company-specific biomarker qualification toward consortium-driven qualification efforts aimed at broader application.
Key Differences Between FDA and EMA Approaches
Table 1: Comparison of FDA and EMA Biomarker Validation Pathways
| Aspect | FDA Approach | EMA Approach |
|---|---|---|
| Legal Basis | Drug Development Tool Qualification Program | Qualification of Novel Methodologies for Medicine Development |
| Committee Responsible | Center for Drug Evaluation and Research (CDER) | Committee for Medicinal Products for Human Use (CHMP) advised by Scientific Advice Working Party (SAWP) |
| Qualification Outcomes | Qualification for specific Context of Use | Qualification Advice (confidential) or Qualification Opinion (public) |
| Public Consultation | Not typically part of process | Draft Qualification Opinion published for 2-month public consultation |
| Companion Diagnostic oversight | FDA assesses both therapy and diagnostic | Notified bodies assess diagnostics with EMA consultation [110] |
| Success Rate | Not specified in search results | 15% (13 qualified out of 86 procedures from 2008-2020) [106] |
Table 2: Common Challenges in Biomarker Qualification
| Challenge Category | Frequency in EMA Procedures (2008-2020) | Examples |
|---|---|---|
| Biomarker Properties | 79% of procedures | Analytical validation, biological rationale |
| Assay Validation | 77% of procedures | Performance characteristics, reproducibility |
| Context of Use & Rationale | 54% of procedures | Proposed use case, clinical applicability |
Biomarker Validation in Companion Diagnostics
Companion Diagnostic Regulatory Pathways
Companion diagnostics (CDx) represent a critical application of biomarker validation in immunotherapy. A CDx is defined as a validated test for a predictive biomarker that identifies patients most likely to benefit from a specific therapeutic product [111]. The regulatory frameworks for CDx differ significantly between the US and EU.
In the US, the FDA conducts complete assessment of both the therapy and the diagnostic through cooperation between the Center for Devices and Radiological Health and the Center for Drug Evaluation and Research [111]. When a CDx is co-developed with a new medicine, both are typically approved simultaneously.
In the EU, the system is more fragmented. CDx are regulated under the In Vitro Diagnostic Medical Devices Regulation (IVDR), with conformity assessment conducted by notified bodies [110] [111]. However, for certain high-risk categories including CDx, the notified body must seek a scientific opinion from the EMA on the suitability of the companion diagnostic for the medicinal product if the drug falls under the centralized procedure [110]. This consultation procedure represents how the EMA gains input on CDx despite the separate regulatory pathways for drugs and devices.
Assessment Focus Areas for Companion Diagnostics
Analysis of EMA assessment reports for marketing authorization applications from 2017-2019 reveals that clinical performance and analytical performance of CDx were the most frequently discussed topics [111]. These aspects were addressed 11 and 7 times respectively in European Public Assessment Reports, and 59 and 29 times in the more detailed internal assessment reports [111]. This demonstrates the rigorous scrutiny applied to biomarker-based tests even before the full implementation of the new IVDR.
Diagram 1: Companion Diagnostic Regulatory Pathways - FDA vs. EMA. The diagram illustrates the centralized FDA assessment versus the fragmented EU approach with separate assessments by notified bodies and EMA consultation.
Methodological Framework for Biomarker Validation
Analytical Validation Protocols
Analytical validation forms the foundation of biomarker development, establishing that the biomarker test accurately and reliably measures the intended analyte. The search results indicate that issues related to assay validation were raised in 77% of EMA biomarker qualification procedures [106], highlighting its critical importance. The methodological framework must demonstrate that the biomarker assay meets predefined performance specifications across several key parameters:
- Accuracy and Precision: Experiments must establish both the closeness of agreement between the test result and accepted reference value (accuracy), and the closeness of agreement between independent test results obtained under stipulated conditions (precision). This typically involves testing inter-assay and intra-assay variability using control samples across multiple runs, days, and operators.
- Sensitivity and Specificity: The analytical sensitivity (detection limit) and specificity (ability to measure solely the intended analyte) must be characterized through dilution studies and cross-reactivity testing with structurally similar molecules.
- Linearity and Range: The analytical range over which the test provides accurate results must be defined through experiments demonstrating a directly proportional relationship between test result and analyte concentration.
- Robustness and Reproducibility: The method's capacity to remain unaffected by small, deliberate variations in method parameters (robustness) and its precision under reproducibility conditions (reproducibility) must be established through multisite validation studies.
Clinical Validation Methodologies
Clinical validation establishes that the biomarker reliably identifies the clinical status or predicts the clinical outcome for its intended use. For immunotherapy biomarkers, this typically requires demonstrating a statistically significant association between the biomarker and treatment response. Key methodological considerations include:
- Retrospective-Prospective Study Design: Many biomarker validations utilize archived samples from previously conducted clinical trials, with a predefined statistical analysis plan that specifies the primary endpoint, analysis population, and statistical methods before performing the biomarker analysis.
- Blinded Evaluation: Both biomarker testing and clinical outcome assessment should be performed independently and blinded to the other data to prevent assessment bias.
- Pre-specified Cutpoints: For continuous biomarkers, threshold values that define biomarker-positive and negative populations should be established before clinical validation, ideally using training and validation datasets.
Table 3: Essential Research Reagent Solutions for Biomarker Validation
| Reagent Category | Specific Examples | Function in Validation |
|---|---|---|
| Reference Standards | Certified reference materials, synthetic biomarkers | Establish assay accuracy and calibration curves |
| Quality Control Materials | Commercial control sera, pooled patient samples | Monitor assay precision and reproducibility across runs |
| Assay Kits/Components | Antibody pairs, PCR primers/probes, NGS panels | Detect and quantify biomarker using appropriate technology platform |
| Sample Processing Reagents | Specific anticoagulants, preservatives, fixation buffers | Maintain biomarker integrity from collection to analysis |
| Instrument Calibration Solutions | Calibrators, normalization standards | Ensure consistent instrument performance across sites |
The regulatory pathways for biomarker validation at the FDA and EMA, while distinct in structure and process, share a common goal: ensuring that biomarkers used to guide immunotherapy decisions are scientifically valid and clinically useful. The FDA's Drug Development Tool Qualification Program and the EMA's Qualification of Novel Methodologies both provide frameworks for establishing evidentiary standards, though the EMA process has resulted in only 13 qualified biomarkers from 86 procedures between 2008-2020 [106]. For companion diagnostics specifically, the regulatory approaches differ more significantly, with the FDA maintaining integrated assessment of drug and diagnostic, while the EMA operates through a consultation procedure with notified bodies [110] [111]. Successful navigation of these regulatory landscapes requires careful attention to both analytical performance and clinical validation, with a clear understanding of the specific requirements and challenges emphasized by each agency. As immunotherapy research advances, continued dialogue between researchers and regulators will be essential for developing biomarker validation strategies that support the safe and effective personalization of cancer treatment.
In the evolving landscape of precision oncology, the validation of biomarkers to predict response to immunotherapy has become a critical research focus. Companion diagnostics (CDx) and complementary diagnostics (CoDx) represent two distinct regulatory and clinical pathways for linking diagnostic tests with therapeutic decisions. These tools are indispensable in immuno-oncology, where patient response to immune checkpoint inhibitors (ICIs) and other immunotherapies varies significantly, with only 20-30% of patients achieving durable responses [12] [13]. The accurate classification and application of these diagnostics directly impact clinical trial design, drug development, and ultimately, patient access to optimally targeted treatments.
The emergence of these diagnostic categories reflects the growing complexity of biomarker-driven cancer care. Since the first FDA-approved companion diagnostic (HercepTest for HER2 detection in breast cancer) in 1998, the field has expanded to include over 50-60 approved CDx devices, with an average of approximately 3 new CDx approvals annually from 2011-2024 [112]. Complementary diagnostics represent a more recent conceptual evolution, with the first approved in 2015 for use with nivolumab (OPDIVO) in non-small cell lung cancer (NSCLC) and melanoma patients [112]. This article provides a comprehensive comparison of these two diagnostic pathways within the context of validating biomarkers for immunotherapy response.
Definitions and Regulatory Frameworks
Companion Diagnostics (CDx)
Companion diagnostics are in vitro diagnostic devices or imaging tools that provide information essential for the safe and effective use of a corresponding therapeutic product [112] [113]. These tests are required to be used when the corresponding drug is administered, as they identify patients who are most likely to benefit from a specific targeted therapy or who may be at increased risk for serious side effects [114]. CDx devices undergo rigorous review by regulatory agencies like the U.S. Food and Drug Administration (FDA) and must be approved concurrently with their corresponding therapeutic partners [112] [115].
From a clinical perspective, CDx tests provide binary treatment decisions based on biomarker status. For example, Keytruda (pembrolizumab) is administered only to NSCLC patients who test positive for PD-L1 via the specific IHC 22C3 diagnostic test [112]. The development of a novel CDx typically occurs in parallel with therapeutic development during preclinical and clinical trial stages, with the diagnostic's analytical and clinical studies analyzing its pathophysiological compatibility with the tested patient cohort [112].
Complementary Diagnostics (CoDx)
Complementary diagnostics are biomarker-specific tests that help healthcare professionals assess the risk-benefit profile of a drug, where the difference in benefit-risk is clinically meaningful [112]. Unlike CDx, CoDx tests are not strictly required to be used when prescribing the corresponding drug, though the information they provide aids in making informed treatment decisions.
The fundamental distinction lies in the mandatory nature of testing. While CDx testing is stipulated in the therapeutic product labeling as a requirement for drug administration, CoDx provides additional information that can guide treatment choices without being absolutely mandatory [112]. For example, the therapeutic drug OPDIVO (nivolumab) can be used to treat NSCLC patients even if PD-L1 detection is negative via its complementary IHC 28-8 assay, because the response rate remains similar to the comparator drug in biomarker-negative patients [112].
Table 1: Key Conceptual Differences Between Companion and Complementary Diagnostics
| Parameter | Companion Diagnostic (CDx) | Complementary Diagnostic (CoDx) |
|---|---|---|
| Definition | A biomarker-specific test essential for safe and effective use of a specific therapeutic | A biomarker-specific test that helps assess risk-benefit profile of a drug |
| Regulatory Requirement | Required for drug administration | Not mandatory for drug use |
| Treatment Population | Only biomarker-positive patients receive the drug | All patients may be eligible, with biomarker status informing likelihood of benefit |
| Clinical Decision Impact | Binary: treatment or no treatment based on result | Informative: guides choice between options but doesn't definitively exclude |
| Example | HER2 testing for trastuzumab in breast cancer | PD-L1 testing (clone 28-8) for nivolumab in NSCLC |
Regulatory Evolution and Current Landscape
The regulatory framework for both CDx and CoDx continues to evolve. The FDA has provided specific guidance on "group claims" for companion diagnostics, allowing a single test to be used for multiple therapies within a class [114]. This approach decreases the need for physicians to order multiple companion diagnostic tests and additional biopsies for patients. The first companion diagnostic approved using this framework could be used with five different therapies for NSCLC [114].
As of late 2024, Foundation Medicine alone had 98 approved companion diagnostic indications, with 50% of all approved CDx indications for next-generation sequencing (NGS) testing across the United States and Japan [115]. This represents significant growth from the early days of companion diagnostics, when fewer than one CDx was approved per year up to 2010 [112].
Methodological Pathways and Experimental Validation
Development Pathways for Companion Diagnostics
The development of a novel CDx follows a structured co-development pathway with its corresponding therapeutic:
1. Preclinical Biomarker Discovery: Identification of potential biomarkers using techniques such as genomic sequencing, proteomic analysis, or immunohistochemistry. For example, the development of HER2 as a biomarker involved discovering its overexpression in aggressive breast cancer subtypes [112] [114].
2. Assay Development and Analytical Validation: Creation of a robust diagnostic assay with demonstrated accuracy, precision, sensitivity, and specificity. This phase includes determining the optimal scoring system, as seen with PD-L1 IHC assays where different scoring systems (TPS vs. CPS) were developed for different clinical contexts [12].
3. Clinical Validation in Trial Populations: The assay is tested within clinical trials to establish its predictive value for therapeutic response. For instance, the KEYNOTE-001 trial established PD-L1 expression as a predictor of response to pembrolizumab, with ORR of 45%, 16.5% and 10.7% in patients with TPS ≥50%, 1-49% and <1%, respectively [12].
4. Regulatory Submission and Concurrent Approval: Submission of analytical and clinical performance data to regulatory agencies for approval alongside the therapeutic product.
The following diagram illustrates the co-development pathway for companion diagnostics:
Validation Approaches for Complementary Diagnostics
The validation of complementary diagnostics follows a different evidentiary standard:
1. Biomarker-Drug Response Correlation: Establishing a statistically significant association between biomarker status and treatment outcomes, without necessarily being definitive for treatment eligibility. For example, the PD-L1 IHC 28-8 assay showed that NSCLC patients with higher PD-L1 expression had better outcomes with nivolumab, but benefit was still observed in PD-L1 negative patients [112].
2. Risk-Benefit Profiling: Demonstrating that the diagnostic provides information that meaningfully alters the risk-benefit calculation for a particular therapy. This may involve showing differential response rates, progression-free survival, or overall survival across biomarker subgroups.
3. Clinical Utility Evidence: Generating evidence that using the diagnostic leads to improved treatment decisions or patient outcomes compared to not using it, without making it absolutely required.
4. Regulatory Review as Complementary: Submission of evidence showing the test provides clinically meaningful information for risk-benefit assessment, without being essential for safe use.
Experimental Designs for Biomarker Validation
Validation of both CDx and CoDx in immunotherapy research employs several key experimental approaches:
Prospective-Retrospective Analysis: Using archived samples from previously conducted clinical trials to validate the biomarker-therapy relationship. This approach was used in the validation of TMB as a biomarker for pembrolizumab in the KEYNOTE-158 trial [12].
Basket Trials: Enrollment based on biomarker status regardless of tumor histology, as seen in trials leading to the tumor-agnostic approval of pembrolizumab for MSI-H/dMMR tumors [12].
Adaptive Enrichment Designs: Trials that begin with all-comers but can restrict enrollment to biomarker-positive subgroups based on interim analyses. This approach optimizes patient selection while maintaining statistical validity.
Blinded Independent Central Review: For imaging-based diagnostics or complex biomarker assessments, independent verification of results reduces bias and increases reliability.
Table 2: Key Methodological Approaches in Diagnostic Validation
| Methodological Approach | Application in CDx Development | Application in CoDx Development |
|---|---|---|
| Analytical Validation | Demonstrate high accuracy, precision, sensitivity, specificity with strict predefined thresholds | Establish reproducibility and reliability with clinically relevant performance |
| Clinical Cutpoint Determination | Define binary positive/negative thresholds with clinical outcome correlation | Establish continuous or categorical relationships with outcome probabilities |
| Prospective Clinical Trials | Required for regulatory approval, often as part of therapeutic pivotal trials | Used to demonstrate clinical utility but not always required for regulatory clearance |
| Real-World Evidence | Supplemental to pivotal trial data | May play larger role in establishing utility across diverse populations |
| Comparison to Standard of Care | Often compared to biomarker-negative control or standard therapy | Often shows incremental benefit over standard selection methods |
Technical Platforms and Detection Methodologies
Established Technological Platforms
Multiple technological platforms support both companion and complementary diagnostics in immunotherapy:
Immunohistochemistry (IHC): Remains a foundational method for protein biomarker detection, particularly for PD-L1 expression assessment. Different antibody clones (22C3, 28-8, SP142, SP263) have been developed as companion or complementary diagnostics for various PD-1/PD-L1 inhibitors [112] [12]. Standardized scoring systems (TPS, CPS) are essential for reproducible results.
Next-Generation Sequencing (NGS): Enables comprehensive genomic profiling from limited tissue samples. Foundation Medicine's FoundationOne CDx analyzes 324 genes plus genomic signatures including MSI and TMB, serving as a companion diagnostic for multiple therapies [115]. NGS-based tests like MI Cancer Seek provide whole exome and whole transcriptome sequencing for comprehensive molecular profiling [116].
Polymerase Chain Reaction (PCR): Provides highly sensitive detection of specific mutations. PCR-based platforms represent the largest proportion of CDx assays, with examples including the cobas EGFR Mutation Test v2 for detecting EGFR mutations in NSCLC [112] [114].
Liquid Biopsy: Analyzes circulating tumor DNA (ctDNA) from blood samples, offering a less invasive alternative to tissue biopsies. The first liquid biopsy CDx was approved in 2016 for EGFR mutation detection in NSCLC [114].
Emerging Technologies and Multi-Omics Approaches
The field is rapidly evolving toward more comprehensive biomarker assessment:
Multi-Omics Integration: Combining genomic, transcriptomic, proteomic, and epigenomic data for improved prediction. The Comprehensive Oncological Biomarker Framework integrates multiple data types to generate a molecular fingerprint for each patient [20].
Digital Pathology and AI: Artificial intelligence enhances traditional pathology assessment. Deep learning algorithms improve PD-L1 scoring accuracy and immune cell profiling, with some systems achieving AUC values above 0.85 in predicting ICI response [13].
Spatial Profiling: Technologies that preserve spatial relationships in the tumor microenvironment, providing critical information about immune cell distribution and tumor-immune interactions.
Multi-Cancer Early Detection (MCED): Tests like the Galleri assay detect multiple cancer types simultaneously through ctDNA analysis, potentially expanding applications for immunotherapy biomarkers [24].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Tools for Immunotherapy Diagnostic Development
| Tool/Category | Specific Examples | Research Application |
|---|---|---|
| IHC Assays | PD-L1 IHC 22C3, 28-8, SP142, SP263 pharmDx assays | Protein expression analysis in tumor microenvironment |
| NGS Platforms | FoundationOne CDx, MI Cancer Seek, TruSight Oncology Comprehensive | Comprehensive genomic profiling, TMB, MSI assessment |
| Liquid Biopsy Technologies | FoundationOne Liquid CDx, Guardant360 | Non-invasive biomarker monitoring and detection |
| Single-Cell Analysis | 10X Genomics, ATLAS-seq technology | Immune cell repertoire analysis, T cell reactivity screening |
| Spatial Biology Platforms | NanoString GeoMx, 10X Visium | Tumor microenvironment mapping, immune cell localization |
| Multiplex Immunofluorescence | Akoya PhenoImager, Standard BioTools | Simultaneous detection of multiple immune markers |
| AI-Assisted Pathology | HALO, QuPath with custom algorithms | Automated scoring, pattern recognition in tissue sections |
| Biosensor Platforms | SPR, electrochemical biosensors | Rapid biomarker detection with high sensitivity |
Clinical Applications in Immunotherapy
Established Biomarkers for Immune Checkpoint Inhibitors
Several biomarkers have been validated as companion or complementary diagnostics for immunotherapy:
PD-L1 Expression: The most extensively characterized biomarker for ICIs, approved as both companion and complementary diagnostic depending on the specific drug and context. PD-L1 IHC testing is required as a companion diagnostic for first-line pembrolizumab in NSCLC (TPS ≥1%), while serving as a complementary diagnostic for nivolumab in the same setting [12].
Microsatellite Instability (MSI) / Mismatch Repair Deficiency (dMMR): Approved as a tissue-agnostic companion diagnostic for pembrolizumab in 2017, representing a paradigm shift in biomarker-defined therapy [12]. MSI-high status predicts response across multiple tumor types.
Tumor Mutational Burden (TMB): Approved as a tissue-agnostic companion diagnostic for pembrolizumab in 2020 based on the KEYNOTE-158 trial, which showed an ORR of 29% in TMB-high (≥10 mut/Mb) solid tumors [12].
Additional Emerging Biomarkers: Gene expression profiles (such as T-cell inflamed signature), immune cell infiltration patterns, and gut microbiome composition are under investigation as potential complementary biomarkers [20] [12].
Clinical Decision Pathways
The clinical application of CDx versus CoDx follows distinct decision pathways:
Comparative Clinical Performance Data
Table 4: Performance Characteristics of Selected Immunotherapy Diagnostics
| Diagnostic Test | Biomarker | Therapeutic Context | Clinical Performance | Regulatory Classification |
|---|---|---|---|---|
| PD-L1 IHC 22C3 | PD-L1 expression | Pembrolizumab in NSCLC (1L) | ORR: 45% in TPS≥50%, 16.5% in TPS1-49%, 10.7% in TPS<1% | Companion Diagnostic |
| PD-L1 IHC 28-8 | PD-L1 expression | Nivolumab in NSCLC | Improved survival in PD-L1+ but benefit also in PD-L1- patients | Complementary Diagnostic |
| FoundationOne CDx | TMB | Pembrolizumab in solid tumors | ORR: 29% in TMB-H (≥10 mut/Mb) vs. 6% in TMB-L | Companion Diagnostic |
| MSI Testing | Microsatellite instability | Pembrolizumab in solid tumors | ORR: 39.6% in MSI-H vs. 0% in non-MSI-H cancers | Companion Diagnostic |
| MI Cancer Seek | Comprehensive profiling | Multiple targeted therapies | >97% concordance with other FDA-approved CDx | Companion Diagnostic |
The distinction between companion and complementary diagnostics represents more than semantic differences—it reflects fundamental variations in regulatory pathways, clinical utility, and evidentiary standards. For researchers validating biomarkers to predict immunotherapy response, understanding these pathways is crucial for appropriate trial design and regulatory strategy.
Future developments in the field will likely include:
Multi-modal Algorithmic Approaches: Combining multiple biomarkers into integrated algorithms, such as the SCORPIO and LORIS machine learning systems that have demonstrated superior performance compared to single biomarkers (AUC values of 0.763) [13].
Dynamic Biomarker Assessment: Moving beyond single-timepoint assessment to serial monitoring using liquid biopsy and other minimally invasive approaches to track biomarker evolution during treatment.
Standardization and Harmonization: Efforts to align scoring systems, assay requirements, and analytical validation approaches across platforms and regulatory jurisdictions.
Expansion Beyond Oncology: While currently dominated by oncology applications, both CDx and CoDx concepts are expanding to neurological, cardiovascular, and infectious diseases [117].
As precision medicine continues to evolve, the strategic implementation of both companion and complementary diagnostics will be essential for maximizing the clinical benefit of immunotherapies while ensuring their appropriate use in defined patient populations. For researchers in the field, careful consideration of the regulatory and clinical pathways for these diagnostics will facilitate more efficient translation of biomarkers from discovery to clinical practice.
Cancer immunotherapy, particularly the use of immune checkpoint inhibitors (ICIs), has fundamentally transformed oncology treatment, offering durable responses and prolonged survival for patients with various malignancies [105] [12]. However, a significant challenge persists: these remarkable benefits are confined to a subset of patients. Response rates to ICIs vary widely, meaning that a considerable proportion of patients do not respond to treatment, yet remain exposed to potential immune-related adverse events, treatment delays, and unnecessary costs [2] [1]. This reality underscores the critical need for robust predictive biomarkers—biological indicators that can identify patients most likely to benefit from a specific therapy [1].
The validation of predictive biomarkers through clinical research is a complex but essential process for the advancement of personalized medicine. Among the various strategies for biomarker validation, two primary approaches have emerged: retrospective analysis of existing clinical trial data and prospective enrichment of new trial populations. This guide provides an objective comparison of these two core designs, framing them within the broader thesis of validating biomarkers to predict response to immunotherapy. It is intended to equip researchers, scientists, and drug development professionals with a clear understanding of the applications, methodologies, and trade-offs inherent in each strategy.
Foundational Concepts: Biomarkers and Clinical Trial Designs
Predictive vs. Prognostic Biomarkers
A critical distinction in biomarker development is between predictive and prognostic markers. A predictive biomarker identifies patients who are more likely to respond to a particular targeted therapy. Its clinical utility lies in enabling individualized therapy selection. In contrast, a prognostic biomarker provides information about a patient's overall cancer outcome, such as disease recurrence or survival, independent of any specific treatment [118] [38]. This review focuses exclusively on the validation of predictive biomarkers for immunotherapy response.
Clinical studies are broadly classified as observational studies or interventional clinical trials. Key observational designs relevant to biomarker research include:
- Cohort Studies: Follow groups of individuals (cohorts) over time. They can be prospective (following participants forward in time) or retrospective (using pre-existing data to look back in time) [119].
- Case-Control Studies: Compare a group with the disease or outcome (cases) to a group without it (controls) to identify differences in exposure to risk factors. These are typically retrospective [119].
For predictive biomarker validation, Randomized Controlled Trials (RCTs) are the gold standard, as the randomization process ensures that patients receiving the investigational agent are comparable to those in the control group, isolating the treatment's causal effect [118] [38].
Retrospective Analysis for Biomarker Validation
Definition and Application
Retrospective biomarker validation involves testing a pre-specified biomarker hypothesis using data and biological samples (e.g., tumor tissue) collected from a previously completed, well-conducted randomized controlled trial [118]. This approach does not require a new clinical trial to be initiated; instead, it leverages existing resources to investigate whether a biomarker can identify a subgroup of patients who derived particular benefit (or lack thereof) from the therapy under investigation.
Methodology and Experimental Protocol
A rigorous retrospective validation study requires a meticulous, pre-planned protocol to minimize bias and generate reliable evidence.
- Step 1: Prerequisite - A High-Quality RCT. The foundation is a previously conducted RCT comparing the immunotherapy of interest against a control treatment. The trial must have been well-designed and properly executed.
- Step 2: Sample Availability and Selection. Archival tumor samples must be available for a large majority (>90%) of patients enrolled in the original trial. A high percentage is crucial to avoid selection bias, where the patients with available tissue are not representative of the entire trial population [118].
- Step 3: Prospectively Defined Analysis Plan. Before any laboratory analysis begins, researchers must pre-specify the hypothesis, the patient population, the specific biomarker assay, the scoring system, and the statistical analysis plan, including how the biomarker will be dichotomized (e.g., positive vs. negative) [118].
- Step 4: Assay Performance. The biomarker assay (e.g., immunohistochemistry for PD-L1, next-generation sequencing for TMB) is performed on the collected samples using a predefined and standardized protocol.
- Step 5: Statistical Analysis and Interpretation. The treatment effect (e.g., overall survival, progression-free survival) is compared between the experimental and control arms within each biomarker-defined subgroup (e.g., biomarker-positive vs. biomarker-negative). A statistically significant interaction test provides strong evidence that the treatment effect differs by biomarker status [118].
Table 1: Key Requirements for a Robust Retrospective Validation Study
| Requirement | Description | Rationale |
|---|---|---|
| Source RCT | Data from a well-conducted prior randomized controlled trial. | Ensures the patient populations are comparable and the treatment effect is reliably estimated. |
| Sample Availability | Biomarker samples available for a large majority (>90%) of original trial patients. | Minimizes selection bias that can invalidate the study conclusions. |
| Pre-specified Plan | Prospectively stated hypothesis, analysis techniques, and patient population. | Prevents data dredging and false-positive findings from exploratory analyses. |
| Standardized Assay | Predefined and standardized biomarker assay and scoring system. | Ensures consistency and reproducibility of biomarker measurement. |
Case Study: KRAS in Colorectal Cancer
A seminal example of successful retrospective validation is the KRAS gene in metastatic colorectal cancer. Retrospective analysis of phase III trial data for the anti-EGFR antibodies panitumumab and cetuximab demonstrated that clinical benefit was restricted to patients with tumors harboring wild-type KRAS, with no benefit observed in those with KRAS mutations [118]. The analysis was performed on samples from over 90% of the trial participants, showed a dramatic treatment-by-biomarker interaction, and was consistent across multiple studies. This compelling retrospective evidence led to a change in drug labels and clinical practice, restricting treatment to the biomarker-defined subgroup [118].
Prospective Enrichment for Biomarker Validation
Definition and Application
A prospective enrichment design (also known as a targeted design) is a strategy for a new clinical trial where only patients with a specific biomarker profile are enrolled [118] [38]. This design is based on the premise that compelling preliminary evidence suggests the treatment benefit is largely or entirely confined to a biomarker-defined subgroup. All patients are screened for the biomarker, but only those who are "positive" (or sometimes only those who are "negative") are entered into the trial and randomized to receive either the investigational therapy or the control.
Methodology and Experimental Protocol
Implementing a prospective enrichment design requires significant upfront planning and infrastructure.
- Step 1: Preliminary Evidence Assessment. Strong preliminary data from early-phase trials or mechanistic studies must indicate that the treatment is highly effective in a biomarker-defined group and ineffective in others.
- Step 2: Assay Validation and Logistics. The biomarker assay must be analytically validated and clinically feasible. This includes establishing its reproducibility, accuracy, and turnaround time that is practical for clinical decision-making [38].
- Step 3: Patient Screening and Enrollment. A large number of patients are screened to identify the biomarker-positive subgroup. Only these eligible patients provide informed consent and are randomized into the trial.
- Step 4: Randomization and Treatment. Enrolled patients are randomized to receive the immunotherapy or the control treatment. The trial is conducted like a standard RCT, but within a selected population.
- Step 5: Analysis. The primary analysis compares outcomes between the treatment and control arms within the enriched, biomarker-positive population.
Table 2: Key Considerations for a Prospective Enrichment Design
| Consideration | Implication for Trial Design |
|---|---|
| Strength of Preliminary Evidence | Must be compelling to justify excluding a potentially large subset of patients. |
| Marker Prevalence | Determines the screening burden; low prevalence requires extensive screening to accrue the required number of patients. |
| Assay Reliability & Turnaround Time | The assay must be robust and provide results quickly enough to guide treatment decisions without delaying care. |
| Ethical Justification | It must be ethically defensible to withhold the experimental treatment from biomarker-negative patients. |
Case Study: HER2 in Breast Cancer
The validation of HER2 for trastuzumab (Herceptin) therapy in breast cancer is a classic example of a prospective enrichment design. The pivotal phase III trials that led to the drug's approval enrolled only women whose breast cancers were HER2-positive, based on strong evidence that the drug's mechanism of action targeted this pathway [118]. This strategy successfully identified a patient population that derived substantial benefit. However, subsequent questions arose about whether some patients with lower levels of HER2 expression might also benefit, and issues of assay reproducibility between local and central testing were highlighted because the design did not include biomarker-negative patients [118].
Direct Comparison: Strengths, Limitations, and Applications
The choice between retrospective and prospective validation strategies is not a matter of one being universally superior, but rather of selecting the right tool for a specific research context based on the available evidence and resources.
Table 3: Objective Comparison of Retrospective Analysis vs. Prospective Enrichment
| Parameter | Retrospective Analysis | Prospective Enrichment |
|---|---|---|
| Definition | Testing a biomarker hypothesis using data/samples from a completed RCT. | Conducting a new RCT exclusively in a biomarker-defined patient subgroup. |
| Time & Cost | Relatively faster and less expensive. | Lengthy and costly, requires new patient recruitment and screening. |
| Level of Evidence | Can provide strong evidence if done rigorously; often considered hypothesis-strengthening. | Considered the gold standard for prospective validation when feasible. |
| Key Advantage | Efficient use of existing resources; can bring treatments to biomarker-defined groups faster. | Maximizes efficiency for testing a therapy in its most likely responder population. |
| Key Limitation | Dependent on the quality and sample availability of a prior trial; potential for bias. | Does not provide information on the treatment effect in biomarker-negative patients. |
| Ideal Use Case | When a highly effective therapy exists and a plausible biomarker candidate emerges post-trial. | When pre-clinical/early clinical data strongly suggest benefit is restricted to a biomarker subgroup. |
| Ethical Considerations | Minimally invasive, uses already-collected data. | Requires denying a potentially active treatment to biomarker-negative patients. |
The following decision pathway can guide researchers in selecting an appropriate validation strategy:
The Scientist's Toolkit: Essential Reagents and Technologies
The execution of both retrospective and prospective biomarker studies relies on a suite of core technologies and reagents.
Table 4: Key Research Reagent Solutions for Immunotherapy Biomarker Validation
| Tool / Reagent | Primary Function | Application in Immunotherapy Biomarkers |
|---|---|---|
| Immunohistochemistry (IHC) | Visualize protein expression in formalin-fixed paraffin-embedded (FFPE) tissue sections using labeled antibodies. | Measuring PD-L1 protein expression on tumor or immune cells (e.g., with Dako 22C3, 28-8, or Ventana SP142 assays) [2] [12]. |
| Next-Generation Sequencing (NGS) | High-throughput DNA sequencing to identify genomic alterations across many genes simultaneously. | Assessing Tumor Mutational Burden (TMB), Microsatellite Instability (MSI), and specific gene mutations (e.g., KRAS) [2] [1]. |
| RNA Sequencing | Profile the entire transcriptome to measure gene expression levels. | Developing gene expression signatures (e.g., T-cell inflamed signature) and multi-omics biomarkers [105]. |
| Multiplex Flow Cytometry | Analyze multiple surface and intracellular proteins on single cells within a heterogeneous population. | Characterizing immune cell populations in blood or tissue, such as T-regulatory cells, MDSCs, or activated T cells [2]. |
| Circulating Tumor DNA (ctDNA) Assays | Detect and quantify tumor-derived DNA fragments from a blood sample (liquid biopsy). | Monitoring dynamic changes in tumor burden and molecular landscape during therapy; early detection of resistance [1]. |
Both retrospective analysis and prospective enrichment are powerful, validated strategies for the clinical validation of predictive biomarkers in immunotherapy. The choice between them is dictated by the maturity of the biomarker hypothesis, the availability of high-quality retrospective resources, and practical considerations around assay development.
- Retrospective analysis provides a powerful, efficient, and timely method to bring effective treatments to biomarker-defined patient subgroups, as dramatically demonstrated by the KRAS validation story.
- Prospective enrichment is the gold-standard prospective design when preliminary evidence strongly suggests a treatment's benefit is restricted to a specific biomarker-defined population, exemplified by the HER2/trastuzumab paradigm.
The ongoing challenge in immuno-oncology is that single biomarkers like PD-L1, TMB, and MSI, while validated and useful, are imperfect, with significant heterogeneity in response [1] [12] [120]. The future of biomarker development likely lies in integrated, multi-parametric approaches that combine genomic, transcriptomic, and proteomic data to build more accurate predictive models [2] [1]. Regardless of the complexity of the biomarker signature, the fundamental principles of rigorous clinical validation—through either meticulous retrospective analysis or carefully executed prospective enrichment—will remain the cornerstone of delivering on the promise of personalized cancer immunotherapy.
Cancer immunotherapy, particularly the use of immune checkpoint inhibitors (ICIs), has fundamentally transformed oncology care by offering durable responses for several malignancies [1]. However, a significant challenge persists: these therapies benefit only a subset of patients, with response rates remaining variable [1] [13]. This reality underscores the critical need for robust predictive biomarkers to guide therapy selection, maximize clinical benefit, and minimize unnecessary toxicity and costs [1].
The clinical utility of a biomarker is established when its use directly leads to improved patient outcomes by informing medical decision-making. In the context of immunotherapy, a biomarker with demonstrable clinical utility reliably identifies patients who are likely to respond to treatment, thereby linking biomarker testing to tangible clinical benefits such as prolonged survival and enhanced quality of life. This guide provides a comparative analysis of established and emerging biomarkers, evaluating their performance and utility in predicting response to immunotherapy.
Comparative Analysis of Biomarker Performance
The following tables summarize the clinical utility, supporting evidence, and limitations of key biomarkers used to predict response to immunotherapy.
Table 1: Comparison of Validated Predictive Biomarkers in Immunotherapy
| Biomarker | Clinical Utility & Mechanism | Key Supporting Evidence (Trial/Study) | Representative Clinical Outcome | Major Limitations |
|---|---|---|---|---|
| PD-L1 Expression | Predicts response to anti-PD-1/PD-L1 therapies; reflects pre-existing immune response [1]. | KEYNOTE-024 (NSCLC) [1] | In NSCLC with PD-L1 ≥50%, mOS 30.0 mo vs 14.2 mo with chemo (HR: 0.63) [1]. | Assay variability, tumor heterogeneity, limited predictive value in 71.1% of FDA approvals [1] [13]. |
| MSI-H/dMMR | Tissue-agnostic biomarker; high neoantigen load from defective DNA repair [1]. | KEYNOTE-016, -164, -158 (multiple cancers) [1] | ORR 39.6% with 78% durable responses; led to tissue-agnostic FDA approval [1]. | Limited to a small subset of patients across cancer types [1]. |
| Tumor Mutational Burden (TMB) | High mutation count correlates with increased neoantigens and immunogenicity [1]. | KEYNOTE-158 (multiple cancers) [1] | ORR 29% in TMB-H (≥10 mut/Mb) vs 6% in TMB-Low [1]. | Cost, standardization issues, variable predictive value across cancer types [1]. |
Table 2: Emerging and Investigational Biomarkers in Immunotherapy
| Biomarker | Clinical Utility & Mechanism | Key Supporting Evidence (Trial/Study) | Representative Clinical Outcome / Finding | Major Limitations / Status |
|---|---|---|---|---|
| Circulating Tumor DNA (ctDNA) | Dynamic monitoring of tumor burden and minimal residual disease; early response indicator [1]. | Multiple meta-analyses [1] | ≥50% ctDNA reduction within 6-16 weeks of ICI correlates with better PFS and OS [1]. | Requires further standardization; clinical utility for early decision-making under investigation [1]. |
| TET2-mutated Clonal Hematopoiesis | Myeloid cell mutations prime antitumor immunity by enhancing antigen presentation [121]. | MD Anderson study (NSCLC, Colorectal Cancer) [121] | Significantly improved OS with ICI in NSCLC (n=35,000) and colorectal cancer (n=25,064) cohorts [121]. | Novel finding; potential biomarker requiring prospective validation [121]. |
| Early On-Treatment Liquid Biopsy (LiBIO) | Detects early expansion of effector memory T and B cells in blood post-ICI, predicting tumor regression [122]. | Murine HNSCC model & human validation [122] | Outperformed existing biomarkers; generalized to melanoma, NSCLC, and breast cancer without retraining [122]. | Defines a new, dynamic biomarker class; validation in large-scale clinical trials is the next step [122]. |
| Tumor-Infiltrating Lymphocytes (TILs) | High levels indicate a pre-existing, active anti-tumor immune response [1]. | Studies in TNBC and HER2+ breast cancer [1] | Associated with improved response and prognosis; recognized in Scandinavian and ESMO guidelines [1]. | No universal scoring standard, though considered low-cost and reproducible [1]. |
Experimental Protocols for Biomarker Validation
The journey from biomarker discovery to clinical application is a rigorous, multi-stage process. The following protocols outline the key experimental and statistical methodologies required to robustly validate a biomarker's clinical utility.
Protocol 1: Distinguishing Predictive from Prognostic Biomarkers
A fundamental step in validation is correctly classifying a biomarker's function. This requires specific statistical approaches using data from randomized clinical trials.
- Objective: To determine whether a biomarker is predictive (interacts with a specific treatment to influence outcome) or prognostic (provides information on outcome independent of therapy) [7].
- Experimental Design:
- Cohort: Utilize biospecimens and data from a prospective randomized clinical trial where patients were assigned to the immunotherapy of interest or a control therapy [7].
- Measurement: Measure the candidate biomarker in all patient samples, ensuring blinding of laboratory personnel to clinical outcomes and treatment arms to prevent bias [7].
- Statistical Analysis:
- For a predictive biomarker, the primary test is for a statistical interaction between the treatment and the biomarker in a model for the clinical outcome (e.g., overall survival, progression-free survival). A significant interaction term (e.g., P < .05) indicates that the treatment effect differs based on the biomarker's status [7]. The IPASS study, which established EGFR mutation as a predictive biomarker for gefitinib, is a classic example of this approach [7].
- For a prognostic biomarker, test for a main effect of the biomarker on the outcome in a statistical model, which can be done using data from a single-arm trial or a cohort study, though prospective designs are more reliable [7].
- Key Considerations: Control for multiple comparisons, pre-specify the analysis plan, and ensure the study is powered to detect an interaction effect, which typically requires a larger sample size than detecting a main effect [7].
Protocol 2: Analytical Validation and Performance Assessment
Before clinical utility can be assessed, the biomarker test itself must be analytically validated.
- Objective: To establish the technical performance and reliability of the biomarker assay.
- Experimental Workflow:
- Assay Development: Define the standard operating procedure for the assay (e.g., IHC, NGS, ctDNA sequencing).
- Performance Metrics: Evaluate the assay for [123]:
- Analytical Sensitivity: The lowest detectable quantity of the biomarker.
- Analytical Specificity: The assay's ability to measure solely the intended biomarker.
- Reproducibility: Consistency of results across different operators, instruments, and laboratories over time.
- Precision: The assay's repeatability under unchanged conditions.
- Cohort Testing: Run the assay on a well-characterized set of clinical samples that represent the intended-use population.
- Statistical Metrics: Calculate standard performance metrics based on the intended application [7] [123]:
- Sensitivity & Specificity
- Positive Predictive Value (PPV) & Negative Predictive Value (NPV)
- Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve to measure overall discrimination.
Figure 1: The biomarker development and validation pathway, from discovery to clinical adoption.
Visualizing Biomarker Function and Validation
The Mechanism of a Predictive Biomarker
The following diagram illustrates the conceptual mechanism of a predictive biomarker for immunotherapy, such as PD-L1 or MSI-H, which identifies patients whose tumors are susceptible to a specific therapy.
Figure 2: How a predictive biomarker guides treatment for improved patient outcomes.
Multi-Modal and AI-Enhanced Biomarker Approaches
Given the limitations of single biomarkers, the field is moving towards integrated models. For instance, machine learning systems like SCORPIO and LORIS have demonstrated superior performance (AUC values up to 0.85+) compared to traditional single-biomarker methods [13]. These models integrate diverse data types—including clinical parameters, genomic data (TMB, MSI), transcriptomic signatures (T cell exhaustion), and digital pathology features (TIL density, spatial organization)—to generate a more comprehensive prediction of treatment response [1] [13]. This multi-modal approach more accurately captures the complex biology of the tumor-immune interaction.
Table 3: Key Reagents and Resources for Immunotherapy Biomarker Research
| Tool / Resource | Function in Biomarker Research | Example Application |
|---|---|---|
| Next-Generation Sequencing (NGS) | Comprehensive profiling of genomic (TMB, MSI, mutations) and transcriptomic biomarkers [7]. | Targeted or whole-exome sequencing for TMB calculation; RNA-seq for immune gene signatures [1]. |
| Immunohistochemistry (IHC) Antibodies | Detect protein expression of biomarkers (e.g., PD-L1) in tumor tissue [1]. | Standardized PD-L1 scoring using validated antibodies (e.g., 22C3, SP142, SP263 pharmDx assays) [1]. |
| Single-Cell RNA Sequencing | Characterize cellular composition and transcriptional states within the tumor immune microenvironment [122]. | Identification of expanded T and B cell clonotypes in responders vs. non-responders in liquid biopsies [122]. |
| Circulating Tumor DNA (ctDNA) Assays | Enable non-invasive "liquid biopsy" for dynamic monitoring of tumor burden and molecular response [1] [122]. | Tracking ctDNA levels pre- and on-treatment to correlate clearance with improved PFS/OS [1]. |
| Flow Cytometry Panels | Quantify and phenotype immune cell populations (e.g., T cell subsets, myeloid cells) in blood or tissue. | Monitoring changes in relative eosinophil count (REC) or other peripheral immune cells as a prognostic indicator [1]. |
| FDA Biomarker Qualification Program | Provides a collaborative regulatory pathway to qualify biomarkers for a specific Context of Use (COU) in drug development [124]. | Submitting a Letter of Intent (LOI) and Qualification Plan (QP) to gain regulatory endorsement for a novel biomarker [124]. |
The demonstration of clinical utility remains the definitive step in the translation of a biomarker from a research observation to a clinically impactful tool. While established biomarkers like PD-L1 and MSI-H provide a foundational framework, their limitations are clear. The future of predicting immunotherapy response lies in the rigorous validation of novel, dynamic biomarkers—such as TET2-mutated CH and early on-treatment liquid biopsies—and, more importantly, in the intelligent integration of multi-modal data through sophisticated computational models. For researchers and drug developers, adhering to robust statistical principles, following structured regulatory pathways, and focusing on the complex, integrated biology of the immune response will be key to delivering biomarkers that truly improve patient outcomes.
The validation of robust biomarkers is a critical cornerstone in the advancement of cancer immunotherapy, enabling the precise identification of patients most likely to benefit from treatment. Immune checkpoint inhibitors (ICIs) have fundamentally transformed the oncology landscape, producing remarkable and durable responses in subsets of patients with advanced metastatic disease [125]. However, the majority of patients do not respond, and these therapies can cause significant immune-related adverse events (irAEs) [125]. This clinical reality underscores the urgent need for reliable predictive biomarkers to guide therapeutic decision-making. The validation pathway for a biomarker—from discovery to regulatory acceptance—is complex and stringent, with only about 0.1% of potentially clinically relevant cancer biomarkers described in literature progressing to routine clinical use [66]. This comparative guide objectively analyzes the performance, validation methodologies, and clinical applications of the key validated biomarkers currently shaping immunotherapy research and practice.
Established Biomarkers for Immunotherapy Response
Three biomarkers have achieved widespread validation and regulatory endorsement for predicting response to immune checkpoint blockade: Microsatellite Instability/ Mismatch Repair Deficiency (MSI-H/dMMR), Tumor Mutational Burden (TMB), and Programmed Death-Ligand 1 (PD-L1) expression. Each possesses distinct strengths, limitations, and contexts of use.
Table 1: Comparative Analysis of Validated Immunotherapy Biomarkers
| Biomarker | Mechanistic Rationale | Key Clinical Evidence | Response Rates (ORR) | Regulatory Status | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| MSI-H/dMMR | Genomic instability generates numerous neoantigens, enhancing immunogenicity [125]. | Pivotal trial: 40% ORR in MMRd colorectal cancer; 71% in non-colorectal cancers [125]. | 40-71% (tumor-agnostic) [125]. | FDA-approved, tissue-agnostic for pembrolizumab and dostarlimab [125] [126]. | Tissue-agnostic; high response rates; strong predictive value. | Rare in common cancers (e.g., colon, endometrial); some patients still do not respond [125]. |
| High TMB | High somatic mutation load increases likelihood of immunogenic neoantigen formation [125]. | Combined ORR of 29% in TMB-high (≥10 mut/Mb) solid tumors; other studies suggest cut-off of ≥16 mut/Mb may be more predictive [125]. | ~29% (at ≥10 mut/Mb) [125]. | FDA-approved, tissue-agnostic for pembrolizumab (TMB ≥10 mut/Mb) [125]. | Tissue-agnostic; quantitative measure. | Lack of universal assay harmonization; variable predictive cut-offs [125]. |
| PD-L1 Expression | Directly measures target of PD-1/PD-L1 inhibitors; reflects pre-existing immune response [125]. | Linked to response in NSCLC, bladder cancer, TNBC, and others; specific thresholds vary by cancer type and assay [125]. | Varies by cancer type and defined threshold. | Multiple FDA approvals with companion diagnostics [125]. | Mechanistically intuitive; validated in multiple cancer types. | Dynamic expression; intra-tumoral heterogeneity; differing assays and cut-offs [125]. |
Experimental Protocols and Methodologies for Biomarker Assessment
The accurate assessment of these biomarkers relies on standardized, validated experimental protocols. The following sections detail the core methodologies.
Assessment of Microsatellite Instability (MSI) and Mismatch Repair (MMR) Status
1. Protocol for Immunohistochemistry (IHC) for dMMR:
- Objective: To detect the loss of MMR protein expression (MLH1, MSH2, MSH6, PMS2) in tumor tissue.
- Methodology:
- Tissue Sectioning: Formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections are cut at 4-5 μm thickness.
- Staining: Sections are stained with antibodies against the four MMR proteins using automated IHC platforms.
- Interpretation: Nuclear staining in tumor cells is compared to internal positive controls (e.g., non-neoplastic stromal cells, lymphocytes). Loss of nuclear expression in tumor cells for one or more proteins is indicative of dMMR. The specific pattern of loss helps identify the affected gene [125] [126].
2. Protocol for PCR- or NGS-based MSI Testing:
- Objective: To detect instability in repetitive DNA microsatellite sequences.
- Methodology:
- DNA Extraction: DNA is isolated from matched tumor and normal (e.g., blood, buccal swab) FFPE samples.
- PCR Amplification: A panel of standardized monomorphic mononucleotide repeat markers (e.g., BAT-25, BAT-26) is amplified by PCR.
- Fragment Analysis: PCR products are sized by capillary electrophoresis. Shifts in the size distribution of tumor DNA amplicons compared to normal DNA indicate MSI.
- Classification: Tumors are classified as MSI-High (instability in ≥30-40% of markers), MSI-Low (instability in <30-40%), or Microsatellite Stable (MSS) [125] [126].
Assessment of Tumor Mutational Burden (TMB)
1. Protocol for TMB calculation using Next-Generation Sequencing (NGS):
- Objective: To quantify the total number of somatic mutations per megabase (mut/Mb) of the genome examined.
- Methodology:
- Sequencing: DNA from matched tumor-normal pairs undergoes whole-exome sequencing (WES) or targeted NGS using large panels (≥1 Mb).
- Bioinformatic Analysis:
- Variant Calling: Somatic single nucleotide variants (SNVs) and small insertions/deletions (indels) are identified.
- Filtering: Known driver mutations and germline polymorphisms are filtered out using population databases.
- TMB Calculation: The number of synonymous and non-synonymous mutations is summed and divided by the size of the coding region targeted (in megabases). The result is reported as mut/Mb [125].
- Challenges: TMB estimation can vary based on the NGS panel size and bioinformatic pipeline, highlighting the need for harmonization [125].
Assessment of PD-L1 Expression
1. Protocol for PD-L1 IHC Assay:
- Objective: To quantify PD-L1 protein expression on tumor and/or immune cells.
- Methodology:
- Assay Platform: Utilizes specific companion diagnostic IHC assays (e.g., PD-L1 IHC 22C3 pharmDx for pembrolizumab, SP142 for atezolizumab).
- Staining: FFPE tissue sections are stained with validated anti-PD-L1 antibodies.
- Scoring: Scoring methods are assay- and indication-specific. The most common are:
- Tumor Proportion Score (TPS): Percentage of viable tumor cells with partial or complete membrane staining.
- Combined Positive Score (CPS): Number of PD-L1 staining cells (tumor cells, lymphocytes, macrophages) divided by the total number of viable tumor cells, multiplied by 100 [125].
- Critical Consideration: PD-L1 expression is dynamic and can be heterogeneous within a tumor, which can lead to sampling bias [125].
Signaling Pathways and Biomarker Rationale
The biomarkers discussed are integral components of the complex biological interplay between tumors and the immune system. The following diagram illustrates the key pathways and their relationship to predictive biomarkers.
Case Studies in Biomarker-Driven Clinical Response
Real-world evidence and clinical trial data provide powerful illustrations of how these biomarkers translate into patient outcomes.
Case Series: Prolonged Response to Dual Checkpoint Blockade
A 2025 case series highlights exceptional responses to combination anti-CTLA-4 and anti-PD-1 therapy in patients with advanced solid tumors who had exhausted standard options [126]. These cases underscore the potential for durable benefit even in challenging clinical scenarios.
- Patient 1 (MSS Rectal Adenocarcinoma): A patient with microsatellite stable (MSS) rectal adenocarcinoma, a subtype typically less responsive to immunotherapy, achieved a complete response on PET/CT and remained progression-free for over 34 months after treatment with anti-CTLA-4/anti-PD-1 combination therapy. This case demonstrates that durable responses can occur even in the absence of classic MSI-H biomarkers [126].
- Patient 4 (dMMR Prostate Adenocarcinoma): A patient with advanced, deficient Mismatch Repair (dMMR) prostate adenocarcinoma experienced a complete metabolic response on PET/CT and maintained this response for over 68 months, showcasing the profound and durable efficacy of immunotherapy in a biomarker-selected population, even in a cancer type not traditionally considered immunogenic [126].
Clinical Trial: SERENA-6 and ctDNA as a Dynamic Biomarker
The phase 3 SERENA-6 trial represents a paradigm shift in using dynamic, circulating biomarkers to guide therapy. The study enrolled patients with estrogen receptor-positive, HER2-negative advanced breast cancer who were receiving first-line aromatase inhibitor therapy. Researchers used circulating tumor DNA (ctDNA) analysis to monitor for the emergence of ESR1 mutations, a known mechanism of resistance. Upon detection of the mutation (molecular progression) but before radiographic progression, patients were randomized to either switch to camizestrant or continue the original therapy. The study demonstrated a 56% reduction in the risk of progression or death with the early switch strategy, significantly improving progression-free survival (median PFS 16.0 vs. 9.2 months) [45] [127]. This trial validates the use of ctDNA as a dynamic biomarker to preemptively alter treatment and delay clinical progression.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The discovery and validation of biomarkers rely on a suite of sophisticated research tools and platforms. The following table details key solutions used in the field.
Table 2: Essential Research Reagent Solutions for Biomarker Validation
| Research Solution | Function in Biomarker Workflow | Key Examples & Applications |
|---|---|---|
| Multiplex Immunoassays | Simultaneously measure multiple protein biomarkers (e.g., cytokines, chemokines) from a single small-volume sample [66]. | Meso Scale Discovery (MSD) U-PLEX: Used for quantifying inflammatory biomarkers (IL-1β, IL-6, TNF-α) with higher sensitivity and a broader dynamic range than ELISA, and at a lower cost per sample [66]. |
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Provides high-precision, high-sensitivity quantification of proteins and metabolites for biomarker discovery and validation, capable of analyzing thousands of proteins in a single run [66]. | Applied in proteomic and metabolomic profiling to identify novel biomarker signatures with superior specificity, moving beyond traditional immunoassays [66]. |
| Next-Generation Sequencing (NGS) | Enables comprehensive genomic profiling for biomarker assessment, including TMB calculation, MSI status, and identification of specific genetic mutations [26] [125]. | Large Panels (≥1 Mb) and Whole-Exome Sequencing: Essential for accurate TMB estimation and for discovering novel genetic alterations associated with response or resistance to therapy [125]. |
| Validated Antibodies for IHC | Critical for detecting protein expression and localization in tissue sections, forming the basis of companion diagnostics for PD-L1 and dMMR [125] [126]. | PD-L1 Clones (e.g., 22C3, SP142) and MMR Protein Antibodies: Used in standardized, FDA-approved companion diagnostic tests to determine patient eligibility for specific immunotherapies [125]. |
| Digital Pathology & AI Tools | Computational analysis of digitized pathology slides to identify and quantify histological features, including biomarker expression patterns. | EAGLE (EGFR AI Genomic Lung Evaluation): An AI tool that analyzed over 8,000 lung cancer slides, reducing the need for molecular tests by over 40% while maintaining clinical standards for EGFR mutation assessment [128]. |
The comparative analysis of MSI-H/dMMR, TMB, and PD-L1 reveals a maturing but incomplete landscape for predicting immunotherapy response. While these biomarkers provide a critical foundation for precision oncology, their imperfect specificity and sensitivity highlight the complexity of tumor-immune interactions. The future of biomarker development lies in integrating multi-omic data—genomics, transcriptomics, proteomics, and digital biomarkers from wearables—to create more comprehensive predictive models [129] [130]. Furthermore, the rigorous validation pathway, exemplified by the FDA's Biomarker Qualification Program where development of a qualification plan can take a median of 32 months (and 47 months for surrogate endpoints), underscores the immense challenge of bringing new biomarkers to the clinic [131]. Success will depend on collaborative efforts, standardized analytical frameworks, and the continued adoption of advanced technologies like AI and multiplexed assays to build upon the foundational lessons learned from today's validated biomarkers.
Conclusion
The successful validation of biomarkers to predict response to immunotherapy is a multi-faceted process requiring rigorous analytical and clinical evaluation. The field is moving beyond single-analyte biomarkers towards integrated, multi-omic signatures that better reflect the complex biology of the tumor-immune interaction. Future progress hinges on standardizing assays, embracing collaborative data-sharing models, and adopting innovative trial designs that facilitate biomarker co-development. As technologies like single-cell sequencing and liquid biopsies mature, they promise to deliver more dynamic and comprehensive biomarker tools, ultimately enabling truly personalized immunotherapy and improving outcomes for a broader range of cancer patients.
References
- 1. Predictive Biomarkers in Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289453/]
- 2. Validation of biomarkers to predict response ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5109744/]
- 3. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 4. Could Flow Cytometry Provide New Prognostic Markers in ... [https://pubmed.ncbi.nlm.nih.gov/39200895/]
- 5. Companion Diagnostics Explained [https://www.foundationmedicine.com/blog/companion-diagnostics-explained-their-critical-role-cancer-care-and-our-latest-approvals]
- 6. Biomarker Validation: Common Data Analysis Concerns [https://pmc.ncbi.nlm.nih.gov/articles/PMC4122484/]
- 7. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 8. Artificial intelligence for predictive biomarker discovery in ... [https://pubmed.ncbi.nlm.nih.gov/37879443/]
- 9. The role of artificial intelligence in predicting cancer ... [https://www.sciencedirect.com/science/article/pii/S277290602500055X]
- 10. Immuno-Oncology 2025: Expert Panel Weighs in on AI, ... [https://www.cancerresearch.org/blog/immuno-oncology-2025-expert-panel]
- 11. Optimizing early-phase immunotherapy trials - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586187/]
- 12. Optimizing early-phase immunotherapy trials: the role of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1664443/full]
- 13. Predictive models for immune checkpoint inhibitor ... [https://www.sciencedirect.com/science/article/pii/S1040842825003683]
- 14. Evaluating Immune Checkpoint Inhibition Biomarkers [https://www.jax.org/education-and-learning/clinical-and-continuing-education/clinical-topics/tumor-testing/pd-l1]
- 15. Advancing immunotherapy for esophageal cancer [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1679365/full]
- 16. Biology and evolving management of resectable dMMR/ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592604/]
- 17. Inflammation and mutational burden differentially ... [https://www.nature.com/articles/s41467-025-63960-8]
- 18. Efficacy of First-Line Nivolumab Plus Chemotherapy in ... [https://www.mdpi.com/2072-6694/17/22/3716]
- 19. Nivolumab and ipilimumab combination treatment in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616531/]
- 20. A Comprehensive Oncological Biomarker Framework Guiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466961/]
- 21. Recent advances in biomarkers for predicting the efficacy ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1554871/full]
- 22. Plasma proteomics profiling identifies predictive ... [https://pubmed.ncbi.nlm.nih.gov/41197383/]
- 23. Plasma proteomics profiling identifies predictive ... [https://www.sciencedirect.com/science/article/pii/S0169500225007032]
- 24. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 25. Biomarkers in 2025: From Liquid Biopsy to AI-Driven ... [https://www.barchart.com/story/news/35377423/biomarkers-in-2025-from-liquid-biopsy-to-ai-driven-discovery-what-business-leaders-must-know]
- 26. Biomarkers Market Research Report 2025-2030 | Assay Kit ... [https://finance.yahoo.com/news/biomarkers-market-research-report-2025-084300917.html]
- 27. 寻找生物标志物来预测和优化T细胞治疗癌症的结果 [https://pcm.amegroups.org/article/view/5095/9709]
- 28. Validation of biomarkers to predict response ... [https://pubmed.ncbi.nlm.nih.gov/27895917/]
- 29. Overview of Multiplex Immunohistochemistry and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7849039/]
- 30. Prediction of checkpoint inhibitor immunotherapy efficacy ... [https://www.nature.com/articles/s41591-024-03398-5]
- 31. 肿瘤微环境的多维特征及其靶向递送策略研究进展 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382323/]
- 32. 研究宿主基因与环境因素的交互作用是癌症预防和治疗的关键 [https://paper.sciencenet.cn/htmlnews/2025/8/550539.shtm]
- 33. 超越单一生物标志物:多组学策略预测血液癌症免疫治疗结果 [https://www.ebiotrade.com/newsf/2025-11/20251106223910202.htm]
- 34. 肿瘤与微生态研究进展篇(二)——《中国恶性肿瘤学科发展报告 ... [https://wap.cacakp.com/appnews/detail/id/22694]
- 35. 肿瘤与微生态研究进展篇(三) [http://www.caca.org.cn/system/2025/05/30/030149340.shtml]
- 36. 癌症代谢生物标志物的全球研究动态:2015-2025年的文献 ... [https://www.ebiotrade.com/newsf/2025-11/20251106224116996.htm]
- 37. Biomarker-Driven Clinical Trials in Oncology [https://www.precisionformedicine.com/blog/biomarker-driven-clinical-trials-in-oncology-enrichment-stratification-all-comers-basket-when-to-use-what-and-why]
- 38. A review of phase II trial designs for initial marker validation [https://www.sciencedirect.com/science/article/abs/pii/S1551714413000682]
- 39. Adaptive Biomarker‐Based Design for Early Phase Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12510287/]
- 40. Design and Analysis of Biomarker-Integrated Clinical Trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7954851/]
- 41. A Comparative Analysis of Data Normalization Approaches ... [https://www.mdpi.com/2079-3197/12/7/137]
- 42. a continuous challenge for laboratory professionals - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4062337/]
- 43. Prediction performance comparison of biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11062874/]
- 44. Immunoassays: Analytical and Clinical Performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10889711/]
- 45. Nuanced Biomarker Tests and Immunotherapy Strategies ... [https://www.onclive.com/view/nuanced-biomarker-tests-and-immunotherapy-strategies-may-usher-asco-2025-data-into-the-clinic]
- 46. Pre-Analytical, Analytical, & Post-Analytical Phases of Lab ... [https://genemod.net/blog/pre-analytical-lab-testing-phase]
- 47. Analytical Performance of ELISA Assays in Urine [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0149471]
- 48. A rapid and highly sensitive biomarker detection platform ... [https://www.nature.com/articles/s41598-020-75011-x]
- 49. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 50. Analytical Validation of Blood-Derived Tumor Mutation ... [https://www.sciencedirect.com/science/article/pii/S1525157825001850]
- 51. Precision-Driven Biomarker Validation: A Biotech ... [https://www.criver.com/eureka/precision-driven-biomarker-validation-biotech-perspective-part-i]
- 52. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 53. Preclinical vs. Clinical Biomarkers: Understanding Their ... [https://blog.crownbio.com/preclinical-vs-clinical-biomarkers-understanding-their-distinct-roles-in-drug-development]
- 54. Application of spatial and single-cell omics in tumor ... [https://www.sciencedirect.com/science/article/pii/S3050474025000254]
- 55. Single-cell RNA sequencing: enhancing the predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12493173/]
- 56. Integrative mass spectrometry-driven multi-omics and ... [https://www.sciencedirect.com/science/article/pii/S2589909025000541]
- 57. Advances in Mass Spectrometry-Based Single Cell Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC10045136/]
- 58. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 59. Variant biomarker discovery using mass spectrometry- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10165118/]
- 60. Comprehensive mass spectrometry based biomarker ... [https://www.sciencedirect.com/science/article/pii/S2212968516300393]
- 61. Single-cell RNA sequencing technologies and ... [https://www.nature.com/articles/s12276-018-0071-8]
- 62. 2025 SITC共识声明:免疫治疗临床方案的基本生物标志物 [https://www.medsci.cn/guideline/show_article.do?id=f750b1c00a2230cb]
- 63. 临床试验中的指标敏感性、特异性_敏感性和特异性计算-CSDN博客 [https://blog.csdn.net/weixin_41033647/article/details/126453246]
- 64. 敏感性、特异性、灵敏度...检验人必须弄清楚的十大问题!_全国体外诊断网(全国实验医学网) [https://caivd-org.cn/article.asp?id=7879]
- 65. 什么是灵敏度、特异性和 ROC 曲线 · 白汤四物 [https://www.fournoas.com/posts/What-is-sensitivity-specificity-and-receiver-operating-characteristic/]
- 66. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 67. Guide to Multiplex Immunoassays: Multiplex ELISA and More [https://www.thermofisher.com/blog/life-in-the-lab/guide-to-multiplex-immunoassays-multiplex-elisa-and-more/]
- 68. The Evolution of Multiplex Immunoassay Technologies [https://olink.com/blog/the-evolution-of-multiplex-immunoassay-technologies]
- 69. 2025 SITC 共识声明:免疫治疗临床方案的基本生物标志物 [https://www.pfizermedicalinformation.cn/clinical-guidelines/3932]
- 70. of Validation to predict response to immunotherapy in... biomarkers [https://jitc.biomedcentral.com/articles/10.1186/s40425-016-0179-0]
- 71. ROC Analysis with Covariate Adjustment Using Neural ... [https://arxiv.org/html/2510.14494v1]
- 72. ROC Plotter - Online ROC analysis [https://rocplot.com/]
- 73. Multi-omics and experimental validation studies reveal key... [https://link.springer.com/article/10.1186/s13098-025-01899-y]
- 74. Biology-guided deep learning predicts prognosis and ... [https://www.nature.com/articles/s41467-023-40890-x]
- 75. Machine learning driven biomarker selection for medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12157214/]
- 76. Predicting Immunotherapy Efficacy with Machine Learning ... [https://pubmed.ncbi.nlm.nih.gov/40649716/]
- 77. 综述:新兴的特征以及肿瘤复杂性和异质性的增加 [https://www.ebiotrade.com/newsf/2025-11/20251110083411543.htm]
- 78. Recent advances in the diagnosis and management of Ph+ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439738/]
- 79. 肿瘤学临床实验设计的发展趋势 [https://m.ofweek.com/medical/2025-07/ART-11163-8500-30666412.html]
- 80. 2025 ICML大师课丨追踪动态靶标,推进套细胞淋巴瘤风险评估 [https://www.ihemato.com/Detail?id=790]
- 81. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11931240/]
- 82. CAP Publishes New Guideline on PD-L1 Testing ... [https://www.cap.org/member-resources/articles/cap-publishes-new-guideline-on-pd-l1-testing-of-patients-with-lung-cancer]
- 83. Interlaboratory comparison of serum lipoprotein(a) ... [https://pubmed.ncbi.nlm.nih.gov/40102115/]
- 84. Comparative evaluation of six immunoassays for the detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7832212/]
- 85. Comparative evaluation of in-house ELISA and two ... [https://www.nature.com/articles/s41598-025-97050-y]
- 86. Viral Vector | Capsid Titer Interlab Study RFA2025.03 [https://www.niimbl.org/projects-programs/viral-vector-capsid-titer-study-rfa2025-03/]
- 87. Predictive Modeling for Immunotherapy Response in Cancer [https://oncodaily.com/oncolibrary/immunotherapy-respons]
- 88. Informing immunotherapy with multi-omics driven machine ... [https://www.nature.com/articles/s41746-024-01043-6]
- 89. Beyond single biomarkers: multi-omics strategies to predict ... [https://link.springer.com/article/10.1007/s10238-025-01902-w]
- 90. Algorithms and tools for data-driven omics integration to ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06446-x]
- 91. Evaluation and comparison of multi-omics data integration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8384175/]
- 92. Integrative analysis of multi-omics data and gut microbiota ... [https://www.nature.com/articles/s41598-025-08915-1]
- 93. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 94. Liquid biopsy for cancer immunotherapy: Biomarkers to ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525003376]
- 95. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 96. Liquid biopsy: current technology and clinical applications [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-022-01351-y]
- 97. The Evolution of Affordable Technologies in Liquid Biopsy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10670715/]
- 98. Identification of prognostic liquid biopsy biomarkers in patients ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06957-7]
- 99. Liquid biopsy - a narrative review with an update on current ... [https://pubmed.ncbi.nlm.nih.gov/40772765/]
- 100. Data and sample sharing as an enabler for large-scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9748546/]
- 101. How C-Path's Biomarker Data Repository Brings Patients ... [https://c-path.org/story/how-c-paths-biomarker-data-repository-brings-patients-to-the-table-to-discuss-biomarkers-and-their-impact/]
- 102. External validation of biomarkers for immune-related ... [https://pubmed.ncbi.nlm.nih.gov/36248910/]
- 103. External validation of biomarkers for immune-related ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.1011040/full]
- 104. Unlocking the Power of Digital Biomarkers in Clinical Trials [https://acrpnet.org/2025/08/19/unlocking-the-power-of-digital-biomarkers-in-clinical-trials]
- 105. Predictive biomarkers of immunotherapy response with ... [https://www.nature.com/articles/s41401-023-01079-6]
- 106. Biomarker Qualification at the European Medicines Agency [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313861/]
- 107. Biomarker Guidances and Reference Materials [https://www.fda.gov/drugs/biomarker-qualification-program/biomarker-guidances-and-reference-materials]
- 108. FDA Approvals in Oncology: July-September 2025 | Blog [https://www.aacr.org/blog/2025/10/02/fda-approvals-in-oncology-july-september-2025/]
- 109. Opinions and letters of support on the qualification of novel ... [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-advice-protocol-assistance/opinions-letters-support-qualification-novel-methodologies-medicine-development]
- 110. Medical devices | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/human-regulatory-overview/medical-devices]
- 111. Evaluation of Companion Diagnostics in Scientific Advice and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9120537/]
- 112. Companion Diagnostics Trends in Precision Medicine [https://www.leicabiosystems.com/us/educational-resources/articles/companion-diagnostics-precision-medicine-depth-review-and-future-trends/]
- 113. List of Cleared or Approved Companion Diagnostic Devices [https://www.fda.gov/medical-devices/in-vitro-diagnostics/list-cleared-or-approved-companion-diagnostic-devices-in-vitro-and-imaging-tools]
- 114. Companion diagnostics in targeted therapy | LabLeaders [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/companion-diagnostics-targeted-therapy.html]
- 115. Forging Forward - Our Progress in Biopharmaceutical ... [https://www.foundationmedicine.com/blog/progress-biopharma-partnerships-outlook-2025]
- 116. FDA-approved MI cancer seek test enhances tumour ... [https://ecancer.org/en/news/26894-fda-approved-mi-cancer-seek-test-enhances-tumour-profiling-for-precision-oncology]
- 117. Companion Diagnostics Market Forecast Report 2025-2034 | [https://www.globenewswire.com/news-release/2025/07/23/3120013/28124/en/Companion-Diagnostics-Market-Forecast-Report-2025-2034-Next-Generation-Sequencing-Enhancing-Accuracy-Precision-Medicine-Advancements-Propel-Growth.html]
- 118. Clinical Trial Designs for Predictive Biomarker Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2734400/]
- 119. Overview of clinical study designs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11009715/]
- 120. Immunotherapy-related biomarkers: Confirmations and ... [https://www.sciencedirect.com/science/article/pii/S1040842823002238]
- 121. Researchers find new biomarker for improved ... [https://www.mdanderson.org/newsroom/research-newsroom/researchers-find-new-biomarker-for-improved-immunotherapy-response-in-solid-tumors.h00-159780390.html]
- 122. Longitudinal liquid biopsy identifies an early predictive ... [https://www.nature.com/articles/s41467-025-63538-4]
- 123. Navigating biomarker validation [https://www.tempus.com/resources/content/articles/navigating-biomarker-validation/?srsltid=AfmBOoonWNdCI-dqF9DoS7jQXwnhYBZMc37UVEfoAE6k2HUJNxBwc1ww]
- 124. About Biomarkers and Qualification [https://www.fda.gov/drugs/biomarker-qualification-program/about-biomarkers-and-qualification]
- 125. Lessons learned from a decade of immune checkpoint ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11971148/]
- 126. Prolonged response to dual immune checkpoint blockade ... [https://www.nature.com/articles/s41698-025-01115-0]
- 127. ASCO 2025 Showcases New Oncology Paradigms, From ... [https://biopharmaapac.com/report/80/6448/asco-2025-showcases-new-oncology-paradigms-from-breast-cancer-breakthroughs-to-ai-led-precision-medicine.html]
- 128. MSK Research Highlights, July 15, 2025 [https://www.mskcc.org/news/msk-research-highlights-july-15-2025]
- 129. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 130. Biomarker discovery pipeline: 3 Critical Steps 2025 [https://lifebit.ai/blog/biomarker-discovery-pipeline/]
- 131. Timelines and Takeaways from the Biomarker Qualification ... [https://link.springer.com/article/10.1007/s43441-025-00889-6]